Abstract
As coronavirus disease 2019 cases increase throughout the country and health care systems grapple with the need to decrease provider exposure and minimize personal protective equipment use while maintaining high-quality patient care, our specialty is called on to consider new methods of delivering inpatient palliative care (PC). Telepalliative medicine has been used to great effect in outpatient and home-based PC but has had fewer applications in the inpatient setting. As we plan for decreased provider availability because of quarantine and redeployment and seek to reach increasingly isolated hospitalized patients in the face of coronavirus disease 2019, the need for telepalliative medicine in the inpatient setting is now clear. We describe our rapid and ongoing implementation of telepalliative medicine consultation for our inpatient PC teams and discuss lessons learned and recommendations for programs considering similar care models.
Key Words: Inpatient, hospital medicine, telemedicine, telehealth, COVID-19, coronavirus
Identification of Need
In a few short weeks, local, regional, and national conditions changed rapidly. On February 26, the California Department of Public Health reported the first community spread case of coronavirus disease 2019 (COVID-19). The University of California at San Francisco (UCSF) then limited in-hospital personnel to essential providers only. On March 15, UCSF instituted a hospital-wide visitor ban with exceptions for patients at the end of life. Personal protective equipment (PPE) scarcity then prompted calls for minimizing in-person visits by providers. Finally, on March 16, UCSF opened its first closed COVID-19/respiratory illness unit with 31 negative pressure rooms. In the setting of these rapid and unprecedented changes, our inpatient palliative care services (PCS) team recognized that telepalliative medicine consultation would be critical to protect providers, limit PPE use, and provide adequate services to patients throughout the hospital and especially within closed COVID-19 units.
Inpatient Telepalliative Medicine Need in COVID-19 Pandemic
Telepalliative medicine as the remote delivery of PCS has rapidly expanded in recent years largely in outpatient and home-based settings, with the highest increase in video-based services.1 , 2 When used for communication, counseling, and disease monitoring, telemedicine has been associated with reductions in mortality and hospital admissions and improvement in quality of life.3 , 4 Telepalliative medicine expands access to palliative medicine, reaches vulnerable patients, and allows for unique forms of relationship building.5 With the emergency expansion of telehealth reimbursement by the Centers for Medicare and Medicaid Services, telemedicine is also now increasingly financially feasible.6
In this global COVID-19 pandemic, we expect a surge in need for symptom management, early goals-of-care conversations, and care at the end of life. We already observed increased psychosocial, spiritual, and existential suffering. Anxiety and hopelessness are exacerbated by the social isolation of hospitalized patients. Goals-of-care conversations will be imperative as part of a strategy to avoid painful resource allocation decisions, and restrictions on visitors make family meetings impossible without the use of technology. Moral distress, trauma, and helplessness for providers will be elevated in caring for isolated ill and dying patients. These diverse needs will fast outstrip the current inpatient palliative care (PC) workforce, especially if providers are limited by personal illness or if team members are reassigned to help in other areas.
Implementation
Given the expected increased need for palliative medicine and hospital mandates to limit PPE use and provider exposure, we rapidly moved to implement an inpatient telepalliative medicine program. During the past two years, we implemented a pilot using iPads to allow outpatient PC clinicians to conduct video visits with their patients while hospitalized to promote continuity. This experience demonstrated that inpatient video visits are feasible and beneficial.
At UCSF, the inpatient PCS team is composed of three teams at two hospitals, with 11 attending physicians (one per team), 2.5 social workers, a registered nurse, and a chaplain. We decided that consultations by all PCS team members for patients with confirmed or suspected COVID-19 would be done via telemedicine and encouraged remote visits for other patients requiring PPE to limit exposure and reduce PPE use. We launched three forms of remote interventions for patients in the inpatient setting: chart-based e-consult for symptom management recommendations, telephone consultation, and video consultation.
