Abstract
Surgically Facilitated Orthodontic Therapy (SFOT) in combination with bone augmentation and the placement of anchorage devices installed into bone have been used to accelerate and facilitate orthodontic treatment. This is usually performed after flap surgery, which is associated with moderate morbidity, as well as possible negative sequale such as gingival recession. The present case report illustrates the clinical benefits of vestibular incision subperiosteal tunnel access (VISTA) for SFOT, and tissue augmentation to facilitate orthodontic therapy. VISTA entails making vertical incision(s) in the vestibule followed by subperiosteal elevation of tunnels to provide direct access to the facial alveolar bone. Unlike previously reported vestibular access surgical procedures, VISTA allows for wider elevation of an access tunnel for clear visual and surgical access to perform careful inter-radicular corticotomy. The present report describes VISTA for corticotomy surgery (anterior mandible and maxillary teeth) in combination with the placement of titanium fixation devices and bone augmentation to facilitate orthodontic treatment of an adult female with borderline Class II Division 1 malocclusion, with excessive overjet and deepbite. In view of the fact that VISTA does not require surface incisions in the gingival margins or papillae, it potentially minimizes gingival recession that sometimes accompanies flap surgery.
Keywords: Corticotomy, orthodontics, regional acceleratory phenomenon, tooth intrusion, vestibular incision subperiosteal tunnel access
Introduction
Reducing the orthodontic treatment time is attractive for patients and may eliminate the risk of external apical root resorption,[1] demineralization,[2] and loosing patient compliance.[3] Various systemic and localized methods have been used to accelerate the orthodontic tooth movement.[3] The use of prostaglandin E2,1,25-dihydroxy Vitamin D3, and parathyroid hormone as well as using pulsed electromagnetic fields, electrical currents, distraction osteogenesis, mechanical vibration, low-level laser irradiation, and corticotomy, have been reported to accelerate orthodontic tooth movement.[3,4]
Animal studies demonstrated that alveolar corticotomies with bur/piezosurgery[5,6,7] lead to a regional acceleratory phenomenon (RAP). The RAP, described by Frost,[8,9,10] is proportional to the extent of the surgical insult and associated with a localized surge in osteoclastic and osteoblastic activities that collectively lead to a decrease in bone density and an increased bone turnover, facilitating orthodontic tooth movement.[5,7,11,12]
Accelerated orthodontics using alveolar corticotomies with/without augmentation bone grafting has been described by Wilcko et al.[13] and has the potential to resolve malocclusions 3–4 times faster.[14] Various terminologies such as “periodontally accelerated osteogenic orthodontics” and modifications have been introduced, but techniques are generally involve full-thickness periosteal flap reflection followed by the alveolar bone corticotomies (with surgical burs or piezotome), at labial/lingual sides, in the area of desired tooth movement.[14] It has been recommended to see the patient every 2 weeks after the surgery for orthodontic adjustments. Generally, fixed appliances are placed a week before surgery and the appliance is activated at the time of surgery.[14]
The present case report describes a novel approach of using the vestibular incision subperiosteal tunnel access (VISTA)[15] for corticotomy surgery in combination with placement of mini implants[16] and orthodontic miniplate with tube (C-tube)[17,18,19,20] to facilitate orthodontic treatment of an adult case with Class II division 1 malocclusion and deep bite.
Case Report
Summary of the clinical findings
The patient was a 42-year-old female, presenting with Class II division I malocclusion on Class II skeletal base, slight facial asymmetry at the lower third of the face, deep overbite, increased overjet, and proclined maxillary incisors [Figures 1 and 2]. She presented with a convex profile with a retrognathic mandible, pronounced labiomental fold, and a dominant chin. The molar relationship was asymmetric, full Class II on the right side and Class I on the left side. There was some spacing in the maxillary arch and mild crowding in the mandibular arch. Medically, there was no relevant medical condition.
Figure 1.

Pre-treatment clinical images. Facial photographs show repose and smile views. Clinical intra-oral images illustrate excessive horizontal and vertical overlaps of the dentition, consistent with Class II Division 1 malocclusion
Figure 2.
