Abstract
Nitrogen dioxide (NO2) is an ambient trace-gas result of both natural and anthropogenic processes. Long-term exposure to NO2 may cause a wide spectrum of severe health problems such as hypertension, diabetes, heart and cardiovascular diseases and even death. The objective of this study is to examine the relationship between long-term exposure to NO2 and coronavirus fatality. The Sentinel-5P is used for mapping the tropospheric NO2 distribution and the NCEP/NCAR reanalysis for evaluating the atmospheric capability to disperse the pollution. The spatial analysis has been conducted on a regional scale and combined with the number of death cases taken from 66 administrative regions in Italy, Spain, France and Germany. Results show that out of the 4443 fatality cases, 3487 (78%) were in five regions located in north Italy and central Spain. Additionally, the same five regions show the highest NO2 concentrations combined with downwards airflow which prevent an efficient dispersion of air pollution. These results indicate that the long-term exposure to this pollutant may be one of the most important contributors to fatality caused by the COVID-19 virus in these regions and maybe across the whole world.
Keywords: COVID-19, Coronavirus, Nitrogen dioxide (NO2), Sentinel-5P
Graphical abstract
1. Introduction
The outbreak of the novel coronavirus (COVID-19) is an ongoing global epidemic event which started in the city of Wuhan, China in late 2019. By March 2020 the virus has spread globally and was declared as pandemic by the World Health Organization (World Health Organization, 2020). COVID-19 is an acute respiratory disease which may lead to pneumonia with symptoms such as fever, cough and dyspnea (Jiang et al., 2020) and has an approximate fatality rate of 2–3% (Rodriguez-Morales et al., 2020). As of March 19, 2020, there have been 209,839 confirmed cases and 8788 deaths reported globally. Early studies concluded that the risk factors associated with the development of the disease are older age (Wu et al., 2020), history of smoking (Liu et al., 2020), hypertension and heart disease (Chen et al., 2020). The Italian institute of health (Istituto Superiore di Sanità) reported background diseases of 481 patients in Italy who passed away due to COVID-19 infection. Table 1 shows the information about the most common background diseases which are evident in over 20% of the cases. Furthermore, recent studies suggest that the cause of death of many COVID-19 patients was related to cytokine storm syndrome (Guo et al., 2020; Mehta et al., 2020). This syndrome, also known as hypercytokinemia is an uncontrolled release of proinflammatory cytokines (Tisoncik et al., 2012) and it is a severe reaction of the immune system, leading to a chain of destructive processes in the body that can end in death.
Table 1.
The most common background diseases evident in over 20% of the cases.
| Disease | % of patients |
|---|---|
| Hypertension | 73.8 |
| Diabetes | 33.9 |
| Ischemic heart diseases | 30.1 |
| Atrial fibrillation | 22.0 |
| Chronic renal failure | 20.2 |
Many studies have shown that the incidence of these diseases can also be caused by a long exposure to air pollution, especially nitrogen dioxide (NO2), a toxic component. NO2 enters the atmosphere as a result of anthropogenic activity (mostly fossil fuel combustion from vehicles and power plants) and natural processes (lightning and soil processes). Elevated exposure to NO2 has been associated with hypertension (Saeha et al., 2020), heart and cardiovascular diseases (Gan et al., 2012; Mann Jennifer et al., 2002; Arden et al., 2004), increased rate of hospitalization (Mann Jennifer et al., 2002), chronic obstructive pulmonary disease (COPD) (De et al., 1993; Euler et al., 1988), significant deficits in growth of lung function in children (Avol et al., 2001; James Gauderman et al., 2000), poor lung function in adults or lung injury (Bowatte et al., 2017; Rubenfeld et al., 2005) and diabetes (Saeha et al., 2020). In addition to these, other studies have focused on the immune system's response to NO2 exposure. Blomberg et al., 1999, found that exposure to NO2 causes an inflammatory response in the airways and Devalia et al., 1993, showed that these exposures may induce the synthesis of proinflammatory cytokines from airway epithelial cells which consequently play an important role in the etiology (cause) of airway disease. Moreover, the epithelial cells in the lung may be uniquely susceptible to death when exposed to NO2 (Persinger et al., 2002).
