Abstract
Histoplasmosis is an emerging fungal disease, with global distribution. The disseminated form of the disease is a more severe infection, generally associated with AIDS. Classic diagnostic methods for histoplasmosis consist of microscopy, culture, and histopathology. More recently, the importance of Histoplasma antigen detection has dominated the literature on histoplasmosis diagnosis, but the relevance of molecular assays has not been as much studied. Here we describe the results of a systematic literature review focusing on studies that mainly compared immunological techniques (Histoplasma urine antigen detection) with molecular tests for the diagnosis of histoplasmosis. In addition to the review of comparative studies using such diagnostic techniques, the literature on polymerase chain reaction (PCR) tests in patients with disseminated histoplasmosis is also summarized. Two studies reported the comparison between immunological and molecular methods applied simultaneously for the diagnosis of disseminated histoplasmosis. PCR demonstrates a satisfactory performance assisting in the detection of Histoplasma spp. DNA in clinical samples.
Keywords: AIDS, histoplasmosis, immunological tests, molecular diagnosis, PCR
1. Introduction
Histoplasmosis is a global emerging fungal disease, with most cases reported in the American continent. The disease is the most common cause for hospitalization and death among the endemic mycoses in the U.S. [1,2]. In Brazil, 3530 patients were diagnosed with histoplasmosis between the years 1939 and 2018, which is likely to be underestimated. Histoplasmosis is endemic in all Brazilian regions, particularly in the Northeast, Central-West, Southeast, and South [3].
Histoplasmosis mainly affects the lungs from which it can disseminate to other body sites such as the adrenal glands, bone marrow, gastrointestinal tract, joints and the brain [2]. Disseminated histoplasmosis (DH)–the more severe and common form of the disease–generally occurs in AIDS patients, in addition to immunocompromised person on treatment with steroids, presenting with severe neutropenia as a result of cancer chemotherapy, as well as recipients of hematopoietic stem cell and solid organ transplantation [2,3].
Classical diagnosis of DH relies on histopathology, microscopy and fungal culture. However, these methods are known for their limited sensitivity, in addition to the prolonged time for culture to reveal results [4,5]. Over the last decade, several studies have shown Histoplasma antigen detection to be the main non-invasive test to diagnose such conditions [6,7]. Detection of circulating Histoplasma antigens in urine has proven to be highly sensitive (95%), but this methodology still has some limitations, such as cross-reactivity with other dimorphic fungi [8,9]. Conversely, in many countries where DH is endemic, Histoplasma antigen test is commercially not available, which opens a field of opportunities for other diagnostic tests to be used in association or in substitution for antigen detection [8,10].
Molecular tests are routinely used in many clinical centers to detect a variety of pathogens, including fungi. In this context, several articles have documented the performance of molecular tests (particularly PCR [polymerase chain reaction]) in DH patients. However, assays vary largely in terms of sequence of probes and primers, in addition to DNA extraction methods and tests platforms [11,12,13]. The diagnostic performance of molecular tests in patients for whom Histoplasma antigen detection is also available has not been properly explored. In view of this, the aim of this study was to compare the performance of molecular tests in the diagnosis of DH considering two main scenarios, related to the presence or the absence of Histoplasma antigen detection.
2. Methods
A PubMed systematic literature review was conducted using the following search strategy: “(histoplasmosis or histoplasma) and (diagnosis or sensitivity or specificity or performance or accuracy) and ((molecular or PCR or sequencing) and (antigen or antigenuria or ELISA))”. The literature review was built using the classical PICO structure, in which “P” stands for “population/patients”; “I” for “intervention”; “C” for “comparison/control”; and “O” for “outcome”. No language or date restriction was applied. References from selected articles were also reviewed. Publications describing the diagnosis of the disease by other methods (i.e., non-molecular) were excluded from the review, as well as studies involving histoplasmosis in non-humans.
