Abstract
Introduction
In late 2019, an outbreak of a new coronavirus named severe acute respiratory syndrome coronavirus 2 was detected in Wuhan, China. A great percentage of patients with this disease developed symptoms of dry cough, malaise, and a high fever. During this time, several patients requiring assessment and treatment of endodontic emergencies were directed to the School and Hospital of Stomatology at Wuhan University, Wuhan, China. We examined the characteristics of these patients.
Methods
A total of 96 patients with a mean age of 42.24 ± 18.32 years visited the general and emergency department of the School and Hospital of Stomatology at Wuhan University because of endodontic emergencies during the peak period of February 22 to March 2, 2020. Patient information was collected and organized by date of visit, sex, age, and systemic disease history. Body temperature was measured and acquired for each patient, a coronavirus disease 2019 (COVID-19) epidemiologic investigation questionnaire was given to each patient, an endodontic diagnosis was determined for the offending tooth, and a verbal numerical rating scale (VNRS) was used to record pain levels.
Results
Of the total patient visits during this period, 50.26% of visits were for endodontic treatment. No patients had a fever (>37.2°C). One patient with a confirmed COVID-19 history was admitted after recovery. Three admitted patients had been exposed to confirmed or suspected COVID-19 patients. Twelve admitted patients (12.5%) with a mean age of 62.42 ± 13.77 years had a history of systemic diseases. The most common age group for endodontic emergencies was 45–64 years (30.21%), and patients of this group showed a significantly higher mean VNRS score compared with that of the 6- to 19-year age group and the 20- to 34-year age group (P < .05). The majority of endodontic emergency diagnoses were diseases of symptomatic irreversible pulpitis (53.10%). Patients who were diagnosed with symptomatic irreversible pulpitis, symptomatic apical periodontitis, and acute apical abscess showed a significantly higher mean VNRS score than that of other groups (P < .05).
Conclusions
Endodontic emergencies, with symptomatic irreversible pulpitis being the most common, consist of a much higher proportion of dental emergencies in a COVID-19 high-risk area than normally. Vital pulp therapy can advantageously reduce treatment time, resulting in a reduced risk of infection for vital pulp cases. Rubber dams, personal protective equipment, and patient screening are of great importance during the COVID-19 outbreak in protecting clinicians.
Key Words: Coronavirus disease 19 outbreak, endodontic emergency, epidemiologic investigation, verbal numerical rating scale, vital pulp therapy
Significance.
Endodontic emergencies consist of a significantly higher proportion of dental emergencies in a COVID-19 high-risk area than normally. Rubber dams, personal protective equipment, and patient screening play an important role in protecting clinicians during the COVID-19 outbreak.
Cases of the novel severe acute respiratory syndrome coronavirus, the causative agent of coronavirus disease 2019 (COVID-19), were first reported in Wuhan, Hubei, China, in December 20191. Ever since the emergence of these first cases, COVID-19 has become a public health crisis globally. As of March 2, 2020, the National Health Commission of China reported 49,426 cumulative cases and 2251 deaths in the city of Wuhan2. To halt transmission, Hubei Province activated its level 2 response to public health emergencies on January 23, 2020, and the city of Wuhan with a population exceeding 11 million was under lockdown and remains under lockdown at present3, 4, 5. In consideration of the risk dental treatment may pose during the outbreak, the Hubei Province government suspended regular dental treatments, allowing only emergency treatments4. Endodontic infections can cause serious pain6, and endodontic emergencies are considered to be an important category of dental emergencies7. From January 24, 2020, all patients receiving emergency dental treatment were directed to the general and emergency department of the School and Hospital of Stomatology, Wuhan University (WHUSS), which remained the only hospital open within Wuhan for emergency dental treatments until March 2, 2020. Since February 22, 2020, the general and emergency department began administering a COVID-19 epidemiologic investigation questionnaire, which was of particular interest for the purposes of this study. This study aimed to analyze the characteristics of endodontic emergency patients at WHUSS between February 22 and March 2, 2020, and is the first descriptive study that examines endodontic emergency dental patients at the epicenter of the COVID-19 outbreak. In this study, we also provided suggestions for endodontic practice and infection control strategies based on these novel observations.