High NO2 concentration is significantly associated with respiratory mortality (Beelen et al., 2008; Chen et al., 2007; Hoek et al., 2013) and is also responsible for generating some harmful secondary pollutants such as nitric acid (HNO3) and ozone (O3) (Khoder, 2002). As a result, the WHO has stated that the health risks may potentially occur due to the presence of NO2 or its secondary products (World Health Organization, 2003). Accordingly, the WHO understands the health issues arising from NO2 and suggests that the world population should be protected from exposure to this pollutant.
The objective of this work is to assess the contribution of a long-term exposure to NO2 on coronavirus fatality. This is achieved by combining three databases: the tropospheric concentration of NO2, the atmospheric condition as expressed by the vertical airflow, and the number of fatality cases. The data is processed at the administrative level for each country to obtain high spatial resolution.
2. Materials and methods
2.1. Fatality database
The data concerning the number of fatality cases was collected from each country on a regional/administrative level. The use of this method is intended to highlight the spatial variation of the epidemic which exists not only between different countries, but more importantly within each country. Moreover, if high mortality rates are observed in two remote regions in two different countries, we need to identify their common factor which may explain mortality. For that, data was collected from 66 administrative regions in Italy, Spain, France and Germany. Information about fatalities was taken from the Ministry of Health (Italy), Ministry of Health, Social Services and Equality (Spain), The National Agency of Public Health (France) and the Robert-Koch-Institute and the State Health Offices (Germany).
2.2. The NO2 spatial distribution
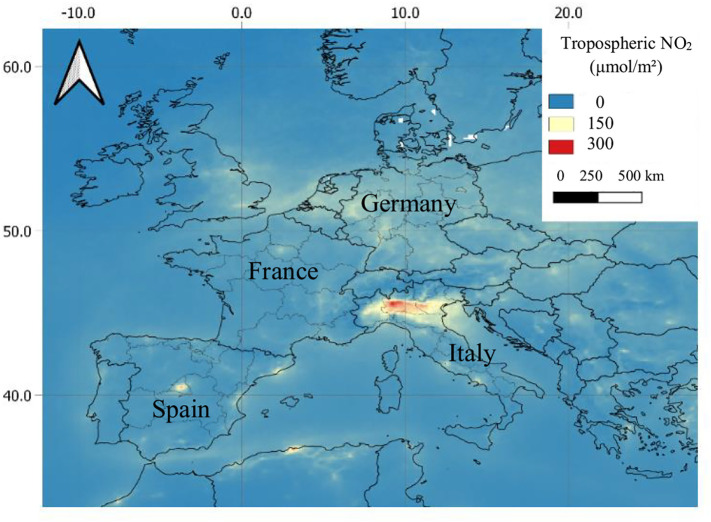
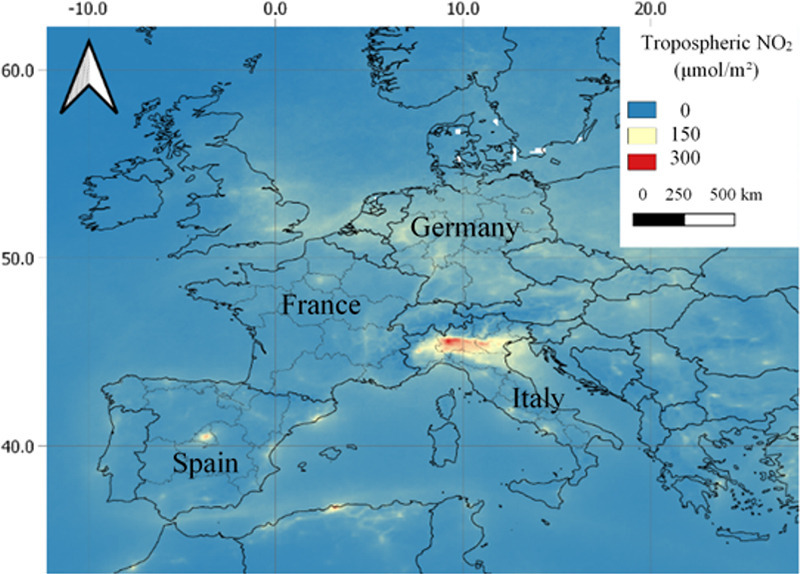
For the NO2 concentration in the troposphere (from surface up to ~10 km), the Sentinel-5 Precursor space-borne satellite (spatial resolution of 5.5 km) was used which is operated and managed by the European Commission under the “Copernicus” program (Fig. 1 ). The satellite operates in a sun-synchronous orbit at 824 km and an orbital cycle of 16 days. The satellite carries a TROPOspheric Monitoring Instrument (TROPOMI) which provides a (near-)global coverage of air pollution caused by NO2 and other pollutants such as O3, SO2, CO, CH4, CH2O and aerosols (Veefkind et al., 2012).
