Abstract
Travel by air is a safe means of transport, but from the physiologic point of view it is a means of putting people at risk as well as a potential means of spreading infectious disease. Atmospheric pressure falls with altitude and above about 10,000 feet, blood desaturation leads to hypoxia. The aircraft cabin is pressurized to maintain an effective altitude below 8000 feet, which provides adequate protection for healthy travelers. Those individuals with cardiopulmonary impairment or other conditions affecting fitness to travel should seek advice from the airline in consultation with their medical provider. People are the primary source of microorganisms in aircraft cabins and are the most important reservoirs of infectious agents on aircraft. Recirculated cabin air is filtered to remove microorganisms, but this does not prevent person-to-person spread of infectious disease in vulnerable people. The World Health Organization and Centers for Disease Control and Prevention produce guidelines; and people with febrile illnesses should postpone air travel.
Keywords: Air travel, Cosmic radiation, Deep vein thrombosis, Fitness to fly, Hypoxia, Infectious disease, Pressurization
Introduction
Although the physiology of the human being is optimized for existence at sea level, most fit and healthy individuals can ascend to around 10,000 feet (3048 m) above sea level before lack of oxygen (hypoxia) begins to have ill effects and reduces performance.
With increasing altitude, there is a fall in atmospheric pressure and a decrease in ambient air density and temperature. The pressure at sea level in the standard atmosphere is 760 mmHg (29.92 inHg, 1013.2 mb); this falls by half at 18,000 feet (5486 m), where the ambient temperature is about −20°C. Up to the tropopause (approximately 36,000 feet [10,973 m]), the ratio of gases in the atmosphere remains constant at nearly 78% nitrogen and 21% oxygen; <1% is contributed by gases such as argon, carbon dioxide, neon, hydrogen, and ozone.
Ascent to an altitude of 10,000 feet (3048 m) produces a significant fall in the partial pressure of oxygen in the alveoli, but because of the relationship between the oxygen saturation of hemoglobin in blood and oxygen tension, there is only a slight fall in the percentage of oxygen saturation of hemoglobin in the blood. However, hemoglobin saturation falls quickly upon further ascent, resulting in hypoxia with a decrease in an individual's ability to perform complex tasks.1
Fig. 47.1 shows the oxygen dissociation curve of blood. The curve illustrated is the average for a fit young adult but is influenced by factors such as age, state of health, tobacco use, and ambient temperature.
Fig. 47.1.
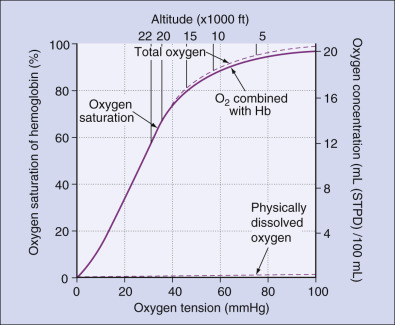
The oxygen dissociation curve of blood. Hb, Hemoglobin; STPD, standard temperature and pressue, dry.
While normal healthy individuals can tolerate altitudes up to about 10,000 feet (3048 m) with no harmful effects, individuals suffering from impairment of the respiratory or circulatory system may be less able to tolerate the mild hypoxia experienced at even this altitude. In an ideal world, the aircraft cabin would be pressurized to simulate sea level conditions.
To achieve this would require an extremely strong and heavy aircraft structure with severe implications on load-carrying capacity, fuel consumption, and range. As a result, a compromise is struck, with airworthiness regulations stating that “pressurized cabins and compartments to be occupied must be equipped to provide a cabin pressure altitude of not more than 8,000 ft at the maximum operating altitude of the airplane under normal operating conditions.”2 Most aircraft maintain a cabin altitude of around 6000–7000 feet during normal operation. Newer aircraft, such as the Boeing 787 and Airbus A350, are manufactured from composite material enabling them to operate at lower cabin altitudes of around 5000–6000 feet.
The Pressurized Cabin
The aircraft's environmental control system (ECS) maintains comfortable pressure and temperature within the cabin. In most commercial civilian aircraft, pressurization is achieved by tapping bleed air from the engine compressors, cooling it, and distributing it throughout the cabin. The Boeing 787 uses electrically driven air compressors rather than utilizing bleed air. This is related to the use of a completely electrical infrastructure, and Boeing continues to utilize engine bleed air in its other later aircraft types. In both systems, the cabin pressure is maintained at the desired level by regulating the outflow of air from the cabin. Fig. 47.2 illustrates typical ambient and cabin altitudes for a typical flight. Fig. 47.3 shows air circulation in the cabin of a typical twin-aisle aircraft.
Fig. 47.2.
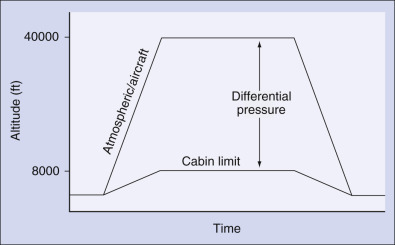
Typical cabin pressure flight profile.
Fig. 47.3.
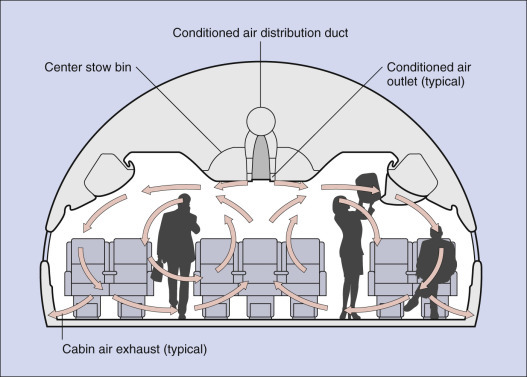
Examples of air flow patterns in the twin-aisle cabin.
