Respiratory tract infections (RTIs) constitute a major health problem, with significant cost and mortality rates worldwide. Laboratory methods for the identification of infectious agents that cause respiratory illness are aimed at (1) direct detection by microscopic or antigenic techniques, (2) isolation by means of culture and antibiotic susceptibility testing if needed, (3) serologic evidence of infection in the patient (antibody detection), and (4) molecular genetic detection.
Clinicians should be able to suggest the suspected etiologic agent to facilitate the most cost-effective diagnostic approach and prevent infections from occurring among laboratory staff. Moreover, information should be provided about patient's basic demographic data, clinical condition and history of present illness, antibiotic treatment, immune status, and recent travel or potential exposure. In general, the necessary prerequisites for a successful diagnosis are the collection of an appropriate respiratory and blood sample, prompt transportation in a suitable medium, and laboratory processing within an acceptable time interval.
Laboratory diagnosis of respiratory viral infections
Acute viral respiratory illnesses are the most common reason for hospitalization of children in the United States.1 Respiratory virus diagnosis may be important for a number of reasons including epidemiologic studies; avoidance of hospitalization; reduction in hospital stay and diagnostic workup; decrease in rates of unnecessary antibiotic administration; timely antiviral treatment; and decisions on isolation of infected children to prevent hospital-acquired infections.
Brief Overview of Viruses Involved in Respiratory Illness
The most prevalent are rhinoviruses (RVs) or “common cold” viruses that belong to the picornavirus (small RNA) family, which also includes the enteroviruses (e.g., poliovirus, echovirus, and Coxsackie virus) as well as cardiovirus and aphthovirus. Over 100 RV serotypes have been identified; these are divided into major (90% of serotypes) and minor groups that use as their cellular receptor the intercellular adhesion molecule-1 (ICAM-1) and the low-density lipoprotein (LDL) receptor, respectively. RV-induced colds are closely related to social contact, and peaks are usually seen when children return to school after a vacation period. They usually cause mild disease, but one of the most prominent roles of RV is the triggering of asthma exacerbations.2 Replication is more active in the nose compared to the mouth and pharynx. RVs, however, may also replicate in the lower airway, as demonstrated with the use of molecular biology-based detection techniques.3 Although the severity of upper respiratory tract (URT) symptoms after RV infection does not differ between patients with asthma and normal subjects, both the duration and the severity of lower respiratory tract (LRT) symptoms are more pronounced in patients with asthma.4 LRT epithelial cells of asthmatics demonstrate a deficient innate immune response to RV infection, resulting in diminished apoptosis and accentuated late cytotoxicity.5, 6 Furthermore, RV-infected LRT epithelium is a rich source of inflammatory mediators and growth factors that may trigger or propagate airway inflammation and remodeling.7
Respiratory syncytial virus (RSV) belongs to the Pneumovirinae subfamily and is a medium-sized (100 to 300 nm) RNA virus. Variations in the attachment glycoprotein of the viral envelope give rise to the two antigenically distinct strains of RSV, namely A and B. The majority of studies report that A strains are more common and produce more severe disease. RSV enters the body through the eye or nose and, to a lesser extent, through the mouth. The virus subsequently spreads along the airway mucosa, mostly by cell-to-cell transfer along intracytoplasmic bridges, and also through aspiration from the upper to the lower airway. RSV follows a well-characterized epidemiologic pattern, with yearly outbreaks occurring between October and May in temperate climates. In infants, maternal antibodies reach nondetectable levels at 6 months of age. At least half of the infant population becomes infected during their first RSV epidemic, and almost all children have been infected by 2 years of age. During the first infection, IgM is detected after the first week and IgG during the second week. RSV infection does not confer immunity, and re-infection is common throughout life. All immunoglobulin classes appear, and after three episodes, titers approximate those of adults.8 Although infection usually leads to mild respiratory illness, which is indistinguishable from other viral infections of the RT, some infants have more severe disease. Bronchiolitis is the characteristic clinical manifestation of such infection. There is evidence that hospitalizations for bronchiolitis—now the most common reason for admission among neonates (> 125,000 per year in the United States)—have considerably increased during recent decades and that hospitalized children have an increased probability of wheezing later in life (with immune status of the host probably playing an important role in the process).
Three types of influenza virus (IFV) have been identified; they are designated A, B, and C, and they belong to the orthomyxovirus family of viruses. They are negative-stranded segmented RNA viruses. The two IFV envelope glycoproteins hemagglutinin (H) and neuraminidase (N) determine both viral entry into target cells (by binding to sialic acids and fusing with cellular membrane elements) and the release of the virus. Infection with IFV occurs via respiratory droplets, and infected cells become round and swollen with pyknotic nuclei. The progressive changes in epithelial cells suggest that infection starts in the trachea and then ascends or descends. The epidemiology is characterized by yearly epidemics lasting for 6 to 8 weeks during late winter; each year, there is usually only one dominant type or subtype. Illnesses initially appear in children, among whom the incidence of infection is higher, virus shedding is prolonged, and transmission to the community is greater. Later in the epidemic, more adults are affected. Viruses are present in the community before and after the epidemic, causing illness at a low frequency. Antigenic variation readily occurs in H and N primary structures, giving rise to new subtypes (antigenic shift) and to intrasubtype changes (antigenic drift). Antibodies against H appear 2 weeks after infection and are protective for the specific subtype that caused the disease. Type A IFV has been associated with pandemics that have occurred every 10 to 40 years. Swine flu (a new subtype of IFV A H1N1) was the agent responsible for the 2009 pandemic, with higher pediatric mortality and higher rates of hospitalizations in children and young adults than in previous seasons, while asthma appeared to be a significant risk factor for developing severe disease.
Human parainfluenza viruses (PIVs) include four RNA viruses, numbered 1 to 4, and belong to the Paramyxoviridae subfamily, together with mumps and measles. Each PIV has distinct epidemiologic and clinical characteristics, as well as different age distribution patterns. PIV 1 and PIV 2, members of the Respirovirus genus, are generally associated with laryngotracheobronchitis (croup), URT illness, and pharyngitis, whereas PIV 3, a member of the Rubulavirus genus, is also a major cause of infant bronchiolitis and is associated with the development of pneumonia in susceptible subjects. PIV 4 is rare and less well studied. PIV 1 occurs in biennial epidemics during autumn, coinciding with croup outbreaks; its peak incidence occurs in children 2 to 3 years of age. PIV 2 epidemics are less predictable; however, they more or less follow the biennial pattern of PIV 1, affecting mostly children younger than 5 years of age. PIV 3 is more frequent and infects infants < 6 months of age in yearly epidemics during spring and summer. Infection is mediated by interaction of the viral H and N glycoproteins with cellular sialic acid receptors. Protective antibodies against H and N appear early (1 to 2 weeks after infection) and persist for several years. Several infections are needed, however, for full protection. For transmission, aerosol spread is considered important, although deposition on surfaces and subsequent self-inoculation may also occur. Virus replication can occur throughout the tracheobronchial tree, causing local inflammation; however, only mild and rapidly repaired focal tissue destruction is observed in vivo. In immunocompromised hosts, fatal giant cell pneumonia may develop. Central to the pathogenesis of PIV infection is the ability of these viruses to escape interferon-mediated immune responses.9
In contrast to the rest of the respiratory viruses, adenoviruses (AdVs) are deoxyribonucleic acid (DNA) viruses. This large family of viruses includes 6 subgenera and more than 50 serotypes. Their overall size is 70 to 90 nm; the virion is naked and contains 36 to 38 kb double-stranded DNA, encoding > 50 polypeptides from both strands. Some of these proteins allow efficient endosomal lysis and escape, leading to genome entrance into the host cell nucleus. The propensity of AdVs to shut off the expression of host messenger RNA and induce excess synthesis of adenoviral proteins leads to an accumulation of such proteins as intranuclear bodies, which are incompatible with normal cell function. In upper airway epithelial cells, ciliary and microtubular abnormalities lead to defective mucociliary clearance. An important feature of AdV is its ability to persist in the host for a long time, through low-grade replication, or for even longer periods, with production of adenoviral proteins without replication of a complete virus. AdVs may cause pneumonia, bronchiolitis, or conjunctivitis, while infection after solid organ or bone marrow transplantation can induce severe myelosuppression. The duration of virus isolation is 3 to 6 weeks from the pharynx or stool of children with RTI and 2 to 12 months in immunosuppressed patients. Antibodies that bind to complement appear 1 week after infection, remain for 1 year, and recognize the hexone antigen, which is common for all AdVs. Neutralizing antibodies develop against the specific serotype that caused the infection, and the titer remains stable for over a decade.
Human coronaviruses (HCVs) are RNA viruses that were isolated during the mid-1960s. The majority of HCVs studied to date are related to one of two reference strains, designated OC43 and 229E, which differ extensively. NL63, which was isolated from an infant with bronchiolitis and conjunctivitis, is a new group I HCV that shares 65% sequence identity with 229E.10 Human aminopeptidase N, which is present on lung, intestinal, and renal epithelial cells, has been identified as a receptor for HCV 229E. OC43 binds to major histocompatibility complex class I molecules. Viral replication has been demonstrated in the nasal mucosa, inducing inflammation, ciliary damage, and epithelial cell shedding, although its in vivo cytopathic effect (CPE) is not pronounced. Volunteers can be successfully infected by intranasal inoculation, although replication in the lower airway has not been confirmed. HCV causes approximately 15% of common colds, which are usually mild. In general, HCVs may cause milder LRT symptoms than other viruses, with some exceptions of more severe LRT involvement in young children and the elderly.
The Eastern Asia–based SARS epidemic has been attributed to a new HCV with limited homology to the other known HCVs.11 Sequencing of the Tor2 isolate showed a number of distinctive features of its genome (e.g., several small, open reading frames between its genes) that are of potential biologic significance.12 The virus causes diffuse alveolar damage, with interstitial infiltrates. After 3 to 7 days of fever, a nonproductive cough may progress to dyspnea and hypoxemia in 15% of patients. The associated mortality rate is 3% to 6% (or as high as 43% to 55% when considering patients older than 60 years of age), but it is much lower in children.13 The appearance of IgM and IgG antibodies takes place at the same time, with the former remaining for 11 weeks and the latter for months and possibly for years.
Finally, a new respiratory RNA virus, human metapneumovirus (MPV) of the Metapneumovirus genus, was isolated in 2001 from the nasopharyngeal aspirates of young children in the Netherlands.14 MPV was later shown to be responsible for a significant proportion of RTI in children worldwide. This new virus proved to have paramyxovirus-like pleomorphic particles on electron microscopy (EM), while there are two potential genetic clusters. The clinical symptoms of the children from whom the virus was initially isolated ranged from URT disease to severe bronchiolitis and pneumonia.14 Subsequent studies, conducted in different locations and using mixed patient populations with various respiratory symptoms, established the association of this virus with acute respiratory illness in both the URT and LRT, and in all age groups.15
Treatment of Clinical Samples
Samples that are intended for polymerase chain reaction (PCR) should be maintained at –70° C in order to minimize degradation of nucleic acids. For the same purpose, tubes, solutions, and buffers that are used for the collection, transport, and processing of samples should be ribonuclease free.
Blood Specimen
Infrequently, blood may be collected for PCR on serum or cells (usually on white blood cells), antigen detection, or serology. PCR on white blood cells requires that whole blood be sent at room temperature in tubes that contain ethylenediaminetetraacetic acid (EDTA) or citrate (heparin may inhibit the polymerase during subsequent PCR) and that cells be extracted within 24 hours of collection. Antigen assays may also be performed on the Buffy coat; however, clotted whole blood is needed for PCR on serum. For serology, an acute sample of clotted blood is collected as early as possible during the course of the disease, and a convalescent sample is sent 2 to 3 weeks later. Ideally, at least 2 mL of blood is obtained, although in infants less will often suffice. The sample should arrive in the laboratory within 1 day and should not be frozen, as this will provoke hemolysis. In the laboratory, serum is separated from the clot and stored at –20 ° C for future processing.
Upper Respiratory Tract Specimen
Samples collected during the first days of symptoms (when viral shedding is maximal) lead to higher recovery rates. URT samples include material from the rhinopharynx and oropharynx, with the former providing a lower rate of contamination by lower respiratory components. Throat swabs should be collected vigorously to ensure that mucus and cellular material is obtained from the pharynx, while in older children throat gargles can be obtained. Nasal wash is shown to produce the highest viral detection rate and relatively low patient discomfort compared to swabs, aspirates, and brushings.16 Specimens should be placed in viral transport medium (VTM) in the presence of antibiotics to inhibit bacterial growth. Usually this is contained in a small sterile bottle, and, after immersion, the wooden shaft of the swab is broken level with the neck of the container, the cap is replaced, and the fluid is gently agitated. VTM prevents drying and maintains viral viability during transport and contains either Eagle's minimum essential medium or Hank's balanced salt solution, along with fetal bovine serum or bovine serum albumin (BSA). When the time interval between collection and delivery is less than 2 hours, specimens should be transferred to the laboratory at room temperature; when the time interval is 2 to 24 hours, they should be transferred on ice. When the time interval is more than 24 hours, specimens should be surrounded by solid CO2 and packed in an insulated container. Specimens suspected of containing RSV should not be frozen; they must be transferred to the laboratory as soon as possible. They can also be used to prepare slides for immunofluorescent detection, either by rolling the swab directly on the slide or after recovery of cells by centrifugation.
Lower Respiratory Tract Specimens
Specimens from the LRT are usually obtained in the setting of an immunocompromised child (early in the course of a pulmonary infection) or in the immunocompetent child with severe atypical pneumonia. Although induced sputum is often contaminated by oropharyngeal components that hinder viral recovery, it is an easily obtainable sample, at least in older children, in whom the success rate is > 70%. Therefore, it is often used after either filtration through 200-nm membrane filters or dilution, usually in the presence of a reducing agent such as 0.1% dithiothreitol (DTT) to reduce the viscosity. Transtracheal and bronchial aspirates, and bronchial biopsy specimens are all considered better sources than sputum for both culture (in VTM at 4 ° C) and direct immunodetection of viruses in pelleted cells (a few drops in a container without VTM). Similarly, after mild centrifugation (10 minutes, 500 × g), both the supernatant and the pellet of bronchoalveolar lavage (BAL) are good sources for isolation and immunofluorescent detection of respiratory viruses.
Pulmonary biopsies are suitable for EM; BAL and nasopharyngeal aspirate (NPA) samples that are intended for EM should not be diluted with VTM because it contains salts and proteins that obscure the field and dilute viral particles.
Diagnostic Techniques
A variety of methodologies have been developed for the diagnosis of respiratory virus infections, each with different characteristics (Table 24-1 ).
Table 24-1.
Comparison of Respiratory Virus Diagnostic Techniques
| Method Characteristics | Culture | Immunofluorescence (IFA, DFA) | Enzyme-Linked Immunosorbent Assay (ELISA) | Use of Probes Without Target Amplification | Polymerase Chain Reaction (PCR) |
|---|---|---|---|---|---|
| Speed | + | +++ | +++ | ++ | ++/+++ |
| Sensitivity | +++ | ++ | ++ | ++ | ++++ |
| Specificity | +++ | ++ | ++ | +++ | ++++ |
| Quantitative measurement | ++ | ++ | ++ | + | +++ |
| Ease of use | + | + | +++ | + | ++/+++ |
| Cost | ++ | + | + | ++ | +++ |
Modified from Myint S. Recent advances in the rapid diagnosis of respiratory tract infection. Br Med Bull. 2002;61:97-114.
Virus Cultures
Culture of a virus from a clinical specimen confirms the presence of viable virus.
Cell Culture
For each respiratory virus, there are a number of cell lines that allow its replication in vitro (Table 24-2 ). Susceptible cell cultures may undergo degenerative processes on exposure to respiratory viruses. The speed at which these appear is usually characteristic for a particular virus (e.g., 2 to 5 days for RSV). The most common CPE patterns include syncytia formation (fusion of many cells in multinucleated structures), vacuolation (generation of large, bubblelike regions in the cytoplasm), and granular degeneration. Rounding and detachment are also common features (Fig. 24-1 ).
Table 24-2.
Cell Lines Commonly Used for Identification of Respiratory Viruses
| Cell Line | Origin | Type | Virus |
|---|---|---|---|
| A549 | Human alveolar adenocarcinoma | Continuous | AdV, RSV |
| HeLa | Human cervical carcinoma | Continuous | AdV, RSV, RV |
| Hep-2 | HeLa contaminant | Continuous | AdV, RSV |
| HEK | Human embryonic kidney | Primary | AdV |
| LLC-MK2 | Monkey kidney | Continuous | IFV, PIV, HCV-NL63 |
| MDCK | Canine kidney | Continuous | IFV |
| MRC-5 | Human fibroblasts | Cell strain | AdV, HCV |
| MRC-c/C16 | Human fetal lung fibroblasts | Continuous | HCV |
| Mv1Lu | Mink lung | Continuous | IFV |
| PMK | Monkey kidney | Primary | IFV, PIV |
| tMK | Monkey kidney | Continuous | MPV |
| Vero E6 | Monkey kidney | Continuous | SARS-CoV |
| WI-38 | Human lung fibroblasts | Cell strain | RV, HCV |
Figure 24-1.

Cytopathic effect caused by human rhinoviruses in vitro.A, Primary cultures of human bronchial epithelial cells were infected by RV7 at a multiplicity of infection of 10, and characteristic shrinkage and rounding can be seen in some cells (arrow) 24 to 48 hours later, whereas the rest of the monolayer remains intact. B, At later time points, fully developed cytopathic effect gradually leads to cellular detachment, cell debris, and separation of the cell layer.
The dose that causes CPE in 50% of inoculated cells (TCID50) is used to express the content of a given viral preparation (titer). Alternatively, when the cell monolayer is permitted to grow covered by a solid (agar) medium, the foci of virus-infected cells form plaques that may be stained by specific dyes (e.g., neutral red) in a manner different from uninfected cells, and these can be readily identified and counted.
Viruses that possess H (e.g., IFV and PIV) may be able to adhere to erythrocytes of the host in which they replicate. When a suspension of erythrocytes derived from a suitable species is added to the infected cell culture, they adhere in clumps after a certain period.
Rotation enhances the yield of a cultured virus, while liposomal and other agents added in the media, as well as centrifugation protocols, may increase the detection rate. In addition, a virus can be isolated by culturing cells from a biopsy sample. However, co-culture with helper cells often leads to higher recovery rates because this technique overcomes the viral inhibitory activity of certain tissue homogenates.
Cell culture can be used in two additional ways for the identification of respiratory viruses. First, sera from patients can be assessed for the ability to inhibit the CPE, plaque formation, or hemadsorption activity normally triggered by a stock viral solution of known infectivity. Conversely, virus strains isolated from patients can be exposed to specific immune sera known to prevent such activities, and the final result can be assessed on the cell culture.
In many cases, cell culture remains the gold standard, often achieving the highest sensitivity scores and providing an isolate for epidemiologic and typing purposes or antiviral susceptibility assays. However, it is a rather time-consuming process that demands several days to weeks and many skilled personnel before results can be obtained. More rapid protocols that use a combination of cell culture with another detection method (e.g., immunofluorescence [IF]-, EM-, or PCR-based methods) have recently been developed. With these techniques, the sample is inoculated onto the culture, and the presence of replicating virus is verified after 24 to 48 hours by the second method.
