Highlights
-
•
Thoracic anesthesiologists might be involved in the perioperative care of patients suspected to have or diagnosed COVID-19 who might undergo thoracic surgery during the acute or convalescence phases of the disease.
-
•
Caution should be exercised when securing the airway and performing lung separation (if required), through vigilant donning/doffing of personal protection equipment (PPE), planning ahead, team briefing, proper preparations, systematic approach, and debriefing.
-
•
Lung separation/isolation should be individualized using either bronchial blockers or double lumen tubes according to the patient's status and perioperative care plan.
-
•
Optimal PPE donning should be maintained during surgery and anesthesia. One lung ventilation could be challenging in this group of patients.
-
•
The anesthesiologists should discuss the feasibility of extubating the patient following thoracic surgery, and procedures for postoperative care and transferring the patient to the isolation wards or intensive care unit.
Key Words: thoracic anesthesia, lung separation, personal protective equipment, coronavirus, COVID-19
Abstract
The novel coronavirus has caused a pandemic around the world. Management of patients with suspected or confirmed coronavirus infection who have to undergo thoracic surgery will be a challenge for the anesthesiologists. The thoracic subspecialty committee of European Association of Cardiothoracic Anaesthesiology (EACTA) has conducted a survey of opinion in order to create recommendations for the anesthetic approach to these challenging patients. It should be emphasized that both the management of the infected patient with COVID-19 and the self-protection of the anesthesia team constitute a complicated challenge. The text focuses therefore on both important topics.
In December 2019, a novel, ongoing outbreak of pneumonia was reported in Wuhan, Hubei province, China. A novel coronavirus was found to be responsible for the outbreak in patients from Wuhan and subsequently was named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The disease caused by SARS-CoV-2 is known as coronavirus disease 2019 (COVID-2019). Although primarily a zoonotic infection, COVID-2019 now is known to spread from person to person, and both asymptomatic and symptomatic carriers play a role. In a very short time, COVID-2019 became an international outbreak, and on March 11, 2020, the World Health Organization declared it a “pandemic.”
The most common symptoms of COVID-2019 are dry cough, fever, and shortness of breath that lead to respiratory failure in about 5% of cases. Age and comorbidities are risk factors; older and immunocompromised patients and patients with diseases such as hypertension, diabetes mellitus, and cancer have a higher mortality.
Viral particles entering the lungs via droplets propagated through sneezing, coughing, and even talking to the infected are responsible for the spread of the disease. In patients undergoing procedures such as intubation, extubation, and airway suctioning or even receiving treatment with some types of noninvasive ventilation, aerosols (containing droplets with a diameter <5 µm) that more easily reach small airways may be propagated. Other routes of spread, such as direct contact with the infected, also are possible.
As of March 25, 2020, there were 428,405 confirmed cases of COVID-19 and 19,273 deaths in 195 countries around the world.
General Airway Management and Ventilation of COVID-19 Patients
Patients with COVID-2019 present with a spectrum of respiratory distress ranging from dyspnea and hypoxia to acute respiratory distress syndrome and may require respiratory support in different locations such as the emergency room, isolation ward, and intensive care units (ICUs). A significant portion of these patients require early mechanical ventilation involving urgent or emergency tracheal intubation. In addition, with the pandemic nature of the current outbreak, patients with mild or asymptomatic disease still may present for urgent or emergency, general, or specialized surgery.
Recognizing the unique risks of intubation and mechanical ventilation in these high-risk groups and the great potential of infection risk to health care workers, several useful reports, algorithms, and society-endorsed recommendations have emerged in the recent literature regarding general airway and anesthesia management of these patients. These societies include the Società Italiana di Anestesia Analgesia Rianimazione e Terapia Intensiva, World Federation of Societies of Anaesthesiologists, and Anesthesia Patients Safety Foundation; UK societies (eg, Faculty of Intensive Care Medicine, Intensive Care Society, Association of Anaesthestists, and Royal College of Anaesthetists); Consensus Statement of the Australian Societies; Société Française d'Anesthésie et Réanimation; Canadian Society of Anesthesiologists; Task Force of the Chinese Society of Anesthesiology; and the Chinese Association of Anesthesiologists.1, 2, 3, 4, 5, 6, 7, 8, 9 Most recommendations are in the context of intensive care management or the surgical setting, including emergency surgical cases, and for procedures for specific disciplines, such as Cesarean delivery (in 17 cases).10
Thoracic Surgery and Anesthesia in the COVID-19 Era
The novel coronavirus pandemic has changed the landscape of normal surgical practice radically, with most elective surgeries being postponed. Lifesaving cancer surgery, however, remains a clinical priority, and there is an increasing need to fully define the optimal oncological management of patients with varying stages of lung cancer, allowing for the prioritization of which urgent and emergency thoracic procedures should be performed in the current era. Management of general anesthesia, particularly airway management, ventilation, and perioperative care, of these patients constitutes an additional and important challenge for the anesthesiologist.
The European Association of Cardiothoracic Anaesthesiology's Thoracic Anesthesia Subspecialty Committee considered these challenges and developed a preliminary set of expert recommendations regarding airway management and ventilation of COVID-19 thoracic surgery patients. The consensus builds on previous society recommendations on general airway management principles but expands those recommendations by specifically focusing on unique aspects of thoracic anesthesia.