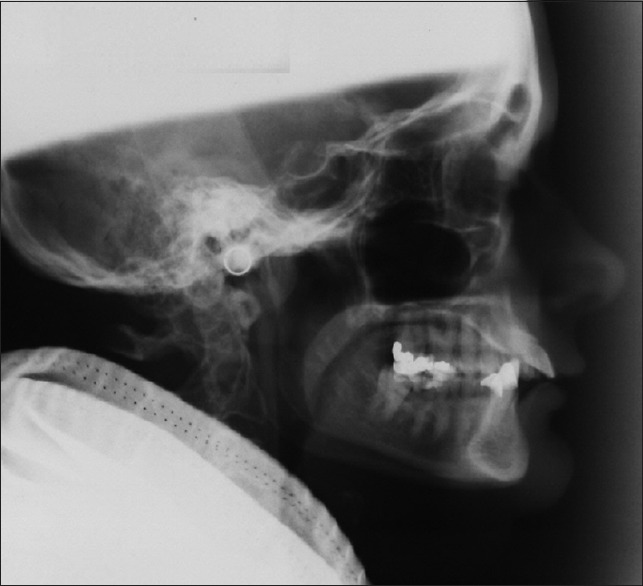
Pre-treatment cephalogram illustrating Class II skeletal structure
Intraoral and radiographic examination revealed restorations on teeth 2, 3, 14, 15, 18, 19, 21, 22, 31, 32, with teeth 22 and 25 had root canal treatment [Figure 3]. Bone loss around teeth 7 and 8, and mobility of teeth 7, 8, 9, and 10 were noted. There was a missing mandibular incisor. The patient received previous orthodontic treatment in 1995 and 1999 in another practice, but this was not successful in correcting the increased overjet and deep overbite.
Figure 3.
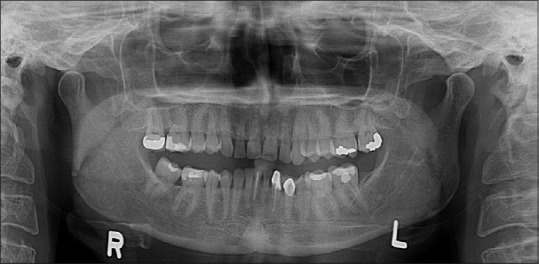
Initial panoramic radiograph illustrates the pre-operative conditions. Supra-eruption of mandibular anterior teeth is evident
Treatment plan
She was diagnosed as a borderline orthognathic case and the combined orthodontics and bilateral sagittal split osteotomy to advance the mandible was initially suggested to her, but after comprehensive risk/benefit assessment with the maxillofacial surgeon, orthodontists and periodontist, she decided to have orthodontic treatment only with intrusion of the anterior teeth to correct her deep overbite and reduce the increased overjet. It was decided to use the VISTA[15] to provide access for corticotomy in combination with simultaneous placement of mini implants,[16] initially, and miniplates at a later stage (C-tube),[17] to facilitate orthodontic treatment.
Sequence of treatment
Following scaling and root planning, the patient was bonded with ceramic self-ligating brackets in the maxillary arch and stainless steel self-ligating brackets in the mandibular arch.
Following initial alignment with NiTi wires and approximately, after 9 months of active orthodontic treatment, a VISTA approach was used simultaneously with vestibular incisions (anterior of 22 and 27) followed by elevation of the full-thickness subperiosteal tunnel flap over teeth 21–28. Corticotomies with piezotome was carried out in the mandible (teeth 22–27) and simultaneously 2 mini implants were placed (anterior mandibular area, between teeth 22/23 and 26/27, Ace Ortho screw, 8 and 10 mm, respectively) [Figure 4]. A mucograft membrane infused with PGDF was also placed under the tunnel and the VISTA approach was sutured back using a 6.0 polypropylene suture. A similar approach was used in the maxilla, 3 weeks later, and 2 C-tubes (posterior maxilla above teeth 3 and 14) were placed and fixed with 5-mm bone screws. Corticotomies were also simultaneously done for maxillary teeth.
Figure 4.

