Some of the most intensive human-animal interactions occur in the occupational setting. Animal workers may encounter hundreds to thousands of animals each day, which increases the risk of exposure to biological, physical, and chemical hazards. In recent years a number of emerging infectious diseases have first appeared—as deadly outbreaks among workers with animal exposures. In addition to zoonotic disease risks, high rates of allergic disease, physical injuries, and psychological stress have also been reported in animal handlers. Many animal workers in both developing and developed countries are not enrolled in formal occupational safety and health programs or may receive medical care from human health care providers who are not familiar with the occupational risks these workers face.
Veterinarians have a special role to play in the development of occupational safety and health strategies for animal workers because they are intimately familiar with animal diseases and the necessary procedures involved in animal care and handling. Therefore improving occupational health and safety among animal workers represents a global health challenge that will require increased communication and cooperation between human health and animal health care providers.
This chapter outlines the occupational health hazards that animal workers encounter, presents a One Health team approach to worker health and safety that involves both human and animal health professionals, and suggests preventive health programs for particular worker groups.
Key Points for Clinicians and Public Health Professionals
Public Health Professionals
-
•
Identify occupational groups in the community that have significant exposures to animals and work to educate them, local medical providers, and veterinary providers to ensure they receive appropriate preventive health services.
-
•
Work with local petting zoos, county fairs, pet stores, and other organizations involved in human contact with animals in public settings to ensure that the guidelines of the National Association of Public Health Veterinarians (NAPHV) for Animals in Public Settings (http://www.nasphv.org/Documents/AnimalsInPublicSettings.pdf) are being followed. This will help protect both the public and workers in such settings.
Human Health Care Providers
-
•
Ask patients whether they work with animals. If they do, assess their occupational risks.
-
•
If asked to provide medical services (such as a preplacement physical) for a worker with animal contact, consider contacting the veterinarian responsible for the health of the animals in the workplace to discuss specific occupational risks.
-
•
When evaluating a worker with an animal-related exposure (e.g., bite, scratch, mucous membrane contact), ensure that all potential zoonotic pathogens are being considered in the risk assessment and that prophylactic medication is started as necessary if indicated.
-
•
When evaluating animal workers with acute or chronic illnesses, including asthma, dermatitis, and other allergic conditions, determine whether work exposures could play a causative role.
-
•
If contracting to provide occupational health services to a group of workers with animal contact, employ a team approach to preventive care. The team should ideally include the veterinarian providing care to the animals as well as experts in exposure reduction such as an infection control/biosafety specialist and/or an industrial hygienist. This team approach will help ensure that relevant health risks in the workplace are being identified and addressed with adequate preventive services, including engineering controls, training, vaccination, postexposure protocols, and surveillance.
-
•
Counsel immunocompromised and pregnant workers about particular risks of animal handling.
-
•
Safeguard the confidentiality of any medical information about animal workers, including medical records and any information regarding immunocompromising conditions.
Veterinary Clinicians
-
•
If managing a clinical practice, ensure that policies and procedures are in place so that veterinary staff receive adequate preventive health services.
-
•
If providing veterinary services to a facility such as a zoo, animal shelter, research laboratory, or pet store, advise management about the need for adequate preventive health services for the animal workers.
-
•
Help inform human health care providers in the community who will be performing preplacement and follow-up examinations of workers about the occupational health risks and needs of animal workers.
-
•
Respect the confidentiality of any medical information about animal workers, including medical records and any information regarding immunocompromised individuals.
TYPES OF ANIMAL WORKERS
More than 2 million people in the United States are engaged in a wide range of occupational activities that involve animals.1 These include approximately 750,000 persons involved with livestock confinement; 500,000 involved with dairy farming2; 200,000 workers employed in animal care and services as kennel attendants, groomers, stable hands, zoo keepers, and animal trainers3; and 125,000 researchers and animal handlers involved with laboratory animal research.4 Globally, as much as 49% of the world's population is estimated to be involved in agriculture, which often involves animal husbandry and animal-associated health risks.5 Some of these workers are formally employed in full-time positions in animal-related care and may receive preventive health services (such as described in this chapter) through their workplace. However, many individuals who work part-time or full-time with animals may receive little or no preventive health services related to their work exposures. For example, staff at pet swap meets, pet store employees, volunteers at zoos and county fair animal exhibits, wildlife rehabilitators, wildlife biologists, volunteer animal rescue workers, individuals engaged in home slaughter of animals for family consumption, and subsistence (bushmeat) hunters may all face significant “occupational” health risks related to their contact with animals, yet may never receive preplacement examinations, prophylactic vaccinations, or follow-up surveillance examinations to prevent or detect work-related disease. If they do see a medical provider for care of a work-related injury or illness, that medical provider may not be aware of the range of health risks these workers face, and therefore the treatment or recommendations for prevention may not be optimal.
OCCUPATIONAL HEALTH APPROACH
The majority of occupational health services in the United States are provided by family physicians and other clinicians without specialized training.6 However, when using a team approach these individuals can learn to provide adequate occupational health services to animal workers.
The components of an occupational health approach are simple and adaptable to a wide range of work settings. They involve identification and control of hazardous exposures, medical services such as careful screening of workers at baseline, vaccination, surveillance of workers’ health, identification of sentinel health events, and management of necessary work restrictions and work-related problems. Although such preventive services may be viewed by some employers as an unnecessary expenditure of resources, they can be cost effective in the long run by preventing potentially compensable work-related illness and injury and promoting worker well-being. Box 12-1 illustrates this approach.
BOX 12-1. Components of Occupational Health Approach to Workplace Health Hazards.
-
•
Hazard identification
-
•
Hazard control using hierarchy of controls
-
•
Preplacement screening of workers
-
•
Preventive vaccines and training
-
•
Medical surveillance
-
•
Acute injury/illness management; identification of sentinel health events
-
•
Management of work restriction, job modification, and return to work
-
•
Confidential management of records and medical information
OCCUPATIONAL HEALTH TEAM
Because of the diversity of the hazards encountered by animal workers, providing effective occupational health services to such workers is best accomplished through a team approach. Such a team can include a medical provider to provide screening and management of medical problems, a veterinarian who is familiar with zoonotic disease risks, industrial hygienists to identify and evaluate hazardous exposures and help devise engineering and work practice controls to reduce them, and biosafety/infection control specialists to focus on zoonotic disease transmission risks. Figure 12-1 diagrams the ideal components of an occupational health team that provides preventive health care to animal workers.
Figure 12-1.

Occupational health team for animal workers.
Actively involving a designated human health care provider in an occupational health approach for animal workers also has many advantages. Such involvement can lead to the medical provider becoming more knowledgeable about the specific health risks faced by animal workers. Ongoing communication between the medical provider and the veterinarian helps ensure that injured workers are properly managed, workers at increased risk of illness (e.g., immunocompromised persons) and injury are adequately counseled, and preventable hazards in the workplace are identified and addressed.
Veterinarians can play key roles in an occupational health team. The veterinarian is the source of knowledge about relevant animal diseases and the necessary procedures of animal handling and typically has regular contact with the animals, the workplace, and the animal workers. In animal research facilities, the veterinarian is often the administrative supervisor of the animal care workers. In veterinary hospitals the veterinarian may be both the chief clinician and the practice director. For wildlife rehabilitation facilities, animal shelters, zoos, and many other settings, the consulting veterinarian may be the principal point of contact with the medical providers as well as the chief source of medical information about occupational health and safety hazards of the workplace. The veterinarian may be the health professional who is most familiar to the workers and with whom the workers have established a trusting relationship. The veterinarian may also be in regular contact with the employer or worksite supervisor and be able to advocate for the provision of occupational health services for the workers. For all these reasons the veterinarian may be the most appropriate professional to assemble and help lead the occupational health team as well as ensure that the services provided to workers are appropriate for the work setting.
Industrial hygienists have training in the identification and engineering control of a wide range of workplace hazards, including chemical, physical, and biological agents. Consultation from such individuals can help an occupational health team design safe strategies for the handling of hazardous chemicals such as cleaning agents and anesthetic gases, control of noise, and methods to reduce dust exposures that can cause allergy and infection.
Infection control and biosafety specialists are professionals who specialize in the prevention of infectious disease transmissions in workplaces and other settings. They can play a consulting role in the occupational health team by identifying specific infectious disease hazards and helping design strategies to reduce both animal-animal and animal-human transmission of disease. This may involve the design of ventilation systems and work policies such as disposal of infectious waste and use of personal protective equipment.
HAZARD IDENTIFICATION
Animal workers face a wide number of potential occupational health hazards that can be classified as biological, chemical, physical, or psychosocial. These hazards and their control are listed in Table 12-1 .
TABLE 12-1.
Occupational Hazards Encountered by Animal Workers and Relevant Hierarchy of Control Strategies
| Hazard | Elimination | Substitution | Engineering Controls | Administrative/ Work Practice Controls | Personal Protective Equipment |
|---|---|---|---|---|---|
| Biological | |||||
| Allergens, endotoxin | Eliminate particular allergenic source | Work with different species/gender with less allergenic potential; substitute bedding material that is less allergenic or dusty | Adequate ventilation in work areas; reduce dust generation; clean frequently; reduce animal density | Avoid wearing street clothes while working with animals1; perform animal manipulations in safety hood if possible; job modification or restriction for sensitized employees | Masks/respirators, gloves, gowns to reduce allergen exposure |
| Zoonoses41 | Vaccinate or otherwise eliminate disease in animals (preventive veterinary care) | Work with different species with less zoonotic potential | Nonporous surfaces; appropriate use of disinfectants; separation of patient areas from staff break areas; physical isolation of sick animals; disposal containers for infectious waste; needlestick prevention devices | Written infection control plan; hand hygiene; bite and other injury prevention; worker vaccination; restrict eating and drinking in care areas; consider job modification/restriction for immunocompromised or pregnant workers | Gloves, sleeves when handling fluids, infected animals, necropsy, dental procedures, resuscitation, obstetrics, diagnostic specimens, tick removalFacial protection for splash or spray Respirator use for abortions, poultry deaths, other aerosol riskFootwear and head cover when gross contamination is suspected |
| Pathogenic fungi | Prevent bats and birds from roosting in buildings | Control aerosolized dust, disinfect contaminated material, dispose of waste safety | Warn workers of risk | Disposable footwear and clothing, respirator use, gloves | |
| Live vaccines | Avoid use of live vaccines | Substitute vaccine with less risk to human beings | Needlestick prevention systems, sharps disposal containers | Needlestick prevention training, avoid recapping needles, report exposures; use tick repellant, perform frequent tick checks | Gloves, sleeves, leg coverings |
| Arthropods | Control mites, ticks, fleas in animals | Use of tick repellant, frequent tick checks | Protective clothing | ||
| Physical | |||||
| Bites, crush injuries | Avoid acquiring dangerous animals | Substitute less-dangerous animals | Rooms, corrals with adequate exits | Allow only trained individuals near dangerous or large animals; bite prevention | Impermeable gloves for certain tasks |
| Lifting animals, carrying heavy loads | Design ergonomic solutions (mechanical lifts, storage solutions that reduce need for lifting) | Training in injury prevention; housekeeping training and maintenance | Footwear selection | ||
| Slip, trip, and fall | Eliminate fall risks | Floor material selection | Control access to areas with slippery environment and provide appropriate signage | ||
| Noise | Eliminate noisy machines | Substitute less-noisy machines or processes | Noise shielding/barrier | Motivate/train regarding use of hearing protection; limit time in noisy areas | Hearing protection |
| Radiation | Eliminate need for on-site x-rays, other radiation | Substitute equipment with less radiation hazard | Appropriate radiologic housing facility | Training in radiation safety, sun exposure protection; restrict access to radiologic facilities | Use of sunscreen, protective clothing, and radiation shielding (lead gowns, gloves, etc.) |
| Chemical | |||||
| Anesthetic gases | Substitute less-toxic compounds | Adequate scavenging systems | Follow MSDS with chemical-specific guidelines | Gloves, respirators when indicated | |
| Disinfectants, cleaners, pesticides | Substitute safer chemicals | Adequate ventilation when cleaning; safe application systems | Safety policies to restrict use to trained individuals | Gloves, respirators when indicated | |
| Nitrogen dioxide, H2S, ammonia (farms) | Silage management, manure management | Safety policies regarding entry into silos, manure storage areas | Air respirators, other respirators as indicated | ||
| Psychosocial | |||||
| Stress of euthanasia, compassion fatigue, burnout; fear of trauma, isolation | Work with different species | Safety equipment, injury prevention as above | Support groups, coping skills training, animal handling skills training | ||
MSDS, Material Safety Data Sheet.
Biological Hazards
Allergens
As discussed in Chapter 7, many animal proteins are potential allergens in human beings. Although guinea pigs, mice, rats, and cats are common causes of allergy, virtually any species, including primates, larger domestic animals (such as horses and cattle), and reptiles can also pose an allergic risk to workers.7, 8 Exposure to insects such as roaches, flies, and mites as well as insect parts, shellfish (e.g., snow crabs, king crab, lobster, shrimp, scallops), and fish species (e.g., salmon, trout, pilchard, anchovy, hake) has also been associated with allergic reactions.9 Other animal-related sources of allergens in the workplace include molds and thermophilic bacteria that infect animal foods (including hay and prepared animal food) and cause asthma, rhinitis, dermatitis, and hypersensitivity pneumonitis.10
In addition to animal allergens, other allergen exposures for animal workers may include latex gloves, allergenic chemicals such as disinfecting agents (e.g., glutaraldehyde), other cleaning agents and detergents, and organic dusts (e.g., red cedar shavings used as animal bedding).
