See editorial on page 36.
Up to 20% of health care personnel (HCP) were found to be infected with coronavirus disease (COVID-19)1 in the outbreak in northern Italy.2 Recommendations on patient and HCP protection have been made, such as postponing procedures, triage, use of personal protective equipment (PPE), and creation of differentiated in-hospital pathways.3 , 4 However, several barriers against the adoption of these strategies exist, including cultural factors and shortages of medical resources; therefore, there are few reports of real-world experiences and outcomes with their adoption.5
The aim of this survey was to investigate the burden of COVID-19 on endoscopic activity in a high-risk area of COVID-19 outbreak, approaches to evaluating patients, adoption and compliance of HCP with protective measures, and initial possible viral transmission outcomes from endoscopy units within a large, community-based setting (both between patients and HCP and between HCP).
Methods
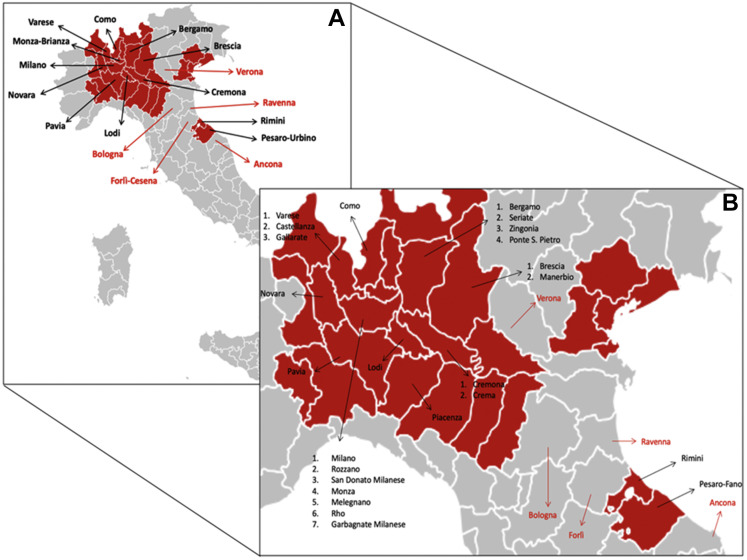
The study was conducted as a survey between March 16 and March 21, 2020. Directors of emergency departments in high-risk areas of northern Italy (Supplementary Figure 1) were invited by e-mail to complete a questionnaire (Figure 1 and Supplementary Table 1). Participation was voluntary. Additional methodology is provided in the Supplementary Material.
Supplementary Figure 1.
(A) The Italian provinces included in our survey: black arrows indicate the first ones quarantined, and red arrows show the ones quarantined later. (B) Cities where the endoscopic units that answered the survey are present; black arrows show those belonging to areas immediately quarantined and red arrows indicate those quarantined later.
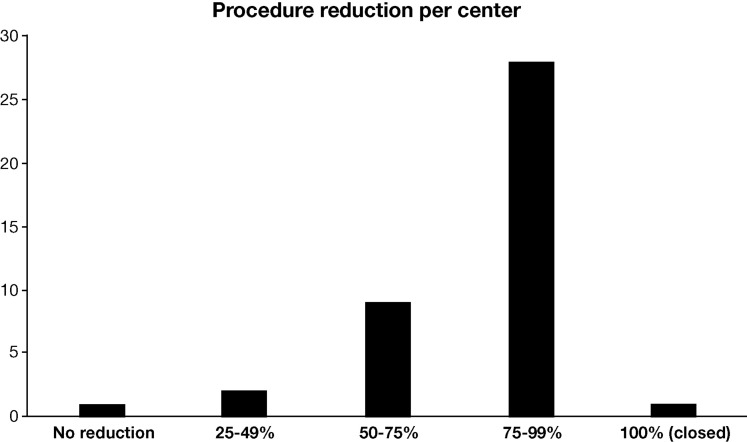
Figure 1.
Reduction of endoscopic activities.