Materials and Methods
Selection of Subjects
This study was approved by the Ethics Committee of the School and Hospital of Stomatology at Wuhan University (project number: 2020B08). Patients who visited the general and emergency department at WHUSS for endodontic emergencies from February 22 to March 2, 2020, were reviewed. Body temperature was acquired for each patient, and a COVID-19 epidemiologic questionnaire was given before dental treatment.
The questionnaire consisted of the following 4 questions:
-
1.
Are you a confirmed or suspected COVID-19 patient who has recovered after treatment?
-
2.
Are you a confirmed or suspected COVID-19 patient with no symptoms?
-
3.
Have you recently been showing COVID-19 symptoms? (optional) Such as a fever, cough, fatigue, vomiting, etc.
-
4.
Have you been in contact with confirmed or suspected COVID-19 patients recently?
Patients were asked to describe their level of pain using a verbal numerical rating scale (VNRS)6. Only patients who had answered the questionnaire, described their level of pain, had their body temperature measured, and received an endodontic diagnosis were included in this study.
Evaluations of Subjects
Patient information such as date of visit, sex, age, systemic disease history, and VNRS score were included in the study. The acquired body temperatures and the COVID-19 epidemiologic investigation questionnaires were reviewed. Diagnoses were based on the recommended consensus by the American Board of Endodontics and the American Association of Endodontics8. The number of total patient visits and the type of visits at the general and emergency department of WHUSS during the dates studied were compared with past statistics corresponding to these same dates in 2018 and 2019.
Statistical Analysis
The characteristics of patients with endodontic emergency were stratified by subgroups including sex, age group, and diagnosis by multivariate Poisson regression. The independent sample t test or 1-way analysis of variance was performed to compare the mean VNRS score. VNRS scores with P set to <.05 were used for statistical significance. All statistical analyses were performed with SPSS 20.0 software (IBM Corp, Armonk, NY).
Results
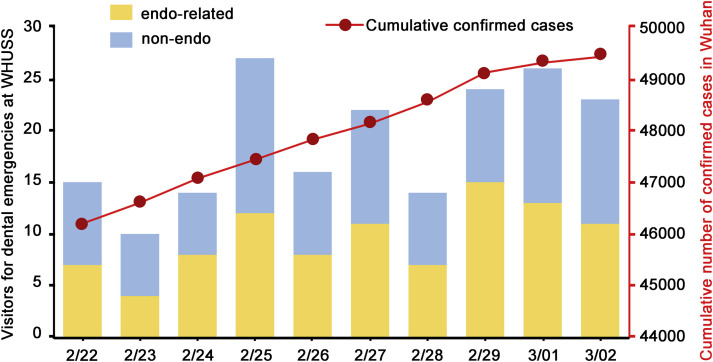
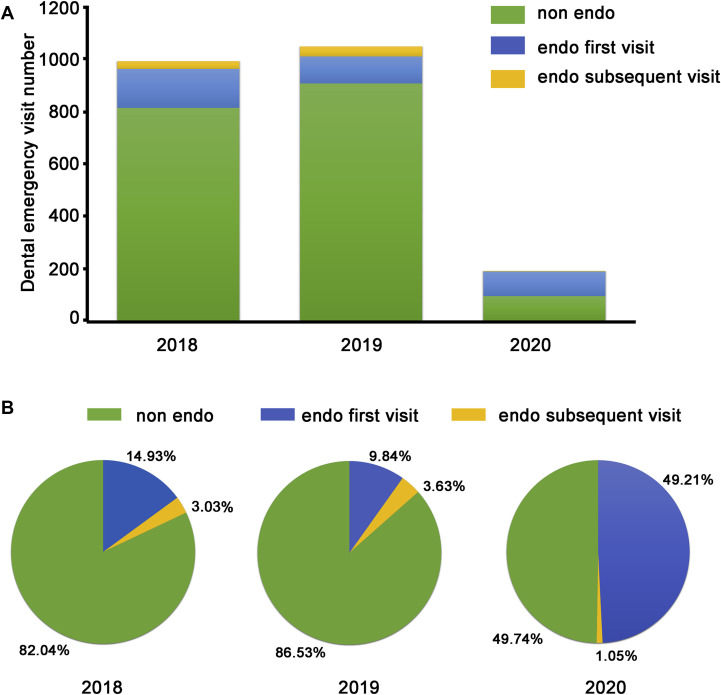