In an interesting advance, IFV-susceptible, mink lung–derived Mv1Lu cells and the human adenocarcinoma A549 cell line were co-cultured in shell vials to detect respiratory viruses. The R-mix monolayers that can be used directly from cryopreserved vials are inoculated on coverslips with the clinical sample, and 24 hours later the coverslips are removed and stained with a mixture of antisera against many respiratory viruses. If a positive signal is present, cells from a parallel coverslip can be dispersed onto a suitable chamber containing multiple coverslips that can be examined separately for the presence of individual respiratory viruses using monoclonal antibodies. Using this method, definitive results can be obtained within 2 days.17 However, in conventional single-cell–culture CPE observation, the respective result takes approximately 10 days. Although of similar sensitivity to conventional cell culture and direct IF with respect to most respiratory viruses (IFV, PIV, and RSV), this method is less sensitive in detecting AdV.18
Eggs
Fertile eggs are used for the culture of respiratory viruses (e.g., IFV) after being chilled to prevent the release of red blood cells and subsequent virus loss due to cell adsorption. Inoculation into the amniotic cavity is used mainly for the isolation of such viruses from clinical samples. Harvesting is usually conducted 48 to 72 hours after inoculation.
Animals
Inoculation of a susceptible animal is a common practice for the detection of many viruses. In the SARS epidemics, for instance, one of the first tests to identify the virus was intracranial and intraperitoneal injection of clinical samples into suckling mice, with observation of the mice for 14 days for pathologic findings.11 Other examples include AdV serotype 5, which when given intravenously to adult mice, kills them within 3 to 4 days, whereas other AdVs, when administered subcutaneously to newborn hamsters, cause their death within 4 to 12 days.
Detection of Whole Viruses by Electron Microscopy
This is the only method that allows direct inspection of viruses, detects pathogens that are difficult to cultivate, and is applied during epidemics of unknown etiology. Preparation of samples and negative staining techniques are fast, easy, and inexpensive processes. On the other hand, the sensitivity limit is approximately 106 viral particles/mL, which renders detection difficult after the first days of infection. Also, EM requires expensive equipment and skilled personnel and cannot differentiate between infectious and noninfectious organisms.
Fluid Samples
In a typical protocol, a 300- or 400-mesh grid is placed on a drop of sample for 5 to 15 minutes. After draining with filter paper, the grid can be stained. Fluid samples should be placed on support films, made either from Collodion films (2% solution in isoamyl acetate) or from the mechanically stronger 0.3% to 0.5% polyvinyl formal in ethylene dichloride (Formvar solution). The films are cast on a glass slide by experienced personnel, and grids are made by pressing the grid onto the film slide in the presence of water. A silver-gray rather than charcoal-gray or gold color coincides with optimal film thickness, and additional carbon coating under vacuum facilitates spreading of the sample, which improves the results. Glow discharging under the vacuum or treatment of the grids with a suitable agent (e.g., poly-l-lysine, Alcian blue, Cytochrome C, or BSA) is commonly used to overcome spreading problems.
Concentration of particles contained in BAL and NPA samples is recommended. This can be achieved with ultracentrifugation, ultrafiltration, or agar diffusion. With agar diffusion, a drop of suspension is placed on top of 2% agar, in which liquid and salts diffuse, leaving a film-coated grid containing the virus that can be drained on filter paper and stained for EM. The pseudoreplica technique is a variation whereby the drop is allowed to diffuse into the agar and then is irradiated and covered by Formvar film. Then the Formvar membrane is carefully removed and allowed to float onto a water surface. Grids are then applied on the replica membrane and picked up with the aid of filter paper.
Antibodies are also used for the concentration of viruses in suspension (clumping). For aggregation, the samples can be incubated with the antiserum, centrifuged, and placed onto grids with the pseudoreplica technique; alternatively, antiserum is mixed with agar, and a grid is placed onto the gel. Virus suspension is then added and allowed to absorb, followed by removal and staining of the grid. In solid-phase immunoelectron microscopy, the film is coated with antibodies before incubation with virus suspension.
Immunoprecipitation techniques are particularly helpful when picornaviruses need to be detected. These viruses are so small that they sometimes appear similar to lipid droplets. Some viruses tend to clump in the absence of antiserum, reducing the specificity of this procedure. Viruses in suspension or on grids can be incubated with primary antiserum, allowed to aggregate, and after the antibody has been washed away, the preparation can be treated with a colloidal gold-labeled secondary antibody. Gold labeling has been used specifically to detect immune complexes in serum, as well as subviral particles. In a somewhat different approach, viruses are exposed to excess antibodies, resulting in extensive coating rather than aggregation of the viruses. This method allows specific identification and serotyping of viruses and can serve to assess the reactivity of convalescent serum against known viruses.
Finally, short-term culture of virus in vitro with harvesting before the appearance of the CPE is a good alternative for the enrichment of a sample. AdVs and paramyxoviruses can be detected in supernatants before a massive CPE occurs. On the other hand, AdV is membrane-associated and may be lost on removal of the debris with centrifugation.
An additional problem with NPA specimens is the presence of mucus, which inhibits spreading of the samples. These specimens can be treated with an equal volume of a DTT-containing buffer to break down the mucus.
Biopsy Specimens
Specimens should be placed in 2% to 5% glutaraldehyde in cacodylate or phosphate buffer and stored at -20 ° C to maintain the tissue architecture and specifically localize the virus. Osmium fixation (1% to 2% OsO4 in a 4-[2-hydroxyethyl]-1-piperazineethanesulfonic acid [HEPES] or a piperazine diethanesulfonic acid [PIPES]–based buffer) is also used. En bloc staining can then be conducted with uranyl acetate in veronal buffer. Otherwise, dehydration and embedding in resins should follow the fixation step. Although it is not optimal, formalin-fixed material and paraffin-embedded sections can also be used for EM after suitable treatment. Because the sample area used is limited, it is wise first to stain sections with suitable stains (e.g., toluidine blue) to select areas of particular interest (e.g., with a CPE) and then trim the sections further for thin sectioning. Viruses can also be seen by extracting solid tissue with a suitable buffer after homogenization or repeated freezing and thawing, and further treatment as a liquid sample. Thin sectioning is also the method of choice for identification of virus in cell culture. If the virus has triggered cell lysis, it can be detected in cell supernatant or medium (after ultracentrifugation is performed to remove the debris), followed by negative staining of the pellet. Cells can also be embedded in agar and further treated as tissue blocks.
Electron Microscopic Appearance of Respiratory Viruses
Table 24-3 summarizes the main morphologic characteristics of respiratory viruses. Picornaviruses and AdVs are naked virions of icosahedral symmetry and a round appearance on EM. AdVs have the higher size ranges among naked virions, while picornaviruses are very small and are often confused with some tailless bacteriophage species. Immunoprecipitation techniques can be used in such cases. In addition, AdVs can degenerate, and individual capsomers may appear separately, forming hexagonal lattices. Enveloped respiratory viruses (e.g., IFV, PIV, and HCV) have a soft membrane that can become deformed during drying for negative staining. Thus, the particles may appear pleomorphic, and may vary in size. The enveloped respiratory viruses are spiked, rather than smooth. HCVs have long (20-nm) spikes on the surface, whereas paramyxoviruses and orthomyxoviruses contain projections that appear as a fringe on the outer side. However, even these forms can sometimes be confused with mitochondria or inverted bacterial membrane debris. Discrimination between orthomyxovirus and paramyxovirus families is often challenging.
Table 24-3.
Main Morphologic Characteristics of Respiratory Viruses
| Virus | Envelope | Capsid Symmetry | Genome | Virion Size (NM) | Projections (NM) | Nucleocapsid Size (NM) |
|---|---|---|---|---|---|---|
| AdV | No | I | ds DNA | 70–90 | ||
| RV | No | I | + sRNA | 24–30 | ||
| HCV | Yes | C | + sRNA | 80–150 | 20 | 10–20 |
| SARS-CoV | Yes | C | + sRNA | 80–140 | 20–40 | |
| IFV | Yes | H | - sRNA | 80–120 | 9–15 | |
| PIV | Yes | H | - sRNA | 150–250 | 12–18 | |
| MPV | Yes | H | - sRNA | 150–600 | 13–17 | |
| RSV | Yes | H | - sRNA | 100–300 | 12 | 6–7 |
C, Complex; H, helical; I, icosahedral; +/– sRNA, negative or positive sense single-stranded RNA.
The cellular location of viruses in thin sections of solid tissues also provides important evidence of their properties (e.g., DNA viruses replicate in the nucleus, whereas RNA viruses replicate in the cytoplasm). Naked viruses, such as AdVs, cause cell lysis and can be seen as round shells with a core of different density surrounded by dead cells. If the cytopathology is advanced, AdVs may be seen in both the nucleus and the cytoplasm. Picornaviruses cause swelling of the endoplasmic reticulum, and the ribosomes may appear as large beads on a string. Enveloped viruses acquire their membranes by budding through the nuclear envelope, through the plasma membrane, or into vesicles within the cells. There are some difficulties in discriminating virions from normal cell organelles (e.g., lysosomes and Golgi complexes); however viruses with spikes appear to have a thicker membrane than the cellular compartments. Nucleocapsids, which contain nucleic acids and viral proteins, are present in enveloped viruses and can be spherical, helical, or complex. PIVs, for instance, have helical filamentous nucleocapsids. AdVs can be discriminated from the otherwise similar but larger herpesviruses by the smaller size of their nucleocapsid.
Transmission electron microscopy (TEM) is a method of reference for the identification of many viruses. TEM allows detection of even one virus particle. However, it needs specialized and expensive instrumentation and skilled technicians. Moreover, it is unable to discriminate among viruses of the same family or among particular subtypes.
Other Whole-Virus Detection Methods
Fluorescent dyes can be used to stain a purified virus preparation and allow enumeration of virus in a solution consistent with data obtained by TEM. OliGreen (a dye that specifically binds to nucleotides) has been successfully used for the enumeration of AdV 5, RSV, and IFV A, and the method can be performed within 1 hour.19 To that end, density-gradient–purified virus preparations are incubated with the dye and subjected to analysis in a modified-flow cytometer. This method also provides information about the virus genome size.
Antigen Detection
Antigen-based detection methods presuppose the knowledge or suspicion that a particular virus is present in the sample and preclude the discovery of unknown viruses. However, they are rapid, accurate, easy to perform, and do not depend on virus viability. Table 24-4 compares the sensitivity and specificity of these methods with cell culture detection of RSV. These features are of major importance for the surveillance and control of epidemic diseases (e.g., IFV infection) but are usually not recommended among the immunosuppressed, the elderly, and at times when prevalence is low in a community. Thus, the American Academy of Pediatrics does not recommend the routine use of antigen-detection assays for the diagnosis of RSV infection because it is thought that it does not influence the management of the patient who has been clinically diagnosed with bronchiolitis.20 Viral antigens can be revealed based on the ability of the antigen to interact with an antibody or to elicit a specific immune response. In addition, specific functional assays (e.g., hemagglutination tests that assess the presence of particular proteins that are found in the envelope of orthomyxoviruses and paramyxoviruses) can be conducted to reveal the respective virus. These are described in the section on “Serologic Methods” later in the chapter.
Table 24-4.
Rapid Diagnostic Methods for RSV Based on Antigen Detection Compared to Cell Culture Techniques
| Method | Sensitivity (%) | Specificity (%) |
|---|---|---|
| IFA/DFA | 93-98 | 92-97 |
| EIA | 59-97 | 75-100 |
| DIA | 93 | 91 |
| OIA | 88-95 | 97-100 |
IFA/DFA, Indirect immunofluorescence/direct immunofluorescence; EIA, enzyme immunoassay; DIA, direct enzyme immunoassay; OIA, optical immunoassay.
Modified from Henrickson KJ, Hall CB. Diagnostic assays for respiratory syncytial virus disease. Pediatr Infect Dis J. 2007;26:S6-S40.
Immunoassays
Immunoassays are laboratory tests based on the use of antibodies and are routinely used in the diagnosis of infectious diseases.
Immunofluorescence
Immunofluorescence (IF) is based on the chemical conjugation of a fluorochrome with an antibody, without compromising either the ability of the fluorochrome to fluoresce or the specificity of the antibody. Fluorescein isothiocyanate and tetramethyl rhodamine isothiocyanate are the most widely used fluorochromes; the former fluoresces yellowish-green, whereas the latter appears reddish-orange. Fluorescein isothiocyanate seems to be more suitable for clinical samples because the background is more often red than green. In addition, red-fluorescing dyes (e.g., Congo red) can be used to stain all cellular components red and provide a contrast to the green fluorescence of fluorescein isothiocyanate. A fluorescence microscope is required for the detection of light emitted by excited fluorochrome, and the interpretation of results is partially subjective, depending on the experience of the examiner. In modern fluorescence microscopes with epi-illumination systems, light of selected wavelengths is deflected through the objective to the top surface of the sample. The resulting emitted light is directed to the observer through the objective, a dichroic mirror, a barrier filter, and the oculars. Each fluorochrome has specific fluorescence characteristics. For instance, fluorescein isothiocyanate absorption is at 495 nm, and emission is at 525 nm. With the available interference filters in fluorescence microscopes, 85% of transmitted light is between 400 and 500 nm (i.e., the visible part of the spectrum).
Practically, the sample should be fixed onto a slide first. Thereafter, it is incubated, either with a specific antibody conjugated with a fluorochrome (direct immunofluorescence assay [DIF]) or with a primary specific antibody and thereafter with a secondary antibody raised against the primary one that has been conjugated with the fluorochrome (indirect immunofluorescence assay [IIF]). The first method is less sensitive, but it avoids nonspecific staining of negative samples, as is often seen with the indirect method. However, the generation of primary conjugates for many viruses is laborious and costly, whereas secondary conjugates may be common for several antigens. Incubation times are short for both procedures (30 to 45 minutes, 37 ° C), making IF a good method for rapid virus detection.
Viral samples can also be detected by IF with spin cultures, whereby suitable cell monolayers are grown on coverslips within flat-bottom vials. The sample is then applied on top of the coverslip, and the vial is centrifuged (650 to 900 × g, 30 to 60 minutes). This technique facilitates virus entry into the target cells, and usually the coverslip is removed, fixed, and stained for IF, 18 to 24 hours later.
DIF and IIF have been used for the development of a number of rapid tests for the detection of respiratory viruses. These can be accomplished within a few minutes, and they have become very popular due to their rapidity and ease of performance. Usually, a spot or slide containing the sample is prepared for every virus being tested, cytospun, and incubated with the monoclonal antibody. In a recent advance, a single spot can be used for the simultaneous detection of seven respiratory viruses (RSV, IFV A and B, AdV, and PIV 1 to 3).21 A rhodamine label is used with the RSV antibody system, whereas fluorescein is used in all other cases. Thus, the development of a reddish-gold color in the spot suggests the presence of RSV particles in the sample, whereas a green color (fluorescein) is followed by a second reaction in another spot to determine which of the other viruses is present. The sensitivity of this method was greatly enhanced by centrifugation and was superior to that of enzyme immunoassay (EIA)–based protocols, but was inferior to that of cell culture.22 Another IIF method proved more efficient than cell culture in detecting respiratory viruses in nasopharyngeal swabs.23
Radioimmunoassay
There are two types of radioimmunoassay (RIA). In competitive RIA methods, a known quantity of radioactivity-labeled antigen competes with unlabeled antigen that is added (test sample). The inhibition of binding of labeled antigen depends on the concentration of unlabeled antigen in the clinical sample. The labeled antigen that is finally bound to antibody is measured and referred to as bound antigen, whereas the unconjugated labeled antigen is referred to as free antigen. To circumvent problems arising from the separation of bound antigen from free antigen in solid-phase RIA, the immunoreactant that is used first (antibody or antigen) is immobilized on a solid support. After each step, unwanted reactants can be removed readily by washing. In contrast to the laborious and expensive generation of labeled viral antigens, noncompetitive RIA methods use labeled antibodies. The former are more stable, with more predictable structures and biochemical properties. Noncompetitive RIAs are, therefore, more popular in diagnostic virology. In a technique known as sandwich RIA, unlabeled viral antibodies adsorbed to a solid-phase support are allowed to capture viral antigens present in the clinical sample. Then a radiolabeled antibody (indicator antibody) is allowed to bind to the captured viral antigens. This procedure can be either direct or indirect. In the latter case, a primary unlabeled indicator antibody is used initially, followed by incubation with a secondary radiolabeled antibody. In all of these procedures, free antibody is removed after the final incubation, and bound iodine-125-labeled antibody is measured.
Nasal aspirates are a suitable source for assessing the presence of respiratory viruses (e.g., RSV) with RIA. For the direct detection of viruses in tissue or cell culture,125 I-labeled viral antibody is incubated with the cell monolayers or tissue sections, and unbound labeled antibody is removed. The bound radioactivity is then measured. The radioactivity bound to the infected tissue or culture is then compared with the radioactivity bound to uninfected control samples. Ratios exceeding 2:1 are considered positive. In the indirect version of this technique, the sample is first incubated with unlabeled antibody, followed by 125 I-labeled secondary antibody.
Enzyme Immunoassays
As indicated by their name, EIAs are based on the conjugation of suitable enzymes (e.g., horseradish peroxidase, alkaline phosphatase [ALP]) to antibodies and their subsequent use for the qualitative and quantitative detection of antigens. Enzyme-labeled antibodies are reacted with substrates that generate soluble color products and are used to detect viral antigens (directly or indirectly) in tissues or cell cultures in cytoimmunoenzymatic staining. Colored substrates can be observed with the naked eye, with light microscopy, with EM (in the case of electron-dense products), or they can be evaluated with a spectrophotometer. As in the IF methods described earlier in the chapter, infected and control cell monolayers and tissue sections on slides are fixed and incubated directly with enzyme-coupled antibody (or with an uncoupled primary and an enzyme-coupled secondary antibody, in the indirect approach). Unbound enzyme conjugate is removed by washing, and the slides are incubated with enzyme substrates. After development of the colored product, the slides are rinsed, counterstained, and mounted in mounting medium to be observed under a light microscope.
A modification of the indirect approach includes an additional step whereby an antibody raised against the enzyme is incubated with the sample. Because this antibody is also conjugated with enzyme, its sensitivity is greatly enhanced. Both peroxidase- antiperoxidase and ALP–anti-ALP are being used, and the final reaction products can be either soluble color complexes or insoluble substrates that can be observed with the naked eye, observed with a light microscope, or measured with a spectrophotometer.
Avidin-biotin is another system that is widely used to increase sensitivity in such approaches. The binding reaction between these two molecules is strong, and it occurs independently of the immune reactions in the assay. In a typical avidin-biotin complex protocol, biotin-conjugated primary antibodies are incubated with the samples, and after the unbound antibodies have been washed out, enzyme-conjugated avidin or streptavidin is added. The complex formed is monitored, with the final addition of substrate and mounting of the slide. In the indirect approach, an unlabeled primary antibody is first incubated with the sample, followed by secondary incubation with biotinylated antibody and the biotin-avidin enzyme complex incubation.