Due to the change in cabin pressure during climb and descent, individuals may experience discomfort from the expansion of gas trapped within the body. Gas trapped within the gut or the middle ear and sinuses is normally able to escape without any problem, but there may be occasions when this is not so. The human ear is particularly sensitive to rates of pressure change. The middle ear cavity, separated from the outer ear by the tympanic membrane, communicates with the nasopharynx and hence the ambient atmosphere by way of the eustachian tube, the proximal two-thirds of which has soft walls that are normally collapsed. During ascent to altitude, the gas in the middle ear cavity expands and escapes through the eustachian tube into the nasopharynx, thereby equalizing the pressure across the tympanic membrane. The pharyngeal portion of the eustachian tube acts as a one-way valve, allowing expanding air to escape easily to the atmosphere, which may be felt as a “popping” sensation as air escapes from the tube during ascent.
During descent, the opposite occurs. The air in the middle ear contracts and air from the nasopharynx must enter the middle ear to maintain equal pressure across the tympanic membrane. This can cause difficulties for some individuals, as now the eustachian tube can collapse due to the negative pressure developing in the middle ear, which prevents passive flow of air back into the middle ear cavity. This relative increase of pressure on the outside of the tympanic membrane pushes it into the middle ear cavity, and may result in a sensation of fullness, a decrease in hearing acuity, and pain. Active maneuvers such as swallowing, yawning, and jaw movements can open the eustachian tube, and relieve the pressure. If this is not effective, it may be necessary to occlude the nostrils and raise the pressure in the mouth and nose to force air into the middle ear cavities. This can usually be achieved simply by raising the floor of the mouth with the glottis shut, or by raising the pressure in the entire respiratory tract by contracting the expiratory muscles (Valsalva maneuver). Because descent causes more problems with eustachian tube dysfunction than ascent, infants often begin crying during the descent portion of the flight which can passively assist pressure equalization.
As well as regulating the airflow to pressurize the aircraft, the ECS removes airborne contaminants and controls temperature in the cabin. This is facilitated by the recirculation of approximately 50% of the cabin air and mixing it with conditioned outside air delivered from the engine bleed air or electric compressors.
Recirculation allows the total airflow rate into the cabin to be higher than the inflow rate of outside air, so good circulation in the cabin can be maintained independently of the outside airflow. In most older generation jet aircraft, all the air supplied to the cabin came from outside air, without the benefits of recirculation (leading to perceived draughts and reduced humidity). This practice was inefficient, with a substantial energy and environmental cost, because tapping bleed air can reduce engine thrust and increase fuel consumption. Recirculation reduces this cost.
In modern jet aircraft, the recirculated air is passed through high-efficiency particulate air (HEPA) filters which remove in excess of 99.97% of particles rated at 0.3 µm in diameter. They are effective in removing bacteria and viruses from the recirculated air, thus preventing their spread through the cabin by this route.
Recirculated air is obtained from the area above the cabin or along the floor; air from the cargo bay, lavatories, and galleys is not recirculated. The flow rate of outside air per seat ranges from 3.6–7.4 L/s (7.6–15.6 ft3/min), with the percentage of recirculated air distributed to the passenger cabin being in the order of 30%–55% of the total air supply.3 The result of filtering the recirculated air is a significant improvement in cabin air quality by the removal of particles and biological microorganisms.
Building environmental systems commonly use up to 90% of recirculated air, compared to the maximum recirculated air flow in aircraft of 55% and do not have the benefit of HEPA filtration. Thus aircraft cabin air is of higher quality than the air in most commercial buildings.
The air supply to the flight deck (or cockpit) is delivered at a slightly higher pressure than the air supplied to the cabin, ensuring a positive pressure differential to prevent the ingress of smoke or fumes to the flight deck in the event of a fire. The flow rate of the flight deck air supply is also slightly higher than that to the cabin to assist cooling of the avionics and other electronic equipment.
Concerns have been expressed that oil fumes may be present in cabin air as a result of leakage into the engine bleed air. Independent research has so far failed to confirm adverse health effects caused by such minor and intermittent cabin air contamination.4, 5
Humidity
Humidity is the concentration of water vapor in the air. Relative humidity is the ratio of the actual amount of vapor in the air to the amount that would be present if the air was saturated at the same temperature, expressed as a percentage. Saturated air at high temperature contains more water vapor than at low temperature, and if unsaturated air is cooled enough, it becomes saturated. Extremes of humidity can lead to passenger and crew discomfort. High humidity can cause condensation of moisture on the inside of the aircraft shell, leading to problems such as corrosion. Condensation can give rise to biological growth causing adverse effects on cabin air quality.
At a typical aircraft cruising altitude of 30,000 feet (9144 m), the outside air temperature is around −40°C and is extremely dry, typically containing about 0.15 g water/kg of air. For pressurized aircraft flying at these levels, the conditioned air entering the cabin has a relative humidity of <1%. Exhaled moisture from passengers and crew, together with moisture from galleys and toilet areas, increases the humidity to an average of 6%–10%, which is below the 20% normally accepted as comfort level.6 Improvements in the materials used in the cabins of new aircraft, such as the Boeing 787 and Airbus A350, have led to better retention of moisture in cabin air, without increased corrosion, leading to humidity levels of around 15% during the cruise. Very large aircraft, such as the A380, may achieve similar ambient relative humidity levels because of the high density of passengers and crew.
