Abstract
Public health emergencies have the potential to place enormous strain on health systems. The current pandemic of the novel 2019 coronavirus disease has required hospitals in numerous countries to expand their surge capacity to meet the needs of patients with critical illness. When even surge capacity is exceeded, however, principles of critical care triage may be needed as a means to allocate scarce resources, such as mechanical ventilators or key medications. The goal of a triage system is to direct limited resources towards patients most likely to benefit from them. Implementing a triage system requires careful coordination between clinicians, health systems, local and regional governments, and the public, with a goal of transparency to maintain trust. We discuss the principles of tertiary triage and methods for implementing such a system, emphasizing that these systems should serve only as a last resort. Even under triage, we must uphold our obligation to care for all patients as best possible under difficult circumstances.
Key Words: COVID-19 pandemic, disaster preparedness, scarcity of resources, surge capacity, triage
Abbreviations: COVID-19, novel 2019 coronavirus disease; HCW, health-care worker; PPE, personal protective equipment; SARS-CoV-2, severe acute respiratory syndrome coronavirus-2; SOFA, Sequential Organ Failure Assessment
Perspective
The current pandemic of the novel 2019 coronavirus disease (COVID-19) because of the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has led to a substantial increase in the demands on acute and critical care services in hospitals around the world. Even modest numbers of critically ill patients with COVID-19 are rapidly exceeding existing hospital capacity. Although a minor or moderate surge can be accommodated by using conventional and contingency surge strategies such as conserving, substituting, adapting, and reusing existing resources, current experiences from other countries managing COVID-19 suggest that the magnitude of the surge will substantially exceed capacity, necessitating a crisis surge response.1, 2, 3, 4 The clinical demands will exceed the ability to provide one or more crucial resources essential to deliver basic critical care, therefore necessitating decisions regarding the reallocation of resources. This potential requires preparation of a triage system to best allocate available critical care resources to meet severe surge to maximize benefit for the greatest number of people.4 , 5 Importantly, this triage system should only be deployed as a last resort and implemented as resources become limited and after all attempts to surge, move patients, or shift resources from regions with greater availability have been made.
When implemented, triage must be applied to all current and new patients presenting with critical illness, regardless of the diagnosis of COVID-19 or another illness, while maintaining underlying ethical principles of social justice, beneficence, nonmaleficence, respect for people and their dignity, veracity and the need to uphold trust within society, and fidelity to one another within health systems. We must uphold our duty to care for all patients, even those unable to receive critical care interventions. To enact this triage plan, a triage decision support protocol, infrastructure, processes, legal and regulatory protections, and training5 are required, all of which are currently lacking in most institutions and regions.
Additionally, there is a need to ensure that patients who do not initially receive critical care resources are still provided the best supportive care possible and are reevaluated, at minimum daily, for consideration of resource allocation as supplies become available. This will result in a sliding scale from crisis to contingency, and flexibility should be anticipated. The absence of a triage system, consistently applied within and between hospitals, may lead to unnecessary deaths, increased moral distress for frontline physicians, and a lack of public confidence in the fairness of scarce resource allocation. It is important to recognize that the initiation of adult triage levels does not itself imply initiation of pediatric triage (or vice versa). However, dependent on the level of impact within the pediatric system, pediatric hospitals will need to consider lower-level triage initiation at a point when adult systems have reached crisis triage, to respect the principles of utility and fairness population-wide.
With appropriate critical care surge planning, we hope that the use of a triage plan that limits the delivery of critical care should be rare, but the potential consequences of failing to prepare for this eventuality are serious.
Table 1 provides operational steps to implement a triage system within a state, county, or jurisdiction and highlights respective stakeholder responsibilities.
Table 1.
Operational Steps to Implement a Triage System
| Specific Actions Suggested | Stakeholders Responsible |
|---|---|
1. Inventory of potential ICU resources for a surge in demand
|
Individual health-care facilities |
2. Establish identification triggers for and initiation of triage: as clinical demand reaches crisis stage and that crisis standards of care, including triage, should be initiated
|
Regional government health authorities (county/state/province/national) Regional or national emergency management authorities (eg, CDC or equivalent, state/province public health department) |
3. Preparation of a triage system
|
Public health department/ministry of health Local hospitals with an ICU |
| 4. Agreement on a triage protocol to target resources to those with the greatest incremental benefit | Regional health authorities and coalitions Critical care professional societies and community, along with multistakeholder input |
5. Consideration of changes to allow limits to the delivery of life-sustaining measures in times of crisis care, and indemnity against litigation for decisions made in accordance with the triage policy
|
Regional health authority (ie, state health commissioner, provincial health minister) Regional justice authority (ie, attorney general, governor) |
6. Standards of care
|
State/provincial physician licensing board Critical care/palliative care community |
7. Family and societal support
|
Institutional social work, mental health, and palliative care services Consideration of COVID-19 hospice services |
8. Health-care worker support
|
Regional health authorities and attorney general, in collaboration with regional critical care leaders and ICU directors Individual institutions |
9. Pediatric considerations
|
Local health-care coalitions |
CDC = Centers for Disease Control and Prevention; COVID-19 = novel 2019 coronavirus disease; OR = operating room; PACU = post-anesthesia care unit; PPE = personal protective equipment.
Justification/Rationale
Surge Planning
COVID-19 is caused by a novel coronavirus that can cause severe acute respiratory illness. Early experience with the virus in China and Italy suggests that the virus has a community symptomatic attack rate of COVID-19 of up to 30% (with approximately double that number of SARS-CoV-2 infections because up to one-half of cases appear to be asymptomatic or paucisymptomatic). Of these, as many as 5% to 25% may require hospital admission, 5% to 8% may require ICU admission, and 2% to 4% may require mechanical ventilation for acute respiratory failure. For example, in the greater New York City metropolitan area alone (with a population of 8.4 million people), a community attack rate of 35% (ie, a symptomatic attack rate of 17.5%), leading to 1.3 million people with varying levels of disease from now until midsummer, could generate approximately 88,000 total hospitalizations and 13,000 ICU admissions under a scenario in which 7% of all affected people require hospitalization and 14% of those require critical care beds. Under a more severe scenario (20% hospitalized and 24% to ICU, rates now seen during the week of March 23, 2020, at New York City hospitals), this could lead to up to 190,000 hospitalizations and 58,000 ICU admissions over the course of the pandemic, with a peak concurrent ICU census of approximately 22,000 before summer. At baseline, the United States has approximately 68,000 adult and 5,000 PICU beds, a per capita ICU bed availability that exceeds most other countries.6 Clearly, either scenario is likely to vastly overwhelm any current health system, as is occurring in Italy and elsewhere.