The VISTA technique was used for corticotomy and adjunctive augmentation of the recipient site. The procedure consisted of two vestibular vertical incisions positioned between canines and lateral incisors. The incision was made through the mucosa and periosteum to elevate a subperiosteal tunnel, gaining access to the facial alveolar bone. The tunnel elevation was extended and retracted in an effort clearly visualize the alveolar bone and perform careful inter-radicular corticotomy. A series of piezosurgery inserts (OT7, OT8R, OT8L) were used to make the corticotomy cuts. Two orthodontic titanium screws were placed between lateral incisor and canine (Ace Surgical Ortho screws, 8 and 10 mm) to provide effective anchorage. The VISTA technique is differentiated from previous techniques for vestibular access and corticotomy, since the VISTA technique enabled much wider tunnel elevation and direct visual access to the surgical field
Class II elastics and intrusive mechanics using elastic power chains, in the mandibular anterior area, were subsequently used to correct the Class II malocclusion, reduce the overjet, and intrude the lower incisors [Figure 5], to correct the deep bite. Glass ionomer cement was also used to disarticulate the bite and remove occlusal interferences. To achieve more intrusion of mandibular incisors, approximately 15 months into active orthodontic treatment, 2 mini implants in the anterior mandible were removed and replaced with a C-tube, using the VISTA approach. The C-tube was secured in place with 4-mm and 5-mm bone screws [Figures 6 and 7].
Figure 5.

Orthodontic treatment resumed immediately following surgical procedure of VISTA, corticotomy, and installation of titanium screws and plates. Mandibular titanium screws were connected to the orthodontic arch wire through an elastic chain. The maxillary titanium plates were connected to the orthodontic brackets with elastic chains
Figure 6.

Orthodontic treatment continued, utilizing the maxillary titanium plates. As intrusion of mandibular teeth progressed, it was necessary to replace the titanium screws with a single titanium plate in the midline. The titanium plate was connected to the orthodontic brackets with elastic chains
Figure 7.

Mid-therapy panoramic radiograph taken at 14 months following initiation of orthodontic therapy, showing significant progress toward intrusion of mandibular teeth and establishment of a more harmonious occlusal plane. The radiographic studies were used to monitor the patient for adverse response in the teeth (eg root resorption) or periodontal structures (eg. marginal bone loss, peri-apical pathology, etc)
In the end, achieving the Class I molar relationship on both sides was found to be challenging, which was due to the tooth size discrepancy caused by relatively small maxillary lateral incisors, malformed mandibular second premolars, and the presence of three mandibular incisors [Figures 8-10]. The whole treatment took 21 months.
Figure 8.

Post-therapy intra-oral clinical images showing significant intrusion of mandibular teeth and establishment of a more harmonious occlusal plane. It is notable that the periodontal status was maintained in a healthy manner following comprehensive therapy which did not lead to significant gingival recession
Figure 10.

Post-therapy clinical images, showing extra-oral and intra-oral improvements
Figure 9.

Post-therapy panoramic radiograph taken at 22 months following initiation of orthodontic therapy, showing significant intrusion of mandibular teeth and establishment of a more harmonious occlusal plane. The comprehensive surgical and orthodontic therapy was uneventfully completed with no adverse consequences to the teeth and periodontal structures
Overview of Vestibular Incision Subperiosteal Tunnel Access for Surgical Corticotomy
The VISTA[15] technique for corticotomy and adjunctive augmentation of the recipient site entails a vestibular access incision. The location of the access incision depends on the sites being treated. In the maxillary anterior region, the midline frenum is an optimal location that provides access to two teeth in either direction posteriorly. Additional vestibular incisions are generally required anterior of each canine. The incision is made through the periosteum to elevate a subperiosteal tunnel, gaining access to the facial osseous plate. Beginning at the base of the interdental papilla, the access incision is extended apically approximately 10 mm to 15 mm or as long as necessary to provide adequate access to the alveolar bone. The VISTA elevator is introduced through the vestibular access incision and inserted between periosteum and bone to elevate the periosteum away from the bone, creating the subperiosteal tunnel. A series of periosteal elevators are used for the elevation of subperiosteal tunnel. Specially designed elevators (Regenimmune, Inc. Woodland Hills, CA) are used for creating the tunnel from the initial access in a lateral and coronal direction. A contiguous tunnel is created from the vestibular region through the gingival sulci of the teeth and under each of the papillae.
It is important to extend the tunnel elevation to an extent necessary to allow for access to the facial plate to perform the required osteotomy cuts. To accomplish tension-free gingival mobilization, the subperiosteal tunnel is extended beyond the mucogingival margin, as well as through the gingival sulci of the teeth being augmented. Furthermore, the subperiosteal tunnel is extended interproximally under each papilla as far as the embrasure space permits, without making any surface incisions through the papillae. As in the maxilla, the VISTA approach to mandibular corticotomy entails creating a subperiosteal tunnel under the buccal gingiva of the teeth requiring treatment. Choosing an appropriate access incision site is particularly critical in the mandible, especially when addressing posterior corticotomy.