Demographic patient information is shown in Figure 1 along with the cumulative COVID-19 cases in Wuhan2. The percentage (50.26%) of endodontic emergency patients (n = 96) among all dental emergency patients (N = 191) is shown in Figure 2 as well as that at the corresponding period in 2019 (13.47%, 141/1047) and 2018 (17.96%, 178/991). Endodontic emergency patients who were included in the study had a mean age of 42.24 ± 18.32 years, 52.08% of whom (n = 50/96) were male and 47.92% (n = 46/96) were female. Twelve admitted patients with a mean age of 62.42 ± 13.77 years had a history of systemic diseases, including diabetes, cardiovascular disease, and hypertension. A fever (>37.2°C) was not detected in any of the patients who presented because of endodontic emergencies, and the results of the COVID-19 questionnaires are presented in Table 1 . One admitted patient (1.04%, 1/96) had a confirmed COVID-19 history and was recovering at the time of treatment. Three admitted patients (3.13%, 3/96) had a history of exposure to confirmed or suspected COVID-19 patients recently. Two of the 3 were health care workers, 1 of whom was the child of a suspected COVID-19–positive patient. No patients reported a history of confirmed or suspected asymptomatic COVID-19 or were showing symptoms of COVID-19.
Figure 1.
The demographic information of patients who had visited WHUSS because of dental emergencies and the cumulative number of confirmed cases with COVID-19 in the city of Wuhan from February 22 to March 2, 2020.
Figure 2.
Dental emergency patients from February 22, 2020, to March 2, 2020, and in 2019 and 2018. (A) The total dental emergency visits by year and by type of visit. (B) The proportion of patients with endodontic emergency, including the endodontic (endo) first visit and endo subsequent visit.
Table 1.
The Results of the COVID-19 Epidemiologic Investigation Questionnaires
| Variables | Number | Percentage |
|---|---|---|
| Confirmed or suspected COVID-19 patients who have recovered after treatment | 1 | 1.04 |
| Confirmed or suspected COVID-19 patients with no symptoms | 0 | 0.00 |
| Patients having COVID-19 symptoms recently | 0 | 0.00 |
| Patients having come in contact with confirmed or suspected COVID-19 patients recently | 3 | 3.13 |
COVID-19, coronavirus disease 2019.
VNRS scores by sex, age, and endodontic emergencies are summarized in Table 2 . Patients in the 45- to 64-year age group accounted for 30.02% of the total endodontic emergency patients and showed significantly higher VNRS scores compared with those of patients in the 6- to 19-year and 20- to 34-year age groups (P < .05). Among the patient population in this study, 97.90% were first-visit patients, and the most common endodontic emergency diagnosis was symptomatic irreversible pulpitis (53.13% or 51/96 patients). In addition, patients with symptomatic irreversible pulpitis, symptomatic apical periodontitis, and acute apical abscess had significantly higher reported VNRS scores than any other diagnosis (P < .05).
Table 2.