Methods
The principal methodologies underpinning the recommendations include expert opinions through broad discussions reviewing clinical experience of routine thoracic surgery in similar cases during the Middle East respiratory syndrome outbreak and during the current pandemic with suspected COVID-19 patients. Methodologies also include literature searching and a limited survey of members of the subcommittee.
Literature Search
The literature was searched for direct and indirect evidence on the management of COVID-19, severe acute respiratory syndrome, Middle East respiratory syndrome, and H1N1 patients. Major databases were searched electronically (eg, MEDLINE and Google) to identify recent consensus recommendations, guidelines, relevant systematic reviews, randomized controlled trials, observational studies, and case series. These electronic searches were performed to seek out studies published in English from inception of the databases to March 23, 2020. To develop recommendations on airway management and lung separation, recently published articles were used and the expert panel was asked to identify any novel relevant studies.
Opinion Survey
The survey was sent to 28 members of the European Association of Cardiothoracic Anaesthesiology's Thoracic Network via WhatsApp and Facebook. Twenty-one responses (75%) were received after 2 reminders were sent. The responses were evaluated in light of recent publications of the different previously mentioned societies and groups.
Recommendation Formulation
The group considered a broad spectrum of issues regarding thoracic anesthesia in COVID-19 patients and decided to focus on overall approaches to general and specific aspects of airway management, preparation for anesthesia, lung isolation/separation, and ventilation.
To arrive at consensus recommendations, the principles outlined in the reviewed publications were combined with expert opinions from members of the subspecialty committee. The recommendations take into consideration the balance between benefit and harm, safety concerns, and feasibility in specific environments.
The committee's goal was to make this preliminary consensus rapidly available to all thoracic teams, and the authors acknowledge limitations of the adopted methodology. The present document should be the basis of future work to develop a more comprehensive and perhaps multisociety consensus taking new evidence uncovered during the COVID-19 epidemic into appropriate consideration.
Recommendations
General Considerations and Principles
Table 1 summarizes the recommendations regarding general aspects of airway management. The recommendations provide a comprehensive framework with a major emphasis on efficient team efforts to achieve successful airway control and establish controlled ventilation without compromising the high-risk patient while providing maximal protection to the health care team. It appears that most of the recommendations considering vigilant infection control and the required organizational tasks and technical conduct of intubation are fairly consistent among the societies.
Table 1.
Comparisons Among Different Societies’ General Recommendations on Airway Management
| Management | United Kingdom | SIAARTI | WFSA | APSF | Canada | Australia | China |
|---|---|---|---|---|---|---|---|
| Team safety | |||||||
| Tracheal intubation is a high-risk aerosol generating procedures | + | + | + | + | + | + | + |
| Prefer elective tracheal intubation | + | + | + | + | + | + | |
| Recommendation for PPE | + | + | + | + | + | + | |
| Hair cover | + | + | + | + | + | + | + |
| Hood | + / cover | + / cover | |||||
| N95 or FFP2 | + | + | + | + | + | + | |
| FFP3 | + | 3rd level | |||||
| Goggles/eye wear | + | + | + | + | + | + | |
| Face shield | + | + | + | + | + | ||
| Shoe cover | + | + | + | + | |||
| Double gloving | + | + | + | + | + | + | + |
| Long-sleeve, waterproof gown | Plastic apron | + | + | + | + | + | |
| HEPA or HME filters | + | + | + | + | + | + | + |
| Organization aspects, team communication | |||||||
| An isolated negative pressure room, if available | + | + | + | + | + | + | + |
| Limit staff present at tracheal intubation | + | + | + | + | + | + | |
| Consider excluding staff vulnerable to infection from the team | + | ||||||
| Effective communication | + | + | + | + | + | + | |
| Developed checklist | + | + | |||||
| Intubation with SAS principles | |||||||
| A dedicated airway cart should be available | + | + | + | + | + | ||
| Preoxygenation | |||||||
| 3-5 min | + | ||||||
| 5 min | + | + | + | + | + | + | |
| Apnea | + | + | + | + | |||
| Tidal volume or FVC | + | + | |||||
| Avoid BM ventilation if possible | + | + | + | + | + | + | |
| RSI | + | + | + | + | + | + | + |
| Avoid cricoid pressure | ? | + | - | ||||
| Ensure full neuromuscular blockade | + | + | + | + | + | + | + |
| Video laryngoscopy | + | + | + | + | + | + | + |
| Limit awake intubation | + | + | + | + | + | ||
| Avoid topicalization | + | + | |||||
Abbreviations: APSF, Anesthesia Patients Safety Foundation; BM, Bag-mask; FFP, Filtering facepiece; FVC, Forced vital capacity; HEPA, high-efficiency particulate air; HME, Heat and Moisture Exchangers; PPE, personal protective equipment; RSI, rapid sequence induction; SAS, mnemonic for the procedure “S”afe (for staff and patient), “A”ccurate (avoiding unreliable, unfamiliar, or repeated techniques), and “S”wift (timely, without rush and delay); SIARRTI, Società Italiana di Anestesia Analgesia Rianimazione e Terapia Intensiva; WFSA, World Federation of Societies of Anaesthesiologists.
