Abstract
Patients with hypertension who develop atrial premature complexes (APCs) are at a particularly high risk for atrial fibrillation (AF). We sought to identify medications and modifiable risk factors that could reduce the risk of AF imposed by presence of APCs in such a high risk group. This analysis included 4,331 participants with treated hypertension from the REGARDS study who were free of AF and cardiovascular disease at the time of enrollment (2003–2007). APCs were detected in 8.2% (n=356) of the participants at baseline. During a median follow-up of 9.4 years, 9.9% (n=429) of the participants developed AF. Participants with APCs, compared to those without, were more than twice as likely to develop AF (Odds ratio (95% confidence interval): 2.36(1.75, 3.19)). This association was significantly weaker in statin users than non-users (Odds ratio (95% confidence interval):1.42(0.81,2.48) vs. 3.01(2.11,4.32), respectively; interaction p-value= 0.02), and in angiotensin-II receptor blocker users than non-users (Odds ratio (95% confidence interval):1.31(0.66,2.61) vs. 2.78(1.99,3.89), respectively; interaction p-value= 0.05). Borderline weaker associations between APCs and AF were also observed in alpha-blocker users than non-users, non-diabetics than diabetics, and in those with systolic blood pressure level 130–139 mmHg compared to those with other systolic blood pressure levels. No significant effect modifications were observed by use of other medications or by presence of other cardiovascular risk factors. In conclusion, the significant AF risk associated with APCs in patients with hypertension could potentially be reduced by treatment with angiotensin-II receptor blockers and statins along with lowering blood pressure and management of diabetes.
Keywords: Premature Atrial Complexes, Atrial fibrillation, Hypertension, Effect Modification
Atrial premature complexes (APCs) play a critical role in the pathogenesis of atrial fibrillation (AF) by acting as a trigger for AF in the presence of the appropriate substrate (1). In a previous report from the Reasons for Geographic and Racial Differences in Stroke (REGARDS), presence of APCs on routine resting electrocardiogram was associated with a 92% increased risk of AF (2). Also, high blood pressure is an established risk factor for AF, explaining more than one-fifth of AF cases (3). Hence, patients with hypertension who develop APCs are exposed to two major AF risk factors; high blood pressure and APCs. Identifying factors that could potentially modify the risk of AF associated with APCs in patients with hypertension will inform AF prevention in such a high-risk group. In particular, since there are multiple therapeutic options for treatment of hypertension, some of which may also affect APCs, it would be helpful to know if certain therapies or combinations are associated with a higher or lower incidence of AF. In this analysis from the REGARDS study, we examined the effect modification of several classes of blood pressure lowering medications as well as modifiable cardiovascular risk factors on the association between baseline APCs and incident AF among REGARDS participants who had hypertension requiring medical treatment.
Methods
The REGARDS study is a longitudinal cohort study aimed to investigate the regional and racial disparities in stroke mortality (4). Between January 2003 to October 2007, 30,239 participants were recruited from the continental United States, oversampling blacks and residents of the Southeastern stroke belt region (North Carolina, South Carolina, Georgia, Alabama, Mississippi, Tennessee, Arkansas, and Louisiana]. Demographic information and medical history data were collected via a computer-assisted telephone interview followed by an in-home physical examination which included blood pressure measurement, electrocardiogram recording, and blood draw. Verbal consent was obtained initially on the telephone then written informed consent was obtained during the in-home physical exam.