Fig. 1.
The tropospheric NO2 distribution.
For this study, long-term exposure was defined as a two-month period (January–February 2020) prior to the outbreak of COVID-19 in Europe. The spatial data was collected using the Google Earth Engine API (Gorelick et al., 2017). The global coverage of tropospheric NO2 for this time period was extracted using 832 different images followed by calculating the mean concentration for each administrative region. Subsequently, only the maximum concentration value was used due to differences in the size of the regions.
2.3. The atmospheric condition
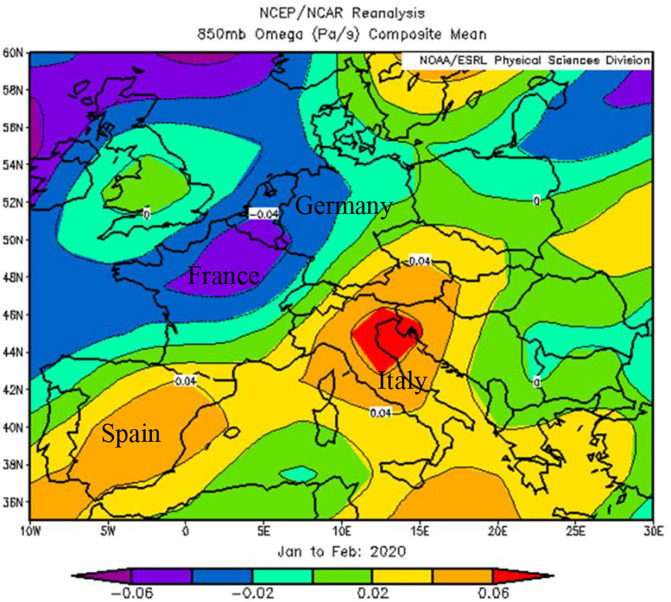
Due to the thickness of the troposphere, the value which represents the NO2 concentration is not enough. There is also a need to understand the vertical airflow during the same period of the event. For that purpose, the vertical airflows at 850 mb (~1.5 km above sea level) was used as it defines the atmospheric capability to disperse the gas (Fig. 2 ). This data was provided by the NOAA/OAR/ESRL PSD, Boulder, Colorado, USA (http://www.esrl.noaa.gov/psd/). Downwards airflows are given by positive values of omega (in Pa/s), while upwards airflow by negative values of omega. In regions where positive omega is observed, the atmospheric will force the NO2 to stay close to the surface which leads the population to be exposed to the risk factor. In contrast, in regions with negative omega, the atmospheric conditions will disperse the gas further away and to higher altitudes. In these regions, the population is less exposed to the air pollution and to its associated health risks.
Fig. 2.
The vertical airflow (omega) at 850 mb (~1500 m above sea level).