An acute awareness of the location of the mental foramen, mental neurovascular bundle, and its associated branches is necessary to avoid damage following the initial incision and subsequent full-thickness mucoperiosteal dissection. Therefore, given the position of the mental foramen, the optimal location of the access incision is in the vestibule between the mandibular lateral incisor and canine teeth. If necessary, the incision may be positioned between canine and first premolar. Vestibular incisions should not be placed between mesial of the first premolar to distal of the second premolar to avoid severing branches of this vital sensory structure. The availability of three-dimensional imaging such as cone-beam computed tomography would assist in identifying the exact location of the mental foramen.
Once the creation of the subperiosteal tunnel is completed, piezosurgery saws are used to make the corticotomy cuts of approximately 5-mm long and 3-mm deep. Straight or angled piezosurgery saws are used to access the vertical and horizontal corticotomy cuts.
Discussion
The present case report described the treatment of a borderline female adult with Class II malocclusion. Corticotomy-assisted orthodontics has offered a new perspective for borderline orthognathic cases and presented with an expanded envelope of tooth movement[21] as well as accelerating orthodontic tooth movement.[22,23,24] This means with corticotomy-assisted orthodontics or its combination with alveolar bone grafting (Periodontally Accelerated Osteogenic Orthodontics [PAOO][25]) greater retraction, protraction, intrusion, and extrusion for central incisor tooth movements in the maxilla and mandible may be possible.[21] Using mini implants and miniplates, as skeletal anchorage, in combination with PAOO or corticotomy facilitated orthodontics can offer treatment for some severe malocclusions, where orthognathic surgery is the most common approach,[19,26] or at least, reduce the complexity of the orthognathic surgery,[27] as well as reducing the treatment time for orthognathic cases.[28]
Recently, by assessing the recession scores (sum of the recession depths), it was reported that, overall, using localized piezoelectric alveolar decortication was not associated with an increase in a gingival recession.[29] However, similar to all periodontal flap surgery procedures, potential negative sequelae of surgical corticotomy with flap surgery is the soft tissue recession in mid-facial, as well as the loss of interdental papilla.[30,31] The potential loss of periodontal attachment in participants with preexisting bone dehiscences may lead to negative esthetic outcomes that can adversely affect the outcome of therapy, necessitating simultaneous hard-tissue augmentation via a flap surgery[25] or tunneling technique.[29,32] This is particularly important as the beneficial effect of corticotomy is mainly in the first 4 months,[29] and the addition of second-stage surgery may become relevant. Therefore, attempts to reduce the gingival margin discrepancies or residual scars,[29] and reducing unnecessary flap reflection are of great importance to the profession. In order to reduce the invasiveness of corticotomy techniques,[33] flapless alternatives to the RAP technique that employ piezoelectric devices,[12,32] reinforced scalpels and mallets,[34] piezopuncture,[35] or micro-osteoperforations[36] have been proposed.
In an effort to avoid some of the inherent limitations and potential negative sequelae of surgical corticotomy, VISTA was employed in the case series reported herein. Compared to flap surgery, VISTA is a minimally invasive approach, which has been utilized for the treatment of multiple contiguous recession defects, alveolar ridge augmentation, as well as traction of impacted teeth in the aesthetic zone.[15,37,38,39,40,41,42,43,44] The rationale of VISTA is to access the alveolar bone through one or more vertical incisions made in the vestibule without any surface incisions in the gingival margins or papillae. This approach has been demonstrated to be effective in achieving bone and soft tissue augmentation.
Conclusions
The present case demonstrates the application of VISTA for corticotomy and augmentation as adjunct to orthodontic therapy. The prospective randomized controlled clinical trial is warranted to compare the efficacy of the approach outlined herein to the conventional approach of elevating mucoperiosteal surgical flaps for corticotomy as well as bone- and soft-tissue augmentation.
