Abstract
Sonographers need to be familiar with and prepared to implement strategies for reducing the risk of exposure to and transmission of the COVID-19 virus. Strategies to employ can be grouped into three broad categories: (1) whom to scan, (2) where to scan, and (3) how to scan. Whom to scan addresses sonographer strategies for determining essential and emergent scan status. Where to scan addresses sonographer practice strategies for selecting equipment, use of rooms, portable examinations, and training personnel. How to scan addresses the topics of scanning techniques (tailored protocols, right-handed scanning, use of barrier devices) and equipment cleaning and disinfecting.
Keywords: Sonographer, ASE, COVID-19, Protection
Background
The American Society of Echocardiography (ASE) recently provided the “ASE Statement on Protection of Patients and Echocardiography Service Providers during the 2019 Novel Coronavirus Outbreak.”1 This supplement focuses on three key areas of that document, (1) whom to scan, (2) where to scan, and (3) how to scan, with additional details and resources to guide sonographer practice.
Whom to Scan
Only emergent essential echocardiographic studies should be performed to limit the risk for exposure to other patients and health care providers. Several professional societies have provided statements that all nonessential ultrasound examinations be rescheduled to reduce the risk for exposure to the novel coronavirus.1, 2, 3, 4 Various mechanisms for doing so have been advocated on the basis of ultrasound specialty, and definitions of “essential” may be determined by local and institutional standards.1, 2, 3, 4 In addition to the guidance provided in the “ASE Statement on Protection of Patients and Echocardiography Service Providers during the 2019 Novel Coronavirus Outbreak” main document, sites are also implementing additional requirements for placing orders. These include approval of the procedure by a cardiologist or cardiology fellow, review of the proposed study with the cardiologist to plan the examination and determine if a comprehensive echocardiographic study is needed, justification for why the echocardiographic study is to be performed emergently, and why it is essential. In general, there is consensus that echocardiographic studies for patients with heart failure, heart transplantation, and ongoing chemotherapy or stem cell transplantation are considered essential (the list is not all inclusive). Sonographers are encouraged to work with their medical teams to reschedule and/or defer all nonessential and nonemergent patients.
Within the echocardiography laboratory, there should be tracking and rotation of sonographers performing examinations in patients suspected and/or positive for coronavirus disease 2019 (COVID-19), in order to reduce exposure of any one team member and the potential for transmission to an entire team or laboratory.
Where to Scan
The goal is to limit exposure to the novel coronavirus to as few individuals as possible. Strategies for sonographers to consider are as follows: using a dedicated ultrasound system(s) and room(s) for performing all studies in suspected and/or confirmed COVID-19 cases, performing all inpatient examinations portably, and first using handheld devices to determine if complete comprehensive echocardiographic examination is needed. The advantage of handheld devices in the COVID-19 environment is that these devices can be completely draped and are easily cleaned. Use of handheld devices by other trained providers may limit exposure to sonographers and conserve personal protective equipment (PPE). In this scenario, it is recommended that devices that offer remote connection to picture archiving and communication systems be used. Sonographers may be involved in producing training videos and can be available remotely to facilitate the use of handheld devices to tailor examinations and acquire additional views that may not be included as part of the traditional point-of-care ultrasound imaging. Using handheld devices that connect remotely (i.e., wireless network, cloud, etc.) is desirable, as the images can be sent directly to the echocardiography laboratory workstation for immediate review by a cardiologist to determine whether a comprehensive echocardiographic examination is needed.
