Some gastrointestinal (GI) problems (e.g., vomiting, diarrhea, weight loss, anorexia, icterus, hepatomegaly, abnormal behavior associated with eating, abdominal pain) typically necessitate laboratory testing. On the other hand, dysphagia, regurgitation, ptyalism, halitosis, constipation, mucoid stools, hematochezia, and melena are usually best approached initially by other means (e.g., physical examination, radiology, ultrasonography, endoscopy, laparotomy, and/or biopsy).
Differentiation of Expectoration, Regurgitation, and Vomiting
Whenever fluid, mucus, foam, food, or blood is expelled from the mouth, one must determine whether vomiting, regurgitation, gagging, or expectoration is occurring. The history sometimes allows differentiation.
Expectoration
Expectoration is the coughing up of material from the lungs or major airways. The material typically is frothy mucus or red blood; bile and food are absent. The characteristic sequence of coughing followed by oral expulsion must be determined from the history or observation. Regurgitation and vomiting typically occur without simultaneous coughing, although regurgitation is often accompanied by tracheitis and aspiration pneumonia. However, a patient that is expectorating may “gag” so hard because of pharyngeal/laryngeal irritation that it eventually vomits.
Regurgitation
Regurgitation is due to oral, pharyngeal, or esophageal dysfunction and is typically characterized as a relatively passive expulsion of esophageal contents. Gagging is the expulsion of oral or pharyngeal material and may be associated with disorders causing dysphagia (i.e., difficult swallowing) or regurgitation. The relatively minor abdominal contractions associated with gagging are typically different than the vigorous abdominal contractions that classically occur with vomiting. Regurgitation may follow seconds to hours after eating or drinking. Patients may regurgitate white foam (i.e., salivary secretions that have been swallowed) and/or food. Regurgitated food material is undigested and sometimes has a tubular form conforming to the shape of the esophageal lumen. Most clients cannot reliably distinguish undigested from digested food. Regurgitated material that has remained in the esophagus for long time periods can appear “partially digested” because it is macerated, odoriferous, and mixed with saliva. If blood is present, it is usually undigested (i.e., bright red), whereas blood originating from the stomach is usually partially digested by gastric acid and has a “coffee grounds” appearance readily distinguishing it from the undigested form (unless the patient vomits before the blood can be partially digested).
It is sometimes difficult to differentiate vomiting from regurgitation via history, and in some patients the processes are concurrent. Vomiting may cause secondary esophagitis and subsequent regurgitation, or a patient with long-standing esophageal disease may develop another concurrent disorder causing vomiting. It is therefore important to clarify the chronologic order of specific signs. Finally, some patients with signs “classic” for regurgitation are vomiting instead. To aid in differentiation, one may attempt to observe the act of expulsion by feeding the patient, although this is very unreliable (“watched” regurgitating patients often do not regurgitate). Watching the patient eat occasionally helps if there is obvious pharyngeal dysphagia that suggests oropharyngeal disease. Some patients with pharyngeal dysphagia also have concurrent esophageal dysfunction. Contrast radiographs and/or fluoroscopy of the pharynx and esophagus can usually differentiate vomiting from regurgitation.
Regurgitation is usually best evaluated by history, physical examination, plain and contrast radiographs, and/or esophagoscopy (Figure 9-1 ). Contrast radiographs should use barium instead of iodide contrast agents unless esophageal rupture is suspected (e.g., finding air or fluid in the mediastinum on plain radiographs). The main purpose of a contrast esophagram is to distinguish esophageal motility abnormalities from anatomic lesions (e.g., obstruction, mass, inflammation, fistula). Some drugs (e.g., xylazine, ketamine) can cause esophageal hypomotility, making the radiographs potentially misleading. Esophagoscopy is insensitive for diagnosing esophageal muscular weakness but sensitive for finding anatomic lesions, differentiating intramural from extramural obstruction, identifying esophagitis, and removing foreign objects. Patients with acquired esophageal weakness should be evaluated for myopathies, neuropathies, and myasthenia gravis (generalized or localized to the esophagus). Occasionally, hypoadrenocorticism, hyperkalemia, lead poisoning, Spirocerca lupi, and selected central nervous system (CNS) disorders (e.g., distemper, hydrocephalus) may be responsible. Generalized or localized myopathies and neuropathies have several causes (e.g., trauma, dermatomyositis, thymoma, botulism, tick paralysis, systemic lupus erythematosus, nutritional factors, toxoplasmosis, trypanosomiasis). Dysautonomia occurs in dogs and cats, causing generalized dysfunction of the autonomic nervous system producing esophageal hypomotility. It is important to detect underlying disorders so that one may treat the cause rather than just the symptoms. It is also wise to evaluate patients with unexpected esophageal foreign objects (e.g., a relatively small bolus of food) for partial obstructions (e.g., subclinical vascular ring anomaly, stricture).
FIGURE 9-1.

Diagnostic approach to chronic regurgitation in dogs and cats. ACTH, Adrenocorticotropic hormone; CBC, complete blood count; CNS, central nervous system; EMG, electromyogram.
Vomiting
Vomiting is a reflex act originating in the CNS that can be stimulated by various conditions. One must consider primary GI disease and non-GI disorders (e.g., metabolic, inflammatory, and toxic conditions) as causes of vomiting. Many vomiting patients have non-GI problems.
Vomiting is classically characterized by prodromal nausea (i.e., salivation, licking of lips) followed by retching or forceful abdominal contractions. Vomiting may occur any time after eating or drinking (seconds to hours). A patient may vomit food, water, fresh blood, or mucus that is indistinguishable from regurgitated material. Bile, partially digested blood (i.e., “coffee grounds”), or expelled material with a pH of 5 or less strongly suggests vomiting as opposed to regurgitation. Vomited duodenal contents may have a pH greater than or equal to 7 and are usually positive for bile. A urine dipstick with a pH indicator is useful in making pH determinations. A patient that has “dry heaves” is typically vomiting as opposed to regurgitating.
Vomiting patients are best divided into those with acute (<2 weeks) versus those with chronic (>2 weeks) vomiting. The most common categories of causes for each are listed in Box 9-1, Box 9-2 . Patients with acute vomiting often spontaneously resolve if they are supported by fluid therapy. A thorough history and physical examination are indicated first. Laboratory evaluation and/or imaging should be considered if the disease is severe or a serious disease (e.g., obstruction) is suspected. If vomiting persists, is progressive, or is attended by other clinical signs (e.g., polyuria-polydipsia [pu-pd], weight loss, icterus, painful abdomen, ascites, weakness, hematemesis), additional testing is indicated (Figure 9-2 ).
Box 9-1. Major Causes of Acute Vomiting in Dogs and Cats.
Motion Sickness
Acute Gastritis-Enteritis (various viral or bacterial agents or toxins)
Parvoviral enteritis (dogs and cats)
Hemorrhagic gastroenteritis
Parasites
Gastrointestinal (GI) Obstruction
Foreign body (obstructing or linear)
Intussusception
Diet
Overeating
Poor-quality or spoiled food
Food to which patient is allergic or intolerant
Acute Pancreatitis
Iatrogenic (Drugs)
Amoxicillin plus clavulanic acid
Chemotherapeutics (e.g., cisplatin, cyclophosphamide, doxorubicin)
Chloramphenicol
Digitalis
Erythromycin
Narcotics
Nitrofurantoin
Tetracyclines (including doxycycline)
Theophylline
Xylazine
Intoxication
Ethylene glycol
Mushrooms
Organophosphates
Pesticides (including herbicides, fungicides, etc.)
Box 9-2. Major Causes of Chronic Vomiting in Dogs and Cats.
Gastrointestinal Obstruction
Foreign objects (common)
Intussusception
Neoplasia (gastric or intestinal)
Pyloric stenosis (infrequent)
Gastric antral mucosal hyperplasia
Inflammatory infiltrates of the stomach or intestines (e.g., pythiosis, eosinophilic masses)
Chronic partial gastric volvulus (uncommon)
Hypomotility of stomach/intestines (physiologic obstruction) (uncommon)
Congenital structural abnormalities (rare)
Abdominal Inflammation
Pancreatitis (common)
Chronic enteritis (dietary-responsive or antibiotic-responsive) (common)
Gastrointestinal ulceration/erosion
Peritonitis (sterile or septic)
Inflammatory bowel disease
Chronic gastritis (infrequent)
Pharyngitis (caused by upper respiratory virus in cats) (rare)
Parasites (e.g., Physaloptera) (regionally important)
Systemic (extra–alimentary tract diseases) (common)
Hepatic disease/insufficiency (common)
Hypoadrenocorticism (uncommon but important)
Diabetic ketoacidosis (common)
Uremia (common)
Hypercalcemia (important)
Cholecystitis
Pyometra (common)
Feline hyperthyroidism (common)
Central nervous system (CNS) disease (e.g., “limbic epilepsy”, tumor, encephalitis, or increased intracranial pressure) (rare)
Psychotic or behavioral changes (rare)
FIGURE 9-2.

Diagnostic approach to chronic vomiting in a dog or cat that has been unresponsive to dietary change and anthelmintic therapy. ACTH, Adrenocorticotropic hormone; CBC, complete blood count.
Diet and Parasites
Diet and parasites commonly cause acute and chronic vomiting; hence, dietary change (to a bland or hypoallergenic diet), fecal examination, and broad-spectrum anthelmintic therapy (e.g., fenbendazole, pyrantel) are reasonable initial choices in patients not suspected of having a clinically important disease. Continued vomiting is an indication for laboratory tests or imaging.
Obstruction
Gastric or intestinal obstruction does not usually require clinicopathologic testing for diagnosis. A complete blood count (CBC) may suggest sepsis, disseminated intravascular coagulation (DIC), or severe blood loss. Renal function, electrolyte, and acid-base evaluations are recommended before anesthesia. One cannot reliably predict changes in these parameters even when the site of obstruction is known. Persistent and profuse loss of gastric contents from any cause may produce hypokalemic, hypochloremic metabolic alkalosis with aciduria. However, most patients with gastric vomiting are not alkalotic. Insignificant acid-base changes or metabolic acidosis due to dehydration are probably more common. Intestinal obstruction may cause acidosis due to loss of pancreatic bicarbonate, although some patients have a normal blood pH or a metabolic alkalosis if the obstruction is high in the duodenum.
Abdominal radiographs and ultrasound are the best initial tests. In otherwise occult cases, contrast radiographs may be necessary, in which case barium is preferred over iodide compounds unless intestinal rupture is suspected. Barium leakage into the abdomen causes peritonitis and requires vigorous abdominal lavage at the time of surgery (see Chapter 10).
Extra–alimentary Tract Disease
A serum chemistry profile should be obtained to help rule out hepatic disease (alanine aminotransferase [ALT], serum alkaline phosphatase [SAP], blood urea nitrogen [BUN], and albumin), hypoadrenocorticism (sodium and potassium), hypercalcemia (calcium and albumin), uremia (creatinine, BUN, and urinalysis), and diabetic ketoacidosis (glucose and urinalysis). Very young (i.e., <12 to 14 weeks of age) and very small (i.e., <3 kg) patients should undergo blood glucose monitoring to detect secondary hypoglycemia. More precise testing is occasionally required to diagnose these disorders (e.g., serum bile acids for hepatic insufficiency, adrenocorticotropic hormone [ACTH] stimulation test for hypoadrenocorticism). Other tests to consider are serum gastrin for gastrinoma, and serum thyroxine for feline hyperthyroidism.
Pancreatitis
Acute pancreatitis occurs commonly. Predisposing causes in dogs include hyperlipidemia, fatty meals, or obesity. Pancreatitis can occur in any dog, but middle-aged obese female dogs, schnauzers, and Yorkshire terriers seem to be predisposed. Vomiting may or may not be associated with eating, abdominal pain, fasting hyperlipidemia, bloody diarrhea, and, rarely, diffuse subcutaneous fat necrosis. On radiographic examination, a mass or indistinctness due to localized peritonitis may be visible in the cranial right abdominal quadrant. CBC, serum amylase, and serum lipase activities are insensitive and nonspecific; patients with pancreatitis can have almost any result on these tests. Increased ALT and SAP concentrations (as the result of the proximity of the pancreas to the liver and obstruction of the biliary duct) are common but insensitive and nonspecific. Mild to moderate hypocalcemia sometimes occurs. Abdominal ultrasonography can be very specific for canine pancreatitis, but its sensitivity depends upon operator skill and timing (i.e., ultrasound findings can change dramatically in a matter of hours). If a pancreatic mass is discovered during surgery, it must be biopsied; chronic pancreatitis can be grossly indistinguishable from pancreatic neoplasia. The canine immunoreactive pancreatic lipase (spec cPL) (IDEXX, Westbrook, ME) test is the most sensitive test for pancreatitis, but its specificity for clinically important disease is still being determined. Chronic pancreatitis may be presumptively diagnosed if one finds exocrine pancreatic insufficiency in a breed that is not affected by pancreatic acinar cell atrophy.
Pancreatitis is an important but difficult-to-diagnose disease in cats. Chronic pancreatitis in older cats sometimes occurs in conjunction with cholangiohepatitis and/or inflammatory bowel disease (IBD) (often referred to as a triaditis syndrome involving all three organs). Vomiting is not as prominent in feline pancreatitis as it is in canine pancreatitis. Feline trypsin-like immunoreactivity (fTLI) concentrations are increased in some patients. Abdominal ultrasonography is specific, but the sensitivity is uncertain. A pancreatic biopsy may be required for a definitive diagnosis. The feline immunoreactive pancreatic lipase (spec fPL) test appears to be useful in diagnosing pancreatitis. Feline pancreatitis occasionally is due to toxoplasmosis or to feline infectious peritonitis (FIP) (see Chapter 15).
Gastritis, Enteritis, and Colitis
Chronic enteritis, colitis, or gastritis can cause various degrees of vomiting and may require mucosal biopsy for diagnosis. Abdominal ultrasound is potentially specific and may delineate infiltrative or inflammatory intestinal patterns, but it is insensitive. If gastritis or enteritis is suspected or if the other major causes of chronic vomiting have been ruled out, gastric and intestinal mucosal biopsies via endoscopy or laparotomy may be helpful. Inflammatory bowel disease is an important cause of feline chronic vomiting. Duodenitis is also a significant cause of vomiting without diarrhea in dogs; therefore both gastric and intestinal biopsies should be performed. Finally, because 10% to 20% of patients with colitis vomit, it is sometimes helpful to perform endoscopy on the upper and lower intestinal tracts in patients (especially cats) with chronic vomiting. It is critical that good-quality mucosal tissue samples be taken and handled properly to avoid artifacts, which can render them nondiagnostic.