The authors of the present article recognize that many of the recommendations are relevant to thoracic patients, and they generally endorse the conclusions with some modifications as follows.
Tracheal Intubation in COVID-19 Patients for Thoracic Surgery
-
•
Tracheal intubation for thoracic surgery in COVID-19 patients is a high-risk procedure for the anesthesia team because of the risks of aerosol transmission of the infection during placement of the airway device and bronchoscopic check. It also is a risk for patients with severe COVID-19 who would not tolerate long periods of apnea or inadequate oxygenation in case of delayed or failed tracheal intubation.
-
•
The procedure should be safe (for staff and patient), accurate (avoiding unreliable, unfamiliar, or repeated techniques), and swift (timely, without rush and delay). (Mnemonic: SAS).4
-
•
As asymptomatic patients may also have the viral infection during the pandemic, with potential contagiousity, and false negative tests cannot be excluded with certainty, it is prudent that the team takes a cautious approach and considers every patient undergoing surgery as potentially positive for infection. These considerations require specific protective measures and sophisticated organization and team practices.
-
•
An elective intubation should be postponed if possible because emergency intubation may compromise protective procedures and could increase the patient's risk.
-
•Ideally, the location of intubation should be an “isolated” negative pressure room with >12 air changes/min. However, there are few operating rooms (ORs) with negative pressure facilities; these are more commonly available in ICUs. If a negative pressure OR is not available, the following measures may be considered:
-
○The level of personal protection equipment (PPE) should be increased (eg, respirators in place of masks, face shield or helmet).
-
○Alternatively, intubation can be performed in a negative pressure room followed by transfer to the OR, such as in an isolated ward or ICU. The benefits of such an approach, however, need to be judged against its disadvantages and possible complications.
-
○In rooms with positive pressure, the room can be put under the least possible positive pressure and the remainder of the unit under higher positive pressure, and the doors should be kept closed so that the high exchange rate of air in the room limits dispersion of aerosols outside the room despite the positive pressure.
-
○
Medical staff involved in tracheal intubation should be limited to those with essential roles. Because of the high risk of infection, it is suggested that members of the intubating team should not include practitioners with significant vulnerability (eg, older age [>60 y], immunosuppressed, pregnant, or serious chronic comorbidities).
Inside the room, 2 attendants must be in the “red zone.” Intubation should be performed by the most experienced physician to minimize delay or related complications, and a second doctor should help administer drugs and monitor the patient in case of unanticipated difficulty. The authors note that many other societies suggest 3 attendants (with full donning) in the red zone; however, in this period of the pandemic, this criterion probably is not possible to achieve.
There must a “runner” physician available directly outside the room in the “yellow zone” with full donned PPE, in case of need for help.
Outside the dedicated OR “white zone,” an observer must be present to monitor the “donning/doffing” process of the PPE.
The surgical, anesthesia, nursing, and paramedical staff who are not involved with airway management should not enter the OR until after the airway has been secured.
Several levels of PPE have been defined for different procedures by different societies. Intubation and bronchoscopy are among the “aerosol-generating” procedures and are associated with increased infection risk. During intubation in thoracic anesthesia, it is suggested to work with so-called “airborne level” precautions, which include the following components of appropriate PPE:
-
•
Hair covers/hoods
-
•
Fitted filtering facepiece 3 or N95 or fitted filtering facepiece 2 masks
-
•
Goggles or face shield
-
•
Long sleeve fluid-resistant gown
-
•
Double gloves
-
•
Overshoes
Preparation
Maintaining the sequence for donning and doffing PPE (Table 2 ) is very important to avoid any contact with the contagion. This process can be challenging especially for attendants with less experience and therefore requires thorough training, practice, and constant monitoring during the actual procedures by an external observer.
Table 2.
Donning and Doffing of Personal Protective Equipment
| Donning PPE | B. Doffing PPE |
|---|---|
| Hand hygiene | Remove shoe covers |
| Inner gloves | Remove gown |
| Hand hygiene | Remove outer glove |
| Hair covers/hood | Hand hygiene |
| Shoe covers | Remove eye protection |
| Gown | Remove mask |
| Mask fit check | Remove hair covers/hood |
| Eye protection: fit check again | Remove inner glove |
| Hand hygiene + Outer glove | Hand hygiene |
Abbreviation: PPE, personal protective equipment.
-
•
Trolley: It is recommended to prepare a dedicated trolley for tracheal intubation of this special group of patients (Table 3 shows possible contents). Disposable devices (eg, single-use blades, laryngoscopes, video laryngoscopes with remote screens, and flexible bronchoscopes) should be included. A closed system for suction should be kept ready. Antifogging material is required. Specific equipment for thoracic surgery (eg, appropriate sizes of double-lumen tubes [DLTs], bronchial blockers [BBs], and fiberoptic bronchoscopes) also should be ready and prepared.
-
•
Before intubation, a complete evaluation and optimization of the patient's position (45-degree, head-up, sniffing position), oxygenation, and hemodynamic status should be performed using a developed checklist.
-
•
Standard routine monitoring, including continuous waveform capnography, should be available before, during, and after tracheal intubation.
-
•
The breathing circuit should be checked as per normal routine. The authors suggest that antiviral filters should be attached to the expiratory limb of the circuit.
Table 3.