How to Scan
As stated previously, the goal is to limit exposure. Appropriate PPE should always be used according to patient status (see Figure 1 in the main document, “ASE Statement on Protection of Patients and Echocardiography Service Providers during the 2019 Novel Coronavirus Outbreak”1). In addition to the use of appropriate PPE, sonographers can use strategies that limit exposure while actually scanning (adjusting protocols and technique) and through appropriate cleaning of equipment. These are described below. Refer to your institution's safety guidelines for appropriate PPE and protocol for donning and doffing PPE.1 Additional information regarding the types of PPE are described in the “ASE Statement on Protection of Patients and Echocardiography Service Providers during the 2019 Novel Coronavirus Outbreak.”1
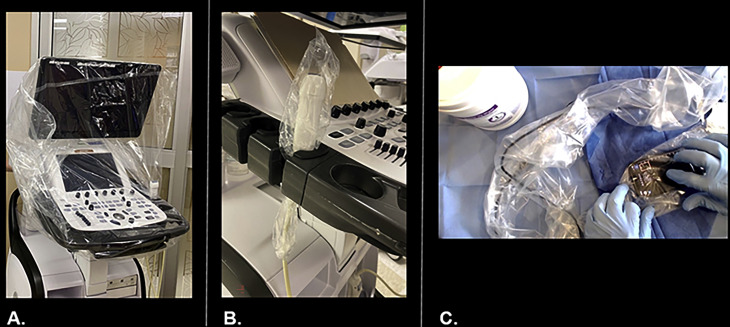
Figure 1.
(A) Draped ultrasound system. (B) Draped transducer. (C) Draped handheld system.
Reproduced with permission from Stainback et al.13
One strategy for limiting exposure is shortening examination time. To shorten examination time, sonographers should have discussions with their medical teams to determine if a comprehensive echocardiographic examination (with or without contrast) is needed on the basis of the patient's history and current medical history. Cardiovascular sequelae associated with COVID-19 have been previously described,5, 6, 7, 8 and an abbreviated, limited, or focused examination might yield the desired information while decreasing the amount of time needed for the sonographer to be exposed to the patient.
In addition to using abbreviated imaging protocols, measurements should be made offline in the echocardiography laboratory to shorten the time in the room with the patient. In general, there is consensus that echocardiographic studies in de novo patients be limited to assessing left ventricular and right ventricular size and function, with screening for valvular disease. As myocarditis is a potential COVID-induced pathology, global longitudinal strain assessment may be performed from this limited study. Follow-up studies should be discussed ahead of time to identify the imaging goals in an effort to reduce examination time and exposure.
Sonographers may want to consider scanning right-handed so that they are positioned away from the patient's face. Right-handed scanning should be considered only if the sonographer is proficient at scanning right-handed and would not incur additional scanning time. Another strategy is to allow providers who are trained in point-of-care cardiac imaging to perform screening echocardiography and send images remotely to the picture archiving and communication system for expert interpretation. Then, after an expert has reviewed the images, a decision can be made if a full comprehensive echocardiographic study is needed.
Another way to limit exposure is to keep equipment clean and disinfected. Systems with flatter surfaces and fewer crevices will be easier to clean and disinfect. Thus, if an echocardiography laboratory has the choice of selecting an ultrasound system with a touch screen and fewer crevices (such as a keyboard), it may be desirable to use this piece of equipment to perform all studies in patients with suspected or confirmed COVID-19.6, 10 Single-use gel packets (not bottles) should be used when entering a room to scan a patient with suspected and/or confirmed COVID-19, and unused gel packets can be discarded in the room. If single-use gel packets are not available, an alternative may be to fill syringes with ultrasound gel to be used in place of single-use packets. The gel-filled syringes can then be discarded after the examination is completed. In addition, draping the equipment with plastic covers and using transducer covers (if available) will further help with cleaning and disinfecting equipment (see Figure 1).9, 10, 11, 12, 13 In rooms in which patients are on ventilators and individuals and equipment are exposed to airborne pathogens, the transducer should be draped.9 Handheld devices again may be used as first-line screening devices, as these systems are easily cleaned. On the basis of current Centers for Disease Control and Prevention guidelines12 and the American Institute of Ultrasound in Medicine's updated statement “Guidelines for Cleaning and Preparing External- and Internal-Use Ultrasound Transducers and Equipment between Patients as Well as Safe Handling and Use of Ultrasound Coupling Gel,” low-level disinfection is still appropriate for external and interventional procedures, and a list of approved disinfectants for use with COVID-19 is available online.9 , 12 , 14