We created shareable templates and dot phrase attestations in the electronic health record (EPIC) for providers to document these visits and to mark note types for billing (Appendix). The Stupski Foundation donated 10 iPads, cases, and trackers. An electronic sign-out sheet tracks iPads and scheduled meetings.
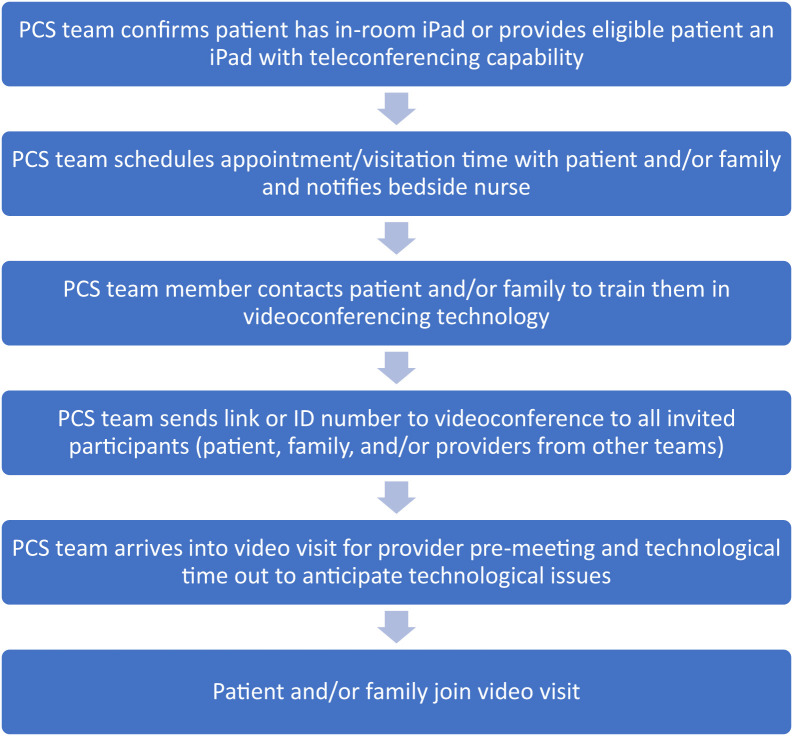
We worked with nursing and hospital medicine leadership involved in launching the closed COVID-19 unit, outfitted with iPads and cameras in every room, to design workflows to reach patients via telepalliative video visits (Fig. 1 ).
Fig. 1.
Example workflow for inpatient telepalliative consultation. PCS = palliative care services.
Zoom videoconferencing software is the video platform of choice at UCSF based on security and accessibility. However, with the recent liberalization of Health Insurance Portability and Accountability Act compliance guidelines by the U.S. Department of Health and Human Services, other options can be considered. Providers initiate videoconferencing sessions from their work computers or phones in the hospital or at home.
Technological Considerations
Programs should consider the following technological concerns as part of implementation. Quality Wi-Fi and/or cell phone reception and clear audio is key. Studies have shown that technological issues with video result in decreased engagement and patient satisfaction and harm rapport building.7 Videoconferencing technology should ideally integrate with interpreter services, which may be audio only. It is helpful to create or repurpose educational materials (many already exist for the outpatient setting) to introduce patients to videoconferencing and how/when palliative providers might contact them remotely. Many patients have personal smart phones/devices, and these can be leveraged when hospital-provided technology is not available. Finally, videoconferencing can be used both for fully remote consultation as well as by in-person providers to include remote team members or family members.
Lessons Learned
Interacting with patients and families via videoconferencing is fundamentally different from in-person consultation. In palliative medicine, we rely heavily on nonverbal cues to guide us in redirecting conversations and responding to emotions. Many of the techniques we turn to, including touch and even the act of sitting down with a patient, are not available to us via telemedicine. Some consults will still require in-person consultation, for example, when patients are hard of hearing, unable to use technology, or require physical examination. However, in most cases, PC providers can apply their skills of listening, perceiving, and connecting via video. Telepalliative skills are novel and take time to develop. And yet, telemedicine is a powerful tool that can promote good communication and high-quality care.