Contents of the Intubation Trolley
| Item | Checkboxes |
|---|---|
| PPE × 4 (these are only for anesthesia team) | □ |
| Drugs | □ |
| Video laryngoscope trolley with screen | □ |
| Video laryngoscope blades (preferably disposable) (1 of each size—3.4 and Difficult) | □ |
| Disposable Mapleson C breathing circuit | □ |
| Standard endotracheal tube in appropriate sizes (3 sizes around the expected size) | □ |
| Intubatable supraglottic airway device | □ |
| DLTs (if not otherwise indicated: left-sided; in 2 sizes appropriate for the patient) | □ |
| Bronchial blocker (according to the policies of the clinic) | □ |
| Bougie (1 pc) | □ |
| Airway exchange catheters (different sizes) | □ |
| Airways in appropriate sizes | □ |
| Sealing face mask in appropriate sizes | □ |
| Antiviral filters connected to each interface (mask with Y connection, expiration limb, and ETT or DLT) | □ |
| Two capnography sampling lines | □ |
| Adhesive plaster for ETT fixation | □ |
| Adult Magill forceps | □ |
| Swivel connector, 15 mm (with valve) | □ |
| Stylets | □ |
| Front of Neck kit (preferably scalpel-bougie-tube technique) | □ |
| Water-soluble gel lubricant | □ |
| Disposable self-inflating resuscitation bag with an antiviral filter | □ |
NOTE. The trolley is prepared for the anesthesia team only; all disposable equipment should be discarded after the surgery, even if not used; and to avoid unnecessary waste, the trolley should be prepared for each specific case and the anticipated plan.
Abbreviations: DLT, double-lumen tube; ETT, endotracheal tube; HEPA, high-efficiency particulate air; PPE, personal protective equipment.
Preoxygenation
-
•
Appropriate preoxygenation is crucial because it can prevent or decrease the need for mask ventilation before securing the airway.
-
•
Preoxygenation should be performed using a well-fitting face mask and a Mapleson C (“Waters”) or anesthetic circuit. Patients would take 8 deep breaths at forced vital capacity (amount of air that can be forcibly exhaled from your lungs after taking the deepest breath possible) for one minute, or with continuous positive airway pressure (CPAP)/pressure support ventilation of 10 cmH2O and positive end-expiratory pressure (PEEP) of 5 cmH2O for 3 to 5 minutes.
-
•
Face mask ventilation should be avoided unless needed. If necessary, a 2-person, low-flow, low pressure technique should be used; 2-person, 2-handed mask ventilation with a VE grip should be performed to improve seal.
Induction
-
•
A “rapid sequence induction” should be performed in all patients.
-
•
Ketamine 1.5 to 2 mg/kg or appropriate doses of propofol and an opioid are recommended for hypnosis and analgesia (rocuronium 1.2 mg/kg or suxamethonium 1.5 mg/kg for neuromuscular blockade).
Intubation
-
•
Intubation should be performed using video laryngoscopy, preferably via a laryngoscope with a single-use blade if applicable and separate remote screen. The latter would extend the distance between the airway of the patient and the anesthesiologist to minimize or avoid “airborne spread.”
-
•The pathway for an unanticipated difficult airway in thoracic surgery is similar to that of general airway management (Fig 1 , A):
-
○The first laryngoscopy should be performed with an endotracheal tube (ETT) preloaded on an introducer.
-
○If the first attempt fails, a reoxygenation period may be needed, which should be performed with a low tidal volume/pressure to avoid leakage of contaminated air.
-
○If a third attempt is necessary, an early switch to a second-generation intubatable supraglottic airway device should be considered. Intubation through this device should be performed with a flexible (preferably disposable) endoscope, again with a separate remote screen.
-
○
-
•
The ETT cuff or the cuff of the tracheal lumen of the DLT should be inflated to seal the airway before starting ventilation, and the depth should be noted and recorded. The cuff pressure should be kept at least 5 to 10 cmH2O above the maximum airway pressure using an inflatable manometer to ensure adequacy of cuff seal and minimize the risks for aerosol spread.
Fig 1.
Systematic approach for (A) tracheal intubation and (B) lung separation for COVID-19 patients scheduled for thoracic surgery. BB, bronchial blocker; CPAP, continuous positive airway pressure; DLT, double-lumen tube; ETT, endotracheal tube; FiO2, fraction of inspired oxygen; FNAC, front of neck access; OLV, one lung ventilation; PEEP, positive end-expiratory pressure; PPE, personal protective equipment; PSV, pressure support ventilation; RSI, rapid sequence induction; SGD, 2nd generation supraglottic device; TLV, two lung ventilation.