Clinical Relevance: Application of VISTA allowed for clear direct visual and surgical access to the alveolar bone without incision or flap in the gingival margins to performa careful inter-radicular corticotomy. Surgically facilitated orthodontic therapy (SFOT) has been shown to be useful in accelerating the therapy and avoiding some adverse effects such as root resorption. However SFOT is sometimes accompanied with gingival recession secondary to flap reflection. The avoidance of gingival margin incision lead to surgical and orthodontic therapy with stable periodontal tissues. The combination of surgical and orthodontic therapy in conjunction with anchorage devices allowed for complex orthodontic tooth movements that was completed in shortened period without adverse dental and periodontal consequences.
Financial support and sponsorship
Nil.
Conflicts of interest
First author (HHZ) declares patents on instruments used for VISTA, as well as commercial interest in Regenimmune, Inc. which is involved in distribution of VISTA instruments.
References
- 1.Weltman B, Vig KW, Fields HW, Shanker S, Kaizar EE. Root resorption associated with orthodontic tooth movement: A systematic review. Am J Orthod Dentofacial Orthop. 2010;137:462–76. doi: 10.1016/j.ajodo.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 2.Benson PE, Parkin N, Dyer F, Millett DT, Furness S, Germain P, et al. Fluorides for the prevention of early tooth decay (demineralised white lesions) during fixed brace treatment. Cochrane Database Syst Rev. 2013;12:CD003809. doi: 10.1002/14651858.CD003809.pub3. [DOI] [PubMed] [Google Scholar]
- 3.Kasai K, Chou MY, Yamaguchi M. Molecular effects of low-energy laser irradiation during orthodontic tooth movement. Semin Orthod. 2015;21:203–9. [Google Scholar]
- 4.Alansari S, Sangsuwon C, Vongthongleur T, Kwal R, Teo MC, Lee YB, et al. Biological principles behind accelerated tooth movement. Semin Orthod. 2015;21:151–61. [Google Scholar]
- 5.Sebaoun JD, Kantarci A, Turner JW, Carvalho RS, Van Dyke TE, Ferguson DJ, et al. Modeling of trabecular bone and lamina dura following selective alveolar decortication in rats. J Periodontol. 2008;79:1679–88. doi: 10.1902/jop.2008.080024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baloul SS, Gerstenfeld LC, Morgan EF, Carvalho RS, Van Dyke TE, Kantarci A, et al. Mechanism of action and morphologic changes in the alveolar bone in response to selective alveolar decortication-facilitated tooth movement. Am J Orthod Dentofacial Orthop. 2011;139:S83–101. doi: 10.1016/j.ajodo.2010.09.026. [DOI] [PubMed] [Google Scholar]
- 7.Dibart S, Yee C, Surmenian J, Sebaoun JD, Baloul S, Goguet-Surmenian E, et al. Tissue response during piezocision-assisted tooth movement: A histological study in rats. Eur J Orthod. 2014;36:457–64. doi: 10.1093/ejo/cjt079. [DOI] [PubMed] [Google Scholar]
- 8.Frost HM. The regional acceleratory phenomenon: A review. Henry Ford Hosp Med J. 1983;31:3–9. [PubMed] [Google Scholar]
- 9.Frost HM. The biology of fracture healing An overview for clinicians Part I. Clin Orthop Relat Res. 1989;248:283–93. [PubMed] [Google Scholar]
- 10.Frost HM. The biology of fracture healing An overview for clinicians Part II. Clin Orthop Relat Res. 1989;248:294–309. [PubMed] [Google Scholar]
- 11.Wang L, Lee W, Lei DL, Liu YP, Yamashita DD, Yen SL, et al. Tisssue responses in corticotomy- and osteotomy-assisted tooth movements in rats: Histology and immunostaining. Am J Orthod Dentofacial Orthop. 2009;136:770e1–11. doi: 10.1016/j.ajodo.2009.05.015. [DOI] [PubMed] [Google Scholar]
- 12.Dibart S, Keser E, Nelson D. Piezocision™-assisted orthodontics: Past, present, and future. Semin Orthod. 2015;21:170–5. [Google Scholar]