Results
Characteristics of the Endoscopy Units
A total of 42 endoscopy units were invited, of which 41 participated (97.6%). Most respondents (n = 37, 90.2%) were from high-volume endoscopy units, for a total of 968 endoscopy personnel, including 323 endoscopists, 496 nurses, and 149 health care assistants.
Changes in Endoscopy Activity Related to Coronavirus Disease 2019
All endoscopy units had patients diagnosed with COVID-19 in their hospital. All but 1 center (40/41, 97.6%) reduced normal endoscopic activities because of COVID-19. Quantification of the reductions is shown in Figure 1. After the COVID-19 outbreak, 39 endoscopy units (95.1%) continued to perform urgent procedures, 39 (95.1%) continued inpatient procedures, 28 (68.3%) continued screening colonoscopies for colorectal cancer (positive fecal immunochemical test, [FIT +]), 9 endoscopy units (22.0%) continued outpatient therapeutic procedures, and 7 (17.1%) performed all procedures.
Procedures in Patients With Coronavirus Disease 2019 or Those at High Risk
A total of 35 endoscopic procedures, performed in 14 of 41 (34.1%) endoscopy units, were performed on patients with COVID-19. All procedures were urgent or nondeferrable, and none were for COVID-19–related gastrointestinal diseases. In addition, 99 endoscopic procedures, performed by 20 of 41 (48.8%) endoscopy units, were performed on patients with suspected COVID-19, of whom 40 (40.4%) were subsequently diagnosed with the disease. Only 11 of 41 (26.8%) endoscopy units performed a direct follow-up on patients with suspected disease. No cases of HCP infection/transmission directly related to endoscopic procedures in COVID-19–positive patients were reported.
For all asymptomatic patients, only 1 endoscopy department performed follow-up for the development of respiratory symptoms in the next 14 days, whereas 18 endoscopy units were only informed of COVID-19–positive patients.
Infection Prevention and Control Measures for Coronavirus Disease 2019
Regarding the preventive measures taken after the first Italian case (February 18, 2020), 5 (12.2%) endoscopy units did not take any measures, 29 (70.7%) endoscopy units adopted a triage for risk stratification of COVID-19 infection, 7 (17.1%) endoscopy units decreased endoscopic procedures, 13 (31.7%) endoscopy units modified the use of PPE, 3 (7.3%) endoscopy units modified the waiting room, 1 (2.4%) emergency department performed nasopharyngeal swab tests on inpatients before endoscopy, and 2 (4.9%) endoscopy units prohibited patient caregivers from entering the unit. Furthermore, 31 endoscopy units (75.6%) have further modified these measures since March 9, 2020, including adopting a phone triage for COVID-19 (6 [14.6%] endoscopy units), reducing staff or procedures (12 [29.3%] endoscopy units), updating PPE use (19 [46.3%] endoscopy units), providing PPE to patients (2 [4.9%] endoscopy units), and establishing specific hospital protocols (2 [4.9%] endoscopy units).
When considering changes in emergency endoscopic procedures, 27 (65.9%) endoscopy units made modifications (PPEs for COVID-19 patients themselves; emergency endoscopic procedures in the operating room, in the emergency department, or in the patient’s room; and disinfection of the room after emergency endoscopic procedures, nasopharyngeal swabs before emergency endoscopic procedures, and/or a different endoscopic station).
Regarding PPE availability, surgical masks were available in 37 (90.2%) endoscopy units; N95/Filtering Face Piece 2-3 in 39 (95.1%); gloves in 39 (95.1%) ; hairnets in 37 (90.2%); goggles/face shields in 39 (95.1%); and long-sleeved, water-resistant gowns in 35 (85.4%). Additionally, 33 (80.5%) endoscopy units provided PPE to patients who had to undergo endoscopic procedures. When performing procedures on patients who tested positive for COVID-19, a surgical mask was used in 9 (22.0%) endoscopy units; N95/FFP2-3 in 40 (97.6%); a single pair of gloves in 5 (12.2%); a double pair of gloves in 36 (87.8%); hairnets in 39 (95.1%); goggles/face shields in 40 (97.6%); and long-sleeved, water-resistant gowns in 36 (87.8%). Finally, 7 endoscopy units (17.1%) have the availability of a negative-pressure room, and 16 endoscopy units (39.0%) dedicated specific areas for endoscopy in patients with COVID-19.
