To the Editor:
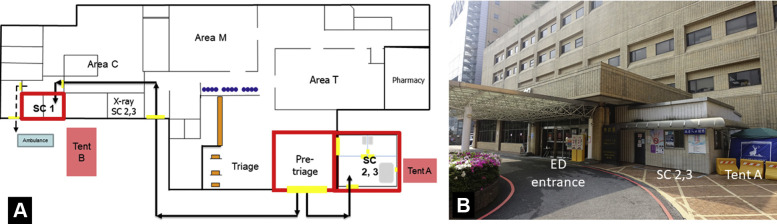
The World Health Organization declared the novel coronavirus disease 2019 (COVID-19) outbreaks a global pandemic.1 , 2 To avoid contamination and to protect health care workers, we designed a unique patient diversion strategy at the emergency department (ED) of the National Taiwan University Hospital. It was composed of 1 pretriage unit, 3 special clinics, and 2 tents (Figure ). Personal protective equipment included an N95 mask covered by a surgical mask, a hair cap, a goggle, a facial shield, gloves, a gown, and shoe coverings.
Figure.
Flow of patients with a history of travel, occupation, cluster, and contact (arrows). A, Red squares represent the pretriage unit and the special clinics, possible contaminated areas. Yellow rectangles represent doors. Area C denotes the critical and resuscitation area. Area M denotes the area for medical patients. Area T denotes the area for trauma patients. Dashed lines depict patient traffic (special clinic 1) to the ward. B, The entrance to special clinics 2 and 3 and tent A. SC, Special clinic.
The pretriage unit was located at the main entrance, including 1 nurse, 2 security guards, and 1 administrative officer. One guard was responsible for entry-gate control with an infrared thermal camera, and the other for patient traffic outside the ED. The officer checked immigration records from health insurance cards. If patients had any history of travel, high-risk occupation, cluster, or contact with patients with suspected COVID-19 and fever or respiratory symptoms, the nurse led pediatric patients to the special clinic 2 and adult patients to special clinic 3. If a patient with a positive history of travel, high-risk occupation, cluster, or contact with patients with suspected COVID-19 presented with respiratory distress, he or she was sent to a negative-pressure room, special clinic 1. Every patient was required to use hand hygiene and wear a surgical mask.
Special clinic 3 was a well-ventilated separate room staffed by 2 emergency physicians and nurses. One nurse provided nursing services and the other staying outside conducted specimen, medicine, and checkout delivery.
The patient stayed inside special clinic 3 at a distance of more than 6 feet from others. The nurse accompanied the patient to and from the isolated radiograph room. The physician talked to the patient by intercom. If pneumonia was suspected, the patient was transferred to tent B until admission; otherwise, he or she received a throat swab at tent A. Given instructions to self-quarantine, patients were discharged without entering the main area. If the swab result was positive, health authorities called the patient back for admission.
Staff removed personal protective equipment and washed hands in the anteroom. The nurse used a fluorescent agent to check the thoroughness of hand washing.
Special clinic 2 was the same as special clinic 3, except the physicians were ED pediatricians. One person wearing a surgical mask treated pediatric patients.
Special clinic 1 was the same as special clinic 3, except staffed by different emergency physicians and nurses. Patients received a radiograph inside the clinic. If they needed intubation, video-assisted laryngoscopy was used and gowns were changed to a level C protective suit.
This design separated patients at risk of COVID-19 infection from uninfected patients to restrict contaminated areas. Our experience allowed us to use the existing hospital for the current outbreak instead of a separate building.
From January 21 to March 27, 2020, average daily visits to special clinics 1, 2, and 3 were 3, 4, and 17, respectively. Four new cases of COVID-19 infection were diagnosed; no nosocomial infection was identified.
Footnotes
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
References
- 1.Mahase E. Covid-19: WHO declares pandemic because of “alarming levels” of spread, severity, and inaction. BMJ. 2020;368:m1036. doi: 10.1136/bmj.m1036. [DOI] [PubMed] [Google Scholar]
- 2.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]