Providers may express grief at being separated from patients and team members. Health care providers have a known tendency toward pathological altruism, especially in humanitarian crises, and can experience guilt around not being part of the frontline team in the hospital.8 Teams should reframe and emphasize the need for all providers to work to redesign our health care delivery system and imagine new ways of providing care, not only for this crisis but also for the future as well. Preventing provider illness enables individuals to continue to provide care and preserves our most precious resource: the limited palliative medicine workforce. Moreover, remote consultation decreases PPE use and ensures that first responders and bedside providers are protected for the duration of this crisis. It is helpful to acknowledge these emotions and address them in teams openly, ensuring that providers working in all settings are respected and no role is treated as more or less heroic.
Apart from the emotional challenge around working remotely from home, there are functional struggles. Working at home can be distracting, especially if many family members are at home sheltering in place. Homes are not always functionally or ergonomically set up to perform remote clinical visitation. It can be difficult to maintain work-life separation, and providers may find identities and schedules bleeding into each other. Teams should be kind to one another amid this new chaos of life. We are working to practice humility and patience with ourselves and our team members as we practice in a new way.
Policy changes and workflow innovations should be established with the expertise of all palliative disciplines. It is helpful to reassure individuals that emergent variations to work flow are fluid and do not necessarily reflect permanent changes. Ensuring continued interdisciplinary collaboration will maintain holistic policies and, ultimately, optimal care for patients and families.
Workflows for videoconferencing should be designed to minimize nursing burden, given the many demands on their time. Programs can consider identifying PC team members to schedule visits and remotely train patients and families to videoconference. It is helpful to leverage the wisdom and advice of outpatient teams experienced with videoconferencing.5 , 9
Rapid implementation of technology relies on robust health infrastructure support. Health systems should empower teams with technology and flexibility and emphasize that while piloting new interventions, billing may be suspended as a top priority. Lifting limitations and empowering providers leads to novel and previously unimagined ideas.
Conclusions
In this unprecedented time, we have a unique opportunity to redesign the way we provide care. For example, UCSF is currently embarking on ways to equip rooms with video capability connected to hospital room phones, allowing providers to call in and ring patient iPads to immediately and automatically activate their videoconferencing to perform visits. This type of intervention has the potential to revolutionize inpatient medicine. The great hope for our field is that we emerge from this crisis as leaders not only in humanistic patient care but also as leaders in our health systems and experts in novel technology to deliver quality care.
With our national move toward social distancing, we reframe that idea to highlight that despite physically distancing, we can still socially connect. This is especially critical for our patients with COVID-19, who are isolated in hospital rooms, unable to see or touch loved ones, and rarely interact with health care providers covered in PPE. Telepalliative medicine provides the opportunity—particularly by video—to connect to patients, connect them to others, and provide as intimate and interdisciplinary support as possible in these times.
Disclosures and Acknowledgments
The authors are grateful to the Stupski Foundation for the donation of iPads. The authors declare no conflicts of interest.
Appendix. PC Telemedicine ConsultNote
My date of service is ∗∗∗
Consult requested by Dr. ∗∗∗ of the ∗∗∗ service.
Reasons given by referring provider for initial PC consult (check all that apply): ∗∗∗
Primary diagnosis leading to PC consult (check one): ∗∗∗
Surrogate decision maker: ∗∗∗
History of PresentIllness
∗∗∗
SymptomScores
Pain: none/mild/moderate/severe/not assessed
Anxiety: none/mild/moderate/severe/not assessed
Nausea: none/mild/moderate/severe/not assessed
Dyspnea: none/mild/moderate/severe/not assessed
Pain
-
1.
Pain character: ∗∗∗
-
2.
Pain duration: ∗∗∗
-
3.