Not surprisingly, allergic reactions are a well-recognized health problem among animal workers.11 In some settings almost half of animal workers have been reported to develop allergy-related symptoms such as rhinitis, conjunctivitis, asthma, contact urticaria, and other types of allergic dermatitis.1, 4, 12, 13 Risk factors for developing allergic responses to antigens include the intensity and duration of exposure to specific antigens4, 13 and a history of atopy (allergic predisposition).14 Allergic exposures can pose a difficult problem for sensitized workers because even low levels of exposure to an allergen may provoke a response in a previously sensitized individual. In addition, personal protective equipment may not adequately protect them from further allergic reactions.
Zoonotic Pathogens
As described in Chapter 9, a large number zoonotic pathogens can pose a hazard to animal workers, who generally have increased exposures to zoonotic diseases compared with the general public. Many of these individual zoonotic diseases with occupational exposure potential are covered in Chapter 9. Selected pathogens of relevance to particular worker groups are described in the sections that follow. For example, occupational cases of Campylobacter and Chlamydophila psittaci infection have been documented among poultry workers15, 16 and reported human plague cases have been reported among veterinary staff attending to infected cats.17 With the increasing focus on emerging infectious diseases, it should be remembered that many such diseases appear first or with greatest intensity in the occupational setting. The first recognized (index) human case for the epidemic of severe acute respiratory syndrome (SARS) that began in China was a chef who had extensive exposure to wild game animals in his work.18 Nipah virus, another deadly emerging viral pathogen, first broke out among Malaysian pig farm workers.19 Human outbreaks of Ebola virus infection in Africa are believed to originate at least in part from exposures to nonhuman primates and other wildlife during bushmeat hunting and butchering.20 A strain of highly pathogenic avian influenza (HPAI) has caused fatal work-related infection in a veterinarian, and human cases of H5N1 HPAI remain strongly associated with working in animal markets, poultry rearing, slaughtering, defeathering, and preparing infected birds for consumption.21 Rift Valley fever, another emerging viral disease, often occurs in human beings as an occupational disease among herdsmen engaged in activities such as assisting with cattle birthing and caring for sick animals.22
Direct routes of exposure for zoonotic pathogens include a bite or scratch from an infected animal, exposure to infected fluids through splashes to the eye or mucous membranes, touching of contaminated surfaces, needlestick or other sharp instrument injuries, or inhalation of infectious particles in dusts. Vector-borne transmission can also occur in certain workplaces (see arthropod exposures later in this chapter).
In addition to animal-human transmission, some zoonotic diseases can be “reverse zoonoses,” potentially transmitted from human beings to animals in the occupational setting. Examples include tuberculosis, which may be transmitted by human beings to nonhuman primates,23 elephants,24 and dogs.25
Live Vaccines
Accidental autoinoculation of live vaccines for diseases with zoonotic potential has been reported to result in worker infections. An example is the vaccine for Brucella abortus strain RB51.26 A 1995 survey of veterinarians found that 23% of large animal veterinarian respondents reported accidental self-inoculation with live Brucella vaccine.27
Endotoxin and Organic Dusts
Endotoxin is a biological hazard consisting of lipopolysaccharide compounds from the cell walls of gram-negative bacteria that can grow in animal bedding or feed. When the bedding or feed is disturbed, dusts are generated that can have endotoxin concentrations of 3000 nanograms per meter cubed (ng/m3), in excess of a proposed guideline2 of 9 ng/m3. Adverse respiratory effects such as bronchitis and airway obstruction have been reported in workers who inhale such dusts, especially when working in confined areas with less than adequate ventilation.28 Organic dusts from moldy grain used for animal feed can cause organic dust toxic syndrome (ODTS), a self-limited disease with symptoms including fever, cough, myalgias, headache, and shortness of breath.2
Pathogenic Fungi
A hazard related to work around areas of bird or bat droppings is the exposure to potentially pathogenic fungi including Histoplasma, Cryptococcus, and Blastomyces. Histoplasma capsulatum is a fungus that exists in two forms: a mold form in the soil environment and a yeast form that develops when human beings or other animals inhale or ingest the spores. Although many infected human beings are asymptomatic, some may develop complications ranging from mild flulike illness to chronic lung and eye infections and pericarditis.29 Skin infection can also occur. Immunocompromised individuals are at increased risk of severe disease. The nutrients in bird or bat guano can encourage the growth of spores in the environment. Therefore areas of pigeon and other bird roosting where bird droppings accumulate may be more likely to have high levels of H. capsulatum spores that can lead to inhalation or ingestion by human beings. Poultry litter can also contain Histoplasma spores. Farmers, construction workers, forestry workers, and other workers exposed to disturbed soil or poultry guano can be at risk of infection, especially if individuals are immunocompromised. Unlike birds, bats appear to shed infectious Histoplasma in their droppings. Caves and other areas where bat guano accumulates have been associated with human cases of histoplasmosis.30 The National Institute for Occupational Safety and Health (NIOSH) has published guidelines for reduction of occupational risk of Histoplasma infection that also can be applied to the risk of other fungal pathogens such as Cryptococcus and Blastomyces. These guidelines include the use of respiratory protection, disposable protective clothing and shoe coverings, and gloves that avoid skin trauma to reduce the risk of skin infection. The types of respirators that should be worn during occupational activities with exposures to spore-contaminated dusts depend on intensity of exposure. In low-risk situations (e.g., site surveys of bird roosts), disposable, filtering facepiece respirators may be adequate, whereas extremely dusty work such as removing accumulated bird or bat manure from an enclosed area such as a barn or attic may require full-facepiece, powered air-purifying respirators.31
Cryptococcus is another genus of potentially pathogenic fungi found in soil. Like Histoplasma, high concentrations of Cryptococcus spores can be found in soil enriched by bird droppings. Cryptococcus neoformans is found worldwide and can cause significant infections, including meningitis, in immunocompromised individuals. However, C. neoformans has not been extensively associated with occupational or environmental exposures. In contrast, Cryptococcus gatii infection (a species formerly thought to be confined to the tropics) has been tied to environmental and occupational exposures to disturbed contaminated soil in both human beings and domestic animals (including cats, a ferret, and a llama) in North America. In these recent outbreaks, human C. gatii infection has involved both chronic pulmonary manifestations as well as meningitis.32
Another fungus associated with environmental exposures is Blastomyces, which can cause chronic lung disease in human beings and other animals as well as extrapulmonary manifestations. The typical human case of blastomycosis related to occupational or environmental exposure is a male who works or recreates outdoors where there is wildlife activity. A history of a pet dog with the disease helps support the diagnosis because dogs appear to act as sentinels for environmental exposure risk.33
Arthropod Exposures
Animal workers may be exposed to ticks, mites, and other arthropods that may be attached to animals or in the vicinity. Such exposures can lead to transmission of zoonotic pathogens as well as bites and allergic reactions. Grain mites are a cause of allergy among agricultural workers.
Chemical Hazards
Exposure to chemical hazards can occur in workers with animal contact, especially among laboratory animal research staff and veterinary workers. Anesthetic gases are a significant risk to veterinary personnel and are discussed below. Other chemicals include immobilizing agents, disinfectants, animal-related pesticides (see Chapter 8), rodenticides, and protocol-specific chemicals in animal research.34 These chemicals can cause a wide range of health effects from skin and mucous membrane irritation to neurological effects and adverse pregnancy outcomes (e.g., miscarriage from anesthetic exposures).35 A Materials Safety Data Sheet (MSDS) on the hazards, safe handling, and exposure management of specific chemicals should be available to all animal workers encountering chemicals in the workplace. Depending on the particular exposure, specific types of decontamination and acute medical care may be needed. In addition, inspection of the workplace should be considered in coordination with the industrial hygienist and other safety personnel.
Farm workers, especially those working in animal confinement facilities with large numbers of animals such as swine, may be exposed to pesticides as well as high levels of ammonia and hydrogen sulfide levels related to animal waste. These irritating chemical fumes can cause toxic chemical pneumonitis and bronchitis.10 Hydrogen sulfide, produced by decaying organic waste, is a mitochondrial toxin that can cause acute loss of consciousness, respiratory arrest, and death.36
Cattle silage can be a source of nitrogen dioxide toxicity causing “silo filler's disease,” an acute syndrome characterized by pulmonary edema, respiratory distress, and death in sufficiently high exposures.37
Physical Hazards
Common physical hazards faced by animal workers include bites and crush injuries from animals; acute and chronic musculoskeletal strain from handling animals and equipment; slip, trip, and fall injuries; and, in certain settings, exposure to noise, extremes of temperature, and radiation.38
Psychosocial Stressors
Although there are many psychosocial benefits of human-animal interaction (see Chapter 5), animal workers may face particular psychosocial stressors. These can include fear of attack and injury; fear of infectious disease; emotional reactions to performing euthanasia, necropsies, slaughtering, or other procedures; compassion fatigue39; and professional burnout.40
HAZARD CONTROLS
Once workplace hazards are identified, the goal is to reduce exposures to these hazards. Taking an occupational health approach to such hazards involves using a hierarchy of controls that range from most effective to least effective methods to reduce the health risks to workers. This hierarchy is listed in Table 12-2 . Many hazards can be eliminated at the source, or a less-dangerous substance or process can be substituted. Engineering controls include physical methods to reduce exposures such as improved ventilation and use of nonporous surfaces on counters that can be easily disinfected. Administrative and work practice controls involve job restrictions for susceptible persons, limiting individual worker exposure times in high-exposure areas, and preventive practices such as hand hygiene. Reliance on personal protective equipment such as gloves, gowns, and respirators is considered to be the least effective and often most cumbersome approach to hazard control.
TABLE 12-2.
Hierarchy of Controls for Workplace Hazards
| Control Strategy | Effectiveness |
|---|---|
| 1. Eliminate the hazard | Most effective |
| 2. Substitute for the hazard | |
| 3. Engineering controls | |
| 4. Administrative/work practice controls | |
| 5. Use of personal protective equipment (e.g., gloves, masks) | Least effective |
Table 12-1 shows examples of such controls for handling biological, chemical, physical, and psychosocial hazards in animal work. Obviously the most effective controls vary by the specific type of hazard, and the occupational health team must consider the most feasible type of control for each particular hazard. Although they may require a greater up-front investment, controls at the top of the hierarchy, such as elimination, substitution, or engineering controls, may be most cost effective at preventing work-related health problems. For example, eliminating a zoonotic disease (such as brucellosis) in an animal population through vaccination and other preventive veterinary care may be more cost effective over time than relying on personal protective equipment such as respirators and gloves for animal workers. Similarly, substituting a less-toxic cleaning agent (see Chapter 8) may be more cost effective in reducing health complaints of eye and throat irritation among exposed workers than the use of gloves and respirators.
OCCUPATIONAL MEDICINE SERVICES
Because not all health hazards in the workplace can be eliminated or completely controlled by the methods listed above, animal workers may require occupational medicine services to prevent and treat work-related illnesses and injuries. Such services may involve both human health care providers and other members of the occupational health team.
Preplacement Screening
Preplacement examination (or post–job offer evaluation) is a medical evaluation conducted to determine if a newly hired worker is able to safely perform the essential functions of the job with or without accommodation. Such examinations can present an ideal opportunity for preventive risk assessment and counseling as well as prophylactic vaccination. However, for many animal workers such examinations are not required by law and may not be provided because an employer believes they are not necessary. Even when animal workers do have such clearance examinations, the service may be provided by a personal physician or other health care provider who is not familiar with the health risks of animal work. As a result, there may be many missed opportunities for prevention.
The content of the preplacement examination can vary depending on the particular job type and set of exposure risks but often involves a screening medical history, physical examination, and diagnostic testing, if indicated, to identify important preexisting conditions that might place an individual at increased risk of injury or illness, including immunocompromising conditions41 or history of allergy. A history of previous animal contacts and whether animals are kept in the home may provide useful information. The use of standardized history and physical forms may assist in this process. Figure 12-2 shows an example of an animal worker questionnaire that might be appropriate for a worker in an animal care facility or a veterinary practice.
Figure 12-2.
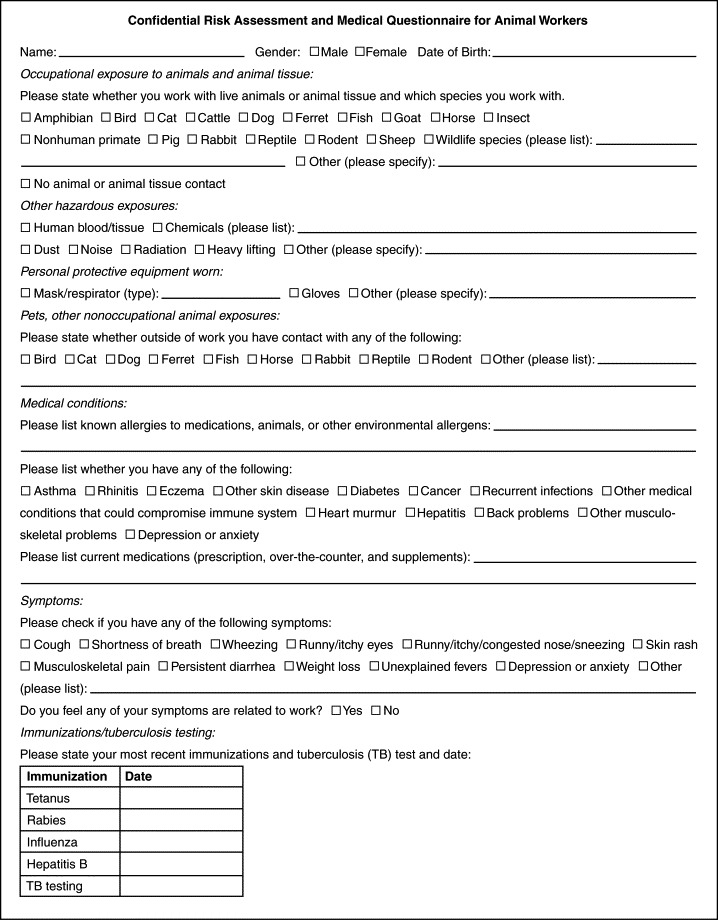
Sample medical questionnaire for animal workers.