3. Results
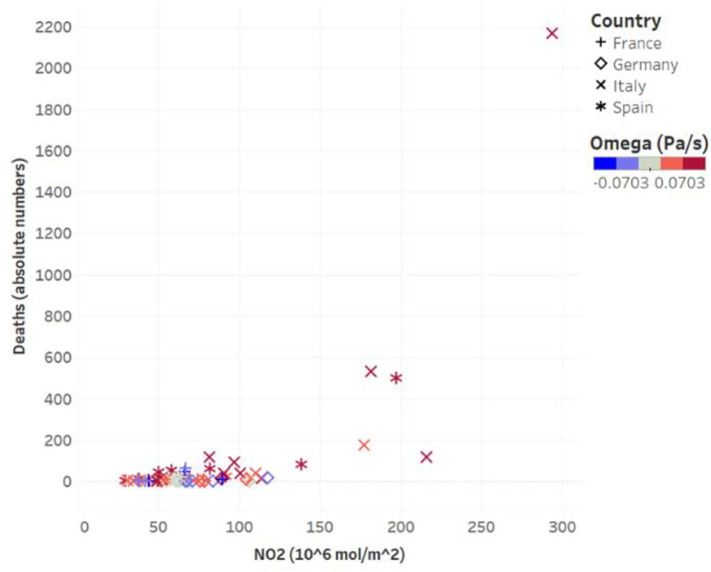
Mapping the tropospheric NO2 over Europe reveals a major ‘hotspot’ of high concentration in the northern part of Italy. The ‘hotspot’ is observed in the Po valley which extends from the slopes of the western Alps to the coastal plains of the Adriatic Sea. Out of the top five regions where high fatality was observed, four of them were in northern Italy (Fig. 3 ): Lombardia, (2168 cases), Emilia-Romanga (531), Piemonte (175 cases) and Veneto (115 cases). The other region was in the administrative region ‘Community of Madrid’ (Comunidad de Madrid), Spain (498 cases) which, like the Po valley, is also surrounded by mountain ranges.
Fig. 3.
NO2 vs. the absolute number of death cases.
As shown in Fig. 4 , 78% of all fatalities due to coronavirus in these selected countries occurred in those regions. The concentrations of NO2 were high and ranged between 177.1 and 293.7 μmol/m2, accompanied by downwards airflows (positive omega ranged between 0.04 and 0.07 Pa/s).
Fig. 4.
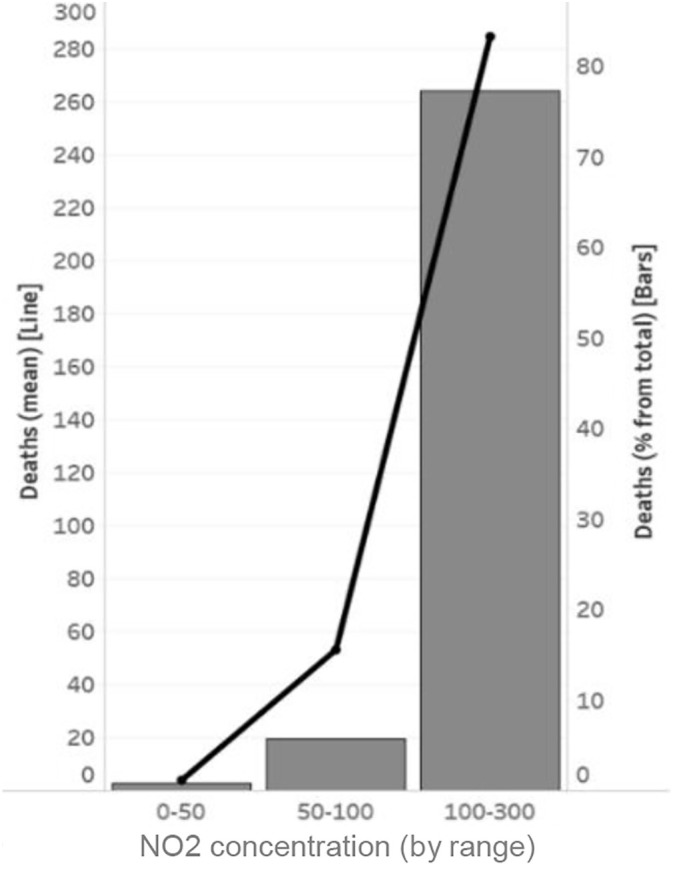
The mean death cases and the percentage of deaths in each NO2 concentration range.