Heterogenous EIA assays, in which unbound enzyme-labeled antibody is removed and incubation is relatively long, are used for quantitation of viral antigens. Like viral RIA assays, quantitative EIAs use unlabeled antiviral antibody bound to a solid phase (e.g., microtiter plates, cuvettes). Unbound antibody is removed after adsorption, and nonspecific binding sites are blocked by blocking agents, such as BSA. After samples are added, unbound material is removed and enzyme-conjugated antibody is added. This antibody binds to antigen captured by solid-phase bound antibody. After removal of unbound material, enzyme substrate is added and the formation of the reaction product is measured. This measurement reflects the amount of enzyme bound to antigen that is retained in the solid phase. Control samples are always included to define the background levels of each modification. IFV, AdV, and RSV can be measured by these methods.
The cassette EIA method is based on the fact that large amounts of antibody can be bound to nitrocellulose, nylon, and other membranes. Such a membrane is attached to a plastic well, and the entire system is attached to a cassette containing a material that can absorb all waste fluid generated during the assay. The antibody and the controls can be dotted or slotted onto the membrane in separate wells. The method offers the advantages of increased sensitivity, reduced time required for its completion, and detection of many different respiratory viruses from many samples. Based on the same principle, numerous variations are used, with different sensitivity scores. The solid phase, for instance, can be substituted by beads coated with antibody. After incubation with the sample, the beads can be transferred to the membranes and the assay can go on as a standard EIA. Alternatively, a classic dot-blot apparatus can be used to place an antibody in dots on the membrane. The additional binding sites on the membrane are then blocked. Samples and controls can then be added as serial dilutions for quantitation, and waste fluids are collected from the associated vacuum system. However, although these systems are able to discriminate between serotypes of the same species (e.g., IFV A versus IFV B), they may not be as sensitive as cell culture or DIF in detecting virus.
Fluoroimmunoassay
In time-resolved fluoroimmunoassay (FIA), the unusually long fluorescence decay time of the lanthanide element Europium (Eu+ 3) is used to discriminate the fluorescence decay characteristics of Europium-conjugated antibodies (Europium is first chelated with ethylenediaminetetraacetic acid [EDTA]) from the fluorescence decay of clinical samples. In a representative protocol, a microtiter plate or strip is coated with antibody and the remaining binding sites of the plates are blocked. The clinical sample is then added simultaneously with the Europium-conjugated antibody, and after incubation, the unbound material is washed out. AdV, RSV, IFV, and PIV have been detected with time-resolved FIA, although sometimes with limited sensitivity.
Optical Immunoassay
An advance in the field of antigen detection is optical immunoassay (OIA) technology. This allows direct visual detection of a macromolecule that is bound onto a molecular thin film. Binding causes an increase in the thickness of the optical surface (silicon wafer film) that will alter the reflected light path and will be perceived as a color change that is observable with the naked eye. Practically, viral-specific antibodies are immobilized on the surface and allowed to capture extracted viral antigens that are placed directly onto the surface and incubated at room temperature for a short period. After addition of a suitable substrate, a positive result appears as a color spot, whereas in the absence of antigens in the sample, the background color remains unchanged. Commercially available tests for IFV and RSV can take as little as 15 minutes to be completed and do not require sophisticated laboratory equipment, although reported sensitivity varies.
Agglutination Assays
In the latex agglutination assay, antibody-coated nanoparticles from polystyrene, polyacrylamide, and other latexes; agarose beads; or colloidal gold agglutinate in the presence of viral antigens. In a typical protocol for respiratory viruses, a clarified and diluted NPA sample is mixed with antibody-coated latex particles on a microscope slide. The method is simple, and an agglutination reaction can be observed usually after 10 to 15 minutes, but the overall sensitivity and specificity are low.
Serologic Methods
As indicated by the name, serologic methods attempt to detect viruses in the host by assessing the presence of specific antibodies in blood samples, but sputum and urine also may be used. Serology is a rather sensitive, specific, and relatively cheap diagnostic technique that is also used to confirm the results of other methods. There are five classes of human immunoglobulins: IgG, IgM, IgA, IgE, and IgD. IgM antibodies represent approximately one tenth of serum immunoglobulins, while secretory IgA constitutes the first line of defense against mucosal viral infections. The four IgG subclasses (IgG1 to IgG4) have a longer half-life than the others (22 days) and are associated with long-term protection by triggering complement fixation (CFix) and improving the specificity of the immune response by binding to the surface of cytotoxic effector cells. Most viruses induce mainly IgG1 and IgG3 responses.
There are many potential antigens in each virus that may be presented at different time points in the course of infection. The primary antibody response to a virus is typically characterized by early onset of IgM production (peaking at 2 weeks) that declines later, followed by IgG production (reaching a plateau 2 weeks later) that may persist for years. When the antigen is localized in the mucosa, the immune response, driven by B cells of the interstitial lymphoid follicles (e.g., tonsils, Peyer's patches) also produces high quantities of IgA. Re-infection may result in overproduction of IgG by memory B cells, which may remain throughout life, together with a low or undetectable production of IgM. Infants younger than 6 months of age, however, mount a relatively poor IgG response, thus viral detection by isolation is the best way to diagnose a viral infection.
Diagnosis of the pathogen responsible for a recent infection may be achieved through detection of specific IgM in serum, 1 week after symptoms begin. Although useful clinically, this approach faces a number of problems upon evaluation of results. In some cases, patients remain seronegative during acute infection (e.g., 10% to 30% of patients with acute RSV infection, or 20% to 50% of those with acute AdV infection). In other cases, IgM persists at high levels (even during convalescence), thus not representing recent infection. The presence of specific IgG is a cause of false-positive results when rheumatoid factor (RF) is also present in the serum, but also of false-negative results because of its competition with IgM. Such problems are minimized with the removal of IgG or RF pre-analytically, although the ideal way is the use of the μ-capture IgM technique.
Therefore, in most cases, blood samples should be collected at least twice during the course of an illness within a 2- to 3-week interval: in the acute phase (as soon as possible after the onset of disease and no later than 1 week) and during convalescence (at least 2 weeks after onset). Comparison of the antibody pattern in these two states allows safe demonstration of diagnostically significant active virus, and seroconversion is defined as a 4-fold increase in antibody titer. The long delay before a definite diagnosis is made limits its use in urgent decision making. However, in many cases rapid methods of antigen detection are inefficient (e.g., RSV detection in adults), and serologic testing is considered a reference method (e.g., Epstein-Barr virus [EBV] pharyngitis infection). Moreover, it is a fast automated method that remains the method of choice for archival material; it is as sensitive as PCR in detecting influenza infections.24 It is also used to check on the effectiveness of vaccination and in confirming causation of illness (e.g., with AdVs and Enteroviruses that colonize the URT for a long time). On the other hand, serology is not indicated for immunosuppressed individuals, neonates, or infants because of their impaired immune responses.
Another major issue in antibody measurement is the type of antibodies targeted by the test. Thus, antibodies detected by EIAs may be different from those that confer neutralization activity. Neutralizing antibodies are raised against epitopes usually found on the surface of the virus, and upon binding to the virus, render it noninfectious by blocking its attachment to receptors or preventing uncoating of the virus. Neutralizing antibodies persist after viral infection; their measurement aims to determine vaccine efficacy and is used in epidemiologic studies rather than for the diagnosis of primary infection. In tests assessing neutralizing antibody, the serum sample is usually incubated with a viral preparation of known titer, and its ability to inhibit TCID50 during CPE development in cell culture is assessed. Alternatively, the reduction in the ability of the viral preparation to form plaques can be measured. In the case of IFV for example, a titer 1:8 denotes protective immunity. Such tests are the method of choice for viral infections and can be performed in specialized laboratories.
There are three main ways to detect respiratory virus in the host serologically. Immunoassays (conducted in a manner similar to that described earlier for the detection of viral antigens) directly measure antibody-virus interaction through the use of labeled reagents. CFix and passive agglutination assays are based on the ability of virus-antibody interactions to interfere with the functions discussed earlier, but do not allow differentiation between antibody classes. Finally, assays such as hemagglutination inhibition allow the measurement of particular antibodies that specifically interact with viral surface proteins. Possible cross-reactivity between viruses belonging to the same family and retrospective diagnosis are the main disadvantages of these methods, which do not necessarily produce comparable results because they detect antibodies of different types and specificity.
Immunoassays
As in the antigen detection immunoassays described earlier in the chapter, reporter molecules conjugated with antibodies (or antigens) allow the assessment of virus-antibody interactions. The reporter molecules may fluoresce (IF), have enzymatic activity for color-developing substrates (EIA), or have radioactivity (RIA).
Immunofluorescence
In IF assays, purified hyperimmune animal sera or monoclonal antibodies are labeled with a fluorescent dye (e.g., fluorescein isothiocyanate). In a typical protocol, a serum sample is incubated with virus-infected cells that are fixed on a slide. After unbound material is washed out, the slide can be dried, mounted, and observed under a fluorescence microscope. Streptavidin-biotin and similar systems that are currently used provide greater flexibility and sensitivity in antibody detection. Background fluorescence is a common obstacle in IF procedures. In solid-phase FIA, the viral antigen is immobilized on an opaque solid-phase surface rather than a slide, and use of a fluorometer allows quantitation and automation. However, FIA instrumentation cannot discriminate between background and positive fluorescence.
IF is the method of choice for the diagnosis of EBV infection, where a single serum sample in the acute phase of pharyngitis is sufficient for the diagnosis of 90% to 95% of infectious mononucleosis cases with detection of capsid (VCA-M, VCA-G) and nuclear (EBNA-G) viral antibodies. IFA is easy to perform and inexpensive but can be time-consuming and requires an expensive fluorescence microscope and interpretation by skilled personnel. Only rare cases with ambiguous results require additional testing with Western blot or avidity tests (Table 24-5 ).
Table 24-5.
Antibodies for the Diagnosis of Infectious Mononucleosis
| Evaluation | Antibody Against EBV Antigens | ||
|---|---|---|---|
| VCA-M | VCA-G | EBNA-G | |
| Seronegative | – | – | – |
| Present infection | +++ | ++ | – |
| Recent infection | + | ++ | – |
| Past infection | – | + | + |
–, Absence of antibodies; +, presence of antibodies; ++ or +++, presence of antibodies in high or very high titer.
Enzyme Immunoassays
EIAs are used to detect and quantitate antibody raised against viral antigens. Antigens are obtained from various sources, such as lysates from virus-infected cells. To that end, cells are washed, re-suspended in serum-free medium, and subjected to repeated freeze-thaw cycles. Virus is then clarified with ultracentrifugation, providing a rich source of antigens. Synthetic peptides also may be used for antigen preparation. For IFV, this method is more sensitive than CFix, may discriminate between antibody classes, and may use antigens specific for virus serotypes or subtypes, but it needs standardization. Seroconversion for RSV, which may be delayed for 4 to 6 weeks, has been detected in 50% of infants younger than 6 months of age.
For indirect EIA, the antigen is bound to a solid-phase surface, and after incubation with the serum sample, bound antibodies are detected with an anti-human antibody enzyme conjugate. The more abundant IgG antibodies compete for antigens with the other classes and, thus, should be removed before IgM measurement. Nonspecific binding is common in this method, and impurities present in the antigen preparation may cause false-positive results. Pre-incubating the sera with uninfected cells may reduce this problem.
To increase the specificity of this method, inhibition (or competitive) EIAs have been used. In this case, serum antibodies are detected by their ability to block the binding of a known antibody conjugate to the antigen. The detector antibody can be added simultaneously or after the antigen and the serum sample. In this case, false-negative results can be caused by serum antibodies that do not compete with the conjugated antibody, but inhibit the ability of the antibody that is being tested to do so.
In the capture EIA method, anti-human immunoglobulin class-specific antibodies are first bound on a solid-phase (capture-phase) surface. After incubation with the serum sample, viral antibodies are bound on the capture phase, together with viral-unrelated antibodies. Viral antigens are added last and subsequently detected with an antigen-specific antibody conjugate. Because of the selective class-specific adsorption in the first step, this method avoids the problems caused by competition between antibody classes, particularly improving IgM detection. On the other hand, low-level IgG detection may be less sensitive due to the presence of large quantities of total IgG antibodies in serum.
Other Immunoassays
When it is necessary to detect low levels of virus-specific antibodies in serum, standard immunoblot techniques (Western blot) can be used. Briefly, the protein content of semipurified virus propagated in cell culture is applied onto a nondenaturing polyacrylamide gel, and after electrophoretic separation, protein bands are transferred to a nitrocellulose or nylon membrane that can be cut into narrow strips and stored in the freezer. Serum samples can be diluted in buffer containing a protein that blocks free binding sites to reduce nonspecific binding, and then incubated with the membrane. After a washing step, bound antibodies are measured with the use of a radioactive or enzyme-labeled conjugate bound to a suitable secondary antibody. In dot immunobinding assays, viral antigens are bound in a dotted membrane. The membrane is then treated so that the potential protein-binding sites remaining in the membrane are blocked. The dots are then covered with small (e.g., 3-mm) strips saturated with the test serum. After a washing step, anti-human IgG conjugated with the appropriate enzyme is added, followed by incubation with the appropriate chromogen substrate. The intensity of the color spots is compared with that produced by the control sera to reveal specific antiviral antibodies. Dot immunobinding assays serve as qualitative rather than quantitative assays and are also subject to problems with nonspecific binding.
In radioimmunoprecipitation assays, antigen-antibody complexes formed after incubation of the serum being tested with viral antigens are cross-linked and immunoprecipitated with protein A or anti-human IgG antibody. The quantity of radioactivity bound in the precipitate can be measured and is proportional to the concentration of specific antibodies in the serum.
Avidity assays measure the relative degree of dissociation between specific antiviral antibodies and their respective antigens. During maturation of the immune response, the avidity (strength of the combined interaction of an antiserum with a pattern of antigens) of IgG antibodies remains high, whereas their concentration declines. Thus, sera from recent infection are characterized by high-avidity antibodies, and sera from re-infection have low-avidity antibodies. Practically, serum is incubated first with antigen bound to a solid-phase surface. The complex is then allowed to dissociate in the presence or absence of urea, and the relative degree of antibody dissociation (ratio of absorbance in the presence of urea to absorbance in the absence of urea) is measured by standard EIA methods.
Finally, three types of methods have been used to specifically measure IgM antibodies. First, in IgG absorption methods, an IgG absorbent (e.g., staphylococcal protein A, streptococcal protein G) is incubated with the serum, and after a centrifugation step, IgM antibodies can be measured in the supernatant. These absorbents are believed to be superior to anti-human IgG antibodies for this method, because the latter may also remove some types of IgM. However, staphylococcal protein cannot bind IgG3, and this could interfere with the accuracy of the method because viral antibodies may be significantly represented in this subclass. Streptococcal protein G, on the other hand, binds all IgG subclasses, but not IgM; accordingly, combinations of streptococci and protein A have been used to remove all IgG and IgA from serum samples before IgM measurement. IgA can interfere with IgM measurement, resulting in false-negative findings by competing with IgM for antigenic sites. Second, in one of the early IgM separation methods, rate zonal centrifugation allowed purification of the IgM subclass based on its higher sedimentation coefficient compared with that of the other antibody classes. Gel filtration takes advantage of the higher molecular weight of IgM compared with the other classes (900 versus 150 to 400 kd). However, serum lipoproteins and nonspecific cell agglutinins may be fractionated, together with IgM, and could interfere with the assay. Ion-exchange chromatography, based on the differential binding of IgM and IgG classes to anion-exchange resins, has been used, but the IgM yield is relatively low, whereas IgG and IgA may still be present in the IgM fraction after elution from the column. Third, in the popular IgM immunoassays, anti-human IgM-specific antibodies are employed. IIF and EIA are the methods typically used for IgM detection. Capture IgM assays show reduced nonspecific binding; in this method, solid-phase, fixed anti-human IgM antibodies separate IgM after incubation with the serum sample. The potential presence of antiviral elements is further detected using labeled viral antigen or unlabeled antigen, followed by a labeled antigen-specific antibody. Detection of anti-PIV IgM has been also reported with the use of hemadsorption.
Complement Fixation
CFix systems take advantage of the fact that complement proteins bind, or “fix,” to antigen-antibody complexes during the host immune response to a foreign antigen. If this antigen is cell-localized, then the deposition of complement elements will cause cell lysis. CFix to IgM is stronger (> 1000 times/antibody molecule) than that to IgG. CFix antibodies can be raised against some or all viral proteins. Their titers increase slowly during primary infection, reaching lower levels than antibody titers detected by the other methods. In addition, they decline gradually, making this method less sensitive than others for the detection of viral infection. An additional problem is the interference of some serum elements (e.g., heparin, IgG aggregates) with complement formation. In a typical CFix assay, the serum sample is incubated with a particular antigen in the presence of a known amount of guinea pig complement. If a specific antibody is present in the serum, the complement will be bound and depleted from the solution. Subsequently, sheep erythrocytes coated with hemolysin (anti-sheep erythrocyte antibody) are added, and their lysis is proportional to the availability of complement proteins that did not react with the specific antibody during the first step. CFix may measure antibodies against IFV nucleoprotein (NP), which is common across strains of the same serotype and can discriminate between serotypes A and B, but not among subtypes. The antibodies tested are not protective and disappear in weeks or months. CFix can be used for the diagnosis of recent infection by testing for seroconversion, and, due to the fact that NP is stable, there is no need to prepare a new antigen every time a new IFV subtype emerges. The method is standardized but tends to become replaced by enzyme-linked immunosorbent assay (ELISA). CFix for RSV infection in infants younger than 3 months of age is not reliable.
In immune adherence agglutination assay, a rapid and more sensitive variation, aggregation, rather than lysis, of erythrocytes occurs and is measured. In this detection method, complement that is bound to antigen-antibody complexes is allowed to bind to C′3b receptors in human primate erythrocytes. Thus, agglutination of the erythrocytes reveals specific antibodies in the sample.
A simple technique used earlier for the detection of hemagglutinating activity–containing viruses (e.g., IFV and PIV) is the hemolysis-in-gel test. Erythrocytes from sheep or chicken were first sensitized by coupling to a viral antigen in a chromium chloride solution. After a washing step, the erythrocytes were suspended in an agarose gel–containing guinea pig complement. The serum sample was then loaded onto a well in the gel and allowed to diffuse. The presence of antibodies against the virus would lead to the formation of a zone of hemolysis around the well.
Anticomplement antifluorescence is a modified IF assay for the detection of CFix antibodies. In this assay, complement is added during or after exposure of virus-infected cells to the serum being tested. Any complement that is bound can then be detected with anti-C′3 antibody. Because nonspecifically bound IgG cannot trigger CFix, anticomplement antifluorescence assays do not have the common background problems associated with conventional IF.