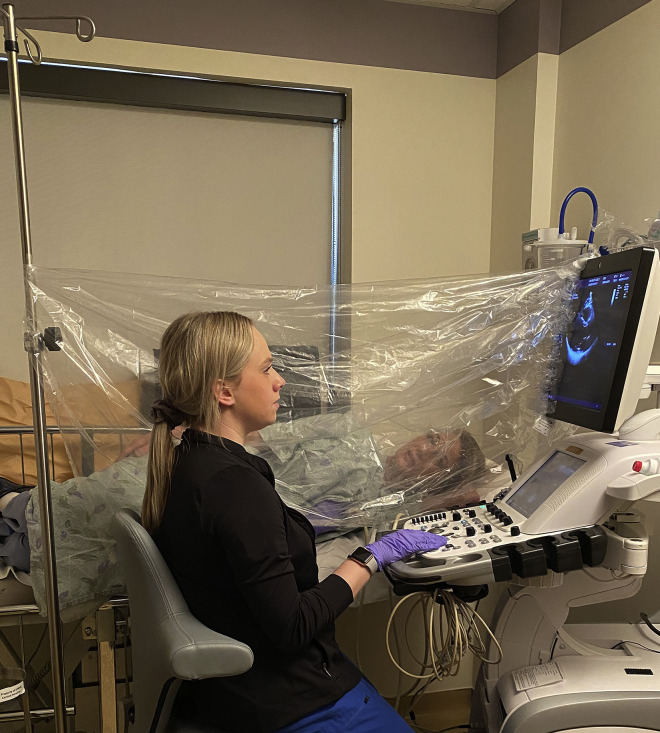
Before entry into a room to scan a patient with suspected and/or confirmed COVID-19, all ancillary equipment (extra transducer, electrocardiography [ECG] leads, linens, etc.) should be removed from the ultrasound system to limit exposure of additional equipment. Sonographers should explore whether the patient is already hooked up to an ECG system that could be imported into the echocardiographic machine, as opposed to taking the ultrasound system cable and ECG leads. This reduces the need for cleaning ECG cables and leads, which may be difficult to disinfect. If available, the use of a barrier between the bed (where the patient is lying) and sonographer could be set up before imaging (see Figure 2 ).15, 16, 17, 18
Figure 2.
Barrier example used between the patient and the sonographer.15, 16, 17, 18 This is a posed photograph demonstrating the barrier technique and how the sonographer's arm can maneuver under the barrier shield. If this were a real situation, the sonographer would be wearing appropriate PPE.
The equipment should be cleaned after the examination is performed. The ultrasound equipment needs to be cleaned in its entirety, from top to bottom, including the wheels. Equipment should be cleaned in the anteroom or immediately outside the patient's room to limit exposure to others. Cleaning of equipment and doffing of PPE should be followed per institutional standards.1
The focus in this communication has been to address sonographer-specific issues for performing transthoracic echocardiographic examinations. Transesophageal echocardiography considerations are addressed in the Council on Perioperative Echocardiography's “Specific Considerations for the Protection of Patients and Echocardiography Service Providers When Performing Perioperative or Periprocedural Transesophageal Echocardiography during the 2019 Novel Coronavirus Outbreak: Council on Perioperative Echocardiography Supplement to the Statement of the American Society of Echocardiography.”19
Footnotes
NOTICE AND DISCLAIMER: This statement reflects recommendations based on expert opinion, national guidelines, and available evidence. Our knowledge with regard to COVID-19 continues to evolve, as do our institutional protocols for dealing with invasive and noninvasive procedures and practice of personal protective equipment. Readers are urged to follow national guidelines and their institutional recommendations regarding best practices to protect their patients and themselves. These reports are made available by the American Society of Echocardiography (ASE) as a courtesy reference source for its members. The reports contain recommendations only and should not be used as the sole basis to make medical practice decisions or for disciplinary action against any employee. The statements and recommendations contained in these reports are primarily based on the opinions of experts, rather than on scientifically verified data. ASE makes no express or implied warranties regarding the completeness or accuracy of the information in these reports, including the warranty of merchantability or fitness for a particular purpose. In no event shall ASE be liable to you, your patients, or any other third parties for any decision made or action taken by you or such other parties in reliance on this information. Nor does your use of this information constitute the offering of medical advice by ASE or create any physician-patient relationship between ASE and your patients or anyone else.