DLT or BB
-
•
The attending anesthesiologist should be aware of the indications for and the difference between lung separation and isolation. This definition has replaced the historical classification of absolute and relative indications of one lung ventilation (OLV) (Fig 1, Table 4 ). There are some absolute indications of lung isolation using DLTs as the prevention of the contamination of the healthy lung in the case of abscess or hemorrhaging. In addition, other absolute indications are due to the need for differential ventilation of both lungs in the case of giant emphysematous bullae, bronchopleural fistulas, or bronchial interruptions finally, some other absolute indications are lung transplants or about carrying out any type of unilateral, pulmonary lavage or cleaning activities. Relative indications using BBs or DLTs can consist in cases that need to improve the surgical exposure as in upper lobectomy and lesser lung resection, thoracic aorta aneurysms, lung volume reduction or minimally invasive cardiac surgery.11
-
•
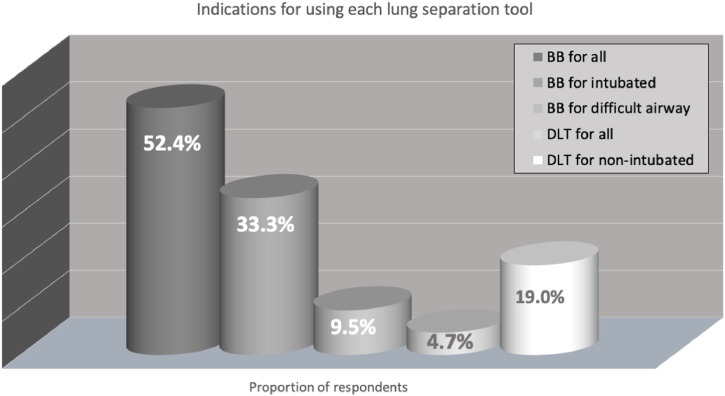
In general, 95.2% of the survey respondents reported that they would use a BB and 47.6% a DLT in patients with or suspected COVID-19. The sum for this was >100% because some members advocated for the possible use of both devices for different indications (Fig 2 ).
-
•
The use of a BB for all patients is advocated by 52.4%, and 33.3% would use a BB in already intubated patients and 9.5% in patients with difficult airway. Conversely, 28.6% would use a DLT in all cases and 19% only in nonintubated cases (Fig 3 ).
Table 4.
Indications for Lung Isolation
| Indications | Main Goal | Suggestion | ||
|---|---|---|---|---|
| Absolute indications | Unilateral lung abscess or cyst | Contralateral lung protection | DLT | |
| Unilateral lung hemorrhage (eg, thromboembolism, aneurysm) | Contralateral lung protection | DLT | ||
| Bronchoalveolar lavage with saline to treat alveolar proteinosis | Contralateral lung protection | DLT | ||
| Bronchopulmonary fistula, trachea-bronchial injury | Secure the airways and gas exchange | DLT | ||
| Severe unilateral disease (giant emphysematous bullae) | Differential lung ventilation | DLT | ||
| Lung transplantation | Secure the airways and differential ventilation | DLT | ||
| Relative indications | High priority | Pneumonectomy, sleeve resection on the bronchial mainstem Tumor obstructing the main bronchial stem |
Surgical exposure | DLT |
| Thoracic aneurysm with cardiopulmonary bypass | Surgical exposure | DLT > BB | ||
| Lobectomy and lesser lung resection (any surgical approach) | Surgical exposure | DLT = BB | ||
| Low priority | Interventions on the pleura and mediastinal structures | Surgical exposure | DLT = BB | |
| Esophagectomy | Surgical exposure | DLT = BB | ||
| Orthopedic surgery on the chest, thoracic spine surgery | Surgical exposure | DLT = BB | ||
| Minimally invasive cardiac surgery | Surgical exposure | DLT = BB | ||
| Bilateral cervical sympathectomy | Surgical exposure | BBs > DLT | ||
NOTE. In cases of absolute lung “isolation,” double-lumen tubes should be used. In other cases, the indication for bronchial blockers should be considered according the suggestions in the text
Abbreviations: BB, bronchial blocker; DLT, double-lumen tube; VATS, video-assisted thoracoscopy.
Fig 2.
The lung separation tools preferably used by the respondents for COVID-19 patients. Respondents would use only either a bronchial blocker (52.4%) or double-lumen tube (4.7%). The remaining 47.6% chose to use a bronchial blocker or double-lumen tube according to the intubation status (intubated v nonintubated), airway difficulty, and duration of the surgical procedure. BB, bronchial blockers; DLT, double-lumen tubes.
Fig 3.
The most common indications for using bronchial blockers or double-lumen tubes.
The use of bronchial blockers in all patients is advocated by 52.4%; 33.3% would use bronchial blockers in already intubated patients and 9.5% in patients with difficult airway. On the other and, 28.6% would use double-lumen tubes in all cases and 19% only in nonintubated cases. BB, bronchial blockers; DLT, double-lumen tubes.
BBs
-
•Lung separation with an ETT and a BB can be performed particularly for the following:
-
○In already intubated patients (this approach would avoid the risk of aerosolization during tube exchange)
-
○In patients with difficult airway (a “difficult” airway for ETT can be even more difficult for DLT)
-
○In short procedures
-
○In patients in whom mechanical ventilation will be continued in the postoperative period (to avoid the need for tube exchange at the end of the surgery, which can be more difficult because of the edema of the airways and be an additional mechanism of contagion)
-
○
-
•
It is suggested to use an ETT swivel connector with a valve. Before opening the valve of the swivel and introducing the bronchoscope, the anesthesia ventilator should be paused. If saturation is critical, preoxygenation can be performed in advance. During bronchoscopy, ventilation may be resumed, but it is important to ensure that the valve of the swivel fits snuggly enough such that there is no leakage; otherwise bronchoscopy should be performed during apnea. The same procedure should performed when the bronchoscope is withdrawn from the tube. Other procedures for which the airway is opened (eg, suctioning) also should be performed with apnea.