Pain effect: ∗∗∗
-
4.
Pain factors: ∗∗∗
-
5.
Pain frequency: ∗∗∗
-
6.
Pain location: ∗∗∗
Palliative Performance Scale at time of consult: ∗∗∗
Screening and interventions (check all that apply):
Screening: pain/nonpain symptom/psychosocial/spiritual/goals of care
Intervened: pain/nonpain symptom/psychosocial/spiritual/goals of care
Spiritual screen: ∗∗∗
Vitals
Vital signs
Inputs/outputs
Telemedicine Physical Examination
Via Video Observation:
Constitutional: Patient is oriented to person, place, and time. Patient appears well developed and well nourished.
Head: normocephalic and atraumatic.
Pulmonary/chest: respiratory effort normal.
Psychiatric: Normal mood and affect. Behavior is normal. Judgment and thought content is normal.
Data
I spoke with ∗∗∗ from ∗∗∗ team regarding ∗∗∗.
Assessment and Recommendations
Mr. N is a ∗∗∗
#Problem list
Outpatient PCS: (Please place a discharge referral to ∗∗∗/already followed by ∗∗∗)
A family meeting was held today: yes/no.
Other interventions: advance directive/POLST/code status clarified/∗∗∗
Code status: ∗∗∗
Counseling/coordination of care
I provided guidance for the patient and/or family and/or medical team: ∗∗∗
Telemedicine Visit
I performed this consultation using real-time Telehealth tools, including a live video connection between my location and the patient's location. Before initiating the consultation, I obtained informed verbal consent to perform this consultation using Telehealth tools and answered all the questions about the Telehealth interaction.
Dr. ∗∗∗
Date
References
- 1.Maguire R., Fox P.A., McCann L. The eSMART study protocol: a randomised controlled trial to evaluate electronic symptom management using the advanced symptom management system (ASyMS) remote technology for patients with cancer. BMJ Open. 2017;7:e015016. doi: 10.1136/bmjopen-2016-015016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Read Paul L., Salmon C., Sinnarajah A., Spice R. Web-based videoconferencing for rural palliative care consultation with elderly patients at home. Support Care Cancer. 2019;27:3321–3330. doi: 10.1007/s00520-018-4580-8. [DOI] [PubMed] [Google Scholar]
- 3.Worster B., Swartz K. Telemedicine and palliative care: an increasing role in supportive oncology. Curr Oncol Rep. 2017;19:37. doi: 10.1007/s11912-017-0600-y. [DOI] [PubMed] [Google Scholar]
- 4.Totten A.M., Womack D.M., Eden K.B. Agency for Healthcare Research and Quality (US); Rockville, MD: 2016. Telehealth: Mapping the evidence for patient outcomes from systematic reviews. [PubMed] [Google Scholar]
- 5.Calton B.A., Rabow M.W., Branagan L. Top ten tips palliative care clinicians should know about telepalliative care. J Palliat Med. 2019;22:981–985. doi: 10.1089/jpm.2019.0278. [DOI] [PubMed] [Google Scholar]
- 6.Medicare telemedicine health care provider FACT sheet|CMS. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet Available from.
- 7.Henry B.W., Block D.E., Ciesla J.R., McGowan B.A., Vozenilek J.A. Clinician behaviors in telehealth care delivery: a systematic review. Adv Health Sci Educ Theor Pract. 2017;22:869–888. doi: 10.1007/s10459-016-9717-2. [DOI] [PubMed] [Google Scholar]
- 8.Oakley B.A., editor. Pathological altruism. Oxford University Press; Oxford; New York: 2012. [Google Scholar]
- 9.Wootton A.R., McCuistian C., Legnitto Packard D.A., Gruber V.A., Saberi P. Overcoming Technological Challenges: Lessons Learned from a Telehealth Counseling Study. Telemed J E Health. 2019 doi: 10.1089/tmj.2019.0191. [DOI] [PubMed] [Google Scholar]