Graphical abstract
The case series provides radiographers with essential information to preliminarily evaluate chest imaging and prompt the rapid diagnosis of COVID-19.
Keywords: COVID-19, Preliminary clinical evaluation, Radiograph, Computed tomography, Radiographer
COVID-19 is the disease cause by infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1 The World Health Organisation (WHO) declared COVID-19 a global pandemic on 11 March 2020.2 Radiographers, patient facing, frontline health professionals, have a key role in the diagnosis and management of COVID-19. Diagnosis of SARS-CoV-2 is confirmed by reverse transcription polymerase chain reaction (RT-PCR) of nasopharyngeal swabs.3 However, sensitivity is variable reported to be 70%–90% on initial swab4 and 90% on second swab at 72 h.5
The British Society of Thoracic Imaging (BSTI) have developed a clinical decision support tool to aid clinicians, radiographers and radiologists when managing patients where COVID-19 is within the differential diagnosis – the chest radiograph (CXR) forms the bedrock of this tool.6 CXRs are a key diagnostic test when investigating patients with respiratory symptoms and are advocated as the first imaging examination in patients with suspected COVID-19. Mobile CXRs are an important diagnostic test in the evaluation of critically unwell patients, and in particular will have a role in minimising the transmission risk of SARS-CoV-2 associated with patient transfer. Baseline CXRs have a reported sensitivity of 69% compared to baseline RT-PCR thus far, but analysis has been lacking due to puzzlingly limited use of CXR in the outbreak to date.4
Preliminary clinical evaluation (PCE) by radiographers at time of image acquisition is an expected competency of practitioners in many regions including the United Kingdom7 and Australia.8 As radiographers are almost invariably the first practitioner to see the diagnostic image, it follows that radiographer PCE and triage for an immediate clinical report plays a vital role in identifying possible COVID-19 patients. There are increasing case reports of patients presenting to hospital without classical symptoms of COVID-19 (fever, cough), including abdominal symptoms,9 , 10 and may be referred for non-COVID diagnostic workup without respiratory precautions in place. Rapid radiographer PCE and triage will facilitate prompt reporting of the investigation, aid patient diagnosis and management decisions in a timely way. This rapid triage also allows for the potential of all imaging to be performed during a single hospital attendance and, more crucially, immediate appropriate decontamination of imaging equipment.
It is crucial that radiographers, radiologists and referring clinicians are aware that a normal imaging investigation (CXR or CT) does not exclude COVID-19 in high risk patients.4 Thus, a ‘completion’ chest CT to identify COVID-19 when the lung bases are normal on a routine CT abdomen in a patient who has no COVID-19 respiratory symptoms is not advocated. Also, personal protective equipment (PPE) and infection control precautions should continue, based on clinical suspicion. When imaging is abnormal, findings are frequently non-specific and need to be incorporated with the relevant clinical symptoms and findings on blood tests (most notably elevated C-reactive protein (CRP) and lymphopenia <1100 μ/L).6
This case report series presents a summary of key findings frequently associated with COVID-19 and will assist radiographer PCE. Chest imaging features associated with COVID-19 (ref BSTI reporting template) are presented in Table 1 .11
Table 1.