Research has shown that the maximum additional water lost from an individual during an 8-hour period in zero humidity, compared to normal day-to-day loss, is around 100 mL. The sensation of thirst experienced by healthy individuals in this environment is due to local drying of the pharyngeal membranes, leading to the spurious sensation of thirst. There is no evidence that exposure to a low-humidity environment itself leads to dehydration, although local humidity can cause mild subjective symptoms such as dryness of the eyes and mucous membranes.7
No significant effect has been shown on measures of psychomotor performance, although there can be some changes in the fluid regulatory hormones.7 It is unlikely that low humidity has any ill effects, provided overall hydration is maintained by drinking adequate fluid. The body's homeostatic mechanisms ensure that central hydration is maintained, although the peripheral physical effects can lead to discomfort. Dry skin can be alleviated by using aqueous moisturizing creams, particularly just before flight, and dry eye irritation can be alleviated by using moisturizing eye drops. Individuals prone to develop dry eyes are advised not to wear contact lenses during long flights in pressurized aircraft.8
Although the aircraft cabin environment is similar to many other indoor home and office environments where people are exposed to a mixture of external and recirculated air, the cabin environment is also different in many respects: the high occupant density, the inability of the occupants to leave at will, and the need for pressurization. In flight, there is a combination of environmental factors, including low air pressure and low humidity, low-frequency vibration, and constant background noise. Although the noise and vibration can contribute to fatigue, the levels are all below those accepted as potentially harmful to hearing.8, 9
Ozone
Ozone is a highly reactive form of oxygen found naturally in the upper atmosphere. It is formed primarily above the tropopause from the action of ultraviolet (UV) light on oxygen molecules, varying with latitude, altitude, season, and weather conditions. The highest concentrations in the northern hemisphere are generally found at high altitude over high-latitude locations during the winter and spring.
The effects of ozone on humans can include eye irritation, coughing due to irritation of the upper respiratory system, nose irritation, and chest pains. Thus regulatory authorities require that transport category aircraft operating above 18,000 feet (5486 m) must show that the concentration of ozone inside the cabin will not exceed 0.25 parts per million (ppm) by volume (sea level equivalent) at any time, and a time weighted value of 0.1 ppm by volume (sea level) for scheduled segments of more than 4 hours.10 Accordingly, long-haul transport jet aircraft are equipped with ozone catalytic converters which break down or “crack” the ozone before it enters the cabin air circulation.
Cosmic Radiation
Cosmic radiation is an ionizing radiation produced when primary photons and α particles from outside the solar system interact with components of the earth's atmosphere. A second source of cosmic radiation is the release of charged particles from the sun, which become significant during periods of solar flare (“sun storm”). Ionizing radiation is a natural part of the environment in which we live, present in the earth, buildings, the food we eat, and even in the bones of our bodies.
The other type is nonionizing radiation which includes UV light, radio waves, and microwaves. Humans, animals, and plants have all evolved in an environment with a background of natural radiation and, with few exceptions, it is not a significant risk to health.
The amount of cosmic radiation that reaches the earth from the sun and outer space varies: its energy is effectively absorbed by the atmosphere and is also affected by the earth's magnetic field. The effect on the body will depend on the latitude and altitude at which the individual is exposed, and on the length of time of exposure.
Cosmic radiation may be measured directly using sophisticated instruments, as was done routinely in the Concorde supersonic transport, or it can be estimated using a computer program integrating the route, time at each altitude, and phase of the solar cycle to calculate the radiation dose for any given flight. Several research organizations have confirmed actual measurements taken on board an aircraft to verify the computer estimations.11 Effective doses of cosmic radiation are in fact very low.
The International Commission for Radiological Protection (ICRP) recommends maximum mean body effective dose limits of 20 milliSieverts (mSv) per year (averaged over 5 years) for workers exposed to radiation as part of their occupation (including flight crew), and 1 mSv/year for the general population
For typical annual flight schedules, crew members accumulate around 4–5 mSv/year on long-haul operations, and 1–2 mSv/year on European short-haul operations from cosmic radiation.
The ICRP also recommends that it is not necessary to treat the exposure of frequent-flyer passengers as occupationally exposed for the purpose of control. Thus essentially they recommend that only aircrew should be considered.12
Cosmic radiation is of no significance at altitudes <25,000 feet (7620 m) because of the attenuating properties of the earth's atmosphere. There is no evidence from epidemiologic studies of flight crew of any increase in incidence of cancers linked to ionizing radiation exposure, such as leukemia.
All available evidence indicates an extremely low probability of airline passengers or crew suffering any effects from exposure to cosmic radiation.11
Pesticides in the Cabin
The use of pesticides in the aircraft cabin is important for the control of vectorborne diseases, but controversy remains about the potential adverse health effects on passengers and crew members.13 The World Health Organization (WHO) in 1995 concluded that no toxicologic hazard was attributable to any chemicals or methods recommended for use in aircraft disinsection.14 Requirements may be found at https://www.transportation.gov/airconsumer/spray. The issue remains controversial: some advocate nonpesticide methods of disinfection, and WHO is currently reevaluating the safety of chemicals in use and proposed for use in aircraft.
Infectious Diseases and Cabin Air: Droplet and Airborne Spread
People are the primary source of microorganisms in aircraft cabins and are the most important reservoirs of infectious agents on aircraft.15 These microorganisms are found normally on or in the human body (normal flora) and very rarely cause infections. Studies have shown insignificant differences in concentrations of microorganisms sampled between the following:
-
•
different aircraft, airline, or flight durations
-
•
aircraft cabins and other types of public transport vehicles
-
•
aircraft cabins and typical indoor and outdoor urban environments
There has been increasing concern over the respiratory spread of infections during air travel, via droplet and airborne transmission which may occur during coughing, sneezing, or talking.16 Droplets are relatively large (>5 µm) particles that can travel only a short distance through the air; they do not remain suspended. Infection occurs when microorganisms within the droplets come into contact with a susceptible person. Tuberculosis is an example of an infection spread by droplet transmission.
