Highlights
-
•
TEE carries a high risk for SARS-CoV-2 spread.
-
•
TEE should be performed when clinical benefits outweigh the risks.
-
•
Proper handling and cleaning of equipment is critical.
-
•
Airborne precautions should be used in patients suspected or confirmed COVID-19.
Keywords: COVID-19, Patient, Protection, Perioperative, Periprocedural
Background
Protecting health care workers and preventing the transmission of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) should be a top priority during the ongoing coronavirus disease 2019 (COVID-19) pandemic. Transesophageal echocardiography (TEE) carries a heightened risk for SARS-CoV-2 spread in nonintubated patients due to possible direct droplet transmission and/or viral aerosolization during insertion and removal of the probe, as well as coughing. Although performing TEE in an already intubated patient may reduce the risk for viral aerosolization, viral transmission may still occur through direct contact with the patient's secretions, resulting in contaminated hands and surfaces. These infection risks apply not only to echocardiographers but also to other patients and personnel in the vicinity, as a result of cross-contamination whenever there may have been improper handling or cleaning of the equipment.
The performance of TEE therefore deserves special consideration in determining appropriate use and special precautions. This statement reflects recommendations based on expert opinion, national guidelines, and available evidence specifically as they pertain to performing safe perioperative TEE. This document does not address specific recommendations during point-of-care surface ultrasound (lung, heart, abdomen, or vascular), nor does it address criteria used in the decision-making regarding postponing elective procedures or proceeding with cardiac surgical procedures deemed urgent or emergent.
Whom to Image?
Practice guidelines for the use of perioperative TEE were developed by the American Society of Echocardiography (ASE) and the Society of Cardiovascular Anesthesiologists.1 , 2 As indicated in the main statement of the ASE on protection during COVID-19,3 TEE should be postponed or canceled if it is unlikely to change clinical care or if an alternative imaging modality (e.g., transthoracic echocardiography using off-axis views, ultrasound-enhancing agents with transthoracic echocardiography) can provide the necessary information. Although nonessential TEE should be either deferred or postponed, patients under investigation or confirmed to have COVID-19 may still require TEE in several clinical situations, including (1) urgent or emergent cardiac surgery, (2) patients with cardiac comorbidities undergoing emergent noncardiac surgery, and (3) hemodynamic instability due to undifferentiated shock in the perioperative period.
Deployment of alternative imaging modalities may not always be possible in the perioperative patient population undergoing cardiac surgery, and special consideration should be given to triaging these patients on a case-by-case basis. Additionally, TEE provides invaluable dynamic information, paramount to performing successful procedures in certain clinical situations. Surgical procedures in which the benefit of performing TEE may outweigh the risk for contamination or cross-contamination include but are not limited to the following:
-
•
infective endocarditis with valvular and perivalvular involvement;
-
•
Stanford type A aortic dissection, especially in the presence of associated complications (e.g., aortic insufficiency, aortic root involvement, pericardial effusion);
-
•
initiation of temporary or durable mechanical circulatory support;
-
•
myocardial infarction with mechanical complications (e.g., ventricular septal defect, left ventricular wall rupture, papillary muscle rupture); and
-
•
prosthetic valve assessment.
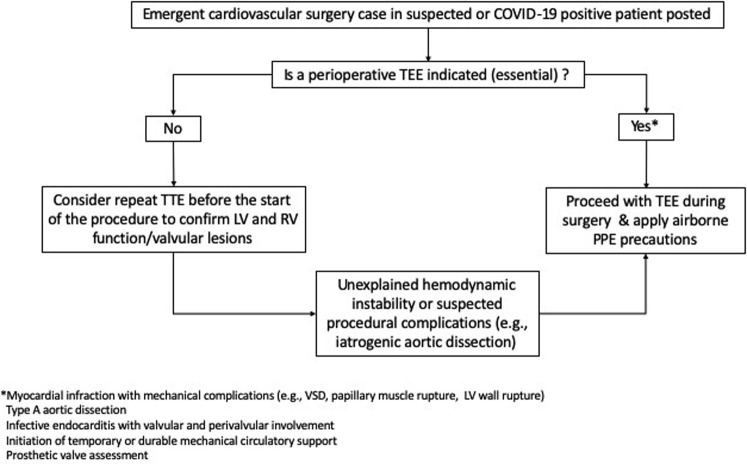
There are surgical procedures in which the use of TEE can be supplanted by observing invasively derived hemodynamic data, other imaging modalities (e.g., fluoroscopy, epicardial ultrasound imaging), or direct visualization of the heart in the surgical field, such as coronary artery bypass graft or endovascular stenting for Stanford type B aortic dissection with peripheral malperfusion. In these procedures, TEE can be considered in situations of severe hemodynamic instability or procedural complications, which require immediate diagnosis and in which the findings of TEE would have a strong impact on patient outcomes (Figure 1 ).
Figure 1.
Suggested algorithm for determining indication for intraoperative TEE. LV, Left ventricular; RV, right ventricular.
Where to Image?
