Abstract
A 48-year-old-male diagnosed transitional cell carcinoma of bladder was underwent laparoscopic radical cystectomy with intracorporeal Y pouch neobladder. The patient's Y pouch neobladder was described in three-dimensional printing for follow-up and in order to help the surgeon understand the morphology and capacity after surgery. Laparospcopic radical cystectomy with intracorporeal neobladder is challenging. In this case, we performed the first case of intracorporeal orthotopic Y pouch neobladder and investigated an early postoperatively using a three-dimensional digital printing model in order to help with pouch after surgery.
Keywords: Orthotopic intracorporeal Y-Pouch neobladder, 3D digital printing model, Materialise mimics
Highlights
-
•
Case report of successful transitional cell carcinoma of bladder treatment.
-
•
Special attention for treatment for transitional cell carcinoma underwent laparoscopic radical cystectomy with orthotopic intracorporeal Y pouch neobladder.
-
•
Three-dimensional digital printing model for surgical post op pouch evaluation.
Introduction
Traditionally, open radical cystectomy has been the gold standard treatment for patients with muscle invasive bladder cancer and high-risk nonmuscle invasive bladder cancer. Laparoscopic radical cystectomy has been gaining in popularity and feasible with superior outcomes in terms of blood loss, shorter hospital stay and earlier return to bowel function.1 Prolong operative time has remained an important issue, and many centers preferred extracorporeal urinary diversion to reduce the operative time and costs. Intracorporeal ileal neobladder still remains technically challenging with a significant learning curve and is usually performed only in centers with experienced surgeons.
This is the first case of laparoscopic radical cystoprostatectomy with intracorporeal Y pouch neobladder in Thailand. The Y pouch, also known as a Tanta pouch, was first described in 1988.2 The Y pouch was reconstructed using 40 cm of terminal ileum, which consists of the central detubularized segments arranged in a U-shape and two limbs for ureteroileal anastomosis.2 A recent report demonstrated similar functional outcomes of the Y pouch compared with the conventional spherical pouch with daytime and nighttime. It has been shown that the Y pouch is a low pressure, high volume reservoir with similar long-term functional outcomes compared with other spherical pouches.3
Case presentation
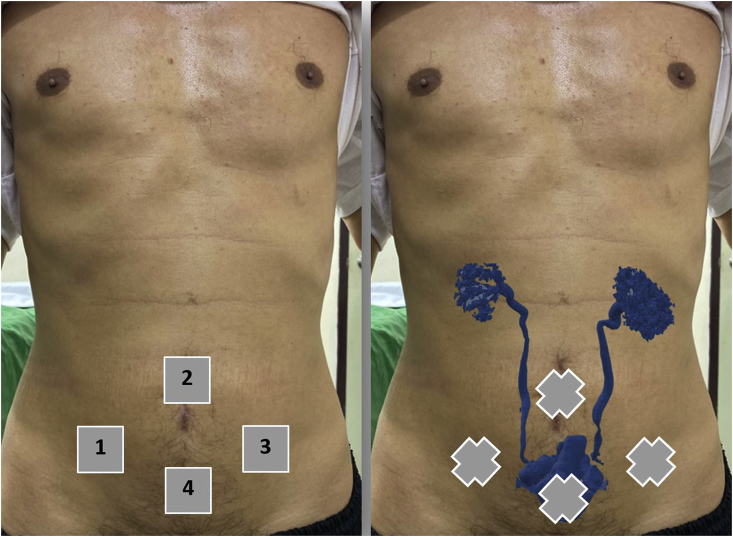
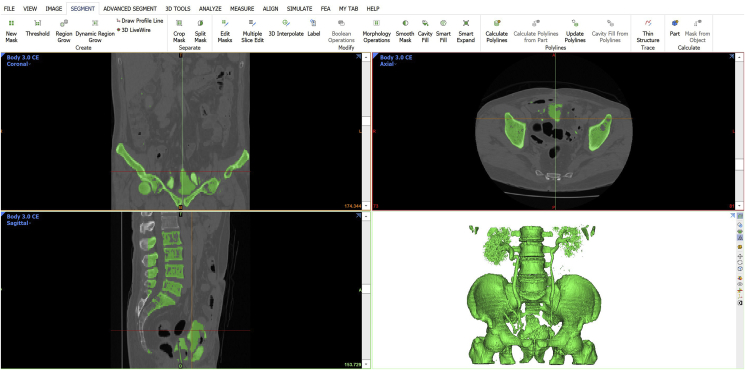
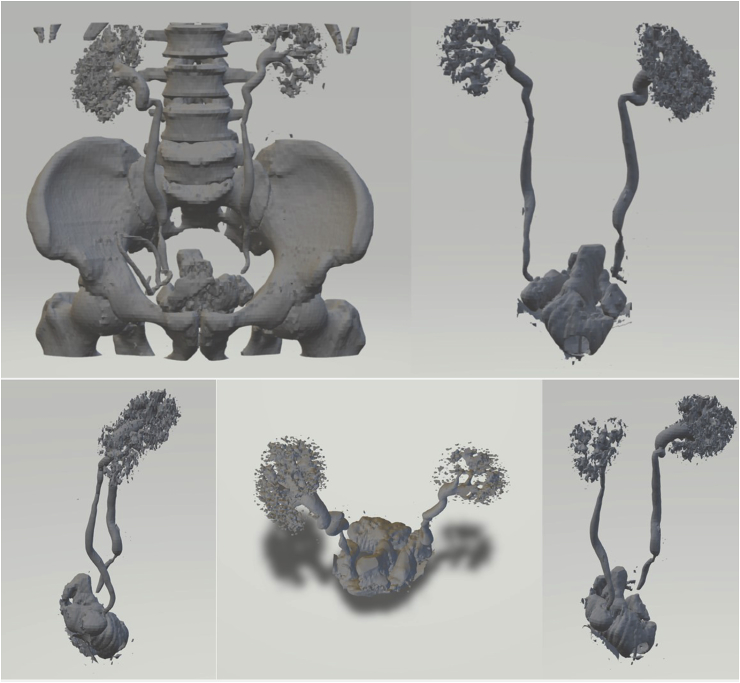