In airborne transmission, smaller (≤5 µm) respiratory particles, called droplet nuclei, are inhaled by a susceptible host. These particles remain suspended in air indefinitely and may spread over long distances, depending on environmental factors. Measles is an example of a disease spread this way.
There is no evidence that the pressurized cabin itself makes transmission of disease any more likely. The risk of exposure to infectious individuals is highest for the passengers seated closest to a source person, typically within 3 feet.16 Microorganisms suspended in cabin air will be removed by the HEPA filters during air recirculation, but these filters provide little protection from the microorganisms emitted by an infected person seated close by who coughs or sneezes. Fortunately most individuals are protected by natural or acquired immunity.
Tuberculosis
The transmission of Mycobacterium tuberculosis (MTB), the bacterium that causes tuberculosis (TB), during air travel has been most extensively studied.17 No cases of active TB resulting from transmission during air travel have been reported. While uncommon, there is reliable evidence that in-flight transmission from highly infectious individuals on long-haul flights (>8 hours) has occurred.18 The identification of secondary cases of active TB is one of the most important activities for controlling worldwide TB. Therefore it is important to assess and quantify airline exposures, even though transmission risk of TB among passengers is difficult to determine.19
Infectious individuals may be prevented from traveling by commercial aircraft. If an infectious individual is found to have flown any leg for over 8 hours, the US Centers for Disease Control and Prevention (CDC) can assist a health department to perform a contact investigation of the appropriate number of passengers seated around the index case for that flight.
WHO updated its guidance for the prevention and control of TB during air travel in 2008: http://www.who.int/tb/publications/2008/WHO_HTM_TB_2008.399_eng.pdf.20
Influenza
There is little well-documented evidence for the transmission of influenza virus during air travel.21 Since 1997 a new strain of avian influenza virus (H5N1) has been responsible for several outbreaks and continues to be closely monitored around the world. A novel strain of influenza A H1N1, so-called “swine flu,” emerged from a pig farm in central Mexico in 2009 and eventually caused over 200,000 deaths worldwide within the first year the virus circulated.22 Although air travel was strongly associated with the importation of cases to other countries, actual transmission during air travel, though often suspected, was difficult to document.23, 24, 25 An investigation by the CDC among passengers who flew on four North American flights in April 2009 with individuals who were ill with laboratory-confirmed H1N1 showed low risk of in-flight transmission to passengers and crew. In-flight transmission of the new virus is unlikely in flights of relatively short duration, although longer intercontinental flights may pose a greater risk of transmission. Offering symptomatic passengers medical care upon arrival at airport checkpoints may be an effective way to screen for influenza, and is likely to be more cost effective than exit and entry screening, quarantine, and travel restrictions.26 The simplest, most effective, and least costly control measures involve the individual behaviors of travelers and of their health care providers.27
Measles
Measles is a highly contagious viral disease that is spread by airborne transmission. Therefore the potential for disease transmission during air travel exists. Because of the occasional outbreaks of measles not only in developing countries but also in the developed world due to lower than desirable immunization rates, this continues to be a concern, as imported cases of measles are increasing in many countries. Cases of measles continue to be identified as a direct result of in-flight exposure,28, 29, 30 but this risk is exceedingly low for flights into and within the United States, explained in great part by the high level of immunity in the US population.31 As with any infectious disease, it is possible that exposures occur before or after the flight, such as in the check-in or boarding areas, jetway, baggage claim area, or other exposure unrelated to the flight.
Mumps
In-flight risk of mumps transmission is not high, and passenger contact investigations have low yield and are resource intensive. Therefore in the United States, the CDC no longer conducts flight-related mumps contact investigations.
Infectious Diseases and Contamination of Aircraft Interior Furnishings
Norovirus probably has been transmitted from symptomatic flight attendants to passengers32 and likely also caused infection in several flight attendants through contact with a contaminated aircraft over several flights.33 Transmission can occur via interior surfaces of any mode of public transportation, but is a particularly difficult situation in aircraft as cleaning agents must be viricidal as well as compatible with aircraft materials. In the absence of in-flight vomiting and diarrhea, norovirus is not likely to be transmitted on short domestic flights.
Ebola Virus, Middle East Respiratory Syndrome, and Other Intermittent Outbreaks of Concern to Air Travel
Although it is unlikely for a person to become infected with a disease of public health significance while traveling on a commercial aircraft, commercial air travel can be a major contributor to the global spread of infectious diseases. Despite the 2014 WHO declaration of the Ebola outbreak in West Africa as a public health emergency of international concern, no transmission of Ebola occurred on flights known to have transported passengers who developed the condition.34
Travel restrictions were briefly put in place to control the spread of Middle East respiratory syndrome coronavirus (MERS-CoV) in South Korea in 2015, illustrating the use of travel restriction and air contact investigations as public health tools to limit the spread of emerging infectious diseases of public health significance.
Guidelines exist to assist flight crew in the management of ill passengers and can be accessed from www.who.org, www.cdc.gov, or www.iata.org. In general, good respiratory and hand hygiene practices should always be encouraged, and people with febrile illnesses should postpone air travel.
Passenger Health
Flying as a passenger should be no problem for the fit, healthy, and mobile individual.