Hematemesis
Hematemesis is the vomiting of blood; it suggests GI ulceration/erosion, coagulopathy, or ingestion of blood. The vomitus may contain bright-red blood or digested blood that resembles coffee grounds. Administration of nonsteroidal anti-inflammatory drugs (especially concurrently with corticosteroids) is a major reason for canine ulceration. Hepatic failure, mast cell tumor, shock, submaximal exertion, and dexamethasone administration must also be considered. After these have been ruled out, endoscopy is indicated and allows diagnosis of ulceration (especially because of a foreign object, inflammatory disease, or neoplasia). Depending upon the particulars of the case, one may perform endoscopy or treat symptomatically.
Abdominal Inflammation
Septic or nonseptic peritonitis (or inflammation of any abdominal organ) may cause vomiting. Abdominocentesis or abdominal lavage (see Chapter 10) may be needed, especially if physical examination or abdominal imaging suggests abdominal fluid. Occult cases may require laparoscopy or exploratory surgery for diagnosis.
Amylase
Rare Indications
Used to diagnose pancreatitis, this test is no longer recommended.
Disadvantages
The test has poor sensitivity and specificity.
Drug Therapy That May Cause Hyperamylasemia
Some drugs occasionally cause pancreatitis (Box 9-3 ) and may cause hyperamylasemia. Corticosteroids sometimes increase serum amylase concentrations.
Box 9-3. Drugs that May Cause Acute Pancreatitis.
Asparaginase
Azathioprine
Clomipramine
Furosemide
N-methylglucamine
Metronidazole
Potassium bromide (unproven association)
Salicylazosulfapyridine (Azulfidine)
Sulfonamides
Tetracycline
Thiazide diuretics
NOTE: These drugs do not reliably cause pancreatitis, and a history of administration of one of these drugs plus signs of pancreatitis cannot be assumed to be cause and effect. A patient with acute pancreatitis that is receiving one of these drugs, however, should undergo drug withdrawal, if possible.
Causes of Hypoamylasemia
Insignificant.
Causes of Hyperamylasemia
Decreased glomerular filtration (i.e., azotemia) and pancreatitis are causes of hyperamylasemia. Patients with pancreatitis may have normal to markedly increased values. Intestinal disease, ruptured intestines, and hepatic disease can increase serum amylase.
Causes of Increased Fluid Amylase
When abdominal fluid amylase is greater than serum amylase concentrations, pancreatic disease is possible. Bowel rupture is also possible.
Lipase
Rare Indications
Used to diagnose pancreatitis, the test is not recommended.
Disadvantages
The test has poor sensitivity and specificity. Duodenal foreign objects, chronic gastritis, and abdominal carcinomas sometimes cause increased serum lipase activity.
Drug Therapy That May Cause Hyperlipasemia
Drugs causing pancreatitis and hyperlipasemia are the same as for amylase (see Box 9-3) plus heparin. Corticosteroids (dexamethasone) may increase serum lipase activity without histologic evidence of acute pancreatitis.
Causes of Hypolipasemia
Not significant.
Causes of Hyperlipasemia
Causes of hyperlipasemia are similar to the causes of hyperamylasemia. Renal dysfunction increases serum lipase. Not all patients with acute pancreatitis have increased serum lipase, and the increase in serum lipase activity is not proportional to the severity of the pancreatitis. Extremely increased lipase values are sometimes caused by pancreatic carcinomas.
Canine Immunoreactive Pancreatic Lipase (Spec cPL)
Common Indications
Measurement of spec cPL is indicated in patients with vomiting, abdominal pain, nonseptic inflammatory abdominal exudate, icterus, or a prior history of pancreatitis.
Advantages
The spec cPL is the most sensitive test for pancreatitis. It only requires a serum sample and can be run in house when using SNAP technology (IDEXX, Westbrook, ME).
Disadvantages
Specificity for clinically important pancreatic lesions (as opposed to pancreatic lesions that are not causing clinical disease) is currently unknown.
Analysis
The spec cPL is measured in serum by enzyme-linked immunosorbent assay (ELISA).
Normal Values
Less than 200 µg/L is normal.
Artifacts
Uncertain.
Causes of Decreased Values
Exocrine pancreatic insufficiency (EPI) or isolated pancreatic lipase deficiency may decrease spec cPL. More overlap exists between normal dogs and dogs with EPI than exists for serum trypsin-like immunoreactivity (TLI) concentration. TLI is the test of choice for EPI. Because the spec cPL test is so sensitive, a negative result strongly suggests that acute pancreatitis is not present, and the clinician should look elsewhere for the cause of the vomiting.
Causes of Increased Values
Values greater than 400 µg/L are consistent with and suggestive of pancreatic inflammation or necrosis. It is currently unclear whether all microscopic pancreatic lesions (i.e., inflammation, necrosis) that are associated with a high spec cPL are clinically important.
Feline Immunoreactive Pancreatic Lipase (Spec fPL)
Common Indications
Indications for measurement of spec fPL are cats suspected of having pancreatitis and those with vague clinical signs (e.g., unexplained anorexia, abdominal discomfort, unexplained weight loss) that remain undiagnosed despite testing.
Advantages
The spec fPL is the most sensitive test for feline pancreatitis.
Disadvantages
The spec fPL has uncertain specificity for clinically important pancreatic disease.
Analysis
The spec fPL is measured in serum by ELISA.
Normal Values
Less than 3.5 µg/L.
Artifacts
None known.
Drug Therapy That May Alter spec fPL
None known, but any drug that can cause pancreatitis may increase the spec fPL.
Causes of Decreased Values
Uncertain, but EPI might be a cause.
Causes of Increased Values
Values greater than 5.4 µg/L are consistent with and suggestive of pancreatitis.
Gastrin
Occasional Indications
Measurement of gastrin is indicated in cases of chronic vomiting, diarrhea, weight loss, suspected gastrinoma, or gastric or duodenal ulceration of unknown cause. This test is usually not requested until more common diseases have been ruled out.
Advantages
The test detects otherwise occult gastrinomas.
Disadvantages
The sample requires careful handling (i.e., rapid harvesting of serum and freezing if analysis is delayed).
Analysis
Gastrin is measured in serum by radioimmunoassay (RIA).
Normal Values
Depends on laboratory (the assay must be validated for the species). To convert pg/ml to ng/L, multiply pg/ml × 1.0 = ng/L.
Artifacts
Gastrin may be falsely decreased by hormone degradation as the result of sample storage for several days at temperatures above freezing.
Drug Therapy That May Increase Gastrin
Antacids, including histamine2 (H2) receptor antagonist drugs and proton pump inhibitors, may increase gastrin concentration.
Causes of Hypogastrinemia
Not significant.
Causes of Hypergastrinemia
Atrophic gastritis (uncommon), antral G-cell hyperplasia (rare), short bowel syndrome, hyperparathyroidism, gastric ulcers, gastric outlet obstruction, renal failure, and gastrinoma may cause hypergastrinemia; the last four are probably the most common. If gastrinoma is suspected in a patient that has a normal or equivocal serum gastrin concentration, secretin or calcium stimulation tests may be performed. A rise in the serum gastrin concentration after giving either of these drugs suggests a gastrinoma.
Acute Diarrhea
Patients with diarrhea are best classified into those with acute (<2 to 3 weeks) versus those with chronic (>2 to 3 weeks) diarrhea. Acute diarrhea (Box 9-4 ) is usually self-limiting, although some conditions may be severe and cause mortality (e.g., acute hemorrhagic gastroenteritis, parvoviral disease, hookworms, intoxication). History should explore the possibility of recent dietary change and exposure to infectious agents. Diet, bacteria, viruses, and parasites are the major identifiable causes of acute diarrhea in dogs and cats. Because intestinal parasites may contribute to any diarrheic state, fecal examinations (direct and flotation) are typically warranted in diarrheic patients. Giardiasis may require special diagnostic techniques (see Fecal Giardia Detection later in this chapter). The need for diagnostics depends upon (1) the severity of the problem (i.e., more severely ill patients require more diagnostics), and (2) the likelihood that the patient has an infectious agent that has potential to be nosocomial or zoonotic.
Box 9-4. Major Categories of Causes of Acute Diarrhea in Dogs and Cats.
Intestinal Parasites (common)
Hookworms
Roundworms
Whipworms (primarily dogs)
Coccidia
Giardia (sometimes difficult to diagnose)
Strongyloides
Tritrichomonas (primarily cats)
Diet (common)
Poor-quality food/food poisoning
Sudden dietary change (especially young animals)
Food intolerance/allergy
Acute Viral or Bacterial Enteritis
Parvovirus (canine and feline) (common)
Coronavirus (canine and feline)
Clostridium perfringens (common)
Campylobacteriosis (rare)
Salmonellosis (rare)
Escherichia coli (suspected, but not proven)
Intussusception
Intoxication
Garbage
Food poisoning
Heavy metal
Organophosphate
Hemorrhagic Gastroenteritis
Feeding bland or elimination diets may be diagnostic and therapeutic. Depressed, weak, and dehydrated patients should undergo electrolyte and acid-base evaluations to aid in selecting fluid replacement therapy. All patients less than 12 to 14 weeks of age and those that are emaciated or weighing less than 3 kg should undergo blood glucose monitoring to detect secondary hypoglycemia. CBC is indicated in most febrile or severely depressed patients so that sepsis or transmural inflammation can be detected. Fecal cultures, ELISA, and/or polymerase chain reaction (PCR) for Salmonella spp., Campylobacter jejuni, Yersinia enterocolitica, verotoxin-positive Escherichia coli, Clostridium perfringens, or Clostridium difficile may be performed, but establishing a cause-and-effect relationship between the organism and disease can be difficult.
Not all patients with canine parvoviral diarrhea are severely ill, diarrheic, febrile, or have identifiable leukopenia. Leukopenia may only persist 24 to 36 hours and be missed if a CBC is not performed during that period. Other diseases causing severe sepsis (i.e., perforating linear foreign body with peritonitis or overwhelming salmonellosis) can cause leukopenia indistinguishable from that of canine parvoviral enteritis. Routinely used vaccination schedules do not necessarily guarantee protection against canine parvovirus. In-house ELISA tests for parvovirus performed on feces appear to be specific for parvoviral antigen, but testing may be negative if done too early or too late. Fecal shedding of viral particles may not occur for 1 to 3 days after signs begin and decreases rapidly with time. The test result should be strongly positive within 3 days of the onset of clinical signs and remain positive for several days. A recent vaccination may result in a weakly positive fecal ELISA.
Chronic Diarrhea
Chronic diarrhea should first be defined as either small intestinal or large intestinal in origin (Table 9-1 ). Occasionally, large and small intestines are concurrently involved. Patients with chronic diarrhea in which clinical disease is not severe are often treated with therapeutic trials before aggressive diagnostics are instituted. The specifics of the therapeutic trials are influenced by whether the patient has large or small bowel disease. Patients should usually have at least three fecal examinations at 48-hour intervals. If these tests are negative, it is still acceptable (depending upon the risk of parasites in the geographic location) to treat empirically for Giardia infection and whipworms before aggressive diagnostics are begun. Giardiasis may be particularly difficult to diagnose (see Fecal Giardia Detection later in this chapter). Adverse food reactions (i.e., allergy, intolerance, fiber deficiency) commonly cause chronic diarrhea. Dietary intolerances are a reaction to a particular substance in the diet, whereas true food allergies are immunologic reactions to specific antigens. Dietary food trials are indicated in suspected cases. There are antibiotic-responsive intestinal diseases that are also treated empirically; however, the specific therapy varies with whether the patient has large or small bowel disease (see next section). Failing to respond to empirical anthelmintic, dietary, and antibacterial therapy indicates the need for further diagnostics.
TABLE 9-1.
DIFFERENTIATION OF CHRONIC SMALL INTESTINAL DIARRHEA FROM CHRONIC LARGE INTESTINAL DIARRHEA
| SMALL INTESTINAL DIARRHEA | LARGE INTESTINAL DIARRHEA | |
|---|---|---|
| Weight loss (very important criterion) | Expected | Uncommon except with severe disease (e.g., histoplasmosis, pythiosis, or cancer) |
| Polyphagia | Often present | Uncommon |
| Vomiting | May occur | Occurs in 10%–20% of patients |
| Volume of feces | May be normal or larger than normal | May be normal or smaller than normal |
| Frequency of defecation | Normal to slightly increased | Normal to markedly increased, may have many small defecations per bowel movement |
| Slate-gray feces (steatorrhea) | Rare | No |
| Hematochezia | No | Sometimes |
| Melena | Rare | No |
| Mucoid stools | Rare (unless ileum is diseased) | Often present |
| Tenesmus/dyschezia | Rare | Sometimes |
Large Intestinal Disease
Large intestinal disease has different parasites (i.e., Trichuris vulpis, Tritrichomonas fetus), dietary problems (i.e., fiber-responsive diarrhea), and bacterial problems (i.e., so-called clostridial colitis that responds best to tylosin or amoxicillin) than small bowel disease. Once parasitic, dietary, and “clostridial colitis” are eliminated by diagnostics and therapeutic trials, additional diagnostic steps, such as rectal mucosal scrapings (not swabs) with cytologic examination (Figure 9-3 ) might be appropriate. Persistent large intestinal disease that fails to respond to these therapeutic trials or that is associated with hypoalbuminemia or obvious weight loss is usually an indication for abdominal ultrasound followed by fine-needle aspiration and/or colonoscopy-ileoscopy plus biopsy. Rigid colonoscopy of the descending colon is adequate for diagnosis in most cases. Flexible endoscopy allows access to the descending, transverse, and ascending colon; ileocolic valve; cecum; and ileum. If flexible endoscopy is unavailable, abdominal ultrasonography may reveal lesions in areas not accessible with rigid endoscopy.
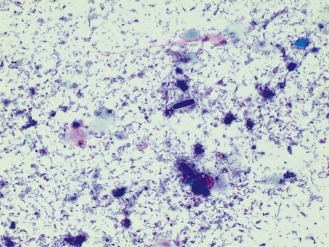
FIGURE 9-3.

A, A canine rectal scraping showing a macrophage with numerous engulfed yeasts. These are Histoplasma capsulatum.B, A canine rectal scraping that shows inflammatory cells and spherical organisms with a clear halo. The organisms are Prototheca.
(Courtesy of Dr. Rick Cowell.)
Small Intestinal Disease
Small intestinal disease has different parasites (e.g., Giardia), dietary problems (e.g., lymphangiectasia), and bacterial problems (i.e., so-called antibiotic-responsive enteropathy [ARE] or dysbiosis that may respond to a variety of antibacterials) than large bowel disease. Chronic and severe small intestinal diarrhea necessitates differentiation of maldigestion, protein-losing enteropathy (PLE), and malabsorptive disease without protein loss (Figure 9-4 ). Weight loss and diarrhea are usually present, but some patients only have weight loss.
FIGURE 9-4.

Diagnostic approach to chronic diarrhea in dogs and cats in which multiple fecal examination results are negative and empirical anthelmintic, antiprotozoal, and dietary therapy do not resolve the diarrhea. CBC, Complete blood count; ELISA, enzyme-linked immunosorbent assay; EPI, exocrine pancreatic insufficiency; PCR, polymerase chain reaction; TLI, trypsin-like immunoreactivity.