Modifications in Endoscopy Department Organization Due to the Coronavirus Disease 2019 Outbreak
In 27 (65.9%) endoscopy units, endoscopists were relocated to other hospital departments, for example, to assist with COVID-positive patients with pneumonia or in the emergency department. In 31 (75.6%) endoscopy units, nurses were relocated to other hospital departments. Twenty-five (61.0%) endoscopy units received specific Infection Prevention and Control instructions from the Hospital Health Direction. A protocol for PPE use was written in agreement with Hospital Health Direction by 26 (63.4%) endoscopy units, and a protocol on how to manage patients positive or highly suspicious for COVID-19 was written by 23 (56.1%) endoscopy units.
Potential Severe Acute Respiratory Syndrome Coronavirus 2 Infection Within the Endoscopy Department
We asked if there were cases of infection within endoscopic departments; 12 endoscopy units confirmed infections among nurses and physicians, with 6 endoscopy personnel (3 nurses and 3 physicians) requiring hospitalization: none of the infections were through the endoscopic equipment; 1 was presumed to be from the environment outside the endoscopy unit; 3 were presumed to be from contact with unrecognized infected patients in early/middle February, when stringent protective measure were not yet adopted by endoscopy personnel; and the remaining was from a combination of presumed exposures from the external environment and/or infected colleagues/endoscopy personnel.
Discussion
Our survey shows dramatic burden for endoscopy units related to the COVID-19 outbreak in a high-risk area. Most routine procedures have been cancelled or postponed, limiting endoscopy to urgent cases; we outline here the variability of approaches taken in different centers. In addition, all endoscopy units are in hospitals with at least 1 case of COVID-19, and in more than half of the departments, procedures were performed in infected/high-risk patients. This was offset by a reassuring availability of adequate protectors, especially N95/FFP2-3 respirators.
Most endoscopy units limited their activity to urgent cases, also including patients at high risk of cancer, such as FIT+. This underlines a multicenter approach to how the triage of cases can be done through case-by-case determination of the risk of gastrointestinal cancer versus that of infection.3
The second relevant result of our survey is the fact that at least 1 in every 2 endoscopy units is directly involved in emergent or urgent procedures in patients with COVID-19. Such contact is to be deemed as potentially dangerous, because upper gastrointestinal endoscopy is an aerosol-generating procedure.2 Thus, most of the staff of endoscopy units in a high-risk area of COVID-19 must be ready to face the highest risk of infection. Third, despite the shortage of medical resources, most endoscopy units have availability of N95 respirators for high-risk procedures.
The third relevant result is the very limited risk of known patient-to-HCP transmission within the endoscopy unit setting but the presence of possible transmission from health care providers to other health care providers, emphasizing the importance of maintaining vigilance in all contacts and settings.
The burden of COVID-19 on endoscopy units is substantial, disrupting daily routines and exposing HCP to risk of infection.
Acknowledgments
ITALIAN GI-COVID19 Working Group: Roberta Maselli, MD, PhD1, Marco Spadaccini, MD1,2, Massimiliano Mutignani, MD3, Armando Gabbrielli, MD4, Clementina Signorelli, MD5, Cristiano Spada, MD6, Piera Leoni, MD7, Carlo Fabbri, MD8, Sergio Segato, MD9, Nicola Gaffuri, MD10, Benedetto Mangiavillano, MD11, Franco Radaelli, MD12, Raffaele Salerno, MD13, Stefano Bargiggia, MD14, Luca Maroni, MD, PhD15, Antonio Benedetti, MD15, Pietro Occhipinti, MD16, Federico De Grazia, MD17, Luca Ferraris, MD18, Gianpaolo Cengia, MD19, Salvatore Greco, MD20, Costanza Alvisi, MD21, Antonella Scarcelli, MD22, Luca De Luca, MD22, Fabrizio Cereatti, MD23, Pier Alberto Testoni, MD24, Roberto Mingotto, MD25, Giovanni Aragona, MD26, Gianpiero Manes, MD27, Paolo Beretta, MD28, Georgios Amvrosiadis, MD29, Vincenzo Cennamo, MD30, Fausto Lella, MD31, Guido Missale, MD32, Pavlos Lagoussis, MD33, Omero Triossi, MD34, Mauro Giovanardi, MD35, Giuseppe De Roberto, MD36, Paolo Cantù, MD37, Elisabetta Buscarini, MD38, Andrea Anderloni, MD, PhD1, Silvia Carrara, MD1, Alessandro Fugazza, MD1, Piera Alessia Galtieri, MD1, Gaia Pellegatta, MD1, Giulio Antonelli, MD39, Thomas Rösch, MD40, Prateek Sharma, MD41.