-
•
If a BB is to be used, the trachea of the patient is intubated with a standard ETT. A 7.5 to 8.0 mm ID (females) or 8.0 to 9.0 mm ID (males) ETT with a subglottic suction port should be used. It is a general rule to choose the largest possible ETT for intubation in order to allow enough room for the insertion of both the BB and the fiberoptic bronchoscope. These diameters are convenient for this approach. Because the confirmation of the position of the tube may be difficult while PPE is worn, the cuff should be passed 1 to 2 cm below the cords to avoid bronchial placement.
-
•
Tracheal intubation should be confirmed with continuous waveform capnography.
-
•
In patients intubated with an ETT and BB, the position of the BB (and the tube) should be confirmed with a disposable flexible bronchoscope or an ETT with an embedded camera.
DLTs
-
•Lung separation/isolation with a DLT has the general following advantages of DLT for OLV:
-
○Allows better suction
-
○CPAP application is easier
-
○Most importantly, anesthesiologists are more familiar with the DLT (which can lead to complications in cases in which a BB is recommended)
-
○
-
•
The position of the DLT should be confirmed with a disposable flexible bronchoscope; use of a DLT with an embedded camera can minimize the requirement for a bronchoscope and avoid the need to open the airway.
-
•Ideally, disposable bronchoscopes are the best option to avoid the need for decontamination after the procedure. If disposable devices are not available, reusable bronchoscopes also can be used with strict adherence to cleaning regulations. In any case, procedures for using a bronchoscope (either disposable or reusable) should not be compromised; only tubes (ETT or DLT) with an embedded camera can replace the need for position confirmation by bronchoscopy. Even when using tubes with embedded cameras, bronchoscopes occasionally still can be necessary. It should be kept in mind that the most common reason for hypoxemia during thoracic anesthesia is malposition of the airway device. If a bronchoscope is not available at all, the following are advised:
-
○A DLT can be used with clinical evaluation of the position
-
○A DLT with an embedded camera can be used
-
○An EZ-blocker can be used
-
○
Difficult Intubation
-
•
Awake intubation should be avoided when possible and should be limited to strict indications in patients with an anticipated difficult airway. In these cases, no aerosol or vaporization should be used for airway topicalization. Titrated sedation with an infusion pump and sedation depth monitoring must be performed.1 , 4 For intubation, a flexible (preferably disposable) endoscope with a separate remote screen should be used. A rescue intubation through a third-generation supraglottic airway device or front of neck access can be necessary (FONA), and equipment therefore should be ready before the intubation attempt.
After Intubation
-
•
If necessary, a nasogastric tube can be placed immediately after the intubation.
-
•
If the diagnosis of COVID-19 is not already confirmed, a deep tracheal aspirate for virology should be taken using closed suction.
-
•
The patient should remain connected to the breathing circuit as much as possible. A closed system with infraglottic catheter tip should be used for suction.4 , 5 , 12 If a disconnection from the breathing circuit is inevitably necessary, the ventilator should be switched to standby, and the ETT should be clamped.
-
•
After tracheal intubation, disposable equipment should be discarded appropriately, and reusable equipment should be placed inside sheaths immediately and decontaminated according to the manufacturer's recommendations,
-
•
Doffing should be performed according to the prescribed sequence (see Table 2) and be monitored by the doffing observer meticulously.
-
•
If the intubation room is separate to the OR, this room should be cleaned 20 minutes after intubation (and after all similar aerosol-generating procedures).
-
•
PPE should be worn until the end of the surgery beginning immediately after changing the outer gloves.6 , 12 Otherwise, hand hygiene must be performed before and after all patient contact. For tracheal extubation, caution should be exercised in view of the risks of aerosol transmission with coughing or need for reintubation.6 , 12 The whole donning and doffing procedure should be repeated as described.
Nonintubated Thoracic Surgery
Although some guidelines for other clinical conditions advocate regional anesthesia for nonintubated surgery as an option for nonintubated, less unwell patients to avoid the need for airway management, the authors of the present recommendations do not suggest this approach during thoracic surgery. Regional anesthesia would leave the airway open to the room for the duration of the procedure with risks of contagion spread. There is no supporting evidence or previous reports describing the nonintubated technique in patients with highly contagious diseases. Even in the “healthy” (non-COVID-19) population, nonintubated thoracic surgery is a novel, less well-described approach, which contrary to some beliefs, is more challenging for the anesthesiologist. Under the new condition with SARS-CoV-2, there may be some exceptional cases that would benefit from this approach, but overall, it should be considered as too heroic and cannot be recommended.
It should be kept in mind that all techniques of non-invasive ventilation (NIV) are associated with an increased risk of aerosol spread. Cautious use of NIV is then recommended, with full airborne level PPE donned and preferably in an isolated environment. Given the higher theoretical potential of viral spreading, the use of high-flow nasal ogygenation is discouraged.