In-flight medical problems can result from the exacerbation of a preexisting medical condition, or can be an acute event in a previously healthy individual. Although the main problems relate to the physiologic effects of hypoxia and expansion of trapped gases, the complex airport environment can be stressful and challenging to the passenger, leading to problems before even getting airborne.
Although passengers with medical needs require medical clearance from the airline, passengers with disabilities do not. However, disabled passengers need to notify the airline about their requirement for special services such as wheelchair assistance. This should be done at the time of booking, ideally several days before travel.
Preflight Assessment and Medical Clearance
The objectives of medical clearance are to provide advice to passengers and their medical attendants on fitness to fly, and to prevent delays and diversions to the flight because of deterioration in the passenger's well-being. It depends upon self-declaration by the passenger, and upon the attending physician having an awareness of the flight environment and how this might affect the patient's condition.
Most major airlines provide services for passengers who require extra help, and have a medical adviser to assess the fitness for travel of those with medical needs. Individual airlines work to their own guidelines, generally based on those published by the Aerospace Medical Association (AsMA) on fitness for travel.35
The International Air Transport Association (IATA) publishes a recommended Medical Information Form (MEDIF) for use by member airlines.36 The MEDIF is normally downloaded from the airline website; it should be completed by the passenger's medical health care provider and passed to the airline, or travel agent, at the time of booking.
Medical clearance is required when:
-
•
Fitness to travel is in doubt because of recent illness, hospitalization, injury, surgery, or instability of an acute or chronic medical condition
-
•
Special services are required (e.g., oxygen, stretcher, or authority to carry or use accompanying medical equipment such as a ventilator or a nebulizer)
Medical clearance is not required for carriage of an invalid passenger outside these categories, although special needs (such as a wheelchair) must be notified to the airline at the time of booking. Cabin crew members are unable to provide individual special assistance to invalid passengers. Passengers unable to provide for their own personal needs during flight (such as toileting or feeding) must travel with an accompanying adult who can assist.
It is vital that passengers remember to carry with them any essential medication, and not pack it in checked baggage in case of delay of baggage retrieval or loss enroute. Also baggage in the hold is not accessible during flight.
Deterioration on holiday or on a business trip of a previously stable medical condition or accidental trauma may give rise to the need for medical clearance for the return journey. A stretcher may be required, together with medical support, which can incur considerable cost. It is thus important for all travelers to have adequate travel insurance, including provision for the use of a specialist repatriation company to provide necessary medical support.
Assessment Criteria
In determining the passenger's fitness to fly, a basic knowledge of aviation physiology and physics can be applied to the pathology. Trapped gas will expand in volume by up to 30% during flight, and consideration must be given to the effects of the relative hypoxia associated with a cabin altitude of up to 8000 feet above mean sea level. The altitude of the destination airport may also need to be considered in assessing individual fitness to travel.
The passenger's exercise tolerance can provide a useful guide on fitness to fly: if unable to walk a distance >150 feet (50 m) without developing dyspnea, there is a risk of being unable to tolerate the relative hypoxia of the pressurized cabin. More specific guidance can be gained from knowledge of the passenger's blood gas levels and hemoglobin value. Information is available on the websites of the AsMA37 and the IATA,38 but individual cases might require individual assessment by the attending physician.
Deep Vein Thrombosis and Prevention of Pulmonary Embolism
The prolonged period of immobility associated with long-haul flying can be a risk for those individuals predisposed to develop deep vein thrombosis (DVT). Preexisting risk factors include:
-
•
Blood disorders and clotting factor abnormalities
-
•
Cardiovascular disease
-
•
Malignancy
-
•
Recent major surgery
-
•
Lower limb/abdominal trauma
-
•
DVT history
-
•
Pregnancy
-
•
Estrogen therapy (including oral contraception and hormone replacement therapy)
-
•
Age >40 years
-
•
Immobilization
-
•
Pathologic body fluid depletion
Those passengers known to be vulnerable to DVT should seek guidance from their attending physician on the use of compression stockings and/or anticoagulants. There is no evidence that flying itself is a risk factor for the development of DVT, but those at high risk should always have medical guidance prior to any form of prolonged travel or immobility to prevent the development of potentially fatal pulmonary embolism.
Considerations of Physical Disability or Immobility
As well as the reduction in ambient pressure and the relative hypoxia, it is important to consider the physical constraints of the passenger cabin, including not impeding the free egress of cabin occupants in case of emergency evacuation.
There is limited leg space and a passenger with an above-knee leg plaster or an ankylosed joint may simply not fit in the available space. There may be long periods of immobility in an uncomfortable position and adequate pain control must be ensured for the duration of the journey. Even in the premier class cabins, there are limits on space.
To avoid impeding emergency egress, immobilized or disabled passengers cannot be seated adjacent to emergency exits, despite the possible availability of increased leg room. Similarly, a plastered leg cannot be stretched into the aisle.
There is limited space in aircraft toilet compartments, and if assistance is necessary a traveling companion is required.
The complexities of the airport environment, including check-in and security, should not be underestimated, and must be considered during the assessment of fitness to fly.39
The operational effect of the use of equipment such as wheelchairs must be taken into account, and the possibility of aircraft delays or diversion to another airport considered. It may be necessary to change aircraft, and transit between terminals and medical facilities will not easily be available to a transiting passenger.
There is often a long distance between the check-in desk and the boarding gate. Not all flights operate from jet-ways, and it may be necessary to use stairs and transfer coaches. It is important for the passenger to specify the level of assistance required when booking facilities such as wheelchairs.