Triage is the course of action that we take when we have exhausted our ability to expand our critical care resources, that is, to surge. Surge capacity refers to the ability of a hospital or other health-care system to expand its normal operating capacity in the setting of an emergency. Surge capacity includes the key features of staff, space, supplies, and systems with communications as a critical fifth feature. All five of these elements are necessary to permit hospitals to surge effectively in disasters. The Task Force for Mass Critical Care3 provided a classification system for differing levels of surge response in their 2014 guidelines on the management of the critically ill during disasters and pandemics.
Conventional Capacity
A hospital should be able to increase its critical care capacity by approximately 20% above its normal limitations. This level would be implemented in major mass casualty incidents that trigger activation of the hospital emergency operations plan. Most facilities should be able to achieve this level of response using existing staffing and resources, including strategies such as cancellation of elective procedures and transferring of appropriate patients out of ICUs.
Contingency Capacity
This level would be used during a disaster whose medical demands significantly exceeded routine hospital and community resources. At this level, a hospital will expand its critical care capacity by up to 100%, in part through modification of existing spaces and expanding the use of certain staff members. For example, critical care services may be provided in a postanesthesia care unit, stepdown unit, or other high-dependency area with cross-training of staff under the direction of critical care team members. Ventilators intended for the operating room, noninvasive ventilation, or transport can be repurposed to augment the overall ventilator supply. At this level of surge response, it can be expected that medical care will be at or near the predisaster prevailing community standard.
Crisis Capacity
This level would be implemented in catastrophic situations, such as suggested by the current COVID-19 modeling, that result in a significant impact on the standard of medical care that can be provided. Severe limitations of space, staff, and supplies would not allow hospitals to provide the usual standard of medical care. At this level, hospitals and communities will need to consider triage principles.
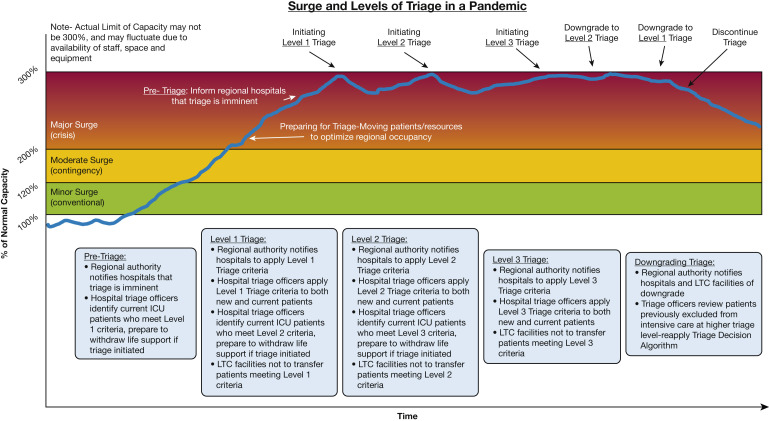
The numbers provided are a construct, not absolute rules. As the balance of resources vs demand shifts over time during an emergency, the degree of the surge response and any necessary triage will shift as well (Fig 1 ). Shortages of trained staff, ventilators, or personal protective equipment (PPE) are very real threats in the current pandemic and will likely be triggers for shifting to triage and crisis standards of care if they should occur. As such, we need to have an accurate inventory of those resources, understanding that the limitations would likely be staff rather than ventilators or space; however, the ongoing experiences in New York suggest that all three may easily be in short supply. However, the early experience in Italy, which has roughly the same number of ICU beds and ventilators per capita as many other developed countries, indicates that our current critical care resources are insufficient to manage a similar outbreak.
Figure 1.
Impact of triage in crisis surge response to balance demand and capacity, demonstrating different levels of triage depending on the degree of demand in relation to system capacity. LTC = long-term care.
A Triage Plan Is Necessary to Ensure the Greatest Benefit to the Greatest Number, and to Reduce the Number of Patients Who Will Be Unable to Receive Critical Care Resources
A number of pandemic triage plans have already been proposed for viral respiratory illness and are outlined in a recent overview on triage.7 When the demand for critical care overwhelms the resources available, a resource allocation plan is essential to deliver both the greatest benefit to the greatest number of people, and to maintain the function of the health-care system and prevent random or otherwise inequitable distribution of scarce resources.
Triage require us to accept that some individuals will not receive critical care resources which might have been dedicated to their care under normal circumstances, whereas some individuals will have critical care interventions withdrawn if they fail to improve. Although as yet untested in practice, modeling studies evaluating predicted mortality in pandemics have demonstrated that more people will die because of lack of critical care resources than would have died if triage systems were implemented.8 , 9 Without a triage plan, patients will receive critical care resources by random chance or a first-come, first-serve basis, likely leading to overall worse outcomes across a population and more individuals being denied critical care.
