Here, we present a patient with locally advanced NSCLC who had fatal coronavirus disease 2019.
In February 2020, a 74-year-old Caucasian man with 50 pack-years of smoking presented with fatigue, weight loss, and dyspnea. He was diagnosed with pulmonary adenocarcinoma cTNM stage T3N2M0. Comorbidities included hypertension and bilateral hip arthroplasty.
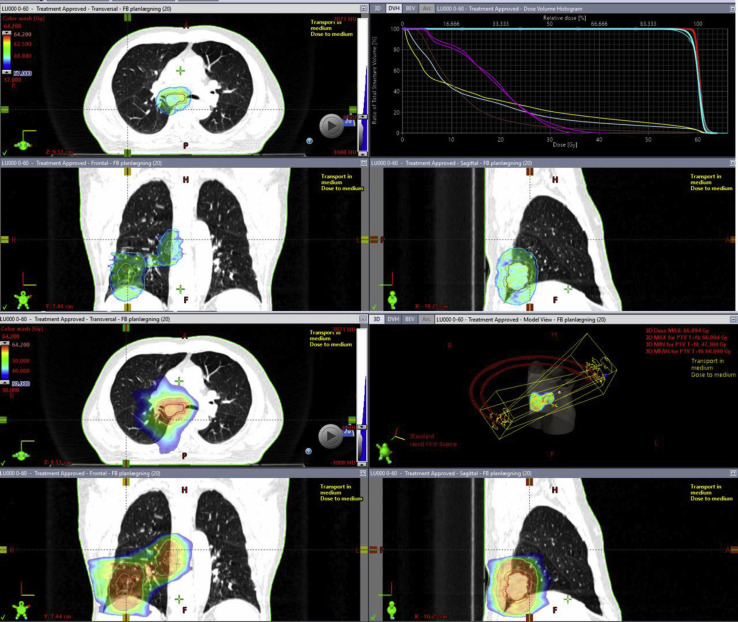
The patient was referred for chemoradiotherapy regimen of 60 Gy in 30 fractions (Fig. 1 ) with a total of three cycles of platinum-doublet chemotherapy.
Figure 1.
Radiotherapy treatment plan. The upper panels revealing the dose color wash in the range of 95% to 107% (i.e., 57–64.2 Gy), along with the dose volume histogram. Gross tumor volume is in red, clinical target volume in orange, planned target volume in cyan, lungs in light blue, heart in brown, esophagus in yellow, and spinal cord and spinal cord planning risk volume in magenta. The lower panels reveal dose color wash in the range of 50% to 107% (i.e., 30–64.2 Gy), along with the plan geometry with two half arcs for volumetric-modulated arc therapy treatment.
Clinical Course
In the evening after the ninth radiotherapy fraction, the patient had fever, dry cough, increased fatigue, and myalgia and was tested positive with severe acute respiratory syndrome coronavirus 2. He was discharged because of mild clinical symptoms. Owing to unknown severity of disease development, a radiotherapy treatment break was issued. The patient was monitored with daily telephone consultations, in which he reported fatigue and dry cough. Three days after testing positive, he had severe dyspnea and was admitted to the hospital. During the admission, he had severe hypoxia and was transferred to the intensive care unit for ventilator treatment (Fig. 2 ). Six days after the occurrence of the first symptoms, the patient died from respiratory failure.
Figure 2.
Chest radiograph on day 4 after severe acute respiratory syndrome coronavirus 2 diagnosis revealing progressive bilateral lung changes before rapid respiratory failure.