Oxygen
In addition to the main ventilation system, all commercial aircraft carry an emergency oxygen supply for use in the event of pressurization failure or emergencies. The passenger supply is delivered via dropdown masks from chemical generators or an emergency reservoir, and the crew supply is from oxygen bottles strategically located within the cabin. The dropdown masks are automatically released en masse (the so-called rubber jungle) in the event of the cabin altitude exceeding a predetermined level. This supply has a limited duration if provided by chemical generators—usually about 10 minutes. The flow rate is between 4 and 8 L (normal temperature and pressure; NTP) per minute, and is continuous once the supply is triggered. In some aircraft, oxygen is supplied from an emergency reservoir and delivered to the cabin via a “ring main”; it may be possible to plug a mask into this ring main to provide supplementary oxygen for a passenger.
Sufficient first-aid oxygen bottles are carried to allow the delivery of oxygen to a passenger in case of an in-flight medical emergency, at a rate of 2 or 4 L (NTP) per minute. However, this cannot be used to provide a premeditated supply for a passenger requiring it continuously throughout a journey.
If a passenger requires continuous (“scheduled”) oxygen for a journey, this must be prenotified to the airline. Most airlines make a nominal charge. Some carriers allow the use of portable oxygen concentrators, provided the unit meets regulatory specifications.
Oxygen equipment must meet minimum regulatory safety standards, and the oxygen must be of “aviation” quality, which is different with respect to water content from “medical” quality.36, 37 Airlines provide an oxygen service only during flight and not during the time spent in the airport terminal. Arrangements need to be made for oxygen provision at the passenger's destination and, if necessary, during connections to other flights.
In-Flight Medical Emergencies
An in-flight medical emergency is defined as a medical occurrence requiring the assistance of the cabin crew. It may involve the use of medical equipment or drugs, and involve a request for assistance from a medical professional traveling as a passenger. It can be as simple as a headache or a vasovagal episode, or something major such as a myocardial infarction or impending childbirth. In some respects, dealing with an in-flight medical emergency is akin to a “wilderness medicine” situation, as the responding provider is in an unfamiliar and austere environment, with limited resources, often requiring improvisation and a common-sense approach.40
However, since health care professionals are not guaranteed to be on board every flight, or may not be willing or able to render aide, most airlines have ground-based medical consultation services available to provide recommendations for care during flight. Associated liabilities for volunteer medical care are generally determined by the law of the country in which the incident occurs. In the United States, legal protection is provided by the Aviation Medical Assistance Act (1998), but such volunteers are not protected if they engage in gross negligence or intentionally cause harm.41
The incidence is comparatively low, although the media impact of an event can be significant. One major international airline reported 3022 incidents occurring in something over 34 million passengers carried in 1 year, the figures remaining consistent despite changes in the demography of travelers. Most in-flight medical emergencies are related to syncope, respiratory symptoms, or gastrointestinal symptoms; few of these result in diversion of the aircraft or in death.42
Any acute medical condition occurring during a flight can be alarming owing to the remoteness of the environment. The cabin crew receive training in advanced first aid and basic life support and the use of the aircraft emergency medical equipment. Many airlines give training in excess of the regulatory requirements, particularly when an extended range of medical equipment is carried. In serious cases the crew may request assistance from a medical professional traveling as a passenger, referred to as a Good Samaritan.
Responsibility for the conduct of the flight rests with the aircraft captain, who makes the final decision as to whether an immediate unscheduled landing or diversion is required. The captain must consider operational factors as well as the medical condition of the passenger, taking advice from all sources. An assisting Good Samaritan has an important role to play, perhaps in radio consultation with the airline's medical adviser.
Telemedicine
Many airlines use an air-to-ground link to allow the captain and/or the Good Samaritan to confer with the airline's medical adviser on the condition of the sick passenger.43 The airline operations department is also involved. Some airlines maintain a worldwide database of medical facilities available at or near the major airports, possibly in association with a third-party provider giving medical advice and assistance with arranging emergency medical care for the sick passenger at the diversion airport.
The link from the aircraft is made using radio-telephone voice or data link (VHF or ACARS), high-frequency (HF) radio communication, or a satellite communication system (satcom). Satcom is unaffected by terrain, topography, or atmospheric conditions, allowing good transmission of voice and data from over any point on the globe.
An aircraft cabin at 37,000 feet (11,278 m) is a remote location in terms of the availability of medical support. Satcom can enable air-to-ground transmission of physiologic parameters such as pulse oximetry or electrocardiogram. This can assist the medical adviser to give appropriate advice to the aircraft captain, although the cost-benefit analysis of installing such equipment must be considered.
Aircraft Emergency Medical Equipment
National regulatory authorities stipulate the minimum scale of all equipment to be carried on aircraft operating under their jurisdiction, including the emergency medical kit (EMK) and associated equipment. The Federal Aviation Administration (FAA) requires an EMK for carriers operating under Part 121, when at least one flight attendant is required. European Aviation Safety Authority (EASA) requirements are similar. Many airlines carry considerably more than the minimum equipment.44
Resuscitation Equipment
Although basic cardiopulmonary resuscitation (CPR) techniques are an essential part of cabin crew training, the outcome of an in-flight cardiac event may be improved if appropriate resuscitation equipment is available.
The European Resuscitation Committee and the American Heart Association endorse the concept of early defibrillation for a cardiac event both in and out of the hospital setting. However, the protocol includes early transfer to an intensive care facility, which is not always possible in the flight environment. Despite this inability to complete the resuscitation chain, it has become increasingly common for commercial aircraft to be equipped with automatic external defibrillators (AEDs) and for the cabin crew to be trained in their use. This has been mandated in the United States by the FAA for all aircraft of air carriers operating under Part 121 with a maximum payload capacity of >7500 pounds and with at least one flight attendant.44
Some types of AEDs have a cardiac monitoring facility, and this can be of benefit in reaching the decision on whether to divert. For example, there is no point in initiating a diversion if the monitor shows asystole, or if the chest pain is unlikely to be cardiac in origin.