After 9.4 years (median) of the first in-home visit, 15,521 participants completed a similar second in-home follow-up examination. Out of the REGARDS participants who completed both in-home visits, we applied the following exclusions to the baseline data: no hypertension, hypertension not requiring medical treatment, missing blood pressure measurements data, missing blood pressure medications data, prevalent baseline AF, prevalent cardiovascular disease (coronary heart disease, heart failure and stroke), missing baseline APCs. We also excluded those with missing incident AF data. Figure 1 outlines the inclusions and exclusions criteria we applied to reach our REGARDS subsample we used in this analysis.
Figure 1.
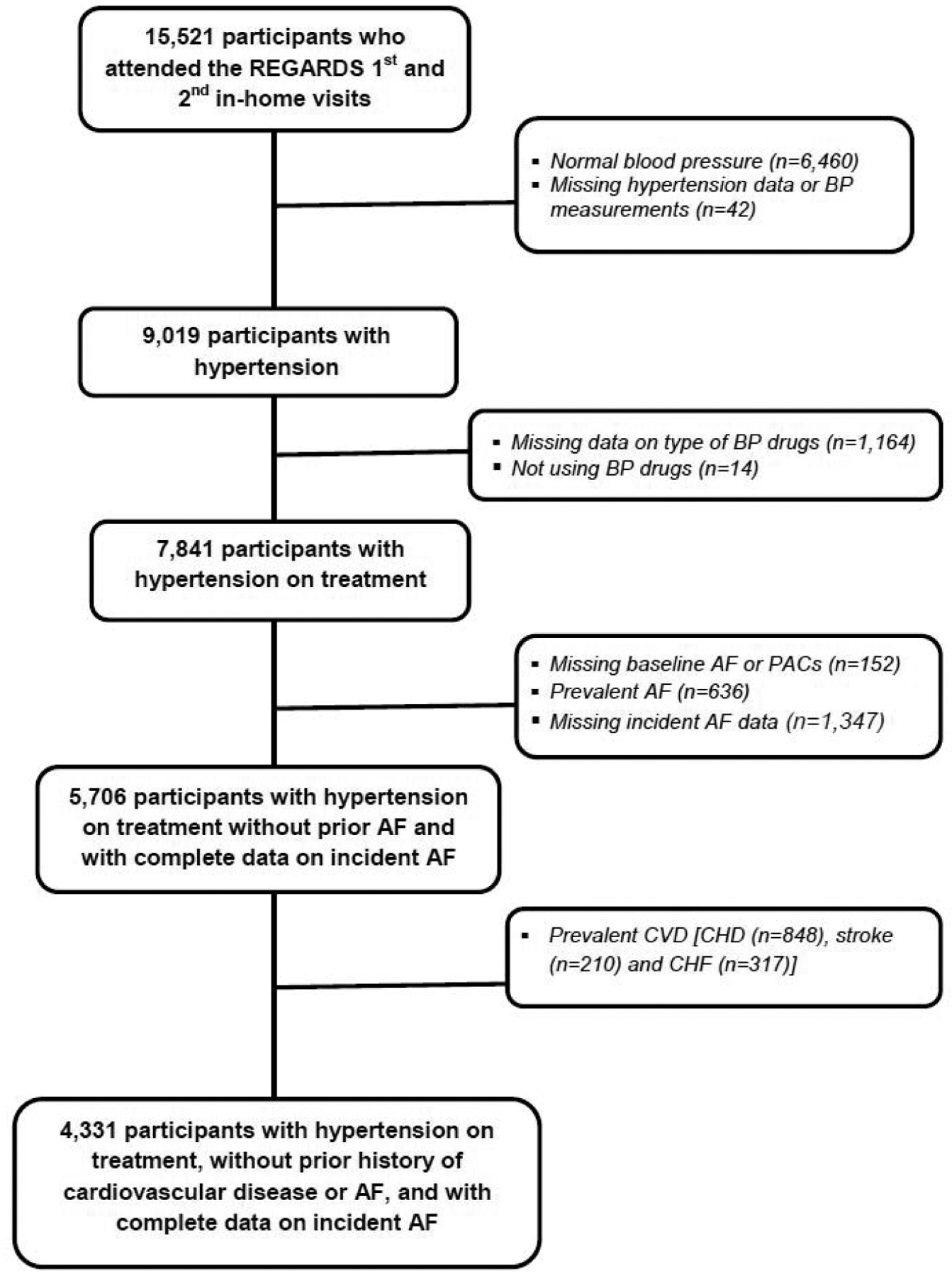
Flow Diagram Outlining the Inclusion and Exclusion Criteria
Blood pressure was obtained with an aneroid sphygmomanometer using appropriate cuff size after the participant had been seated for 5 minutes with both feet on the floor. Using the mean of two blood pressure measurements, hypertension was defined as systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, or self-reported use of blood pressure lowering medications.
During the baseline in-home visit, the names of all prescription medications including blood pressure lowering medications were recorded from the pharmacy label. The following classes of blood pressure lowering medications were later determined from the medications inventory: angiotensin-converting enzyme inhibitors, aldosterone antagonists, alpha-blockers, angiotensin-II receptor blockers, beta-blockers, calcium channel blockers, central agonists, diuretics, or direct vasodilators. Participants who reported not taking or had no blood pressure lowering medications in the inventory were defined as not taking blood pressure lowering medications.
Standard resting electrocardiograms were recorded during the baseline and the 2nd in-home visits and were sent to the Epidemiological Cardiology Research Center at Wake Forest School of Medicine (Winston- Salem, North Carolina) for processing and reading. Incident AF was ascertained during the 2nd in-home visit using two methods: 1) from the study electrocardiograms; and 2) self-reported history of a previous physician diagnosis of AF (5).
All covariates were collected from the first in-home visit (baseline). Data on age, sex, race, income, smoking status, alcohol drinking, and physical activity were self-reported. Use of regular aspirin was based on self-report, while statins and anti-hypertensive medications were based on pill-bottle review. Body mass index was calculated from height and weight. Electrocardiographic left ventricular hypertrophy was defined by Sokolow-Lyon criteria. Diabetes mellitus was defined as fasting glucose ≥126 mg/dL, non-fasting glucose ≥200 mg/dL, or taking medications to control blood sugar. Dyslipidemia was defined as total cholesterol ≥240 mg/dl, low-density lipoprotein cholesterol ≥160 mg/dl, high-density lipoprotein cholesterol ≤40 mg/dl or the participant was on cholesterol-lowering medication. Chronic kidney disease was defined as an estimated glomerular filtration rate <60 ml/min per 1.73 m2.
Baseline characteristics of the participants were tabulated and compared between those with and without APCs using Student’s t test for continuous variables and Chi square for categorical variables. We conducted two main sets of analyses:
First, we examined the association between baseline APCs and incident AF. The purpose of this step in the analysis was to ensure that the previously reported relationship between APCs and AF is generalizable to our unique study population composed entirely of participants with treated hypertension. We used logistic regression models to examine the association between APCs at baseline (first in-home visit) with incident AF during follow-up (second in-home visit). The following models were constructed with incremental adjustments: Model 1 (Socio-demographics): age, sex, race, region of residence, and income; Model 2 (Behavioral factors): Model 1 plus smoking, alcohol drinking, physical activity; Model 3 (cardiovascular risk factors): Model 2 plus dyslipidemia, diabetes, obesity, chronic kidney disease; Model 4 (Markers of hypertension severity) Model 3 plus systolic blood pressure, number of blood pressure medications, and left ventricular hypertrophy; Model 5 (Medications): Model 4 plus statin use and regular use of aspirin; Model 6 (Inflammatory markers): Model 5 plus high sensitivity C-reactive protein. A 2-sided value of p<0.05 was considered significant.