Chest imaging features associated with COVID-19.11
| COVID-19 | Imaging Features |
|---|---|
| Classic/Probable (>70% confidence) |
|
| Indeterminate (<70% confidence) | Does not fit into definite or probable or Non-COVID. |
| Normal |
|
| Non-COVID |
|
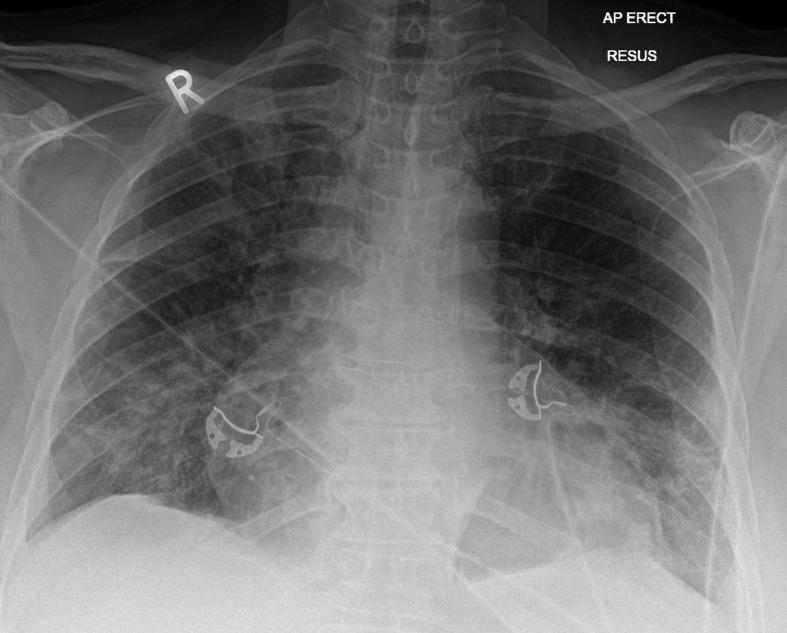
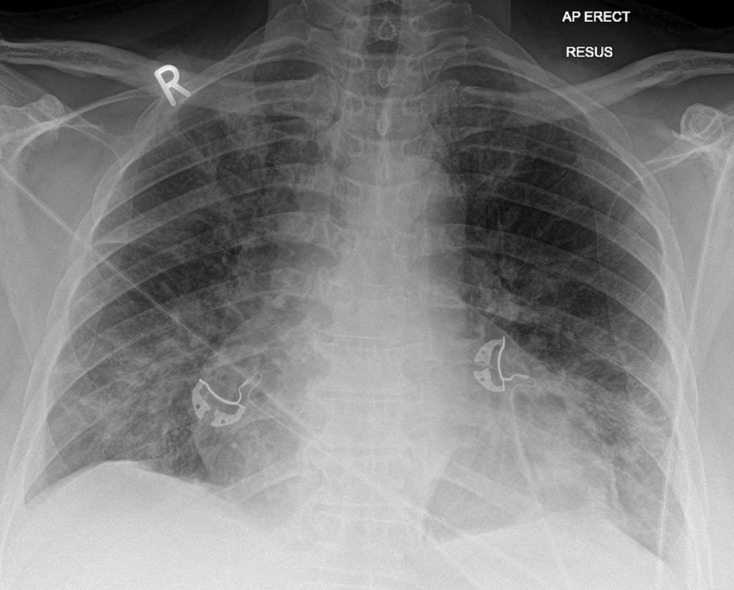
A 69-year-old female presented to the emergency department with a three-day history of fever (temperature 38.2 C) and shortness of breath (oxygen saturation 87%), normal white cell count (6400 μ/L) but lymphopenia (890 μ/L) and an elevated CRP (149, normal <5). Mobile chest radiograph (Fig. 1 ) demonstrates classical findings associated with COVID-19 of bilateral, predominantly peripheral lower zone ground glass and interstitial opacification. Nasopharyngeal swab RT-PCR was positive for SARS-CoV-2.
Figure 1.
Index chest radiograph of a 69 year old female with bilateral, peripheral ground glass and interstitial opacification (Classic/Probable COVID-19).