3. Results
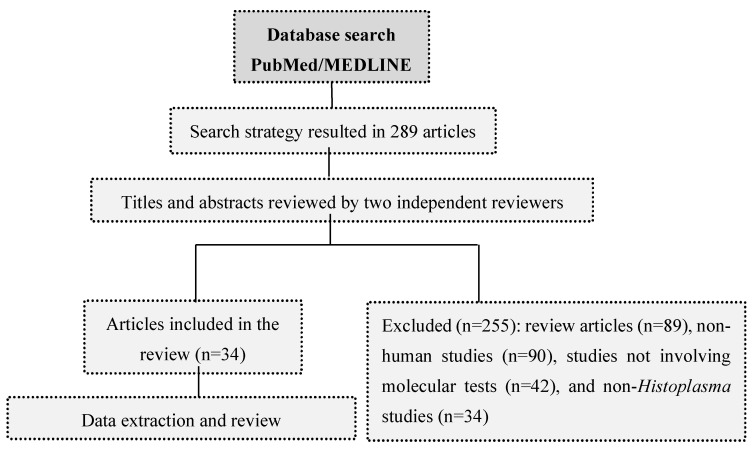
Figure 1 shows the flowchart with data selection and analysis methods used in the study. A total of 289 articles were found in the search. After exclusion of non-appropriate manuscripts, 34 publications were selected to review. From these publications, only two studies directly compared the use of molecular tests with Histoplasma antigen detection, in patients with DH. We summarize below the evidence regarding the use of molecular tests for the diagnosis of histoplasmosis.
Figure 1.
Flowchart with data selection and analysis methods used in the systematic review.
3.1. Comparison of Molecular and Immunological Diagnosis of DH
One of the studies comparing molecular tests with Histoplasma antigen assays was performed using urine samples [14]. The study evaluated the performance of a PCR-enzyme immunoassay (PCR-EIA) test against three comparators: two groups with variable concentrations of Histoplasma antigenuria and a negative control group (healthy volunteers) [14]. Twelve H. capsulatum and Blastomyces dermatitidis isolates were chosen to assess the pattern of recognition of the PCR primers. The MiraVista® test was used to detect Histoplasma antigen, fungal cultures were incubated for 8 weeks, and the molecular test targeted a 99-bp portion of the H. capsulatum 100-kDa protein gene. From 51 samples known to be positive by Miravista® test, only 5 (9.8%) were positive by culture and 4 (7.8%) were detected in the PCR-EIA test. Positive PCR results in urine specimens correlated well with positive culture results, but not with antigenuria.
In another publication, an HIV-infected patient with pulmonary histoplasmosis was reported for presenting a false-positive result with serum Aspergillus galactomannan testing [15]. Amplification and sequencing of the ITS1, 5,8S and ITS4 regions of ribosomal DNA, made directly from lung biopsy using panfungal primers, allowed for H. capsulatum identification. Mycological cultures turned positive after three weeks, with the presence of numerous thick-walled, echinulate macroconidia, typical of the Histoplasma genus, confirming the diagnosis of pulmonary histoplasmosis, primarily detected by the molecular (sequencing) method. The study addressed the potential interest of the Histoplasma DNA for the diagnosis of histoplasmosis, especially in endemic countries where H. capsulatum antigen testing may not be available.
3.2. Overview of the Performance of Molecular Methods in the Diagnosis of DH
There are several factors that influence the reliability and reproducibility of molecular tests, including the number and the type of samples tested. A summary of all studies in which molecular methods were used to diagnose histoplasmosis is presented in Table 1. Fungal culture is one of the best-performing specimens but this has little applicability in the routine diagnostic laboratory, since 4 to 6 weeks are required for fungal growth before PCR application [13]. Most studies in the literature evaluated the performance of nested PCR in the diagnosis of DH, a method that is associated with the increased risk of amplicons contamination, since it involves the manipulation of amplified products. Many of the PCR tests for histoplasmosis were developed in-house [11,12,13,16,17,18,19,20,21,22,23,24,25,26,27]. The gene encoding a 100 kDa molecular protein, which is described as necessary for the survival of H. capsulatum in human cells, has been the most common target for the diagnosis of histoplasmosis [11,12,16,19,23,24,27]. Hcp100 is part of the p100 gene family, and it is expressed in large quantities during fungal macrophage invasion [12]. This marker was first tested and standardized in a nested PCR test, with a reported sensitivity of 100% and a specificity of 95% [16,19]. However, as already stated nested PCR is a method that involves great care because of increased risk for contamination, since it involves the manipulation of amplified products.