If workers will be using respiratory protection involving N-95 respirators or other types of respirators, they should complete the Occupational Safety and Health Administration (OSHA) respirator questionnaire as part of the respirator medical clearance required under the OSHA Respirator Standard 1910.134 (available at http://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=STANDARDS&p_id=9783). If latex is used in the workplace, workers should be asked about any previous reactions to latex, including rash, hives, nasal or eye inflammation, breathing difficulties, or anaphylaxis.
In addition to the history and physical, other baseline testing may be indicated. Audiometry at baseline is required by OSHA if the worker will be exposed to noise at levels of 85 A-weighted decibels (dBA) or higher for an 8-hour time-weighted average. Testing of lung function (spirometry) is recommended for individuals with potential exposure to respiratory allergens, including veterinary workers and workers in animal facilities. Allergy testing is not usually performed routinely at baseline but may be warranted if the history suggests sensitization to particular allergens found in the work setting. In certain settings baseline serology or serum banking may be indicated to detect immunologic response to zoonotic pathogens.
Based on the findings of the preplacement examination, the medical provider can perform a risk assessment for the individual and decide whether the individual can safely do the job with or without accommodation. To do this, the medical provider may need to consult a veterinarian, biosafety professional, or other members of the occupational health team to learn more about specific risks of the job. For example, a person with valvular heart disease may need to be restricted from working in a research facility with pregnant sheep because of the risk of Q fever. A worker who developed allergy to mice or rats in a previous job may need to be restricted from future contact with such animals. In discussing disease risks with other professionals, it is important (although sometimes a challenge) to keep medical information about the worker confidential and prevent possible workplace discrimination because of a medical condition. If work restrictions are necessary, they can be indicated on a work status form that can be given to the employer to outline such restrictions without revealing confidential health information about the employee. In general, confidential health information on employees should not be shared with the employer, supervisor, or other management personnel by the human health clinician evaluating the worker.42
Vaccinations
A number of preventive vaccinations may be indicated for animal workers. Previous vaccination history should be assessed at the preplacement evaluation and the need for additional vaccination determined. As with other aspects of the preplacement risk assessment, consultation with a veterinarian may be advisable or clear instructions conveyed to the health care provider regarding necessary vaccinations. All animal workers should be up to date with respect to tetanus vaccination. Table 12-3 lists vaccines to consider for particular groups of workers. Rabies vaccination is indicated for a number of workers.43 Table 12-4 shows recent recommendations for which individuals should receive preexposure rabies vaccine.
TABLE 12-3.
Occupational Medicine Services for Animal Workers
| Category of Medical Service | Specific Medical Services Indicated | Types of Animal Workers Requiring Occupational Medicine Services |
|---|---|---|
| Preplacement screening |
|
All |
| Respirator clearance questionnaire, spirometry | Workers exposed to respiratory hazards, workers who will be using respirators | |
| Audiometry | Noise-exposed workers | |
| HIV and TB screening | Animal research and workers in contact with nonhuman primates | |
| Consider serum banking | Zoological, wildlife, or research workers; others with zoonotic exposures | |
| Vaccination | Rabies | See Table 12-4 |
| Tetanus (every 10 years) | All | |
| Annual influenza vaccine | All (especially poultry and swine workers) | |
| Anthrax | Laboratory workers routinely working with concentrations of anthrax or aerosol potential87 | |
| Q fever (consider)* | Laboratory workers, researchers working with pregnant sheep, slaughterhouse workers70 | |
| Hepatitis A and B, measles, polio | Workers in contact with chimpanzees and other nonhuman primates | |
| Training | Veterinary standard precautions, anesthetic safety, bite and injury prevention, OSHA training, safe chemical handling | All |
| Medical surveillance | Periodic questionnaire about allergy/respiratory symptoms | NIOSH recommendations in all animal workers with allergen exposures |
| Reassess zoonotic disease risk | All animal workers with change in medical status | |
| OSHA respirator questionnaire; spirometry; further evaluation in positive responses to questionnaire | Workers using respirators | |
| TB testing (skin test or interferon assay) | Animal workers with nonhuman primate and/or elephant contact (see Figure 12-2) | |
| Annual audiometry | Workers with noise exposures ≥85 dBA (8-hour average) | |
| Acute injury and illness management |
|
All |
| Herpes B exposure prophylactic treatment65 | Workers with exposure to nonhuman primates | |
| Confidential medical record management | Protect confidentiality of medical records | All |
HIV, Human immunodeficiency virus; TB, tuberculosis; OSHA, Occupational Safety and Health Administration; dBA, decibels (acoustic).
Not commercially available in the United States. Persons wishing to be vaccinated should first have a skin test to determine a history of previous exposure. Individuals who have previously been exposed to C. burnetii should not receive the vaccine because severe reactions, localized to the area of the injected vaccine, may occur.
TABLE 12-4.
Rabies Preexposure Prophylaxis Guide
| Risk Category | Nature of Risk | Typical Population | Preexposure Recommendations |
|---|---|---|---|
| Continuous | Virus present continuously, often in high concentrations; specific exposures likely to go unrecognized; bite, nonbite, or aerosol exposure | Rabies research laboratory workers; rabies biologics production workers | Primary course*; serologic testing every 6 months; booster vaccination if antibody titer is below acceptable level |
| Frequent | Exposure usually episodic and with source recognized, but exposure also may be unrecognized; bite, nonbite, or aerosol exposure | Rabies diagnostic lab workers, spelunkers, veterinarians and staff, animal control and wildlife workers in rabies-endemic areas; all persons who frequently handle bats | Primary course; serologic testing every 2 years; booster vaccination if antibody titer is below acceptable level |
| Infrequent | Exposure nearly always episodic with source recognized; bite or nonbite exposure | Veterinarians and terrestrial animal control workers in areas where rabies is uncommon to rare; veterinary students; travelers visiting areas where rabies is enzootic and immediate access to appropriate medical care, including biologics, is limited | Primary course; no serologic testing or booster vaccination |
| Rare (population at large) | Exposure always episodic with source recognized; bite or nonbite exposure | U.S. population at large, including persons in rabies-epizootic areas | No vaccination necessary |
Primary vaccination: three 1.0-mL injections of HDCV or PCEC vaccine should be administered intramuscularly (deltoid area)–one injection per day on days 0, 7, and 21 or 28.
From Manning SE et al, Centers for Disease Control and Prevention: Human rabies prevention–United States, 2008: recommendations of the Advisory Committee on Immunization Practices, MMWR Recomm Rep 57(RR-3):1-28, 2008.
Training
Training at the time of job entry is recommended by the National Association of Public Health Veterinarians (NAPHV) for workers in veterinary facilities41 and is relevant for other animal workers as well. Aspects of such training include education about zoonotic disease risks, infection control practices, use of personal protective equipment, safe chemical handling techniques, and injury prevention, with emphasis on proper animal handling, restraints, and recognition of behavioral cues in animals. Such training should be provided by an individual familiar with the risks of a particular workplace and the safety policies in place, such as a safety officer. Training should be documented. Follow-up training in health and safety can take place on a regular basis with animal workers to identify and mitigate hazards, address institutional occupational health policies (including record keeping), address personal hygiene, provide points of contact for more information or for when to seek medical attention for work-related problems, review unit inspection standards, and evaluate future training needs.
Medical Surveillance
Depending on the degree of occupational risk, animal workers should receive periodic evaluations to detect evidence of work-related disease, reassess risk factors for occupational illness and injury, and ensure that vaccinations are current. Table 12-1 suggests medical surveillance that may be appropriate for different types of animal workers.
Questionnaires should ask about new health problems that have developed since the last examination, including symptoms of allergy or infection that could indicate increased risk of disease or the occurrence of work-related disease or injury. A key aspect of such history is whether the symptoms show a temporal relation with work exposures. Box 12-2 shows characteristic symptom patterns suggesting work-related occupational asthma. Similar temporal relations may occur with other occupational diseases.
BOX 12-2. Pattern of Symptoms of Work-Related Asthma.
-
•
Symptoms of asthma develop after a worker starts a new job or after new materials are introduced on a job (a substantial period of time may elapse between initial exposure and development of symptoms).
-
•
Symptoms develop within minutes of specific activities or exposures at work.
-
•
Delayed symptoms occur several hours after exposure, during the evenings of workdays.
-
•
Symptoms occur less frequently or not at all on days away from work and on vacations.
-
•
Symptoms occur more frequently on returning to work.
From National Institute for Occupational Safety and Health (NIOSH): NIOSH alert: preventing asthma in animal handlers, DHHS (NIOSH) Publication No. 97-116.http://www.cdc.gov/Niosh/animalrt.html.
Based on the results of screening questions, further testing may be indicated, such as serial peak flow diaries, spirometry, and methacholine testing of lung function in a worker reporting shortness of breath. Another example of periodic medical surveillance testing is annual audiometry, which is required by OSHA for workers exposed to noise and enrolled in hearing conservation programs.
Management of Acute Injuries, Exposures, and Illnesses
When an animal worker seeks medical attention for an acute illness or injury that may be work related, the health care provider should be familiar with the worker's occupational hazards. As previously stated, many medical providers in emergency departments or clinics may not be aware of the zoonotic or other disease risks faced by animal workers. It may therefore be advisable for workers with acute work-related injuries or illnesses to carry a card listing relevant zoonotic disease exposures and other work hazards and be able to show the card to the health care provider. An example of such a card is shown in Figure 12-3 . This type of card should be customized to the specific work setting.
Figure 12-3.

Example of hazard card for animal workers seeking medical care for acute illness or exposure (to be customized to particular work setting).
If an animal worker has an acute exposure, illness, or injury the work supervisor should document and report the incident. This documentation should include the date, time, location; persons injured or exposed; other persons present; description of the incident; the species, breed, and health status (vaccination history, clinical signs, diagnostic testing) of any involved animals; contact with public health and health care providers; and follow-up plans.41 If possible, pertinent documentation of the incident should be made available to the treating medical provider. Because work-related injuries and illnesses must be reported on the employer's OSHA 300 Log, attending clinicians will need to provide a medical opinion and rationale on the work-relatedness of the injury, illness, or exposure.44
A key part of the evaluation of any work-related illness or injury is determining whether it represents a sentinel health event indicating a problem with existing hazard controls and potentially representing an index case in terms of other workers and possibly animals being at risk. This may require communication between the health care provider and the veterinarian and/or other members of the occupational health team (see Figure 12-1).
After an episode of acute injury or illness, or because of results of a periodic surveillance evaluation, the employee may not be able to resume full duties immediately. In this case the medical provider should specify the necessary job restrictions that would allow the worker to safely return to work and how long those restrictions are expected to be required. Again, making appropriate recommendations may require a team approach involving the veterinarian and other professionals. As with preplacement evaluations, it is important that the worker's privacy and the confidentiality of medical information be respected during this process.
Management of Confidential Medical Records and Information
Medical evaluations of workers must uphold standards of privacy and confidentiality in the provision of care and in record keeping. In agreement with the Health Information Portability and Accountability Act (HIPAA), the American College of Occupational and Environmental Medicine has published a position paper in support of confidentiality of medical information in the workplace.45 Results of baseline and periodic questionnaires and physical examinations (including, but not limited to, information about immunocompromised conditions) represent medical information that should be treated with the same confidentiality as information in a hospital and not shared with the employer. Such information should be kept in a secure chart in a medical office and not placed in an employee's personnel file in the workplace.
Table 12-3 summarizes occupational medical services for different groups of animal workers.
OCCUPATIONAL HEALTH IN SPECIFIC SETTINGS
Veterinary Personnel
As a group, veterinarians and their staff are at increased risk for work-related injuries and illnesses. A study of 10,000 veterinary practices in Europe found that the rate of work accidents and occupational disease was almost three times as great as that of general medical practitioners and their staff, and the rate of severe accidents resulting in lost work time was nine times greater. The most common occupational diseases reported were skin disorders (39%), followed by allergic respiratory diseases (31%) and infectious diseases (19%).46 In the United States federal law requires veterinary practices to implement a workplace plan to comply with OSHA Hazard Communication Standards (http://www.avma.org/issues/policy/workplace_hazards.asp). It also appears that veterinarians may be held liable for harm if their employees develop a work-related illness such as a zoonotic infection.47 It is not clear how many workers in veterinary practices receive occupational medicine services from human health care providers or have access to members of the occupational health team, such as industrial hygienists or infection control specialists. Many veterinary offices are located in rural or other areas where shortages of occupational medicine providers exist.48 The practice director, who is often a veterinarian, or another staff member may have to perform a number of functions such as identifying hazards and designing control strategies. The National Association of State Public Health Veterinarians (NASPHV) has published a compendium of veterinary standard precautions that provides useful practice guidelines as well as a model infection control plan (Figure 12-4 ).41 The veterinarian may need to educate local medical providers to ensure adequate and confidential preplacement screening, medical surveillance, and acute injury/illness follow-up of veterinary care workers. Having a designated medical provider as well as a designated emergency medical care facility that is aware of the special exposures of the veterinary workers can help ensure improved preventive and acute care of exposure-related health problems.