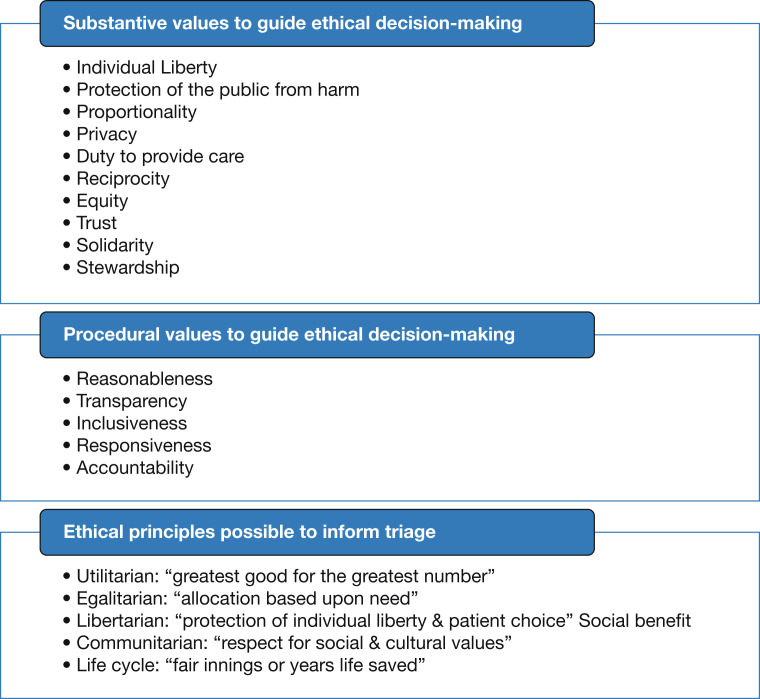
A triage system requires an ethical basis, which we summarize in Figure 2 .10 Limiting and withdrawing critical care resources are justified by the utilitarian principle of providing the greatest good to the greatest number of people. Although the general principle of saving the most lives possible holds true in any system, the decisions of identifying which patients to prioritize for access to critical care will be difficult. A first-come, first-served model of triage has the advantage of simplicity but will exclude patients who lack transportation or easy access to care. A system based on age alone, with mechanical ventilation denied to patients over a given age cutoff, does not account for differences in baseline mortality risk because of underlying health.
Figure 2.
Ethical principles involved in triage systems.10
Communities may choose to prioritize to key groups, to include health-care workers (HCWs), first responders, research volunteers, or others who are either perceived as risking their own safety for the public’s benefit or who have a special role in pandemic response; however, strict definitions of who is included in these key groups and the social utility of such preferences remain unresolved. Children and pregnant women may receive special priority in other schema, with the concept of saving not only the most lives but also the greatest number of years of life.11 , 12 All of these must be taken in consideration, and different cultural priorities will vary between (and within) different countries. This paper is inadequate to answer these questions for a given community; sample triage protocols are available on the CHEST website for review and guidance.
These decisions to implement a triage system should be driven by the inability of regional health systems to deliver care to all critically ill patients because of an overwhelming surge in demand that reaches crisis levels. The triage protocol we are referring to in this case is for tertiary triage, which takes place at an acute care hospital when deciding whether or not to admit for critical care services.5 In a broad sense, patients who present for tertiary triage are going to fit into one of three categories: (1) too well to benefit from critical care, (2) too sick to benefit from critical care because of severe underlying illness or a poor likelihood of surviving their hospitalization, or (3) sick enough to benefit from critical care. The goal of triage protocols is not to exclude categories of patients based on age or underlying disease, and protocols that explicitly exclude patients based on a single criterion alone may run afoul of antidiscrimination laws in many jurisdictions. Rather, the goal of a triage protocol is to maximize the use of critical care resources for patients in the third category. These categories apply to all patients presenting with critical illness under crisis standards of care, not just those infected with SARS-CoV-2.13 Although we must recognize that patients less likely to benefit from critical care may not be provided those services and interventions under a triage system, reallocation may occur as resources and demand change.
The best available epidemiologic data, combined with expert input, will be required to create triage protocols that reflect COVID-19-specific mortality and resource utilization predictions. Although the use of acute illness scores, such as the Sequential Organ Failure Assessment (SOFA) score, were proposed for previous pandemic triage plans, a growing body of evidence suggests such scoring systems are unlikely to predict critical care outcomes with sufficient accuracy,14 , 15 in particular patients suffering from COVID-19,16, 17, 18, 19 or be a useful basis for triage decisions based on the current protocol cut points.13 , 20 , 21
The prognostic accuracy of SOFA varies across its range of scores, with greater variability and less accuracy at lower scores than at higher scores, and is not immediately applicable to all disease states: a patient with sepsis may have a SOFA score of 4 and a low mortality risk, for example, whereas a patient with an intracranial hemorrhage and a Glasgow Coma Scale score of 3 could share this SOFA score of 4 but have a very high risk of death. Potentially subjective elements, such as the dose of vasopressor administered or the assessment of Glasgow Coma Scale during sedation breaks, are subject to physician judgment and are affected by drugs and other interventions.22 Because outcomes at differing SOFA scores vary across studies and are generally absent in the context of crisis standards of care, system-level data are necessary to guide selection of threshold values.
All of these factors combine to raise a number of logistical and ethical concerns regarding the use of the SOFA score in a triage algorithm. Therefore, we propose triage protocols that are not solely dependent on SOFA (or another single scoring tool) because SOFA is unlikely to be adequate in and of itself for triage decisions. It is important to mention that any scoring system at this stage of the pandemic will need to be pragmatic and combine other predictors of ICU mortality, such as disease-specific indicators for non-COVID-19 conditions, frailty scores, comorbidity indices, and physician judgment as best possible. This will need to be balanced against the need for a triage scoring tool that is actionable: complex enough to provide prognostic information with acceptable accuracy, but simple enough to be implemented in a timely manner.
As our knowledge of COVID-19 increases, it is likely that better prognostic scoring tools will be developed; when this occurs, triage systems should incorporate these into their protocols to improve our prediction of critical care outcomes and mitigate the limitations of physiological indices in isolation.
Periodic reassessment of patients is a necessary part of any triage algorithm, to assess for clinical improvement, deterioration, or any other changes that affect prognosis. COVID-19 illness seems to last longer than influenza, suggesting that reassessments at 48 and 120 h noted in earlier triage protocols5 , 13 are too short to provide an adequate trial of therapy in patients with COVID-19. Therefore, any triage protocol will need to be reassessed and modified as clinical experience with SARS-CoV-2 infection grows.