Agglutination Assays
H or H-N proteins expressed in the envelopes of viruses such as IFV and PIV are able to bind to specific erythrocyte surface receptors and cause their agglutination. Practically, erythrocyte cross-linking leads to observable cell clumping. Hemagglutination inhibition tests measure the presence of specific antibodies in the sera that inhibit virus-mediated agglutination of erythrocytes. This is a sensitive assay that is affected, however, by both nonspecific H and agglutinin inhibitors present in the serum. Nevertheless, it is a particularly reliable method in IFV surveillance protocols, in which case titers ≥ 1:40 are considered protective, while 1:10 to 1:20 levels are less protective.25, 26
Fusion proteins present in the envelope of viruses such as PIV and RSV allow their entry into cells by triggering fusion of the viral surface with the cell surface membrane. In the case of erythrocytes, fusion may lead to hemolysis. Hemolysis inhibition assays take advantage of these properties to measure the presence of antibodies in a serum sample that bind and block viral antigens and inhibit hemolysis. In this way, the hemolysis inhibition assay detects both anti-H and antifusion antibodies in the serum. In a typical protocol, serum dilutions are mixed and incubated with purified virus. A 10% suspension of suitable erythrocytes is then added. After some hours of incubation, the erythrocytes are removed by centrifugation and the optical density of the “cleared” supernatant is read with a spectrophotometer. A classic endpoint titer can then be calculated by defining the highest serum dilution that causes 50% inhibition of hemolysis.
In passive agglutination assays, sera are incubated with viral antigens attached to erythrocytes or to materials such as latex or bentonite. The particles or cells agglutinate in the presence of a specific antibody, forming precipitates in the bottom of the tubes. In the passive hemagglutination method, aggregates of erythrocytes develop due to “antibody bridges” formed between antigen-coated erythrocytes. These can be visible, even with the naked eye, and may detect low levels of antibodies.
Detection of Viral Nucleic Acids
A constellation of methods that gained increasing attention during recent years due to their increased sensitivity, specificity, reliability, and accuracy are genetic material-based methods, with PCR in the leading position. The common element in these methods is the isolation and partial purification of viral RNA or DNA and its subsequent detection and analysis in suitable molecular biology systems. Of course, the clinical significance of viral nucleic acid in a specimen needs to be determined because its presence does not always confirm that it is causing disease or that it is in an infectious state.
Hybridization
Hybridization-based protocols require the presence of single-stranded RNA or DNA. In this approach, a suitable oligonucleotide probe sharing a certain degree of homology that allows base pair matching with the single- stranded viral nucleic acid is allowed to anneal under stringent reaction conditions (hybridization). Whereas single-stranded RNA viruses provide ready-made yet labile genetic material, the double-stranded DNA content of AdV must first be denatured or dissociated by chemical (e.g., sodium hydroxide) or physical (heat) means. The resulting single-stranded DNA would return to its double-stranded configuration on removal of the dissociation agent. The probe can be labeled directly with enzymes or other reporter molecules. Alternatively, linker moieties (e.g., biotin or digoxigenin; the latter is more sensitive for in situ hybridization [ISH]) can be attached to probes and serve as bridges for the attachment of reporter molecules. In a typical protocol, the viral nucleic acid is isolated, purified, denatured, and bound to a nitrocellulose or nylon membrane. The denatured and labeled probe is incubated under carefully defined conditions with the viral nucleic acid, and unbound material is thoroughly washed out. A reporter molecule is then added (e.g., ALP-labeled streptavidin), and after a second incubation period the unbound reporter is washed out, and the final chromogen or other suitable substrate is added to give rise to a measurable signal.
Several hybridization-based techniques are used for viral nucleic acid detection (e.g., the molecular biology dot-blot and Southern blot protocols, liquid hybridization, and ISH). As suggested by its name, liquid hybridization allows the detection of nucleic acid that is free in solution rather than attached to a solid-phase surface. Microtiter plates and strips can be used in this method, increasing ease of handling. ISH allows the detection of virus in various sources, including cells and tissues grown or fixed on slides, respectively. ISH-based detection of RV in a human bronchial biopsy is shown in Figure 24-2 . The method is very sensitive in RNA virus detection, with a limit of 30 to 100 viral genome copies per cell, and it sometimes may be even superior to PCR (with which it can be used in combination to increase overall sensitivity).
Figure 24-2.

Detection of rhinovirus ribonucleic acid with in situ hybridization in a bronchial biopsy specimen obtained from a volunteer, (A) at baseline and (B) after experimental inoculation with rhinovirus. No signal could be observed in the baseline biopsy specimen, whereas an intense signal located at the bronchial epithelium (black spots) is present 3 days after nasal inoculation with the virus.
Polymerase Chain Reaction
PCR methods allow specific amplification of defined DNA sequences to a level at which they subsequently can be detected and can be applied to any virus for which part of the genome sequence is known. The majority of respiratory viruses are RNA viruses; therefore, an additional step of reverse transcription (RT) is required before their PCR detection in clinical samples. First, total RNA is extracted by standard molecular biologic techniques from samples that have been kept at - 70 ° C in an appropriate virus transport medium. Alternatively, some samples may be placed directly into a denaturing solution to inactivate ribonuclease enzyme activity, and then stored or transported at room temperature. Extracted RNA is then reverse transcribed into complementary DNA (cDNA; e.g., with heat-stable reverse transcriptase isolated from a retrovirus, such as murine MoMuLV) and further amplified by PCR using virus-specific oligonucleotides (primers) that have been designed with the aid of computer software. These primers are usually planned to amplify sequences that are 100 to 1000 base pairs long (amplicons) and can be designed so that they discriminate between different serotypes of the same virus. Nucleotide diversity that is frequently observed among different strains of a given virus species should also be taken into account, and areas of high homology should be selected for serotype-specific primer pairs design. Continuous cycles of denaturation, renaturation, and extension result in an exponential accumulation of the target DNA. The reaction is limited by the availability of substrate (nucleotides) and the possible competition between the target genome and other amplicons for the reaction's reagents. The amplicons then can be electrophoresed in a 1% to 2.5% agarose gel and visualized as DNA bands under an ultraviolet transilluminator following ethidium bromide or another DNA dye staining. This is readily accomplished within 1 working day, a fact that is of particular clinical importance.
To further improve the specificity and sensitivity of the test, the amplicons can be hybridized with labeled nucleic acid probes directed against regions of the amplicon. Alternatively, RT-PCR can be combined with EIA techniques that consist of hybridization of the amplicon with biotinylated RNA probes directed against the internal sequences of the amplicon. Time-resolved fluorometry has also been combined with PCR for the detection of picornaviruses. Moreover, in the “nested” PCR, PCR amplicons can be used as a source for a second round of PCR. In this approach, a second set of primers is designed against sequences that were localized internally in the sequences that were amplified in the first round. The method can be so sensitive as to detect a few particles of respiratory virus.27 Nested-type PCR may not only increase sensitivity, but it also may discriminate between serotypes within viral species that are of similar size and thus are difficult to separate with gel from the first round of PCR. Discrimination within or between species can be also accomplished by digesting the amplicons with restriction endonucleases. Human RVs, for instance, can be discriminated from enteroviruses, which lack a BglI recognition site in their respective amplified sequence, based on the fact that their product remains undigested, retaining its original size after digestion with BglI restriction endonuclease28 (Fig. 24-3 ).
Figure 24-3.

Detection of rhinovirus genetic material by reverse transcriptase polymerase chain reaction and its differentiation from enteroviruses. Picornavirus amplicons generated by the OL26-OL27 primer pair were digested with BglI. Rhinovirus (lanes 1 to 6) is detected as a single band with approximately 190 base pairs (bp) consisting of two almost identical bands. This easily allows differentiation from a poliovirus isolate (lane 10), whose amplicon remains undigested (~ 380 bp) and from a coxsackie virus (lane 11), which produces a duplet (~ 175 and 200 bp, respectively). M, DNA size marker.
In multiplex PCR, a mix of primer pairs is used, allowing simultaneous amplification and detection of several serotypes or viruses. Each primer pair demands different conditions for optimal target amplification, and therefore increased attention is needed upon development of this technique. For instance, Hexaplex (Prodesse, Waukesha, Wisconsin) allows prompt detection with high sensitivity and specificity of H1N1, H3N2, IFV A, IFV B, both RSV subtypes, and three of the four human PIVs in children.29 The detection limits of multiplex RT-PCR protocols allow the identification of as few as 100 to 140 copies of viral particles/mL, or one TCID50. This method can be at least as sensitive as combined tissue culture and IF methods. Combination with hybridization may further improve detection scores. In a combination of multiplex RT-PCR and enzyme hybridization assay, the amplicons of seven respiratory viruses (RSV A, RSV B, IFV A, IFV B, PIV 1, PIV 2, and PIV 3) were purified and hybridized with peroxidase-labeled probes into avidin-coated, 96-well microplates. The signal emitted after incubation of the complex with the substrate allowed the detection of almost twice as many positive clinical samples compared with conventional culture and IIF methods.30 A multiplex PCR enzyme-linked immunosorbent assay that can detect seven respiratory viruses, in addition to the common respiratory pathogens Mycoplasma pneumoniae and Chlamydia pneumoniae, was less efficient in revealing RSV and PIV 1, although it proved to be more sensitive than cell culture in detecting PIV 3, AdV, and IFV. Recent developments in this method include semi-quantitation of results with the use of specialized equipment and primers specific for additional viral and bacterial species (e.g., Reovirus, Bordetella pertussis), allowing for the detection of as many as 19 different microorganisms in a clinical sample.31 Finally, multiplex PCR assays have been designed to discriminate between multiple subtypes within one species, as is the case with AdVs and picornaviruses.32, 33 In another approach, degenerate primers have been used to discriminate between AdV serotypes.34
Amplicons can also be subjected to sequence analysis to identify potential point mutations or deletions or specific serotypes. Cloning of PCR fragments that are generated with a series of partially overlapping or degenerate primers into bacterial plasmids allows sequencing of the entire viral genome, a laborious activity that is not necessary for usual clinical practice, but is indispensable when a previously unknown viral species is characterized (e.g. MPV) or when a high-risk epidemic from an initially unknown viral strain or mutation must be confronted efficiently and quickly (e.g. SARS). Heteroduplex formation between the amplicons may result in differential mobility of the product when run in a gel, and can be used for subtyping viral genomes. By combining, for instance, RT-PCR and heteroduplex formation, variant strains of IFV can be differentiated.35
In situ PCR allows the detection of viral genetic material and, furthermore, its localization at the cellular and tissue levels, providing information that is of particular importance for clinical pathology. Thus, paraffin-embedded fixed cells or tissue sections are treated with xylene and then digested with protease and DNAse solutions. The PCR mixture containing Taq polymerase is placed on top of it, and the entire slide is placed on an aluminum foil boat, transferred onto a conventional or modified PCR apparatus, and subjected to PCR amplification. If the one of the four deoxynucleoside 5′-triphosphates (dNTPs) that is present in the PCR mixture and is providing the nucleotide source is reduced and replaced by a modified nucleotide (e.g., biotinylated or digoxigenin-coupled deoxyuridine 5-triphosphate), then the emerging amplicons can be detected by incubation with an enzyme-labeled probe (e.g., ALP, antidigoxigenin). Alternatively, in the absence of modified nucleotides, the amplified DNA can be detected by conventional ISH, conducted as described earlier in the chapter. Alternatively, the PCR mixture can be transferred to a test tube and run in an agarose gel or subjected to Southern analysis to identify the viral genomic fragments.
Real-Time Polymerase Chain Reaction
Recent advances in PCR technology allowed the development of real-time PCR, which is costly and requires appropriate instrumentation. On the other hand, real-time PCR can be more sensitive and time-efficient than conventional PCR, cell culture, and IF in detecting respiratory viruses in clinical samples.36, 37 Further, it is quantitative, allowing for assessment of the exact number of viral copies in a clinical sample. The final detection step employs either a fluorescent dye able to bind to double-stranded DNA (e.g., SYBR Green I) or a more specific hybridization probe (e.g., TaqMan, Molecular Beacons, Light Cycler probes) to monitor the presence and quantity of amplicons. For quantitative analysis as well as determination of the detection limits, serial dilutions of plasmid DNA containing a known amount of viral genome (virus genome equivalent) per microliter can be used as a standard reference solution.
In fluorescent dye SYBR Green protocols, the dye is incorporated into the amplicons in each cycle and assessment of fluorescing DNA is collected during each extension phase. However, such dyes bind to DNA, independent of the specific sequence, and thus can also detect undesired, nonspecifically amplified DNA. Thus, the specificity of the method is tested by the melting curves at which the final amplicon is briefly heated to denature (e.g., 95 ° C), allowed to re-associate at a lower temperature (e.g., 65 ° C, 15 sec), and finally re-denatured to 95 ° C by gradually increasing the temperature at a defined rate (e.g., 0.1° C/sec). The continuously measured fluorescence data recorded during this last stage are plotted against the temperature and allow calculation of the melting peak that characterizes a given amplicon under the conditions used. When the melting peak of a particular product coincides with the standard, it is considered specific. Highly sensitive one- and two-step, real-time PCR assays for the qualitative and quantitative detection of most respiratory viruses have been reported.38, 39
In hybridization-based protocols, a specific probe sharing consensus homology with the sequenced strains of a viral species is labeled with a reporter fluorogenic dye (e.g., 6-carboxyfluoroscein) at the 5′ end and a quencher dye (e.g., carboxytetramethylrhodamine) at the 3′ end. The probe is present in the conventional PCR master mix (containing buffer, Mg+ 2 salts, dNTPs, water, and the primers) during PCR, and the real-time apparatus records the fluorescence emerging during time. The reporter dye fluorescence (e.g., 6-carboxyfluoroscein) is considered positive and, compared with the fluorescence emitted by a reference dye, present in the PCR master mix to normalize for non-PCR–related fluorescence fluctuations among samples. A threshold is usually set, above which a signal is considered positive.
Recent approaches to the detection of respiratory viruses include the development of multiplex real-time PCR protocols. A SYBR Green–based reaction, for instance, allowed simultaneous detection of IFV A, IFV B, and RSV, with specificity comparable to that achieved with commercially available rapid antigenic tests and considerably higher sensitivity scores.40 Discrimination between the particular species was based on the specific melting temperature curves elicited by the amplicons. Limitations in the number of viruses and viral serotypes are inherent in the real-time approach, especially in the protocols using a labeled probe, because most platforms do not allow the simultaneous use of more than two fluorochromes. Using a more advanced apparatus that can detect up to four fluorochromes, Templeton and colleagues41 succeeded in detecting both IFV serotypes, RSV, and all four PIV subtypes in a two-tube reaction. In their approach, the specific probes were labeled with different fluorochromes (i.e., 6-carboxyfluoroscein, Texas red, hexachlorofluoroscein, and cyanin 5); the overall reaction could be accomplished within 6 hours and proved to be more sensitive than cell culture, with detection limits ranging from 0.1 to 0.0001 TCID50 of viral stocks of known titer, depending on the virus. Molecular methods allowing for simultaneous detection of 7 to 26 different viruses at the same time have been attempted.21
Other Methods
Advances in molecular biology continuously offer additional PCR- and hybridization-based methods. In a study, as few as 100 RNA copies of PIV (or one TCID50) could be detected by probe hybridization and electrochemiluminescence or by using molecular beacons.42 The first step in this approach, nucleic acid sequence–based amplification, was used. This technique employs avian myeloblastosis virus reverse transcriptase, together with ribonuclease H and T7 RNA polymerase, under isothermal conditions, and is able to directly amplify RNA. The use of nucleic acid sequences to amplify RNA with primers directed against the 5′ noncoding region of RV serotypes allows discrimination between RV subgroups.43
Complementary DNA-amplified restriction fragment length polymorphism (RFLP) allows the identification of previously unknown viral sequences. In this method, double-stranded cDNA is synthesized from viral RNA and digested with frequently cutting restriction endonucleases. Double-stranded adaptors are then ligated to the ends of the emerging restriction fragments and provide primer sites during PCR amplification. A second selective fragment amplification step is conducted by adding one or more bases to the PCR primers. If the complementary bases are present in the viral sequence, then successful amplification will occur. A modification of this method was successfully employed in the discovery of the NL63 HCV.10
Wang and colleagues used the powerful microarray technology to detect approximately 140 distinct viral genomes simultaneously, including most respiratory viruses.44 To that end, 1600 oligonucleotides with a relatively greater length than those commonly used in array technology (70 versus 20 to 25 bases) were selected after a genome-wide BLAST analysis (Basic Local Alignment Search Tool, a method for rapid searching of nucleotide and protein databases) and ranked according to shared homology to regions of the viral genomes. Using an inkjet oligonucleotide synthesizer, these oligonucleotides are synthesized in situ and placed onto directed locations of a glass wafer.45 The glass surfaces can then be hybridized, under strict conditions, with cDNA, PCR amplicons, RNA, or another form of genetic material derived from viral stocks, virally infected cells in cultures, or clinical samples. Human and cellular transcripts are also included to normalize against nonspecific hybridization. This material is labeled with cyanin 5 or cyanin 3, which provides red or green coloring, respectively, to allow color visualization of microarray data that are obtained after the arrays are scanned with confocal laser scanners and analyzed with suitable instrumentation and software. This method allows the detection of paramyxoviruses, orthomyxoviruses, AdVs, and picornaviruses from clinical samples. It can also detect and discriminate among all 102 RV serotypes, based on the hybridization pattern obtained from each serotype. After human volunteers were experimentally infected with RV, the array could detect as few as 100 infectious RV particles in NPA samples.44 Analysis of a small number of samples from naturally acquired colds showed different RV serotypes and PIV 1, which also has been confirmed by conventional RT-PCR. Although it is extremely promising, this technique needs further evaluation, including cost-effectiveness, before being applied in clinical practice.
Practical Considerations in the Use of Nucleic Acid–Based Techniques
The identification of a particular virus can be further, and without doubt, confirmed by restriction analysis or sequencing of the product and subsequent comparison with published genome databases. In addition, PCR-based methods have proved to be very sensitive, usually exceeding the sensitivity scores of cell culture techniques. However, false-positive or false-negative findings can be a problem, if certain practical measures in the handling of viral genetic material are not meticulously followed. First, preservation of the sample is of particular importance for the integrity of the viral genomic material. RNA, the genomic material of most respiratory viruses, is particularly vulnerable to degradation by RNAses that are present in all biologic samples and fluids. RNAse-free vials, solutions, and buffers should be used by specialized personnel in designated areas of the laboratory. In addition, if it takes too long for an NPA sample to be transported from the clinic to the laboratory, or if the sample remains on ice for too many hours instead of being placed in the freezer immediately, the sensitivity of the method can be unexpectedly low. Further, biologic fluids often contain substances that can inhibit PCR amplification (e.g., mucus). In this case, dilution of the sample or treatment with a suitable agent such as dimethyl sulfoxide may facilitate detection of the virus. The use of clinical samples spiked with stock virus or the inclusion of synthetic heterologous competitor RNA in the reaction may facilitate normalization of PCR outcomes.
On the other hand, PCR-based techniques are also subject to problems with contamination, especially if large numbers of samples are handled simultaneously. In the case of a nested PCR protocol, the first and second rounds of PCR should be conducted in separate areas, with separate sets of pipettes, and of course, with different plasticware, and several negative controls should be included for monitoring of contamination. If contamination occurs, replacement of the pipettes is required, as well as a review of laboratory and handling practices.