Second, we examined the effect modification of the association between APCs and AF. The goal was to identify subgroups of participants who would get more benefit (or harm) by their exposure to different medications or by having different characteristics (6). Effect modification was tested using the following subgroups: use of angiotensin-converting enzyme inhibitors, use of alpha blockers, use of angiotensin-II receptor blockers, use of beta-blockers, use of calcium channel blockers, use of diuretics, use of statins, use of aspirin, age (≤65 years and >65 years), sex, race (black and white), smoking status (current, past, and never), alcohol drinking (current, past, and never), physical activity (0, 1–3, and ≥ 4 times/week), dyslipidemia, chronic kidney disease, left ventricular hypertrophy, number of blood pressure lowering medications (1, 2 and ≥3 medications), systolic blood pressure levels (<120 mmHg, 120–129 mmHg, 130–139 mmHg, and >140 mmHg), obesity (obese, overweight, and normal), diabetes, and high sensitivity C-reactive protein (≤3.0 mg/L and >3.0 mg/L). Due to the small number of participants receiving direct vasodilators, we did not test effect modification by the use of direct vasodilators. In each subgroup, logistic regression analysis was used to calculate the AF odds ratio and 95% confidence interval associated with the presence (vs. absence) of baseline APCs. Unless the variable is the stratifying variable, models were adjusted for age, sex, race, region of residence, income, smoking, alcohol drinking, physical activity, dyslipidemia, diabetes, obesity, chronic kidney disease, systolic blood pressure, number of blood pressure medications, left ventricular hypertrophy, statins use, use of regular aspirin, and high sensitivity C-reactive protein. Potential interaction was examined by including a product term of each variable with the APCs and comparing the models with and without the product terms using the likelihood ratio test. Significant effect modification was considered present if interaction p-value is <0.05. Because using a more relaxed p-value for interaction is an increasingly acceptable approach (7), and since prior REGARDS publications used p-value of 0.10 to indicate significant interaction (8), we also used interaction p-value <.15 to indicate a “borderline significant” interaction. All analyses were conducted using SAS 9.4 [SAS Institute, Cary, NC].
Results
This analysis included 4,331 participants with treated hypertension (mean age 64.6 years, 59.5% women, 45.8% blacks) who were free of cardiovascular disease and AF at baseline. APCs were detected in 8.2% (n=356) of the study participants at baseline. Participants with APCs were more likely to be older, men, have a history of chronic kidney disease, and have higher levels of systolic blood pressure. Baseline characteristics of the study participants, overall and stratified by presence of APCs, are detailed in Table 1.
Table 1.
Baseline Characteristics
| Characteristics | All Participants | Atrial Premature Complexes (APCs) | ||
|---|---|---|---|---|
| mean ±SD or n (%) | (n=4,331) | Absent (n=3975) | Present (n=356) | p-value |
| Age (years) | 64.6 ± 8.1 | 64.3 ± 8.0 | 67.7 ± 8.4 | <0.001 |
| Women | 2576 (59.5%) | 2391 (60.2%) | 185(52.0%) | 0.003 |
| Income ($) | 0.35 | |||
| < 20,000 | 609 (14.1%) | 547 (13.8%) | 62 (17.4%) | |
| 20,000–34,000 | 1018 (23.5%) | 934 (23.5%) | 118 (33.2%) | |
| 35,000–74,000 | 1464 (33.8%) | 1346 (33.9%) | 56 (15.7%) | |
| $75,000 and above | 784 (18.1%) | 728 (18.3%) | 36 (10.1%) | |
| Refused | 456 (10.5%) | 420 (10.6%) | 52 (11.1%) | |
| Black | 1983 (45.8%) | 1830 (46.0%) | 153 (43.0%) | 0.27 |
| Smoking | 0.29 | |||
| Current | 411 (9.5%) | 376 (9.5%) | 35 (9.9%) | |
| Past | 1732 (40.1%) | 1577 (39.8%) | 155 (43.7%) | |
| Alcohol drinking | 0.41 | |||
| Current | 2326 (53.7%) | 2143 (53.9%) | 183 (51.4%) | |
| Past | 665 (15.4%) | 602 (15.1%) | 63 (17.7%) | |
| Exercise (times/week) | 0.36 | |||
| 1 to 3 | 1668 (38.9%) | 1532 (38.9%) | 136 (38.4%) | |
| >4 | 1251 (29.2%) | 1137 (28.9%) | 114 (32.2%) | |
| Dyslipidemia | 2515 (59.8%) | 2318 (59.9%) | 197 (57.6%) | 0.40 |
| Diabetes mellitus | 949 (22.5%) | 870 (22.5%) | 79 (22.8%) | 0.89 |
| High sensitivity C-reactive protein (mg/dL) | 4.4±6.9 | 4.4±6.9 | 4.6±6.5 | 0.64 |
| Body mass index (kg/m2) | 0.37 | |||
| >35 | 1991 (46.2%) | 1832 (46.3%) | 159 (44.8%) | |
| ≥25–30 | 1579 (36.6%) | 1456 (36.8%) | 123 (34.75%) | |
| <25 | 17 (0.4%) | 15 (0.4%) | 2 (0.6%) | |
| Chronic kidney disease | 430 (10.0%) | 379 (9.6%) | 51 (14.4%) | 0.004 |
| Left ventricular hypertrophy | 465 (10.8%) | 421 (10.6%) | 44 (12.4%) | 0.29 |
| Number of Blood Pressure drugs | 0.021 | |||
| 1 | 1991 (46.0%) | 1831 (46.1%) | 160 (44.9%) | |
| 2 | 1553 (35.9%) | 1426 (35.9%) | 127 (35.7%) | |
| 3 | 603 (13.9%) | 554 (13.9%) | 49 (13.8%) | |
| 4 | 156 (3.6%) | 141 (3.6%) | 15 (4.2%) | |
| 5 | 27 (0.6%) | 23 (0.6%) | 4 (1.1%) | |
| 6 | 1 (0.0%) | 0 (0.0%) | 1 (0.3%) | |
| Systolic blood pressure (mmHg) | 128.7 ± 15.3 | 128.5 ± 15.1 | 130.6 ± 17.6 | 0.015 |
| Angiotensin-converting enzyme inhibitors | 1512 (34.9%) | 1379 (34.7%) | 133 (37.4%) | 0.31 |
| Aldosterone receptor antagonists | 56 (1.3%) | 50 (1.3%) | 6 (1.7%) | 0.49 |
| Alpha blockers | 271 (6.4%) | 237 (6.0%) | 34 (9.6%) | 0.007 |
| Angiotensin II receptor blockers | 1053 (24.3%) | 960 (24.2%) | 93 (26.1%) | 0.41 |
| Beta-blockers | 1257 (29–0%) | 1166 (29.3%) | 91 (25. 6%) | 0.13 |
| Calcium channel blockers | 1307 (30.2%) | 1193 (30.0%) | 114 (32.0%) | 0.43 |
| Central agonists | 12 (0.3%) | 11 (0.3%) | 2 (0.4%) | 0.99 |
| Diuretics | 2185 (50.5%) | 2014 (50.7%) | 171 (48.0%) | 0.34 |
| Direct vasodilators | 18 (0.4%) | 14 (0.4%) | 4 (1.1%) | 0.030 |
| Aspirin | 1999 (46.2%) | 1833 (46.1%) | 166 (46.6%) | 0.85 |
| Statin | 1516 (35.0%) | 1409 (35.5%) | 107 (30.1%) | 0.041 |
Left ventricular hypertrophy was defined by Sokolow-Lyon criteria from ECG.