The VNRS (Mean ± Standard Deviation) in Different Sex, Age Groups, and Endodontic Emergency Diagnoses at 10 Working Days during the Coronavirus Disease 2019 Outbreak
| Variables | Number | Percentage (%) | Mean VNRS score | P value |
|---|---|---|---|---|
| Sex | >.05 | |||
| Male | 50 | 52.10 | 6.24 ± 1.76 | |
| Female | 46 | 47.90 | 6.35 ± 1.78 | |
| Age | <.05 | |||
| <6 years | 0 | 0.00 | NA | |
| 6–19 years | 11 | 11.50 | 5.09 ± 1.76 | |
| 20–34 years | 20 | 20.80 | 6.05 ± 2.14 | |
| 35–44 years | 20 | 20.80 | 6.7 ± 1.38 | |
| 45–64 years | 29 | 30.20 | 6.86 ± 1.53 | |
| ≥65 years | 15 | 15.60 | 6.67 ± 1.35 | |
| Diagnoses | <.05 | |||
| Diagnosis at endodontic first visit | 94 | 97.90 | ||
| Reversible pulpitis | 8 | 8.30 | 4.25 ± 1.98 | |
| Symptomatic irreversible pulpitis | 51 | 53.13 | 7.22 ± 0.70 | |
| Symptomatic apical periodontitis | 16 | 16.67 | 6.63 ± 1.89 | |
| Chronic apical abscess | 10 | 10.40 | 5.10 ± 1.52 | |
| Acute apical abscess | 4 | 4.20 | 7.00 ± 0.00 | |
| Complicated crown fracture | 2 | 2.10 | 6.00 ± 0.00 | |
| Dislocation of tooth | 3 | 3.10 | 4.33 ± 2.08 | |
| Endodontic subsequent visit | 2 | 2.10 | 3.00 ± 0.00 |
NA, not applicable; VNRS, verbal numerical rating scale.
Discussion
The total number of patients attending the general and emergency department at WHUSS during the COVID-19 outbreak (N = 191) in our study was 18.24% of that of the corresponding periods in 2019 (n = 1047) and 19.27% of that in 2018 (n = 991). These results are consistent with that of a previous study9 that examined patient visits at the Prince Philip Dental Hospital in Hong Kong 10 working days after the severe acute respiratory syndrome outbreak in 2003, during which visits dropped to less than one fifth. The percentage of endodontic emergency patients has increased from 13.47% in 2019 and 17.96% in 2018 to 50.26% during the COVID-19 outbreak in the study. This observed increase could be accounted for by the closing of other facilities that were available to treat endodontic patients under normal operations and possibly by the reduction of trauma as an indirect result of the lockdown. The reduction of outdoor activities by the lockdown may consequently result in a decrease in trauma occurrences, which was reportedly the chief complaint among patients who visited the dental emergency room of a dental hospital in Korea10. These results highlight patient needs for endodontic treatment even under public health emergencies.
In this study, there was nearly the same ratio of male to female patients for both endodontic emergency patients (1.1:1) and all dental emergency patients (1.2:1), which is in contrast to other studies11, 12, 13, 14, 15 that have shown a greater percentage of male patients presenting with dental emergencies. However, this discrepancy may be caused by the higher proportion of endodontic emergency patients in our patient population. The largest age group for endodontic emergencies was 45–64 years (30.21%, 29/96) in our study. Importantly, older age and the existence of underlying comorbidities are associated with a poorer COVID-19 prognosis4 , 16 , 17. Because patients older than 65 years represented approximately 15% of all patients, care should be exercised to avoid cross contamination.
Patient screening was crucial during the severe acute respiratory syndrome epidemic in 2002 and 200318. An important tool in patient screening is the use of disease-specific questionnaires, which can differ depending on the location at which they are used (eg, epicenter vs other sites). In this study, 4 patients with a previous COVID-19 history or possible COVID-19 cases were identified using the questionnaire. A fever was reported to be the most common clinical symptom (98%) for 41 patients diagnosed with COVID-19 in a previous study19. No patient with a fever presented to WHUSS for endodontic emergencies. Conversely, a patient with pyogenic osteomyelitis of the jaw was found to have a fever (>37.2°C) but tested negative for COVID-19 by a series of diagnostic tests. Notably, several infections of the oral cavity could present with a fever that could confound the diagnosis of COVID-19; thus, a fever alone should not be the only sign and symptom of COVID-19 to be evaluated, and oral disease needs to be accurately diagnosed. The diagnosis of COVID-19 is currently based on a combination of epidemiologic information, clinical symptoms, chest computed tomographic imaging findings, and laboratory tests such as on reverse-transcription polymerase chain reaction (RT-PCR) respiratory tract specimens4. Sabino-Silva et al20 have raised important questions about the role saliva plays in the human-to-human transmission of diseases, in particular respiratory coronaviruses21 , 22.