Techniques to Diagnose Respiratory Viruses in Clinical Practice
Threatening influenza pandemics and mortal epidemics of previously unknown respiratory viruses (e.g., SARS-CoV) require the use of rapid and reliable detection methods in clinical practice. Moreover, large epidemiologic studies are required to better define the involvement of these viruses in noninfectious diseases (e.g., asthma). These studies will help in drug development and the implementation of intervention strategies, even during an outbreak. Drugs are being developed that specifically block infection by individual viruses (e.g., anti-influenza neuraminidase inhibitors), but they are useless if the patient has been infected by another virus.
It is not possible to determine the optimal method for virus detection because many factors vary, depending on the particular conditions and the scope of the analysis (cost-effectiveness, time required, sensitivity, availability of skilled personnel, and laboratory equipment). A combination of methods, rather than a single one, is best used in particular cases because most protocols are not ideal or do not provide enough information. EM is still recognized as an indispensable method.46 Although cell culture remains the gold standard, it is time-consuming and is being replaced by antigen-detection methods and molecular biological techniques. Their commercial availability, ease of performance, and rapidity have made antigen-based methods increasingly popular, especially in small units that lack advanced facilities. They can be accomplished within 15 minutes to a few hours. However, they can be inferior to cell culture in terms of sensitivity and are of limited value for the detection of some respiratory viruses. On the other hand, PCR has been widely used as a research tool during the last decade, and its clinical use is steadily increasing. PCR cannot, however, replace the use of cell culture in worldwide influenza surveillance, an aspect of classic virology that is vital for informing vaccine manufacture.47
Developing Techniques and Future Directions
Rapidity, high sensitivity and specificity, ease of use, and cost-effectiveness are the major requirements imposed on the respiratory viral detection field. In particular, the need for rapid diagnostics is likely to increase as more specific antiviral therapies enter the market. Although PCR-based analysis was the major breakthrough in recent years, none of the existing methods can be considered ideal, and usually a combination of techniques is used for more accurate results, increasing the costs, time, and skills required for analysis. Thus, combination of hybridization with electroluminescence or the use of molecular bonds is capable of detecting just a few PIV particles.42 Other techniques, such as real-time loop-mediated amplification (LAMP),48 nucleic acid sequence-based amplification (NASBA),49 and asymmetrical multiplex PCR in combination with microarray hybridization50 have shown similar sensitivity with conventional real-time PCR with regard to respiratory virus diagnosis. Additionally, the use of restrictive enzymes on a double cDNA helix that has been transcribed from viral RNA (cDNA-amplified RFLP), as well as 3' degenerate primers in a randomized PCR allow the amplification of genetic material of any virus in a clinical sample from patients with respiratory illness of unknown etiology.
Simultaneous and reliable detection of as many viruses as possible, in the shortest time possible, and ideally in a single test, is the goal of any novel and future technique. Although it is specific, sensitive, and reliable, multiplex real-time PCR can still detect a restricted number of viruses simultaneously. Nowadays, microarray technology is one of the most sensitive and high-throughput choices for concurrent diagnosis of many different viral strains (> 100) or specific virus serotypes.51 This technique also can be combined with assays revealing expression patterns of target genes in the host, thus providing an overall picture, not only of viral presence, but also of host response.
Another combination that has also been used for detection of the SARS genome52 is the use of molecular bonds connected to microspheres, which can detect multiple nucleic acids in solution, followed by conventional flow cytometry. Finally, some techniques such as surface plasmon resonance, quartz crystal microbalance and chromatometric functional polymers that do not use labeling may be used for direct detection of respiratory viruses.53
Laboratory diagnosis of respiratory bacterial infections
Bacteria rarely exist in mono-cultures, and species-species interactions can deeply affect the behavior of individual species. Moreover, bacterial load, virulence and pathogenicity, and the host's ability to mount an effective immune response all influence transition from mere contamination to colonization and infection.
Specimens for bacteriologic culture should be collected as soon as possible after the onset of disease and before the initiation of antimicrobial therapy. Optimal transport times depend on the volume of the sample, with small volumes of fluid (< 1 mL) or tissue (< 1 cm3) having to be submitted within 15 to 30 minutes to avoid evaporation, drying, and exposure to ambient conditions. Larger volumes in holding medium can be stored up to 24 hours; specimens should not be stored for longer than 24 hours under any circumstance. Some bacteria are particularly sensitive and should therefore be held at room temperature and immediately processed. Such bacteria include N. gonorrhoeae, N. meningitidis, H. influenzae, S. pneumoniae, and anaerobes. Delays of up to 6 hours result in minimal loss of colony-forming units (CFU) when transport media are used, but longer delays (even with the use of transport medium) result in significant losses of organisms. For delays beyond 6 hours, refrigeration improves recovery, except for the aforementioned organisms.
Upper Respiratory Tract Infections
Upper Respiratory Tract Specimens
Fresh pus, fluid, or tissue from the nose or nasopharynx (swab, wash, or aspirate), the sinuses (wash, aspirate, biopsy, scraping, or debridement), the gums and oral cavity (swab), as well as a pharyngeal swab from the tonsils and/or the posterior pharynx are the main URT biological specimens. Tympanocentesis is usually reserved for complicated, recurrent or chronic persistent otitis media. When the eardrum is intact, an aspiration is performed after cleaning the ear canal with soap solution, while a flexible shaft swab via an auditory speculum is used for collection of fluid (for aerobic culture only) when the eardrum is ruptured. Oral specimens should be collected with vigorous swabbing of the lesion, avoiding any areas of normal tissue following removal of oral secretions and debris from the surface of the lesion. Throat swabbing should be vigorous (with sampling of the posterior pharynx, tonsils, and inflamed areas while avoiding contact with the tongue and oral cavity) and should be transferred promptly to the lab in modified Stuart's or Amies medium with or without active carbon. For the diagnosis of group A streptococcal pharyngitis, which involves the performance of a rapid antigen detection assay and culture, two pharyngeal swabs should be collected (one swab/assay). Throat swab cultures in patients with epiglottitis should be collected by a physician only in a setting where emergency intubation can be immediately performed to secure a patent airway. Swabs for N. gonorrhoeae should be placed in charcoal-containing transport medium and plated immediately after collection. Nasal swabs for identification of S. aureus carriers should be premoistened with sterile saline, inserted 1 to 2 cm into the nares, rotated against the mucosa and transported in Stuart's or Amies medium. Nasopharyngeal aspirates (NPA), typically 0.5 mL, are collected over a 10-second procedure that involves introduction of a thin elastic catheter through the nasal cavity to a 5- to 7-cm depth or proportional to the distance between the nose and the ear. If the material does not pass into the container, the catheter may be washed off with saline or cut in order to obtain the specimen. The collection of nasopharyngeal wash is performed with installation of 1 to 2 mL of saline inside the nasal cavity of patients who have tilted their head backward (approximately 70%). Patients then lean forward, and the wash is collected in a sterile container or Petri dish. Nasopharyngeal swabs are collected with the help of flexible sterile swabs, which are passed through the nostrils until resistance is felt, and they are slowly rotated for 5 seconds to allow for mucus absorption. If possible, direct medium inoculation should be performed at bedside.
The material of the swab is important for the survival of certain microorganisms; cultures for B. pertussis are obtained by aspiration through a suction catheter or a Dacron or flexible wire calcium alginate swab of the nasopharynx. Samples intended for PCR for B. pertussis should not be collected with calcium alginate swabs, which is an inhibitor for the reaction, but with Dacron or rayon swabs. Cotton swabs contain fatty acids, which may be toxic for B. pertussis. For delays up to 24 hours, Amies medium with charcoal can be used, but Regan-Lowe medium is preferred for transportation times longer than 24 hours. Dacron swabs are also advocated for isolation of C. pneumoniae. Swabs without a buffer-type non-nutritive blood/charcoal transport medium (Stuart's or Amies) should not be used when transport is delayed more than a few hours because the specimen dries out and a lower microbial viability has been observed. This is of particular significance when clinically significant bacteria are present in low numbers or fastidious organisms such as anaerobes are involved.
Microscopic Examination
Microscopy following Gram staining is useful for the examination of paranasal sinus material, (normally sterile), pharyngeal smear, or material from the oral cavity for the detection of polymorphonuclear neutrophils (PMNs) and some microbes (e.g., corynebacteria [diphtheria], spirochetes [Vincent angina] or Candida spp.) and nasopharyngeal smear for C. diphtheriae and B. pertussis.
Gram staining is not useful for the diagnosis of streptococcal pharyngotonsillitis or the detection of N. meningitides carriage because these cannot be discriminated over the nonpathogenic normal flora of the URT. Occasionally, other stains also may be used such as Loeffler's Methylene blue for C. diphtheriae (appear as pleomorphic, beaded rods with swollen/club-shaped ends and reddish purple metachromatic granules) and DIF for Bordetella.
Culture
Normally, the initial part of the nasopharynx is colonized mainly by Staphylococcus spp.; the middle part is colonized by nonpathogenic aerobic and anaerobic microorganisms as well as potentially pathogenic bacteria such as S. pneumoniae, H. influenzae, and M. catarrhalis; and the posterior part is colonized by flora similar to that of the oropharynx, in which α- and β-hemolytic Streptococci and anaerobes dominate. Bacterial pathogens implicated in URTI are: β-hemolytic group A Streptococcus, S. pneumoniae, S. aureus, H. influenzae, M. catarrhalis, N. meningitidis, B. pertussis, C. diphtheriae, Klebsiella spp. and other Enterobacteriacae, Bacteroides spp., Fusobacterium spp., Borrelia spp., Arcanobacterium haemolyticum, and other anaerobes.
To isolate distinct colonies, samples are inoculated on small areas of agar plates and then linearly on three consecutive areas using sterile loops. Pharyngeal smears are routinely cultured for Streptococcus group A on 5% sheep blood agar (SBA) or group A Streptococcus selective blood agar at 35 ° C for 48 hours in an environment of reduced oxygen achieved by anaerobic incubation or in air with multiple “stabs” through the agar surface. Low oxygen concentration allows the recovery of group C and G streptococci. The selective agar is easier to visualize because it inhibits accompanying flora but delays the appearance of colonies. Plates are checked for β-hemolytic colonies, and verification of the presence of Streptococcus group A versus group C and G is done based on the fact that the former microorganisms are catalase-negative and pyrolidonyl aminopeptidase– positive as well as with the help of bacitracin disks in the initial agar and antigen detection. A number of other pathogens may cause pharyngotonsillitis or may colonize the URT without causing disease, and their isolation may be important in patients with CF; organ transplantation; or ear, nose, and throat (ENT) disorders. Such bacteria include C. diphteriae (Loeffler's serum medium or potassium tellurite blood agar incubated at 5% CO2, 48 hours, 35 ° C), Arcanobacterium haemolyticum (same culture media as for S. pyogenes but up to 72 hours incubation), N. gonorrhoeae (prompt inoculation on modified Thayer-Martin agar and incubation at 5% CO2, 35 ° C, 72 hours), epiglottitis pathogens, which are mainly H. influenzae B and less frequently S. pneumoniae, and S. pyogenes (chocolate blood agar [CBA] with incubation at 5% CO2, 35 ° C, 72 hours).
Nasopharyngeal specimens are useful for the diagnosis of infection by pertussis, diphtheria, and Chlamydia spp.; detection of the N. meningitides, S. aureus, and S. pyogenes carriage; and epidemiologic surveillance of S. pneumoniae antibiotic susceptibility among children. Such samples are usually inoculated on SBA (aerobically at 37 ° C, 48 hours) or CBA (5% CO2, 37 ° C). Samples suspected for B. pertussis and B. parapertussis should be inoculated on Regan-Lowe charcoal agar with 10% horse blood and cephalexin and incubated aerobically under moist conditions (35 ° C, 5 to 7 days). Optimal recovery requires the use of the aforementioned medium with and without cephalexin because some strains do not grow in the presence of cephalexin. possible N. meningitides containing specimens should be transferred in Stuart's or Amies medium or directly inoculated on SBA, CBA, or, if interference with normal flora is expected, modified Thayer-Martin or other selective medium for incubation under 5% CO2 at 35 ° C for 72 hours in a humidified atmosphere. For culturing C. pneumoniae, a nasopharyngeal swab is transferred in antibiotic-containing medium to permissive cell culture systems.
Selective media such as Canada colistin-nalidixic acid (CNA), or a selective and differential medium such as BBL CHROMagar S. aureus (BD Diagnostics, Sparks, MD), BBL CHROMagar MRSA (BD Diagnostics, Sparks, MD) or mannitol salt agar is helpful in differentiating S. aureus or MRSA (methicillin-resistant S. aureus) from other flora and is useful when interpreting large numbers of specimens.54 Specimens from the inner ear may be inoculated on SBA and CBA and under anaerobic conditions on Brucella blood agar (BBA). Specimens from the paranasal sinuses, gums, or the oral mucosa can be inoculated on other media as well, depending on the occasion (e.g., MacConkey's for Gram negatives, Fildies for H. influenzae, media for anaerobes, Capnocytophaga spp.).
Following the isolation of the pathogen, serologic typing (e.g., Streptococcus group A, H. influenzae group B, N. meningitidis groups A, B, C) as well as antibiotic susceptibility testing are usually performed.
Lower Respiratory Tract Infections (LRTI)
Lower respiratory tract infections (LRTIs) are the third most important cause of mortality globally and are responsible for more than 4 million deaths annually.55
Blood Specimens and Culture
There are > 100 pathogens that may infect the lower respiratory tract (LRT) and produce secondary bacteremia. Additionally, invasive techniques cannot be routinely used, and sputum samples cannot be easily obtained from young children. The detection of living microorganisms in the blood of an ill child is of great diagnostic and prognostic significance, and blood culture should be considered when there is fever (≥ 38 ° C), hypothermia (≤ 36 ° C), leukocytosis, or fever and neutropenia (< 1000 PMN/mL). Semi-automated blood culture systems are present in nearly every clinical laboratory. Two or three separate blood cultures per 24 hours (ideally before initiation of treatment) should be collected under aseptic conditions and directly into culture bottles from every child hospitalized with pneumonia. Avoidance of transport tubes allows bacteria to begin growing immediately, decreases the amount of anticoagulant to which bacteria are exposed (anticoagulant may be inhibitory for some bacteria), and decreases the risk of needlestick accidents among health care personnel. Skin should always be disinfected with povidone iodine (must be allowed to completely dry), 70% isopropyl alcohol, or iodine prior to venipuncture to minimize contamination with skin microorganisms. Obtaining blood for culture from intravascular catheters in the absence of peripheral blood culture should be discouraged because of the frequent isolation of coagulase-negative Staphylococci and other skin flora. However, if there is no other option, the line must be adequately disinfected and flushed of all inhibitory substances before the specimen is obtained. The amount of fluid flushed from the line is based on the weight and size of the child.56 For infants, minimal discard volumes are in the range of 0.3 to 1.0 mL.57 Media-containing resins are often used to adsorb antibiotics or inhibitory substances that may be present in a patient's blood and thus improve microbial detection. In infants and young children, 1 to 5 mL/culture and in older children 10 mL/culture provide optimal recovery for the diagnosis of sepsis.58 In general, the total blood volume withdrawn for two bacterial cultures should not exceed 1% of the patient's total blood volume. Larger volumes of blood are necessary to maximize yield since 10% to 20% of pediatric patients may have low-grade bloodstream infections. Blood culture bottles that contain approximately 20 mL of broth and that accommodate an inoculation volume of up to 4 mL are available, thus allowing for a close approximation of the recommended blood-to-broth ratio necessary to diminish the effect of growth inhibitors. For the majority of patients, culture of the entire volume in a single (or additional) aerobic bottle is the most effective approach because anaerobic infections are rare among children. Patients at increased risk for anaerobic sepsis include immunocompromised children and those with infections located at areas outside the respiratory tract. Blood and tissue specimens for the diagnosis of Q fever (C. burnetii) should be frozen at -70 ° C until shipped, while clinical samples suspected of Francisella tularensis infection should be rapidly transported to the laboratory or frozen and shipped on dry ice. Prolonged incubation beyond 5 days is not necessary for automated instruments, although blind subculture may be needed if the patient is receiving antimicrobials at the time of blood collection.59, 60
Positive blood culture bottles are initially evaluated by Gram staining of a smear, and subculturing on suitable media should commence, depending on the organism seen. Blood cultures are polymicrobial in 5% to 10% of cases. Therefore additional inoculation on a CNA or other medium inhibitory for Gram-negative organisms is recommended for smears indicative of Gram-negative bacilli, and on MacConkey's or related selective agar for smears showing Gram-positive organisms. Inoculation on media for anaerobes is advocated when the smear is suggestive of such microbes or when the organism is recovered from the anaerobic culture bottle only.
Blood isolates should be evaluated in relation to the clinical findings of a patient. Growth of common pathogens such as S. pneumoniae, H. influenzae, S. aureus, β-haemolytic Streptococcus group A or B, and K. pneumoniae demonstrates the etiologic microorganism. In specific groups of children, such as immunocompromised or hospitalized patients in intensive care units (ICUs), other uncommon pathogens may develop such as Candida spp., Cryptococcus neoformans, and others. Some bacteria (e.g., Legionella spp., mycobacteria, some N. meningitidis strains, and N. gonorrhoeae) cannot grow on routine media, and detection takes place by other methods such as lysis centrifugation. Growth of Staphylococcus epidermidis (coagulase-negative), corynebacteria, Bacillus spp. and propionibacteria is usually associated with contamination of the sample. In general, single cultures that are positive for any of these bacteria represent contamination, whereas multiple separate positive cultures are more likely to indicate a clinically significant bacteremia, which may result in sepsis, septic shock, or severe sepsis.
Blood cultures are positive in only < 10% of pediatric RTIs due to either the characteristics of the pathogen, the fact that a microbe may not be causing bacteremia or it may be causing limited or intermittent bacteremia, insufficient sample collection, autolysis of a microbe during culture, prior antibiotic intake, or other factors.
Urine Specimens
Urinary samples may be used for the detection of antigens from pneumococcus, H. influenzae, and Legionella.
Lower Respiratory Tract Specimens
Candidate samples for processing include the noninvasive sputum and tracheobronchial aspirates (TBA through catheter), as well as the invasive transtracheal (percutaneous) aspirates, bronchial wash, bronchoalveolar lavage (BAL), protected bronchial brush (PBB), pulmonary aspirate, pulmonary tissue specimens (collected either via fine-needle transthoracic aspiration or open or thoracoscopic biopsies), and pleural fluid (via thoracocentesis). See Table 24-6 for sensitivity and specificity of these methods. Among these, percutaneous pulmonary and transtracheal aspirates and PBB specimens are the only samples, acceptable for culturing under anaerobic conditions. BAL is collected after washing of the lower airways with normal saline, which is aspirated at low pressure (< 100 Torr) in order to avoid collapse and damage of the bronchial wall (a hemorrhagic specimen has a lower diagnostic value). For children < 20 kg, the volume of the administered normal saline is 3 mL/kg divided into 3 equal parts, and the collected specimen is considered adequate when > 40% of the instilled volume is returned back (the patient's age is usually inversely proportional to the percentage of aspirated fluid).61 Indications for BAL include hospital-acquired pneumonia (ventilator-associated pneumonia [VAP], aspiration pneumonia); complicated community acquired pneumonia (CAP); CF; severe viral respiratory tract infections; mycobacterial, fungal, and parasitic infections; as well as pneumonia among immunosuppressed individuals. The PBB technique is applied since 1979 for collection of specimens mainly in the context of complicated bacterial CAP with introduction of a double telescopic catheter via a bronchoscope. On the other hand, saliva, oropharyngeal secretions, sinus drainage from the nasopharynx, swab samples, and 24-hour sputum collections are considered unsuitable for identification of organisms from the LRT.