Ventilation and OLV
-
•
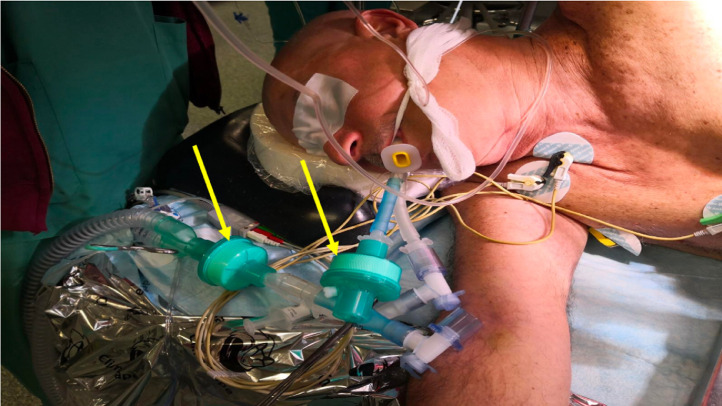
Another antiviral filter should be applied to the end of the lumen corresponding to the nondependent lung, which is disconnected during OLV to avoid (or decrease) the risk of aerosolization through the disconnected lumen (Fig 4 ).
-
•
Because the oxygenation of COVID-19 patients already is compromised, OLV could be more challenging, and a higher incidence of hypoxemia during OLV can be expected.
-
•Generic recommendation for the conduct of OLV also can be considered as valid in these patients, including the following:
-
○Fraction of inspired oxygen of 100%
-
○Low tidal volume of 4 to 6 mL/kg predicted body weight
-
○Some degree of hypercapnia can be permitted by adjusting the respiratory frequency (pH >7.2)
-
○Potentially a higher PEEP may be required than that for a patient without COVID-19: approximately 13-15 cm H2O; a PEEP titration strategy is suggested but should be performed very cautiously so as not to cause a decrease in cardiac output in higher PEEP levels
-
○It is an advantage that lung compliance is usually good in COVID-19 patients (as reported by the Italian group)13
-
○Patients may benefit from the application of an alveolar recruitment maneuver, and a trial is recommended; it should be kept in mind, however, that the recruitment strategy can impair the hemodynamic stability in a more extended way than in “healthy” patients
-
○
-
•
Clearly in some patients with active lung disease, maintenance of OLV may be impossible because of oxygenation problems. It should be kept in mind that in cases without obligatory indications for lung “isolation” (eg, airway leakage, unilateral bleeding), the principle for continuing OLV must never be to compromise oxygenation. This general rule must be adhered to even more strictly in challenging cases such as COVID-19 patients.
-
•
In open thoracotomies, application of CPAP to the nondependent lung can be very useful to prevent hypoxemia. The authors suggest that the benefits to achieve sufficient oxygenation would overcome the (unproven) possibility of aerosolization from the open CPAP system.
-
•
In some cases, application of extracorporeal assist systems (for oxygenation and/or carbon dioxide removal) can be indicated; however, these cases are beyond the scope of this review.
Fig 4.
An antiviral filter connected to the double-lumen tube.
(A permission to use was obtained from Dr. Domenico Massullo, Rome, Italy.)
Extubation
-
•
The authors assume that in almost all COVID-19 patients undergoing thoracic surgery, mechanical ventilation may need to be continued after the surgery.
-
•
If a BB is used, it simply can be removed at the end of the surgery.
-
•
If a DLT is used, it should be changed to a normal ETT using an appropriate tube exchanger (caveat: specific tube exchangers for DLTs should be used). In such cases, regulations for PPE (donning and doffing) should be repeated step by step.
-
•
If a DLT is used, an exchange to an ETT may not be warranted in some circumstances (eg, the anticipated need for a brief duration of mechanical ventilation); a classical method in such cases—after deflating both cuffs—is to pull back the DLT above the carina. Now, only the bronchial cuff can be inflated, and ventilation can be continued only via the bronchial lumen.
-
•
It has been reported that patients with COVID-19 usually have excessive retained secretions, especially during the weaning phase. Therefore it makes sense to postpone this phase to a later time frame than the immediate postoperative period.
-
•In patients who are to be extubated, the following are recommended (Fig 5 ):
-
○Before extubation, aspiration should be performed via a closed system, followed by a recruitment maneuver.
-
○Patients should be ready for extubation on to facemask. Air flow to surrounding area should be avoided as much as possible. A tight-fitting facemask is therefore essential.
-
○Again, aerosolizing procedures (eg, NIV, high-flow nasal oxygenation) should be avoided.
-
○Regarding PPE, the same level, conditions, and logistics as applied during intubation are required.
-
○Any maneuver that risks the production of precipitating coughing should be avoided; oral suctioning (if any) should be very gentle, and patients should not be asked to cough. In difficult airway cases, using an extubation catheter (eg, with a soft thin tip) may be possible, but in these cases, keeping the patient intubated is more rational.
-
○Use of medication known to effectively lower the incidence of coughing (eg, dexmedetomidine and lidocaine).
-
○Placing of a surgical mask or N95 respirator on the patient given supplementary oxygen via face mask or nasal prongs after extubation could prevent hypoxemia and reduce risk of environmental viral spreading.
-
○Transferring extubated patients should follow local regulations.
-
○
Fig 5.
Systematic approach for tracheal extubation plans for COVID-19 patients scheduled for thoracic surgery. BB, bronchial blockers; DLT, double lumen tubes; ETT, endotracheal tube; HFNO, high-flow nasal oxygen; ICU, intensive care unit; NIV, noninvasive ventilation; PPE, personal protective equipment.