Figure 12-4.




NASPHV model infection control plan for veterinary practices, 2008.
Rights were not granted to include this figure in electronic media. Please refer to the printed book.
(Adapted from National Association of State Public Health Veterinarians: NASPHV compendia. http://www.nasphv.org/documentsCompendia.html.
© 2010
Allergens
A survey of California veterinarians found that 40% reported animal-related allergic symptoms, especially to cats and dogs.49 Allergens identified as hazards in veterinary practice include animal hair and dander, feathers, latex, mites, organic dust, and amniotic fluid. Fortunately, a study of skin allergy in veterinarians found that most sensitized individuals were allergic to only one species of animal.50
Hypersensitivity pneumonitis has been reported in veterinarians from exposure to antigens in animal feeds.46
Latex allergy is also a risk among veterinary personnel who use latex gloves and other latex equipment.
Measures to control these hazards in veterinary practices include frequent cleaning of facilities and adequate ventilation. Personal protective devices such as gloves and respirators can reduce allergen exposure. Box 12-3 shows the recommendations for animal handler allergen control published by NIOSH that target veterinary and research animal workers.
BOX 12-3. Preventing Asthma In Animal Handlers.
WARNING! Exposure to animals or animal products in the workplace can cause asthma and allergies. Animal handlers should take steps to protect themselves from exposure to animals and animal products.
-
•
Perform animal manipulations within ventilated hoods or safety cabinets when possible.
-
•
Avoid wearing street clothes while working with animals.
-
•
Leave work clothes at the workplace to avoid potential exposure problems for family members.
-
•
Keep cages and animal areas clean.
-
•
Reduce skin contact with animal products such as dander, serum, and urine by using gloves, lab coats, and approved particulate respirators with face shields.
-
•
Employers of animal handlers should take steps to protect workers from exposure to animals and animal products.
-
•Modify ventilation and filtration systems:
-
•Increase the ventilation rate and humidity in the animal housing areas.
-
•Ventilate animal housing and handling areas separately from the rest of the facility.
-
•Direct airflow away from workers and toward the backs of the animal cages.
-
•Install ventilated animal cage racks or filter-top animal cages.
-
•
-
•
Decrease animal density (number of animals per cubic meter of room volume).
-
•
Keep cages and animal areas clean.
-
•
Use absorbent pads for bedding. If these are not available, use corncob bedding instead of sawdust bedding.
-
•
Use an animal species or sex that is known to be less allergenic than others.
-
•
Provide protective equipment for animal handlers: gloves, lab coats, and approved particulate respirators with face shields.
-
•
Provide training to educate workers about animal allergies and steps for risk reduction.
-
•
Provide health monitoring and appropriate counseling and medical follow-up for workers who have become sensitized or have developed allergy symptoms.
From National Institute for Occupational Safety and Health (NIOSH): NIOSH alert: preventing asthma in animal handlers, DHHS (NIOSH) Publication No. 97-116. http://www.cdc.gov/Niosh/animalrt.html.
However, even with these measures, sensitized individuals may have difficulty working around animals to which they are allergic. Job modification may be necessary; there may be areas of the building with a lower allergy load that a sensitized individual could tolerate. Allergy desensitization should be considered as part of the management of some allergic conditions.
Zoonoses
Many different zoonotic infections, including fatal cases, have been reported in veterinarians.41 In a European study of work-related claims by veterinary workers, the most frequent infections were ringworm, brucellosis, Lyme disease, and psittacosis.46 A survey of American veterinarians found that the occupational infections of current greatest concern to small-animal veterinarians were ringworm, gastrointestinal bacteria, gastrointestinal parasites, leptospirosis, rabies, toxoplasmosis, and unknown or emerging pathogens. Large-animal veterinarians were concerned about ringworm, gastrointestinal bacteria, leptospirosis, brucellosis, gastrointestinal parasites, and rabies. Despite these concerns, most veterinarians responding to the survey reported low rates of personal protective equipment use and other protective behaviors currently recommended to protect against zoonotic disease transmission.51
Veterinarians and their staff have been identified as a group at increased risk for many other zoonotic infections, including Q fever, salmonellosis, methicillin-resistant Staphylococcus aureus, avian influenza,51 cat-associated plague, animal bite infections including pasteurellosis, other bacterial infections, and cat-associated sporotrichosis (see Chapter 10).
The NASPHV Veterinary Standard Precautions for Zoonotic Disease Prevention in Veterinary Personnel includes a model infection control plan for veterinary offices.41 Figure 12-4 shows this model plan.
This NASPHV document recommends engineering controls such as single-purpose isolation rooms for sick animals; separate rooms for patient care and employee breaks; designated sharps containers; the use of nonporous, easily cleaned surface materials in areas where animals are housed, examined, or treated; and sealing up of rodent entry portals. Recommended work practice controls include training new employees in practices such as hand hygiene before and after each patient encounter and after contact with body fluids, secretions, or excretions as well as after eating, drinking, smoking, using lavatories, and cleaning animal areas. Additional work practices include bite prevention and avoidance of needlesticks by not recapping needles. Bite prevention could include physical or chemical restraints, muzzles, and bite-resistant gloves. Personal protective equipment recommendations include gloves or sleeves and facial protection with a mask or goggles when splashes or sprays are expected. An N-95 respirator should be worn when evaluating abortions in small ruminants, poultry deaths, sick psittacine birds, and other situations with the risk of aerosolized pathogens.41 The NASPHV document also recommends that immunocompromised individuals and pregnant workers be counseled about their increased risk of zoonotic disease, especially when working with high-risk animals such as young animals and animals that are parturient, unvaccinated, stray or feral, housed in shelters or crowded conditions, fed raw meat diets, or with parasites; wildlife; reptiles and amphibians; and exotic or nonnative species.41 Such counseling should ideally be done by a health care professional who is aware of the zoonotic disease risks faced by the worker. For this reason the NASPHV document recommends that all workers inform their health care providers of their work activities, but additional direct communication between a health care provider and a veterinarian about disease risks may be advisable. However, as previously mentioned, such communication needs to respect patient privacy and confidentiality of medical information (see Chapter 2).
Chemical Hazards
Chemical hazards in veterinary practices include disinfectant chemicals, pesticides (see Chapter 8), and anesthetic gases. These chemicals are capable of allergic, irritant, and other toxic effects. Chemical irritant effects such as irritant contact dermatitis and eye irritation have been associated with the use of chemical disinfectants.52 Table 12-5 lists disinfectant chemicals commonly used in veterinary practices. As can be seen among the list of disadvantages, a number of these chemicals are highly irritating to skin, eyes, and mucous membranes. If a particular disinfectant chemical is causing adverse effects in workers, substitution should be considered.
TABLE 12-5.
Disinfectants Used in Veterinary Practices
| Alcohols | Aldehydes | Biguanides | Halogens: Hypochlorites | Halogens: Iodine Compounds | Oxidizing Agents | Phenols | QACs | |
|---|---|---|---|---|---|---|---|---|
| Sample trade names |
|
|
|
Bleach |
|
|
|
|
| Mechanism of action | Precipitates proteins; denatures lipids | Denatures proteins; alkylates nucleic acids | Alters membrane permeability | Denatures proteins | Denatures proteins | Denature proteins and lipids | Denatures proteins; alters cell wall permeability | Denatures proteins; binds phospholipids of cell membrane |
| Advantages | Fast acting; leaves no residue | Broad spectrum | Broad spectrum | Broad spectrum; short contact time; inexpensive | Stable in storage; relatively safe | Broad spectrum | Good efficacy with organic material; noncorrosive; stable in storage | Stable in storage; nonirritating to skin; effective at high temperatures and high pH (9 to 10) |
| Disadvantages | Rapid evaporation, flammable | Carcinogenic mucous membrane and tissue irritation; only use in well-ventilated areas | Only functions in limited pH range (5 to 7); toxic to fish (environmental concern) | Inactivated by sunlight; requires frequent application; corrodes metals; mucous membrane and tissue irritation | Inactivated by QACs; requires frequent application; corrosive; stains clothes and treated surfaces | Damaging to some metals | Can cause skin and eye irritation | |
| Precautions | Flammable | Carcinogenic | Never mix with acids; toxic chlorine gas will be released | May be toxic to animals, especially cats and pigs | ||||
| Vegetative bacteria | Effective | Effective | Effective | Effective | Effective | Effective | Effective | Yes, gram-positive; limited, gram-negative |
| Mycobacteria | Effective | Effective | Variable | Effective | Limited | Effective | Variable | Variable |
| Enveloped viruses | Effective | Effective | Limited | Effective | Effective | Effective | Effective | Variable |
| Nonenveloped viruses | Variable | Effective | Limited | Effective | Limited | Effective | Variable | Not effective |
| Spores | Not effective | Effective | Not effective | Variable | Limited | Variable | Not effective | Not effective |
| Fungi | Effective | Effective | Limited | Effective | Effective | Variable | Variable | Variable |
| Efficacy with organic matter | Reduced | Reduced | ? | Rapidly reduced | Rapidly reduced | Variable | Effective | Inactivated |
| Efficacy with hard water | ? | Reduced | ? | Effective | ? | ? | Effective | Inactivated |
| Efficacy with soap/detergents | ? | Reduced | Inactivated | Inactivated | Effective | ? | Effective | Inactivated |
The use of trade names does not in any way signify endorsement of a particular product.
For additional product names, please consult the most recent Compendium of Veterinary Products.
?, Information not available. QACs, quaternary ammonium compounds.
Adapted from Linton AH, Hugo WB, Russel AD: Disinfection in veterinary and farm practice, Oxford, UK, 1987, Blackwell Scientific; Quinn PJ, Markey BK: Disinfection and disease prevention in veterinary medicine. In Block SS, ed: Disinfection, sterilization and preservation, ed 5, Philadelphia, Lippincott, 2001, Williams & Wilkins.
Approximately 50,000 veterinary workers in the United States risk potential exposure to anesthetic agents, including nitrous oxide and halogenated agents, mostly through significant inhalation and accidental injections in veterinary operating rooms.53, 54 Many of these workers are women of childbearing age. Adverse reproductive outcomes, such as spontaneous abortion, have also been reported among workers exposed to these anesthetic agents.54 Control of anesthetic hazards involves ensuring 100% fresh air and 100% exhausted air for dilution of waste gases and odors in animal rooms, filtering of supplied air prior to recirculation, and institution of a scavenging system for waste anesthetic gases and vapors. This scavenging system should be checked periodically to ensure it is working properly. Air levels of anesthetic gases can also be monitored periodically.55
Physical Hazards
Physical hazards in veterinary practices include bites and crush injuries from animals; lifting hazards related to equipment and patients; and slip, trip, and fall injuries. A survey of 2800 Australian veterinarians found that more than half had sustained a significant work injury.56 Animals have been reported to be the most common cause of occupational accidental injuries, with cats and dogs causing the most accident-related injuries in small-animal practices and horses and cows causing the most injuries in large-animal practices. Large animal accidents were more likely to cause broken bones.46 Some of the major causes of accidents involving animals are dangerous animal behaviors, such as panic, male dominance aggression, fear aggression, and maternal aggression. Control of these physical hazards includes bite prevention, proper animal handling and restraint, training animals to voluntarily cooperate with veterinary procedures,57 and inadequate barriers or animal handling facilities to protect workers.
Repetitive trauma from carrying and handling animals and cages as well as acute trauma from lifting and carrying can result in musculoskeletal injuries such as acute and chronic low back injury, carpal tunnel syndrome, and tendonitis.
Barking dogs, other noisy animals, and noisy machinery can cause significant noise exposure to animal workers. Veterinary staff can be exposed to significant noise, especially during the cleaning of cages with power washers. Noise levels above 85 dBA over an 8-hour period require inclusion of workers in a hearing conservation program that complies with the OSHA standard on occupational noise exposure.58 If a person has to shout to converse with another person at arm's length, the noise is likely to exceed 85 dBA.
Radiation is another physical hazard for staff in veterinary practices where radiographs are taken. Although evidence of adverse effects in veterinary staff from radiation exposure is limited, staff performing radiography should be monitored for radiation exposure.
Psychosocial Stressors
Psychosocial hazards of veterinary work include the stress of euthanizing animals, compassion fatigue, and professional burnout.39 Increased rates of suicide have been reported for veterinarians.59 There is little published evidence of successful interventions to reduce psychosocial stressors in veterinary practice, but strategies used in other occupational groups include job rotation and increased time off, coping skills training, support groups, and stress-reduction techniques.60
Occupational Medicine Services for Veterinary Personnel
As previously described, human health care providers who care for workers in a veterinary facility may not be familiar with the particular occupational health risks faced by such workers. Such practitioners may need to be provided with information about the disease risks and the preventive services required. Table 12-3 outlines some suggested occupational services for veterinary staff, including preplacement evaluation, vaccination, and management of acute injuries and illnesses.
