The outbreak of novel coronavirus diseases (COVID-19) has been spreading rapidly and become a global pandemic (World Health Organization). COVID-19 patients present common cold symptoms, like fever, cough, and myalgia or fatigue at the onset of disease (Guan et al., 2020; Huang et al., 2020). Typically, pulmonary inflammation and compromised oxygen exchange in the infected cases can cause dyspnea or hypoxia, autopsy report of the non-survivors showed viscous secretions in respiratory tracts and air sacs of the lung (Liu et al., 2020; Xu et al., 2020). Hypoxia as an often seen problem is frequently accompanied by cellular glucose metabolism disorders (Hjalmarsen et al., 1996; Oltmanns et al., 2004). Indeed, a large proportion of the COVID-19 patients represent high blood lactate dehydrogenase (LDH) levels, concomitantly developing hyperglycemia and increased blood lactate concentrations along with the disease aggravation (Guan et al., 2020; Huang et al., 2020; Yang et al., 2020). Similar to severe acute respiratory syndrome (SARS) patients, high mortality and morbidity risks occurred in COVID-19 patients with the known history of diabetes (Yang et al., 2006; Guan et al., 2020). These evidences strongly suggest that the imbalance of glucose metabolism could be crucially involved in respiratory pathogenic virus infection, and high attention should be paid to rescue this process to prevent the further deterioration of COVID-19.
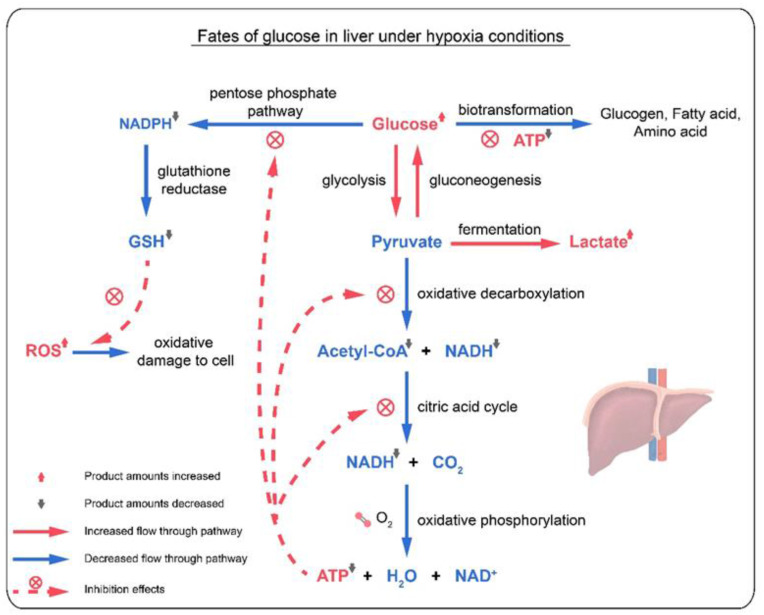
It is well known that glucose mainly goes through aerobic metabolism to yield substantial amount of adenosine triphosphate (ATP), providing essential energy for diverse biological processes (Nelson and Cox, 2016). Under aerobic condition, glucose can also be oxidized through pentose phosphate pathway, generating nicotinamide adenine dinucleotide phosphate (NADPH) to maintain the proper ratio of oxidized glutathione to glutathione (GSH), which works for the anti-oxidant defense system in the body and takes part in fighting against the invasive pathogenic microorganisms together with the immune system. Under anaerobic condition in COVID-19 patients, the pyruvate generated from glucose through glycolysis was fermented to lactate, which produces limited amount of adenosine triphosphate (ATP) for urgent biological needs in the body (Nelson and Cox, 2016). Meanwhile, the high replication of SARS-CoV-2 viruses in infected cells consumed large amount of cellular ATP, and further accelerated the anaerobic glycolysis process of the glucose, thus forming large amount of lactate. As the hypoxia and ATP depletion continued, lactate delivered to liver failed to be metabolized for gluconeogenesis or oxidized through citric acid cycle, thus causing the elevated blood lactate and LDH levels in COVID-19 patients. The insufficient ATP production under hypoxia state could greatly inhibit all ATP-consuming processes, including blood glucose uptake, pentose phosphate pathway, oxidative decarboxylation of pyruvate and citric acid cycle. ATP shortage might also accelerate the decomposition of hepatic glycogen to glucose, whereas glucose failed to be converted to amino acids or fatty acids. Therefore, the COVID-19 patients were likely to develop hyperglycemia under the persistent hypoxia state (Fig. 1 ). Additionally, the depletion of glutathione (GSH) from the blockage of pentose phosphate pathway could barely maintain the oxidative and anti-oxidative balance in the body, thus failing in attenuating oxidative damage induced by the invasion of SARS-CoV-2 viruses.