Imaging During Radiotherapy
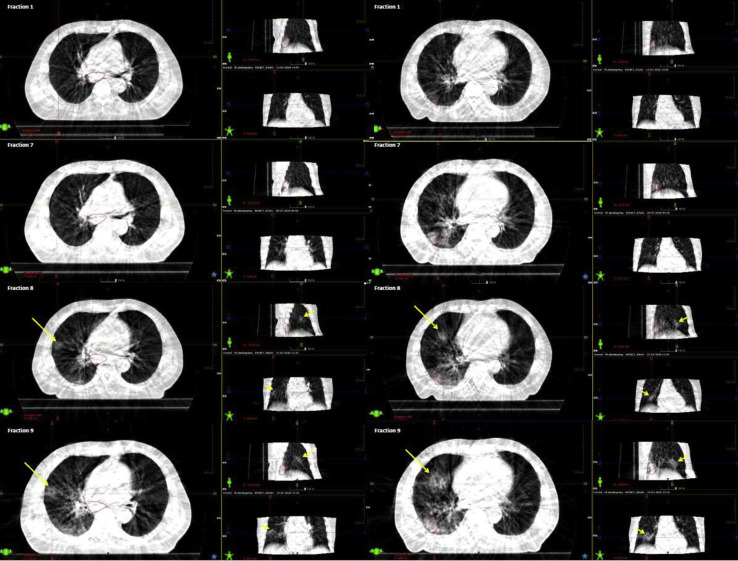
On retrospective workup, a senior radiologist assessed the daily-acquired cone beam computer tomography (CBCT). The CBCT acquired at the first treatment fraction revealed no new infiltrates in the lung tissue. Similar findings were found on the CBCT acquired at the seventh fraction. On the CBCT acquired at the eighth fraction, two ground-glass opacities (GGOs) with patchy consolidation were found, one in a subpleural location and one more centrally in the middle lobe. At ninth fraction, progression of the infiltrates in the middle lobe was observed, and one new GGO appeared in a subpleural location in the right upper lobe. These GGOs were, hence, visible on the CBCT images up to 36 hours before the patient exhibited the clinical symptoms of coronavirus disease 2019 (COVID-19) (Fig. 3 ).
Figure 3.
Daily imaging during radiotherapy: The cone beam computer tomographies taken as image guidance. Left and right panels focus on two different areas in the lungs that had changes in the lung tissue at treatment fractions 8 and 9. No changes in the lung tissue were detected on fraction 7; however, there was a 3-day interval between fraction 7 and 8 (i.e., the weekend).
Discussion
The epidemiology of COVID-19 highlights the problem with spread of severe acute respiratory syndrome coronavirus 2 before a patient becomes symptomatic. This increases the risk of exposure of treatment personnel and other patients undergoing radiotherapy before the symptom occurrence and referral for COVID testing. During the current pandemic situation, the CBCT images, often acquired daily, may provide additional information on changes in the lung tissue, despite the impaired image quality compared with the diagnostic CT.1 , 2 Early identification of changes in the pulmonary tissue has been reported to lead toward improved prognosis in patients with COVID-19.3 Despite poorer image quality in the thoracic CBCT, we were retrospectively able to identify changes in the lung tissue before the patient exhibited the clinical COVID-19 symptoms. Staff in radiotherapy departments can immediately prioritize review of daily CBCT or kilovoltage images for the presence of lung tissue density as potential harbingers for COVID infection. Observation of new patchy infiltrates may be an early signal supporting COVID-19 testing, which would expedite patient management and timely use of appropriate personal protective equipment by clinic staff. The consequences of continuation of radiotherapy in patients positive for COVID-19 are unknown.
Footnotes
Disclosure: Dr. Josipovic reports grants from Varian Medical Systems and personal fees from Siemens Healthcare outside the submitted work. The remaining authors declare no conflict of interest.
References
- 1.Bissonnette J.P., Balter P.A., Dong L. Quality assurance for image-guided radiation therapy utilizing CT-based technologies: a report of the AAPM TG-179. Med Phys. 2012;39:1946–1963. doi: 10.1118/1.3690466. [DOI] [PubMed] [Google Scholar]
- 2.Song J.Y., Nam T.K., Ahn S.J., Chung W.K., Yoon M.S., Nah B.S. Respiratory motional effect on cone-beam CT in lung radiation surgery. Med Dosim. 2009;34:117–125. doi: 10.1016/j.meddos.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 3.Huang G., Gong T., Wang G. Timely diagnosis and treatment shortens the time to resolution of coronavirus disease (COVID-19) pneumonia and lowers the highest and last CT scores from sequential chest CT. AJR Am J Roentgenol. 2020;200:1–7. doi: 10.2214/AJR.20.23078. [DOI] [PubMed] [Google Scholar]