Affiliations:
1 Humanitas Clinical and Research Center, Digestive Endoscopy Unit, Rozzano (Milan). Italy.
2 Humanitas University, Department of Biomedical Sciences, Rozzano (Milan). Italy .
3 Niguarda-Ca' Granda Hospital, Digestive and Operative Endoscopy Unit, Milan. Italy.
4 The Pancreas Institute, University Hospital of Verona, Gastroenterology and Digestive Endoscopy Unit, Verona. Italy.
5 ASST Bergamo Ovest, Gastroenterology and Digestive Endoscopy, Bergamo. Italy.
6 Fondazione Poliambulanza, Digestive Endoscopy Unit, Brescia. Italy.
7 AO Lodi, Gastroenterology & Digestive Endoscopy Unit, Lodi. Italy.
8 AUSL Bologna Bellaria-Maggiore Hospital, Gastroenterology and Digestive Endoscopy Unit, Bologna. Italy.
9 ASST Dei Sette Laghi, Gastroenterology and Gastrointestinal Endoscopic Unit, Varese. Italy.
10 Humanitas Gavazzeni, Gastrointestinal Endoscopy Unit, Bergamo. Italy.
11 Humanitas Mater Domini, Gastrointestinal Endoscopy Unit, Castellanza (Milan). Italy.
12 Valduce Hospital, Gastroenterology Unit, Como. Italy.
13 Fatebenefratelli Sacco, Gastroenterology and Digestive Endoscopy Unit, ASST Milan. Italy.
14 Clinica San Carlo, Gastroenterology and Digestive Endoscopy Unit, Paderno Dugnano (Milan). Italy .
15 Università Politecnica delle Marche, Department of Gastroenterology and Hepatology, Ancona. Italy.
16 Department of Gastroenterology, "Maggiore Della Carità" Hospital, Novara. Italy.
17 Fondazione IRCCS Policlinico San Matteo, University of Pavia, First Department of Internal Medicine, Pavia. Italy.
18 ASST Valleolona PO, Gastroenterology and Digestive Endoscopy, Gallarate (Varese). Italy.
19 Ospedale di Manerbio, Endoscopy Unit, Brescia. Italy.
20 Papa Giovanni XXIII Hospital, Gastroenterology and Digestive Endoscopy Units, Bergamo. Italy.
21 ASST Pavia, Digestive Endoscopy Unit, Pavia. Italy.
22Azienda Ospedaliera Ospedali Riuniti Marche Nord, Gastroenterology and Digestive Endoscopy Units, Pesaro (Pesaro-Urbino). Italy.
23 Cremona Hospital, Digestive Endoscopy and Gastroenterology Unit, Cremona. Italy.
24 Vita Salute San Raffaele University, IRCCS San Raffaele Scientific Institute, Division of Gastroenterology and Gastrointestinal Endoscopy, Milan. Italy.
25 ASST Melegnano-Martesana, Gastroenterology and Digestive Endoscopy, Melegnano (Milan). Italy.
26 "Guglielmo da Saliceto" Hospital, Department of Internal Medicine, Gastroenterology and Hepatology Unit Piacenza. Italy.