Perioperative TEE will likely be performed in operating rooms, structural heart and catheterization laboratory rooms, or intensive care units. Patients with suspected or confirmed COVID-19 should undergo surgical or interventional procedures in dedicated COVID-19 operating rooms or may be admitted to intensive care unit rooms. Specific considerations should be given to entering and especially exiting these spaces to limit virus transmission.
How to Image?
Protocols
TEE performed in patients with suspected or confirmed COVID-19 should follow an abbreviated but adequate pathology-directed protocol to limit personnel exposure time. This focused examination approach should also be extensive enough to detect and adequately evaluate any significant unexpected pathology. Limiting factors in performing comprehensive TEE may be related to the patient's clinical condition and the nature of the surgical procedure, especially in patients undergoing urgent or emergent cardiac surgery. It is important to record and store the acquired imaging data and cine loops so that they are available for review by other clinicians. Findings should be communicated and reported in a timely manner, as per routine practice.
Protection
Personnel
The levels and categories of personal protective equipment (PPE) are detailed in the main statement of the ASE on protection during COVID-19.3 Although the type of PPE may depend on institutional policies and available resources, it is generally accepted that performing TEE in patients with suspected or confirmed COVID-19 warrants the use of airborne precautions, irrespective of the intubation status of the patient. All personnel should be educated in appropriate utility of PPE as per institutional policies. Whenever possible, trained observers or the use of a “buddy system” should ensure appropriate donning and doffing of PPE. The most experienced echocardiographer should perform the examination, including probe insertion and removal. Although airborne precautions should be followed in all high-risk patients (patients under investigation or confirmed COVID-19-positive patients), droplet precautions are recommended for TEE in all patients without COVID-19.4 , 5
Equipment
Proper handling and cleaning of equipment is critical in prevention of virus transmission to other health care providers and other patients. The exact steps to be followed for disinfection of the transesophageal probe and equipment will depend on local institutional protocols that should be guided by infectious disease experts and resource availability. Plastic covers for the ultrasound machine, its touchable parts (knobs, screen), and transducer ports are commercially available and should be considered to reduce bioburden on these “high-touch” surfaces with hard-to-clean grooves, slots, or crevices (Figure 2 ). To avoid contamination of surfaces, one person can be designated to probe manipulation and another to adjusting instrument settings for image optimization and data acquisition, although this approach must be balanced with PPE availability. As noted in the ASE's main document,3 removal of any nonessential accessory equipment from the ultrasound machine (cart), such as additional alternative transducers, electrocardiographic cables and stickers, paperwork, gel, and any other items, will facilitate thorough cleaning and minimize risk for cross-contamination.
Figure 2.
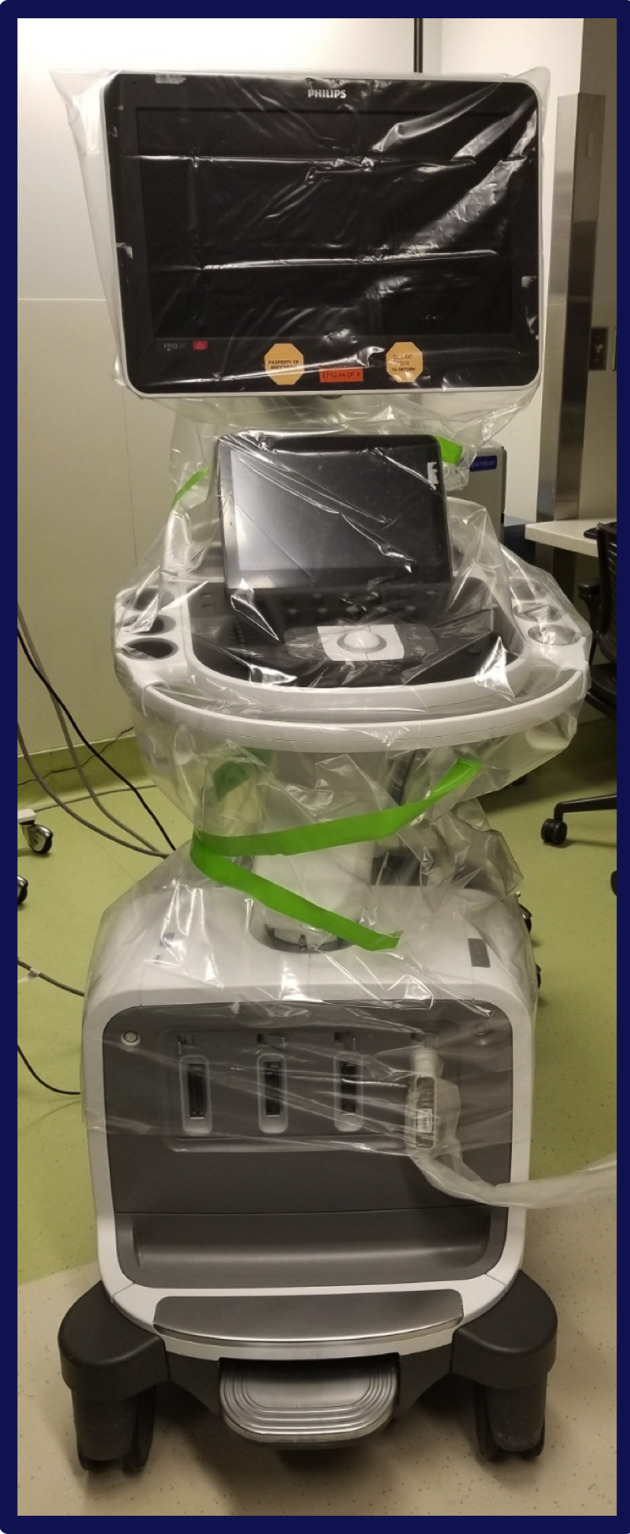
An ultrasound system with transesophageal echocardiographic capabilities is shown with a plastic cover. The screen, touchable parts, and transducer ports are covered by the disposable plastic cover.