Diabetes mellitus was defined as fasting glucose ≥126 mg/dL, non-fasting glucose ≥200 mg/dL, or use of medications to control blood sugar.
Dyslipidemia was defined as total cholesterol >240 mg/dl, low-density lipoprotein >160 mg/dl, high-density lipoprotein <40 mg/dl or the participant was on cholesterol-lowering medication.
Chronic kidney disease was defined as an estimated glomerular filtration rate <60 ml/min per 1.73 m2.
During a median follow-up of 9.4 years, 429 (9.9%) of the participants developed AF. More participants with baseline APCs developed AF during follow-up compared to those without baseline APCs (p-value <0.001). In a multivariable logistic regression model adjusted for socio-demographics, behavioral risk factors, cardiovascular risk factors, markers of hypertension severity, medications and inflammatory markers, presence (vs. absence) of baseline APCs was associated with more than double the odds of incident AF (p-value <0.001) (Table 2).
Table 2:
Association between Baseline Atrial Premature Complexes and Incident Atrial Fibrillation
| Model 1: | Model 2: | Model 3: | Model 4: | Model 5: | Model 6: | ||
|---|---|---|---|---|---|---|---|
| Baselin eAPCs | Participants (n) / AF (n %)) | Socio-demographics | Model 1 + Behaviora 1 factors | Model 2+ cardiovascular risk factors | Model 3+ Markers of hypertension severity | Model 4 + Medications | Model 5+ Inflammatory markers |
| Odds Ratio (95% Confidence Interval) | |||||||
| Absent | 3975/351(8.8 %) | Reference | Reference | Reference | Reference | Reference | Reference |
| Present | 356/78 (21.9%) | 2.43(1.83, 3.24) | 2.45 (1.84, 3.27) | 2.35(1.75, 3.15) | 2.37(1.76, 3.18) | 2.37(1.76, 3.18) | 2.36 (1.75, 3.19) |
APCs= atrial premature complexes; AF= atrial fibrillation
Socio-demographics: Age, sex, race, region of residence, income
Behavioral factors: Smoking, alcohol drinking, physical activity
Cardiovascular risk factors: Dyslipidemia, diabetes mellitus, obesity, chronic kidney disease
Markers of hypertension severity: Systolic blood pressure, number of blood pressure medications, left ventricular hypertrophy
Medications: Statins use and regular aspirin
Inflammatory markers: High sensitivity C-reactive protein
We observed a significant effect modification for the association between presence of APCs and AF by angiotensin-II receptor blockers use and statin use, i.e., the risk of AF associated with APCs was significantly weaker in the ARB users than non-users (interaction p-value =0.05), and in statin users than non-users (interaction p-value= 0.02). When the study participants were stratified by concomitant use of angiotensin-II receptor blockers and statins, the risk of AF associated with APCs showed a dose-response relationship i.e., the risk of AF associated with APCs was weakest in those using both statins and angiotensin-II receptor blockers, strongest in those not using either medications, and somewhere in the middle in those using only one of the medications (interaction p-value 0.043). Borderline significant effect modification was also observed by alpha-blocker use (i.e., borderline significant weaker risk of AF in alpha-blocker users than non-users; interaction p-value= 0.12). On the other hand, no significant effect modifications were observed by other medications (angiotensin-converting enzyme inhibitors, beta-blockers, calcium channel blockers, diuretics, and aspirin) (Figure 2)
Figure 2: Effect Modification of the Association between APCs and AF by Cardiovascular Medications.