Preplacement Screening
Because all veterinary workers encounter the risk of allergic reactions, preplacement examination should focus on history of skin, respiratory, or other allergies and any history of asthma or other underlying respiratory conditions as well as medical conditions associated with immunocompromised status. The OSHA Respirator Medical Evaluation questionnaire previously mentioned should be part of this baseline health history for any worker who will be using respiratory protection.61
Along with a thorough physical examination, baseline testing can include spirometry for anyone with allergen exposures. Even nonclinical personnel such as office staff could be exposed to allergens in waiting rooms or other parts of the facility.
Baseline vaccination should include a rabies preexposure series if not previously vaccinated against rabies (see Table 12-4). All veterinary staff should have a current tetanus vaccination and be encouraged to have an annual influenza vaccination. If the veterinary practice cares for pregnant sheep and goats, baseline titers for the etiologic agent of Q fever (Coxiella burnetii) should be considered. Other components of the preplacement evaluation can be tailored depending on the specific type of veterinary practice and the expected hazards.
Medical Surveillance
After a baseline medical evaluation, there are few guidelines for periodic examination of veterinary personnel by a medical provider. However, NIOSH recommends that veterinary workers receive periodic monitoring for the development of allergy and asthma. Such monitoring could be accomplished with a screening questionnaire (see Figure 12-2) that could also assess any reported infectious disease symptoms or diagnoses that could be work related (such as febrile illnesses, diarrhea, and/or skin infections) as well as newly developed medical conditions that could affect risk of zoonotic disease. If workers use respirators, repeat medical evaluations may be required under the OSHA Respiratory Protection standard if a change occurs in workplace conditions. NASPHV also recommends that veterinary personnel who have a change in their health status, such as pregnancy, should discuss their work exposures with their medical providers. They should also see their medical providers periodically for follow-up rabies vaccine boosters. Workers enrolled in a hearing conservation program because of excessive noise exposures require annual audiometry.
Acute Injury, Illness, or Exposure Evaluation and Follow-up
As with other animal workers, it is ideal that the health care provider treating veterinary workers for acute work-related injuries and illnesses be familiar with the hazards in the workplace. Medical providers providing such care should take a careful history of occupational exposures. Common acute injuries in veterinary personnel are animal bites (see Chapter 10). In such situations use of a zoonotic disease risk card (see Figure 12-3) may help guide the medical care provider to adequately consider zoonotic disease risks. Care of animal bites in veterinary workers involves a review of rabies risk from the bite and rabies vaccination status (see Chapter 9), as well as consideration of antibiotic treatment.
Any acute injury or illness in a veterinary worker can be considered a sentinel event indicating a hazard in the workplace that has not been adequately controlled. Therefore communication between the medical care provider and the veterinarian or other members of the occupational health team can help turn an acute illness or injury event into an opportunity to identify and reduce workplace hazards. In addition, the medical care provider will need to consider whether and when the worker can safely return to work and whether job modification or restriction is necessary. Again, this may require communication between the medical provider and a work supervisor or veterinarian. Individuals with suspected allergy should be evaluated and may need to be restricted from exposure to the animal to which they are sensitized (see Chapter 7). Individuals with musculoskeletal injuries may need temporary job modification while they recover. The possibility of posttraumatic stress should be considered in all employees returning to work after an acute work-related injury or illness.
Workers in Animal Research Facilities
Because many animal research facilities have affiliation with larger institutions, there is often a designated industrial hygienist and/or infection control specialist to help design and implement preventive workplace hazard controls. There is also often a designated medical care provider for the employees working in such facilities and a formal occupational health and safety program. In 1997 the Committee on Occupational Safety and Health in Research Animal Facilities, Institute of Laboratory Animal Resources, published Occupational Health and Safety in the Care and Use of Research Animals, which outlines guidelines for occupational health programs for research animal workers.62
Allergens
As with veterinary workers, allergy can be a significant problem in workers in research animal facilities. Allergy to rodents is common, resulting in the spectrum of allergic rhinitis, dermatitis, and asthma. Rodent allergy may be species specific; individuals sensitized to mice may be able to work safely with rats.
Control of allergens in animal facilities can involve engineering controls including adequate fresh air ventilation, filtering of any recycled air, and airflow of ventilation to blow air to the back of cages from the aisles to reduce worker exposures (see Box 12-3).63 Control by substitution may be feasible in some situations because male rats are more allergenic than female rats, and species such as rabbits are less allergenic than rats.1
Zoonoses
Several zoonoses are of particular concern to animal facility workers who work with nonhuman primates and rodents.64 Some can result in death. Therefore occupational exposures are considered medical emergencies. Unlike veterinary hospitals where elimination of zoonotic hazards is not possible, the control of many zoonotic diseases in animal facilities often involves control at the source through screening and eliminating disease in the animal colony. Separation of species prevents interspecies transmission, and signage helps increase awareness of risks among employees. Use of instruments and equipment with safety features such as retractable needles can help prevent bloodborne pathogen exposures.
Herpes B
Cercopithecine herpesvirus 1 infection, herpes B, is endemic in monkeys of the genus Macaca. This group of Asiatic monkeys includes rhesus macaques, pig-tailed macaques, and cynomolgus monkeys. Human beings who work with these monkeys can be infected by bites, scratches, needlesticks, and mucocutaneous exposure.65 In monkeys herpes B can be subclinical or cause lesions on the oral mucosa. In human beings herpes B can result in fatal encephalomyelitis. Although rare, death has been reported in up to 80% of cases. Workers dealing with these nonhuman primates must be informed of the risk of herpes B infection and receive training in proper use of appropriate personal protective equipment, including gowns, gloves, masks, and face shields and the maintenance of a safe workplace. They should seek medical care immediately if an exposure occurs because early prophylaxis with antiviral agents has resulted in favorable outcomes.66 The Centers for Disease Control and Prevention (CDC) has developed guidelines for assessment and medical management of monkey scratches and bites, wound contaminations, cage scratches, and other potential exposures.67
Simian Retroviruses
A number of simian retroviruses, including simian immunodeficiency virus and simian foamy virus, are found in a variety of nonhuman primates. Cases of transmission of these viruses to laboratory workers with nonhuman primate exposure have been reported. Prevention is similar to that for herpes B infection.68
Measles
Measles (rubeola), a paramyxovirus infection, is primarily a disease of human beings. The primary concern for laboratory animal workers is therefore reverse zoonosis (anthropozoonosis) when working with nonhuman primates because measles can cause lethal infection in these animals. Outbreaks of measles in captive nonhuman primates usually originate from an infectious human animal handler.69 Therefore animal workers with contact with nonhuman primates must have documented measles vaccination and receive booster vaccinations if necessary.
Viral Hepatitis
Hepatitis A, B, and C are primarily viral diseases of human beings. However, chimpanzees and other nonhuman primates have been experimentally infected.70 Therefore there is risk of reverse zoonosis. Workers in animal facilities who have direct contact with nonhuman primates should be immunized against hepatitis A and B,64 have baseline serology for protective hepatitis B antibodies (HbSAb), and consider having baseline serology for hepatitis C.
Tuberculosis
Nonhuman primates are susceptible to infection with Mycobacterium tuberculosis (TB) and can transmit the disease to human beings by the respiratory route. Likewise, human beings infected with TB can potentially infect nonhuman primates. All animal workers with nonhuman primate contact should have skin testing for TB at baseline and annually. New employees who have not had a TB skin test in the previous 5 years should be tested with a two-step technique (retesting after 1 week if the first test is negative) to detect boosted immunity from previous infection. Alternative testing methods include an assay for interferon specific to TB (see Chapter 9).71 Workers with positive TB tests should be evaluated medically. Such evaluation may include a chest radiograph to exclude active disease and a determination of the need for treatment with antituberculous medication.72
Rat-Bite Fever (Streptobacillosis)
Rat-bite fever is caused by infection with the bacterium Actinobacillus muris (formerly Streptobacillus moniliformis), usually as a result of a rat bite or contact with rat saliva or urine. The incubation period is between 3 and 10 days. Symptoms include the acute onset of fever, headache, and muscle pain, followed by the development of a maculopapular rash on the extremities over the next several days. In untreated cases complications can include endocarditis, parotitis, and abscesses.
Doxycycline or penicillin can be used as a prophylactic treatment after a rat bite. Cases of infection are treated with penicillin or tetracyclines (see Chapter 10).70
Lymphocytic Choriomeningitis Virus
Lymphocytic choriomeningitis virus (LCMV) is an arenavirus infection found especially in mice but also hamsters (see Chapter 9). Infected animals shed the virus in urine, saliva, and feces. Nude mice, used in some animal research laboratories, appear to shed increased amounts of LCMV.70 Transmission to human beings can involve contact of secretions with broken skin or oral or respiratory contact with dust or contaminated food. Handling contaminated surfaces and objects is considered a risk factor for infection.70 Infection in human beings can range from mild flulike symptoms to severe meningoencephalitis. Diagnosis involves viral cultures and serology. Cerebrospinal fluid can show lymphocytosis and decreased glucose level. The disease is usually self-limiting in immunocompetent individuals. Immunocompromised individuals are at increased risk of severe disease, sometimes with hemorrhagic complications and fatal outcomes. There is no specific treatment. Control measures include screening of laboratory animals for infection (see Chapter 9).
Q Fever
Laboratory animal personnel engaged in research with pregnant sheep and goats are at risk for infection with Q fever (see Chapter 9). High-risk individuals include immunocompromised individuals and persons with valvular heart disease.
Human Immunodeficiency Virus
Another human disease with potential to be a reverse zoonosis in nonhuman primates is human immunodeficiency virus (HIV), and some research facilities using nonhuman primates have adopted policies requiring anonymous periodic HIV testing be part of the job requirement. These HIV-related policies should include outlining the steps undertaken to safeguard each individual worker's privacy.
Chemical Hazards
Chemical exposures in laboratory animal facilities include disinfectants and anesthetics, as previously mentioned. Protocol-specific chemicals such as medications and toxins used in research can pose additional risks from a wide variety of chemicals. Eyewash stations and showers may be necessary for immediate decontamination by some agents.
Control of anesthetic gases and disinfectant chemical risks is similar to that for veterinary personnel.
Physical Hazards
Physical hazards for workers in animal care facilities are similar to those of veterinary workers and include ergonomic risks for musculoskeletal injury, noise, and radiation. Sources of radiation exposure may include both diagnostic and protocol-related radiation.73
Psychosocial Stressors
Work-related stress, anxiety, uneasiness, and depression have been reported in laboratory animal handlers. Particular psychosocial stressors include developing strong attachments to laboratory animals, having strong sentiments about “sacrificing” the animals, having friends and acquaintances who are critical of animal experimentation, and having doubts about the clinical value of animal research.74
Occupational Medicine Services for Animal Research Facility Workers
As previously mentioned, many animal research facilities have designated medical providers for both preventive and acute care services.
Preplacement Screening
Preplacement evaluations are similar to those for veterinary personnel. Particular work restrictions to consider based on the preplacement evaluation include the risk of previously sensitized persons working with animal allergens, the increased risk of immunocompromised persons working with rodents possibly infected with LCMV as well as other zoonotic risks, and risks to women of childbearing age from working with pregnant sheep and goats (Q fever). Baseline testing often includes spirometry, serology to document immunity, and HIV and TB skin testing for primate workers.
Vaccination services include ensuring that primate workers are current with measles, hepatitis B, hepatitis A, and polio immunizations. If wild stock animals that could carry rabies (such as stray dogs) are used in the facility, rabies vaccine should be considered for workers exposed to such animals.75
Medical Surveillance
Many research animal workers are enrolled in periodic medical surveillance on a yearly basis. Periodic screening may include a questionnaire that inquires about allergic and infectious symptoms. For primate workers, HIV and TB testing is often repeated on a regular (every 6 months or annual) basis.
Acute Injury, Exposure, and Illness Evaluation and Follow-up
Special issues in the acute care of animal care workers include management of exposures to nonhuman primates and the need for possible herpes B prophylaxis. Workers with rodent exposures should ensure that acute febrile episodes are evaluated by medical providers for the possibility of rat-bite fever and LCMV. As with veterinary workers, all acute injuries and illnesses should be considered possible sentinel health events with implications for the health of coworkers as well as the laboratory animals.
Issues regarding job modifications and restrictions after acute injuries and illnesses are similar to those of veterinary personnel.
Zoo and Aquarium Workers
Although zoo and aquarium employees share many of the same occupational health issues as veterinary and animal research workers, there are particular challenges for occupational health programs targeting these workers. Depending on the zoo, the diversity of species may far exceed that encountered by most other animal workers. Workers are employed in only one area of the zoo or aquarium, and therefore their occupational health needs may differ widely. Although the animals in a particular collection are likely captive bred, some have originated in the wild, where potential for zoonotic infections could be greater. Many zoos and aquariums are also open to the outdoor environment, allowing contact between wild animals and the captive specimens, with the possibility of disease introduction. For example, outbreaks of highly pathogenic animal influenza (HPAI) have been reported in captive birds in zoos after contact with wild birds. Cases of avian influenza have also occurred in captive felids, presumably as a result of feeding on infected poultry carcasses. Both of these introductions posed infectious risks to zoo workers. For these reasons, zoo workers (as well as zoo animals) may serve as sentinels of emerging infectious disease threats. For example, primate workers in zoos have been found to have evidence of possible infection with simian viruses considered to have potential for emergence.76 A special issue with zoo and aquarium workers is the significant number of volunteers working in many facilities who may not receive medical screening or prophylactic vaccinations.
