Abstract
The coronavirus 2019 (COVID-19) pandemic has led to an unprecedented emergency scenario for all aspects of health care, including urology. At the time of writing, Italy was the country with the highest rates of both infection and mortality. A panel of experts recently released recommendations for prioritising urologic surgeries in a low-resource setting. Of note, major cancer surgery represents a compelling challenge. However, the burden of these procedures and the impact of such recommendations on urologic practice are currently unknown. To fill this gap, we assessed the yearly proportion of high-priority major uro-oncologic surgeries at three Italian high-volume academic centres. Of 2387 major cancer surgeries, 32.3% were classified as high priority (12.6% of radical nephroureterectomy, 17.3% of nephrectomy, 33.9% of radical prostatectomy, and 36.2% of radical cystectomy cases). Moreover, 26.4% of high-priority major cancer surgeries were performed in patients at higher perioperative risk (American Society of Anesthesiologists score ≥3), with radical cystectomy contributing the most to this cohort (50%). Our real-life data contextualise ongoing recommendations on prioritisation strategies during the current COVID-19 pandemic, highlighting the need for better patient selection for surgery. We found that approximately two-thirds of elective major uro-oncologic surgeries can be safely postponed or changed to another treatment modality when the availability of health care resources is reduced.
Patient summary
We used data from three high-volume Italian academic urology centres to evaluate how many surgeries performed for prostate, bladder, kidney, and upper tract urothelial cancer can be postponed in times of emergency. We found that approximately two-thirds of patients with these cancers do not require high-priority surgery. Conversely, of patients requiring high-priority surgery, approximately one in four is considered at high perioperative risk. These patients may pose challenges in allocation of resources in critical scenarios such as the current COVID-19 pandemic.
Keywords: Coronavirus, COVID-19, High priority, Italy, Major cancer surgery, Pandemic
Take Home Message
Our study involving three Italian high-volume centres provides real-life data to contextualise ongoing recommendations on the selection of priority surgeries in the emergency scenario caused by the COVID pandemic. Overall, 67.8% of elective major uro-oncologic surgeries can be postponed.
The coronavirus 2019 (COVID-19) pandemic has led to an unprecedented emergency scenario for all aspects of health care, including urology [1], [2], [3], [4]. At the time of writing, Italy was the country with the highest rates of infection and mortality from COVID-19. According to the updated Italian statistics released on March 25, 2020, 74 386 people had been infected, with 7503 deaths [5]. The dramatic spread of this epidemic is leading to major changes in the management of patients with cancer, including those affected by genitourinary malignancies [6]. In this context, virtually all urology centres have been forced to prioritise surgical interventions for cancer patients by applying a series of restrictions on elective approaches to optimise health care resources and minimise the risk of hospital-acquired infection [4], [7], [8], [9]. This prioritisation process started early in Italy [3], [4].
By looking at the ongoing Italian situation, many opinion leaders worldwide have proposed recommendations for the triage of elective urologic surgeries during the COVID-19 pandemic. A panel of experts from Europe and the USA recently proposed a list of urologic procedures that should be prioritised, taking into account factors that include the aggressiveness of each disease (and its stage), the impact of short-term delays to care, and the availability of alternative treatment modalities [7]. Of note, the focus should be on major cancer surgery, which represents a large and demanding proportion of practice in most referral centres.
However, the exact burden of major urologic cancer procedures is unknown and the impact of such recommendations on urologic practice still needs to be investigated. The importance of such an analysis is even more important given the heterogeneous outcomes for uro-oncologic patients and the possible need to shift surgical candidates to other forms of treatment as an alternative to surgery.
To fill these gaps, we provide a real-life overview of the yearly proportion of high-priority major uro-oncologic surgeries at three academic referral centres in northern and central Italy (San Luigi Hospital in Turin, San Raffaele Hospital in Milan, and Careggi Hospital in Florence, all performing >500 major cancer procedures annually), where the COVID-19 pandemic has put a strain on health care resources.
We queried our respective institutional prospectively collected databases for the most common urologic cancers (prostate, urothelial, and kidney) to select patients undergoing elective major surgery during a 12-mo period (2018 or 2019). Among the surgeries, Stensland et al [7] included radical cystectomy (RC), radical nephroureterectomy (RNU), nephrectomy (NEP) for cT3+ disease, and radical prostatectomy (RP) for high-risk patients if not eligible for radiation. From an analytic standpoint, besides all RC, RNU, and NEP procedures for cT3+ tumours, we also considered NEP for cT2 masses as high-priority surgery, as the decision-making is highly nuanced for several patient-specific considerations and the tumour growth rate [7]. In addition, we included RPs for patients with locally advanced prostate cancer (defined according to the European Association of Urology guidelines [9]) because even though alternative treatment strategies may be offered, their availability for all eligible patients could be potentially limited by logistic issues in times of emergency.