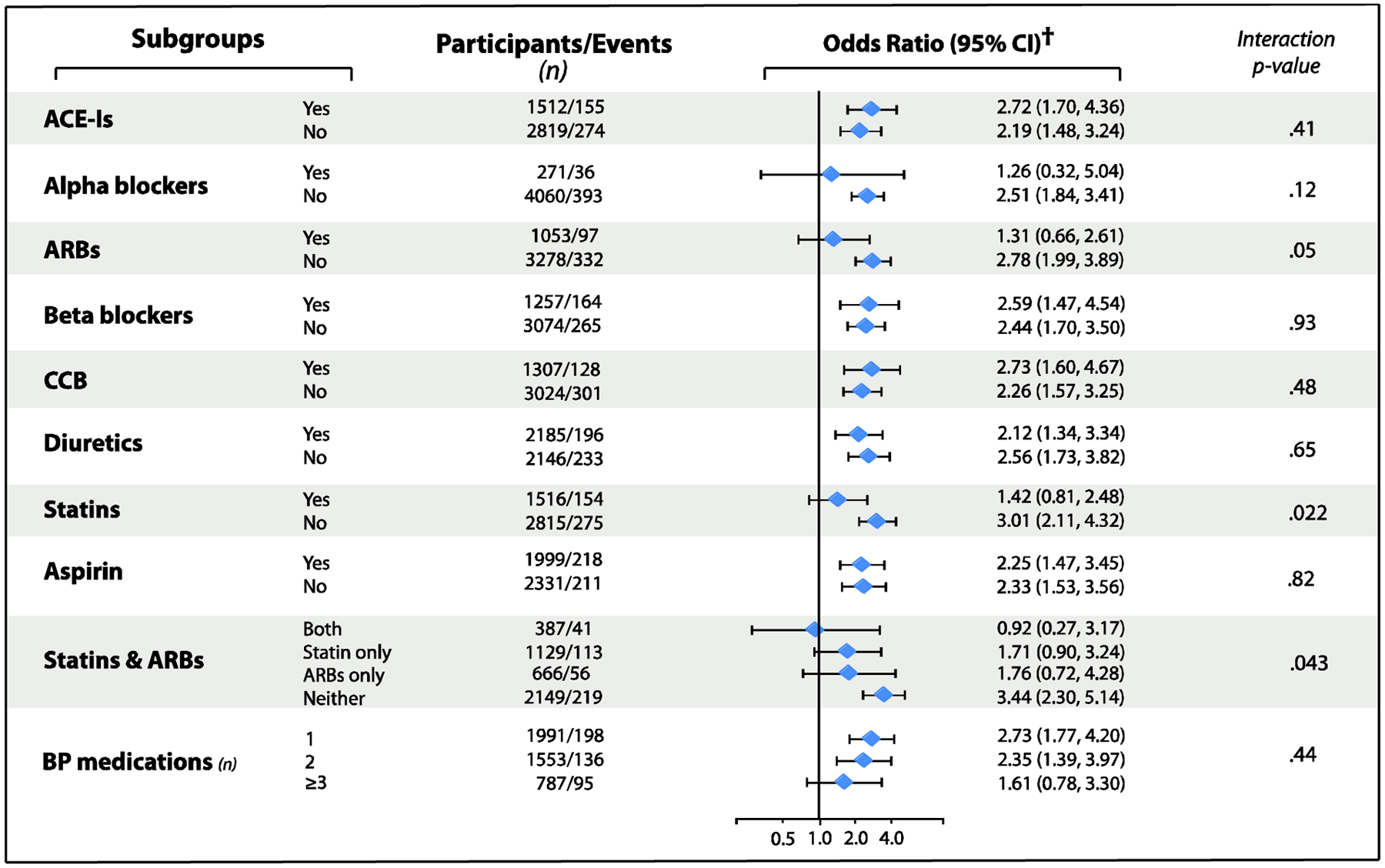
APCs= premature atrial complexes; AF= atrial fibrillation; CCBs= Calcium channel blockers; ARBs= angiotensin II receptor blockers; ACE-Is= Angiotensin-converting enzyme inhibitors; BP= blood pressure
†Model adjusted for age, sex, race, region of residence, income, smoking, alcohol drinking, physical activity, dyslipidemia, diabetes, obesity, chronic kidney disease, SBP, number of blood pressure medications, left ventricular hypertrophy, statin use, regular aspirin use, and high sensitivity C-reactive protein, unless the variable is the stratifying variable.
Borderline significant effect modifications were observed by diabetes (i.e., borderline significant higher risk of AF in those with than without diabetes; interaction p-value=0.13), and systolic blood pressure levels (i.e., borderline significant weaker risk of AF in those with systolic blood pressure 130–139 mmHg compared to those with other systolic blood pressure levels; interaction p-value 0.14). On the other hand, no significant effect modifications were observed by cardiovascular risk factors, or other participant characteristics (Figure 3).
Figure 3: Effect Modification of the Association between APCs and AF by Cardiovascular Risk Factors.