Table 24-6.
Comparison of Specimen Collection Techniques Intended for Culture from the Lower Respiratory Tract
| Non-Bronchoscopic Techniques | Sensitivity (%) | Specificity (%) |
|---|---|---|
| Collection of endotracheal secretions | 38-100 | 14-100 |
| Blind specimen collection (BBS) | 74-97 | 74-100 |
| Mini-BAL | 63-100 | 66-96 |
| Blind specimen collection with protected bronchial brush (BPBB) | 58-86 | 71-100 |
| Bronchoscopic Techniques | ||
| Bronchoalveolar lavage (BAL) | 42-93, 73* | 45-100, 82* |
| Protected bronchial brush (PBB) | 33-100, 67* | 50-100, 95* |
Median value.
Modified from Baselski VS, Wunderink RG. Bronchoscopic diagnosis of pneumonia. Clin Microbiol Rev. 1994;7:533-558.
At least 1 mL of any aforementioned LRT secretion should be transported in a sterile container, while tissue should be placed in an anaerobic transport system or a sterile screw-cap container with several drops of sterile saline to keep small pieces of tissue moist. Lavage specimens are collected in the trap, which is adjusted to the bronchoscope, while the PBB specimen is the brush itself that is cut and placed in a sterile container with 1 mL of sterile normal saline or Brain-Heart Infusion broth. A sucrose-phosphate-glutamate transport medium containing BSA is often used to transport Rickettsiae, Mycoplasmas, and Chlamydiae.62 Occasionally, quantitative cultures of BAL or PBB specimens may help in distinguishing upper-tract contamination from lower-tract disease. If > 10 mL of BAL is collected, the sample should be centrifuged prior to plating.
With the exception of CF patients, obtaining adequate sputum specimens in children may prove problematic, and the help of a physiotherapist is highly advisable. The latter aid in provocation of induced cough (e.g., with slight pressure over the cricothyreoid cartilage), mobilization of secretions (e.g., with vibration and percussion manipulations, huffing games), and bronchial drainage.63 Preferably the first morning sputum before breakfast or alternatively sputum induced by the inhalation of aerosolized 0.9% to 7% sterile saline should be expectorated in a sterile container following appropriate oral hygiene with sterile water or normal saline and a toothbrush (without toothpaste for 5 to 10 minutes) to remove the normal oral flora. Tap water should be avoided because it may contain atypical mycobacteria or Legionella spp. and may obscure culture results. Occasionally, a Dacron or rayon swab is placed at the posterior pharynx of CF patients younger than 10 years of age for the induction of cough and collection of an LRT specimen (gagged or cough specimen), which is shown to have a high positive predictive value.64 Alternatively, one can ask the patient to cough twice over a plate (or more than one plate possibly with different nutritive media), which is a more sensitive method compared to cough specimens.65 In general, LRT specimens should be transferred to the laboratory within 2 hours at room temperature or stored for up to 24 hours at 2° to 8 ° C, with the exception of induced sputum that should be constantly kept at room temperature (up to 24 hours) since its collection. Sputum of CF patients may be preserved at 4 ° C for 24 hours without affecting the isolation of pathogens, which are of interest in this disorder.
Macroscopic and Microscopic Examination of an LRT Specimen
The appearance, color, consistency (e.g., purulent, mucoid, serous, bloody), quantity, smell, and presence of visible formations (e.g., Curschmann's spirals, Actinomyces granules) in LRT specimens should all be considered. The sample should be first vortexed and, if applicable, inoculated for a qualitative culture and then processed with equal volume of 0.5% to 2% N-acetyl-L-cysteine (Mucomyst) or DTT (Sputasol) solution if mucoid. Cell counts are determined with flow cytometry, and cytocentrifugation (600 to 800 rpm, 20 minutes) follows. Gram (or other) staining of the sediment and microscopic examination is necessary for evaluating the suitability of a sample. A number of > 10 squamous epithelial cells (SECs)/100× objective microscopic field shows that the sputum sample contains saliva and is unsuitable. For endotracheal aspirates, specimens are acceptable when there are < 10 SECs/average 100× field and bacteria detected in at least 1 of 20 such fields. In BAL, alveolar macrophages prevail (> 90%), while the presence of > 1% SECs indicates contamination with URT flora and renders the sample unacceptable. Unsuitable samples should be discarded, and the treating physician should be informed, except from the case of immunosuppressed patients, where samples are kept. Also, LRT specimens for the detection of M. pneumoniae, Legionella spp., dimorphic fungi, and M. tuberculosis should not be screened for adequacy and should be processed directly.
Specimens are also examined for inflammatory cells and the presence and characteristics of microbes such as how they Gram stain (positive versus negative); their shape (e.g., cocci versus diplococci, hyphae, blast cells), layout, and number; their intracellular or extracellular position; the prevalence of a single microbe population, and so on. Direct examination of the specimen with Gram staining along with compatible symptomatology is sensitive in only 10% of cases but has a specificity of 70% to 80%, which often allows for timely diagnosis and treatment of an LRTI since it is an easy, cheap, and fast method that provides information within 1 hour. Gram staining following processing with sterile normal saline in order to remove URT flora (washed sputum) demonstrates a sensitivity of 86%, 81%, and 91% and a specificity of 95%, 97%, and 98% for H. influenzae, S. pneumoniae, and M. catarrhalis, respectively.66 Bacteria in Gram-stained smears should be reported if they are potential pathogens and should be reported as normal respiratory flora if they are insufficient in quantity or not representative of potential pathogens. Stained smears of patients with aspiration pneumonia are characterized by many PMNs and mixed intracellular respiratory flora, (commonly Streptococci and anaerobes) and should be discriminated from contaminating respiratory flora. The presence of intracellular microbes in alveolar macrophages of BAL has high sensitivity and specificity for the diagnosis of VAP. Depending on the suspected pathogen, other stains are modified (Kinyoun) acid fast stain (Nocardia), Ziehl-Neelsen (mycobacteria), Giemsa, Gomori's Methenamine silver, Toluidine blue, and Calcofluor white (fungi and Pneumocystis). The absence of findings despite related clinical suspicion increases the probability of an atypical pneumonia due to mycoplasmas, mycobacteria, Legionella spp., parasites, and so on. Moreover, an endotracheal tube may add inflammatory cells to a tracheal aspirate, even in the absence of infection.
Culture of Lower Respiratory Tract Specimen
LRT bacterial pathogens include S. pneumoniae, H. influenzae, M. catarrhalis, K. pneumoniae, Enterobacteriacae, P. aeruginosa, S. aureus, Legionella spp., Mycobacterium spp., Fusobacterium nucleatum, Chlamydia spp., M. pneumoniae, S. pyogenes, P. multocida, Bordetella spp., Pseudomonas spp., Nocardia spp., Prevotella melaninogenicus, and various oropharyngeal flora anaerobes. S. aureus is found in the BAL fluid in 30% of CF children with an average age of 3 months.67 The small-colony variant (SCV) phenotype of S. aureus is also common among these patients,68 and the prevalence of MRSA is steadily increasing.69 Non-encapsulate and non–type B capsulate H. influenzae are more common in children with CF than in older patients. P. aeruginosa is the most common pathogen cultured from CF sputum and may be seen early in infancy and often cultured intermittently thereafter. Eventually chronic infection develops, and this leads to a faster decline in lung function. Other bacteria, such as Burkholderia cepacia complex, Burkholderia pseudomallei, Stenotrophomonas maltophila, Achromobacter xylosoxidans, Pandoraea apista, and non-tuberculous mycobacteria are also commonly isolated from this patient population.
Positive cultures from blood or pleural fluid are obtained in only about 10% of pneumonias, while sputum cultures offer clinically useful information in 10% to 15% of cases only. Approximately 30% of patients with purulent sputum do not have clinically evident pneumonia, and only 60% of patients with pneumonia produce purulent sputum. Moreover, 10% of patients with nonpurulent sputum suffer from pneumonia and 40% to 50% of the samples are unsuitable for culture, even from patients with indicative symptomatology.
Qualitative (or Semiquantitative) Culture
Common Microbes:
Sputum samples are initially centrifuged (1500 to 1800 × g, 15 to 20 minutes) and subsequently inoculated on SBA (35 °C, 5% CO2, 48 to 72 hours), CBA with 20,000 IU/L or 10 IU disk of bacitracin (35 ° C, 5% to 10% CO2, 24 to 48 hours), and MacConkey's agar (35 ° C, aerobically, 24 to 48 hours) (Fig. 24-4 ). As with URT specimens, inoculation should be performed on a small part of the agar plate (~¼), and a sterile loop should be used to dilute the sample satisfactorily and obtain isolated colonies.
Figure 24-4.

Culture of Streptococcus pneumoniae on blood Agar with an inhibition zone around the optochin disk (P).
The same procedure is applied for bronchoalveolar brushings and washings, TBA, and BAL with additional inoculation on anaerobic CNA for the two latter. In the case of BAL fluid, it can also be cultured under anaerobic conditions on BBA, laked blood with kanamycin and vancomycin (LKV), and CNA. Table 24-7 features criteria for interpretation of LRT specimen cultures.
Table 24-7.
Interpretation of Bacterial Lower Respiratory Culture Results
| Specimen | Probably Significant | Probably Insignificant | Additional Information Supporting Significance |
|---|---|---|---|
| Spontaneous or induced sputum | Predominant organism present in Gram stain and culture Abundant PMNs |
Organism not present in Gram stain and only 1 to 2+ growth in culture No abundant PMNs |
Intracellular location of organism |
| Endotracheal tube aspirate | Predominant organism present in Gram stain and culture Abundant PMNs |
Organism only 1 to 2+ growth in culture No abundant PMNs |
Organism in > 106 CFU/mL Intracellular location of organism |
| Bronchoalveolar lavage fluid | Predominant organism seen in every 100× field of Gram stainQuantitative culture detects > 105 CFU of organism/mL | Organism not present in Gram stain Quantitative culture detects < 104 CFU of organism/mL |
Intracellular location of organism |
PMN, Polymorphonuclear neutrophil.
Modified from Thomson RJ. Use of microbiology laboratory tests in the diagnosis of infectious diseases. In: Tan J, ed: Expert Guide to Infectious Diseases. Philadelphia: American College of Physicians, 2002, pp 1-41.
Uncommon Microbes:
Special transport and culture media are used for some microbes such as Hemophilus spp. (Fildies medium at 35 ° C, 10% CO2, 24 to 48 hours), Legionella spp. (buffered charcoal yeast extract with and without antimicrobial agents such as vancomycin, polymyxin B, and anisomycin; aerobically at 35 ° C, humidity, 5 to 10 days), Chlamydia spp. (prompt transport in antibiotic, e.g., gentamycin and nystatin containing media for 24 to 48 hours at 4 ° C, or for longer periods at –70 ° C, and inoculation in shell vials using McCoy cells for C. trachomatis and C. psittaci, and Hep-2 cells for C. pneumoniae), Burkholderia (Pseudomonas) cepacia in CF patients (P. cepacia selective agar and oxidative-fermentative-polymyxin B-bacitracin-lactose [OFPBL] agar), Mycoplasma pneumoniae (albumin and penicillin containing transport medium for up to 24 to 48 hours at 4 ° C, or for longer periods at –70 ° C and inoculation on Mycoplasma-Glucose agar, Methylene Blue-Glucose biphasic agar, or SP-4 agar for up to 3 weeks), SCV S. aureus (Mannitol Salt Agar) and Nocardia spp. (incubation up to 3 weeks at 35 ° C using the selective BCYE agar, while samples without significant cross-contamination may be inoculated on SBA, CBA, and Sabouraud with added bovine heart extract, Lowenstein-Jensen, and so on) (Fig. 24-5 ). For Legionella spp., the specimen is initially diluted 10-fold in a bacteriologic broth (e.g., tryptic soy or sterile water) to dilute inhibitory substances, and because this organism grows slowly, heavily contaminated samples should be subsequently disinfected from other bacteria by 1:10 dilution in KCl-HCl pH = 2.2, irrigation, and incubation for 4 minutes only at room temperature. In CF patients, it is now necessary to cultivate sputum for Nontuberculous Mycobacteria spp. (NTM), which is performed by treatment with 0.25% N-acetyl-L-cysteine-1% sodium hydroxide-5% oxalic acid for removal of P. aeruginosa and inoculation on Lowenstein-Jensen medium or automated liquid systems. Molecular techniques such as Accuprobe are used for typing.70 If the sample is suitable for anaerobic culture, one can use the BBA, LKV agar (Laked blood with canamycin and vancomycin), BBE (Bacteroides bile esculin) agar, and CNA.
Figure 24-5.
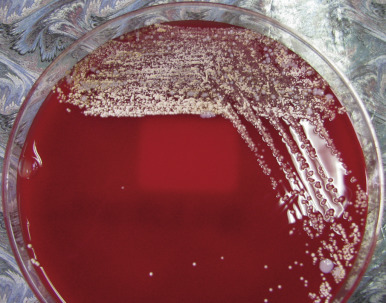
Sputum culture on sheep blood Agar with chalk-white colonies of Nocardia spp.
Quantitative Culture
Such cultures are necessary for the diagnosis of VAP, aspiration pneumonia, pneumonia in immunosuppressed individuals or CF patients, and tuberculosis. The most common microbial pathogens among ICU patients are: S. aureus, P. aeruginosa, Enterobacter spp., and multiresistant Acinetobacter baumanii. VAP is polymicrobial in 20% to 40% of cases, while the role of anaerobes has not been yet determined.71 Aspiration pneumonia is usually attributed to oral flora anaerobes (e.g., Bacteroides, Prevotella, Porphyromonas, Fusobacterium, and anaerobic cocci), either alone or together with aerobes. Middle-lobe syndrome is usually due to H. influenzae, S. pneumoniae, and S. aureus.
Protected Bronchial Brush (PBB) Specimen
A bronchial brush, which contains approximately 1 to 10 μL of secretions, should be placed in 1 mL of normal saline or common broth, transferred promptly to the lab, and homogenized with Vortex for 30 seconds. A smear is prepared by cytocentrifugation for Gram staining, and 10 and 100 μL samples are cultured in the appropriate culture media in aerobic and anaerobic conditions. A single colony in the agar plate corresponds to 10 CFU/mL of the initial sample, and this should be multiplied by the dilution factor of the sample in order to estimate the colonies/mL. Identification of ≥ 103 CFU/mL (corresponding to 106 CFU of original specimen/mL) is associated with active infection,72, 73 while lower counts represent possible cross-contamination.
Bal
Five to 10 mL samples are used without prior centrifugation after 30 to 60 seconds vortexing, while 10 to 100 mL BAL is considered to contain 1 mL of bronchopulmonary secretions.72, 73 Culture is made by means of both calibrated loops and 100-fold successive dilutions.74 Ten μL and 1 μl BAL are inoculated on agar media, and the respective 1:100 and 1:1000 dilution is noted. The agar plates are incubated at 35 ° C, aerobically for 4 to 7 days. Recovery of < 104 bacteria/mL is most likely to represent contamination, while > 105 bacteria/mL is indicative of active infection. Detection of 104 to 105 bacteria/mL constitutes a “gray zone.” The presence of intracellular bacteria in > 5% to 7% of the total number of cells is associated with VAP.
Detection of Elastin Fibers in LRT Specimen
Elastin fibers in bronchoscopy samples derive from destruction of the parenchyma, which is associated with necrotic pneumonia from aerobic Gram-negative bacteria, Enterobacteriaceae (Klebsiella spp., Enterobacter spp.). Detection is simple with the use of KOH solution and is increased among patients with VAP or ARDS compared to normal subjects.72, 73 Elastin fibers may also be visualized microscopically in stained smears using a 10× objective.
Antigen Detection
Such assays allow prompt diagnosis of the underlying pathogen using any respiratory, blood, or urine specimen by means of DIF (e.g., diagnosis of pertussis), EIA with polyclonal or monoclonal antibodies causing Latex particle agglutination, OIA, and plaque or strip immunochromatography (e.g., diagnosis of group A Streptococcus, S. pneumoniae, M. pneumoniae, C. pneumoniae, Legionella). The reported sensitivity for EIA and OIA for the detection of group A Streptococcus is 60% to 95% but can be as low as 31%.75 The Wellcogen-Latex urine test, which is applied on heated noncondensed urine, has been shown to have high sensitivity and specificity for the detection of H. influenzae type B among chidren,76 while good results have also been obtained with the Directigen and Bactigen reagents for Latex among adults.77 Membrane immunochromatography for the detection of Legionella antigen in urine provides a result within 15 minutes but covers serogroup 1 only. Urine detection of the polysacharitic antigen C, which is present in all pneumococcal serotypes, is performed with the use of the Binax NOW immunochromatography method (Binax, Portland, ME), with high sensitivity among children with documented invasive pneumococcal infection (bacteremia and segmental pneumonia).78 However, the capability of this method to discriminate between patients with true pneumococcal disease and children with rhinopharyngeal carriage is questionable.79, 80, 81
Serology
This method is of particular importance for the diagnosis of pathogens responsible for atypical pneumonias. Immune response for M. pneumoniae is against glycolipids and proteins of the microbe. IgM may persist for months or years, while there is a variety of nonspecific antibodies that help in diagnosis.82 CFix by incubation of the patient's serum with M. pneumoniae antigen and a defined quantity of guinea pig complement is used for the detection of anti-glycolipid antibodies, which gradually decrease after 1 month and remain low for 3 to 4 years.83 A four-fold rise in titer or a titer ≥ 1:32 in convalescent serum sets the diagnosis. The sensitivity is 80% to 95% for the first criterion and 60% for the second. There are cross-reactions in 10% of patients with bacterial meningitis or pancreatitis.83, 84 CFix is mainly used for measurement of IgM and detection of recent infection among children,82 and although inexpensive, this method can be technically demanding and time-consuming and is thus gradually replaced by ELISA, which is nowadays the method of choice. ELISA for IgM detection may diagnose infection using only one sample, if this is collected after the tenth day of illness. The method has a > 99% sensitivity and 98% specificity when compared to samples positive with CFix. Only μ-capture IgM-ELISA is absolutely specific, while the specificity of other ELISA kits ranges between 25% and 90%.85 Sensitivity is lower with IgG-ELISA.86 Commercially available reagents with rapid membrane ELISA are easy to perform and give results in less than 15 minutes. ImmunoCard (Meridian) measures IgM antibodies and is reliable in children. Remel EIA detects total antibodies in sera with a CFix titer ≥ 1:64. They do not require specialized equipment, and they have a positive and negative predictive value of > 90%.83 Qualitative agglutination assays in card form and quantitative agglutination as microtiter plates are simple, and a titer ≥ 1:160 or four-fold increase is indicative of recent infection.82 Cryoagglutinins are nonspecific IgM antibodies, appear 1 week after infection, and remain for 3 to 5 months. A titer of ≥ 1:32 is sufficient for a diagnosis, while higher titers are associated with more severe disease. They are detected in 50% to 60% of pneumonia cases, and cross-reactions with other bacterial and viral infections are observed.83 A combination of μ-capture IgM-ELISA and PCR provides a > 90% success rate during the acute phase of illness.