Table 1.
Results of the literature review of studies in which molecular tests were used to diagnose disseminated histoplasmosis.
| Author and Year | n | Samples | Molecular Technique | DNA Extraction | Molecular Target | Probe | Sensitivity | Specificity |
|---|---|---|---|---|---|---|---|---|
| Bialek R et al. (2002) [16] | 100 | Biopsy | Nested PCR | QIAamp tissue kit Qiagen | 18S rDNA Hcp 100 |
None | NA | NA |
| Bracca, A. et al. (2003) [17] | 30 | Blood, biopsy, scraping from mucocutaneous lesions | Semi-nested PCR | Manual extraction | β-glucosidase | None | NA | NA |
| Guedes, H.L. et al. (2003) [18] | 31 | Fungal cultures | DNA Sequencing | Puregene DNA Kit Gentra.Systems | M Protein | None | 100% | 100% |
| Muñoz, C. et al. (2009) [19] | 146 | Fungal cultures | Nested PCR | DNA Minikit Qiagen | Hcp 100 | None | 100% | 92% |
| Muñoz, B. et al. (2010) [20] | 6 | Fungal cultures | Conventional PCR | Manual extraction | M Protein | None | NA | NA |
| Frías-De-León, M. G. et al. (2012) [21] | 40 | Fungal cultures | (RAPD)-PCR | NA | SCAR Markers | None | NA | 100% |
| Ohno, H. et al. (2013) [22] | 7 | Fungal cultures and cinical samples * | Nested PCR | NA | M Protein | None | NA | NA |
| Dantas, K. C. et al. (2013) [23] | 40 | Whole blood and serum | Nested PCR | NA | 18S rDNA Hcp 100 |
None | 96%–98% | HC100 (97%-Whole Blood, 95%-Serum) e HC18S (90% Whole Blood, 88% Serum) |
| Buitrago, M. J. et al. (2013) [24] | 10 | Fungal cultures | Nested, Real Time and Conventional PCR | DNeasy Plant MiniKit Qiagen | Hcp 100, SCAR, ITS1 | Taqman HcITS-155 |
SCAR–43% Hcp 100 - 89.5 |
100% |
| Scheel, C. M. et al. (2014) [12] | 50 | Fungal cultures | Nucleic acid amplification via LAMP | Qiagen Dneasy Kit | Hcp100 | None | NA | 100% |
| Gago, S. et al. (2014) [25] | 43 | Fungal cultures and bronchoalveolar lavage | Multiplex real-time PCR | DNeasy Plant MiniKit Qiagen | ITS | None | 90% | 100% |
| Muraosa, Y. et al. (2015) [13] | 19 | Fungal cultures and clinical samples * | Cycling probe-based real-time PCR and Nested real-time PCR | PrepManTM Ultra Life Technologies | NAALADase Gene | Hist1probe3 | Real Time PCR–77% Nested PCR–33% |
NA |
| Brilhante, R. S. et al. (2016) [26] | 16 | Blood | Conventional PCR | CTAB | RYP1 | None | 100% | 100% |
| Frías-De-León, M. G. et al. (2017) [11] | 4 | Serum | Nested PCR | Qiagen Dneasy Kit | Hcp100 | None | NA | NA |
| Dantas, K.C. et al. (2018) [27] | 40 | Blood | Nested PCR | QIAamp Blood DNA Mini Kit | 18S rDNA Hcp 100 |
None | 18%–60% | 85%–100% |
Legend: NA, data not available; RAPD, random amplified polymorphic DNA; LAMP, Loop mediated isothermal amplification; PCR, Polymerase chain reaction; CTAB, cetyltrimethylammonium bromide. * Clinical Samples include blood, serum, biopsy, bronchoalveolar lavage, and scraping.