Surveys of zoos have reported high rates of occupational injury and illness among zoo veterinarians, with more than 60% reporting significant animal-related injury, more than 30% reporting animal allergies, and more than 30% reporting zoonotic infections. Formalin exposures and insect allergies have also been reported as significant concerns.77 A survey of marine mammal workers found that 50% reported suffering injuries from marine mammals (one third of which were considered severe), and 23% reported skin rashes or reactions.78
Allergens
Zoo workers are exposed to allergens in both indoor and outdoor environments. Aquariums may have additional challenges with controlling mold. Control of allergens is similar to that for veterinary personnel.
Zoonoses
Because of the diversity of species and the possibility of introduction of infectious agents from contact between captive and wild animals, zoo and aquarium workers are exposed to perhaps the widest variety of zoonotic diseases compared with any other animal workers (see the species chart in Chapter 9). Guidelines for occupational health programs for zoo workers have been published by the American Association of Zoo Veterinarians.79 Zoonotic risks to nonhuman primate handlers resemble those of workers in primate research facilities. The care of wild ruminants may expose workers to livestock pathogens such as brucellosis and Q fever. Reptile keepers are at risk of Salmonella infection and envenomations, and bird workers are at risk of Chlamydophila infection. Other enteric disease risks to zookeepers include campylobacteriosis and shigellosis. Elephant handlers and staff working with nonhuman primates are at risk of TB exposure (Figure 12-5 ). Zoonotic risk prevention and control in zoo workers are similar to that in veterinary facilities.
Figure 12-5.

Elephant being examined by a veterinarian.
(From Fowler ME: Zoo and wild animal medicine current therapy, ed 6, St Louis, 2007, Saunders Elsevier.)
Aquarium workers are at risk of Mycobacterium marinum from tropical fish tanks. Other dermal exposure risks worthy of mention for aquarium workers include erysipeloid and Vibrio vulnificus.
Erysipeloid
Erysipeloid is an infection from contact with Erysipelothrix rhusiopathiae, a gram-positive rod bacterium found in fish as well as birds and pigs. The bacteria usually enter through broken skin. The most common manifestation is local erythema and wound infection (Color Plate 12-1). Although rare, bacteremia and endocarditis can occur.80
Vibrio Vulnificus
Vibrio vulnificus is a marine bacteria that can be encountered while handling tanks and marine animals. It may infect wounds and cause local wound infections in immunocompetent individuals and fatal septicemia (Color Plate 12-2) in immunocompromised persons.81 Careful hand hygiene after handling tanks and aquatic animals is essential.
Aquarium workers may also be at risk of exposure to pathogens in marine mammals during regular care as well as veterinary care and necropsies. Potential pathogens include leptospirosis, brucellosis, and “seal finger” from bites or other direct contact with seals and other pinnipeds. Seal finger is believed to be caused by infection with Mycoplasma phocacerebrale 82 and is characterized by pain, cellulitis, and joint swelling (Color Plate 12-3). Treatment is with tetracycline.
Chemical Hazards
Disinfectant chemicals are used widely in zoos and aquariums and may be capable of inducing irritation and allergy. If a veterinary facility is present in the zoo, anesthetic exposures may resemble those in other veterinary facilities.
Envenomations from reptiles, insects, fish, and other marine organisms represent a significant hazard to reptile handlers and aquarium workers. Emergency procedures for treating envenomations should be in place, including a stockpile or other resources to ensure the availability of antivenin for specific species housed at the facility (see Chapter 8).
Physical Hazards
Zoo and aquarium workers may have regular contact with captive wild animals capable of inflicting serious and fatal trauma, including large felids, bears, sharks, and elephants. Numerous other ergonomic risks exist, including transport of feed and bedding.
Risks can be controlled by design of enclosures and training of zoo workers in safe procedures for working near dangerous animals as well as engineering solutions for transport of heavy materials, such as ergonomically designed wheelbarrows and hoists. Special training is also needed for injury prevention for workers handling dangerous animals and equipment.
Psychosocial Stressors
Zoo and aquarium workers may share psychosocial stressors with other animal workers, including grief after an animal death and fear of attack by dangerous animals. They also may develop stress related to encounters with the general public.
Occupational Medicine Services for Zoo and Aquarium Workers
Because of the diversity and complexity of the occupational exposures, it would seem advisable that zoos and aquariums designate a medical provider or group of providers for both routine and emergency medical services. This designated provider should be familiar with both the infectious and noninfectious hazards that such workers face.
Preplacement Screening
Preplacement evaluations of zoo and aquarium workers should consider the range of species with which the worker is expected to have contact. Otherwise, baseline evaluations resemble those for veterinary and research animal workers.
Primate handlers should be screened for vaccination status as listed for laboratory primate workers. Nonhuman primate handlers and elephant handlers should be screened for TB. Stool cultures and stool tests for ova and parasites have been recommended at baseline for zoo workers. Such cultures should include Salmonella, Shigella, and Campylobacter.79 Audiometry at baseline should be performed for workers entering noisy jobs. Because of the wide range of infectious disease exposures, some with implications for disease emergence, it has been recommended that zoo workers bank serum at baseline and receive follow-up serology periodically to detect zoonotic infections.83 Such serum banking should be done under strict protocols to preserve confidentiality of workers and should be under the supervision of the consulting medical provider.
Medical Surveillance
Medical surveillance for zoo and aquarium workers is similar to that for veterinary and animal research workers.
Acute Injury, Illness, or Exposure Evaluation and Follow-up
Management of acute injuries and illnesses in zoo workers resembles that for veterinary and research animal workers. Designated emergency facilities should have protocols for antivenin treatment of reptile and other envenomations (see Chapter 8). Nonhuman primate exposures should be handled as emergencies, as with animal research workers, because of the risk of herpes B infection.
Pet Store Workers
Pet store employees share many of the exposures of zoo and aquarium workers yet are rarely enrolled in formal occupational health programs and may not have access to medical providers with a knowledge of the particular risks of the workplace. Compared with zoos, veterinary practices, and animal research facilities, there is a lack of published guidelines for occupational health services for this worker population. Despite this, the pet store industry is large and growing and employs thousands of workers nationwide. The recent multistate outbreak of monkeypox associated with importation of African rodents underscored the potential for disease emergence in pet stores and distribution facilities related to trade in exotic pets (see Chapter 10). Pet stores are generally required by local and federal regulations to have a designated veterinarian. Such an individual could be in a position to advocate for preventive health services for the employees. NASPHV has developed a compendium of measures to prevent disease associated with animals in public settings, which gives general guidelines for infection control in areas where the public has contact with animals, including pet stores, but does not provide detailed guidance on the occupational health of pet store workers.84
Hazards and Their Control in the Pet Store Setting
The hazards and principles of hazard control are similar to those in zoos and veterinary offices, with the exception that veterinary care procedures are not likely to take place. Consequently, exposures to anesthetics and radiation are not expected. Ventilation systems and cleaning of the facility may be geared to the retail setting, with less attention to health concerns. There also is potential for inadequate ventilation and consequent increased risk of airborne allergy.
Zoonotic disease risks depend on the species of animals sold in the facility but generally encompass risks seen in veterinary, animal research, and zoo settings, with the difference being the lack of invasive procedures performed on animals. Chemical and physical hazards to pet store workers are similar to those of other animal workers described.
Occupational Medicine Services for Pet Store Workers
Preplacement Screening
As previously mentioned, many pet store workers do not receive occupational health services, including preplacement examinations. It would seem reasonable, however, to offer such workers preplacement examinations that resemble those for veterinary workers. At the least, pet store workers should inform their health care providers, if they have one, about their work activities. The health care provider could then assess whether the individual is at increased risk of zoonotic infection because of an immunocompromised condition or is at risk of developing allergic reactions from work exposures. As with other animal worker occupational health issues, this requires that the health care provider be aware of the health risks related to animal work or can consult a veterinarian to be updated about such risks.
Vaccination
Vaccination for all workers should include tetanus if not up to date. Because ferrets can be susceptible to human influenza, influenza vaccine should be encouraged for workers with ferret contact.
Medical Surveillance
Ongoing medical surveillance of pet store workers is generally not performed. However, as with other animal handlers, NIOSH has recommended periodic monitoring for allergic symptoms with a symptom questionnaire and follow-up of positive responses as indicated. Such a screening questionnaire could cover infectious disease risk as well. Annual audiometry should be performed on workers with significant noise exposures.
Acute Injury, Illness, or Exposure Evaluation and Follow-up
A wide range of acute infectious conditions can present in pet store workers and should be considered in the differential diagnosis of ill employees. Animal bites and scratches should be treated according to the pathogens associated with particular species. In workers with bird contact who report respiratory symptoms, Chlamydophila infection and hypersensitivity pneumonitis (see Chapter 7) should be considered. Job restrictions and modifications after acute illnesses and injuries are similar to those of zoo and veterinary workers.
Farm Animal Workers
Agricultural workers with animal contact may work in settings ranging from backyard farms with a small number of animals to intensive confinement facilities with hundreds of thousands of animals. Therefore their work status may vary from informal laborers without written job contracts to registered employees in large and well-organized facilities. Job activities may range from feeding to manure management to slaughtering. The informal and varied settings may make use of personal protective equipment difficult, and there may be budgetary and other limitations to implementing engineering controls. There are few comprehensive occupational health guidelines for farm animal workers as well as a lack of OSHA standards directly targeting this setting. Farm managers may therefore be reluctant to see any value in developing relationships with members of an occupational health team or arranging for preplacement and periodic worker evaluations. Although veterinarians are often involved in the care of farm animals, some of the first-aid and other medical treatment may be accomplished by the farmers themselves. Some of the occupational exposures may resemble those of workers in zoos, yet the high density of animals in some production facilities can present unique exposure situations.
Technological changes in swine and poultry production have increased the efficiency of husbandry operations over the past several decades. A single concentrated animal feeding operation (CAFO) facility may house hundreds of pigs or more than 50,000 chickens or other poultry.2 Such facilities produce high concentrations of airborne dusts and gases, large quantities of manure, as well as the potential for rapid spread of diseases among animals and workers.
Allergens
A large variety of animal allergens on farms can pose a significant health hazard to animal workers. Allergy from pigs, horses, chickens, cattle, goats, and other domestic animals is well recognized (see Chapter 7). The development of occupational allergy to such allergens may cause significant difficulties in workers who are skilled in working with one particular type of animal, such as horses. Control strategies include wetting dusts to avoid airborne exposures, frequent washing of animals, and use of respirators and gloves when around animals. Workers may want to consider allergen desensitization to allow them to continue working with particular animal species.
Other significant antigens around farms include those produced by thermophilic bacteria growing on moldy hay or silage and in other moist environments that can cause hypersensitivity pneumonitis (farmer's lung; see Chapter 7), which can produce chills, fever, cough, and shortness of breath. A survey of dairy farmers found antibodies to such antigens in 75% of farmers tested and a history of symptoms consistent with farmer's lung in 17%.2
Endotoxin and Organic Dusts
Farm workers in CAFOs have some of the highest exposure to endotoxins and organic dusts, which can cause obstructive airway changes and the febrile syndrome known as organic toxic dust syndrome (ODTS).28 These organic dusts may contain plant material from bedding and feed; animal particulates, including feces, feathers, hair, skin cells, and urine; bacteria; pathogenic fungi; endotoxins; antibiotics and other feed additives; and chemicals including pesticides, ammonia, hydrogen sulfide, and methane. Significant rates of OTDS have been reported among swine CAFO workers.2 Wetting dusts and regular cleaning of bedding as well as improved ventilation and manure management may reduce worker exposure to organic dusts. When exposures are not able to be controlled, the use of respiratory protection may be necessary.
Zoonoses
Many diseases of domestic livestock and poultry are potentially communicable to workers. Table 12-6 shows some of these pathogens.
TABLE 12-6.
Specific Occupational Pathogens Associated With Animal Husbandry
| Type of Production | Pathogens | High-Risk Activities |
|---|---|---|
| Poultry | Salmonella, Campylobacter fetus, Chlamydophila, avian influenza virus, Newcastle disease virus, Erysipelothrix, Histoplasma | Slaughtering, meat processing, close contact with sick animals |
| Swine | Salmonella, Campylobacter, Streptococcus suis, Brucella, Erysipelothrix rhusiopathiae, vesicular stomatitis virus, hepatitis E virus, Nipah virus, influenza | |
| Cattle | Brucella, B. anthracis | Butchering meat, contact with birthing products, skinning, inadequate cooking of meat |
| Sheep | Orf virus, Coxiella, B. anthracis | Skinning, butchering, marketing |
| Bushmeat, wild game | Francisella, Trichinella, other emerging pathogens, primate viruses (non-U.S.) |
Contact with rodents near animal operations can increase the risk of hantavirus and other rodent-borne infections. Control of zoonotic disease risks involves many of the preventive measures mentioned for veterinary and research animal workers, including control of disease in animals, handwashing practices, disinfection of surfaces, and use of personal protective equipment as necessary. Rodent management and tick control can further reduce zoonotic risks, as can reducing contact between farm animals and wildlife.