Overall, 2387 patients were included. Of these, 771 (32.3%) were classified as high priority (Fig. 1 ). Stratifying these surgeries by cancer type, RNU, NEP, RP, and RC accounted for 12.6%, 17.3%, 33.9%, and 36.2%, respectively, of high-priority procedures. High-priority RPs represented 11.0% of all major cancer surgeries performed in our centres, with NEPs accounting for 5.6%, RCs for 11.7%, and RNUs for 4.1%.
Fig. 1.
Cumulative proportion of patients undergoing high-priority major cancer surgeries, stratified by cancer type, procedure, and surgical approach. (A) Overall proportion of patients undergoing high-priority major cancer surgeries and relative contribution of each cancer to the overall number of high-priority surgeries. (B) Cumulative proportion of patients undergoing high-priority radical prostatectomy, nephrectomy, radical cystectomy, and radical nephroureterectomy among all major cancer surgeries (n = 2387). (C) Cumulative proportion of high-priority major cancer surgeries via minimally invasive (dark grey) or open surgery (light grey) and average length of hospitalisation (LOH; range in days) for each procedure. All data are for either 2018 (from January 1 to December 31) or 2019 (from January 1 to December 31).
BCa = bladder cancer; MIS = minimally invasive surgery; PCa = prostate cancer; RCC = renal cell carcinoma; UTUC = upper tract urothelial carcinoma.
Minimally invasive surgery (MIS) was used for >90% of high-priority RPs, and ranged between 40% for RC and 61% for high-priority NEP among the other surgeries. The average length of hospitalisation (LOH) for high-priority major oncologic surgeries at our centres is higher than the data reported by Stensland et al [7]; this is potentially explained by differences in health care systems across countries. Of note, MIS at our centres appears to have an impact on LOH for all procedures except for RC.
It is notable that a non-negligible proportion of patients undergoing high-priority major cancer surgeries are at higher perioperative risk (with potentially longer LOH and a greater need for postoperative monitoring in intensive care units), posing challenges in resource allocation during the current COVID-19 pandemic [2], [3], [4].
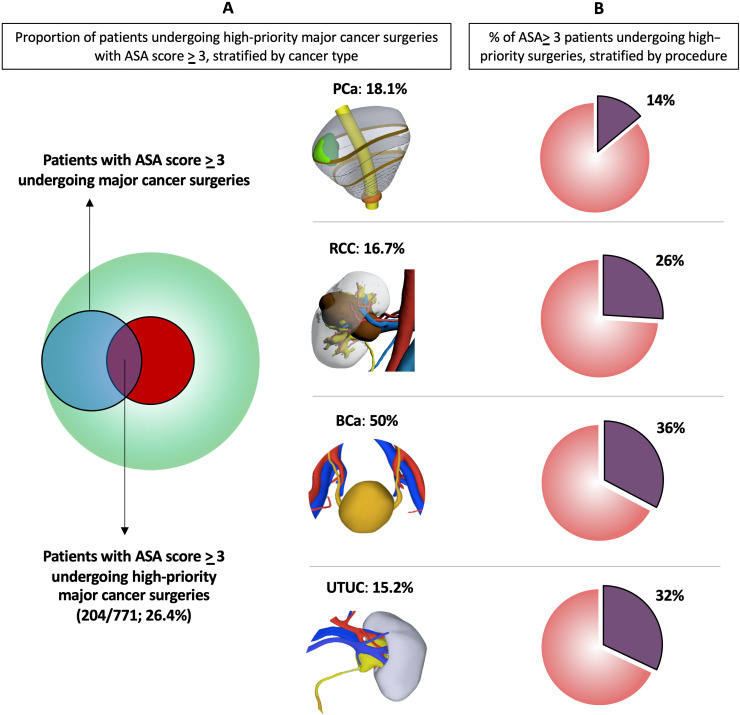
Using an American Society of Anesthesiologists (ASA) score of ≥3 as a surrogate metric, Fig. 2 provides an overview of the burden of these patients. Overall, 26.4% of high-priority major cancer surgeries were performed in patients at higher perioperative risk. Patients undergoing RC contributed the most to this cohort (50%). Stratifying ASA ≥ 3 cases by procedure, high-priority RP accounted for 14% NEP for 26%, RNU for 32.0%, and RC for 36%.
Fig. 2.