4. Discussion
In this literature review, we were able to find only two studies in which molecular tests were used in parallel to Histoplasma immunological antigen detection for DH diagnosis [14,15]. One of the studies [14] reported a very low sensitivity for PCR using urine samples. Urine was tested in the study because this is considered the optimal sample for Histoplasma antigen detection using EIA. However, with regard to PCR, urine is usually seen as a clinical material that contains many potential interferents with the PCR reaction. Additional points must also be considered: (i) some false-positive may have occurred in the Histoplasma antigen test, since this is known to cross-reacts with Blastomyces dermatitidis, also endemic in the U.S.; also, (ii) primers may not have allowed for the detection of all variants of H. capsulatum with satisfactory sensitivity. In any case, the study does not tell us about the performance of Histoplasma PCR in additional clinical samples, such as whole blood, bone marrow aspirate, bronchoalveolar lavage (BAL) fluid, and tissues. Besides that, Histoplasma antigen detection has become consolidated the leading technique to DH diagnosis with excellent performance, easy to obtain specimens and also important for monitoring patients’ responses to antifungal therapy [28].
Our study has shown that more than a dozen publications reported the good performance of molecular methods in patients with DH, either alone or in association with conventional diagnostic methods (i.e., microscopy, culture and histopathology). Most of these studies have used whole blood, serum or fungal culture as the appropriate specimen for PCR testing, with a very high sensitivity and specificity. Molecular diagnosis can be effectively applied to lung biopsies, in situations in which other classical methods of pathogen identification are usually not effective [15,29]. Molecular tests are arguably important in regions where DH is not endemic, due to limited expertise in H. capsulatum identification.
The analytical performance of the molecular assays in the DH diagnosis varies according to disease stage and clinical form of histoplasmosis [30]. A recent meta-analysis showed the lack of consensus regarding the methodologies, particularly PCR protocols and gene targets (100-KDa-like-protein genes and amplification of ITS regions). For molecular assays, the overall specificity in the meta-analysis was 99% and overall sensitivity was 95%. Similar to the antigen testing, PCR presented excellent analytical performance, displaying a similar accuracy in comparison to the antigenuria-based assays [30]. By reviewing studies that compared primers, it was possible to see that Hcp100 is the most widely targeted gene and has shown better methodological performance [23,24].
This review demonstrated the performance of molecular tests in several studies involving patients with DH. PCR was applied to a wide range of clinical samples (e.g., biopsy, whole blood, serum, and cultures) [31,32]. The variability of molecular method applications is noticeable, which makes it difficult to make any relevant comparison. The reactions were done in different ways, with large variability in terms of DNA extraction, amplification targets, probes, and master mixes. No commercial PCR tests is available. In a multicenter comparison of PCR protocols for identification H. capsulatum DNA [24], all the protocols were specific and no false positive results were detected. Even though most studies in the literature have been based on nested PCR, real-time protocols were the most accurate and reliable. The applicability of PCR tests against Histoplasma species in the follow up of patients on treatment with antifungal drugs is also that deserve further investigation.
This study is limited by the scarce number of publications that directly compared immunological and molecular methods in patients with DH. There is a gap in the literature to be filled by future studies that consider this type of analysis, therefore contributing to the diagnosis of histoplasmosis. Most studies applied PCR from fungal cultures, which is of limited clinical interest.
In conclusion, this literature review showed that molecular tests have a good clinical performance in patients with DH. Most studies were performed with nested-PCR, so there is a need to further explore the application of real-time PCR in histoplasmosis. Histoplasma antigen detection by EIA has a central role in the DH diagnosis, but in only two publications these tests were compared to Histoplasma PCR. Considering that Histoplasma antigen is not commercially available in most endemic countries for histoplasmosis, and based on the assumption that many tertiary hospitals have PCR machines in place, molecular tests have the potential to facilitate the diagnostic routine of histoplasmosis in many circumstances.