There were 4443 fatalities in these countries due to COVID-19 by March 19, 2020. 83% of all fatalities (3701 cases) occurred in regions where the maximum NO2 concentration was above 100 μmol/m2, 15.5% (691 cases) occurred in regions where the maximum NO2 concentration was between 50 and 100 μmol/m2, and only 1.5% of all fatalities (51 cases) occurred in regions where the maximum NO2 concentration was below 50 μmol/m2.
4. Discussion and conclusion
In this study, the concentrations of the tropospheric NO2 which were extracted from the Sentinel-5P satellite were used in order to explain the spatial variation of fatality cases in 66 administrative regions in four European countries. The Sentinel-5P data shows two main NO2 hotspots over Europe: Northern Italy and Madrid metropolitan area. According to these results, high NO2 concentration accompanied by downwards airflows cause of NO2 buildup close to the surface. This topographic structure combined with atmospheric conditions of inversion (positive omega) prevent the dispersion of air pollutants, which can cause a high incidence of respiratory problems and inflammation in the local population. This chronic exposure could be an important contributor to the high COVID-19 fatality rates observed in these regions. As earlier studies have shown that exposure to NO2 causes inflammatory in the lungs, it is now necessary to examine whether the presence of an initial inflammatory condition is related to the response of the immune system to the coronavirus. Hence, poisoning our environment means poisoning our own body and when it experiences a chronic respiratory stress, its ability to defend itself from infections is limited.
According to these results, more studies should be conducted which focus on additional factors such as age and presence of pre-existing and background diseases along with the impact of pre-exposure to NO2 and hypercytokinemia in order to verify their impact on fatalities due to the COVID-19 pandemic.
Declaration of competing interest
The author declares no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
I wish to thank Prof. Michael Hopp for his assistance with the drafting and Prof. Hadas Saaroni for her assistance with the analysis of the atmospheric data. Prof. Hopp and Prof. Saaroni are faculty members in the Department of Geography and the Human Environment at Tel-Aviv University. None of these individuals received compensation for their contributions.
Editor: Jay Gan
References
- Arden Pope C., Burnett Richard T., Thurston George D., Thun Michael J., Calle Eugenia E., Daniel Krewski, Godleski John J. Cardiovascular mortality and long-term exposure to particulate air pollution. Circulation. 2004;109:71–77. doi: 10.1161/01.CIR.0000108927.80044.7F. [DOI] [PubMed] [Google Scholar]
- Avol E.L., Gauderman W.J., Tan S.M., London S.J., Peters J.M. Respiratory effects of relocating to areas of differing air pollution levels. Am. J. Respir. Crit. Care Med. 2001;164:2067–2072. doi: 10.1164/ajrccm.164.11.2102005. [DOI] [PubMed] [Google Scholar]
- Beelen Rob, Hoek Gerard, van den Brandt Piet A., Goldbohm R. Alexandra, Fischer Paul, Schouten Leo J., Jerrett Michael, Hughes Edward, Armstrong Ben, Brunekreef Bert. Long-term effects of traffic-related AIR pollution on mortality in a Dutch cohort (NLCS-AIR study) Environ. Health Perspect. 2008;116:196–202. doi: 10.1289/ehp.10767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blomberg A., Krishna M.T., Helleday R., Söderberg M., Ledin M.-C., Kelly F.J., Frew A.J., Holgate S.T., Sandström T. Persistent airway inflammation but accommodated antioxidant and lung function responses after repeated daily exposure to nitrogen dioxide. Am. J. Respir. Crit. Care Med. 1999;159:536–543. doi: 10.1164/ajrccm.159.2.9711068. [DOI] [PubMed] [Google Scholar]