Maldigestion
Maldigestion due to bile acid insufficiency caused by biliary obstruction is rare. Intestinal lactase deficiency is uncommon, but a lactose-free diet may be tried in selected patients (especially cats). EPI is the principal cause of maldigestion but is rare in cats. Differentiation of EPI from malabsorptive intestinal disease is important. EPI is often overlooked in afflicted dogs or may erroneously be diagnosed in patients without the malady. Clinical trials using pancreatic enzyme preparations are very insensitive and nonspecific. Powdered enzyme is often superior to tablet formulations, and some enzyme preparations are clearly superior to others. Some dogs with EPI also require a low-fat diet, antacid therapy (rare), or treatment for concurrent ARE (common) before the enzyme replacement therapy becomes effective, even when appropriate enzymes are administered. Up to 15% of dogs with EPI never respond to therapy. Too often, failure of empirical enzyme replacement therapy leads to unnecessary tests (i.e., biopsy) because EPI was incorrectly eliminated. No consistent hematologic or serum chemistry profile changes are seen. Undigested fats can often be found in the feces; however, this is inconsistent. The fat absorption test yields many false results. The TLI assay is the standard test for EPI. It is important to note that the TLI tests are species specific. Measurement of fecal proteolytic activity is often accurate for diagnosing EPI; however, it is more cumbersome and has limited availability.
Malabsorptive Disease Without Protein Loss
Once maldigestion has been eliminated, malabsorption becomes the most likely diagnosis in diarrheic animals with weight loss. One must then decide whether to perform diagnostic therapeutic trials or diagnostic tests. Patients that are emaciated, have serum albumin less than 2.1 g/dl, or are progressing rapidly should usually next undergo abdominal ultrasonography and intestinal biopsies (preferably via endoscopy unless ultrasonography shows lesions that cannot be diagnosed endoscopically or that can be aspirated with ultrasound guidance). Patients that are not critically ill may first receive carefully designed therapeutic trials. Therapeutic trials may be chosen more rationally with the aid of minimal laboratory data (e.g., biochemical profile, fecal examinations). The two major therapeutic trials are (1) food trials for dietary-responsive diease (i.e., elimination diets) and (2) antibacterial trials for ARE or dysbiosis.
ARE (previously called “small intestinal bacterial overgrowth” or SIBO; now sometimes called dysbiosis) may exist by itself or coexist with another GI malady. No consistent CBC or serum chemistry profile changes are seen in this syndrome. Fecal culture is not informative, and ultrasound and intestinal biopsy are seldom diagnostic. A barium contrast study very rarely identifies a segmental lesion or partial obstruction responsible for secondary ARE. Quantitated culture of duodenal or proximal jejunal fluid for aerobes and anaerobes is difficult to interpret, because clinically normal dogs may have as many as or more bacteria than clinically affected dogs. Serum cobalamin and folate concentrations are insensitive and nonspecific for ARE. Dogs with ARE usually respond within 3 to 4 weeks to appropriate antibacterial therapy (e.g., tetracycline, tylosin, metronidazole ± enrofloxacin), usually combined with a high-quality elimination diet unless irreversible mucosal changes or primary underlying intestinal disease are present.
Dietary intolerance is relatively common, and elimination diets (e.g., fish and potato, turkey and potato, tofu and beans, hydrolyzed) are reasonable trials. At least 3 and preferably 4 weeks should be allotted for such a dietary trial, during which time absolutely nothing else should be fed (including flavored treats or medications).
If dietary, antibiotic, and repeated anthelmintic and antiprotozoal therapies are ineffective, ultrasonography followed by small intestinal biopsy is probably necessary. Ultrasonography is done to look for lesions that can be aspirated (thus avoiding the need for anesthesia and biopsy) and to ensure that endoscopy can reach the lesion. In most patients, the stomach, duodenum, ileum, and colon may be endoscopically sampled. Duodenal cytology is helpful in some disorders (e.g., eosinophilic enteritis, purulent enteritis, giardiasis, lymphoma). If laparotomy is performed, multiple representative full-thickness specimens (e.g., stomach, duodenum, jejunum, ileum, mesenteric lymph node) are indicated, because lesions can be spotty, even in severely affected patients. If endoscopy is performed, multiple high-quality tissue samples (e.g., ≥6 to 8) from each site are obtained. It is critical that the endoscopist be accomplished and trained in obtaining high-quality tissue samples. Many endoscopically obtained tissue samples are nondiagnostic because of the operator's lack of training.
Protein-Losing Enteropathy
PLE is uncommon in cats but seen with some regularity in dogs. PLEs are classically described as causing panhypoproteinemia. However dogs with diseases causing hyperglobulinemia (e.g., chronic skin disease, rickettsial disease, heartworm disease) and some breeds (e.g., basenji dogs) may have only hypoalbuminemia because the serum globulin concentration is initially increased, and even though much of this fraction is lost into the intestines, the amount remaining in the blood keeps concentrations in the normal range. If red blood cells (RBCs) are also being lost, iron deficiency anemia may occur (see Chapter 3).
PLE may be the result of various GI diseases (e.g., hookworms, chronic intussusception, fungal infections, ulcers and erosions), but lymphangiectasia, alimentary lymphosarcoma, ARE, and IBD seemingly are the most common causes in adult dogs. Intestinal lymphangiectasia produces some of the lowest serum albumin concentrations that occur in alimentary disease (e.g., <1.0 g/dl). Hypocholesterolemia is common, and peripheral lymphocyte counts occasionally are decreased. If hepatic insufficiency and loss from the kidneys and skin have been eliminated in a severely hypoalbuminemic patient, PLE becomes the major differential diagnosis by process of elimination. If PLE is suspected in a patient that has another potential explanation for its hypoalbuminemia (e.g., renal protein loss, hepatic insufficiency, severe exudative skin disease), then measuring fecal alpha1-protease inhibitor concentrations may clarify whether or not excessive GI protein loss is occurring. Alpha1-protease is relatively stable and resistant to GI degradation; consequently, it can be measured in the feces. Intestinal biopsy is usually the definitive test for determining the cause of PLE. Full-thickness biopsy may risk dehiscence if the serum albumin level is less than 1.5 g/dl; serosal patch graft techniques decrease the risk of dehiscence. Gastroduodenoscopy-ileoscopy plus biopsy is relatively safe and often diagnostic. Occasionally the intestinal lesion is inaccessible via endoscopy. Although not recommended, dietary trial with an ultra-low-fat diet may be substituted for biopsy in patients suspected of having lymphangiectasia. Therapeutic trials with steroids without a definitive diagnosis can be potentially dangerous (especially in dogs) and are not recommended.
Fecal Character
Mucoid feces should be approached as a large intestinal or a distal small intestinal problem. In dogs and cats with large bowel disease but no weight loss or hypoalbuminemia, multiple fecal examinations, digital rectal examination, and therapeutic trials (i.e., dietary, antibacterial and/or anthelmintic) are often the best initial steps. If these are unsuccessful, then colonoscopy-ileoscopy plus biopsy generally becomes the most useful diagnostic tool. Hematochezia should also be considered as a large bowel problem. Melena signifies swallowed blood from any source, coagulopathy, or gastric and upper intestinal bleeding. Therefore before performing an exploratory laparotomy, one should consider all the possible causes of ingesting blood (e.g., coughing up blood from the respiratory tract, posterior nasal bleeding). Ingestion of bismuth subsalicylate or liver can cause feces to appear melenic. Diet and changes in intestinal bacterial flora influence fecal color but do not generally signify disease.
Fecal Enzyme-Linked Immunosorbent Assay for Parvovirus
Occasional Indications
A fecal ELISA for parvovirus is indicated in dogs suspected of having parvoviral enteritis (especially those not displaying classic signs), or in acute neutropenia of unknown cause. The test can be used in cats to diagnose panleukopenia caused by canine parvovirus 2a and 2b.
Advantages
The test is quick and available, and has good sensitivity and specificity if done at the appropriate time (e.g., approximately 1 to 3 days after onset of clinical signs).
Disadvantages
Dogs with parvoviral enteritis can have negative reactions, especially very early or very late in the course of the disease.
Analysis
Fresh feces are used according to kit instructions (see Chapter 15). The instructions must be carefully followed or false results might be obtained.
Normal Values
Dogs should be negative for fecal parvoviral antigen.
Interpretation
A positive result supports canine parvoviral enteritis. Not all dogs affected with parvoviral enteritis have diarrhea and fever; some show only anorexia, vomiting, or fever. Theoretically, if coproantibody binds all of the antigen in the feces, a false-negative result may occur. If the test is performed too early in the disease, it may yield negative results. With such dogs, one should repeat the test in 36 to 48 hours. Shedding of viral particles decreases after the first week of disease, and a test performed too late in the disease might yield negative results. Modified-live virus vaccination results in transient fecal shedding and can give a weak positive fecal ELISA test result (5 to 15 days after vaccination).
Fecal Analysis for Clostridium Perfringens
Occasional Indications
Fecal analysis for C. perfringens is occasionally indicated in dogs with acute, nosocomial diarrhea or chronic large bowel diarrhea of unknown cause.
Disadvantages
The test has uncertain sensitivity and specificity for C. perfringens–associated disease. Presence of toxin does not mean the patient has disease due to that toxin. Conversely, absence of toxin does not guarantee the patient is not diseased because of the bacteria producing the toxin. Animals may be toxin-positive and not have diarrhea, and dogs with toxin-negative diarrhea may respond to antibiotics. Old fecal samples might yield false-positive results.
Analysis
Fresh or frozen feces are used according to the instructions on the test kit. Reverse passive latex agglutination (RPLA) (i.e., PET-RPLA Toxin detection kit; OxoidLimited, Cambridge, UK) and ELISA (i.e., C. perfringens Enterotoxin Test; TechLab, Blacksburg, VA) methods are available for C. perfringens enterotoxin.
Interpretation
Results from ELISA methodology appear to correlate better with disease than do results from RPLA methodology. Finding C. perfringens enterotoxin in feces plus clinical signs consistent with clostridial diarrhea has been considered diagnostic. However, enterotoxin cannot be found in all patients responding to tylosin or amoxicillin therapy. In suspected cases with a negative toxin assay, one may repeat the test again at the onset of recurrence of clinical signs or perform a therapeutic trial with amoxicillin or tylosin.
Fecal spore counts do not correlate well with C. perfringens enterotoxin production or with the presence of diarrhea. Examining fecal smears (see Fecal Microscopic Cytology later in this chapter) to look for the presence of spores is not an acceptable screening procedure.
Fecal Analysis for Clostridium Difficile
Occasional Indications
The importance of C. difficile in small animal medicine is unknown. The test seems most appropriate for suspected nosocomial or antibiotic-associated diarrheas.
Advantages
The ELISA for C. difficile antigen is very sensitive and has excellent negative predictive value. The ELISA for C. difficile toxin is thought to be specific, but of uncertain sensitivity.
Disadvantages
Interpretation is not simply based upon positive/negative test results. Presence of toxin does not mean the patient has disease due to that toxin. Conversely, absence of toxin does not guarantee the patient is not diseased because of C. difficile. Animals may be toxin-positive and not have diarrhea, and dogs with toxin-negative diarrhea may respond to appropriate antibacterials.
Analysis
ELISA methodology is available to look for C. difficile toxin A (ImmunoCard Toxin A; Meridan Diagnostics, Cincinnati, OH).
Drug Therapy That May Alter Analysis
Unknown.
Interpretation
The best approach is to first check for the presence of bacteria using the ELISA for the bacterial antigen. If the test is negative, then it is very unlikely that C. difficile is present. If the ELISA for the bacterial antigen is positive, then one should test for the toxin using an ELISA that detects both A and B toxin. Finding C. difficile toxin A in feces of diarrheic patients seems suggestive of a cause-and-effect relationship. However, the importance of C. difficile in canine and feline medicine and any risk it may have for people is currently not understood.
Fecal Culture
Rare Indications
Fecal culture is rarely indicated for dogs and cats with diarrhea (especially large bowel) that appears to be nosocomial, is potentially infectious (e.g., fever, leukocytosis, neutrophilic fecal cytology), or is suspected of being due to a specific infectious agent (i.e., Salmonella spp., C. jejuni, verotoxin-positive E. coli, and Y. enterocolitica). Nonculture techniques looking at DNA are probably more useful but are generally limited to research laboratories.
Disadvantages
The clinician must specify which pathogen(s) to culture for and must provide the laboratory with fresh feces or feces submitted in appropriate transport media. Testing requires a microbiology laboratory familiar with the specific enrichment and isolation techniques for each pathogen. Using culture swabs is not adequate for isolation of most enteric pathogens. Finally, growing a “pathogen” does not mean that it is responsible for clinical signs.
Analysis
Fresh feces must be promptly submitted to the laboratory, and the laboratory must know the specific pathogen(s) sought. To submit old feces or feces that have not been collected or handled properly or to request a “general culture for pathogens” is generally a waste of time and money. It requires laboratories that are properly equipped to culture for enteric pathogens. Culture for C. perfringens is not helpful diagnostically.
Interpretation
Any clinically normal animal may have any of the pathogens listed earlier cultured from its feces, although Y. enterocolitica is particularly uncommon in the United States. Interpretation of the fecal culture must consider the history, physical examination, laboratory data, and sometimes numbers of organisms (i.e., number of bacterial colony-forming units per gram of feces) found.
Fecal Fat
Rare Indications
Fecal fat testing may be used to detect malabsorption or maldigestion in animals with diarrhea or unexplained weight loss.
Advantages (Semiqualitative Analysis)
Fecal fat has minimal expense, availability, and reasonable accuracy as a screening test.
Disadvantages (Semiqualitative Analysis)
The test occasionally produces misleading results.
Analysis
The clinician performs a semiqualitative analysis for undigested fats by mixing a drop of fresh feces with a drop of Sudan III, heating the slide to a boil, and examining the smear microscopically. The clinician performs analysis for digested fats by mixing one drop of fresh feces, one drop of 36% acetic acid, and one drop of Sudan III. This is put on a microscope slide, heated to boiling, and examined while still warm. In both cases, identifying orange droplets is a positive finding. It is important that the patient has been eating a moderate- to high-fat diet. Feeding low-fat diets to malabsorptive dogs may cause the test result to be negative.
Normal Values
Semiqualitative: few or no undigested and digested fat globules per high-power field (hpf).
Artifacts
The semiqualitative analysis may have unexplained false-negative and false-positive reactions. Administration of barium sulfate, bismuth, psyllium fiber, mineral oil, or castor oil or feeding a low-fat diet may also confuse semiqualitative analysis.
Causes of Increased Fecal Fat
Finding several orange globules/hpf, if repeatable on several examinations, is principally caused by malabsorption or maldigestion. It is a reasonable screening test and helps distinguish EPI (positive for undigested fats) from malabsorption (positive for digested fats). Despite occasional false-positive reactions, strongly positive results for undigested fecal fat in a dog with signs consistent with maldigestion are an indication for TLI. Fecal fat may not be detectable in some dogs with EPI.