Author Contributions
A.C.P., I.C.d.S.V. and D.F.D.L. were involved in the conception and design of the study; I.C.d.S.V. and D.F.D.L. reviewed the literature and wrote the manuscript; A.C.P conducted a critical review of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
A.C.P. works with the molecular as well conventional diagnosis of fungal infections in a private hospital. He has received research grants as well as given paid talks on behalf of Gilead, Pfizer, MSD, IMMY and Astellas Pharma, all drug companies acting in the mycology field.
References
- 1.Chu J.H., Feudtner C., Heydon K., Walsh T.J., Zaoutis T.E. Hospitalizations for endemic mycoses: A population-based national study. Clin. Infect. Dis. 2006;42:822–825. doi: 10.1086/500405. [DOI] [PubMed] [Google Scholar]
- 2.Wheat L.J., Unlucky M.M., Bahr N.C., Spec A., Relich R.F., Hage C. Histoplasmosis. Infect. Dis. Clin. N. Am. 2016;30:207–227. doi: 10.1016/j.idc.2015.10.009. [DOI] [PubMed] [Google Scholar]
- 3.Almeida M.A., Almeida-Silva F., Guimarães A.J., Almeida-Paes R., Zancopé-Oliveira R.M. The occurrence of histoplasmosis in Brazil: A systematic review. Int. J. Infect. Dis. 2019;86:147–156. doi: 10.1016/j.ijid.2019.07.009. [DOI] [PubMed] [Google Scholar]
- 4.Wheat L.J. Improvements in diagnosis of histoplasmosis. Expert Opin. Biol. Ther. 2006;6:1207–1221. doi: 10.1517/14712598.6.11.1207. [DOI] [PubMed] [Google Scholar]
- 5.Hage C.A., Ribes J.A., Wengenack N.L., Baddour L.M., Assi M., McKinsey D.S., Hammoud K., Alapat D., Babady N.E., Parker M., et al. A multicenter evaluation of tests for diagnosis of histoplasmosis. Clin. Infect. Dis. 2011;53:448–454. doi: 10.1093/cid/cir435. [DOI] [PubMed] [Google Scholar]
- 6.Theel E.S., Jespersen D.J., Harring J., Mandrekar J., Binnicker M.J. Evaluation of an enzyme immunoassay for detection of Histoplasma capsulatum antigen from urine specimens. J. Clin. Microbiol. 2013;51:3555–3559. doi: 10.1128/JCM.01868-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Costa M.R.E., Lacaz C.S., Kawasaki M., De Camargo Z.P. Conventional versus molecular diagnostic tests. Med. Mycol. 2000;38:139–145. doi: 10.1080/mmy.38.s1.139.145. [DOI] [PubMed] [Google Scholar]
- 8.Wheat J., Wheat H., Connolly P., Kleiman M., Supparatpinyo K., Nelson K., Bradsher R., Restrepo A. Cross-reactivity in Histoplasma capsulatum variety capsulatum antigen assays of urine samples from patients with endemic mycoses. Clin. Infect. Dis. 1997;24:1169–1171. doi: 10.1086/513647. [DOI] [PubMed] [Google Scholar]
- 9.Wheat L.J., Connolly P., Durkin M., Book B.K., Tector A.J., Fridell J., Pescovitz M.D. False-positive Histoplasma antigenemia caused by antithymocyte globulin antibodies. Transpl. Infect. Dis. 2004;6:23–27. doi: 10.1111/j.1399-3062.2004.00045.x. [DOI] [PubMed] [Google Scholar]
- 10.LeMonte A., Egan L., Connolly P., Durkin M., Wheat L.J. Evaluation of the IMMY ALPHA Histoplasma antigen enzyme immunoassay for diagnosis of histoplasmosis marked by antigenuria. Clin. Vaccine Immunol. 2007;14:802–803. doi: 10.1128/CVI.00035-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Frías-De-León M.G., Ramírez-Bárcenas J.A., Rodríguez-Arellanes G., Velasco-Castrejón O., Taylor M.L., Reyes-Montes M.R. Usefulness of molecular markers in the diagnosis of occupational and recreational histoplasmosis outbreaks. Folia Microbiol. 2017;62:111–116. doi: 10.1007/s12223-016-0477-4. [DOI] [PubMed] [Google Scholar]