The incubation period of COVID-19 has been estimated to be between 2 and 14 days5. It has been shown that patients with no symptoms or during incubation periods may have the potential to infect others5. Positive RT-PCR test results have been reported in recovered patients23. Endodontists should take appropriate measures to stay safe. During the COVID-19 outbreak, dentists in WHUSS were equipped with disposable N95 masks, gloves, caps, shoe covers, face shields, and gowns4. From February 22, 2020, patients with a fever, patients who had answered “yes” to any of the 4 questions on the questionnaire, or patients needing dental procedures producing droplets and/or aerosols were required to undergo examination and treatment in an isolated clinic room with dentists equipped with protective suits instead of gowns4. To date, no cases of COVID-19 were reported among the 26 working staff members of the general and emergency department at WHUSS working during the COVID-19 outbreak. RT-PCR findings for all working staff came back negative on March 24, 2020. Before the beginning of the study, 9 working staff members at the hospital level were confirmed to have COVID-19, including 3 doctors, 3 nurses, 2 administrative staff, and 1 postgraduate student4. This suggests that the safety precautions and screening measures enforced since February 22, 2020, were effective in protecting working staff.
Symptomatic irreversible pulpitis was the most common endodontic emergency, with a significantly high VNRS score in our study. Treatments for endodontic emergency were challenging during the COVID-19 outbreak because inhalation of airborne particles and aerosols produced during dental procedures on patients with COVID-19 could potentially expose dentists to the virus20, thus making them high-risk procedures. Reducing treatment time and exposure control are 2 ways the risk of infection for endodontic treatment could be reduced. For vital pulp cases such as pulpitis, vital pulp therapy including pulpotomy or pulp capping might be helpful in terms of shortening the treatment time. Pulpotomy has been reported to reduce pain symptoms in nearly 90% of dental emergency patients 1 day after treatment24. Partial pulpotomy using mineral trioxide aggregate (MTA) sustained a good success rate (85%) over 3-year follow-ups in mature permanent teeth clinically diagnosed with irreversible pulpitis25, and full pulpotomy using MTA showed a 92.7% success rate at a 3-year follow-up for caries-exposed pulps in mature permanent molar teeth26. Direct pulp capping with MTA showed a cumulative survival rate of 85% in adult molars with carious pulpal exposure at 36 months27. For cases that required root canal treatments, cone-beam computed tomographic imaging and single-file systems should be considered. Besides the advantages of detecting root canal location and configuration28, cone-beam computed tomographic examination could avoid nausea or vomiting for patients that may occur during intraoral x-ray examination and prevent exposure to patients’ oral cavity4. During root canal preparation, single-file nickel-titanium systems could be used to save working time29 as well as prevent the risk of resterilization. For any treatment that produces droplets and/or aerosols, Ather et al30 suggested a number of preventative measures, such as the use of rubber dams. It has been reported that up to 70% of airborne particles could be reduced around a 3-ft diameter of the operational field when a rubber dam is used31. In addition, a rubber dam is not only able to limit the diffusion of the aerosol but is also likely to dramatically reduce or even eliminate the presence of salivary components in the aerosol.
Only 5 cases of traumatic dental injury including 2 cases of “complicated crown fracture” and 3 cases of “dislocation of tooth,” respectively, were diagnosed in our study. Two patients made a subsequent visit for the completion of their root canal treatments. An online platform for patient consultations by WHUSS was made available starting February 3, 20204. It was reported that more than 1600 patients had used this consultation platform, and only dental emergency cases were suggested for treatment at the hospital4.
In addition to providing endodontic treatment, endodontists should pay attention to patients’ psychological health during the COVID-19 outbreak32. Public health emergencies may negatively impact individuals’ mental health33. For instance, 1 patient in our study who had a diagnosis of reversible pulpitis with dentin hypersensitivity had a high VNRS score of 8. She demonstrated extreme anxiety and fear toward gaining a fever as a result of oral disease inflammation. During the COVID-19 outbreak period, patients may suffer from psychological stress; therefore, endodontists should not only focus on the treatments of patients’ endodontic diseases but also their psychological state at times of emergency.