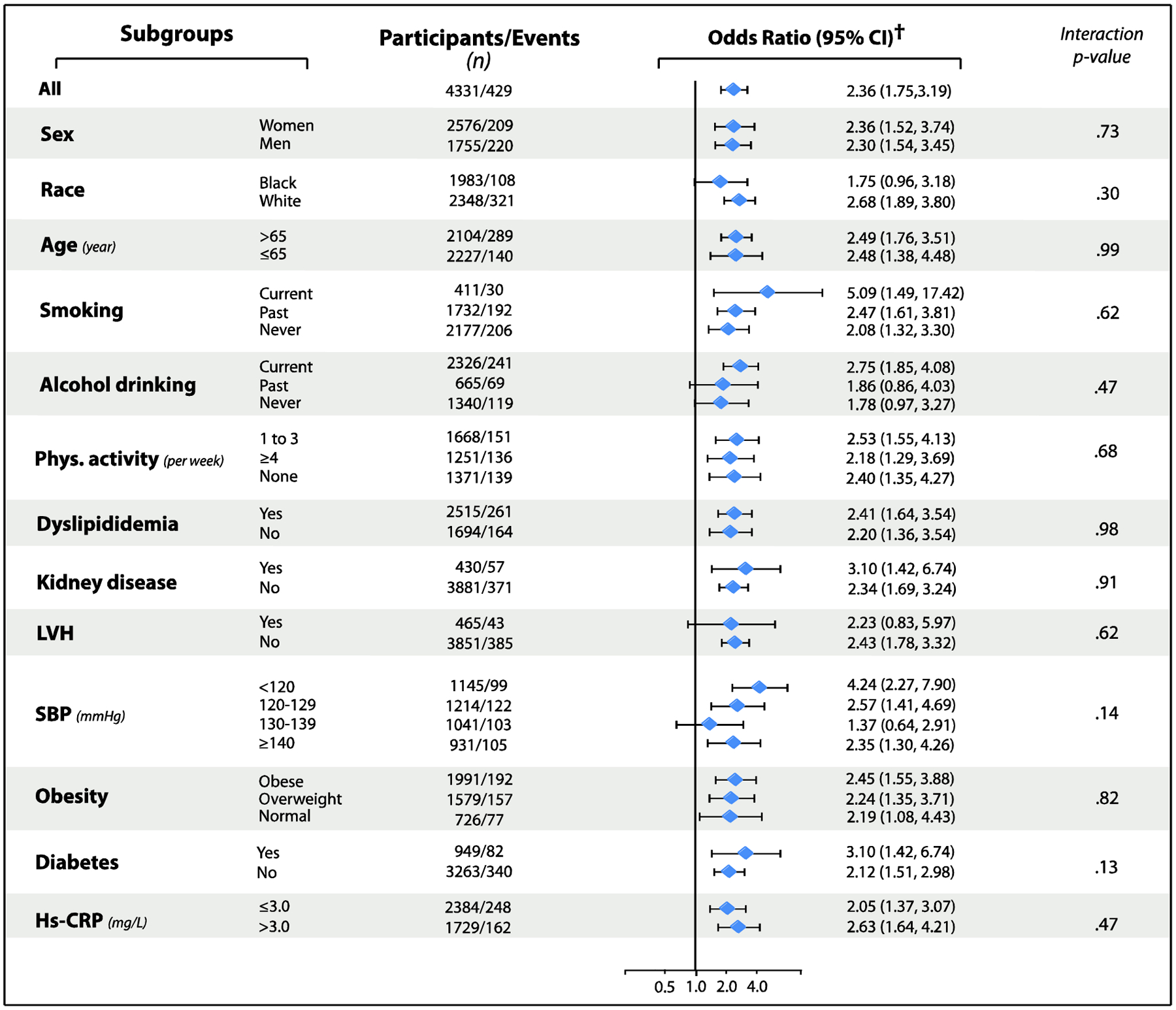
APCs= premature atrial complexes; AF= atrial fibrillation; Hs-CRP= High sensitivity C-reactive protein; LVH= Left ventricular hypertrophy; SBP= Systolic blood pressure
†Model adjusted for age, sex, race, region of residence, income, smoking, alcohol drinking, physical activity, dyslipidemia, diabetes, obesity, chronic kidney disease, systolic blood pressure, number of blood pressure medications, left ventricular hypertrophy, statin use, regular aspirin use, and hs-CPR, unless the variable is the stratifying variable.
Discussion
About 46% of the United States adults are estimated to have high blood pressure, and up to 6.1 million suffer from AF (9). In our study, which was limited to a subset of REGARDS participants with hypertension, presence of APCs was associated with 1.36 higher odds of AF. This compares to only 0.92 higher odds of AF associated with presence of APCs reported among all REGARDS participants (2), which underscore the additive AF risk imposed by APCs on patients with hypertension.
The strong and entangled triangular associations between high blood pressure, AF and APCs highlight the clinical and public health importance of prevention of AF in those with hypertension who have APCs. Our analysis revealed two significant effect modifiers of the association between APCs and AF: use of angiotensin-II receptor blockers and use of statins. The antiarrhythmic effect of angiotensin-II receptor blockers may be attributed to the favorable impact of angiotensin-II receptor blockers on left atrial pressure stretch, improved left ventricular hemodynamics, and prevention of atrial fibrosis (10). Although angiotensin-converting enzyme inhibitors share these properties with angiotensin-II receptor blockers via controlling the renin-angiotensin system and reducing blood pressure, we did not observe significant effect modification by angiotensin-converting enzyme inhibitors similar to angiotensin-II receptor blockers. It is possible that differences in the mechanisms by which angiotensin-converting enzyme inhibitors and angiotensin-II receptor blockers control the renin-angiotensin system enable more favorable impact of angiotensin-II receptor blockers on AF risk. Unlike angiotensin-II receptor blockers, angiotensin-converting enzyme inhibitors increase bradykinin bioavailability by reducing its degradation in the process of reducing angiotensin II (11). Although bradykinin adds to the cardiovascular benefits of angiotensin-converting enzyme inhibitors by enhancing tissue plasminogen activator and inhibiting platelet aggregation (12, 13), it also increases oxidative stress and inflammation (14–16) which are involved in the AF pathogenesis (17). The balance between these contradictory actions of bradykinin, which probably vary across populations, may explain the conflicting reports on the effect of angiotensin-converting enzyme inhibitors in prevention of AF in hypertensive individuals (18–24). This is unlike the reports on the angiotensin-II receptor blockers which have been more consistent in showing benefit compared to other blood pressure lowering medications (21–25).
The antioxidant and anti-inflammatory effects of statins led to the hypothesis that this class of lipid-lowering medications could be promising in AF prevention. However, prior reports found evidence for the benefit only after cardiac surgery (26–28). In our study, we observed an additive effect modification in a dose-response fashion with concomitant use of statins and angiotensin-II receptor blockers. This is probably due to the combined antioxidant and anti-inflammatory effect from both medications.