Chemical Hazards
Chemical hazards encountered by farm animal workers include animal pesticides such as tick dips, oxides of nitrogen causing silo filler's lung from decomposing silage, and ammonia and hydrogen sulfide from manure waste in swine CAFO facilities.28 Silo filler's lung is a toxic pneumonitis that develops hours to days after a filling a silo and inhaling the irritating oxides of nitrogen gas. This exposure can result in acute respiratory distress syndrome (ARDS) and death in severe cases. Hydrogen sulfide can also cause ARDS and death in human beings and animals, often after pumping liquid manure out of a pit. Ammonia fumes can be highly irritating to the respiratory tract. These chemical risks can be reduced by substitution of less-toxic pesticides, proper silage and manure management, improvements in ventilation, and personal protective equipment for short-term, high-exposure tasks.
Physical Hazards
Work with large domestic animals carries a significant risk of crush and other traumatic injuries from kicking, biting, and other direct contact. Other physical hazards include noise and traumatic injuries from farm machinery, ultraviolet radiation, and musculoskeletal strains from lifting objects and animals. Certain tasks such as animal slaughter and processing may involve repetitive motions and result in overuse injuries. Animal slaughter and butchering can also result in injuries from knives and other sharp tools.
Psychosocial Stressors
Psychosocial stressors in working with farm animals include fear of trauma or infection. There may also be feelings of isolation for farmers working in rural locations.85
Occupational Medicine Services for Farm Animal Workers
As previously mentioned, many farm animal workers are not currently enrolled in preventive occupational medicine screening and follow-up programs. Nonetheless, the following components of preventive occupational medicine services for such workers should be considered based on the level of hazardous exposure. Sometimes screening is necessary after an outbreak of disease among either workers or animals; this process would be greatly simplified if baseline medical information were obtained on all workers.
Preplacement Screening
Because of the risk of allergy, workers on farms should be screened for allergic symptoms at baseline and periodically thereafter. Baseline spirometry is advisable. Workers with immunocompromised status are at increased risk of zoonotic transmission, and farm animal workers, especially if zoonotic diseases are endemic, should be screened and counseled for the risk of transmission in immunocompromised individuals. Musculoskeletal problems at baseline should be identified and a preventive plan implemented to prevent injuries. If a respirator will be used, the OSHA respirator medical evaluation and questionnaire should be completed.
Vaccination
Vaccinations for all farm animal workers should include tetanus and seasonal influenza vaccine (especially for swine and poultry workers). Periodic examinations should inquire about allergic and infectious disease symptoms as well as problems related to contact with chemicals or physical hazards.
Acute Injury, Illness, or Exposure Evaluation and Follow-up
The acute care of farm animal workers should consider zoonotic and allergic risks as well as the possibility of hypersensitivity pneumonitis. Cases of zoonotic disease in an animal worker should be considered a sentinel health event with relevance to both co-workers and herd health. Communication back to the veterinarian responsible for the health of the farm animals should occur, perhaps mediated by the public health department. The veterinarian may be simultaneously managing an outbreak in the domestic animals, and close communication between animal and human health professionals is critical. Infectious disease exposures requiring prophylaxis and follow-up may include anthrax and Mycobacterium bovis. Similarly, acute exposures to chemicals could be a sign that other workers and animals are at risk. Acute injuries from animals and other physical factors should also be viewed as opportunities to review possible breakdowns in safety measures and ways to further improve safety. Decisions about job restriction and modification and confidentiality issues are similar to those for other animal workers.
Wildlife Rehabilitators, Hunters, and Other Workers With Wildlife Contact
Although often not included in discussions of occupational risks to animal workers, several groups with significant exposure to wild animals through informal or formal work activities deserve mention. Wildlife rehabilitators are often volunteers who care for injured and sick wild animals in a variety of settings, including wildlife sanctuaries and their homes. Hunters may be amateur or professional and have intimate contact with blood and other body fluids of animals while butchering and skinning mammals and defeathering birds, in addition to the consumption of wild game meat. Other workers with potential wildlife contact include zoologists, who may be trapping, dissecting, and otherwise coming in contact with a wide variety of wild animals; forestry workers; and animal control officers and wildlife management biologists, who may be involved in the immobilization and transportation of wild animals and who are at risk of zoonotic disease through direct contact as well as exposure to vectors, including ticks and mosquitoes.
Hazards With Wildlife Contact
Hazards faced by these groups include a wide range of zoonotic disease exposures similar to those of zoo personnel and vary according to the species encountered. Examples include Lyme disease, ehrlichioses, brucellosis, tularemia, plague, rabies, giardiasis, and hantavirus.86 Vector-borne diseases are a greater threat to these individuals compared with many other animal workers. Wildlife rehabilitators face allergen and chemical exposures similar to those in veterinary practice or zoos. Individuals working around areas of bird and bat roosting, including caves, bridges, and abandoned buildings, are at risk for exposure to pathogenic fungi, including Histoplasma, Cryptococcus, and Blastomyces. Chemical exposures for wildlife management professionals may include inadvertent exposure to immobilizing (tranquilizer) agents and envenomations from reptiles and arthropods. Physical exposures for wildlife biologists include sun exposure, cold, and heat stress. Individuals working with wild animals face physical hazards of attacks and bites. Hunters risk similar hazards as well as the risk of noise exposure from firearms and acute injuries and bloodborne disease transmission during skinning and butchering game.
Occupational Health Services for Persons With Wildlife Contact
Occupational medical services for wildlife workers are often less formalized than for other worker groups such as research animal workers. Depending on the level of exposure, baseline medical screening that includes screening for allergy, immunocompromised status and other major medical conditions, and counseling about ways to reduce risk of exposure to zoonotic pathogens and avoid animal-related injury would appear to be indicated. If individuals have contact with rodents in a hantavirus-endemic area, they should undergo respirator medical clearance and respirator fit testing as required under the OSHA respirator standard. Serum banking should be considered for individuals at high risk of zoonotic disease exposure. Immunizations should include tetanus prophylaxis as well as vaccine rabies for individuals working with bats, raccoons, skunks, or other potentially rabid animals. Personal protective equipment should include respirators (Figure 12-6 ) and gloves for working with rodents in hantavirus-endemic areas. In other areas, gloves and masks are advisable when handling rodents. Hunters should use adequate hearing protection while hunting and impermeable gloves while preparing carcasses.
Figure 12-6.

Powered air purifying respirator for working with rodents in a hantavirus-endemic area.
(From Centers for Disease Control and Prevention: Respirators as a precaution for hantavirus infection. http://www.cdc.gov/ncidod/diseases/hanta/hps/noframes/prevent7.htm.)
Ongoing monitoring for allergy and infectious disease symptoms can be done periodically by using a screening questionnaire, as with other animal workers. Having an identified health care provider for these individuals could be of benefit both for ongoing prevention as well as for appropriate management of acute illnesses and injuries, which may involve unusual zoonotic diseases, envenomations, or other animal-related medical conditions with which many human health clinicians will be less familiar.
ONLINE RESOURCES
-
•
The National Institute for Occupational Safety and Health (NIOSH): http://www.cdc.gov/NIOSH
-
•
Occupational Safety and Health Administration (OSHA): http://www.osha.gov
-
•
Committee on Occupational Safety and Health in Research Animal Facilities, Institute of Laboratory Animal Resources, Commission on Life Sciences, National Research Council: Occupational health and safety in the care and use of research animals, Washington DC: National Academy Press; 1997. Available at http://books.nap.edu/openbook.php?isbn=0309052998
References
- 1.National Institute for Occupational Safety and Health NIOSH Alert: Preventing asthma in animal handlers. http://www.cdc.gov/Niosh/animalrt.html DHHS (NIOSH) Publication No. 97–116.
- 2.Rosenstock, Cullen M.R., Brodkin C.A., editors. Textbook of clinical occupational and environmental medicine. 2nd ed. Saunders Elsevier; Philadelphia: 2005. [Google Scholar]
- 3.Bureau of Labor Statistics. Animal care and service workers . In Occupational outlook handbook, 2008–2009 edition. 2008. http://www.bls.gov/oco/ocos168.htm#outlook Accessed May 27, [Google Scholar]
- 4.Seward J.P. Occupational allergy to animals. Occup Med. 1999;14:285–302. [PubMed] [Google Scholar]
- 5.Stellman J.M., editor. 4th ed. Vol. 4. International Labour Office; Geneva: 1998. (Encyclopedia of occupational health and safety). [Google Scholar]
- 6.Harber, Mummaneni, Crawford Influence of residency training on occupational medicine practice patterns. J Occup Environ Med. 2005;47:161–167. doi: 10.1097/01.jom.0000152924.60289.c9. [DOI] [PubMed] [Google Scholar]
- 7.Lincoln T.A., Bolton N.E., Garrett A.S. Occupational allergy to animal dander and sera. J Occup Med. 1974;16:456–469. [PubMed] [Google Scholar]
- 8.Bush R.K. Mechanism and epidemiology of laboratory animal allergy. ILAR Journal. 2001;42:4–11. doi: 10.1093/ilar.42.1.4. [DOI] [PubMed] [Google Scholar]
- 9.Gordon, Bush R.K., Newman-Taylor A.J. Laboratory animal, insect, fish and shellfish allergy. In: Bernstein I.L., Chan-Yeung, Malo J.L., editors. Asthma in the workplace. 3rd ed. Taylor and Francis Group; New York: 2006. [Google Scholar]
- 10.Von Essen, Donham Illness and injury in animal confinement workers. Occup Med. 1999;14:337–350. [PubMed] [Google Scholar]
- 11.Matsui E.C., Diette G.B., Krop E.J. Mouse allergen-specific immunoglobulin G and immunoglobulin G4 and allergic symptoms in immunoglobulin E-sensitized laboratory animal workers. Clin Exp Allergy. 2005;35(10):1347–1353. doi: 10.1111/j.1365-2222.2005.02331.x. [DOI] [PubMed] [Google Scholar]
- 12.Chan-Yeung, Malo J.L. Aetiological agents in occupational asthma. Eur Respir J. 1994;7:346–371. doi: 10.1183/09031936.94.07020346. [DOI] [PubMed] [Google Scholar]
- 13.Hunskaar, Fosse R.T. Allergy to laboratory mice and rats: a review of the pathophysiology, epidemiology and clinical aspects. Lab Anim. 1990;24(4):358–374. doi: 10.1258/002367790780865877. [DOI] [PubMed] [Google Scholar]
- 14.Seward J.P. Medical surveillance of allergy in laboratory animal handlers. ILAR Journal. 2001;42:47–54. doi: 10.1093/ilar.42.1.47. [DOI] [PubMed] [Google Scholar]
- 15.Wilson I.G. Airborne Campylobacter infection in a poultry worker: case report and review of the literature. Commun Dis Public Health. 2004;7(4):349–353. [PubMed] [Google Scholar]
- 16.Tiong, Vu, Counahan Multiple sites of exposure in an outbreak of ornithosis in workers at a poultry abattoir and farm. Epidemiol Infect. 2007;135(7):1184–1191. doi: 10.1017/S095026880700790X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gage K.L., Dennis D.T., Orloski K.A. Cases of cat-associated human plague in the Western US, 1977–1998. Clin Infect Dis. 2000;30(6):893–900. doi: 10.1086/313804. [DOI] [PubMed] [Google Scholar]
- 18.Cheng V.C., Lau S.K., Woo P.C. Severe acute respiratory syndrome coronavirus as an agent of emerging and reemerging infection. Clin Microbiol Rev. 2007;20(4):660–694. doi: 10.1128/CMR.00023-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention Update: outbreak of Nipah virus–Malaysia and Singapore, 1999. MMWR Morb Mortal Wkly Rep. 1999;48(16):335–337. [PubMed] [Google Scholar]
