Editor—Since December 2019, a pandemic infection caused by a novel coronavirus responsible for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been spreading globally after the first respiratory cases appeared in Wuhan, Hubei Province, China.1 In March 2020, Western Europe and France faced a huge number of SARS-CoV-2 cases. The clinical management of the most severe cases requires tracheal intubation with mechanical ventilation. In order to protect against viral transmission, airway management requires several precautions. Therefore, anticipation of difficult airway management to limit the number of attempts and procedures is recommended.
We have had two recent patients with SARS-CoV-2 infection who had airway trauma during tracheal intubation (written consent was obtained from the patients before reporting these cases).
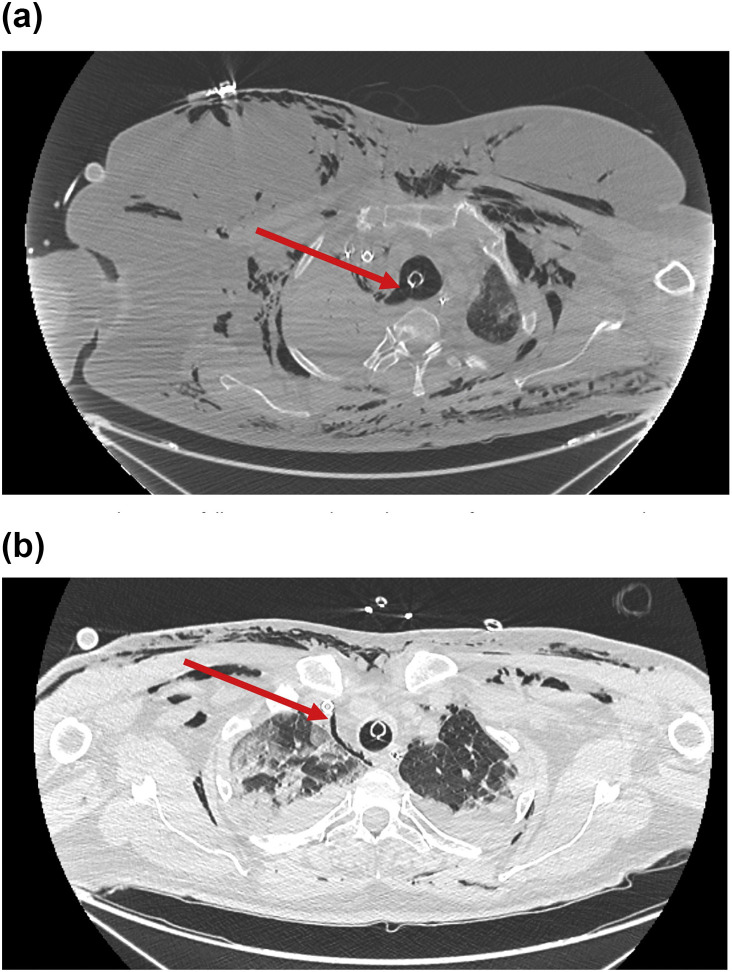
The first case is a 59 yr old woman with a history of morbid obesity (BMI, 41 kg m−2) who was admitted to a tertiary hospital for acute dyspnoea, myalgia, and arthralgia. Initial physical examination revealed the following: heart rate, 90 beats min−1; arterial blood pressure, 120/70 mm Hg; tachypnoea, 30 min−1; fever of 39.2°C; oxygen saturation, 80%; and bilateral dry rales on lung auscultation. Biological investigation showed a white blood count of 8400 mm−3, lymphopaenia of 800 mm−3, and C reactive protein of 230 ng L−1. Blood gas analysis confirmed severe hypoxaemia with a Pao 2 of 7 kPa and respiratory alkalosis (pH 7.5, HCO3 – 24.8 mM, Paco 2 18 kPa). Chest CT was compatible with SARS-CoV-2 infection as it showed bilateral ground-glass like opacities and multiple patchy lung consolidations.2 Real-time reverse transcriptase–polymerase chain reaction (RT–PCR) of nasopharyngeal swabs was positive for SARS-CoV-2. The initial medical management consisted of high-flow nasal cannula (HFNC) oxygen therapy (100% oxygen) and administration of lopinavir and ritonavir. On Day 2 after admission, the patient's respiratory condition worsened requiring tracheal intubation and mechanical ventilation. Direct laryngoscopy showed a Grade IV view requiring use of a single bougie (Eschmann introducer, Vygon 15 Fr, Vygon, Écouen, France) without successful intubation. Cervical and thoracic subcutaneous emphysema occurred just after the first attempt during face mask ventilation. The trachea was intubated on the second attempt using another bougie. Mechanical ventilation was then performed with low tidal volume and high positive end expiratory pressure without loss in tidal volume. However, during the first night after intubation, the patient presented with refractory hypoxaemia (Pao 2/Fio 2 at 50) requiring extracorporeal membrane oxygenation (ECMO) and transfer to our tertiary hospital centre. Chest CT scan confirmed a large pneumomediastinum and a right-sided pneumothorax (Fig 1 a). Fibreoptic bronchoscopy confirmed a large perforation of the membranous trachea. As the pneumomediastinum persisted with difficulty in ventilating the patient, she went for surgical tracheal repair with tracheal suture by right thoracotomy, followed by protective ventilation for severe acute respiratory distress syndrome (ARDS) under ECMO.