Fecal Proteolytic Activity
This test was used to detect maldigestion in animals with chronic diarrhea or weight loss of unknown cause. Theoretically it may diagnose EPI in rare patients that have EPI secondary to obstruction of the pancreatic duct or ducts. However, the radiograph film digestion test is useless and should never be used. The most reliable procedure for measuring fecal proteolytic activity is difficult to perform and requires special handling of the feces; it is described in prior editions. The TLI test is the test of choice for EPI.
Fecal Alpha-1 Protease Inhibitor Activity
Infrequent Indications
Hypoalbuminemia of uncertain cause or suspected PLE in a patient with concurrent hepatic insufficiency or protein loss from the kidneys or skin are indications for testing fecal alpha-1 protease inhibitor activity.
Advantages
The test can define the GI tract as the source of protein loss. Alpha-1 protease inhibitor is a plasma protein. If it leaks into the intestinal lumen, it resists GI degradation and hence can be measured in the feces.
Disadvantages
The test has limited availability. The magnitude of alpha-1 protease inhibitor in the feces is variable and may not reflect the severity of the disease.
Analysis
Three 1-g fecal samples from three different bowel movements are submitted in tubes provided by the laboratory. It is critically important that three samples (preferably from different days or at least different bowel movements) be submitted, that the feces be collected promptly after defecation, and that the feces not be collected by digitally removing them from the rectum. Samples must be frozen while one awaits shipping and must be shipped on a cold pack. Currently the only laboratory offering this test is GI Laboratory, College of Veterinary Medicine, Texas A&M University, College Station, TX 77843-4474.
Normal Values
0.23 to 5.67 µg/g feces. The clinician must look at individual values and the mean of all three values.
Causes of Abnormalities
Abnormally high values in the feces indicate loss of serum proteins into the alimentary tract and might indicate that PLE is the cause of hypoalbuminemia. Interpretation of the magnitude of the loss is as per the laboratory.
Fecal Microscopic Cytology
Rare Indications
Fecal microscopic cytology is rarely indicated in cases of large or small intestinal diarrhea.
Advantages
The test is widely available and easy to perform.
Disadvantages
The test has poor sensitivity and variable specificity for different agents.
Analysis
Thin, air-dried, fresh fecal smears are stained with new methylene blue (NMB) or Wright stain and examined using high-power and oil immersion microscopy. Rectal and colonic mucosal scrapings obtained with a curette are also a means of examining mucosal cells.
Normal Values
A mixed population of rod and cocci bacteria, few bacterial spores or yeast, occasional epithelial cells and amorphous debris.
Artifacts
Old fecal samples may alter results (white blood cells [WBCs] do not remain identifiable in feces for long time periods, and the bacterial population changes and bacterial spores may increase). Fecal debris may resemble degenerate WBCs.
Drug Therapy That May Alter Fecal Microscopic Cytology
Administration of barium and psyllium fiber may make interpretation difficult, and antibiotics change bacterial flora composition.
Interpretation
Fecal WBCs (specifically neutrophils) can be observed with bacterial (e.g., salmonellosis, campylobacteriosis) and inflammatory mucosal disease. Transmural colitides occasionally have increased fecal WBCs. Fecal WBCs can be an indication to biopsy colonic mucosa in patients with chronic colitis. Eosinophils may sometimes be seen with allergic or parasitic colitis. Increased numbers of yeast or a uniform population of bacteria may help identify the cause of diarrhea in a patient, but the mere presence of an organism (e.g., Cyniclomyces guttulatus [Figure 9-5 ]) does not ensure that it is causing disease.
FIGURE 9-5.
Cytology of a fecal smear showing large yeast bodies (i.e., Cyniclomyces guttulatus).
Fecal Occult Blood
Rare Indications
A fecal occult blood test may be used to detect GI bleeding that is not grossly apparent.
Disadvantages
See Artifacts.
Analysis
Fresh feces are smeared on a test pad. The patient must have been on a meat-free diet for at least 3 days before the feces are obtained. Sensitivity varies markedly between different assays.
Normal Values
See Artifacts.
Artifacts
Fecal occult blood results may be falsely decreased by sampling unmixed feces (blood may not be distributed homogeneously throughout the feces) and vitamin C supplementation. Results may be falsely increased by diets containing fresh meats (i.e., hemoglobin) or fresh uncooked vegetables (i.e., peroxidases), which cause a positive reaction.
Causes of Fecal Occult Blood
Bleeding into the GI tract at any level and as the result of any cause may result in fecal occult blood. GI blood loss of volumes of 2 ml blood/30 kg body weight will give positive results.
Fat Absorption Test
Rare Indications
A fat absorption test may be used to detect and distinguish maldigestion from malabsorption in chronic small intestinal diarrhea or unexplained weight loss. The test has many false-negative and false-positive results and is not recommended.
Analysis
The test is described in prior editions.
Trypsin-Like Immunoreactivity
Common Indications
TLI testing is indicated in patients with chronic small bowel diarrhea or unexplained weight loss.
Advantages
TLI has high sensitivity and specificity for EPI. The test only needs one serum sample that does not require special or cumbersome handling procedures.
Disadvantages
The test is species specific. Currently the only laboratory offering the fTLI test (for cats) is the GI Laboratory, College of Veterinary Medicine, Texas A&M University, College Station, TX 77843-4474.
Analysis
TLI is performed on serum using ELISA.
Normal Values
Dogs, 5 to 35 µg/L; cats, 12 to 82 µg/L.
Danger Values
None.
Artifacts
Theoretically, EPI caused by an obstructed pancreatic duct instead of acinar cell atrophy would yield a normal or even increased serum TLI value.
Drug Therapy That May Alter TLI
Drugs causing acute pancreatitis (see Box 9-3) might increase serum TLI. Oral pancreatic enzyme supplementation does not affect serum TLI concentrations.
Causes of Decreased TLI
TLI is the test of choice for EPI. A serum TLI concentration less than 2.5 µg/L (dog) or 8 µg/L (cat) is generally considered diagnostic for EPI. Subclinical canine EPI may be suspected by finding intermediate values (>2.5 µg/L and <5.0 µg/L). In such cases repeated testing should be performed. Some dogs will later develop EPI, whereas others will not.
Causes of Increased TLI
Values greater than 50 µg/L in dogs and greater than 100 µg/L in cats may occur with pancreatitis (the spec PL is better than TLI for this purpose in dogs and cats), renal failure, prerenal azotemia (may increase two times), and malnutrition. An increased fTLI test is potentially consistent with pancreatitis. In dogs, TLI seems to increase early in pancreatitis but then quickly returns to reference ranges.
Serum Cobalamin and Serum Folate
Occasional Indications
Chronic small bowel diarrhea, unexplained weight loss, or uncertain but suspected small intestinal disease are occasional indications for serum cobalamin and folate testing. These tests are more important in the cat than in the dog.
Advantages
Only one serum sample is needed to measure both values.
Disadvantages
The test has poor sensitivity and specificity for ARE and uncertain sensitivity and specificity for other intestinal diseases or EPI. This test should be an adjunct to other tests in patients with possible intestinal disease. The test is specific for cobalamin deficiency.
Analysis
Cobalamin and folate are measured in serum by bioassay or immunoassay. “No boil” methods are unreliable in dogs. Serum should be transported in a covered tube.
Normal Values
Depend on the laboratory. Normal ranges vary widely between laboratories. The particular laboratory must validate the assay for dogs and cats.
Danger Values
None.
Artifacts
Cobalamin concentration may be falsely decreased by sample degradation caused by exposure of serum to sunlight.
Drug Therapy That May Alter Serum Cobalamin Concentrations
Dietary content or vitamin supplementation of cobalamin and folate can affect serum concentrations. Drugs that affect intestinal bacterial concentrations (i.e., antibacterials ) may alter values.
Causes of Decreased Serum Cobalamin Concentrations
The major reasons for decreased serum cobalamin concentrations in dogs and cats are ileal disease or resection (rare), EPI, intestinal mucosal disease, and ARE (“dysbiosis”). In cats, hepatic disease and hyperthyroidism might cause hypocobalaminemia. The major differentiation to be made is among EPI and intestinal disease; therefore decreased serum cobalamin is an indication to measure serum TLI. Not all dogs with EPI, mucosal disease, or ARE have decreased serum cobalamin. Cats with EPI, severe small intestinal disease (e.g., lymphoma, IBD), and some hepatic diseases (e.g., idiopathic hepatic lipidosis) can have very low cobalamin concentrations. Finding a significantly decreased serum cobalamin concentration can be an indication of small intestinal disease in animals that were previously not suspected to have such disease.
Causes of Increased Serum Cobalamin Concentrations
Cobalamin concentration may be increased by cobalamin supplementation.
Causes of Decreased Serum Folate
Severe mucosal disease of the proximal small intestine decreases serum folate. Not all patients with such disease have decreased folate levels.
Causes of Increased Serum Folate
ARE, EPI, and dietary supplementation are probably the major causes. Many patients with these diseases do not have increased folate levels. The combination of low cobalamin plus increased folate is consistent with ARE, but is insensitive and nonspecific.
C-Reactive Protein (Crp)
Occasional Indications
CRP has been used in one formula for determining a Canine IBD Activity Index (CIBDAI).
Advantages
The test is very sensitive for detecting inflammation.
Disadvantages
The test will detect inflammation almost anywhere in the body; it is nonspecific as far as type or location or cause.
Analysis
CRP is measured on a sample of refrigerated or frozen fasting serum.
Normal Values
Less than 7.6 mg/L.
Artifacts
None known.
Drug Therapy That May Alter C-Reactive Protein
Unknown.
Interpretation
Any inflammation almost anywhere in the body can increase the CRP. The greatest utility in measuring CRP is to see what change occurs in a given patient after therapy (i.e., whether therapy is associated with an increase or decrease in CRP). Changes in the CRP can reveal resolving or worsening inflammation, even if all values are normal.
Hydrogen Breath Test
Rare Indications
The hydrogen breath test is rarely indicated in cases of chronic small bowel diarrhea or unexplained weight loss. The test detects hydrogen production as a by-product of bacterial fermentation of carbohydrates. Increase in hydrogen production indicates ARE or carbohydrate malabsorption. It can only be done in clinics/laboratories with specialized equipment and experience. The clinician should contact the laboratory for specifics.
Interpretation
Carbohydrate malabsorption and ARE may increase expired hydrogen. The only source of hydrogen is bacterial fermentation of carbohydrates. The sensitivity and specificity of this test for ARE in dogs are unknown.
Fecal Smear (Wet Mount) for Parasites
Common Indications
A fecal smear is used to screen for parasites and parasitic ova; it is indicated in any patient with diarrhea, melena, hematochezia, fecal mucus, weight loss, or vomiting.
Advantages
The test is widely available, easy to perform, and inexpensive.
Disadvantages
A fecal smear requires fresh feces, and is insensitive compared with concentration and molecular techniques.
Analysis
A thin smear is made of very fresh (<5 minutes old) feces, mixed with a drop of saline solution or water and coverslipped to prevent dehydration. It should be examined immediately. If protozoa are visible and better cytologic detail is desired, a drop of Lugol's iodine or Dobell and O’Connor's iodine may be placed at the corner of the coverslip.
Note.
Iodine kills protozoa, thus stopping motility.
Normal Values
No parasites or ova.
Artifacts
Cooling of the slide or dehydration inhibits the motility of protozoa.
Drug Therapy That May Alter Results
Orally administered compounds containing kaolin, pectin, barium sulfate, bismuth, and other intestinally active compounds (e.g., cathartics, enemas) may make it difficult to find and identify parasites, ova, and cysts.
Parasites, Bacteria, and Ova That May Be Identified
Giardia spp. (Figure 9-6A ), Tritrichomonas spp. (see Figure 9-6A), Entamoeba histolytica, Balantidium coli, Strongyloides stercoralis (Figure 9-6B), and Aelurostrongylus abstrusus may be detected. Any ova may be found, but this test may be useful for detecting Spirocerca lupi and Trichuris vulpis ova. With oil immersion, small motile bacterial spirochetes in conjunction with fecal WBCs suggest Campylobacter spp. as a possible cause.
FIGURE 9-6.

A, Comparison of Giardia trophozoites (small arrows) and Tritrichomonas trophozoites (large arrows) in a smear that has been stained to enhance internal structures. Note that the Tritrichomonas trophozoites are larger and have one large undulating membrane. B, A fecal smear stained with iodine showing larvae from Strongyloides stercoralis. The larvae of other strongylids (e.g., hookworms) appears identical, so it is important to use only fresh feces when looking for S. stercoralis.
(A and B courtesy of Dr. Tom Crain, Texas A&M University.)
Fecal Flotation
Common Indications
Indications for a fecal flotation test are as for a fecal smear.
Advantages
The test has reasonable sensitivity, high specificity, availability, and low cost.
Analysis
Feces are well mixed with either a saturated sugar solution or a zinc sulfate solution (prepared by mixing 331 g ZnSO4 • 7 H2O in 1 L water to attain a specific gravity of 1.18 to 1.20 [as determined with a hydrometer]). This is the best fecal flotation technique for Giardia spp. because it does not distort the cysts. Ova and cysts are allowed to rise to the surface and are retrieved with a coverslip. Samples for Giardia detection should be examined within 15 minutes to avoid distortion and lysis of cysts. Centrifugation of the sample increases the sensitivity of the procedure. Samples that will be sent to an outside laboratory for analysis may be refrigerated (not frozen) for 1 to 2 days or preserved by mixing 1 part feces with 3 parts sodium acetate–acetic acid–formalin (prepared by mixing 1.5 g sodium acetate + 2 ml glacial acetic acid + 4 ml 40% formaldehyde solution + 92.5 ml water).
Normal Values
No ova or oocysts present.
Artifacts
Diarrhea may decrease ova concentration within a sample.
Parasite Ova and Cysts That May Be Identified
Ancylostoma spp., Toxocara spp., Toxascaris leonina, Trichuris vulpis, Spirocerca lupi, Physaloptera rara (using dichromate solution), Capillaria aerophilia, Capillaria plica, Onciolo canis, Dioctophyme renale, Isospora spp., Giardia spp., Toxoplasma gondii, Cryptosporidium spp., Paragonimus kellicotti, and some tapeworms may be detected.
Fecal Sedimentation
Rare Indications
Indications for fecal sedimentation testing are the same as for fecal smear and flotation, especially if flukes are being considered. If feces contain excessive fat, then formalin and ethyl acetate is probably better than water for sedimentation.
Disadvantages
The test requires more time than a direct fecal smear or fecal flotation.
Analysis
Feces are mixed with the sedimentation solution (e.g., water or saline), strained once or twice to remove large debris, and allowed to settle for 30 minutes to 2 hours. The sediment is then examined microscopically. When formalin and ethyl acetate are used, the strained feces are centrifuged, the pellet is resuspended in 9 ml of 5% formalin solution, 3 ml ethyl acetate is added, and the mixture is shaken vigorously. This is recentrifuged, the debris at the formalin and ethyl acetate interface is discarded, and the sediment is then examined.