- Bowatte G., Erbas B., Lodge C.J., Knibbs L.D., Gurrin L.C., Marks G.B., Thomas P.S., Johns D.P., Giles G.G., Hui J. Traffic-related air pollution exposure over a 5-year period is associated with increased risk of asthma and poor lung function in middle age. Eur. Respir. J. 2017;50 doi: 10.1183/13993003.02357-2016. [DOI] [PubMed] [Google Scholar]
- Chen T.-M., Kuschner W.G., Gokhale J., Shofer S. Outdoor air pollution: nitrogen dioxide, sulfur dioxide, and carbon monoxide health effects. Am J Med Sci. 2007;333:249–256. doi: 10.1097/MAJ.0b013e31803b900f. [DOI] [PubMed] [Google Scholar]
- Chen M., Fan Y., Wu X., Zhang L., Guo T., Deng K., Cao J., Luo H., He T., Gong Y. Social Science Research Network; Rochester, NY: 2020. Clinical Characteristics and Risk Factors for Fatal Outcome in Patients With 2019-Coronavirus Infected Disease (COVID-19) in Wuhan, China. [Google Scholar]
- De A., Sd C., Pk M., R B., Wl B., Y T. Chronic disease associated with long-term concentrations of nitrogen dioxide. J. Expo. Anal. Environ. Epidemiol. 1993;3:181–202. [PubMed] [Google Scholar]
- Devalia J.L., Campbell A.M., Sapsford R.J., Rusznak C., Quint D., Godard P., Bousquet J., Davies R.J. Effect of nitrogen dioxide on synthesis of inflammatory cytokines expressed by human bronchial epithelial cells in vitro. Am. J. Respir. Cell Mol. Biol. 1993;9:271–278. doi: 10.1165/ajrcmb/9.3.271. [DOI] [PubMed] [Google Scholar]
- Euler G.L., Abbey D.E., Hodgkin J.E., Magie A.R. Chronic obstructive pulmonary disease symptom effects of long-term cumulative exposure to ambient levels of total oxidants and nitrogen dioxide in California Seventh-day Adventist residents. Arch. Environ. Health Int. J. 1988;43:279–285. doi: 10.1080/00039896.1988.10545950. [DOI] [PubMed] [Google Scholar]
- Gan W.Q., Davies H.W., Koehoorn M., Brauer M. Association of long-term exposure to community noise and traffic-related air pollution with coronary heart disease mortality. Am. J. Epidemiol. 2012;175:898–906. doi: 10.1093/aje/kwr424. [DOI] [PubMed] [Google Scholar]
- Gorelick N., Hancher M., Dixon M., Ilyushchenko S., Thau D., Moore R. Google Earth Engine: planetary-scale geospatial analysis for everyone. Remote Sens. Environ. 2017;202:18–27. [Google Scholar]
- Guo Y.-R., Cao Q.-D., Hong Z.-S., Tan Y.-Y., Chen S.-D., Jin H.-J., Tan K.-S., Wang D.-Y., Yan Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak – an update on the status. Mil. Med. Res. 2020;7:11. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoek G., Krishnan R.M., Beelen R., Peters A., Ostro B., Brunekreef B., Kaufman J.D. Long-term air pollution exposure and cardio- respiratory mortality: a review. Environ. Health. 2013;12:43. doi: 10.1186/1476-069X-12-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James Gauderman W., McCONNELL R., Gilliland F., London S., Thomas D., Avol E., Vora H., Berhane K., Rappaport E.B., Lurmann F. Association between air pollution and lung function growth in southern California children. Am. J. Respir. Crit. Care Med. 2000;162:1383–1390. doi: 10.1164/ajrccm.162.4.9909096. [DOI] [PubMed] [Google Scholar]