- 12.Scheel C.M., Zhou Y., Theodoro R.C., Abrams B., Balajee S.A., Litvintseva A.P. Development of a Loop-Mediated Isothermal Amplification Method for Detection of Histoplasma capsulatum DNA in Clinical Samples. J. Clin. Microbiol. 2014;52:483–488. doi: 10.1128/JCM.02739-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Muraosa Y., Toyotome T., Yahiro M., Watanabe A., Shikanai-Yasuda M.A., Kamei K. Detection of Histoplasma capsulatum from clinical specimens by cycling probe-based real-time PCR and nested real-time PCR. Med. Mycol. J. 2016;54:433–438. doi: 10.1093/mmy/myv106. [DOI] [PubMed] [Google Scholar]
- 14.Tang Y.W., Li H., Durkin M.M., Sefers S.E., Meng S., Connolly P.A., Stratton C.W., Wheat L.J. Urine polymerase chain reaction is not as sensitive as urine antigen for the diagnosis of disseminated histoplasmosis. Diagn. Microbiol. Infect. Dis. 2006;54:283–287. doi: 10.1016/j.diagmicrobio.2005.10.008. [DOI] [PubMed] [Google Scholar]
- 15.Pineau S., Talarmin J.P., Morio F., Grossi O., Boutoille D., Léauté F., Le Pape P., Gay-Andrieu F., Miegeville M., Raffia F. Contribution de la biologie moléculaire et de l’antigénémie galactomannane aspergillaire au diagnostic de l’histoplasmose. Méd. Maladies Infect. 2010;40:541–543. doi: 10.1016/j.medmal.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 16.Bialek R., Feucht A., Aepinus C., Just-Nübling G., Robertson V.J., Knobloch J., Hohle R. Evaluation of two nested PCR assays for detection of Histoplasma capsulatum DNA in human tissue. J. Clin. Microbiol. 2002;40:1644–1647. doi: 10.1128/JCM.40.5.1644-1647.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bracca A., Tosello M.E., Girardini J.E., Amigot S.L., Gomez C., Serra E. Molecular detection of Histoplasma capsulatum var. capsulatum in human clinical samples. J. Clin. Microbiol. 2003;41:1753–1755. doi: 10.1128/JCM.41.4.1753-1755.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guedes H.L., Guimarães A.J., Muniz M.d.M., Pizzini C.V., Hamilton A.J., Peralta J.M., Deepe G.S.J., Zancopé-Oliveira R.M. PCR assay for identification of Histoplasma capsulatum based on the nucleotide sequence of the M antigen. J. Clin. Microbiol. 2003;40:535–539. doi: 10.1128/JCM.41.2.535-539.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muñoz C., Gómez B.L., Tobón A., Arango K., Restrepo A., Correa M.M., Muskus C., Cano L.E., González A. Validation and clinical application of a molecular method for identification of Histoplasma capsulatum in human specimens in Colombia, South America. Clin. Vaccine Immunol. 2009;17:62–67. doi: 10.1128/CVI.00332-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Muñoz B., Martínez M.A., Palma G., Ramírez A., Frías M.G., Reyes M.R., Taylor M.L., Higuera A.L., Corcho A., Manjarrez M.E. Molecular characterization of Histoplasma capsulatum isolated from an outbreak in treasure hunters Histoplasma capsulatum in treasure hunters. BMC Infect. Dis. 2010:10–264. doi: 10.1186/1471-2334-10-264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Frías De León M.G., Arenas López G., Taylor M.L., Acosta Altamirano G., Reyes-Montes M.R. Development of specific sequence-characterized amplified region markers for detecting Histoplasma capsulatum in clinical and environmental samples. J. Clin. Microbiol. 2012;50:673–679. doi: 10.1128/JCM.05271-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ohno H., Tanabe K., Umeyama T., Kaneko Y., Yamagoe S., Miyazaki Y. Application of nested PCR for diagnosis of histoplasmosis. J. Infect. Chemother. 2013;19:999–1003. doi: 10.1007/s10156-013-0548-2. [DOI] [PubMed] [Google Scholar]