Normal Values
No ova.
Artifacts
Same as discussed in the previous section on Fecal Flotation.
Parasite Ova That May Be Identified
Fecal sedimentation may detect all the ova that may be found by fecal flotation, plus Alaria canis, Nanophyetus salmincola, and Heterobilharzia americana (Figure 9-7 ).
FIGURE 9-7.

Ova of Heterobilharzia americana in a fecal sedimentation.
(Courtesy of Dr Tom Craig, Texas A&M University.)
Fecal Giardia Detection
Common Indications
Fecal testing for Giardia is indicated in patients with chronic diarrhea, unexplained weight loss, intermittent bilious vomiting, or when Giardia is suspected clinically and multiple zinc sulfate flotations using centrifugation are negative. Techniques include duodenal aspiration and cytology, fecal ELISA antigen test (e.g., ProSpecT Microplate ELISA Assay for Giardia; Alexon, Lenexa, KS), and immunofluorescence assay (IFA) (e.g., MeriFluor Cryptosporidium/Giardia; Meridian Diagnostics, Cincinnati, OH) performed on feces.
Advantages
These tests are more sensitive than direct smear or fecal flotation for diagnosing Giardia.
Disadvantages
Duodenal aspirate requires surgery or endoscopy.
Analysis
Fresh samples should be used for analysis with fecal ELISA and fecal IFA. The IFA is more sensitive than the ELISA. Duodenal fluid aspirates require fresh direct wet mount observation of motile trophozoites.
Normal Values
No trophozoites or fecal antigen present.
Fecal Tritrichomonas Detection
Occasional Indications
Fecal testing for Tritrichomonas is indicated for chronic large bowel diarrhea in cats, especially exotic breeds such as Somalis, ocicats, and Bengals.
Advantages
Culture is more sensitive (approximately 1000 organisms/50 mg of feces) than direct fecal examination, while PCR is the most sensitive test (approximately 10 organisms per 200 mg feces).
Disadvantages
Different techniques have different sensitivities that the clinician must be aware of. Feces should be fresh, not refrigerated. Old feces can give false-negative results for direct examination and culture. Direct fecal examination is relatively insensitive (<15%).
Analysis
Fresh fecal samples can be examined microscopically (see Fecal Smear earlier in this chapter) (see Figure 9-6A). Feces (very fresh, approximately 0.05 g) can be cultured using commercially available pouches designed for culturing Trichomonas foetus from cattle (i.e., In Pouch TF; Biomed Diagnostics, White City, Oregon). This test is best done in the clinic without sending off the feces or the pouch. The inoculated pouch is incubated upright in the dark at either 37° C or room temperature for 2 or 12 days, respectively. It should be examined microscopically at least every 48 hours.
Finally, feces may be preserved (approximately 200 mg in 3 to 5 ml of 70% isopropyl alcohol; be sure to avoid including litter) and mailed to a laboratory for PCR analysis.
Normal Values
Negative.
Fecal Cryptosporidium Detection
Rare Indications
Fecal testing for Cryptosporidium may be indicated in patients with chronic diarrhea. Cats (especially with feline immunodeficiency virus [FIV] infection) may be more likely to have cryptosporidiosis than dogs, but the prevalence of this disorder and its clinical significance in dogs and cats is currently unknown.
Disadvantages
Oocysts are small and may be difficult to find.
Analysis
Fresh fecal samples should be sent to a referral laboratory experienced in finding Cryptosporidium. Special fecal flotation techniques, direct fecal smears stained with an acid-fast stain, or ELISA methodology (e.g., ProSpecT Cryptosporidium Microplate Assay; Alexon, Lenexa, KS) can be used. The ELISA methodology appears to be the most sensitive.
Normal Values
Negative.
Fecal Heterobilharzia Detection
Occasional Indications
Fecal PCR testing for Heterobilharzia is primarily used in dogs with intestinal or hepatic disease or unexplained hypercalcemia from areas where Heterobilharzia is endemic.
Advantages
The test is more sensitive than fecal sedimentation; it can detect 1 to 2 ova/g of feces.
Disadvantages
There is limited availability of testing. The test is currently available at GI Laboratory, College of Veterinary Medicine, Texas A&M University, College Station, TX 77843-4474.
Analysis
PCR is performed on feces.
Artifacts
None known.
Drug Therapy That May Alter Test Results
None known.
Interpretation
A positive result in an animal with clinical signs consistent with heterobiliharziasis is an indication to treat.
Hepatic Abnormalities
Perhaps the most difficult aspect of dealing with hepatic disease is distinguishing primary hepatic disease (i.e., the liver is or will be the cause of the patient's illness) from secondary hepatic disease (i.e., the liver disease is caused by the patient's nonhepatic illness). Primary hepatic disease may be heralded by relatively suggestive signs (e.g., hepatomegaly, microhepatia, icterus, ascites, hepatic encephalopathy) or associated with nonspecific signs (e.g., depression, weight loss, anorexia, vomiting). The latter are common presenting complaints of many diseases, which is why serum biochemistry profiling is indicated in patients with chronic signs or evidence of systemic disease. There are no signs or laboratory abnormalities consistently found in patients with primary hepatic disease. When screening for hepatic disease, one should request at least a CBC, serum ALT, SAP, total bilirubin, albumin, cholesterol, BUN, glucose, urinalysis, and abdominal imaging. Hepatic function tests (i.e., serum bile acids and/or blood ammonia) and ultrasound are often very helpful. Hepatic cytology/biopsy is usually necessary for definitive diagnosis except in patients with portovascular anomalies. Abnormalities in hepatic-specific enzymes may result from primary hepatic disease or hepatic involvement secondary to nonhepatic disease (e.g., glucocorticoid hepatopathy, septicemia, IBD, pancreatitis). After identifying abnormalities in ALT, aspartate aminotransferase (AST), SAP, or gamma-glutamyl transpeptidase (GGT), one should investigate first for a secondary hepatic disease because these are the most common causes of increased values. In such cases the liver usually has reactive but reversible degenerative changes. Laboratory tests and ultrasound should be used for two main purposes: (1) to identify the presence of hepatic disease and (2) to help determine if hepatic biopsy is indicated.
Microhepatia: Small Liver
A small liver suggests atrophy (i.e., congenital portosystemic shunt [PSS], hepatic arteriovenous [AV] fistula), fibrosis and cirrhosis, or diffuse massive hepatic necrosis (Figure 9-8 ). Hepatic atrophy tends to be characterized by sharp borders as opposed to the rounded or blunted hepatic margins typically associated with fibrosis and cirrhosis. Some patients with primary hepatic fibrosis severe enough to cause portal hypertension also have sharp hepatic margins, however. Many patients with marked hepatic atrophy due to congenital PSS are relatively young (<3 to 4 years) and have had signs of hepatic disease since (or before) weaning, whereas most patients with cirrhosis are middle-aged or older and clearly have late onset of clinical signs. Hepatic AV fistula is an uncommon cause of microhepatia, but it is usually diagnosed in dogs less than 2 years of age. However, some dogs with congenital PSS are first diagnosed when they are more than 10 years old. Likewise, some dogs with acquired PSS due to cirrhosis are diagnosed when less than 6 months old.
FIGURE 9-8.

Diagnostic approach to altered hepatic shape or size in dogs and cats. AV, Arteriovenous; CT, computed tomography.
Hepatic atrophy typically causes abnormalities in hepatic function tests (e.g., serum bile acids, blood ammonia) but may yield normal or abnormal ALT, SAP, BUN, and serum albumin. A single normal or abnormal hepatic function test result does not mean that other hepatic function tests will have similar results. Pre- and postprandial serum bile acid concentrations are generally sensitive function tests. (NOTE: Cholestatic diseases also increase bile acids; therefore, bile acids are not a “pure” test of hepatic function.) However, if hepatic disease is strongly suspected and the serum bile acid concentrations are not as high as anticipated, one should not hesitate to perform other tests to characterize the liver. If hepatic atrophy is likely, abdominal ultrasonography, advanced imaging (e.g., contrast portography, computed tomography, magnetic resonance imaging), hepatic biopsy, or a combination of these might be considered.
Small livers with clearly rounded or blunt hepatic margins are often fibrotic/cirrhotic. Significant increases in serum ALT and SAP are often present, but some dogs with marked hepatic cirrhosis have normal hepatic enzymes. Serum albumin and BUN are more variable. If cirrhosis appears likely, a biopsy is often indicated. An obviously nodular or “cobblestone” appearance is very suggestive of cirrhosis; however, significant fibrosis can be present without major gross changes, and some noncirrhotic diseases (e.g., hepatic collapse with nodular regeneration, nodular hyperplasia) may grossly resemble cirrhosis. Acquired multiple shunts visible at laparoscopy or laparotomy are usually due to cirrhosis but can be secondary to congenital hepatic AV fistula, veno-occlusive disease, portal vein obstruction, or infiltrative disease.
Hepatomegaly: Enlarged Liver
Focal or asymmetric hepatic enlargement generally necessitates further laboratory investigation, imaging, and possibly biopsy. Neoplasia is a prominent but not invariable cause of focal hepatomegaly. The magnitude of the enlargement is not prognostic.
Generalized hepatomegaly necessitates careful clinicopathologic evaluation. Hepatomegaly may be caused by primary or secondary hepatic disease. Diagnosis may be confirmed with a history of exposure to certain toxins (Box 9-5, Box 9-6 ) or diagnosis of a systemic disease (e.g., hyperadrenocorticism) known to affect the liver. Changes in ALT, SAP, hepatic function tests, and hepatic size, although suggestive of hepatic disease, are not diagnostic of specific entities. This is true even in breeds with predispositions to specific hepatic diseases (e.g., Doberman pinschers, Bedlington terriers). Changes in the SAP or ALT may also be caused by primary nonhepatic disease (e.g., hyperadrenocorticism, IBD, diabetes mellitus, heart failure). A definitive diagnosis usually requires hepatic biopsy. The clinician should first seek to rule out nonhepatic causes of secondary hepatic dysfunction. Hepatic biopsy should be considered in patients with obviously significant hepatic disease, those that do not have obvious nonhepatic causes (e.g., hyperadrenocorticism, right heart failure), and those that have persistent (>1 month) changes in serum ALT consistent with chronic or progressive hepatic disease or abnormal hepatic function tests (see Figure 9-8). It is not always possible to accurately distinguish primary hepatic from secondary hepatic disease before biopsy; therefore whenever hepatic biopsy is performed via laparotomy or laparoscopy, the rest of the abdomen should be explored and other organs sampled if they might be involved. Fine-needle aspirates with cytology are sometimes useful in detecting diffuse hepatic infiltrative disease and hepatic lipidosis (Figure 9-9 ); however, fine-needle aspirates (even when guided by ultrasound) often miss infiltrative processes. A negative cytologic finding from a fine-needle aspirate never excludes infiltrative hepatic disease. Hepatic biopsy may be done with ultrasound guidance, laparoscopy, or laparotomy. Laparoscopy allows for much superior hepatic biopsies compared with ultrasound-guided core needle biopsies and is not as invasive as surgery.
Box 9-5. Drugs that Have Been Documented or Suspected to Cause Increased Alanine Aminotransferase (Alt) Levels Due to Hepatic Disease.
Acetaminophen (especially cats) (important)
Amiodarone
l-Asparaginase
Azathioprine
Barbiturates (important)
Carprofen (important)
Clindamycin
Doxycycline
Diazepam
Erythromycin estolate
Glucocorticoids (dogs only) (important)
Griseofulvin
Ibuprofen
Itraconazole
Ketoconazole
6-Mercaptopurine
Methimazole
Methotrexate
Nitrofurantoin
Phenobarbital (important)
Primidone (important)
Salicylates
Salicylazosulfapyridine
Sulfonamides
Tetracycline
Trimethoprim-sulfa drug (important)
NOTE: These drugs do not reliably cause hepatic disease. In a patient with an increased ALT that is receiving one of these drugs, the medication probably should be stopped, if possible, and the ALT rechecked 2 to 4 weeks later. Those drugs that most reliably increase ALT are marked (important). The other drugs are less consistent but may still cause severe hepatic disease. Almost any drug could cause an increased ALT in a particular patient.
Box 9-6. Drugs that Have Been Documented or Suspected to Cause Cholestasis or Hepatic Enzyme Induction Resulting in Increased Serum Alkaline Phosphatase (Sap) Levels.
Anabolic steroids/androgens
Asparaginase
Azathioprine
Barbiturates (important)
Cephalosporins
Cyclophosphamide
Dapsone
Erythromycin estolate
Estrogens
Glucocorticoids (dogs only) (important)
Gold salts
Griseofulvin
Ibuprofen
6-Mercaptopurine
Methimazole
Methotrexate
Nitrofurantoin
Phenobarbital (important)
Phenothiazines
Primidone (important)
Progesterone
Salicylates
Testosterone
Tetracyclines
Thiabendazole
Trimethoprim-sulfa drug
Vitamin A
NOTE: Those drugs that most reliably increase SAP are marked (important). The other drugs are less consistent.
FIGURE 9-9.

Feline fatty liver. This binucleated hepatocyte was stained with both a Sudan stain and new methylene blue to document the abundant fat in intracellular vacuoles and free outside the hepatocyte.
Hepatic Encephalopathy
Abnormal behavior, sometimes associated with eating, may be caused by hepatic encephalopathy; however, hypoglycemia, primary CNS disease, and epilepsy must also be considered. Whenever possible, glucose should be measured on blood obtained during an episode. Evaluation of hepatic function is indicated in patients with behavioral changes (which may be obvious or subtle), transient blindness, seizures, coma, or vague CNS abnormalities. Congenital PSS and severe acquired hepatic disease (e.g., cirrhosis) may cause encephalopathy. Hepatic function testing is mandatory because these diseases may not significantly change serum ALT, SAP, albumin, BUN, glucose, or bilirubin concentrations. Resting blood ammonia concentrations are very specific for hepatic dysfunction, but they are not as sensitive as serum bile acids. A patient in an episode of hepatic encephalopathy may have increased or normal resting blood ammonia concentrations. Ammonia tolerance testing (ATT) and pre- and postprandial serum bile acid concentrations appear to be the most sensitive and specific tests for hepatic dysfunction that causes hepatic encephalopathy. A very rare congenital urea cycle enzyme deficiency may cause hepatic encephalopathy and hyperammonemia without affecting enzymes or bile acids, in which case analysis of urea cycle enzymes in hepatic samples is necessary for diagnosis.
Icterus
Icterus is detected at physical examination or when serum or plasma is inspected at the laboratory. Hyperbilirubinemia always denotes hepatobiliary or hematopoietic disease (Figure 9-10 ). Hepatic and hematopoietic diseases are not always associated with icterus, and disease in either system may be secondary to other disorders. The presence or absence of icterus is not diagnostic or prognostic. Sepsis, pancreatitis, and IBD sometimes cause secondary hepatobiliary dysfunction that may include icterus.