A 48-year-old-male with a diagnosis of muscle invasive bladder carcinoma. A 20F foley cathether was inserted into the bladder. A four-port approach is used (Fig. 1). The patient was placed in a steep Trendelenburg position. The nerve-sparing cystoprostatectomy was completed followed by a standard pelvic lymph node dissection. Surgical postoperatively evaluation by the three-dimensional (3D) printing technique (Fig. 2). The imaging techniques base on computed tomography (DICOM format) was used and analyzed by Materialise's software (Mimic) to standard triangle language (STL file) for 3D printing. Post-operatively outcome was satisfactory and assessed using three-dimensional (3D) printing (Fig. 3).
Fig. 1.
Port placements: 10-mm at right pararectal area (1); 12-mm at umbilical camera port (2); 5-mm at left pararectal (3) and 5 mm above pubic symphysis (4).
Fig. 2.
Surgical post-op Y pouch morphology after 3D-reconstruction materialise's software.
Fig. 3.
The 3D digital printing model.
The creation of the Y pouch neobladder, after completion of the radical cystoprostatectomy and lymphadenectomy, both ligated ureters. An estimated 40-cm segment of terminal ileum 15 cm away from the ileocecal valve was identified as the bowel segment was measured using paper ruler, as well as relation to pelvic anatomy. The ileal segment was brought down to the pelvis to ensure adequate mesenteric length to allow for a tension-free urethroileal anastomosis. The 40-cm segment was arranged in a U-shaped configuration that was made out of two central segments of 14 cm each and two limbs of 6 cm each. A stay suture was placed to mark the most distal portion of the U-shaped loop. The urethroileal anastomosis was completed using the 3/0 V-Loc® suture over a 20F Foley catheter. The proximal and distal end of the 40-cm segment was transected using an Endo-GIA® stapler. The bowel continuity was restored by performing functional end-to-end or anatomical side-to-side anastomosis using an Endo-GIA® stapler. The two central limbs were detubularized at the antimesenteric borders, and the two limbs were left intact. The posterior plate of the two central detubularized segments was joined using 3/0 V-Loc® sutures in a running fashion. This was followed by closure of the anterior plate in a similar fashion.
The ureters were anastomosed to the lateral aspect of the two limbs with 4/0 Vicryl® sutures using the Lich Gregoir technique. In this case, the ureteroileal anastomosis was performed over a 6.8 Fr Double-J stent that inserted via uretethra inside head-cut Foley catheter passed Y pouch through both ureter. After the completion of the anastomosis, the Y pouch was tested with water 200 mL; no leakage was seen. The operating time was 340 minutes with minimal intraoperative blood loss without complications. The urethral catheter and Double-J stents were removed at postoperative day 14 after satisfactory cystography showing an intact neobladder with no significant upper tract dilatation.