Proportion of patients with higher perioperative risk, defined as ASA score ≥3, undergoing high-priority major cancer surgeries. (A) Overall proportion of patients with ASA score ≥3 undergoing high-priority major cancer surgeries and relative contribution of each cancer to the overall number of high-priority patients with ASA score ≥3 (n = 204). (B) Percentage of patients with ASA score ≥3 undergoing high-priority radical prostatectomy (RP), nephrectomy (NEP), radical cystectomy (RC), or radical nephroureterectomy (RNU) as a proportion of all high-priority cases for each procedure. All data are for either 2018 (from January 1 to December 31) or 2019 (from January 1 to December 31).
ASA = American Society of Anesthesiologists; BCa = bladder cancer; PCa = prostate cancer; RCC = renal cell carcinoma; UTUC = upper tract urothelial carcinoma.
Our study provides data that may contextualise the ongoing recommendations [7] on selection of priority major cancer surgeries in the increasingly challenging health care situation caused by the COVID-19 pandemic.
The key finding is that in times of emergency that necessarily lead to a dramatic reduction in operating room availability for urologic procedures, 67.8% of elective major uro-oncologic surgeries can be postponed. Furthermore, of the remaining 32.2% of patients requiring high-priority surgery, a non-negligible proportion might be shifted to alternative treatment strategies if available, after shared decision-making. Finally, careful selection of surgical candidates is key during the COVID-19 pandemic considering that 26.2% of high-priority major surgeries were performed in patients with high preoperative risk. For these patients, use of alternative treatment modalities may be even more important to further reduce the potential need for intensive care units given the limited resources.
Overall, this study may have practical implications considering that in our three centres a progressive significant reduction in or even complete interruption of all elective procedures was mandated, starting 2 wk after the first certified COVID-19 case in Italy.
Our findings should be contextualised considering that many other factors related to patients, resources, and health care scenarios (eg, high- vs low-volume centre) impact on surgical indications and decision-making when prioritising and scheduling surgeries, especially in times of emergency such as the COVID-19 pandemic.
In conclusion, our real-life data from three Italian academic referral centres offer the urology community and policymakers insights into the burden of major cancer procedures that can be postponed in times of emergency. Our study can help other urology centres worldwide in adapting their management strategies for the inflow of uro-oncologic patients in light of the expected reduction in resources caused by the COVID-19 pandemic.
Author contributions: Riccardo Campi had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Campi, Amparore, Serni, Porpiglia.
Acquisition of data: Campi, Amparore, Checcucci, Capitanio.
Analysis and interpretation of data: Campi, Amparore.
Drafting of the manuscript: Campi, Amparore.
Critical revision of the manuscript for important intellectual content: Checcucci, Fiori, Porpiglia, Capitanio, Salonia, Briganti, Montorsi, Carini, Serni, Minervini.
Statistical analysis: Campi, Amparore.
Obtaining funding: None.
Administrative, technical, or material support: None.
Supervision: Serni, Carini, Montorsi, Porpiglia.
Other: None.
Financial disclosures: Riccardo Campi certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: None.
Funding/Support and role of the sponsor: None.
Associate Editor: Giacomo Novara
References
- 1.World Health Organization. Report of the WHO-China Joint Mission on coronavirus disease 2019 (COVID-19). www.who.int/publications-detail/report-of-the-who-china-joint-mission-on-coronavirus-disease-2019-(covid-19).
- 2.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395(10231):1225–1228. doi: 10.1016/S0140-6736(20)30627-9. Apr 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Naspro R., Da Pozzo L.F. Urology in the time of corona. Nat Rev Urol. In press. 10.1038/s41585-020-0312-1. [DOI] [PMC free article] [PubMed]
- 4.Ficarra V., Novara G., Abrate A., et al. Urology practice during COVID-19 pandemic. Minerva Urol Nefrol. In press. 10.23736/S0393-2249.20.03846-1. [DOI] [PubMed]
- 5.Italian Ministry of Health. Nuovo coronavirus. www.salute.gov.it/nuovocoronavirus.
- 6.Gillessen Sommer S., Powles T. Advice for medical oncology care of urological cancer patients during the COVID-19 pandemic. Eur Urol. In press. [DOI] [PMC free article] [PubMed]
- 7.Stensland K.D., Morgan T.M., Moinzadeh A., et al. Considerations in the triage of urologic surgeries during the COVID-19 pandemic. Eur Urol. In press. [DOI] [PMC free article] [PubMed]
- 8.American College of Surgeons. COVID-19: guidance for triage of non-emergent surgical procedures. www.facs.org/about-acs/covid-19/information-for-surgeons/triage.
- 9.Mottet N., Cornford P., van den Bergh RCN, et al. EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer, version 2020. https://uroweb.org/guideline/prostate-cancer/. [DOI] [PubMed]