27 ASST Rhodense, Department of Gastroenterology and Digestive Endoscopy, Garbagnate Milanese (Milan). Italy.
28 Città Studi, Gastroenterology and Digestive Endoscopy Unit, Milan. Italy.
29 Policlinico San Marco, Department of Gastroenterology, Zingonia (Bergamo). Italy.
30 Bellaria-Maggiore Hospital, Division of Gastroenterology, Bologna. Italy.
31 Policlinico San Pietro, Gastroenterology and Digestive Endoscopy Unit, Bergamo. Italy.
32 ASST Spedali Civili, Brescia University, Digestive Endoscopy Unit, Brescia. Italy.
33 IRCCS Policlinico San Donato, Digestive Endoscopy, San Donato Milanese (Milan). Italy.
34 AUSL Romagna, Gastroenterology Unit, Ravenna. Italy.
35 Ospedale di Rimini, Gastroenterology and Digestive Endoscopy, Rimini. Italy.
36 Institute of Oncology IRCCS, Division of Endoscopy, European Milan. Italy.
37 Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico, Gastroenterology and Endoscopy Unit, Milan. Italy.
38 Maggiore Hospital, Gastroenterology and Digestive Endoscopy Unit, Crema (Cremona). Italy.
39 Nuovo Regina Margherita Hospital, Digestive Endoscopy, Rome. Italy.
40 University Hospital Hamburg-Eppendorf, Department of Interdisciplinary Endoscopy, Hamburg, Germany.
41 University of Kansas Medical Center, Division of Gastroenterology & Hepatology, Department of Internal Medicine, Kansas, Missouri, USA.
Footnotes
Conflicts of interest The authors disclose no conflicts of interest.
Note: To access the supplementary material accompanying this article, visit the online version of Gastroenterology at www.gastrojournal.org, and at https://doi.org/10.1053/j.gastro.2020.04.003.
Contributor Information
ITALIAN GI-COVID19 Working Group:
Roberta Maselli, Marco Spadaccini, Massimiliano Mutignani, Armando Gabbrielli, Clementina Signorelli, Cristiano Spada, Piera Leoni, Carlo Fabbri, Sergio Segato, Nicola Gaffuri, Benedetto Mangiavillano, Franco Radaelli, Raffaele Salerno, Stefano Bargiggia, Luca Maroni, Antonio Benedetti, Pietro Occhipinti, Federico De Grazia, Luca Ferraris, Gianpaolo Cengia, Salvatore Greco, Costanza Alvisi, Antonella Scarcelli, Luca De Luca, Fabrizio Cereatti, Pier Alberto Testoni, Roberto Mingotto, Giovanni Aragona, Gianpiero Manes, Paolo Beretta, Georgios Amvrosiadis, Vincenzo Cennamo, Fausto Lella, Guido Missale, Pavlos Lagoussis, Omero Triossi, Mauro Giovanardi, Giuseppe De Roberto, Paolo Cantù, Elisabetta Buscarini, Andrea Anderloni, Silvia Carrara, Alessandro Fugazza, Piera Alessia Galtieri, Gaia Pellegatta, Giulio Antonelli, Thomas Rösch, and Prateek Sharma
Supplementary Methods
The study was conducted as a survey between March 16 and March 21, 2020. The directors of emergency departments of a specific area of northern Italy (Supplementary Figure 1), defined as a red zone, were invited by e-mail to complete a structured questionnaire on the COVID-19–related changes in endoscopic activities, prevention measures, and overall burden of the outbreak in their units (Supplementary Table 1). We arbitrarily defined the red zone the area of northern Italy with the highest incidence of infected people, as well as isolated clusters in the adjacent area with at least 500 confirmed cases of COVID-19 as of March 15, 2020. No incentive was offered for participation.
Statistics
Data were collected, analyzed, and extracted with graphs and analysis by using SPSS (IBM SPSS Inc, Chicago, IL). Percentages were calculated based on the total number of survey participants and the number of responses to each individual question. Data were collected and analyzed by means of descriptive statistics as mean and standard deviation. Categorical variables were compared using the chi-square test. The Student t test was used to compare the distribution of continuous variables by outcome. All differences were considered significant at a 2-sided P value of <.05.