After Extubation
-
•
The breathing circuit should be changed.
-
•
The airway breathing system and soda lime canisters should be decontaminated.
-
•
All disposable material should be discarded; reusable material should be sent for decontamination.
-
•
A waiting period of 20 minutes is necessary to disinfect with 3% to 5% chlorine solution.
Conclusion
The COVID-19 pandemic undoubtedly has become the most important challenge for the human race in recent memory. Health care personnel in all likelihood will have to deal with a wide range of COVID-19 patients undergoing different surgeries.
Observing the changes that the COVID-19 crisis already has caused, it can be foreseen that the “routine life” of daily practice in hospitals will be radically different, with all materials used for anesthesia potentially subject to shortage in time.
The present “opinion survey” was prepared with expert opinions and therefore does not claim to be “evidence based” or “comprehensive.” Still, the authors hope that it will be helpful to colleagues, not only for thoracic anesthesia, but also in the organization of general management for this challenging patient group.
Conflict of Interest
None.
References
- 1.Sorbello M., El-Boghdadly K., Di Giacinto I. The Italian coronavirus disease 2019 outbreak: recommendations from clinical practice [published online ahead of print, 2020 Mar 27] Anaesthesia. 2020 doi: 10.1111/anae.15049. Accessed April 15, 2020. [DOI] [PubMed] [Google Scholar]
- 2.Tang G., Chan I.K.M. World Federation of Societies of Anaesthesiologists. Coronavirus-guidance for anaesthesia and perioperative care providers. https://www.wfsahq.org/components/com_virtual_library/media/1c4ec5c64b9aaacf7c47f76a61fb6edc-atow-422-01.pdf April 6, 2020. Accessed April 15, 2020.
- 3.Zucco L, Levy N, Ketchandj D, et al. 2020 Perioperative Considerations for the 2019 Novel Coronavirus (COVID-19). https://www.apsf.org/news-updates/perioperative-considerations-for-the-2019-novel-coronavirus-covid-19/. Accessed April 15, 2020).
- 4.Faculty of Intensive Care Medicine, Intensive Care Society, Association of Anaesthetists, and Royal College of Anaesthetists. COVID-19 airway management principles. https://icmanaesthesiacovid-19.org. Accessed April 15, 2020.
- 5.Brewster D.J., Chrimes N.C., Do T.B.T. Consensus statement: Safe Airway Society principles of airway management and tracheal intubation specific to the COVID-19 adult patient group. Med J Aust. 2020 doi: 10.5694/mja2.50598. https://www.mja.com.au/system/files/2020-04/Preprint%20Brewster%20updated%201%20April%202020.pdf. Accessed April 15, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Société Française d'Anesthésie et de Réanimation. Propositions pour la prise en charge anesthésique d'un patient suspect ou infecté à Coronavirus COVID-19. Montravers P. 2020. https://sfar.org/propositions-pour-la-prise-en-charge-anesthesique-dunpatient-suspect-ou-infecte-a-coronavirus-covid-19/. Accessed April 15, 2020
- 7.Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients [published online ahead of print, 2020 Feb 12]. Directives concrètes à l'intention des équipes de soins intensifs et d'anesthésiologie prenant soin de patients atteints du coronavirus 2019-nCoV. Can J Anaesth. 2020;1–9. 10.1007/s12630-020-01591-x. Accessed April 15, 2020. [published online ahead of print, 2020 Feb 12]. [DOI] [PMC free article] [PubMed]
- 8.Chen X., Liu Y., Gong Y. Perioperative management of patients infected with the novel coronavirus: Recommendation from the Joint Task Force of the Chinese Society of Anesthesiology and the Chinese Association of Anesthesiologists. Anesthesiology. 2020 doi: 10.1097/ALN.0000000000003301. Accessed April 15, 2020. [E-pub ahead of print] (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peng P.W.H., Ho P.L., Hota S.S. Outbreak of a new coronavirus: what anaesthetists should know. Br J Anaesth. 2020 doi: 10.1016/j.bja.2020.02.008. Accessed April 15, 2020 (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rasmussen S., Smulian J., Lednicky J. Coronavirus disease 2019 (COVID-19) and pregnancy: What obstetricians need to know. Am J Obstet Gynecol. 2020 doi: 10.1016/j.ajog.2020.02.017. Accessed April 15, 2020 (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gil MG, Vivó JT, Sarabia JM, et al. Anesthesia in Thoracic Surgery. Changes of Paradigms. Ed: Manuel Granell Gil and Mert Senturk, Chapter: 5 Bronchial Blockers: Applications in Thoracic Surgery, Springer, 10.1007/978-3-030-28528-9. [DOI]
- 12.ASA, APSF, AAAA and AANA issue joint statement on the use of PPE by anesthesia professionals during the COVID-19 pandemic. https://www.asahq.org/in-thespotlight/coronavirus-covid-19-information. Accessed April 15, 2020.
- 13.Gattinoni L., Coppola S., Cressoni M. Covid-19 does not lead to a “typical” Acute Respiratory Distress Syndrome. Am J Resp Crit Care Med. 2020 doi: 10.1164/rccm.202003-0817LE. Accessed April 15, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]