As well as meeting regulatory requirements, a cost-benefit analysis must balance the cost of acquisition, maintenance, and training against the probability of need and the expectation of the traveling public.
Lives have been saved using AEDs on aircraft, so it could be argued that the cost-benefit analysis is weighted in favor of carrying AEDs. Nonetheless, it is important that unrealistic expectations are not raised. An aircraft cabin is not an intensive care unit, and the AED forms only a part of the first-aid and resuscitation equipment.
The EMKs and AEDs are “no-go” items and must be carried as indicated on the “minimum equipment list.”
Many airlines have in place a procedure for the follow-up of crew members involved in a distressing event such as a serious medical emergency. This can be valuable in avoiding long-term posttraumatic stress disorder, and in reinforcing the training the crew member has undergone.
Conclusions
The pressurized aircraft cabin provides protection against the hostile environment encountered at cruising altitudes.
-
•
Although the partial pressure of oxygen is less than at sea level, it is more than adequate in a pressurized aircraft cabin for normal healthy individuals.
-
•
The cabin air, although dry, does not cause systemic dehydration and harm to health. However, dry skin and eyes can lead to discomfort, which can be alleviated using moisturizing creams and eye drops.
-
•
Although up to half of the air in modern pressurized aircraft is recirculated, the amount of fresh air available to each occupant exceeds that available in air-conditioned buildings. Recirculating the air has the advantage of reducing cold draughts and increasing humidity.
-
•
In modern aircraft, all the recirculated air is passed through HEPA filters, which remove >99% of particles, including bacteria and viruses.
-
•
There is an extremely low probability of airline passengers or crew suffering any abnormality or disease because of exposure to cosmic radiation.
-
•
Air travel continues to be a potential contributor to the spread of communicable diseases between and within countries, but the risk of transmission of serious infectious diseases during flight is low. Proper immunizations and routine hand hygiene practices are important preventive measures for air travelers.
The passenger cabin of a commercial airliner is designed to carry the maximum number of passengers in safety and comfort, within the constraints of cost effectiveness. It is incompatible with providing the facilities of an ambulance, an emergency room, an intensive care unit, a delivery suite, or a mortuary.
The ease and accessibility of air travel to a population of changing demographics inevitably means that there are those who wish to fly who may not cope with the hostile physical environment of the airport, or the hostile physiologic environment of the pressurized passenger cabin. It is important for medical professionals to be aware of the relevant factors, and for unrealistic public expectations to be avoided.
Most airlines have a medical adviser who may be consulted prior to flight to discuss the implications for an individual passenger. Such preflight notification can prevent the development of an in-flight medical emergency that is hazardous to the passenger concerned, inconvenient to fellow passengers, and expensive for the airline.
For those with disability, but not a medical problem, preflight notification of special needs and assistance will reduce the stress of the journey and enhance the standard of service delivered by the airline.
Finally, the importance of adequate medical insurance coverage for all travelers cannot be overemphasized.
References
- 1.Gradwell DP, Rainford DJ. 5th ed. CRC Press; 2016. Ernsting's aviation medicine. [Google Scholar]
- 2.https://www.ncbi.nlm.nih.gov/books/NBK207481/
- 3.Lorengo D, Porter A. 1986. Aircraft ventilation systems study. Final report. DTFA-03–84-C-0084. DOT/FAA/CT-TN86/41-I. Federal Aviation Administration, US Department of Transportation. September. [Google Scholar]
- 4.http://dspace.lib.cranfield.ac.uk/handle/1826/5305
- 5.www.nap.edu/catalog.php?record_id=10238 Pp. 180–1.
- 6.de Ree H, Bagshaw M, Simons R. Ozone and relative humidity in airliner cabins on polar routes: measurements and physical symptoms. In: Nagda NL, editor. Air quality and comfort in airliner cabins, ASTM STP 1393. American Society for Testing and Materials; West Conshocken, PA: 2000. pp. 243–258. [Google Scholar]
- 7.Nicholson AN. Dehydration and long haul flights. Travel Med Int. 1998;16:177–181. [Google Scholar]
- 8.Campbell RD, Bagshaw M. 3rd ed. Blackwell Science; 1999. Human performance and limitations in aviation. [Google Scholar]
- 9.Bagshaw M, Lower MC. Hearing loss on the flight deck – origin and remedy. Aeronaut J. 2002;106(1059):277–289. [Google Scholar]
- 10.FAA Federal Aviation Regulations (FARS, 14CFR); section 25.832.
- 11.Bagshaw M. Cosmic radiation measurements in airline service. Radiat Prot Dosim. 1999;86:333–334. [Google Scholar]
- 12.Valentin J, editor. The 2007 Recommendations of the International Commission on Radiological Protection, Publication 103, Ann. ICRP, Elsevier. [DOI] [PubMed]
- 13.Gratz NG, Steffen R, Cocksedge W. Why aircraft disinfection? Bull World Health Organ. 2000;78:995–1004. [PMC free article] [PubMed] [Google Scholar]
- 14.Report on the Informal Consultation on Aircraft Disinfection. World Health Organization; Geneva: 1995. http://whqlibdoc.who.int/hq/1995/WHO_PCS_95.51_Rev.pdf November 6-10; (WHO/PCS/ 95.51); Available at. [Google Scholar]
- 15.The Airliner Cabin Environment and the Health of Passengers and Crew. Report of the National Research Council. National Academy Press; Washington DC: 2001. December. [PubMed] [Google Scholar]
- 16.US Department of Health and Human Services Guidelines for environmental infection control in health-care facilities. 2003. http://www.cdc.gov/hicpac/pubs.html Available at.