The surface antigens of Chlamydia and Chlamydophila lipopolysaccharide (LPS) produce a strong immune response. CFix detects anti-LPS antibodies, which are specific for the genus and common for all Chlamydia, and microfluorescence (MIF) uses an antigen from the elementary bodies, specific for the species.87 The Centers for Disease Control and Prevention (CDC) considers C. psittaci infection confirmed when there is a compatible clinical presentation and one of the following laboratory findings: IgM titer ≥ 1:16 (MIF), positive culture, or a four-fold increase in titer with CFix or MIF (at least 1:32) in samples that are separated by a 2-week time interval. A titer of ≥ 1:32 in a serum sample with compatible clinical presentation is a possible case.88 In the absence of a history of bird exposure, a positive result may be due to C. pneumoniae infection because of cross-reaction (common LPS).
MIF is the method of choice for the diagnosis of C. trachomatis pneumonia in infants, and only the titer of IgM ≥ 1:32 supports the diagnosis in neonates with compatible symptomatology. IgM (MIF) is present in virtually all neonates with pneumonia and about 30% of those with conjunctivitis due to the same pathogen. IgG does not help because maternal IgG titer is still high when the diagnosis of C. trachomatis is under investigation.
During the first infection with C. pneumoniae, IgM antibodies appear in 2 to 3 weeks from the beginning of disease, and IgG antibodies appear during the sixth to eighth week. During re-infection, IgM is absent or in low titers, and IgG appears in 1 to 2 weeks.89 MIF is the most sensitive and only acceptable method for diagnosis but is cumbersome, and there are limited standardized and reliable reagents on the market. Therefore, with regard to the use of MIF for the diagnosis of C. pneumoniae, the CDC set a number of criteria and requirements for antigen preparation, suitability of sample, evaluation of results, and so on, that should be strictly followed (Table 24-8 ).
Table 24-8.
Recommendations for the Use of Microfluorescence for the Diagnosis of C. Pneumoniae Infection
| Antigen | Purified Elementary Bodies |
|---|---|
| Sample | Couple of serum samples with 4 to 8 weeks in between |
| Test course | Initial dilution 1:8 or 1:16 and 2-fold dilutions Removal of IgG with anti-IgG before testing for IgM |
| Results | Reading with ocular 10× and objective 40× |
| Evaluation | Acute infection: IgM ≥ 1:16 or 4-fold rise in IgG Possible acute infection: IgG ≥ 1:512 Hypothetical past infection: IgG ≥ 1:16 |
| Quality assurance | Positive and negative control in every test Testing of positive control titer for consistency Maintenance of sera and reagents as indicated |
Modified from Dowell SF, Peeling RW, Boman J, et al. Standardizing Chlamydia pneumoniae assays: recommendations from the Centers for Disease Control and Prevention (USA) and the Laboratory Centre for Disease Control (Canada). Clin Infect Dis. 2001;33:492-50.
Upon a Legionella pneumophila infection, approximately 75% of patients seroconvert within weeks or months, and it is often necessary to examine several convalescent samples. IgM may remain for longer than 1 year and is thus a poor indicator of acute infection. IF is the reference method with 75% to 80% sensitivity and > 99% specificity when the L. pneumophila serotype 1 antigen is used,90 but the specificity is lower when the polyvalent antigen is used. For the diagnosis, seroconversion with a titer ≥ 1:128 is needed, while a titer of ≥ 1:256 is an indication of infection only during epidemics. ELISA may serve as a screening test, and its results need to be confirmed with IF. Agglutination assays permit the examination of multiple sera at the same time, have a high sensitivity and specificity, and are positive in 40% of cases during the first week of infection.
IF is the method of choice for Coxiella burnetii infection, and it has a high sensitivity and specificity without cross-reactions. About 90% of patients have detectable antibodies during the third week of infection that are gradually decreased within 12 months. IgM is no longer detected beyond 6 months. C. burnetii exists in two antigenic phases called phase I and phase II. Apart from a 4-fold increase, a titer of IgG ≥ 1:200 and/or/ IgM ≥ 1:50 against phase II is a strong indication of recent infection. There is a commercially available ELISA kit for the detection of phase II IgM, but the method is not standardized. Alternatively, agglutination assays and CFix have been attempted, but they lack in specificity.91 Antibodies to phase I antigens of C. burnetii generally require a longer time to appear and indicate continued exposure to the bacteria (chronic Q fever).
Serology for B. pertussis has a sensitivity that ranges between 60% and 95%.92 Reference laboratories use neutralization assays for the diagnosis of B. pertussis, while ELISA is the method of choice in clinical laboratories. IgM and IgA responses to toxin (PT) are a marker of infection, and 90% of patients have detectable IgG antibodies during the third to fourth week since the beginning of symptoms. Immune response depends on the age but also on prior exposure to the bacterium or to the antigen in the context of vaccination. This renders assessment difficult among vaccinated children. The acute phase sample is usually lost due to the delay in initiation of symptomatology. Comparison of antibody levels between mothers and children helps in the diagnosis of neonatal pertussis.
Antibodies G, A, and M against F. tularensis appear simultaneously during the first week after infection and remain for over 10 years, hence the presence of IgM does not prove recent infection. Agglutination assays are the method of choice, and a titer ≥ 1:160 is considered positive when there is compatible clinical presentation and no history of previous exposure or vaccination.
Detection of bacterial nucleic acid
The use of unsuitable culture media, transport media, and conditions as well as delays in transport may reduce the viability of a pathogen but may leave its nucleic acid still detectable. Also, nucleic acid persists in specimens after initiation of treatment93, 94 and may be detected in smaller and noninvasive specimens. On the other hand, due to the need for isolation of the organism for antibiotic susceptibility testing, cultures have been replaced by molecular methods only in cases in which the pathogens are of predictable susceptibility or the genetics of resistance are well defined, as with MRSA. Contribution of extracellular DNA and DNA that is derived from dead bacteria can be minimized by addition of propidium monoazide (PMA) to clinical samples before nucleic acid extraction. PMA enters cells whose structural integrity has been compromised, and intercalates with DNA, with which it cross-links upon exposure to a bright light source rendering it unsuitable to act as a PCR template. PMA treatment of samples generates bacterial community profiles that derive from DNA contained only intracellularly.
Species-specific PCR assays have been developed for numerous bacterial pathogens (e.g., L. pneumophila, C. trachomatis, N. gonorrhoeae, and Mycobacterium spp.) with greater accuracy and sensitivity of identification compared to conventional culture-based diagnostics. However, this approach requires a prediction to be made as to which is the most likely pathogen, as in the case of selective culture media. The nucleic acid–based assay for the detection S. pyogenes has a sensitivity of > 90%, and by many it is considered sensitive and specific enough to obviate confirmatory culture.95, 96 PCR for the detection of S. aureus in nasal swabs is as sensitive as culture but provides faster results.97 Detection of B. pertussis with PCR in a rhinopharyngeal sample is significantly more sensitive and specific compared to culture or IF and is the new gold standard of diagnosis.98, 99 In the cases of vaccinated patients, recent contact with an infected individual, sample collection during the paroxysmal stage of the illness, or after administration of antimicrobials, culture is often negative while PCR is positive.98 Moreover, the sensitivity of this method for the identification of Bordetella spp. is higher among neonates and infants.98, 99 PCR for the detection of M. pneumoniae on a rhinopharyngeal aspirate or swab, or a throat swab, is the most sensitive and specific method.100, 101 Similarly, C. pneumoniae PCR is highly sensitive and specific, although a positive result may indicate carriage only.100
PCR using blood specimens (whole blood, plasma, or Buffy coat) is mainly applied for the detection of S. pneumoniae, H. influenzae, and meningococcus, and the sensitivity and specificity of the method depends on the specimen. Reliability of blood PCR may be affected by prior antibiotic administration, colonization of the rhinopharynx, insufficient removal of hemoglobin (extended presence of porphyrin complexes interfere with the action of DNA polymerase), and small number of infected cells.102, 103
The more recent advent of real-time PCR allows prompt and accurate determination of bacterial load with even greater sensitivity.104 Multiplex PCR systems that allow simultaneous detection of six respiratory bacterial species have also been developed.105
The most important phylogenetically informative region of bacteria is the 16 S rRNA gene, which contains both highly conserved and highly variable regions; and sequence analysis of this gene allows bacterial identification at the genus or species level. It can be performed either on strains of already isolated bacteria or directly on clinical samples, and it has been used for identification of previously unrecognized species.106 The procedure involves nucleic acid extraction, amplification of the target sequence by PCR, sequence determination, and a computer software–aided search of a relevant sequence database. Disadvantages include the high cost of automated nucleic acid sequencers, lack of appropriate analysis software, and limited databases.
More effective means of resolving mixed bacterial PCR products generated from multispecies templates include MS-based approaches, which generate species identities depending on base composition signatures of the sequences amplified,107 and ultra-high throughput sequencing,108 which offers highly detailed bacterial community composition data.
References
The complete reference list is available online at www.expertconsult.com
References
- 1.Byington C.L., Castillo H., Gerber K. The effect of rapid respiratory viral diagnostic testing on antibiotic use in a children's hospital. Arch Pediatr Adolesc Med. 2002;156:1230–1234. doi: 10.1001/archpedi.156.12.1230. [DOI] [PubMed] [Google Scholar]
- 2.Johnston S.L., Pattemore P.K., Sanderson G. Community study of role of viral infections in exacerbations of asthma in 9-11 year old children. BMJ. 1995;310:1225–1229. doi: 10.1136/bmj.310.6989.1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Papadopoulos N.G., Bates P.J., Bardin P.G. Rhinoviruses infect the lower airways. J Infect Dis. 2000;181:1875–1884. doi: 10.1086/315513. [DOI] [PubMed] [Google Scholar]
- 4.Corne J.M., Marshall C., Smith S. Frequency, severity, and duration of rhinovirus infections in asthmatic and non-asthmatic individuals: a longitudinal cohort study. Lancet. 2002;359:831–834. doi: 10.1016/S0140-6736(02)07953-9. [DOI] [PubMed] [Google Scholar]
- 5.Contoli M., Message S.D., Laza-Stanca V. Role of deficient type III interferon-lambda production in asthma exacerbations. Nat Med. 2006;12:1023–1026. doi: 10.1038/nm1462. [DOI] [PubMed] [Google Scholar]
- 6.Wark P.A., Johnston S.L., Bucchieri F. Asthmatic bronchial epithelial cells have a deficient innate immune response to infection with rhinovirus. J Exp Med. 2005;201:937–947. doi: 10.1084/jem.20041901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Psarras S., Volonaki E., Skevaki C.L. Vascular endothelial growth factor–mediated induction of angiogenesis by human rhinoviruses. J Allergy Clin Immunol. 2006;117:291–297. doi: 10.1016/j.jaci.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 8.Hall C.B., McCarthy C.A. Respiratory Syncytial Virus. In: Mandell G.L., Bennett J.E., Dolin R., editors. Principles and Practice of Infectious Diseases. 6th ed. Elsevier Churchill Livingstone; Philadelphia: 2005. pp. 2008–2026. [Google Scholar]
- 9.Psarras S., Papadopoulos N.G., Johnston S.L. Parainfluenza viruses. In: Zuckermann A., Banatvala J., Griffiths P., editors. Principles and Practice of Clinical Virology. 5th ed. John Wiley & Sons; Chichester, UK: 2004. pp. 299–321. [Google Scholar]
- 10.van der Hoek L., Pyrc K., Jebbink M.F. Identification of a new human coronavirus. Nat Med. 2004;10:368–373. doi: 10.1038/nm1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ksiazek T.G., Erdman D., Goldsmith C.S. A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med. 2003;348:1953–1966. doi: 10.1056/NEJMoa030781. [DOI] [PubMed] [Google Scholar]
- 12.Rota P.A., Oberste M.S., Monroe S.S. Characterization of a novel coronavirus associated with severe acute respiratory syndrome. Science. 2003;300:1394–1399. doi: 10.1126/science.1085952. [DOI] [PubMed] [Google Scholar]
- 13.Poutanen S.M., Low D.E., Henry B. Identification of severe acute respiratory syndrome in Canada. N Engl J Med. 2003;348:1995–2005. doi: 10.1056/NEJMoa030634. [DOI] [PubMed] [Google Scholar]
- 14.van den Hoogen B.G., de Jong J.C., Groen J. A newly discovered human pneumovirus isolated from young children with respiratory tract disease. Nat Med. 2001;7:719–724. doi: 10.1038/89098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Osterhaus A., Fouchier R. Human metapneumovirus in the community. Lancet. 2003;361:890–891. doi: 10.1016/S0140-6736(03)12785-7. [DOI] [PubMed] [Google Scholar]
- 16.Spyridaki I.S., Christodoulou I., de Beer L. Comparison of four nasal sampling methods for the detection of viral pathogens by RT-PCR-A GA(2)LEN project. J Virol Methods. 2009;156:102–106. doi: 10.1016/j.jviromet.2008.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barenfanger J., Drake C., Mueller T. R-Mix cells are faster, at least as sensitive and marginally more costly than conventional cell lines for the detection of respiratory viruses. J Clin Virol. 2001;22:101–110. doi: 10.1016/s1386-6532(01)00171-8. [DOI] [PubMed] [Google Scholar]
- 18.Dunn J.J., Woolstenhulme R.D., Langer J. Sensitivity of respiratory virus culture when screening with R-mix fresh cells. J Clin Microbiol. 2004;42:79–82. doi: 10.1128/JCM.42.1.79-82.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ferris M.M., McCabe M.O., Doan L.G. Rapid enumeration of respiratory viruses. Anal Chem. 2002;74:1849–1856. doi: 10.1021/ac011183q. [DOI] [PubMed] [Google Scholar]
- 20.American Academy of Pediatrics Subcommittee on Diagnosis and Management of Bronchiolitis. Diagnosis and management of bronchiolitis. Pediatrics. 2006;118:1774–1793. doi: 10.1542/peds.2006-2223. [DOI] [PubMed] [Google Scholar]
- 21.Henrickson K.J., Hall C.B. Diagnostic assays for respiratory syncytial virus disease. Pediatr Infect Dis J. 2007;26:S36–S40. doi: 10.1097/INF.0b013e318157da6f. [DOI] [PubMed] [Google Scholar]
- 22.Landry M.L., Ferguson D. Suboptimal detection of influenza virus in adults by the Directigen Flu A+B enzyme immunoassay and correlation of results with the number of antigen-positive cells detected by cytospin immunofluorescence. J Clin Microbiol. 2003;41:3407–3409. doi: 10.1128/JCM.41.7.3407-3409.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hopkins P.M., Plit M.L., Carter I.W. Indirect fluorescent antibody testing of nasopharyngeal swabs for influenza diagnosis in lung transplant recipients. J Heart Lung Transplant. 2003;22:161–168. doi: 10.1016/S1053-2498(02)00467-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frisbie B., Tang Y.W., Griffin M. Surveillance of childhood influenza virus infection: what is the best diagnostic method to use for archival samples? J Clin Microbiol. 2004;42:1181–1184. doi: 10.1128/JCM.42.3.1181-1184.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Petric M., Comanor L., Petti C.A. Role of the laboratory in diagnosis of influenza during seasonal epidemics and potential pandemics. J Infect Dis. 2006;194(suppl 2):S98–S110. doi: 10.1086/507554. [DOI] [PubMed] [Google Scholar]
- 26.Treanor J. Influenza virus. In: Mandell G.L., Bennett J.E., Dolin R., editors. Principles and Practice of Infectious Diseases. 6th ed. Elsevier Churchill Livingstone; Philadelphia: 2005. pp. 2060–2085. [Google Scholar]
- 27.Myatt T.A., Johnston S.L., Rudnick S. Airborne rhinovirus detection and effect of ultraviolet irradiation on detection by a semi-nested RT-PCR assay. BMC Public Health. 2003;3:5. doi: 10.1186/1471-2458-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Papadopoulos N.G., Hunter J., Sanderson G. Rhinovirus identification by BglI digestion of picornavirus RT-PCR amplicons. J Virol Methods. 1999;80:179–185. doi: 10.1016/S0166-0934(99)00045-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kehl S.C., Henrickson K.J., Hua W. Evaluation of the Hexaplex assay for detection of respiratory viruses in children. J Clin Microbiol. 2001;39:1696–1701. doi: 10.1128/JCM.39.5.1696-1701.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liolios L., Jenney A., Spelman D. Comparison of a multiplex reverse transcription-PCR-enzyme hybridization assay with conventional viral culture and immunofluorescence techniques for the detection of seven viral respiratory pathogens. J Clin Microbiol. 2001;39:2779–2783. doi: 10.1128/JCM.39.8.2779-2783.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chi X.S., Li F., Tam J.S. Semiquantitative one-step RT-PCR for simultaneous identification of human influenza and respiratory syncytial viruses. J Virol Methods. 2007;139:90–92. doi: 10.1016/j.jviromet.2006.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Adhikary A.K., Inada T., Banik U. Identification of subgenus C adenoviruses by fiber-based multiplex PCR. J Clin Microbiol. 2004;42:670–673. doi: 10.1128/JCM.42.2.670-673.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Billaud G., Peny S., Legay V. Detection of rhinovirus and enterovirus in upper respiratory tract samples using a multiplex nested PCR. J Virol Methods. 2003;108:223–228. doi: 10.1016/s0166-0934(03)00038-7. [DOI] [PubMed] [Google Scholar]
- 34.Mitchell S., O'Neill H.J., Ong G.M. Clinical assessment of a generic DNA amplification assay for the identification of respiratory adenovirus infections. J Clin Virol. 2003;26:331–338. doi: 10.1016/s1386-6532(02)00082-3. [DOI] [PubMed] [Google Scholar]