- Jiang F., Deng L., Zhang L., Cai Y., Cheung C.W., Xia Z. Review of the clinical characteristics of coronavirus disease 2019 (COVID-19) J. Gen. Intern. Med. 2020 doi: 10.1007/s11606-020-05762-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoder M.I. Atmospheric conversion of sulfur dioxide to particulate sulfate and nitrogen dioxide to particulate nitrate and gaseous nitric acid in an urban area. Chemosphere. 2002;49:675–684. doi: 10.1016/s0045-6535(02)00391-0. [DOI] [PubMed] [Google Scholar]
- Liu W., Tao Z.-W., Lei W., Ming-Li Y., Kui L., Ling Z., Shuang W., Yan D., Jing L., Liu H.-G. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin. Med. J. 2020 doi: 10.1097/CM9.0000000000000775. (Publish Ahead of Print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann Jennifer K., Tager Ira B., Fred Lurmann, Mark Segal, Quesenberry Charles P., Lugg Marlene M., Jun Shan, Van Den Eeden Stephen K. Air pollution and hospital admissions for ischemic heart disease in persons with congestive heart failure or arrhythmia. Environ. Health Perspect. 2002;110:1247–1252. doi: 10.1289/ehp.021101247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta P., McAuley D.F., Brown M., Sanchez E., Tattersall R.S., Manson J.J. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persinger R.L., Poynter M.E., Ckless K., Janssen-Heininger Y.M.W. Molecular mechanisms of nitrogen dioxide induced epithelial injury in the lung. Mol. Cell. Biochem. 2002;234:71–80. [PubMed] [Google Scholar]
- Rodriguez-Morales A.J., Bonilla-Aldana D.K., Tiwari R., Sah R., Rabaan A.A., Dhama K. COVID-19, an emerging coronavirus infection: current scenario and recent developments – an overview. J. Pure Appl. Microbiol. 2020;9 [Google Scholar]
- Rubenfeld G.D., Caldwell E., Peabody E., Weaver J., Martin D.P., Neff M., Stern E.J., Hudson L.D. Incidence and outcomes of acute lung injury. N. Engl. J. Med. 2005;353:1685–1693. doi: 10.1056/NEJMoa050333. [DOI] [PubMed] [Google Scholar]
- Saeha Shin, Li Bai, Oiamo Tor H., Burnett Richard T., Scott Weichenthal, Michael Jerrett, Kwong Jeffrey C., Goldberg Mark S., Ray Copes, Alexander Kopp. Association between road traffic noise and incidence of diabetes mellitus and hypertension in Toronto, Canada: a population-based cohort study. J. Am. Heart Assoc. 2020;9 doi: 10.1161/JAHA.119.013021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tisoncik J.R., Korth M.J., Simmons C.P., Farrar J., Martin T.R., Katze M.G. Into the eye of the cytokine storm. Microbiol. Mol. Biol. Rev. 2012;76:16–32. doi: 10.1128/MMBR.05015-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veefkind J.P., Aben I., McMullan K., Förster H., de Vries J., Otter G., Claas J., Eskes H.J., de Haan J.F., Kleipool Q. TROPOMI on the ESA Sentinel-5 Precursor: a GMES mission for global observations of the atmospheric composition for climate, air quality and ozone layer applications. Remote Sens. Environ. 2012;120:70–83. [Google Scholar]
- World Health Organization . 2003. Health Aspects of Air Pollution With Particulate Matter, Ozone and Nitrogen Dioxide: Report on a WHO Working Group, Bonn, Germany 13–15 January 2003. [Google Scholar]
- World Health Organization Coronavirus disease 2019 (COVID-19) situation report – 51. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
- Wu C., Chen X., Cai Y., Xia J., Zhou X., Xu S., Huang H., Zhang L., Zhou X., Du C. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern. Med. 2020 doi: 10.1001/jamainternmed.2020.0994. Published online March 13, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]