- 13.Wilcko WM, Wilcko T, Bouquot JE, Ferguson DJ. Rapid orthodontics with alveolar reshaping: Two case reports of decrowding. Int J Periodontics Restorative Dent. 2001;21:9–19. [PubMed] [Google Scholar]
- 14.Murphy KG, Wilcko MT, Wilcko WM, Ferguson DJ. Periodontal accelerated osteogenic orthodontics: A description of the surgical technique. J Oral Maxillofac Surg. 2009;67:2160–6. doi: 10.1016/j.joms.2009.04.124. [DOI] [PubMed] [Google Scholar]
- 15.Zadeh HH. Minimally invasive treatment of maxillary anterior gingival recession defects by vestibular incision subperiosteal tunnel access and platelet-derived growth factor BB. Int J Periodontics Restorative Dent. 2011;31:653–60. [PubMed] [Google Scholar]
- 16.Kanomi R. Mini-implant for orthodontic anchorage. J Clin Orthod. 1997;31:763–7. [PubMed] [Google Scholar]
- 17.Chung KR, Kim YS, Linton JL, Lee YJ. The miniplate with tube for skeletal anchorage. J Clin Orthod. 2002;36:407–12. [PubMed] [Google Scholar]
- 18.Chung KR, Kim SH, Mo SS, Kook YA, Kang SG. Severe class II division 1 malocclusion treated by orthodontic miniplate with tube. Prog Orthod. 2005;6:172–86. [PubMed] [Google Scholar]
- 19.Kim SH, Lee KB, Chung KR, Nelson G, Kim TW. Severe bimaxillary protrusion with adult periodontitis treated by corticotomy and compression osteogenesis. Korean J Orthod. 2009;39:54–65. [Google Scholar]
- 20.Chung KR, Kim SH, Kang YG, Nelson G. Orthodontic miniplate with tube as an efficient tool for borderline cases. Am J Orthod Dentofacial Orthop. 2011;139:551–62. doi: 10.1016/j.ajodo.2008.08.041. [DOI] [PubMed] [Google Scholar]
- 21.Ferguson DJ, Wilcko MT, Wilcko WM, Makki L. Scope of treatment with periodontally accelerated osteogenic orthodontics therapy. Semin Orthod. 2015;21:176–86. [Google Scholar]
- 22.Buschang PH, Campbell PM, Ruso S. Accelerating tooth movement with corticotomies: Is it possible and desirable? Semin Orthod. 2012;18:286–94. [Google Scholar]
- 23.Long H, Pyakurel U, Wang Y, Liao L, Zhou Y, Lai W, et al. Interventions for accelerating orthodontic tooth movement: A systematic review. Angle Orthod. 2013;83:164–71. doi: 10.2319/031512-224.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hoogeveen EJ, Jansma J, Ren Y. Surgically facilitated orthodontic treatment: A systematic review. Am J Orthod Dentofacial Orthop. 2014;145:S51–64. doi: 10.1016/j.ajodo.2013.11.019. [DOI] [PubMed] [Google Scholar]
- 25.Wilcko MT, Wilcko WM, Bissada NF. An evidence-based analysis of periodontally accelerated orthodontic and osteogenic techniques: A synthesis of scientific perspective. Semin Orthod. 2008;14:305–16. [Google Scholar]
- 26.Akay MC, Aras A, Günbay T, Akyalçin S, Koyuncue BO. Enhanced effect of combined treatment with corticotomy and skeletal anchorage in open bite correction. J Oral Maxillofac Surg. 2009;67:563–9. doi: 10.1016/j.joms.2008.06.091. [DOI] [PubMed] [Google Scholar]
- 27.Ahn HW, Seo DH, Kim SH, Lee BS, Chung KR, Nelson G, et al. Correction of facial asymmetry and maxillary canting with corticotomy and 1-jaw orthognathic surgery. Am J Orthod Dentofacial Orthop. 2014;146:795–805. doi: 10.1016/j.ajodo.2014.08.018. [DOI] [PubMed] [Google Scholar]
- 28.Kim SH, Kim I, Jeong DM, Chung KR, Zadeh H. Corticotomy-assisted decompensation for augmentation of the mandibular anterior ridge. Am J Orthod Dentofacial Orthop. 2011;140:720–31. doi: 10.1016/j.ajodo.2009.12.040. [DOI] [PubMed] [Google Scholar]
- 29.Charavet C, Lecloux G, Bruwier A, Rompen E, Maes N, Limme M, et al. Localized piezoelectric alveolar decortication for orthodontic treatment in adults: A randomized controlled trial. J Dent Res. 2016;95:1003–9. doi: 10.1177/0022034516645066. [DOI] [PubMed] [Google Scholar]