- 35.Ellis J.S., Zambon M.C. Combined PCR-heteroduplex mobility assay for detection and differentiation of influenza A viruses from different animal species. J Clin Microbiol. 2001;39:4097–4102. doi: 10.1128/JCM.39.11.4097-4102.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dagher H., Donninger H., Hutchinson P. Rhinovirus detection: comparison of real-time and conventional PCR. J Virol Methods. 2004;117:113–121. doi: 10.1016/j.jviromet.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 37.Nijhuis M., van Maarseveen N., Schuurman R. Rapid and sensitive routine detection of all members of the genus enterovirus in different clinical specimens by real-time PCR. J Clin Microbiol. 2002;40:3666–3670. doi: 10.1128/JCM.40.10.3666-3670.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maertzdorf J., Wang C.K., Brown J.B. Real-time reverse transcriptase PCR assay for detection of human metapneumoviruses from all known genetic lineages. J Clin Microbiol. 2004;42:981–986. doi: 10.1128/JCM.42.3.981-986.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ng L.F., Wong M., Koh S. Detection of severe acute respiratory syndrome coronavirus in blood of infected patients. J Clin Microbiol. 2004;42:347–350. doi: 10.1128/JCM.42.1.347-350.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Boivin G., Cote S., Dery P. Multiplex real-time PCR assay for detection of influenza and human respiratory syncytial viruses. J Clin Microbiol. 2004;42:45–51. doi: 10.1128/JCM.42.1.45-51.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Templeton K.E., Scheltinga S.A., Beersma M.F. Rapid and sensitive method using multiplex real-time PCR for diagnosis of infections by influenza A and influenza B viruses, respiratory syncytial virus, and parainfluenza viruses 1, 2, 3, and 4. J Clin Microbiol. 2004;42:1564–1569. doi: 10.1128/JCM.42.4.1564-1569.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hibbitts S., Rahman A., John R. Development and evaluation of NucliSens basic kit NASBA for diagnosis of parainfluenza virus infection with ‘end-point’ and ‘real-time’ detection. J Virol Methods. 2003;108:145–155. doi: 10.1016/s0166-0934(02)00268-9. [DOI] [PubMed] [Google Scholar]
- 43.Loens K., Ieven M., Ursi D. Improved detection of rhinoviruses by nucleic acid sequence–based amplification after nucleotide sequence determination of the 5' noncoding regions of additional rhinovirus strains. J Clin Microbiol. 2003;41:1971–1976. doi: 10.1128/JCM.41.5.1971-1976.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang D., Coscoy L., Zylberberg M. Microarray-based detection and genotyping of viral pathogens. Proc Natl Acad Sci U S A. 2002;99:15687–15692. doi: 10.1073/pnas.242579699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hughes T.R., Mao M., Jones A.R. Expression profiling using microarrays fabricated by an ink-jet oligonucleotide synthesizer. Nat Biotechnol. 2001;19:342–347. doi: 10.1038/86730. [DOI] [PubMed] [Google Scholar]
- 46.Biel S.S., Madeley D. Diagnostic virology—the need for electron microscopy: a discussion paper. J Clin Virol. 2001;22:1–9. doi: 10.1016/s1386-6532(01)00151-2. [DOI] [PubMed] [Google Scholar]
- 47.Ellis J.S., Zambon M.C. Molecular diagnosis of influenza. Rev Med Virol. 2002;12:375–389. doi: 10.1002/rmv.370. [DOI] [PubMed] [Google Scholar]
- 48.Poon L.L., Wong B.W., Chan K.H. Evaluation of real-time reverse transcriptase PCR and real-time loop-mediated amplification assays for severe acute respiratory syndrome coronavirus detection. J Clin Microbiol. 2005;43:3457–3459. doi: 10.1128/JCM.43.7.3457-3459.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Keightley M.C., Sillekens P., Schippers W. Real-time NASBA detection of SARS-associated coronavirus and comparison with real-time reverse transcription-PCR. J Med Virol. 2005;77:602–608. doi: 10.1002/jmv.20498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang Z.W., Zhou Y.M., Zhang Y. Sensitive detection of SARS coronavirus RNA by a novel asymmetric multiplex nested RT-PCR amplification coupled with oligonucleotide microarray hybridization. Methods Mol Med. 2005;114:59–78. doi: 10.1385/1-59259-923-0:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lin B., Wang Z., Vora G.J. Broad-spectrum respiratory tract pathogen identification using resequencing DNA microarrays. Genome Res. 2006;16:527–535. doi: 10.1101/gr.4337206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Horejsh D., Martini F., Poccia F. A molecular beacon, bead-based assay for the detection of nucleic acids by flow cytometry. Nucleic Acids Res. 2005;33:e13. doi: 10.1093/nar/gni015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Amano Y., Cheng Q. Detection of influenza virus: traditional approaches and development of biosensors. Anal Bioanal Chem. 2005;381:156–164. doi: 10.1007/s00216-004-2927-0. [DOI] [PubMed] [Google Scholar]
- 54.Flayhart D., Hindler J.F., Bruckner D.A. Multicenter evaluation of BBL CHROMagar MRSA medium for direct detection of methicillin-resistant Staphylococcus aureus from surveillance cultures of the anterior nares. J Clin Microbiol. 2005;43:5536–5540. doi: 10.1128/JCM.43.11.5536-5540.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Murray C.J., Lopez A.D. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997;349:1269–1276. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- 56.Keller C.A. Methods of drawing blood samples through central venous catheters in pediatric patients undergoing bone marrow transplant: results of a national survey. Oncol Nurs Forum. 1994;21:879–884. [PubMed] [Google Scholar]
- 57.Shulman R.J., Phillips S., Laine L. Volume of blood required to obtain central venous catheter blood cultures in infants and children. JPEN J Parenter Enteral Nutr. 1993;17:177–179. doi: 10.1177/0148607193017002177. [DOI] [PubMed] [Google Scholar]
- 58.Szymczak E.G., Barr J.T., Durbin W.A. Evaluation of blood culture procedures in a pediatric hospital. J Clin Microbiol. 1979;9:88–92. doi: 10.1128/jcm.9.1.88-92.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Baron E.J., Scott J.D., Tompkins L.S. Prolonged incubation and extensive subculturing do not increase recovery of clinically significant microorganisms from standard automated blood cultures. Clin Infect Dis. 2005;41:1677–1680. doi: 10.1086/497595. [DOI] [PubMed] [Google Scholar]
- 60.Petti C.A., Bhally H.S., Weinstein M.P. Utility of extended blood culture incubation for isolation of Haemophilus, Actinobacillus, Cardiobacterium, Eikenella, and Kingella organisms: a retrospective multicenter evaluation. J Clin Microbiol. 2006;44:257–259. doi: 10.1128/JCM.44.1.257-259.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.de Blic J., Midulla F., Barbato A. Bronchoalveolar lavage in children. ERS Task Force on bronchoalveolar lavage in children. European Respiratory Society. Eur Respir J. 2000;15:217–231. doi: 10.1183/09031936.00.15121700. [DOI] [PubMed] [Google Scholar]
- 62.American Society for Microbiology; Washington, D.C: 1992. Clinical Microbiology Procedures Handbook. [Google Scholar]
- 63.Hough A. Physiotherapy in Respiratory Care. Chapman and Hall; London: 1996. Physiotherapy for children and infants; pp. 286–302. [Google Scholar]
- 64.Equi A.C., Pike S.E., Davies J. Use of cough swabs in a cystic fibrosis clinic. Arch Dis Child. 2001;85:438–439. doi: 10.1136/adc.85.5.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Maiya S., Desai M., Baruah A. Cough plate versus cough swab in patients with cystic fibrosis; a pilot study. Arch Dis Child. 2004;89:577–579. doi: 10.1136/adc.2003.037481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cao L.D., Ishiwada N., Takeda N. Value of washed sputum Gram stain smear and culture for management of lower respiratory tract infections in children. J Infect Chemother. 2004;10:31–36. doi: 10.1007/s10156-003-0277-z. [DOI] [PubMed] [Google Scholar]
- 67.Armstrong D.S., Grimwood K., Carzino R. Lower respiratory infection and inflammation in infants with newly diagnosed cystic fibrosis. BMJ. 1995;310:1571–1572. doi: 10.1136/bmj.310.6994.1571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kahl B.C., Duebbers A., Lubritz G. Population dynamics of persistent Staphylococcus aureus isolated from the airways of cystic fibrosis patients during a 6-year prospective study. J Clin Microbiol. 2003;41:4424–4427. doi: 10.1128/JCM.41.9.4424-4427.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Vergison A., Denis O., Deplano A. National survey of molecular epidemiology of Staphylococcus aureus colonization in Belgian cystic fibrosis patients. J Antimicrob Chemother. 2007;59:893–899. doi: 10.1093/jac/dkm037. [DOI] [PubMed] [Google Scholar]
- 70.Pierre-Audigier C., Ferroni A., Sermet-Gaudelus I. Age-related prevalence and distribution of nontuberculous mycobacterial species among patients with cystic fibrosis. J Clin Microbiol. 2005;43:3467–3470. doi: 10.1128/JCM.43.7.3467-3470.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chastre J., Fagon J.Y., Bornet-Lecso M. Evaluation of bronchoscopic techniques for the diagnosis of nosocomial pneumonia. Am J Respir Crit Care Med. 1995;152:231–240. doi: 10.1164/ajrccm.152.1.7599829. [DOI] [PubMed] [Google Scholar]
- 72.Investigation of bronchoalveolar lavage, sputum and associated specimens. Standards Unit, Evaluations and Standards Laboratory Centre for Infections; London: 2007. pp. 1–27. [Google Scholar]
- 73.Baselski V.S., Wunderink R.G. Bronchoscopic diagnosis of pneumonia. Clin Microbiol Rev. 1994;7:533–558. doi: 10.1128/cmr.7.4.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jacobs J.A., De Brauwer E.I., Cornelissen E.I. Accuracy and precision of quantitative calibrated loops in transfer of bronchoalveolar lavage fluid. J Clin Microbiol. 2000;38:2117–2121. doi: 10.1128/jcm.38.6.2117-2121.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Carroll K., Reimer L. Microbiology and laboratory diagnosis of upper respiratory tract infections. Clin Infect Dis. 1996;23:442–448. doi: 10.1093/clinids/23.3.442. [DOI] [PubMed] [Google Scholar]
- 76.Saha S.K., Baqui A.H., El Areefin S. Detection of antigenuria for diagnosis of invasive Haemophilus influenzae type B disease. Ann Trop Paediatr. 2006;26:329–336. doi: 10.1179/146532806X152854. [DOI] [PubMed] [Google Scholar]
- 77.Ajello G.W., Bolan G.A., Hayes P.S. Commercial latex agglutination tests for detection of Haemophilus influenzae type B and Streptococcus pneumoniae antigens in patients with bacteremic pneumonia. J Clin Microbiol. 1987;25:1388–1391. doi: 10.1128/jcm.25.8.1388-1391.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Neuman M.I., Harper M.B. Evaluation of a rapid urine antigen assay for the detection of invasive pneumococcal disease in children. Pediatrics. 2003;112:1279–1282. doi: 10.1542/peds.112.6.1279. [DOI] [PubMed] [Google Scholar]
- 79.Dominguez J., Blanco S., Rodrigo C. Usefulness of urinary antigen detection by an immunochromatographic test for diagnosis of pneumococcal pneumonia in children. J Clin Microbiol. 2003;41:2161–2163. doi: 10.1128/JCM.41.5.2161-2163.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Dowell S.F., Garman R.L., Liu G. Evaluation of Binax NOW, an assay for the detection of pneumococcal antigen in urine samples, performed among pediatric patients. Clin Infect Dis. 2001;32:824–825. doi: 10.1086/319205. [DOI] [PubMed] [Google Scholar]
- 81.Esposito S., Bosis S., Colombo R. Evaluation of rapid assay for detection of Streptococcus pneumoniae urinary antigen among infants and young children with possible invasive pneumococcal disease. Pediatr Infect Dis J. 2004;23:365–367. doi: 10.1097/00006454-200404000-00021. [DOI] [PubMed] [Google Scholar]
- 82.Waites K.B., Talkington D.F. Mycoplasma pneumoniae and its role as a human pathogen. Clin Microbiol Rev. 2004;17:697–728. doi: 10.1128/CMR.17.4.697-728.2004. table of contents. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Koneman's Color Atlas and Textbook of Diagnostic Microbiology. Lippincott Williams & Wilkins; Baltimore: 2006. Mycoplasmas and Ureaplasmas; pp. 1022–1063. [Google Scholar]
- 84.Baum G. Mycoplasma infection: Immunologic and Molecular Biologic Diagnostic Techniques. In: Rose N.R., Detrick B., editors. Manual of Clinical Laboratory Immunology. 6th ed. ASM Press; Washington DC: 2002. pp. 516–521. [Google Scholar]
- 85.Petitjean J., Vabret A., Gouarin S. Evaluation of four commercial immunoglobulin G (IgG)- and IgM-specific enzyme immunoassays for diagnosis of Mycoplasma pneumoniae infections. Pathol Biol (Paris) 2002;50:530–537. doi: 10.1016/s0369-8114(02)00349-8. [DOI] [PubMed] [Google Scholar]
- 86.Baum G. Mycoplasma pneumoniae and Atypical pneumonia. In: Mandell G.L., Dolin R., editors. Principles and Practice of Infectious Diseases. Elsevier Churchill Livingstone; Philadelphia: 2005. pp. 2271–2280. [Google Scholar]
- 87.Schachter J. Chlamydiae. In: Rose N.R., Detrick B., editors. Manual of Clinical Laboratory Immunology. ASM Press; Washington DC: 2002. pp. 522–527. [Google Scholar]
- 88.Schlossberg D. Chlamydophila (Chlamydia) psittaci (Psittacosis) In: Mandell G.L., Dolin R., editors. Principles and Practice of Infectious Diseases. Elsevier Churchill Livingstone; Philadelphia: 2005. pp. 2255–2258. [Google Scholar]
- 89.Kumar S., Hammerschlag M.R. Acute respiratory infection due to Chlamydia pneumoniae: current status of diagnostic methods. Clin Infect Dis. 2007;44:568–576. doi: 10.1086/511076. [DOI] [PubMed] [Google Scholar]
- 90.Edelstein P. Legionella. In: Murray P., editor. Manual of Clinical Microbiology. ASM Press; Washington DC: 2007. pp. 835–849. [Google Scholar]
- 91.Brouqui P., Rault D. Coxiella. In: Murray P., editor. Manual of Clinical Microbiology. ASM Press; Washington DC: 2007. pp. 1062–1069. [Google Scholar]
- 92.Loeffelholz M., Sanden G.N. Bordetella. In: Murray P., editor. Manual of Clinical Microbiology. ASM Press; Washington DC: 2007. pp. 803–814. [Google Scholar]
- 93.Gaydos C.A., Crotchfelt K.A., Howell M.R. Molecular amplification assays to detect chlamydial infections in urine specimens from high school female students and to monitor the persistence of chlamydial DNA after therapy. J Infect Dis. 1998;177:417–424. doi: 10.1086/514207. [DOI] [PubMed] [Google Scholar]
- 94.Lee H.H., Chernesky M.A., Schachter J. Diagnosis of Chlamydia trachomatis genitourinary infection in women by ligase chain reaction assay of urine. Lancet. 1995;345:213–216. doi: 10.1016/s0140-6736(95)90221-x. [DOI] [PubMed] [Google Scholar]
- 95.Heelan J.S., Wilbur S., Depetris G. Rapid antigen testing for group A Streptococcus by DNA probe. Diagn Microbiol Infect Dis. 1996;24:65–69. doi: 10.1016/0732-8893(95)00275-8. [DOI] [PubMed] [Google Scholar]
- 96.Heiter B.J., Bourbeau P.P. Comparison of the Gen-Probe Group A streptococcus Direct Test with culture and a rapid streptococcal antigen detection assay for diagnosis of streptococcal pharyngitis. J Clin Microbiol. 1993;31:2070–2073. doi: 10.1128/jcm.31.8.2070-2073.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Paule S.M., Pasquariello A.C., Hacek D.M. Direct detection of Staphylococcus aureus from adult and neonate nasal swab specimens using real-time polymerase chain reaction. J Mol Diagn. 2004;6:191–196. doi: 10.1016/S1525-1578(10)60509-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Muller F.M., Hoppe J.E., von Konig CH W.irsing. Laboratory diagnosis of pertussis: state of the art in 1997. J Clin Microbiol. 1997;35:2435–2443. doi: 10.1128/jcm.35.10.2435-2443.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Riffelmann M., von Konig CH W.irsing, Caro V. Nucleic acid amplification tests for diagnosis of Bordetella infections. J Clin Microbiol. 2005;43:4925–4929. doi: 10.1128/JCM.43.10.4925-4929.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ramirez J.A., Ahkee S., Tolentino A. Diagnosis of Legionella pneumophila, Mycoplasma pneumoniae, or Chlamydia pneumoniae lower respiratory infection using the polymerase chain reaction on a single throat swab specimen. Diagn Microbiol Infect Dis. 1996;24:7–14. doi: 10.1016/0732-8893(95)00254-5. [DOI] [PubMed] [Google Scholar]
- 101.Waris M.E., Toikka P., Saarinen T. Diagnosis of Mycoplasma pneumoniae pneumonia in children. J Clin Microbiol. 1998;36:3155–3159. doi: 10.1128/jcm.36.11.3155-3159.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Dagan R., Shriker O., Hazan I. Prospective study to determine clinical relevance of detection of pneumococcal DNA in sera of children by PCR. J Clin Microbiol. 1998;36:669–673. doi: 10.1128/jcm.36.3.669-673.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Toikka P., Nikkari S., Ruuskanen O. Pneumolysin PCR-based diagnosis of invasive pneumococcal infection in children. J Clin Microbiol. 1999;37:633–637. doi: 10.1128/jcm.37.3.633-637.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Rosey A.L., Abachin E., Quesnes G. Development of a broad-range 16S rDNA real-time PCR for the diagnosis of septic arthritis in children. J Microbiol Methods. 2007;68:88–93. doi: 10.1016/j.mimet.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 105.Benson R., Tondella M.L., Bhatnagar J. Development and evaluation of a novel multiplex PCR technology for molecular differential detection of bacterial respiratory disease pathogens. J Clin Microbiol. 2008;46:2074–2077. doi: 10.1128/JCM.01858-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Woo P.C., Lau S.K., Teng J.L. Then and now: use of 16S rDNA gene sequencing for bacterial identification and discovery of novel bacteria in clinical microbiology laboratories. Clin Microbiol Infect. 2008;14:908–934. doi: 10.1111/j.1469-0691.2008.02070.x. [DOI] [PubMed] [Google Scholar]
- 107.Ecker D.J., Sampath R., Massire C. Ibis T5000: a universal biosensor approach for microbiology. Nat Rev Microbiol. 2008;6:553–558. doi: 10.1038/nrmicro1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Bentley D.R., Balasubramanian S., Swerdlow H.P. Accurate whole human genome sequencing using reversible terminator chemistry. Nature. 2008;456:53–59. doi: 10.1038/nature07517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Myint S. Recent advances in the rapid diagnosis of respiratory tract infection. Br Med Bull. 2002;61:97–114. doi: 10.1093/bmb/61.1.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Thomson R.J. Use of microbiology laboratory tests in the diagnosis of infectious diseases. In: Tan J., editor. Expert Guide to Infectious Diseases. American College of Physicians; Philadelphia: 2002. pp. 1–41. [Google Scholar]
- 111.Dowell S.F., Peeling R.W., Boman J. Standardizing Chlamydia pneumoniae assays: recommendations from the Centers for Disease Control and Prevention (USA) and the Laboratory Centre for Disease Control (Canada) Clin Infect Dis. 2001;33:492–503. doi: 10.1086/322632. [DOI] [PubMed] [Google Scholar]