Fig 1.
Chest CT scan of two patients with coronavirus disease 2019 (COVID-19) showing pneumomediastinum, subcutaneous emphysema, and pneumothorax. (a) Pneumomediastinum following tracheal trauma. The continuum between the trachea and the mediastinum is represented by a red arrow. (b) Pneumomediastinum after cricoid membrane perforation. Pneumomediastinum is represented by a red arrow.
The second case was a 67 yr old man with a medical history of severe obesity (BMI, 34 kg m−2) who was admitted on March 19, 2020 for dyspnoea and myalgia with onset of symptoms 12 days before admission. Results of his physical examination showed bilateral dry rales on lung auscultation, eupnoea, without signs of acute respiratory failure. Chest CT was compatible with SARS-CoV-2 infection with bilateral ground-glass like opacities, patchy lesions, and an extension of lesions exceeding 50%.2 Initial blood gas analysis showed normoxaemia with a Pao 2 of 19 kPa (oxygen by mask at 6 L min−1), HCO3 – of 26.5 mM, Paco 2 of 4 kPa, and pH 7.4. RT–PCR of nasopharyngeal swabs was positive for SARS-CoV-2. On Day 3 after admission, the patient worsened with acute respiratory failure and oxygen desaturation to 90% with oxygen by mask (9 L min−1). To provide mechanical ventilation and correct hypoxaemia, tracheal intubation was attempted. The first attempt showed a Grade IV view on laryngoscopy requiring use of a bougie (Eschmann introducer, Vygon 15Fr, Vygon) and was unsuccessful. On the second attempt, successful tracheal intubation was performed using videolaryngoscopy (Airtraq®; Prodol Meditec, Guecho, Spain). As the patient presented criteria of severe ARDS according to the Berlin classification,3 and required protective ventilation with high PEEP (13 cm H2O, 6 ml kg−1 of ideal body weight) and high inspired oxygen fraction (100%). Despite early prone positioning, the patient developed refractory hypoxaemia and respiratory acidosis (pH 7.22) requiring veno-venous femoro-jugular ECMO and was transferred to our tertiary hospital centre. Chest CT confirmed pneumomediastinum and bilateral pneumothorax (Fig 1b). Fibreoptic bronchoscopy confirmed perforation of the cricoid membrane. Ventilation was possible without cutaneous emphysema or tidal volume loss.
Both patients had severe obesity with a typical presentation of SARS-CoV-2 infection, and required invasive ventilation after failing noninvasive oxygen therapy. Both rapidly evolved as a severe ARDS refractory to prone positioning, and both met criteria for difficult tracheal intubation owing to severe obesity. Protocols for managing severe ARDS4 and guidelines for protection of healthcare personnel during aerosol-generating procedures5 needed to be taken into account. In both cases, use of a bougie probably induced tracheal trauma thereby worsening the respiratory condition and leading to urgent ECMO. The absence of glottis visibility in both patients might enhance the risk of tracheal trauma forcing intubation with a bougie.6 Videolaryngoscopy is recommended not only for healthcare personnel protection but also to allow successful intubation at first attempt thus avoiding potential tracheal trauma and worsening respiratory failure.
Declarations of interest
The authors declare that they have no conflicts of interest.
References
- 1.del Rio C., Malani P.N. COVID-19—new insights on a rapidly changing epidemic. JAMA [Internet] 2020 doi: 10.1001/jama.2020.3072. https://jamanetwork.com/journals/jama/fullarticle/2762510 [cited 2020 Mar 27]; Available from: [DOI] [PubMed] [Google Scholar]
- 2.Chung M., Bernheim A., Mei X. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020;295:202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Acute respiratory distress syndrome: the Berlin definition. JAMA [Internet] 2012;307 doi: 10.1001/jama.2012.5669. [cited 2019 Nov 10]; Available from: http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 4.Higgs A., McGrath B.A., Goddard C. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth. 2018;120:323–352. doi: 10.1016/j.bja.2017.10.021. [DOI] [PubMed] [Google Scholar]
- 5.Peng P.W.H., Ho P.-L., Hota S.S. Outbreak of a new coronavirus: what anaesthetists should know. Br J Anaesth. 2020;124:497–501. doi: 10.1016/j.bja.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marson B.A., Anderson E., Wilkes A.R., Hodzovic I. Bougie-related airway trauma: dangers of the hold-up sign. Anaesthesia. 2014;69:219–223. doi: 10.1111/anae.12534. [DOI] [PubMed] [Google Scholar]