- 17.Abubakar I. Tuberculosis and air travel: a systematic review and analysis of policy. Lancet Infect Dis. 2010;10:176–183. doi: 10.1016/S1473-3099(10)70028-1. [DOI] [PubMed] [Google Scholar]
- 18.Kornylo-Duong K, Kim C. Three air travel-related contact investigations associated with infectious tuberculosis. Travel Med Infect Dis. 2010;8:e120–8. doi: 10.1016/j.tmaid.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 19.Marienau KJ, Burgess GW. Tuberculosis investigations associated with air travel: U.S. Centers for Disease Control and Prevention. Travel Med Infect Dis. 2010;8:e104–12. doi: 10.1016/j.tmaid.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 20.Martinez L, Thomas K, Figueroa J. Guidance from WHO on the prevention and control of TB during air travel. Travel Med Infect Dis. 2010;8:84–89. doi: 10.1016/j.tmaid.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 21.Mangili A, Gendreau MA. Transmission of infectious diseases during commercial air travel. Lancet. 2005;365:989–996. doi: 10.1016/S0140-6736(05)71089-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dawood FS. Estimated global mortality associated with the first 12 months of 2009 pandemic influenza A H1N1 virus circulation: a modelling study. Lancet. 2012;12(9):687–695. doi: 10.1016/S1473-3099(12)70121-4. [DOI] [PubMed] [Google Scholar]
- 23.WHO Global Alert and Response. Confirmed Human Cases of Avian Influenza A(H5N1) 2011. http://www.who.int/influenza/human_animal_interface/en/ June 22; Available at.
- 24.Khan K, Arino J, Hu W. Spread of a novel influenza A (H1N1) virus via global airline transportation. NEJM. 2009;361:212–214. doi: 10.1056/NEJMc0904559. [DOI] [PubMed] [Google Scholar]
- 25.Baker MG, Thornley CN, Mills C. Transmission of pandemic A/H1N1 2009 influenza on passenger aircraft: retrospective cohort study. BMJ. 2010;340:c2424. doi: 10.1136/bmj.c2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huizer YL, Swaan CM. Usefulness and applicability of infectious disease control measures in air travel: A review. Travel Med Infect Dis. 2015;13:19. doi: 10.1016/j.tmaid.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 27.Communicable disease X (Ebola, MERS, TB, measles) coming soon to a neighborhood near you? Lessons learned about communicable disease and air travel. Editorial. Travel Med Infect Dis. 2015;13:3. doi: 10.1016/j.tmaid.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 28.Mukherjee P, Lim PL, Chow A. Epidemiology of travel-associated pandemic (H1N1) 2009 infection in 116 patients, Singapore. Emerg Infect Dis. 2010;16:22–26. doi: 10.3201/eid1601.091376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Amornkul PN, Takahashi H, Bogard AK. Low risk of measles transmission after exposure on an international airline flight. J Infect Dis. 2004;189:S81–5. doi: 10.1086/377698. [DOI] [PubMed] [Google Scholar]
- 30.CDC Notes from the field: multiple cases of measles after exposure during air travel – Australia and New Zealand, January 2011. MMWR Morb Mortal Wkly Rep. 2011;60(25):851. [PubMed] [Google Scholar]
- 31.Nelson K, Marienau K, Schembri C. Measles transmission during air travel, United States. Travel Med Infect Dis. 2013;11:81. doi: 10.1016/j.tmaid.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 32.Widdowson MA, Glass R, Monroe S. Probable transmission of norovirus on an airplane. JAMA. 2005;293(15):1859–1860. doi: 10.1001/jama.293.15.1859. [DOI] [PubMed] [Google Scholar]
- 33.Thornley CN, Emslie NA, Sprott TW. Recurring norovirus transmission on an airplane. Clin Infect Dis. 2011;53(6):515–520. doi: 10.1093/cid/cir465. [DOI] [PubMed] [Google Scholar]
- 34.Public health response to commercial airline travel of a person with Ebola virus infection—United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64(3):63–66. [PMC free article] [PubMed] [Google Scholar]
- 35.https://www.asma.org/publications/medical-publications-for-airline-travel
- 36.www.iata.org/publications/Pages/medical-manual.pdf
- 37.www.medaire.com
- 38.www.airsep.com
- 39.Bagshaw M, Byrne NJ. La sante des passagers. Urgence Pratique. 1999;36:37–43. [Google Scholar]
- 40.Donner HJ. Is there a doctor on board? Medical emergencies at 40K feet. Emerg Med Clin North Am. 2017;35(2):443–463. doi: 10.1016/j.emc.2017.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nable JV. In-flight medical emergencies during commercial travel. N Engl J Med. 2015;373(10):939–945. doi: 10.1056/NEJMra1409213. [DOI] [PubMed] [Google Scholar]
- 42.Peterson DC. Outcomes of medical emergencies on commercial flights. N Engl J Med. 2013;368:2075–2083. doi: 10.1056/NEJMoa1212052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bagshaw M. Telemedicine in British Airways. J Telemed Telecare. 1996;2(1):36–38. doi: 10.1258/1357633961929213. [DOI] [PubMed] [Google Scholar]
- 44.www.faa.gov/documentLibrary/media/Advisory_Circular/AC121-33B.pdf