FIGURE 9-10.

Diagnostic approach to hyperbilirubinemia in dogs and cats. CBC, Complete blood count; FDP, fibrin degradation products; PCV, packed cell volume; RBC, red blood cell.
Total Serum Bilirubin
Common Indications
Measurement of total serum bilirubin is indicated in cases of icterus (on either physical examination or inspection of nonhemolyzed serum or plasma), bilirubinuria (any amount in a cat or significant amounts in a dog), or suspected hepatic disease that is not apparent on other tests. The sclera has detectable icterus when the serum bilirubin is greater than 3 to 4 mg/dl, and the plasma is icteric when the serum bilirubin is greater than 1.5 to 2 mg/dl.
Note.
Icterus is absent in many animals (especially dogs) with hepatic disease. Serum bilirubin is not a sensitive test for hepatic disease.
Measurement of direct (conjugated) and indirect (unconjugated) bilirubin fractions is not useful because hemolytic, hepatic, and biliary tract diseases have unpredictable variation in the amount of each fraction.
Analysis
Total bilirubin is measured in serum or heparinized plasma by spectrophotometric and dry reagent methods. The latter require dilutions if the bilirubin is greater than 7.5 mg/dl. Bilirubin is stable at 4° C for 7 days if not exposed to bright light. Measurement of urine bilirubin is discussed in Chapter 7.
Normal Values
Dogs, less than 1.0 mg/dl; cats, less than 1.0 mg/dl (depends upon the laboratory).
Danger Values
Dogs, uncertain, but values greater than 20 mg/dl cause concern (i.e., kernicterus); cats, unknown.
Artifacts
Exposure to bright sunlight or fluorescent lighting can decrease bilirubin by 50% per hour (see Chapter 1).
Drug Therapy That May Alter Serum Bilirubin
Decreased bilirubin may be caused by drugs that cause hepatic enzyme induction (e.g., phenobarbital). Increased bilirubin may be the result of drugs causing hemolytic anemia or acute hepatic necrosis or dysfunction (see Box 9-5).
Causes of Hyperbilirubinemia
Hemolytic disease and hepatobiliary disease are the two main causes (see Figure 9-10). A CBC should be determined in every icteric patient to help rule out hemolytic disease. RBC numbers must decrease rapidly and significantly (i.e., packed cell volume [PCV] usually <20%) to cause clinical icterus. Very regenerative anemias may suggest that icterus is due to immune-mediated hemolytic anemia (IMHA). Reticulocytosis, hemoglobinemia, hemoglobinuria, erythrocytic autoagglutination, spherocytosis, positive Coombs test results, splenomegaly, or hepatomegaly are often present. Chapter 3 includes further discussion of IMHA and other regenerative anemias (e.g., Heinz body, zinc intoxication, Babesia, Cytauxzoonosis, hemotrophic Mycoplasma). Bilirubinuria theoretically should be absent in hemolytic disease but is typically present in IMHA because canine kidneys conjugate bilirubin. The clinician must not be misled by increases in ALT, because severe, acute hemolytic anemia may cause increased ALT (ostensibly caused by acute hepatic hypoxia).
Severe hepatic disease (especially acute necrosis) is sometimes accompanied by DIC and subsequent hemolytic anemia. These cases may be difficult to distinguish from IMHA. However, anemia caused by DIC is usually not as regenerative as in IMHA; in addition, the presence of RBC fragments, thrombocytopenia, increased fibrin degradation products (FDP), decreased antithrombin III, prolonged clotting time, and abnormal hepatic function tests usually allow differentiation, as do vomiting, abdominal pain, and encephalopathy when present.
Dogs and cats often have relatively severe hepatic disease before icterus is observed; however, the magnitude of the total serum bilirubin is not prognostic or diagnostic. Secondary hepatic disease (reactive disease or so-called bystander phenomenon as the result of septicemia, toxemia, or inflammation) may cause icterus. Certain bacterial endotoxins and acute phase inflammatory mediators are thought to alter normal bilirubin metabolism and cause increases in total bilirubin concentrations.
Most feline hepatic diseases eventually cause icterus; the most common conditions include hepatic lipidosis, cholangitis and cholangiohepatitis, hepatic lymphoma, and FIP. Icterus in cats is an indication for a CBC and serum biochemistry panel. Icterus in cats that is not caused by hemolysis usually indicates a hepatic biopsy, because most of these cats have primary hepatic disease. Biopsy is necessary to differentiate causes and institute specific treatment.
Common causes of nonhemolytic icterus in dogs include pancreatitis obstructing the bile duct, gallbladder mucoceles, cholecystitis, chronic hepatitis, hepatic lymphoma, acute hepatic necrosis, hepatic cirrhosis, and intrahepatic cholestasis. Icterus in dogs is an indication for a CBC and serum biochemistry panel (to include at least ALT, SAP, BUN, cholesterol, and albumin). Ultrasonography is indicated to help determine if primary hepatic disease or biliary tract obstruction exists. If primary hepatic disease is diagnosed, hepatic biopsy is usually indicated. If pancreatitis is present, surgery is not indicated unless a persistent bile duct obstruction necessitates a biliary drainage procedure (e.g., cholecystoduodenostomy or biliary tract stenting—both are very rarely needed) or a pancreatic abscess is symptomatic despite percutaneous drainage. If coexisting extrahepatic disease is found, it should be investigated.
Alanine Aminotransferase
ALT was formerly known as serum glutamic-pyruvic transaminase (SGPT).
Common Indications
Systemic disease, including weight loss, hepatomegaly, vomiting, diarrhea, icterus, ascites, depression, and anorexia, is an indication for measurement of ALT; also, ALT is used as a screening procedure for hepatic disease in patients with undiagnosed illness. Most patients with known chronic hepatitis should undergo periodic ALT determinations to monitor the problem.
Advantages
The serum ALT is specific for the liver.
Disadvantages
The test has lack of sensitivity (i.e., patients with significant hepatic disease such as cirrhosis or hepatic neoplasia may have normal ALT) and cannot distinguish among different hepatic diseases or determine if there is secondary nonhepatic disease involvement.
Analysis
ALT is measured in serum (heparinized plasma in selected assays) by spectrophotometric and dry reagent methods. ALT is stable in separated serum for approximately 1 (at 22° C) to 7 (at 4° C) days.
Normal Values
Serum enzyme activity may vary markedly among laboratories, depending on the technique and the units used.
Danger Values
Despite correlation between ALT and active hepatic damage, no correlation exists between ALT and hepatic function; hence, no danger values exist.
Artifacts
See Chapter 1.
Drug Therapy That May Alter Serum ALT
Any drug causing hepatocellular damage (i.e., drug-induced hepatopathy) may cause increased ALT. The list of all drugs suspected to cause increased ALT is extensive and includes many that are safe in the majority of patients. A list of selected drugs documented to cause increased ALT in human beings, dogs, and cats is given in Box 9-5. Administration of one of these drugs does not automatically explain an increased ALT, however.
Note.
A patient can have an idiosyncratic reaction to almost any drug, causing an increased ALT.
Causes of Decreased ALT
Not significant.
Causes of Increased ALT
Increase in ALT is principally caused by hepatocellular damage from any cause (Box 9-7 ). RBCs and striated muscle cells contain small amounts of ALT, and damage to these may cause relatively minor increases (i.e., less than two to three times normal) in serum ALT, as may exercise. Dogs with muscular dystrophy may have major increases in ALT, but should also have increases in AST and creatine kinase (CK) values.
Box 9-7. Selected Causes of Increased Serum Alanine Aminotransferase Levels (>3 Times Normal).
| DOGS | CATS |
|---|---|
| Hepatobiliary Disease | Hepatobiliary Disease |
| Cholangitis | Cholangitis |
| Cholangiohepatitis | Cholangiohepatitis |
| Cirrhosis | Feline infectious peritonitis (FIP) |
| Copper storage disease | Hepatic lymphoma |
| Hepatic malignancy | Cirrhosis |
| Chronic hepatitis | Hepatic toxin |
| Hepatic toxin | Trauma |
| Trauma | Pancreatitis |
| Pancreatitis | Hyperthyroidism |
| Other Disorders | Other Disorders |
| Anoxia because of anemia/shock | Anoxia because of anemia/shock |
| Iatrogenic (see Box 9-5) | Iatrogenic (see Box 9-5) |
NOTE: Almost any disease affecting the liver can cause increased ALT levels. The disorders listed are those that may be more likely to cause a significant increase. However, any of these diseases can exist with minor or no increase in ALT values.
Hepatocytes contain substantial amounts of ALT in the cytosol, and major increases in serum ALT (i.e., three or more times normal) indicate hepatocellular leakage of the enzyme but do not always signify primary or irreversible hepatic disease. Hepatic disease may have normal to significantly increased serum ALT activity. The magnitude of the increase in ALT does not correlate with the seriousness of the hepatic disease and is not a prognostic indicator unless a specific disease is being considered. The serum ALT half-life is approximately 1 to 2 days or less, and serum ALT is expected to decrease over 1 to 2 weeks once active hepatic damage ceases. It is thought that ALT remains elevated during hepatic regeneration.
After increased serum ALT is identified, many factors must be considered (Figure 9-11 ). If no other evidence of disease is found, the increased ALT indicates the need for periodic monitoring because it may be the first detectable sign of significant hepatic disease. If other abnormalities consistent with hepatic disease are found, the approach is like that in any other patient with hepatic disease. Common causes of serum ALT more than three times normal include hepatic anoxia, poor hepatic perfusion, spontaneous and surgical trauma (e.g., hit by a car, surgery), chronic hepatitis, cirrhosis, cholangitis and cholangiohepatitis, acute biliary obstruction, hepatic necrosis as the result of any cause, acute pancreatitis, hepatic neoplasia, sepsis, and certain drugs. Sepsis, especially septicemia and toxemia, may secondarily damage hepatocytes. Abdominal inflammation may do the same. The pancreas is close to the liver, and inflammation in the pancreas may cause mechanical damage to the liver. In Doberman pinschers, Bedlington terriers, dalmatians, West Highland white terriers, and Labrador retrievers, a persistently increased serum ALT suggests chronic hepatitis that might be associated with increased hepatic copper concentrations.
FIGURE 9-11.

Diagnostic approach to alanine aminotransferase (ALT) greater than three times normal in dogs and cats. BUN, Blood urea nitrogen; CBC, complete blood count; SAP, serum alkaline phosphatase.
Aspartate Aminotransferase
AST was formerly known as serum glutamic-oxaloacetic transaminase (SGOT).
Occasional Indications
Indications for AST are the same as for ALT.
Disadvantages
Serum AST is not as specific for the liver as ALT.
Analysis
Measurement of AST is the same as for ALT.
Drug Therapy That May Alter AST
Decreased AST may be caused by metronidazole therapy. Hepatotoxic drugs may cause increased AST (see Box 9-5).
Causes of Decreased AST
None.
Causes of Increased AST
Like ALT, AST is present in significant quantities in hepatocytes. Although ALT is present in the cytosol, AST is present in the mitochondria. Increased serum ALT reflects cell membrane damage and leakage; significant AST increases tend to reflect more serious hepatocyte damage because the mitochondria are not damaged as readily as is the cell membrane. AST is, however, present in significant quantities in many other tissues, including muscle and RBCs; therefore increased AST is not as specific for hepatic injury as is increased ALT. Exercise and intramuscular (IM) injections may increase serum AST. The most common causes of increased AST include hepatic disease, muscle disease (inflammation or necrosis), or hemolysis (spontaneous or artifactual). Increased AST is an indication to measure serum ALT to determine whether the increased AST is from the liver (significant increases in both ALT and AST suggest that AST increases are of hepatic origin). One may also measure the hematocrit and observe the color of the plasma and serum on a centrifuged blood sample to check for hemolysis.
Serum Alkaline Phosphatase
Common Indications
Systemic disease, including weight loss, hepatomegaly, vomiting, diarrhea, ascites, icterus, depression, or anorexia, is an indication for measurement of SAP; also, SAP is used as a screen for hepatic disease and hyperadrenocorticism.
Advantages
SAP is useful in evaluating the liver for cholestatic disease.
Disadvantages
Measurement of SAP is affected by corticosteroids (endogenous and exogenous), bone lesions, and osteoblastic activity in young growing dogs.
Analysis
SAP is measured in serum or heparinized plasma by spectrophotometric methods. Different techniques (i.e., heat stability, phenylalanine, electrophoresis) have been used to distinguish SAP of bone origin from SAP of hepatic origin. The diagnostic usefulness of this distinction is doubtful because dogs with various types of hepatic disease often have endogenous steroids released due to the stress of illness.
Normal Values
May vary markedly from laboratory to laboratory. Immature dogs characteristically have SAP (bone origin) activities up to twice those of sexually mature dogs.
Danger Values
There is no correlation with hepatic function; therefore no danger values exist.
Artifacts
See Chapter 1.
Drug Therapy That May Increase SAP
Any drug that causes hepatic enzyme induction or cholestasis (see Box 9-6) may increase SAP. Glucocorticoids, primidone, and barbiturates typically increase SAP in dogs, but other drugs are less consistent. Although glucocorticoids can cause marked SAP increases in dogs, cats are almost never affected.
Causes of Decreased SAP
Not significant.
Causes of Increased SAP
SAP of bone origin is commonly increased (SAP less than three times normal) in dogs less than 6 to 8 months old. Bone disease (e.g., osteosarcoma, osteomyelitis) may increase SAP (usually a minor increase).
Increased SAP is interpreted differently in dogs and cats (Box 9-8 ). Cats have less hepatocellular SAP, which is readily excreted by their kidneys. Therefore any increase in feline SAP is considered important. Not all cats with hepatic disease have increased SAP. The major causes of increased SAP in cats are hepatic lipidosis, cholangitis and cholangiohepatitis, hyperthyroidism, and diabetes mellitus. SAP increases are generally more specific than GGT in cats with hepatic lipidosis (cats with lipidosis classically have very high SAP with little to no increase in GGT; however, this finding is not consistent enough to allow a diagnosis). Hyperadrenocorticism (spontaneous and iatrogenic) very rarely increases SAP in cats. Increased SAP in a cat is an indication for serum thyroid hormone determination, urinalysis, blood glucose, and serum ALT measurement, ± hepatic function testing (e.g., serum bile acids). If hepatic disease is the apparent cause of the increased SAP, one must determine if hepatic biopsy is indicated (see the discussion under Serum Bile Acids later in this chapter).