Effective and Ethical Triage Requires Infrastructure, Oversight, Processes, and Training
Triage criteria are one component of a three-part system designed to integrate clinical decisions with incident commanders at the facility and jurisdictional level. They include the following:
-
•
Concept of operations: what is the process that is followed at the facility when making resource allocation decisions?
-
•
Criteria: what is the protocol that is used, and how is that reviewed and updated as new information becomes available?
-
•
Coordination: how are the efforts of the facility integrated with other hospitals in the area to assure information sharing, consistent policies, and patient and resource movement to diffuse impact as needed to assure a consistent standard of care in the region?
Concept of Operations
Concept of operations describes a proactive approach to triage which should be invoked whenever a prolonged incident occurs. This strategy is preferable to reactive bedside decisions based on physician discretion that may occur early in an event. It involves the following several key elements:
-
•
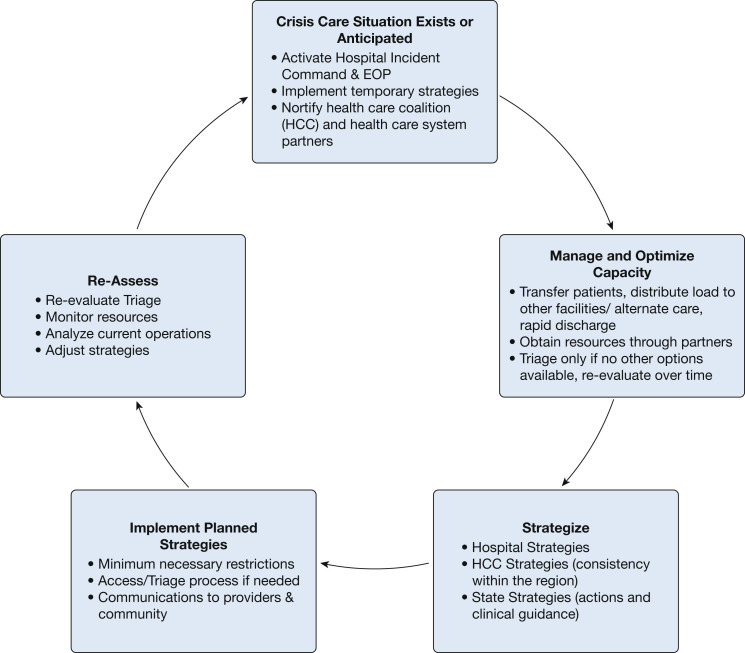
Assuring that resource allocation decisions are integrated into the hospital incident command system, and that the process and protocols are understood and accepted by leadership. The incident command cycle for crisis events is illustrated in Figure 3 .
-
•
A multidisciplinary clinical care committee associated with incident command that makes medical practice recommendations to address increased demand and provides oversight of any triage decisions. This group has broad clinical representation and includes ethics and legal input.
-
•
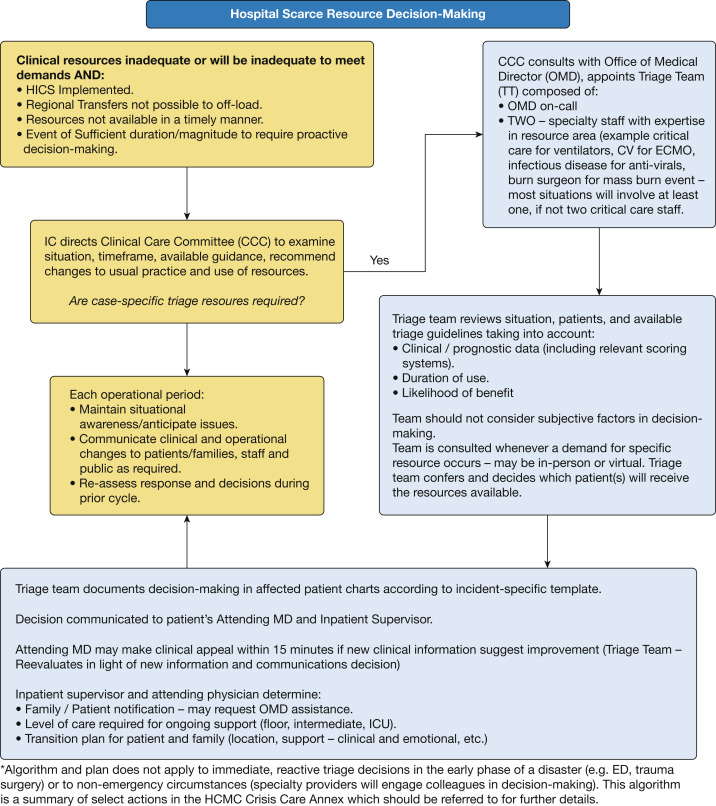
A described process for multidisciplinary decision-making—ideally involving more than one physician with expertise in the area, expectations of the decision process, communication, appeals (where possible), and review (Fig 4 ).
Figure 3.
Process for crisis care integration with incident command. EOP = emergency operations plan; HCC = health-care coalition.
Figure 4.
Sample hospital decision process (Minnesota Department of Health). CCC = Clinical Care Committee; CV = cardiovascular specialist; ECMO = extracorporeal membrane oxygenation; HICS = Hospital Incident Command System; IC = Incident Commander; MD = medical doctor; OMD = Office of Medical Director; TT = triage team.
The decision process is designed to be rapid, but still will likely take up to 1 h. This may have to be abbreviated during times of overwhelming demand, and this expectation should be spelled out. Those providers forced into real-time decision-making should use the same protocol and criteria, and the situation should be documented by incident command.