- 23.Dantas K.C., Freitas R.S., Moreira A.P., Silva M.V., Benard G., Vasconcellos C., Criado P.R. The use of nested Polymerase Chain Reaction (nested PCR) for the early diagnosis of Histoplasma capsulatum infection in serum and whole blood of HIV-positive patients. An. Bras. Dermatol. 2013;88:141–143. doi: 10.1590/S0365-05962013000100025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Buitrago M.J., Canteros C.E., Frías De León G., González Á., Marques-Evangelista De Oliveira M., Muñoz C.O., Ramirez J.A., Toranzo A.I., Zancope-Oliveira R., Cuenca-Estrella M. Comparison of PCR protocols for detecting Histoplasma capsulatum DNA through a multicenter study. Rev. Iberoam. Micol. 2013;30:256–260. doi: 10.1016/j.riam.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 25.Gago S., Esteban C., Valero C., Zaragoza O., Puig de la Bellacasa J., Buitrago M.J. A multiplex real-time PCR assay for identification of Pneumocystis jirovecii, Histoplasma capsulatum, and Cryptococcus neoformans/Cryptococcus gattii in samples from AIDS patients with opportunistic pneumonia. J. Clin. Microbiol. 2014;52:1168–1176. doi: 10.1128/JCM.02895-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brilhante R.S., Guedes G.M., Riello G.B., Ribeiro J.F., Alencar L.P., Bandeira S.P., Castelo-Branco D.S., Oliveira J.S., Freire J.M., Mesquita J.R., et al. RYP1 gene as a target for molecular diagnosis of histoplasmosis. J. Microbiol. Methods. 2016;130:112–114. doi: 10.1016/j.mimet.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 27.Dantas K.C., Freitas R.S., Silva M.V., Criado P.R., Luiz O.D.C., Vicentini A.P. Comparison of diagnostic methods to detect Histoplasma capsulatum in serum and blood samples from AIDS patients. PLoS ONE. 2018;13:1. doi: 10.1371/journal.pone.0190408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Theel E.S., Harring J.A., Dababneh A.S., Rollins L.O., Bestrom J.E., Jespersen D.J. Reevaluation of commercial reagents for detection of Histoplasma capsulatum antigen in urine. J. Clin. Microbiol. 2015;53:1198–1203. doi: 10.1128/JCM.03175-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Falci D.R., Hoffmann E.R., Paskulin D.D., Pasqualotto A.C. Progressive disseminated histoplasmosis: A systematic review on the performance of non-culture-based diagnostic tests. Braz. J. Infect. Dis. 2017;21:7–11. doi: 10.1016/j.bjid.2016.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Caceres D.H., Knuth M., Derado G., Lindsley M.D. Diagnosis of Progressive Disseminated Histoplasmosis in Advanced HIV: A Meta-Analysis of Assay Analytical Performance. J. Fungi. 2019;5:76. doi: 10.3390/jof5030076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Imhof A., Schaer C., Schoedon G., Schaer D.J., Walter R.B., Schaffner A., Schneemann M. Rapid detection of pathogenic fungi from clinical specimens using LightCycler real-time fluorescence PCR. Eur. J. Clin. Microbiol. Infect. Dis. 2003;22:558–560. doi: 10.1007/s10096-003-0989-0. [DOI] [PubMed] [Google Scholar]
- 32.Martagon-Villamil J., Shrestha N., Sholtis M., Isada C.M., Hall G.S., Bryne T., Lodge B.A., Reller L.B., Procop G.W. Identification of Histoplasma capsulatum from culture extracts by real-time PCR. J. Clin. Microbiol. 2003;41:1295–1298. doi: 10.1128/JCM.41.3.1295-1298.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]