Box 9-8. Causes of Increased Serum Alkaline Phosphatase Levels.
| DOGS | CATS |
|---|---|
| Biliary Tract Abnormalities | Biliary Tract Abnormalities |
| Pancreatitis | Same as for dogs |
| Bile duct neoplasia | |
| Cholelithiasis | |
| Cholecystitis | |
| Gall bladder mucocele | |
| Ruptured gallbladder | |
| Hepatic Parenchymal Disease | Hepatic Parenchymal Disease |
| Cholangiohepatitis | Cholangiohepatitis |
| Chronic hepatitis | Hepatic lipidosis |
| Copper storage disease | Hepatic lymphoma |
| Cirrhosis/fibrosis | Feline infectious peritonitis (FIP) |
| Hepatic neoplasia | |
| Lymphoma | |
| Hemangiosarcoma | |
| Hepatocellular carcinoma | |
| Metastatic carcinoma | |
| Toxic hepatitis | |
| Aflatoxin | |
| Mushroom | |
| Sago palm | |
| Drug induced | |
| Other Disorders | Other Disorders |
| Diabetes mellitus | Diabetes mellitus |
| Endogenous steroids (from physiologic stress or pathologic hyperadrenocorticism) | Hyperthyroidism |
| Chronic passive congestion from right heart failure | |
| Diaphragmatic hernia | |
| Septicemia | |
| Ehrlichiosis* | |
| Young dog with bone growth | |
| Osteomyelitis* | |
| Iatrogenic (see Box 9-6) | Iatrogenic (see Box 9-6)* |
NOTE: Almost any disease affecting the liver can cause increased SAP levels. The disorders listed are those that may be more likely to cause a significant increase. However, any of these can exist with minor or no increase in SAP values.
Rarely of importance.
The major causes of SAP values more than three times normal in dogs are hepatobiliary disease, endogenous steroids (i.e., hyperadrenocorticism or stress), and therapy with glucocorticoids or anticonvulsants. Hepatic disease with increased SAP usually has a cholestatic component; however, this does not imply icterus or gross obstruction of the biliary tract. Intrahepatic cholestasis caused by diffuse or focal compression of bile canaliculi may occur in various hepatopathies, even those secondary to septicemia, toxemia, and chronic stress-induced vacuolar (i.e., hydropic change) hepatopathy. Acute hepatocellular necrosis can transiently increase SAP. Extrahepatic biliary tract obstruction and enzyme induction caused by endogenous or exogenous glucocorticoids or drug administration may increase SAP more than 10 times normal. As with ALT, the magnitude of the increase in SAP does not correlate with prognosis.
In dogs, it is important first to rule out young age, drug therapy, and hyperadrenocorticism to avoid performing unnecessary diagnostics (Figure 9-12 ). Hyperadrenocorticism can easily be confused with primary hepatic disease because it typically causes hepatomegaly, pu-pd, increased ALT, and sometimes increased serum bile acids. If a patient has signs of hepatic failure (i.e., icterus, hepatic encephalopathy, hypoglycemia, weight loss, vomiting, hypoalbuminemia, ascites, microhepatia), one generally assumes that the increased SAP is due to primary hepatic disease. If it is not obvious that the patient probably has primary hepatic disease and the patient has signs that might be consistent with hyperadrenocorticism (e.g., pu-pd, cutaneous changes, potbelly), then adrenal gland function testing may be appropriate. If the SAP is increased but the ALT and serum bilirubin concentrations are normal, clinically important hepatic disease is unlikely. If the ALT is substantially increased (and especially if it is higher than the SAP), then primary hepatic disease is much more likely. If a hepatic biopsy specimen is obtained from a patient with hyperadrenocorticism or other systemic disease that is causing “stress,” vacuolar hepatopathy is found.
FIGURE 9-12.

Diagnostic approach to increased serum alkaline phosphatase (SAP) in dogs. ALT, Alanine aminotransferase; CBC, complete blood count; SBA, serum bile acids.
Gamma-Glutamyl Transpeptidase
Rare Indications
GGT is rarely indicated; the indications are similar to those for SAP. SAP appears to be more sensitive for hepatobiliary disease in dogs; however, in cats, GGT has slightly greater sensitivity and perhaps greater specificity for hepatic disease (except hepatic lipidosis). Therefore it is more frequently indicated in cats than in dogs. GGT is less influenced than SAP by secondary hepatic disease conditions or enzyme-inducing drugs. The use of SAP and GGT together has a higher predictive value of hepatic disease.
Analysis
GGT is measured in serum, urine, and body fluids by spectrophotometric methods. GGT is stable in serum at 4° C for at least 3 days and at 20° C for up to 1 year.
Normal Values and Danger Values
Same as for SAP.
Artifacts
See Chapter 1.
Drug Therapy That May Affect GGT
The same drugs that may affect SAP may affect GGT.
Causes of Decreased GGT
Not significant.
Causes of Increased GGT
Causes are similar to those of increased SAP and tend to parallel the magnitude of the rise in SAP, but bone lesions are not recognized to increase GGT. It is induced by glucocorticoid therapy and certain drugs, as is SAP. In cats, GGT may increase more than SAP, except in hepatic lipidosis (where classically the SAP is usually quite high, but GGT values show only a mild [or no] increase). GGT does not tend to increase after acute hepatic necrosis, as does SAP. Increased GGT should be pursued as for increased SAP (see Figure 9-12). Increased GGT may suggest pancreatitis obstructing the bile duct, as for SAP.
Causes of Increased Urine GGT
Increased 24-hour urinary excretion of GGT can be caused by various nephrotoxins (e.g., gentamicin).
Lactate Dehydrogenase
Rare Indications
This test is not recommended.
Disadvantages
Lactate dehydrogenase (LDH) has lack of specificity.
Causes of Increased LDH
LDH is found in many body tissues. Inexplicable increases of small to great magnitude are not uncommon.
Serum Bile Acids
Frequent Indications
Measurement of serum bile acids (SBAs) is indicated in patients with suspected occult hepatic disease, chronic weight loss, abnormal CNS signs, hepatomegaly, and microhepatia. SBAs are used routinely as a screening test for hepatic dysfunction (e.g., PSS).
Advantages
SBAs are easy to measure, and few extrahepatic factors affect it.
Disadvantages
Measurement of SBAs does not reliably distinguish among different hepatobiliary diseases. Values may spontaneously change enough from day to day that it can be difficult to use SBA concentrations to determine if a change in hepatic function has occurred.
Analysis
SBAs are measured in serum by either a direct enzymatic method that quantifies total serum 3-alpha-hydroxylated bile acids or an RIA procedure that measures specific bile acids. It is important that a validated assay for dogs and cats be used because some methods are not accurate. Values for enzymatic and RIA procedures cannot be compared.
Maximum information is obtained by determining a 12-hour fasting preprandial and 2-hour postprandial SBA concentration. Dogs and cats should be fed canned food containing moderate fat content, causing the gallbladder to contract. Preprandial and postprandial SBA concentrations together improve the sensitivity of the test, making it more sensitive than resting blood ammonia concentration. Ceruletide has been administered after taking the fasting sample in an attempt to ensure gallbladder contraction and have more consistent results. It has not demonstrated increased sensitivity and specificity when looking for PSS, but it might be more sensitive when looking for hepatic disease associated with respiratory tract abnormalities.
Normal Values
Because of different techniques and assays (µmol/L or µg/ml), normal values must be established for each laboratory.
Danger Values
None.
Artifacts
Very increased serum dehydrogenase activities may require modification of the spectrophotometric technique. Severe lipemia (i.e., chylomicronemia) and hemolysis may falsely decrease SBA measurements, and hypertriglyceridemia may falsely increase SBA concentrations when spectrophotometric techniques are used, but they do not affect RIA. This test is not useful in icteric patients.
Drug Therapy and Other Factors That May Alter SBA Concentration
Cholestyramine lowers serum concentrations by binding to bile acids in the intestinal lumen, preventing their reabsorption. Ursodeoxycholic acid (a synthetic bile acid) therapy may increase total SBA concentrations. Resection of the ileum (the principal site of bile acid reabsorption), severe ileal disease, or cholecystectomy may also cause SBAs to inaccurately reflect hepatic function. Prolonged anorexia (>1 to 2 days) may cause fasting SBA concentrations to be less than would be found if the patient were eating normally. Intestinal hypomotility may cause the 2-hour postprandial sample to be a less sensitive indicator of hepatic disease because of failure to deliver the bile acids to the ileum in a timely fashion. Hepatic insufficiency does not decrease SBA concentrations.
Causes of Decreased SBA Concentration
Delayed gastric emptying, rapid intestinal transit, malabsorption disorders, and ileal resection may cause subnormal values. With ARE, total measurable moieties may or may not decrease, but it is expected that unconjugated serum bile acid concentrations may increase.
Causes of Increased SBA Concentration
SBA concentrations are increased because of hepatocellular disease, cholestatic disease, hepatic microvascular dysplasia, or PSS. When both fasting and 2-hour postprandial SBA concentrations are determined, the sensitivity of these tests becomes greater than with other hepatic function tests except perhaps the ammonia tolerance test. Because of the ease of performing and the wide availability of the test, it has replaced other clinical hepatic function tests. SBAs offer no additional information in icteric patients with hepatic or extrahepatic biliary tract disease. In nonicteric patients suspected of having hepatic disease, SBAs are a good screening test to support further diagnostic evaluations. Not all patients with primary hepatic disease have increased SBA concentrations. The relative increase in SBAs as well as the percent increase from preprandial to postprandial values is not prognostic or diagnostic for a specific disease. Reported fasting SBAs that are greater than 20 µmol/L or postprandial values greater than 25 µmol/L suggest primary hepatic disease, microvascular dysplasia, or PSS and dictate further hepatic evaluation and possibly hepatic biopsy. If only fasted SBA values are determined and found to be normal, postprandial measurements are indicated. Most animals with chronic hepatitis, marked hepatic necrosis, cholestasis, and hepatic neoplasia have abnormal values. SBAs are usually not markedly altered by secondary hepatic disease or with glucocorticoid or anticonvulsant therapy. Some animals without histologic evidence of primary hepatic disease will have markedly increased SBAs. It has been suggested that these animals might have undiagnosed hepatic microvascular dysplasia, but that is uncertain.
Increased SBAs are possibly the most sensitive biochemical indicator of congenital PSS, but the values will not distinguish between PSS and microvascular dysplasia. Rare dogs with PSS can have normal resting and postprandial SBA concentrations.
Urinary Bile Acids
Occasional Indications
Measurement of urinary bile acids (UBAs) may be indicated when samples for fasting and postprandial SBA determinations are difficult to obtain.
Advantages
The client can bring a urine sample into the clinic instead of bringing the patient. Because the urine bile acids : creatinine ratio represents an average SBA value over time, the urine bile acids : creatinine ratio is probably not substantially affected by transient variation in SBA concentrations and appears to be as or more specific than a random single measurement of SBAs. Bilirubin and glucose in the urine are unlikely to interfere with test results. Treatment with ursodeoxycholic acid is not known to interfere with test results.
Disadvantages
The test may not be as sensitive as SBAs.
Analysis
UBAs are measured in urine (approximately 5 ml) using enzymatic methodology; the UBA concentration is standardized for urine flow and concentration by measuring concurrent urine creatinine concentration and calculating the ratio (µmol of urine bile acids/mg of urine creatinine).
Normal Values
Dog, less than 7.3 µmol/g; cat, less than 4.4 µmol/g.
Artifacts
Hematuria and hemoglobinuria may interfere.
Drug Therapy That May Alter UBA Concentrations
None known.
Causes of Low UBAs
Not significant.
Causes of High UBAs
UBA concentrations are increased by the same factors as for SBA.
Blood Ammonia and Ammonia Tolerance Testing
Frequent Indications
Indications for blood ammonia measurement are the same as for SBAs.
Advantages
Blood ammonia test has good sensitivity and specificity.
Disadvantages
There are specific procedural requirements for submitting the samples, and there is a likelihood of vomiting or CNS signs with ATT.
Analysis
Ammonia is measured in blood, serum, plasma (heparinized is recommended), CSF, or urine by enzymatic, selective electrode, dry reagent, and resin absorption methods. There does not appear to be any advantage of arterial over venous blood. Blood must be drawn into an ice-chilled tube, which is stoppered tightly after filling, immediately put back on ice, and promptly taken to the in-house laboratory. Unless the test is well established at the clinic, a control sample should be taken at the same time using the same technique. The test must be performed within 20 minutes, or the plasma must be frozen at −20° C, which stabilizes the ammonia concentration for at least 2 days. If an ATT is to be performed, samples for ammonia determination should be taken before and 30 or 45 minutes after administration of 100 mg NH4Cl/kg of body weight. The NH4Cl may be administered orally (20 to 50 ml of a 5% aqueous solution), as a dry powder in gelatin capsules, or rectally (recommended) as a 5% solution.
Warning: Administration of NH4Cl to patients with increased resting blood ammonia concentrations may cause encephalopathy. The clinician should not perform ATT if the patient is showing obvious encephalopathic signs or is hyperammonemic. Lack of obvious encephalopathic signs does not guarantee that blood ammonia levels are normal. The ATT is not recommended in cats.
Normal Values
Resting blood ammonia: dogs, 45 to 120 µg/dl; cats, 30 to 100 µg/dl. ATT, ammonia at 30 minutes: dogs, minimal change from normal values.
Danger Values
Dogs, greater than 1000 µg/dl (hepatic encephalopathy may be imminent, although poor correlation exists between clinical signs of encephalopathy and blood ammonia concentrations); cats, unknown.
Artifacts
Blood ammonia concentration may be falsely increased by allowing the blood to stand, and by strenuous exercise (see Chapter 1).
Drug Therapy That May Alter Ammonia
Decreased blood ammonia may be the result of intestinal antibacterial drugs, lactulose, Lactobacillus acidophilus cultures, enemas, and diphenhydramine. Increased blood ammonia may be the result of valproic acid, asparaginase, narcotics, diuretics causing hypokalemia or alkalosis, hyperalimentation, ammonium salts, and high-protein meals (including blood from spontaneous GI bleeding).
Causes of Hyperammonemia
Urea cycle disorders (extremely rare) and hepatic insufficiency (especially congenital or acquired PSS) can cause hyperammonemia. Resting blood ammonia concentrations are probably less sensitive than SBAs in detecting hepatic dysfunction, whereas the ATT is possibly as sensitive as preprandial and postprandial SBAs in detecting PSS. A significantly increased fasting blood ammonia concentration is specific for hepatic insufficiency and renders an ATT unnecessary. Clinical signs are not well correlated with blood ammonia concentrations. An abnormal ATT result or resting blood ammonia concentration in a patient with hepatic disease is generally an indication for imaging (e.g., ultrasound, scintigraphy) ± hepatic biopsy. Rarely, blood ammonia is increased because of urinary tract obstruction, especially if complicated by infection with urease-producing bacteria. Some young dogs (notably Scottish deerhounds in Great Britain) have elevated resting blood ammonia values that spontaneously return to normal as the dog ages. Therefore caution must be used when diagnosing congenital PSS in at least some breeds solely by evaluating the resting blood ammonia concentration.