Discussion
In this case, the ileal segment was taken approximately 15-cm away from the ileocecal valve to ensure adequate mesenteric length for the urethroileal anastomosis. Before transecting the bowels, the ileal segment was brought down to the pelvis to ensure that the mesentery was long enough to ensure a tension-free urethroileal anastomosis. In most series, the operative time is still significantly longer than extracorporeal urinary diversion, and a steep learning curve is expected to perform surgery of such complexity.4,5 From this first case of Y pouch neobladder has a few advantages over the more complex spherical pouches. The Y pouch is easy to construct without any need to fold the bowel segments and less manipulation of the bowel is needed. With the presence of dual limbs for the ureteroileal anastomosis, there is no need to transpose either ureter under the sigmoid mesocolon. This means less traction and less skeletalization of the ureters, therefore making the Y a good option for cases with short ureteral length.
Many surgeons concerned about Y pouch may provide an easy retrograde approach to the upper tract may introduce infection and deterioration. In this case, infection free with good daytime and nighttime continence. The post-op computerized tomography examined a good Y pouch reservoir without bilateral hydroureteronephrosis. Actually, 3D reconstruction mostly examined benefit for preoperative planning evaluation to improve surgical precision, reduce operative time but in this case we used this 3D reconstruction technique for evaluation novel Y pouch neobladder about structural and functional reconstructive outcomes such as contouring of neobladder, capacity and refluxing hydronephrosis and also easy to illustrate Y pouch that easier to perform than conventional spherical pouches without compromising on functional outcomes. It may therefore be a good alternative for patients undergoing laparoscopic radical cystectomy with intracorporeal neobladder.
Conclusion
The successful of intracorporeal Y pouch neobladder is safe and feasible and provides a good alternative for patients undergoing laparoscopic radical cystectomy with intracorporeal neobladder. The patient may be longer follow-up will be needed to conclude the functional outcomes and three-dimensional printing technique could be optional for surgical post-op evaluation in this technique.
Author contributions
Dr. Tanan Bejrananda is the drafted the article, performed surgery in this technique and following up this patient. Dr. Wongthawat Liawrngrueang corresponding author, drafted the article, study design and use of Mimics v20 (Materialise Inc., Leuven, Belgium, licensed by the Faculty of Medicine, Prince of Songkla University) created for 3D printing analysis. All authors approved the final version of the manuscript accepted for publication.
Funding
None.
Consent
The publication of this study has been consented by the relevant patient.
Ethical approval
The study was approved by our research committee, Songklanagarind Hospital, Faculty of Medicine, Prince of Songkla University, Thailand.
Guarantor
Tanan Bejrananda, M.D. and Wongthawat Liawrungrueang, M.D.
Declaration of competing interest
None
Acknowledgement
We gratefully acknowledge the Songklanagarind Hospital for their help in our patient.
References
- 1.Tang K., Li H., Xia D. Laparoscopic versus open radical cystectomy in bladder cancer: a systematic review and meta-analysis of comparative studies. PloS One. 2014;9(5) doi: 10.1371/journal.pone.0095667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.El-Matteet M.S., Emran M., El-Abd S., El- Mahrouky A. Tanta pouch, a double barrel ileo-uretero-cystoplasty. A new continent ileal reservoir. J Urol. 1988;139 242A. [Google Scholar]
- 3.Hassan A.A., Elgamal S.A., Sabaa M.A., Salem K.A., Elmateet M.S. Evaluation of direct versus non-refluxing technique and functional results in orthotropic Y-ileal neobladder after 12 years of follow up. Int J Urol. 2007;14:300–304. doi: 10.1111/j.1442-2042.2006.01716.x. [DOI] [PubMed] [Google Scholar]
- 4.Collins J.W., Tyritzis S., Nyberg T. Robot-assisted radical cystectomy (RARC) with intracorporeal neobladder— what is the effect of the learning curve on outcomes? BJU Int. 2014;113:100–107. doi: 10.1111/bju.12347. [DOI] [PubMed] [Google Scholar]
- 5.Collins J.W., Wiklund P.N., Desai M.M., Goh A.C., Gill I.S. Total intracorporeal robotic cystectomy: Are we there yet? Curr Opin Urol. 2013;23:135–140. doi: 10.1097/MOU.0b013e32835d4cda. [DOI] [PubMed] [Google Scholar]