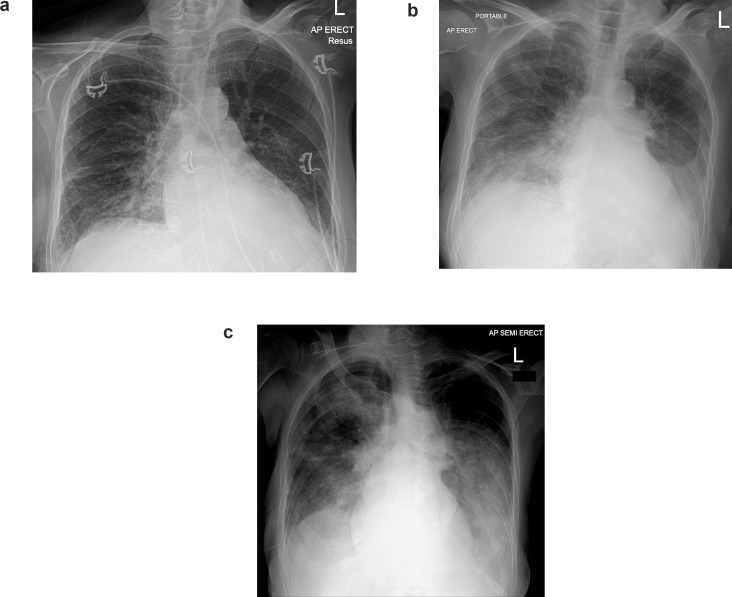
A 93-year-old female presented to the emergency department with a 10-day history of shortness of breath (oxygen saturation 66%), elevated CRP (71), normal white cell count (9500 μ/L) and lymphopenia (930 μ/L). Index (Day 0, Fig. 2 a) chest radiograph appearances were indeterminate with bilateral mid and lower zone interstitial opacification. Rapid progression occurred across seven days, with bilateral ground glass opacification (Fig. 2b) and development of acute respiratory distress syndrome (Fig. 2c). Nasopharyngeal swab RT-PCR was positive for SARS-CoV-2.
Figure 2.
a. Index chest radiograph (Day 0) with unilateral lower zone interstitial opacification (Indeterminate COVID-19). b. Repeat chest radiograph day 5 with bilateral ground glass opacification in the lower zones (Classic/Probable COVID-19). c. Repeat chest radiograph day 7 with diffuse bilateral ground glass opacification (Classic/Probable COVID).
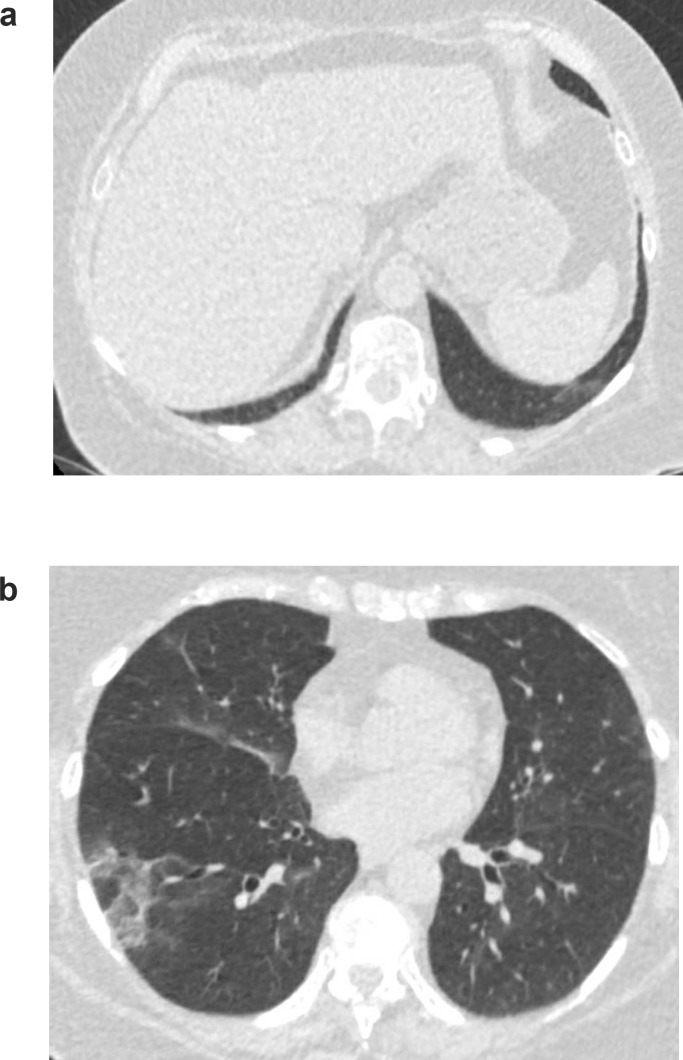
A 72-year-old male presented to the emergency department with a three-day history of right flank pain without dysuria and microscopic haematuria, temperature 37.1 C, oxygen saturation 98%, mildly elevated CRP,11 normal white cell count (4600 μ/L) and lymphocytes (1200 μ/L). A low dose CT abdomen was performed to investigate possible renal calculi. CT was negative for renal calculi however demonstrated subtle ground glass opacification of the left lower lobe (Fig. 3 a). CT chest was performed with peripheral ground glass opacification in the right upper lobe (Fig. 3b). Nasopharyngeal swab was not sent but the patient was given a clinical diagnosis of COVID-19.