Triage Protocol
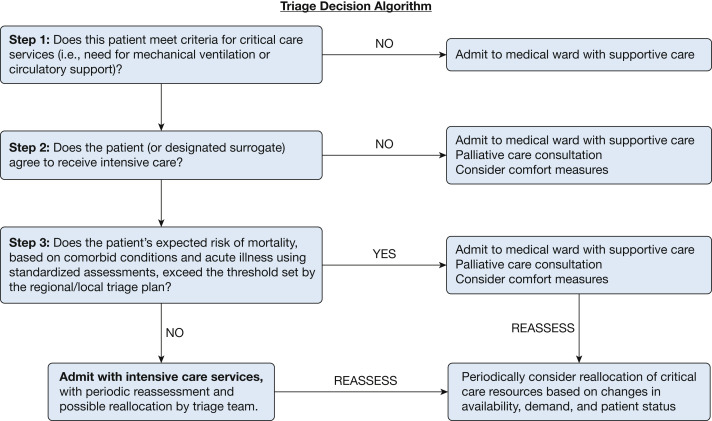
The actual clinical criteria on which the decisions are based should be approved by the clinical care committee and updated as additional information about the specific epidemiologic and outcome characteristics of the disease are understood. Other resources will likely be in short supply and will require guidance from the clinical care committee. A reference card set is available that describes general approaches to a range of resources (https://www.health.state.mn.us/communities/ep/surge/crisis/standards.pdf). A simplified version of a triage protocol is provided in Figure 5 for reference.
Figure 5.
Triage decision process flow.
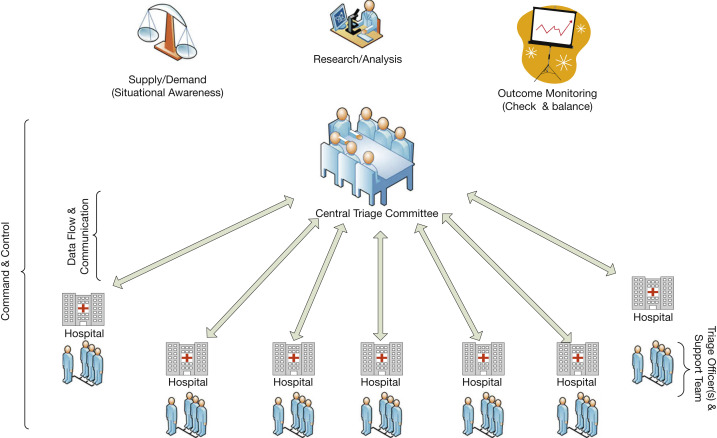
Coordination
Triage criteria and processes should be as consistent as possible within a region. Strong, collaborative regional efforts are a cornerstone of effective response and must be implemented regardless of any competitive posture between health-care systems that may exist during usual operations. Hospitals must share information, adjust protocols, and balance resources and patient loads across the immediate surrounding region to ensure as consistent a standard of care as is possible. The regional structures should involve sharing information about available beds, ventilators, advanced care resources such as extracorporeal membrane oxygenation (a regional approach to extracorporeal membrane oxygenation allocation is found in the card set previously referenced), and staff, and a critical care working group to establish joint triage protocols and coordinate mass critical care planning, and potentially involve a central gatekeeping mechanism for regional referrals and critical care triage. A central triage committee should be appointed, with connections to local triage officers and teams at each hospital. A standardized documentation process (paper or electronic) should be used to allow efficient data collection and decision-making. The protocol should be made available to all triage personnel in advance to allow familiarization and feedback. A mechanism to revisit triage decisions that vary from conventional care practices should be strongly considered to reassess individual patient progress if clinical demand decreases or if capacity increases. Figure 6 illustrates the structure of a triage system at the regional level and integration with a hospital incident command structure.
Figure 6.
Triage infrastructure.
(Reprinted with permission from Christian et al.5)
Many Current Legal and Regulatory Frameworks Preclude a Triage System Because of the Need to Withhold or Withdraw Artificial Life Support Without Consent
Legislation in most states and provinces provides the framework for medical decision-making. Broadly speaking, these laws indicate that plans of treatment require consent of the patient or their surrogate. In some jurisdictions, courts have ruled that physicians do not require consent to withhold CPR (or other life-sustaining measures) that they thought to be outside the standard of care.23 Even within a single country, there may be wide regional variation on the degree to which physicians may make unilateral decisions regarding the provision of resuscitative care.24
A published report from the Institute of Medicine25 outlined some of the important considerations for medical and legal standards of care in a disaster. Key elements of this report include that (1) medical and legal standards of care are not always the same, (2) standards are flexible according to the context of the situation, and (3) authorities need to provide clarity and guidance about standards. Physicians who face uncertainty about how courts and regulatory agencies will assess the standard of care “may react negatively to actual or perceived risks of liability,”25 which would result in worse outcomes for all patients, families, and providers alike whether infected with COVID-19 or not.
To implement a triage system, many jurisdictions would need a modification or suspension of their health-care consent acts to the effect that in the situation of pandemic triage, consent would not be required for decisions about the withholding or withdrawal of artificial life support. In addition, medical licensing bodies should modify their policies to indicate that the standard of care in a pandemic is to triage patients according to an accepted plan, and that consent is not required for treatment decisions taken according to that plan.
Although standards of care may change during a pandemic, crisis standards of care still represent standards; indeed, the need for oversight and review may be even more pressing in this context. If time and circumstances allow, a mechanism for appeal may be built into the system. Such an appeal system must be rapidly accessible and able to decide in a timely enough manner to provide actionable direction to physicians. All triage decisions should eventually be reviewed to allow for transparency and accountability.
Standards of Care
Withholding critical care resources must not mean neglect, and it should not be considered tantamount to terminal care or medical assistance during the dying process. We must care for all patients.
Patients who do not receive critical care because of a triage system must be supported, and the rationale for medical decision-making must be clearly communicated to them or their family members. Shifting the normal role that patients and their surrogates play in decision-making is a substantial deviation from normal medical practice, carrying with it a commensurately large obligation to ensure that these individuals will receive the best possible care given the crisis response.