Protein C
Occasional Indications
Measurement of protein C may help distinguish dogs with congenital PSS from those with hepatic microvascular dysplasia. Protein C concentrations are low in dogs suffering from aflatoxin poisoning.
Advantages
Sensitivity of protein C is less than SBAs for PSS, but the specificity is approximately the same.
Disadvantages
There is limited availability of the test. Protein C testing is currently available at Cornell University Diagnostic Laboratory.
Analysis
Protein C is measured by chromogenic assay performed on citrated plasma (serum gives falsely high values). Samples must be shipped refrigerated or frozen.
Normal Values
75% to 135%.
Artifacts
Hemolysis and lipemia may increase values.
Drug Therapy That May Alter Protein C
Unknown.
Causes of Low Protein C
Protein C is decreased by altered hepatic function and coagulation abnormalities. Protein C less than 70% is suggestive of PSS as opposed to microvascular dysplasia.
Causes of High Protein C
Protein C greater than 70% is suggestive of microvascular dysplasia as opposed to PSS. A protein C value that increased to 70% or greater after corrective surgery for PSS suggests that portal blood is being directed through the liver and not through the shunt.
Hepatic Mineral Analysis
Occasional Indications
Hepatic mineral analysis may be used to distinguish between patients in which copper is the cause of the hepatic disease versus those in which it is the effect of the hepatic disease.
Advantages
Hepatic mineral analysis is more specific and definitive than special stains for copper.
Disadvantages
Hepatic mineral analysis requires 50 mg of liver tissue for analysis.
Analysis
Measurement of hepatic minerals is done by atomic absorption spectroscopy or atomic emission spectroscopy.
Normal Values
Less than 400 µg/g dry weight of liver.
Artifacts
Measurement of hepatic minerals may be affected by an inadequate tissue sample or a contaminated sample.
Drug Therapy That May Alter Mineral Analysis
Unknown.
Interpretation
Secondary hepatic copper retention from cholestasis may range from 400 to 1000 µg/g. Hereditary copper-associated hepatopathies can range from 750 µg/g and higher (often in the several thousands).
Weight Loss or Anorexia of Unknown Cause
Weight loss has many causes (Box 9-9 ). Concurrent problems with fewer potential causes (e.g., regurgitation, vomiting, diarrhea, icterus) should be considered first. If a patient had a reasonable appetite when weight loss began, major differential diagnoses are small intestinal disease, maldigestion, hepatic disease, increased use of calories (e.g., hyperthyroidism, lactation), increased loss of calories (e.g., diabetes mellitus) or caloric-deficient diet. If no other identifiable problems (other than weight loss or anorexia) can be pursued, a systematic search is indicated (Figure 9-13 ). One should first preclude as many causes as possible with the history and physical examination (i.e., lack of food, calorie-deficient food, inability to eat, regurgitation, vomiting and diarrhea). Next, extensive clinicopathologic screening is indicated. Imaging is considered an extension of the physical examination, and abdominal ultrasound plus thoracic radiographs are appropriate. Thoracic radiographs may be very revealing, even if a patient does not have coughing or abnormal lung sounds. Abdominal ultrasonography is particularly desirable and often more useful than radiographs, assuming the operator is accomplished. If laboratory or radiographic abnormalities are not present or are unconvincing, one may repeat the tests at 1- to 3-week intervals, depending on the clinical condition of the patient, or immediately proceed to function tests, biopsies, or both. Certain hepatic and adrenal gland diseases may require such function tests. It is noteworthy that severe gastric or intestinal disease may cause anorexia or severe weight loss without vomiting or diarrhea, respectively.
Box 9-9. Major Causes of Weight Loss in Dogs and Cats.
Lack of Calories (inadequate food or poor-quality food)
Inability or Refusal to Eat
Dysphagia
Oral lesion
Anorexia for any reason
Regurgitation
Pharyngeal or esophageal disease
Vomiting (see Box 9-2 )
Maldigestion (EPI)
Intestinal Malabsorption (does not always cause diarrhea)
Malassimilation (organ failure)
Hepatic failure
Cardiac failure
Diabetes mellitus
Uremia
Cancer cachexia syndrome
Hypoadrenocorticism
Excessive Use or Loss of Calories
Hyperthyroidism
Excessive demand for calories because of environment or exertion
Lactation
Muscle Wasting
Myopathy
Neuropathy
FIGURE 9-13.

Diagnostic approach to chronic weight loss in dogs and cats when no other abnormalities are found on history or physical examination and the animal is not ingesting adequate calories (see Box 9-9). ACTH, Adrenocorticotropic hormone; ANA, antinuclear antibodies; CBC, complete blood count; CSF, cerebrospinal fluid; CT, computed tomography; EMG, electromyogram; FeLV, feline leukemia virus; FIV, feline immunodeficiency virus; T3, triiodothyronine; TLI, trypsin-like immunoreactivity; WBC, white blood cell.
Gastroduodenoscopy and ileoscopy plus biopsy are reasonable in patients with severe weight loss of unknown cause. Some cases with gastric neoplasia may present only for anorexia and weight loss. Clinicians without access to endoscopic equipment may consider exploratory laparotomy. If surgery is performed, gastric, duodenal, jejunal, ileal, mesenteric lymph node, and hepatic biopsies are usually appropriate, regardless of a normal gross appearance of the organs. In cats, the pancreas should also be biopsied.
Cancer cachexia can be particularly difficult to diagnose. It is a poorly defined, multifaceted syndrome that may involve loss of taste, malabsorption, increased metabolism with energy wasting, and other mechanisms. Almost any tumor can cause cancer cachexia, and no consistent laboratory findings exist. The causative cancer may be large or small, focal or diffuse; lymphomas and carcinomas are probably the most common causes.
Anorexia of unknown cause is similar to weight loss in being difficult to evaluate if no other identifiable abnormalities are seen. The diagnostic approach is similar to that for chronic weight loss (see Figure 9-13; Box 9-10 ). Anorexia can be divided into three categories: (1) inability to eat (due to oral, pharyngeal, or esophageal disease), (2) primary anorexia (rare) associated with a primary CNS disorder, and (3) secondary anorexia (the most common), which is caused by systemic or metabolic disease.
Box 9-10. Categories of Diseases that Cause Anorexia.
Psychologic (especially cats)
Inability to Smell Food (Anosmia)
Dysphagia
Systemic Inflammation
Etiologic agent (e.g., viral, bacterial, fungal, rickettsial, parasite)
Immune-mediated disease
Neoplasia
Necrosis
Iatrogenic (drugs)
Alimentary or Abdominal Disease Causing Nausea or Pain
Gastritis/enteritis
Neoplasia
Toxins
Exogenous (various)
Endogenous (e.g., primarily due to organ failure)
Endocrine Disease
Hypoadrenocorticism
Hyperthyroidism
Central Nervous System (CNS) Disease
Primary
Secondary
If necessary, one may elect a therapeutic trial to treat for a suspected problem in a patient in whom a diagnosis cannot be made. It is vital that one design such therapy so that it is safe and extremely likely to succeed if the presumptive disease is present. Then, if the trial fails, one may rule out that disease and go on to treat for something else. To do this, the clinician must be sure that the dose and duration of the treatment are sufficient.
Abdominal Pain
History, physical examination, radiographs, and ultrasonography are the initial tools in diagnosing the cause of abdominal pain (Figure 9-14 ). Extra-abdominal diseases (e.g., spinal problems) and patients predisposed to nonsurgical diseases (e.g., pancreatitis) must be identified early.
FIGURE 9-14.

Diagnostic approach to abdominal pain in the dog and cat. CBC, Complete blood count; spec PL, immunoreactive pancreatic lipase.
In patients with severe, progressive, acute abdomen (severe unrelenting pain or shock or stupor in a deteriorating patient), surgery is often indicated as soon as fluid, electrolyte, and acid-base status are acceptable for anesthesia. Imaging is critically important, but extensive laboratory testing is unlikely to identify the more common causes of acute abdomen (e.g., intestinal obstruction, gastric dilation and volvulus, peritonitis, organ ischemia, tumor, sepsis, or bleeding) and usually only delays surgical resolution of disease. Abdominal exploration offers a good chance for definitive diagnosis plus resolution of the disease process.
Note.
These maladies do not always present as surgical emergencies.
If a patient is not in severe pain and the disease is not progressing rapidly, one must differentiate between problems that ultimately necessitate surgery and those that usually do not (e.g., pancreatitis, hepatitis, cholecystitis, upper urinary tract infection, prostatitis, pansteatitis, heavy metal intoxication, Rocky Mountain spotted fever [RMSF]). Abdominal ultrasonography is useful to examine the liver, spleen, pancreas, kidneys, and prostate, as well as to detect peritoneal fluid. If abdominal fluid is present, abdominocentesis or abdominal lavage with cytologic analysis is indicated. If these procedures are not revealing and the problem continues, exploratory surgery may be necessary. Contrast radiographs are rarely useful because thorough abdominal exploration should diagnose almost anything they reveal; finding an abnormality on contrast radiographs is typically just an indication for surgery. In rare situations the exhibited abdominal pain may be referred from other causes such as pulmonary disease or disk disease.
Suggested Readings
- Balkman CE, Center SA, Randolph JF. Evaluation of urine sulfated and nonsulfated bile acids as a diagnostic test for liver disease in dogs. J Am Vet Med Assoc. 2003;222:1368. doi: 10.2460/javma.2003.222.1368. [DOI] [PubMed] [Google Scholar]
- Bridger N, Glanemann B, Neiger R. Comparison of postprandial and ceruletide serum bile acid stimulation in dogs. J Vet Intern Med. 2008;22:873. doi: 10.1111/j.1939-1676.2008.0114.x. [DOI] [PubMed] [Google Scholar]
- Cave NJ. Evaluation of a routine diagnostic fecal panel for dogs with diarrhea. J Am Vet Med Assoc. 2002;221:52. doi: 10.2460/javma.2002.221.52. [DOI] [PubMed] [Google Scholar]
- Chouicha N, Marks S. Evaluation of five enzyme immunoassays compared with the cytotoxicity assay for diagnosis of Clostridium difficile-associated diarrhea in dogs. J Vet Diagn Invest. 2006;18:182. doi: 10.1177/104063870601800207. [DOI] [PubMed] [Google Scholar]
- Cole TL. Diagnostic comparison of needle and wedge biopsy specimens of the liver in dogs and cats. J Am Vet Med Assoc. 2002;220:1483. doi: 10.2460/javma.2002.220.1483. [DOI] [PubMed] [Google Scholar]
- Gerhardt A. Comparison of the sensitivity of different diagnostic tests for pancreatitis in cats. J Vet Intern Med. 2001;15:329. [PubMed] [Google Scholar]
- German AJ, Day MJ, Ruaux CG. Comparison of direct and indirect tests for small intestinal bacterial overgrowth and antibiotic-responsive diarrhea in dogs. J Vet Intern Med. 2003;17:33. doi: 10.1892/0891-6640(2003)017<0033:codait>2.3.co;2. [DOI] [PubMed] [Google Scholar]
- Gerritzen-Bruning MJ, Van Den Ingh SGAM, Rothuizen J. Diagnostic value of fasting plasma ammonia and bile acid concentrations in the identification of portosystemic shunting in dogs. J Vet Intern Med. 2006;20:13. doi: 10.1892/0891-6640(2006)20[13:dvofpa]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Gookin JL, Foster DM, Poore MF. Use of a commercially available culture system for diagnosis of Tritrichomonas foetus infection in cats. J Am Vet Med Assoc. 2003;222:1376. doi: 10.2460/javma.2003.222.1376. [DOI] [PubMed] [Google Scholar]
- Hall EJ, German AJ. Diseases of the small intestine. In: Ettinger SJ, Feldman EC, editors. Textbook of veterinary internal medicine. ed 7. WB Saunders; Philadelphia: 2010. [Google Scholar]
- Jergens AE, Schreiner CA, Frank DE. A scoring index for disease activity in canine inflammatory bowel disease. J Vet Intern Med. 2003;17:291. doi: 10.1111/j.1939-1676.2003.tb02450.x. [DOI] [PubMed] [Google Scholar]
- Kimmel SE, Washabau RJ, Drobatz KJ. Incidence and prognostic value of low plasma ionized calcium concentration in cats with acute pancreatitis: 46 cases. J Am Vet Med Assoc. 2001;219:1105. doi: 10.2460/javma.2001.219.1105. [DOI] [PubMed] [Google Scholar]
- Marks SL. Genotypic and phenotypic characterization of Clostridium perfringens and Clostridium difficile in diarrheic and healthy dogs. J Vet Intern Med. 2002;16:533. doi: 10.1892/0891-6640(2002)016<0533:gapcop>2.3.co;2. [DOI] [PubMed] [Google Scholar]
- Mekaru S, Marks S, Felley A. Comparison of direct immunofluorescence, immunoassays, and fecal flotation for detection of Cryptosporidium spp. and Giardia spp. in naturally exposed cats in 4 northern California animal shelters. J Vet Intern Med. 2007;21:959. doi: 10.1892/0891-6640(2007)21[959:codiia]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Ruland K, Fischer A, Hartmann K. Sensitivity and specificity of fasting ammonia and serum bile acids in the diagnosis of portosystemic shunts in dogs and cats. Vet Clin Pathol. 2010;39:57. doi: 10.1111/j.1939-165X.2009.00178.x. [DOI] [PubMed] [Google Scholar]
- Stauffer S, Birkenheuer A, Levy M. Evaluation of four DNA extraction methods for the detection of Tritrichomonas foetus in feline stool specimens by polymerase chain reaction. J Vet Diagn Invest. 2008;20:639. doi: 10.1177/104063870802000518. [DOI] [PubMed] [Google Scholar]
- Steiner J, Newman S, Xenoulis P. Sensitivity of serum markers for pancreatitis in dogs with macroscopic evidence of pancreatitis. Vet Ther. 2008;9:263. [PubMed] [Google Scholar]
- Toulza O, Center S, Brooks M. Evaluation of plasma protein C activity for detection of hepatobiliary disease and portosystemic shunting in dogs. J Am Vet Med Assoc. 2006;229:1761. doi: 10.2460/javma.229.11.1761. [DOI] [PubMed] [Google Scholar]
- van Asten A, Allaart J, Grone A. Application of PCR-based detection of Clostridium perfringens cpb2 in fecal samples. Vet Microbiol. 2008;129:215. doi: 10.1016/j.vetmic.2008.01.007. [DOI] [PubMed] [Google Scholar]
- Webster CRL, Cooper JC. Diagnostic approach to hepatobiliary disease. In: Kirk RW, Bonagura JD, Twedt DC, editors. Kirk's current veterinary therapy 14. Saunders; Philadelphia: 2009. [Google Scholar]
- Wilberg ME, Westermarck E. Subclinical exocrine pancreatic insufficiency in dogs. J Am Vet Med Assoc. 2002;220:1183. doi: 10.2460/javma.2002.220.1183. [DOI] [PubMed] [Google Scholar]