A practical approach is suggested in Table 1 . Following a transesophageal echocardiographic examination, all exposed equipment should be wiped down with a hospital-approved and vendor-recommended disinfection product in the procedure or intensive care room and in the induction room or anteroom. The transesophageal probes should also be thoroughly wiped (including handle, cable, and connector), placed in closed containers, and transported in those containers to the cleaning facility. The equipment surfaces should stay wet with the disinfection solution for the minimum recommended “wet time” provided on the product label.
Table 1.
Suggested stepwise approach to performing TEE in a patient with suspected or confirmed COVID-19
Before the procedure
|
During the procedure
|
After the procedure
|
Role of Learners
The educational benefit for trainees of performing TEE in the perioperative period in patients with suspected or confirmed COVID-19 should be weighed against the potential for prolonging the examination time, the risk for contamination and cross-contamination, and the additional use of PPE. One approach would be to have trainees involved in interpreting and reporting but not in performing these examinations. As institutional practices may vary, if trainees in advanced fellowship programs are involved in performing these examinations, they should be knowledgeable and trained in the institutional protocols to reduce infection transmission. This group does not recommend the involvement of medical students and residents in performing perioperative TEE in patients with suspected or confirmed COVID-19.
Conclusion
The performance of TEE carries a heightened risk for transmission of SARS-CoV-2. This risk may be greater in nonintubated patients. TEE should be avoided in these patients and alternative imaging modalities considered. TEE should be performed in intubated patients only in those perioperative situations in which the benefits outweigh the risks. Careful consideration and practice of the recommendations above may help reduce the risk for transmission and cross-contamination.
Footnotes
Notice and Disclaimer: This statement reflects recommendations based on expert opinion, national guidelines, and available evidence. Our knowledge with regard to COVID-19 continues to evolve, as do our institutional protocols for dealing with invasive and noninvasive procedures and practice of personal protective equipment. Readers are urged to follow national guidelines and their institutional recommendations regarding best practices to protect their patients and themselves. These reports are made available by the American Society of Echocardiography (ASE) as a courtesy reference source for its members. The reports contain recommendations only and should not be used as the sole basis to make medical practice decisions or for disciplinary action against any employee. The statements and recommendations contained in these reports are primarily based on the opinions of experts, rather than on scientifically verified data. ASE makes no express or implied warranties regarding the completeness or accuracy of the information in these reports, including the warranty of merchantability or fitness for a particular purpose. In no event shall ASE be liable to you, your patients, or any other third parties for any decision made or action taken by you or such other parties in reliance on this information. Nor does your use of this information constitute the offering of medical advice by ASE or create any physician-patient relationship between ASE and your patients or anyone else.
Conflicts of interest: None.
References
- 1.Practice guidelines for perioperative transesophageal echocardiography. A report by the American Society of Anesthesiologists and the Society of Cardiovascular Anesthesiologists Task Force on Transesophageal Echocardiography. Anesthesiology. 1996;84:986–1006. [PubMed] [Google Scholar]
- 2.Practice guidelines for perioperative transesophageal echocardiography. An updated report by the American Society of Anesthesiologists and the Society of Cardiovascular Anesthesiologists Task Force on Transesophageal Echocardiography. Anesthesiology. 2010;112:1084–1096. doi: 10.1097/ALN.0b013e3181c51e90. [DOI] [PubMed] [Google Scholar]
- 3.Kirkpatrick J.N., Mitchell C., Taub C., Kort S., Hung J., Swaminathan M. ASE statement on protection of patients and echocardiography service providers during the 2019 novel coronavirus outbreak. J Am Soc Echocardiogr. 2020;33:648–653. doi: 10.1016/j.echo.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bowdle A., Munoz-Price L.S. Preventing infection of patients and healthcare workers should be the new normal in the era of novel coronavirus epidemics. https://anesthesiology.pubs.asahq.org/article.aspx?articleid=2763452 Anesthesiology. Available at: [DOI] [PMC free article] [PubMed]
- 5.He H., Zhao S., Han L., Wang Q., Xia H., Huang X. Anesthetic management of patients undergoing aortic dissection repair with suspected severe acute respiratory syndrome coronavirus-2 infection. https://www.jcvaonline.com/article/S1053-0770(20)30270-6/fulltext J Cardiothorac Vasc Anesth. Available at: [DOI] [PMC free article] [PubMed]