Our analysis also revealed three borderline effect modifiers for the AF risk associated with APCs: Systolic blood pressure levels, diabetes and use of alpha-blockers. The borderline lower AF risk associated with APCs in the subgroup with systolic blood pressure 130–139 mmHg compared to other systolic blood pressure subgroups underscores the role of controlling systolic blood pressure to normal levels. A post-hoc analysis from the Losartan Intervention for Endpoint Reduction in Hypertension study showed that the greatest reduction in AF risk occurred in those who achieved optimal systolic blood pressure levels compared to those with systolic blood pressure ≥142 mmHg (25). The borderline significant higher risk of AF associated with APCs in diabetes may be related to the added AF risk from diabetes through other mechanisms such as atrial fibrosis which provides a substrate for APCs to initiate AF. Higher levels of glycosylated hemoglobin have been linked to AF risk (29), and diabetes has been shown to be a risk factor for AF (30). Finally, we also found a favorable borderline effect-modification by alpha-blockers. It is unclear whether this is a chance finding, a result of a unique action by alpha-blocker, or the possibility that alpha-blocker was prescribed to healthier participants at a lower risk for AF.
Management of hypertension coexisting with cardiovascular disease such as heart failure or coronary heart disease is typically dictated by the management of these coexisting conditions. On the other hand, there is no consensus approach to the reduction of AF risk associated with APCs in hypertension without cardiovascular disease. Our study provides insights into how to deal with this common clinical situation in two ways. First, our findings suggest that the relationship between APCs and AF is modifiable in principle, as evident by the heterogeneity among the subgroups. This opens the door for exploring the modifiable factors that could favorably impact the relationship between APCs and AF. Second, our study went further and provided details about a few potential effect modifiers. Pending further investigations in efficacy clinical trials, our results suggest that angiotensin-II receptor blockers and statins, along with control of blood pressure and management of diabetes may have a favorable modifying effect on the AF risk associated with APCs concomitantly occurring with hypertension.
Our study has limitations. Although we used two methods for AF ascertainment (study scheduled electrocardiograms and self-reported history of a previous physician diagnosis), it remains possible that some AF cases such as paroxysmal/intermittent AF were not detected. By design, REGARDS study enrolled only white and black participants and we excluded participants with baseline cardiovascular disease; hence, our results may not apply to certain groups. Although we accounted for the severity of hypertension by adjusting for the number of blood pressure medications, we did not account for the length of time of hypertension which leaves room for residual confounding. Also, we did not adjust for medication discontinuation or changes over time. Despite these limitations, this is the first report from a large population-based study addressing factors modifying the risk of AF associated with APCs in individuals suffering from hypertension.
ACKNOWLEDGMENT-
This research project is supported by cooperative agreement U01 NS041588 co-funded by the National Institute of Neurological Disorders and Stroke (NINDS) and the National Institute on Aging (NIA), National Institutes of Health, Department of Health and Human Service. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NINDS. Representatives of the NINDS were involved in the review of the manuscript but not directly involved in the collection, management, analysis or interpretation of the data. The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICT OF INTEREST: None.
References
- 1).Iwasaki YK, Nishida K, Kato T, Nattel S. Atrial fibrillation pathophysiology: implications for management. Circulation 2011;124:2264–2274 [DOI] [PubMed] [Google Scholar]
- 2).O’Neal WT, Kamel H, Judd SE, Safford MM, Vaccarino V, Howard VJ, Howard G, Soliman EZ. Usefulness of atrial premature complexes on routine electrocardiogram to determine the risk of atrial fibrillation (from the REGARDS Study). Am J Cardiol 2017;120:782–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3).Huxley RR, Lopez FL, Folsom AR, Agarwal SK, Loehr LR, Soliman EZ, Maclehose R, Konety S, Alonso A. Absolute and attributable risks of atrial fibrillation in relation to optimal and borderline risk factors: the Atherosclerosis Risk in Communities (ARIC) study. Circulation 2011;123:1501–1508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4).Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, Graham A, Moy CS, Howard G. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology 2005;25:135–143 [DOI] [PubMed] [Google Scholar]
- 5).Soliman EZ, Safford MM, Muntner P, Khodneva Y, Dawood FZ, Zakai NA, Thacker EL, Judd S, Howard VJ, Howard G, Herrington DM, Cushman M. Atrial fibrillation and the risk of myocardial infarction. JAMA Intern Med 2014;174:107–114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6).Corraini P, Olsen M, Pedersen L, Dekkers OM, Vandenbroucke JP. Effect modification, interaction and mediation: an overview of theoretical insights for clinical investigators. Clin Epidemiol 2017;9:331–338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7).Thiese MS, Ronna B, Ott U. P value interpretations and considerations. J Thorac Dis 2016;8:E928–E931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).Howard G, Lackland DT, Kleindorfer DO, Kissela BM, Moy CS, Judd SE, Safford MM, Cushman M, Glasser SP, Howard VJ. Racial differences in the impact of elevated systolic blood pressure on stroke risk. JAMA Intern Med 2013;173:46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9).American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation 2019;139:e56–e528. [DOI] [PubMed] [Google Scholar]