In conclusion, endodontic emergencies consist of a much higher portion of dental emergencies in a COVID-19 high-risk area than normally. Reducing the treatment time and exposure control are 2 ways to significantly reduce the risk of severe acute respiratory syndrome coronavirus spreading during endodontic treatment. Vital pulp therapy has the advantage of shortening the treatment time. Rubber dams, personal protective equipment, and patient screening are of great importance during the COVID-19 outbreak in protecting clinicians. Dentists should focus not only on the dental treatment but also patients’ psychological status during public health emergencies.
CRediT authorship contribution statement
Jingjing Yu: Methodology, Investigation, Data curation, Project administration, Funding acquisition, Writing - original draft. Tian Zhang: Data curation, Formal analysis, Software, Writing - original draft, Writing - review & editing. Dan Zhao: Conceptualization, Methodology, Data curation, Visualization, Formal analysis, Supervision, Writing - original draft. Markus Haapasalo: Writing - review & editing. Ya Shen: Writing - original draft, Supervision, Validation, Writing - review & editing.
Acknowledgments
Supported by grants from the National Natural Science Foundation of China (grant no. 81901000).
The authors deny any conflicts of interest related to this study.
References
- 1.Zhu N., Zhang D., Wang D. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Health Commission of China Update on the epidemic situation of new coronavirus pneumonia as of 24:00 on March 2, 2020. http://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_11809/202003/t20200303_214026.html Available at: Accessed March 3, 2020.
- 3.Mahase E. China coronavirus: WHO declares international emergency as death toll exceeds 200. BMJ. 2020;368:m408. doi: 10.1136/bmj.m408. [DOI] [PubMed] [Google Scholar]
- 4.Meng L.Y., Hua F., Bian Z. Coronavirus disease 2019 (COVID-19): Emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99:481–487. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sohrabi C., Alsafi Z., O'Neill N. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McCarthy P.J., McClanahan S., Hodges J., Bowles W.R. Frequency of localization of the painful tooth by patients presenting for an endodontic emergency. J Endod. 2010;36:801–805. doi: 10.1016/j.joen.2009.12.035. [DOI] [PubMed] [Google Scholar]
- 7.Huang S.M., Huang J.Y., Yu H.C. Trends, demographics, and conditions of emergency dental visits in Taiwan 1997-2013: a nationwide population-based retrospective study. J Formos Med Assoc. 2019;118:582–587. doi: 10.1016/j.jfma.2018.11.012. [DOI] [PubMed] [Google Scholar]
- 8.Glickman G.N. AAE consensus conference on diagnostic terminology: background and perspectives. J Endod. 2009;35:1619–1620. doi: 10.1016/j.joen.2009.09.029. [DOI] [PubMed] [Google Scholar]
- 9.Smales F.C., Samaranyake L.P. Maintaining dental education and specialist dental care during an outbreak of a new coronavirus infection. Part 1: a deadly viral epidemic begins. Br Dent J. 2003;195:557–561. doi: 10.1038/sj.bdj.4810723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim C., Choi E., Park K. Characteristics of patients who visit the dental emergency room in a dental college hospital. J Dent Anesth Pain Med. 2019;19:21. doi: 10.17245/jdapm.2019.19.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Currie C.C., Stone S.J., Connolly J., Durham J. Dental pain in the medical emergency department: a cross-sectional study. J Oral Rehabil. 2017;44:105–111. doi: 10.1111/joor.12462. [DOI] [PubMed] [Google Scholar]
- 12.Huang J., Yu H., Chen Y. Analysis of emergency dental revisits in Taiwan (1999–2012) from Taiwanese national health insurance research database (NHIRD) J Dent Sci. 2019;14:395–400. doi: 10.1016/j.jds.2019.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Quinonez C. Self-reported emergency room visits for dental problems. Int J Dent Hyg. 2011;9:17–20. doi: 10.1111/j.1601-5037.2009.00416.x. [DOI] [PubMed] [Google Scholar]