- 30.Alghamdi AS. Corticotomy facilitated orthodontics: Review of a technique. Saudi Dent J. 2010;22:1–5. doi: 10.1016/j.sdentj.2009.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mathews DP, Kokich VG. Accelerating tooth movement: The case against corticotomy-induced orthodontics. Am J Orthod Dentofacial Orthop. 2013;144:5–13. doi: 10.1016/j.ajodo.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 32.Dibart S, Sebaoun JD, Surmenian J. Piezocision: A minimally invasive, periodontally accelerated orthodontic tooth movement procedure. Compend Contin Educ Dent. 2009;30:342. [PubMed] [Google Scholar]
- 33.Gil APS, Haas OL, Jr, Méndez-Manjón I. Alveolar corticotomies for accelerated orthodontics: A systematic review. J Craniomaxillofac Surg. 2018;46:438–45. doi: 10.1016/j.jcms.2017.12.030. [DOI] [PubMed] [Google Scholar]
- 34.Kim SJ, Park YG, Kang SG. Effects of corticision on paradental remodeling in orthodontic tooth movement. Angle Orthod. 2009;79:284–91. doi: 10.2319/020308-60.1. [DOI] [PubMed] [Google Scholar]
- 35.Kim YS, Kim SJ, Yoon HJ. Effect of piezopuncture on tooth movement and bone remodeling in dogs. Am J Orthod Dentofacial Orthop. 2013;144:23–31. doi: 10.1016/j.ajodo.2013.01.022. [DOI] [PubMed] [Google Scholar]
- 36.Alikhani M, Raptis M, Zoldan B. Effect of micro-osteoperforations on the rate of tooth movement. Am J Orthod Dentofacial Orthop. 2013;144:639–48. doi: 10.1016/j.ajodo.2013.06.017. [DOI] [PubMed] [Google Scholar]
- 37.Garg S, Arora SA, Chhina S, Singh P. Multiple Gingival Recession Coverage Treated with Vestibular Incision Subperiosteal Tunnel Access Approach with or without PlateletRich Fibrin - A Case Series. Contemp Clin Dent. 2017;8:464–68. doi: 10.4103/ccd.ccd_142_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bariani RC, Milani R, Guimaraes Junior CH. Orthodontic Traction of Impacted Upper Canines Using the VISTA Technique. J Clin Orthod. 2017;51:76–85. [PubMed] [Google Scholar]
- 39.Gil A, Bakhshalian N, Min S, Zadeh HH. Treatment of multiple recession defects with vestibular incision subperiosteal tunnel access (VISTA): A retrospective pilot study utilizing digital analysis. J Esthet Restor Dent. 2018;30:572–79. doi: 10.1111/jerd.12434. [DOI] [PubMed] [Google Scholar]
- 40.Najafi B, Kheirieh P, Torabi A, Cappetta EG. Periodontal Regenerative Treatment of Intrabony Defects in the Esthetic Zone Using Modified Vestibular Incision Subperiosteal Tunnel Access (M-VISTA) Int J Periodontics Restorative Dent. 2018;38(Suppl):e9–e16. doi: 10.11607/prd.3138. [DOI] [PubMed] [Google Scholar]
- 41.S RR, Kumar TA, Gowda TM. Management of Multiple Gingival Recessions with the VISTA Technique: An 18-Month Clinical Case Series. Int J Periodontics Restorative Dent. 2018;38:245–51. doi: 10.11607/prd.2990. [DOI] [PubMed] [Google Scholar]
- 42.Fan KA, Zhong JS, Ouyang XY. Vestibular incision subperiosteal tunnel access with connective tissue graft for the treatment of Miller class I and II gingival recession. Beijing Da Xue Xue Bao Yi Xue Ban. 2019;51:80–85. doi: 10.19723/j.issn.1671-167X.2019.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Borzabadi-Farahani A, Zadeh HH. Adjunctive orthodontic applications in dental implantology. J Oral Implantol. 2015;41:501–8. doi: 10.1563/AAID-JOI-D-13-00235. [DOI] [PubMed] [Google Scholar]
- 44.Borzabadi-Farahani A, Zadeh HH. In: Orthodontic therapy in implant dentistry: Orthodontic implant site development In, Vertical alveolar ridge augmentation in implant dentistry: A surgical manual. Tolstunov L, editor. Hoboken: John Wiley & Sons; 2016. pp. 30–37. [Google Scholar]