- 10).Patlolla V, sheikh-Ali AA, Al-Ahmad AM. The renin-angiotensin system: a therapeutic target in atrial fibrillation. Pace-Pacing Clin Electrophysiol 2006; 29:1006–1012 [DOI] [PubMed] [Google Scholar]
- 11).Gainer JV, Morrow JD, Loveland A, King DJ, Brown NJ: Effect of bradykinin-receptor blockade on the response to Angiotensin-converting-enzyme inhibitor in normotensive and hypertensive subjects. N Engl J Med 1998; 339: 1285–1292 [DOI] [PubMed] [Google Scholar]
- 12).Murphey LJ, Malave HA, Petro J, Biaggioni I, Byrne DW, Vaughan DE, Luther JM, Pretorius M, Brown NJ: Bradykinin and its metabolite bradykinin 1–5 inhibit thrombin-induced platelet aggregation in humans. J Pharmacol Exp Ther 2006; 318: 1287–1292. [DOI] [PubMed] [Google Scholar]
- 13).Pretorius M, Rosenbaum D, Vaughan DE, Brown NJ. Angiotensin-converting enzyme inhibition increases human vascular tissue-type plasminogen activator release through endogenous bradykinin. Circulation 2003; 107: 579–585 [DOI] [PubMed] [Google Scholar]
- 14).Brunius G, Domeij H, Gustavsson A, Yucel-Lindberg T. Bradykinin upregulates IL-8 production in human gingival fibroblasts stimulated by interleukin-1b and tumor necrosis factor a. Regul Pept 2005; 126: 183–188 [DOI] [PubMed] [Google Scholar]
- 15).Santos DR, Calixto JB, Souza GE. Effect of a kinin B2 receptor antagonist on LPS- and cytokine-induced neutrophil migration in rats. Br J Pharmacol 139: 271–278, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16).Pan ZK., Zuraw BL, Lung CC, Prossnitz ER, Browning DD, Ye RD. Bradykinin stimulates NF-kappaB activation and interleukin 1beta gene expression in cultured human fibroblasts. J Clin Invest 1996; 98, 2042–2049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17).Li J, Solus J, Chen Q, Rho YH, Milne G, Stein CM, Darbar D. Role of inflammation and oxidative stress in atrial fibrillation. Heart Rhythm 2010;7:438–444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18).Salehian O, Healey J, Stambler B, Alnemer K, Almerri K, Grover J, Bata I, Mann J, Matthew J, Pogue J, Yusuf S, Dagenais G, Lonn E; HOPE Investigators.. Impact of ramipril on the incidence of atrial fibrillation: Results of the Heart Outcomes Prevention Evaluation study. Am Heart J 2007;154:448–453 [DOI] [PubMed] [Google Scholar]
- 19).Hansson L, Lindholm LH, Niskanen L, Lanke J, Hedner T, Niklason A, Luomanmäki K, Dahlöf B, de Faire U, Mörlin C, Karlberg BE, Wester PO, Björck JE.. Effect of angiotensin-converting-enzyme inhibition compared with conventional therapy on cardiovascular disease morbidity and mortality in hypertension: the Captopril Prevention Project (CAPPP) randomised trial. Lancet. 1999;353:611–616 [DOI] [PubMed] [Google Scholar]
- 20).Dewland TA, Soliman EZ, Yamal JM, BR, Alonso A, Albert CM, Simpson LM, Haywood LJ, Marcus GM. Pharmacologic prevention of incident atrial fibrillation: Long-term results from the ALLHAT (Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial). Circ Arrhythm Electrophysiol 2017;10 pii: e005463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21).Hsieh YC, Hung CY, Li CH, Liao YC, Huang JL, Lin CH, Wu TJ. Angiotensin-receptor blocker, angiotensin-converting enzyme inhibitor, and risks of atrial fibrillation: A Nationwide Cohort Study. Medicine (Baltimore) 2016;95:e3721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22).Chaugai S, Meng WY, Ali Sepehry A. Effects of RAAS blockers on atrial fibrillation prophylaxis: An updated systematic review and meta-analysis of randomized controlled trials. J Cardiovasc Pharmacol Ther 2016;21:388–404 [DOI] [PubMed] [Google Scholar]
- 23).Marott SC, Nielsen SF, Benn M, Nordestgaard BG. Antihypertensive treatment and risk of atrial fibrillation: a nationwide study. Eur Heart J 2014; 35:1205–1214 [DOI] [PubMed] [Google Scholar]
- 24).Healey JS, Baranchuk A, Crystal E, Morillo CA, Garfinkle M, Yusuf S, Connolly SJ. Prevention of atrial fibrillation with angiotensin-converting enzyme inhibitors and angiotensin receptor blockers: a meta-analysis. J Am Coll Cardiol 2005; 45:1832–1839 [DOI] [PubMed] [Google Scholar]
- 25).Wachtell K, Lehto M, Gerdts E, Olsen MH, Hornestam B, Dahlöf B, Ibsen H, Julius S, Kjeldsen SE, Lindholm LH, Nieminen MS, Devereux RB. Angiotensin II receptor blockade reduces new-onset atrial fibrillation and subsequent stroke compared to atenolol: the Losartan Intervention For End Point Reduction in Hypertension (LIFE) study. J Am Coll Cardiol 2005; 45:712–719 [DOI] [PubMed] [Google Scholar]
- 26).Chen WT, Krishnan GM, Sood N, Kluger J, Coleman CI. Effect of statins on atrial fibrillation after cardiac surgery: a duration- and dose-response meta-analysis. J Thorac Cardiovasc Surg 2010;140:364–372 [DOI] [PubMed] [Google Scholar]
- 27).Macfarlane PW, Murray H, Sattar N, Stott DJ, Ford I, Buckley B, Jukema JW, Westendorp RG, Shepherd J. The incidence and risk factors for new onset atrial fibrillation in the PROSPER study. Europace 2011;13:634–639 [DOI] [PubMed] [Google Scholar]
- 28).Schwartz GG, Chaitman BR, Goldberger JJ, Messig M. High-dose atorvastatin and risk of atrial fibrillation in patients with prior stroke or transient ischemic attack: analysis of the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial. Am Heart J 2011;161:993–999 [DOI] [PubMed] [Google Scholar]
- 29).Qi W, Zhang N, Korantzopoulos P, Letsas KP, Cheng M, Di F, Tse G, Liu T, Li G. Serum glycated hemoglobin level as a predictor of atrial fibrillation: A systematic review with meta-analysis and meta-regression. PLoS One 2017;12:e0170955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30).Huxley RR, Filion KB, Konety S, Alonso A. Meta-analysis of cohort and case-control studies of type 2 diabetes mellitus and risk of atrial fibrillation. Am J Cardiol 2011;108:56–62 [DOI] [PMC free article] [PubMed] [Google Scholar]