Figure 3.
a. CT abdomen with left lower lobe ground glass opacification (Indeterminate COVID-19). b. CT chest with right upper lobe peripheral ground glass opacification (Indeterminate COVID-19). Clinico-radiological diagnosis of COVID-19, swab not sent.
Conflict of interest statement
Unrelated to the current submission, Dr Nick Woznitza is a clinical advisor to InHealth, Dr Arjun Nair reports, unrelated to the current submission, part funding from the UCL NIHR Biomedical Research Center, and a medical advisory role with Aidence BV, an artificial intelligence company.
References
- 1.Chung M., Bernheim A., Mei X., Zhang N., Huang M., Zeng X. CT imaging features of 2019 Novel Coronavirus (2019-nCoV) Radiology. 2020;295(1):202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. Word Health Organisation; 11 March 2020. [press release] [Google Scholar]
- 3.Inui S., Fujikawa A., Jitsu M., Kunishima N., Watanabe S., Suzuki Y. Chest CT findings in cases from the cruise ship “diamond princess” with coronavirus disease 2019 (COVID-19) Radiology: Cardiothoracic Imaging. 2020;2(2) doi: 10.1148/ryct.2020200110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wong H.Y.F., Lam H.Y.S., Fong A.H.-T., Leung S.T., Chin T.W.-Y., Lo C.S.Y. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology. 2020 doi: 10.1148/radiol.20202011606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fang Y., Zhang H., Xie J., Lin M., Ying L., Pang P. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020:200432. doi: 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rodrigues J.C.L., Hare S.S., Edey A., Devaraj A., Jacob J., Johnstone A. An update on COVID-19 for the radiologist - a British society of Thoracic Imaging statement. Clin Radiol. 2020 doi: 10.1016/j.crad.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Health and Care Professions Council . Health and Care Professions Council; London: 2013. Standards of proficiency: radiographers. [Google Scholar]
- 8.Medical Radiation Practice Board of Australia . Medical Radiation Practice Board of Australia; 2020. Professional capabilities for medical radiation practitioners. [Google Scholar]
- 9.Pan L., Yang P., Sun Y., Wang R., Yan J., Hu B. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020 doi: 10.14309/ajg.0000000000000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Song Y., Liu P., Shi X.L., Chu Y.L., Zhang J., Xia J. SARS-CoV-2 induced diarrhoea as onset symptom in patient with COVID-19. Gut. 2020 doi: 10.1136/gutjnl-2020-320891. [DOI] [PubMed] [Google Scholar]
- 11.British Society of Thoracic Imaging . British Society of Thoracic Imaging; 16 March 2020. Thoracic imaging in COVID-19 infection: guidance for the reporting radiologist.www.bsti.org.uk/media/resources/files/BSTI_COVID-19_Radiology_Guidance_version_2_16.03.20.pdf [Google Scholar]