- 20.Wolfe N.D., Prosser T.A., Carr J.K. Exposure to nonhuman primates in rural Cameroon. Emerg Infect Dis. 2004;10(12):2094–2099. doi: 10.3201/eid1012.040062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mumford, Bishop, Hendrickx Avian influenza H5N1: risks at the human-animal interface. Food Nutr Bull. 2007;28(suppl 2):S357–S363. doi: 10.1177/15648265070282S215. [DOI] [PubMed] [Google Scholar]
- 22.Wilson M.L., Chapman L.E., Hall D.B. Rift Valley fever in rural northern Senegal: human risk factors and potential vectors. Am J Trop Med Hyg. 1994;50(6):663–675. doi: 10.4269/ajtmh.1994.50.663. [DOI] [PubMed] [Google Scholar]
- 23.Michel A.L., Huchzermeyer H.F. The zoonotic importance of Mycobacterium tuberculosis: transmission from human to monkey. J S Afr Vet Assoc. 1998;69(2):64–65. doi: 10.4102/jsava.v69i2.819. [DOI] [PubMed] [Google Scholar]
- 24.Michalak, Austin, Diesel Mycobacterium tuberculosis infection as a zoonotic disease: transmission between humans and elephants. Emerg Infect Dis. 1998;4(2):283–287. doi: 10.3201/eid0402.980217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hackendahl N.C., Mawby D.I., Bemis D.A. Putative transmission of Mycobacterium tuberculosis infection from a human to a dog. Am Vet Med Assoc. 2004;225(10):1573–1577. doi: 10.2460/javma.2004.225.1573. 1548. [DOI] [PubMed] [Google Scholar]
- 26.Berkelman R.L. Human illness associated with use of veterinary vaccines. Clin Infect Dis. 2003;37(3):407–414. doi: 10.1086/375595. [DOI] [PubMed] [Google Scholar]
- 27.Langley R.L., Pryor W.H., O'Brien K.F. Health hazards among veterinarians: a survey and review of the literature. J Agromedicine. 1995;2:23–52. [Google Scholar]
- 28.Mitloehner F.M., Calvo M.S. Worker health and safety in concentrated animal feeding operations. J Agric Saf Health. 2008;14(2):163–187. doi: 10.13031/2013.24349. [DOI] [PubMed] [Google Scholar]
- 29.Mandell G.L., Bennett J.E., Dolin . Principles and practice of infectious diseases. 6th ed. Churchill Livingstone; New York: 2005. [Google Scholar]
- 30.Huhn G.D., Austin, Carr Two outbreaks of occupationally acquired histoplasmosis: more than workers at risk. Environ Health Perspect. 2005;113(5):585–589. doi: 10.1289/ehp.7484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.National Institute for Occupational Safety and Health . Histoplasmosis–protecting workers at risk. 2009. http://www.cdc.gov/niosh/docs/2005-109/. NIOSH Publication No. 2005–109. Accessed January 1. [Google Scholar]
- 32.MacDougall, Kidd S.E., Galanis Spread of Cryptococcus gattii in British Columbia, Canada, and detection in the Pacific Northwest, USA. Emerg Infect Dis. 2007;13(1):42–50. doi: 10.3201/eid1301.060827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bradsher R.W., Jr Pulmonary blastomycosis. Semin Respir Crit Care Med. 2008;29(2):174–181. doi: 10.1055/s-2008-1063856. [DOI] [PubMed] [Google Scholar]
- 34.Meggs W.J. Chemical hazards faced by animal handlers. Occup Med. 1999;14:213–223. [PubMed] [Google Scholar]
- 35.Study links occupational exposures with risk of miscarriage. Anesthetic gases, radiation, pesticides are areas of concern for pregnant workers J Am Vet Med Assoc. 2008;232(10):1445–1447. [PubMed] [Google Scholar]
- 36.Gerasimon, Bennett, Musser Acute hydrogen sulfide poisoning in a dairy farmer. Clin Toxicol (Phila). 2007;45(4):420–423. doi: 10.1080/15563650601118010. [DOI] [PubMed] [Google Scholar]
- 37.Zwemer F.L., Jr, Pratt D.S., May J.J. Silo filler's disease in New York State. Am Rev Respir Dis. 1992;146(3):650–653. doi: 10.1164/ajrccm/146.3.650. [DOI] [PubMed] [Google Scholar]
- 38.Jeyaretnam, Jones Physical, chemical and biological hazards in veterinary practice. Aust Vet J. 2000;78(11):751–758. doi: 10.1111/j.1751-0813.2000.tb10446.x. [DOI] [PubMed] [Google Scholar]
- 39.Cohen S.P. Compassion fatigue and the veterinary health team. Vet Clin North Am Small Anim Pract. 2007;37(1):123–134. doi: 10.1016/j.cvsm.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 40.Managing stress and avoiding burnout. A self-care primer for overly compassionate and overworked veterinarians J Am Vet Med Assoc. 2004;225(4):492–493. [PubMed] [Google Scholar]
- 41.Elchos B.L., Scheftel J.M., Cherry Compendium of veterinary standard precautions for zoonotic disease prevention in veterinary personnel. J Am Vet Med Assoc. 2008;233(3):415–432. doi: 10.2460/javma.233.3.415. [DOI] [PubMed] [Google Scholar]
- 42.American College of Occupational and Environmental Medicine . ACOEM code of ethical conduct. 2008. http://www.acoem.org/codeofconduct.aspx. Accessed November 7. [DOI] [PubMed] [Google Scholar]
- 43.National Association of State Public Health Veterinarians, Inc., Centers for Disease Control and Prevention Compendium of animal rabies prevention and control, 2008. MMWR. 2008;57(RR-2):1–9. [PubMed] [Google Scholar]
- 44.Occupational Safety and Health Administration . OSHA recordkeeping handbook. 2008. http://www.osha.gov/recordkeeping/handbook/index.html. Accessed July 24, [Google Scholar]
- 45.American College of Occupational and Environmental Medicine . Confidentiality of medical information in the workplace. 2008. http://www.acoem.org/guidelines.aspx?id=3538. Accessed July 2, [Google Scholar]
- 46.Nienhaus, Skudlik, Seidler Work related accidents and occupational diseases in veterinarians and their staff. Int Arch Occup Environ Health. 2005;78:230–238. doi: 10.1007/s00420-004-0583-5. [DOI] [PubMed] [Google Scholar]
- 47.Babcock, Marsh A.E., Lin Legal implications of zoonoses for clinical veterinarians. J Am Vet Med Assoc. 2008;233(10):1556–1562. doi: 10.2460/javma.233.10.1556. [DOI] [PubMed] [Google Scholar]
- 48.Castorina J.S., Rosenstock Physician shortage in occupational and environmental medicine. Ann Intern Med. 1990;113(12):983–986. doi: 10.7326/0003-4819-113-12-983. [DOI] [PubMed] [Google Scholar]
- 49.Susitaival, Kirk J.H., Schenker M.B. Atopic symptoms among California veterinarians. Am J Ind Med. 2003;44(2):166–171. doi: 10.1002/ajim.10253. [DOI] [PubMed] [Google Scholar]
- 50.Susitaival, Kirk, Schenker M.B. Self-reported hand dermatitis in California veterinarians. Am J Contact Dermatitis. 2001;12(2):103–108. [PubMed] [Google Scholar]
- 51.Wright J.G., Jung, Holman R.C. Infection control practices and zoonotic disease risks among veterinarians in the United States. J Am Vet Med Assoc. 2008;232(12):1863–1872. doi: 10.2460/javma.232.12.1863. [DOI] [PubMed] [Google Scholar]
- 52.Bulcke D.M., Devos S.A. Hand and forearm dermatoses among veterinarians. J Eur Acad Dermatol Venereol. 2007;21(3):360–363. doi: 10.1111/j.1468-3083.2006.01935.x. [DOI] [PubMed] [Google Scholar]
- 53.National Institute of Occupational Safety and Health . A recommended standard for occupational exposure to waste anesthetic gases and vapors. 1977. Cincinnati, DHHS (NIOSH) Publication No. 77–140, [Google Scholar]
- 54.Meyer R.E. Anesthesia hazards to animal handlers. Occup Med. 1999;14:225–233. [PubMed] [Google Scholar]
- 55.Panni M.K., Corn S.B. Scavenging in the operating room. Curr Opin Anaesthesiol. 2003;16(6):611–617. doi: 10.1097/00001503-200312000-00007. [DOI] [PubMed] [Google Scholar]
- 56.Fritschi, Day, Shirangi Injury in Australian veterinarians. Occup Med (Oxford). 2006;56(3):199–203. doi: 10.1093/occmed/kqj037. [DOI] [PubMed] [Google Scholar]
- 57.Grandin Safe handling of large animals. Occup Med. 1999;14:195–212. [PubMed] [Google Scholar]
- 58.OSHA: CFR occupational noise exposure. In: Hearing conservation ame ndment (final rule), in 48 Federal Register. http://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=STANDARDS&p_id=9735.
- 59.Miller J.M., Beaumont J.J. Suicide, cancer, and other causes of death among California veterinarians, 1960–1992. Am J Ind Med. 1995;27(1):37–49. doi: 10.1002/ajim.4700270105. [DOI] [PubMed] [Google Scholar]
- 60.Rogelberg S.G., DiGiacomo, Reeve C.L. What shelters can do about euthanasia-related stress: an examination of recommendations from those on the front line. J Appl Anim Welf Sci. 2007;10(4):331–347. doi: 10.1080/10888700701353865. [DOI] [PubMed] [Google Scholar]
- 61.Occupational Safety and Health Administration OSHA respirator medical evaluation questionnaire. http://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=STANDARDS&p_id=9783
- 62.Committee on Occupational Safety and Health in Research Animal Facilities . Institute of Laboratory Animal Resources, Commission on Life Sciences, National Research Council. National Academy Press; Washington, DC: 1997. Occupational health and safety in the care and use of research animals. [Google Scholar]
- 63.Rahija R.J. Animal facility design. Occup Med. 1999;14:407–422. [PubMed] [Google Scholar]
- 64.Van Rhijn D.J. Occupational health for animal research facility. Chem Health Safety. 2004;11:24–27. [Google Scholar]
- 65.Centers for Disease Control and Prevention B virus (Cercopithecine herpesvirus 1) infection. http://www.cdc.gov/ncidod/diseases/bvirus.htm
- 66.Cohen J.I., Davenport D.S., Stewart J.A. Recommendations for prevention of and therapy for exposure to B virus (Cercopithecine herpesvirus 1) Clin Infect Dis. 2002;35:1191–1203. doi: 10.1086/344754. [DOI] [PubMed] [Google Scholar]
- 67.Centers for Disease Control and Prevention Fatal Cercopithecine herpesvirus 1 (B virus) infection following a mucocutaneous exposure and interim recommendations for worker protection. MMWR. 1998;47(49):1073–1076. [PubMed] [Google Scholar]
- 68.Centers for Disease Control and Prevention Nonhuman primate spumavirus infections among persons with occupational exposure–United States, 1996. MMWR Morb Mortal Wkly Rep. 1997;46(6):129–131. [PubMed] [Google Scholar]
- 69.Wachtman L.M., Mansfield K.G. Opportunistic infections in immunologically compromised nonhuman primates. ILAR J. 2008;49(2):191–208. doi: 10.1093/ilar.49.2.191. [DOI] [PubMed] [Google Scholar]
- 70.Heymann DL., editor. Control of communicable diseases manual. 19th ed. American Public Health Association; Washington DC: 2008. [Google Scholar]
- 71.Mazurek G.H., Jereb, Lobue Guidelines for using the QuantiFERON-TB Gold test for detecting Mycobacterium tuberculosis infection, United States. MMWR Recomm Rep. 2005;54(RR-15):49–55. [PubMed] [Google Scholar]
- 72.Jensen P.A., Lambert L.A., Iademarco M.F. CDC guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005. MMWR Recomm Rep. 2005;54(RR-17):1–141. [PubMed] [Google Scholar]
- 73.Langley Physical hazards of animal handlers. Occup Med. 1999;14:181–194. [PubMed] [Google Scholar]
- 74.Arluke Uneasiness among laboratory technicians. Occup Med. 1999;14:305–316. [PubMed] [Google Scholar]
- 75.Lang Y.C. Animal exposure surveillance: a model program. AAOHN Journal. 2005;53(9):407–412. [PubMed] [Google Scholar]
- 76.Engels E.A., Switzer W.M., Heneine Serologic evidence for exposure to simian virus 40 in North American zoo workers. J Infect Dis. 2004;190(12):2065–2069. doi: 10.1086/425997. [DOI] [PubMed] [Google Scholar]
- 77.Hill D.J., Langley R.L., Morrow W.M. Occupational injuries and illnesses reported by zoo veterinarians in the United States. J Zoo Wildlife Med. 1998;29(4):371–385. [PubMed] [Google Scholar]
- 78.Hunt T.D., Ziccardi M.H., Gulland F.M. Health risks for marine mammal workers. Dis Aquat Organ. 2008;81(1):81–92. doi: 10.3354/dao01942. [DOI] [PubMed] [Google Scholar]
- 79.American Association of Zoo Veterinarians . Guidelines for zoo and aquarium veterinary medical programs and veterinary hospitals. 1998. (Appendix 6) [PubMed] [Google Scholar]
- 80.Brooke C.J., Riley T.V. Erysipelothrix rhusiopathiae: bacteriology, epidemiology and clinical manifestations of an occupational pathogen. J Med Microbiol. 1999;48(9):789–799. doi: 10.1099/00222615-48-9-789. [DOI] [PubMed] [Google Scholar]
- 81.Hsueh P.R., Lin C.Y., Tang H.J. Vibrio vulnificus in Taiwan. Emerg Infect Dis. 2004;10(8):1363–1368. doi: 10.3201/eid1008.040047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Baker A.S., Ruoff K.L., Madoff Isolation of Mycoplasma species from a patient with seal finger. Clin Infect Dis. 1998;27(5):1168–1170. doi: 10.1086/514980. [DOI] [PubMed] [Google Scholar]
- 83.Wolfe N.D., Dunavan C.P., Diamond Origins of major human infectious diseases. Nature. 2007;447(7142):279–283. doi: 10.1038/nature05775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.National Association of State Public Health Veterinarians, et al. Inc. Compendium of measures to prevent disease associated with animals in public settings, 2007. MMWR Recomm Rep. 2007;56(RR-5):1–14. [PubMed] [Google Scholar]
- 85.Hovey J.D., Seligman L.D. The mental health of agricultural workers. In: Lessinger J.E., editor. Agricultural medicine: a practical guide. Springer; Porterville, CA: 2006. [Google Scholar]
- 86.Guidotti T.L., Naidoo Hunting, trapping and wilderness-related work. Clin Occup Environ Med. 2002;2:651–661. [Google Scholar]
- 87.Use of anthrax vaccine in the United States: recommendations of the Advisory Committee on Immunization Practices J Toxicol Clin Toxicol. 2001;39(1):85–100. doi: 10.1081/clt-100102886. [DOI] [PubMed] [Google Scholar]