Supplementary Table 1.
List of questions presented in the survey
| Characteristics of Endoscopy Units | |
| 1 |
How many procedures do you perform in your endoscopy unit every year?
|
| 2 | How many physicians do you have in your endoscopy unit? |
| 3 | How many nurses do you have in your endoscopy unit? |
| 4 | How many health care assistants do you have in your endoscopy unit? |
| Changes in endoscopy activity related to COVID-19 | |
| 5 |
When was the first case of infection found in your hospital?
|
| 6 | When did you start reducing the daily endoscopic activity? |
| 7 |
How much has it reduced?
|
| 8 |
What kind of procedures are you still doing?
|
| Procedures in COVID-19–positive or high-risk patients | |
| 9 | How many endoscopic procedures have you performed in SARS-CoV-2a–infected patients? |
| 10 | What were the main indications for the examination? |
| 11 | How many endoscopic procedures have you performed in patients with suspected SARS-CoV-2 infection? |
| 12 | What were the main indications for the examination? |
| 13 |
Did you do follow up with this type of patient?
|
| 14 | How many of them were found to be positive for COVID-19? |
| 15 |
Are you performing follow-up in asymptomatic patients who undergo endoscopic procedures to assess whether they develop respiratory symptoms in the next 14 days?
|
| 16 |
Have you ever been informed of a patient who became positive in the 14 days following an endoscopic procedure?
|
| Infection prevention and control measures for COVID-19 | |
| 17 |
What kind of preventive measures have you taken since the news of the first case of COVID-19breported in Italy (February 18, 2020)?
|
| 18 |
Have you recently (after March 9, 2020) changed any of the previously cited measures?
|
| 19 |
Have you changed something in emergency endoscopic procedures?
|
| 20 |
What kind of personal protective equipment was provided to your endoscopy unit?
|
| 21 |
What kind of personal protective equipment do you use while performing procedures in patients positive or highly suspicious for SARS-CoV-2 infection?
|
| 22 |
Do you provide any personal protective equipment to patients who have to undergo endoscopic procedures?
|
| 23 |
Is your endoscopy unit provided with negative pressure rooms?
|
| 24 |
Have you dedicated specific areas to performing endoscopic procedures in COVID-19 patients?
|
| Modifications in endoscopy department organization due to COVID-19 outbreak | |
| 25 |
How many physicians have been relocated to other departments?
|
| 26 |
How many nurses have been relocated to other departments?
|
| 27 |
Was the endoscopy unit converted to another use?
|
| 28 |
Have you had any specific instructions from the Hospital Health Direction on how to work during this period?
|
| 29 |
Have you developed infectious risk management protocols in agreement with the Hospital Health Direction?
|
| 30 |
Have you written protocols in agreement with the Hospital Health Direction on the proper use of personal protective equipment?
|
| 31 |
Have you received training on how to wear personal protective equipment properly?
|
| 32 |
Have you developed protocols in agreement with the Hospital Health Direction on how to manage positive or highly suspicious cases of SARS-CoV-2 infection?
|
| 33 |
In your opinion, is it possible to transmit the infection within the endoscopy unit?
|
SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
References
- 1.Lancet. 2020;395:922. [Google Scholar]
- 2.Dipartimento della Protezione Civile. http://www.protezionecivile.gov.it/media-comunicazione/comunicati-stampa
- 3.European Society of Gastrointestinal Endoscopy. https://www.esge.com/esge-and-esgena-position-statement-on-gastrointestinal-endoscopy-and-the-covid-19-pandemic/
- 4.Repici A. Gastrointest Endosc. 2020 S0016-5107(20)30245-5. [Google Scholar]
- 5.ASGE Quality Assurance in Endoscopy Committee Gastrointest Endosc. 2018;87:1167–1179. doi: 10.1016/j.gie.2017.12.009. [DOI] [PubMed] [Google Scholar]