Studies of severe acute respiratory illness have suggested that many patients with respiratory failure can recover effectively without mechanical assistance, and opioids can be used to treat dyspnea without increasing mortality.26 A patient unable to receive invasive mechanical ventilation may be able to receive supplemental oxygen through a noninvasive route as resources permit. The implementation of early palliative care interventions can provide a better quality of life, less treatment intensity, and no consistent impact on mortality.27 , 28 This offers a strong rationale for the careful integration of symptom management, in alignment with palliative care principles, for all patients impacted by crisis care.29
Clear clinical guidelines must be established by institutions for the care of all patients with respiratory failure and shock, including those patients unable to receive critical care therapies. It may be possible, depending on the capabilities of a given institution, to provide some forms of critical care monitoring and therapy in a crisis situation outside of the traditional ICU. Protocols to support the use of opioids for dyspnea, other key supportive and palliative interventions, and the conscientious use of therapies subject to shortages (eg, bronchodilators, antimicrobial agents, fluid therapy) can be of service for bedside physicians. Similarly, clear and standardized communication tools, such as information sheets, can inform the public about crisis standards of care, can inform about triage criteria, and may offer the wider community opportunities for feedback as a means of increasing public trust.
Family and Societal Support
An effective triage system must help physicians maintain transparency in their decision-making. The transition of health-care systems to crisis care delivery requires a systematic communication strategy at the community level to explain the situation and ongoing efforts to maintain the best possible level of care. Patients and families have the right to expect that those with similar critical care needs will be treated fairly and equitably, with no preference to any particular group. A hotline and electronic communication platform may help gauge community response and concerns during the event and will inform leaders regarding the emotional reassurances needed by members of the society.30
Many centers have limited the number of caregivers at the bedside, reduced family movement in the hospital, and required the use of PPE for all visitors to the bedside. This use of PPE by visitors and caregivers will become increasingly problematic considering worldwide shortages, with some centers reportedly only permitting their use by visitors at crucial contact times, such as the end of life. These limitations in family contact can only increase the burden of suffering, and new methods will be needed to reduce this burden, to include the use of technologic solutions (eg, video conferencing via tablets and smartphones) to attempt to preserve as much intrapersonal contact as possible.31
With the use of triage algorithms in crisis care, even the most transparent systems of decision- making may lead to prolonged feelings of guilt from lack of personal preparedness, an inability to assist, or frustration toward the government and the medical system. Ancillary team members (including palliative care, psychiatrists, psychologists, other mental health workers, and social workers) will need to assist with the burden of communication with ICU families. These professionals should remain in regular communication with family via telephone, text message, or other means as best possible. It is additionally important to anticipate and plan for supporting these professionals, who themselves will require support because of secondary moral distress.
HCW Support
The term moral injury has been increasingly suggested to describe the distress that HCWs can experience from the excessive demands of energy, strength, and resources often experienced within current health-care systems.32 The resulting constellation of symptoms—fatigue, frustration, cynicism, and inefficiency—has historically been defined as burnout, but this term fails to capture the similarities that this syndrome may share with posttraumatic stress disorder or the severity of the associated psychological injury.33
Beyond the issues of fatigue and burnout, however, there are the very real threats of infection and personal harm because of workplace exposure to COVID-19. Shortages of PPE in the United States and other countries have exacerbated this threat; reports of hospitals curtailing PPE use and sanctioning HCWs for using their own personal PPE in the presence of shortages have only made these issues more acute.
The principles of beneficence and nonmaleficence are core to the practices of medicine and nursing, and the impact of asking physicians to shift their perspective during a crisis surge response should not be underestimated.6 Feelings of social isolation are common in times of crisis and are further exacerbated by current recommendations for social distancing, infection control practices, and prolonged use of PPE. Disruptions in normal routines, concern for personal welfare, and fear for the safety of loved ones all add additional stress. A significant number of physicians in active practice already exhibit signs and symptoms of moral injury, with higher self-reported rates of poor patient safety habits, more medical errors in their practice, and increased rates of suicidal ideation.34 The personal risk to bedside physicians during the COVID-19 pandemic, especially in light of international shortages of PPE, only increases this strain on the workforce. This can be a significant threat to both the quality and efficiency of care in a crisis.
Providing members of the health-care team with structured opportunities to debrief after critical events and ongoing opportunities for engagement and input to improve the inevitably dynamic work environment have also been shown to be effective to promote community, connectedness, and meaning. Incorporating these principles thoughtfully during triage system activation requires a systematic leadership communication plan to explain the reasons for its use; formal training to ensure consistent implementation; and collaborative, team-based approaches to decision-making led by the designated triage officers and including physicians directly caring for patients with the strong support of hospital ethics and palliative care experts.
Similarly, institutions and governments must prevent the sanctioning of HCWs for attempting to protect their own (and their families’) safety through nonstandard PPE usage; instead, health-care organizations need to redouble efforts to expand PPE availability, be it through innovative reusage methods, adoption of acceptable alternative forms of PPE (eg, the use of industrial respirators), and governmental and industry support for increased manufacturing.
Existing resilience measures and support programs will need to be strengthened to protect the psychological well-being of patients, families, and the HCWs treating them both during and after these events.5 It is wise to consider a structured schedule of opportunities within each work unit and the hospital at large to encourage staff to learn about and use these measures, especially in the setting of anticipated prolonged periods of modified work practices that the current COVID-19 pandemic threatens to create.
Institutions may refer to existing resources in implementing plans, such as the National Academy of Medicine in the United States (https://nam.edu/clinicianwellbeing/) and the Intensive Care Society in the United Kingdom (www.ics.ac.uk), which has put a free Wellbeing Resource Library online with specific content relevant to COVID-19.
