Since the coronavirus 2019 (COVID-19) crisis broke out in Italy at the end of February 2020, days before the World Health Organization declared the pandemic,1 , 2 two crucial issues urgently emerged and needed to be addressed by our institution. First was the containment of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic together with the restructuring of national public and private health care to face the spread of the new viral disease among the population. Second, central as well, was to maintain the offer of medical and surgical treatments to the patients who still presented with other severe diseases—of these in particular, oncologic patients.
Our General University Hospital promptly started reorganizing facilities, keeping well in mind the second issue. The hospital management decided to change many divisions into COVID wards, leaving operational the thoracic oncology surgery division. The rationale was to keep working high-volume oncology surgery divisions concentrating all the oncologic patients undergoing surgery in well-established safe paths and protocols during the epidemic and pandemic. All the patients with lung or mediastinal cancer scheduled for operations received a thorough interview. Any clinical sign or symptom potentially related to COVID-19 disease was recorded. A meticulous history of what the patients did and who they met during the previous 15 days was obtained. A nasopharyngeal swab was offered to symptomatic patients or to those who reported clear contact with infected patients.
This policy avoided infected patients being admitted for intervention and likely helped the containment of the coronavirus epidemic by reporting the suspected COVID-19 patients to the health care authorities. All the physicians, residents, nurses, and patients carefully used and adopted individual protection devices and protocols, thereby allowing safe procedures, including bronchoscopy.
The second action was to reduce to a minimum the inpatient waiting list, to limit the risk of infection before the operation. The third action was to reduce the hospital stay and to establish virtual connection by electronic systems between patients and their relatives so to minimize any outside contact. Outpatient clinics have been reorganized and activity reduced to ensure minimal interaction among different patients and no additional risk for health care providers.
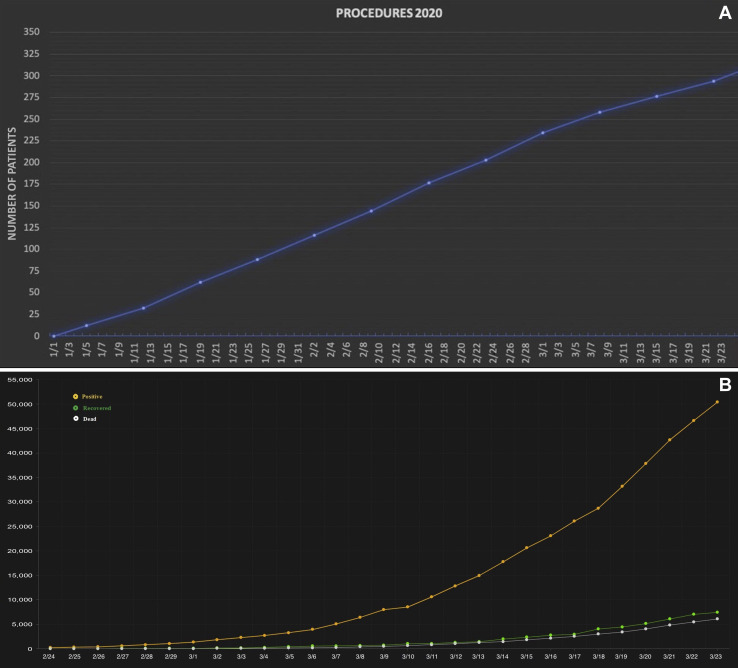
More than a month after the crisis erupted, these actions have allowed our institution to provide a high standard of care for our patients, with a reduction of only 22.4% of operative cases in this period in comparison with the same period last year. Indeed, in the first 3 months of 2020, we performed 305 major operations for thoracic malignancies (Table 1 ), with no further decreased trend immediately after the application of the novel internal working rules described (Figure 1 A), even though the number of COVID-19 patients in our country and in our district has been increasing,3 (Figure 1B). No patients converted to COVID positive during follow-up; moreover, we did not have any postoperative readmissions related to COVID-19.
Table 1.
Major Oncologic Operations for Malignancies Performed February 24, 2020, to March 24, 2020, at our Institution During COVID-19 Epidemic
| Operation | Patients |
|---|---|
| Lobectomy | 36 (38.7) |
| Sleeve resection | 4 (4.3) |
| Pneumonectomy | 3 (3.3) |
| Sublobar resection | 28 (30.1) |
| Mediastinal tumor resection | 10 (10.7) |
| Pleural tumor resection | 8 (8.6) |
| Chest wall tumor resection | 4 (4.3) |
| Total | 93 (100) |
Values are n (%).
Figure 1.
(A) Number of patients undergoing surgery for thoracic malignancies between January 1 and March 24, 2020, at our institution. (B) COVID-19 patients in Italy to March 23, 2020: number of patients who tested positive (yellow line); recovered (green line); or died (white line). Source: Dipartimento della Protezione Civile, Ministry of Health, Italian Government. Daily Bulletin. March 23, 2020.
Clear protocols and their scrupulous application can facilitate safe surgical treatments to patients with thoracic malignancy even during the darkest hours of our recent history. During a storm, we never forget to keep the bar straight.
Acknowledgments
The authors wish to thank all of their institution’s women and men who every day tirelessly make patients’ care possible at this difficult time.
References
- 1.World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19. March 11 2020. Available at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
- 2.Bedford J., Enria D., Giesecke J. for the WHO Strategic and Technical Advisory Group for Infectious Hazards. COVID-19: towards controlling of a pandemic. Lancet. 2020;395:1015–1017. doi: 10.1016/S0140-6736(20)30673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dipartimento della Protezione Civile Ministry of Health, Italian Government. Daily Bulletin. March 23, 2020 Available at: http://www.protezionecivile.gov.it/web/guest/media-communication/press-release/-/content-view/view/1236272. [Google Scholar]