- 14.Quinonez C., Gibson D., Jokovic A., Locker D. Emergency department visits for dental care of nontraumatic origin. Community Dent Oral Epidemiol. 2009;37:366–371. doi: 10.1111/j.1600-0528.2009.00476.x. [DOI] [PubMed] [Google Scholar]
- 15.Verma S., Chambers I. Dental emergencies presenting to a general hospital emergency department in Hobart, Australia. Aust Dent J. 2014;59:329–333. doi: 10.1111/adj.12202. [DOI] [PubMed] [Google Scholar]
- 16.Chen N., Zhou M., Dong X. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. e201585 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Samaranayake L.P., Peiris M. Severe acute respiratory syndrome and dentistry: A retrospective view. J Am Dent Assoc. 2004;135:1292–1302. doi: 10.14219/jada.archive.2004.0405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sabino-Silva R., Jardim A., Siqueira W.L. Coronavirus COVID-19 impacts to dentistry and potential salivary diagnosis. Clin Oral Investig. 2020;24:1619–1621. doi: 10.1007/s00784-020-03248-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lu B., Huang Y., Huang L. Effect of mucosal and systemic immunization with virus-like particles of severe acute respiratory syndrome coronavirus in mice. Immunology. 2010;130:254–261. doi: 10.1111/j.1365-2567.2010.03231.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu L., Wei Q., Alvarez X. Epithelial cells lining salivary gland ducts are early target cells of severe acute respiratory syndrome coronavirus infection in the upper respiratory tracts of rhesus macaques. J Virol. 2011;85:4025–4030. doi: 10.1128/JVI.02292-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lan L., Xu D., Ye G. Positive RT-PCR test results in patients recovered from COVID-19. JAMA. 2020 doi: 10.1001/jama.2020.2783. e202783 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hasselgren G., Reit C. Emergency pulpotomy: pain relieving effect with and without the use of sedative dressings. J Endod. 1989;15:254–256. doi: 10.1016/S0099-2399(89)80219-5. [DOI] [PubMed] [Google Scholar]
- 25.Taha N.A., Khazali M.A. Partial pulpotomy in mature permanent teeth with clinical signs indicative of irreversible pulpitis: a randomized clinical trial. J Endod. 2017;43:1417–1421. doi: 10.1016/j.joen.2017.03.033. [DOI] [PubMed] [Google Scholar]
- 26.Taha N.A., Ahmad M.B., Ghanim A. Assessment of mineral trioxide aggregate pulpotomy in mature permanent teeth with carious exposures. Int Endod J. 2017;50:117–125. doi: 10.1111/iej.12605. [DOI] [PubMed] [Google Scholar]
- 27.Kundzina R., Stangvaltaite L., Eriksen H.M., Kerosuo E. Capping carious exposures in adults: a randomized controlled trial investigating mineral trioxide aggregate versus calcium hydroxide. Int Endod J. 2017;50:924–932. doi: 10.1111/iej.12719. [DOI] [PubMed] [Google Scholar]
- 28.Fan B., Ye W., Xie E. Three-dimensional morphological analysis of C-shaped canals in mandibular first premolars in a Chinese population. Int Endod J. 2012;45:1035–1041. doi: 10.1111/j.1365-2591.2012.02070.x. [DOI] [PubMed] [Google Scholar]
- 29.Kuzekanani M. Nickel-titanium rotary instruments: development of the single-file systems. J Int Soc Prev Community Dent. 2018;8:386–390. doi: 10.4103/jispcd.JISPCD_225_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ather A., Patel B., Ruparel N.B. Coronavirus disease 19 (COVID-19): implications for clinical dental care. J Endod. 2020;46 doi: 10.1016/j.joen.2020.03.008. S0099-2399(20)30159-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Samaranayake L.P., Reid J., Evans D. The efficacy of rubber dam isolation in reducing atmospheric bacterial contamination. ASDC J Dent Child. 1989;56:442–444. [PubMed] [Google Scholar]
- 32.Qu X., Zhou X. Psychological intervention in oral patients in novel coronavirus pneumonia outbreak period. Chin J Stomatol. 2020;55:E003. [Google Scholar]
- 33.Davidson J.R., McFarlane A.C. The extent and impact of mental health problems after disaster. J Clin Psychiatry. 2006;67(Suppl 2):9–14. [PubMed] [Google Scholar]