A personal connection with the patients is perhaps the most important and powerful tool to maintain our sense of purpose and best care for their ongoing needs, and structured opportunities to develop and maintain a human connection with the individuals whose needs we serve will also help to combat feelings of depersonalization in the critical care environment that are only exacerbated by the current crisis.35
Pediatric Considerations
Any triage system must balance the need to save the most lives possible with the need to save total life-years. Critically ill children therefore are usually considered separately from adults when triage considerations are made. The fundamental precepts of crisis critical care—including care and attention to the health of the entire family as a unit and respect for the role of parents—remain critical to the success of disaster management. Institutions must balance the needs of family-centered care vs the risk of disease transmission. One or more caregivers usually accompany pediatric patients; these caregivers are likely to be close contact with a patient and should be treated as presumably exposed; however, they may be asymptomatic at the time, and will require monitoring for symptomatic disease and potential quarantine.
Incorporating children into a regional triage algorithm is complicated for a disease process such as COVID-19 that largely affects adults, at least in terms of critical illness. Much of pediatric critical care is separated into very few pediatric centers, with only some pediatric resources being applicable to adult groups. To prevent any hospital from needing to use crisis standards of care, pediatric-only hospitals in an affected region have a duty to surge to prevent adult and mixed adult/pediatric hospitals going into crisis as regional capacity needs require. In such a scenario, pediatric-only hospitals should consider the steps outlined in Table 1.
Pediatric care should preferably be concentrated in pediatric centers to preserve necessary pediatric systems. Given the low mortality of most conditions with which children are admitted to intensive care (< 5%), patients < 18 years of age who meet the mortality criteria associated with the adult triage levels will be very rare, such that the adoption of the same triage system in pediatrics is unlikely to mobilize further resources. An entirely different algorithm that is pediatric-specific would be necessary in considering pediatric-specific triage policies. Some centers have modeled situations where a certain mortality rate or predicted ventilator-days could preclude the offering of invasive ventilator support to some children at a time of significantly increased short-term ventilator needs,8 but there is a paucity of pediatric-specific data to guide such triage. Medical specifics aside, the guiding ethical principles remain the same for pediatric triage and should still be applied.
Pediatric centers should regionally activate pediatric triage when shared pediatric resources (accounting for transportation capacity) are exhausted, with mortality predictions subject to expert opinion, which should be agreed on and documented by at least two members of the treating team. Prior to movement to higher triage levels, especially considering such steps being unlikely to mobilize resources, discussions should be held regarding movement of ventilators to pediatric centers from adult sites if there is a difference in resource demand.
Conclusions
This framework can provide the essential tools to rapidly assist communities to establish the infrastructure necessary to equitably meet the clinical needs of the greatest number of patients with COVID-19 during a time of scarce resources. It is the goal of the Task Force to minimize the need for allocation of scarce resources as much as possible.
Acknowledgments
Financial/nonfinancial disclosures: None declared.
Other contributions: We thank Christie Martin, MN, MPH, RN, PHN, LHIT-HP, Henry Feldman, MD, Timur Alptunaer, MD, J. Christopher Farmer, MD, Kiersten Henry, DNP, ACNP-BC, CCNS, CCRN-CMC, Sarah Delgado, MSN, RN, ACNP, and Steven Simpson, MD, for their input and critical review of this manuscript and the members of the Task Force for Mass Critical Care for their tireless efforts and support.
Additional information: Some of the authors are US government employees or military service members. This work was prepared as part of their official duties. Title 17 U.S.C. §105 provides that “Copyright protection under this title is not available for any work of the United States Government.” Title 17 U.S.C. §101 defines a US government work as a work prepared by a military service member or employee of the US government as part of that person’s official duties. The opinions and assertions contained herein are those of the authors and do not reflect the official views or position of the Department of the Navy, Department of Defense, Department of Veterans Affairs, the US Government, nor of the academic institutions with which the authors are affiliated.
Endorsed by the American Association of Critical-Care Nurses and the Society of Critical Care Medicine
References
- 1.Einav S., Hick J.L., Hanfling D. Surge capacity logistics: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146(4 suppl) doi: 10.1378/chest.14-0734. e17S-43S. [DOI] [PubMed] [Google Scholar]
- 2.Hick J.L., Christian M.D., Sprung C.L., European Society of Intensive Care Medicine's Task Force for intensive care unit triage during an influenza epidemic or mass d. Chapter 2 Surge capacity and infrastructure considerations for mass critical care. Recommendations and standard operating procedures for intensive care unit and hospital preparations for an influenza epidemic or mass disaster. Intensive Care Med. 2010;36 (suppl 1):S11–S20. doi: 10.1007/s00134-010-1761-4. [DOI] [PubMed] [Google Scholar]
- 3.Hick J.L., Einav S., Hanfling D. Surge capacity principles: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146(4 suppl):e1S–e16S. doi: 10.1378/chest.14-0733. [DOI] [PubMed] [Google Scholar]
- 4.Hick JL, Hanfling D, Wynia MK, Pavia AT. Duty to plan: health care, crisis standards of care, and novel coronavirus SARS-CoV-2. NAM Perspectives. Discussion paper. Washington, DC: National Academy of Medicine. 10.31478/202003b. Accessed June 10, 2020. [DOI] [PMC free article] [PubMed]