Fig. 1.
Glucose utilization under hypoxia condition in COVID-19 patients.
Majority of the COVID-19 patients in China have been cured following the ever-improving treatment methods, and oxygen supplement has been applied as a common treatment strategy for cases in hospitals and cabin hospitals (China National Health Commission). Since 81% of the confirmed cases are in mild condition with non- or mild pneumonia, most of COVID-19 patients outside China are now recommended for self-cured under home quarantine. However, it may only take 9 days for the mild COVID-19 patients without effective nursing to develop into serious or critical cases with acute respiratory distress syndrome (ARDS) (Guan et al., 2020; Huang et al., 2020). Therefore, it is critical to promote the self-cure rate of the mild cases and prevent the disease from deterioration. Considering the harmful consequences induced by hypoxemia and advantages of oxygen therapy in controlling glucose metabolism (Handy et al., 2005), we suggest that adequate oxygen intake is also essential for the newly confirmed or suspected cases under home quarantine.
To evaluate the effect of oxygen therapy and inspect changes of biochemical parameters involved in anaerobic glucose metabolism, we conducted a preliminary study on the clinical data of 65 COVID-19 cases from General Hospital of Chinese PLA Central Theater Command (Wuhan, China). For 23 severe cases with no oxygen supplement before hospital admission, high blood LDH levels (91.3%, >250 IU/L), hyperglycemia (56.5%, >7.1 mmol/L under fasting state) and high blood lactate levels (26.1%, >1.6 mmol/L in arterial blood, > 2.44 mmol/L in venous blood) were detected. As for another 42 mild cases at the hospital admission, the ratios of patients with hyperglycemia, high blood LDH and lactate levels were 21.4%, 30.9% and 2.4%, respectively. Oxygen therapy was continuously performed for these patients in the hospital, and 35 cases maintained stable health condition during 9-day treatment. Their average blood glucose and LDH concentrations were reduced from 6.24 mmol/L to 5.76 mmol/L, and from 238 IU/L to 192 IU/L, respectively. These data suggest that oxygen supplement at the earliest stage of COVID-19 could be favorable to correct the unbalanced glucose aerobic metabolism, regular monitoring of blood glucose using test strips are very promising in improving the recovery process and preventing the disease from deterioration.
Collectively, now COVID-19 is spreading very fast, and has become a global infectious disease, due to the high human transmission of SARS-CoV-2 (Chan et al., 2020). Though the majority had non-critical symptoms, the COVID-19 patients may have high risks in developing into critical cases without proper medical care. We strongly suggest that adequate oxygen intake and blood glucose monitoring should be introduced for patients under home quarantine to prevent further deterioration of the progressive COVID-19.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This work is supported by National Natural Science Foundation of China (21906069, 21876195 and 21477049).
References
- Chan J.F.W., Yuan S., Kok K.H. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- China National Health Commission Diagnosis and treatment standards for COVID-19. http://www.nhc.gov.cn/xcs/zhengcwj/list_gzbd.shtml
- Guan W., Ni Z., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2002032. Published on. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handy R.D., Bryson P., Moody A.J., Handy L.M., Sneyd J.R. Oxidative metabolism in platelets, platelet aggregation, and hematology in patients undergoing multiple hyperbaric oxygen exposures. Undersea Hyperb. Med. 2005;32(5):327–340. [PubMed] [Google Scholar]
- Hjalmarsen A., Aasebo U., Birkeland K., Sager G., Jorde R. Impaired glucose tolerance in patients with chronic hypoxic pulmonary disease. Diabetes Metab. 1996;22:37–42. [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q., Wang R.S., Qu G.Q. A report on the general observation of the necropsy for COVID-19 (in Chinese) J. Forensic Med. 2020;36(1):1–3. [Google Scholar]
- Nelson D.L., Cox M.M. seventh ed. 2016. Lehninger Principles of Biochemistry. Biochemistry and Molecular Biology Education. (Chapter 14) [Google Scholar]
- Oltmanns K.M., Gehring H., Rudolf S. Hypoxia causes glucose intolerance in humans. Am J Resp Crit Care. 2004;169(11):1231–1237. doi: 10.1164/rccm.200308-1200OC. [DOI] [PubMed] [Google Scholar]
- World Health Organization Coronavirus disease (COVID-2019) situation report-69. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
- Xu Z., Shi L., Wang Y.J. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30076-X. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J., Feng Y., Yuan M.Y. Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabet. Med. 2006;23(6):623–628. doi: 10.1111/j.1464-5491.2006.01861.x. [DOI] [PubMed] [Google Scholar]
- Yang X.B., Yu Y., Xu J.Q. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30079-5. Published Online. [DOI] [PMC free article] [PubMed] [Google Scholar]