Conflicts of interest: None.
References
- 1.Kirkpatrick J.N., Mitchell C., Taub C., Kort S., Hung J., Swaminathan M. ASE statement on protection of patients and echocardiography service providers during the 2019 novel coronavirus outbreak. J Am Soc Echocardiogr. 2020;33:648–653. doi: 10.1016/j.echo.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Institute of Ultrasound in Medicine Guidelines for cleaning and preparing external- and internal-use ultrasound transducers and equipment between patients as well as safe handling and use of ultrasound coupling gel. https://www.aium.org/officialStatements/57 Available at: [DOI] [PubMed]
- 3.American Institute of Ultrasound in Medicine Quick guide on COVID-19 protections—patient and ultrasound provider protection. https://aium.s3.amazonaws.com/covid19/Covid19_Quick_Guide_PUPP.pdf Available at.
- 4.Society of Vascular Ultrasound Vascular laboratory responses during the COVID-19 pandemic. https://www.svu.org/svu-news/4183/ Available at:
- 5.Driggin E., Madhavan M.V., Bikdeli B., Chuich T., Laracy J., Bondi-Zoccai G. Cardiovascular considerations for patients, health care workers, and health systems during the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Cardiol. 2020 doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 8.Ruan Q., Yang K., Wang W., Jiang L., Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American Institute of Ultrasound in Medicine Quick guide on COVID-19 Protections—ultrasound transducers, equipment, and gel. https://aium.s3.amazonaws.com/covid19/Covid19_Quick_Guide_UTEG.pdf Available at:
- 10.Minardi J. Point-of-care ultrasound in COVID-19. https://www.youtube.com/watch?v=nx6eHINDveM Available at:
- 11.van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention Cleaning and disinfection for community facilities. https://www.cdc.gov/coronavirus/2019-ncov/community/organizations/cleaning-disinfection.html Available at:
- 13.Stainback R., Plana J.C., Coulter S.A., Krajcer Z. Cardiology in the Time of COVID-19: Troponin Assessment, Telemetry & Echo Lab. Texas Heart Institute. https://youtu.be/ZoNrhzkgLhY Available at:
- 14.United States Environmental Protection Agency List N: disinfectants for use against SARS-CoV-2. https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2 Available at:
- 15.Kolias T.J., Eberhart D., Bradsher K. Echo scanning barrier drape procedure. https://www.asecho.org/wp-content/uploads/2020/04/Echo-Scanning-Barrier-Drape-Procedure-Updated-04092020.pdf Available at:
- 16.Dean M., Schwarz K., Steinmetz, Hills D., Stoddard T. URMC Echo COVID-19 Shield. https://www.asecho.org/wp-content/uploads/2020/03/Echo-COVID-19-Barrier-Description-2020-03-25-002.pdf Available at:
- 17.American Society of Echocardiography. Provider Protection Strategies Shared by ASE Members. Available at: https://www.asecho.org/covid-19-resources/provider-protection-strategies-shared-by-ase-members/. Accessed March 31, 2020
- 18.MacAllister S.J. Echo staff and patients safety. https://www.melbourneheartcare.com.au/echo-staff-and-patients-safety/ Available at:
- 19.Nicoara A., Maldonado Y., Kort S., Swaminathan M., Mackensen G.B. Specific considerations for the protection of patients and echocardiography service providers when performing perioperative or periprocedural transesophageal echocardiography during the 2019 novel coronavirus outbreak: Council on Perioperative Echocardiography supplement to the statement of the American Society of Echocardiography. J Am Soc Echocardiogr. 2020 doi: 10.1016/j.echo.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]