- 5.Christian M.D., Sprung C.L., King M.A. Triage: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146(4 suppl):e61S–e74S. doi: 10.1378/chest.14-0736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Society of Critical Care Medicine United States resource availability for COVID-19. https://sccm.org/Blog/March-2020/United-States-Resource-Availability-for-COVID-19?_zs=jxpjd1&_zl=w9pb6
- 7.Christian M.D. Triage. Crit Care Clin. 2019;35(4):575–589. doi: 10.1016/j.ccc.2019.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gall C., Wetzel R., Kolker A., Kanter R.K., Toltzis P. Pediatric triage in a severe pandemic: maximizing survival by establishing triage thresholds. Crit Care Med. 2016;44(9):1762–1768. doi: 10.1097/CCM.0000000000001759. [DOI] [PubMed] [Google Scholar]
- 9.Kanter R.K. Would triage predictors perform better than first-come, first-served in pandemic ventilator allocation? Chest. 2015;147(1):102–108. doi: 10.1378/chest.14-0564. [DOI] [PubMed] [Google Scholar]
- 10.University of Toronto Joint Centre for Bioethics Pandemic Influenza Working Group . University of Toronto; Toronto, ON: 2005. Stand on Guard for Thee. Ethical Considerations in Preparedness Planning for Pandemic Influenza. [Google Scholar]
- 11.Emanuel E.J., Persad G., Upshur R. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382(21):2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 12.Truog R.D., Mitchell C., Daley G.Q. The toughest triage — allocating ventilators in a pandemic. N Engl J Med. 2020;382(21):1973–1975. doi: 10.1056/NEJMp2005689. [DOI] [PubMed] [Google Scholar]
- 13.Christian M.D., Hawryluck L., Wax R.S. Development of a triage protocol for critical care during an influenza pandemic. CMAJ. 2006;175(11):1377–1381. doi: 10.1503/cmaj.060911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khan Z., Hulme J., Sherwood N. An assessment of the validity of SOFA score based triage in H1N1 critically ill patients during an influenza pandemic. Anaesthesia. 2009;64(12):1283–1288. doi: 10.1111/j.1365-2044.2009.06135.x. [DOI] [PubMed] [Google Scholar]
- 15.Zygun D.A., Laupland K.B., Fick G.H., Sandham J.D., Doig C.J. Limited ability of SOFA and MOD scores to discriminate outcome: a prospective evaluation in 1,436 patients. Can J Anaesth. 2005;52(3):302–308. doi: 10.1007/BF03016068. [DOI] [PubMed] [Google Scholar]
- 16.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang X., Yu Y., Xu J. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study [published online ahead of print] Lancet Respir Med. 2020;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang G, Hu C, Luo L, et al. Clinical features and outcomes of 221 patients with COVID-19 in Wuhan, China [published online ahead of print]. medRxiv.
- 19.Xu Y, Xu Z, Liu X, et al. Clinical findings in critical ill patients infected with SARS-Cov-2 in Guangdong Province, China: a multi-center, retrospective, observational study [published online ahead of print]. medRxiv. 2020.03.02.20030452. doi: 10.1101/2020.03.02.20030452. Accessed June 10, 2020. [DOI]
- 20.Cheung W., Myburgh J., Seppelt I.M. Development and evaluation of an influenza pandemic intensive care unit triage protocol. Crit Care Resusc. 2012;14(3):185–190. [PubMed] [Google Scholar]
- 21.Cheung W.K., Myburgh J., Seppelt I.M. A multicentre evaluation of two intensive care unit triage protocols for use in an influenza pandemic. Med J Aust. 2012;197(3):178–181. doi: 10.5694/mja11.10926. [DOI] [PubMed] [Google Scholar]
- 22.Christian M.D., Hamielec C., Lazar N.M. A retrospective cohort pilot study to evaluate a triage tool for use in a pandemic. Crit Care. 2009;13(5):R170. doi: 10.1186/cc8146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Downar J., Close E., Sibbald R. Do physicians require consent to withhold CPR that they determine to be nonbeneficial? CMAJ. 2019;191(47):E1289–E1290. doi: 10.1503/cmaj.191196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.College of Physicians and Surgeons of Ontario Planning for and providing quality end-of-life care. https://www.cpso.on.ca/Physicians/Policies-Guidance/Policies/Planning-for-and-Providing-Quality-End-of-Life-Car
- 25.Altevogt B.M., Stroud C., Hanson S.L., Hanfling D., Gostin L.O., Institute of Medicine (US) Committee on Guidance for Establishing Standards of Care for Use in Disaster Situations . National Academies Press (US); Washington, DC: 2009. Guidance for Establishing Crisis Standards of Care for Use in Disaster Situations: A Letter Report. [PubMed] [Google Scholar]
- 26.Downar J., Delaney J., Hawryluck L., Kenny L. Neither guidelines nor symptom-targeted opioids are harmful when withdrawing life-sustaining measures. Intensive Care Med. 2016;42(8):1303–1304. doi: 10.1007/s00134-016-4390-8. [DOI] [PubMed] [Google Scholar]
- 27.Wright A.A., Zhang B., Ray A. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665–1673. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang B., Wright A.A., Huskamp H.A. Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med. 2009;169(5):480–488. doi: 10.1001/archinternmed.2008.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Downar J., Seccareccia D. Palliating a pandemic: "all patients must be cared for". J Pain Symptom Manage. 2010;39(2):291–295. doi: 10.1016/j.jpainsymman.2009.11.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Biddison E.L.D., Faden R., Gwon H.S. Too many patients…a framework to guide statewide allocation of scarce mechanical ventilation during disasters. Chest. 2019;155(4):848–854. doi: 10.1016/j.chest.2018.09.025. [DOI] [PubMed] [Google Scholar]
- 31.Carlson E.B., Spain D.A., Muhtadie L., McDade-Montez L., Macia K.S. Care and caring in the intensive care unit: family members' distress and perceptions about staff skills, communication, and emotional support. J Crit Care. 2015;30(3):557–561. doi: 10.1016/j.jcrc.2015.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Talbot S.G., Dean W. Physicians aren’t ‘burning out.’ They’re suffering from moral injury. Stat. July 26, 2018 https://www.statnews.com/2018/07/26/physicians-not-burning-out-they-are-suffering-moral-injury/. Accessed June 10, 2020. [Google Scholar]
- 33.Freudenberger H.J. The staff burn-out syndrome in alternative institutions. Psychotherapy: Theory, Research & Practice. 1975;12(1):73. [Google Scholar]
- 34.Tawfik D.S., Profit J., Morgenthaler T.I. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. Mayo Clin Proc. 2018;93(11):1571–1580. doi: 10.1016/j.mayocp.2018.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gajic O., Anderson B.D. “Get to know me” board. Crit Care Explor. 2019;1(8) doi: 10.1097/CCE.0000000000000030. [DOI] [PMC free article] [PubMed] [Google Scholar]