Key Points
-
1
Chronic obstructive pulmonary disease (COPD) refers to fixed airflow obstruction caused by chronic bronchitis (productive cough for at least 3 months of the year for at least 2 consecutive years) or emphysema (destruction of alveoli).
-
2
Tobacco smoking accounts for almost all cases of COPD.
-
3
Precipitants of COPD exacerbations include viral upper respiratory tract infections, bacterial infections (most commonly Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis), pollution, heart failure, pulmonary embolism, and medications (beta‐blockers, narcotics, sedatives).
-
4
There is no universally accepted definition of an acute exacerbation of COPD. The most commonly used definition is worsening dyspnea, an increase in sputum purulence, or an increase in sputum volume in a patient with COPD.
-
5
Symptoms and signs of COPD exacerbations include wheezing, distant breath sounds, tachypnea, tachycardia, accessory muscle use, cyanosis, agitation, confusion, and stupor.
-
6
Initial testing should include pulse oximetry, chest x‐ray, and an electrocardiogram. Other possible tests include arterial blood gas (if the patient's distress or somnolence raises concern for acute respiratory acidosis) and sputum Gram stain and culture (most appropriate for patients who fail to respond to empiric therapy).
-
7
Administer supplemental oxygen if there is hypoxemia. The goal oxygen saturation is 90% to 92% with a corresponding partial pressure of arterial oxygen of 60 to 65 mmHg. Higher oxygen saturations may cause hypercarbia by reducing the respiratory drive and promoting ventilation–perfusion mismatching.
-
8
Beta‐agonists and anticholinergic agents are equally efficacious at improving airflow during a COPD exacerbation. Combination therapy is typically used in clinical practice, but does not appear to confer substantial benefit over monotherapy with either agent alone.
-
9
The role of aminophylline (methylxanthine bronchodilator) in the setting of a COPD exacerbation is controversial because this medication has uncertain efficacy and potential toxicity.
-
10
Systemic glucocorticoids improve FEV1 and reduce treatment failure rates and length of hospitalization for a COPD exacerbation. The optimal dose, route, and duration of therapy are unknown.
-
11
Patients with a severe COPD exacerbation are the ones most likely to benefit from antibiotics, although the effect of antibiotics on the duration and severity of the exacerbation appears minimal. There are no definitive data regarding optimal duration of therapy.
-
12
Mucolytic agents and mechanical chest percussion are probably not beneficial in patients with a COPD exacerbation.
-
13
Many patients do not use metered‐dose inhalers correctly. We recommend spacers to all patients, especially when inhaled glucocorticoids are prescribed.
-
14
Smoking cessation should be discussed. The pneumonia and influenza vaccines should be administered at the follow‐up clinic visit, if applicable.
Definitions.
Chronic bronchitis: Productive cough for at least 3 months of the year for at least 2 consecutive years. Other causes of chronic cough, such as gastroesophageal reflux disease, postnasal drip, and bronchiectasis, must be excluded.
Emphysema: Destruction of alveoli and abnormal distension of air spaces distal to the terminal bronchioles.
Chronic obstructive pulmonary disease (COPD): Fixed (not fully reversible), chronic airflow obstruction caused by chronic bronchitis or emphysema.
Epidemiology
COPD is a morbid, expensive, and lethal medical condition, affecting an estimated 16 million adults and accounting for 1.4 million emergency room visits in 1998. COPD was directly responsible for 1.9% of hospitalizations in 1998 and was a contributing cause of an additional 7% of hospitalizations during that year. Deaths related to COPD have been increasing steadily in the United States over the past 20 years, especially among women. COPD is now the fourth leading cause of death in the United States.
Pathogenesis
Tobacco smoking accounts for almost all cases of COPD. Cigarette smoke increases the number of neutrophils and macrophages in the airways. These cells release proteases (enzymes that degrade proteins), which destroy lung parenchyma in individuals who are unable to mount an adequate anti‐protease response. As a result, mucus production is increased and airways become narrowed, lose their support structure, and develop increased collapsibility that leads to airway obstruction.
During an acute exacerbation of COPD, inflammation, bronchospasm, and mucus hypersecretion lead to airway narrowing, worsening ventilation–perfusion (V/Q) mismatching, and hypoxemia. The work of breathing increases to overcome the high airway resistance, but this leads to increased oxygen consumption by the respiratory muscles, which further lowers the oxygen content in venous blood.
Precipitants
COPD exacerbations become more frequent with increasing disease severity. An important trigger of these exacerbations is viral upper respiratory tract infections (especially rhinovirus), which cause airway inflammation and oxidative stress (Box 15‐1 ). Although bacteria are often cultured from patients with an acute COPD exacerbation, it is unclear whether these organisms are pathogens or colonizers, because bacteria can also be cultured from many patients with stable COPD. The most common pathogenic bacteria are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. COPD exacerbations are more common in the winter (upper respiratory tract infections are more common during these months, and cold temperatures to cause a small reduction in lung function). Exacerbations have also been linked to increasing environmental pollution, which is thought to increase susceptibility to viral respiratory infections.
Box 15‐1. Causes of Chronic Obstructive Pulmonary Disease Exacerbations.
Infection
Viruses
Rhinovirus (common cold)
Influenza
Parainfluenza
Coronavirus
Adenovirus
Respiratory syncytial virus
Chlamydia pneumoniae
Bacteria
Haemophilus influenza
Streptococcus pneumoniae
Moraxella catarrhalis
Staphylococcus aureus
Pseudomonas aeruginosa
Common Pollutants
Nitrogen dioxide
Particulates
Sulfur dioxide
Ozone
Medications
Sedatives and narcotics—reduce respiratory drive
Beta‐blockers
Other
Congestive heart failure
Pulmonary embolism
Cold temperature—causes a small but significant reduction in lung function
Pneumothorax
No precipitant identified
Adapted with permission from Wedzicha JA. Exacerbations: Etiology and pathophysiologic mechanisms. Chest 2002;121:136S–141S.
Other precipitants of COPD exacerbations include heart failure, pulmonary embolism, and medications. Beta‐blockers may cause bronchospasm, which can worsen ventilation–perfusion mismatch. Narcotics and sedatives may reduce the ventilatory drive, leading to hypercarbia, acidosis, and respiratory failure.
Diagnosis
There is no universally accepted definition of an acute exacerbation of COPD. The most commonly used definition, which has been used most consistently in rigorous clinical trials, is any combination of the following three clinical findings in a patient with established COPD:
-
1
Worsening dyspnea
-
2
An increase in sputum purulence
-
3
An increase in sputum volume
Hypoxemia and hypercarbia are often present.
Signs
Mild COPD exacerbations may present with minimal signs, such as wheezing on auscultation. As the severity of COPD worsens, the breath sounds may be distant and there may be signs of hypoxemia including cyanosis, tachypnea, agitation, and tachycardia. Accessory muscle use may occur with the increased work of breathing. Inward abdominal motion with inspiration (abdominal paradox) is a sign of impending diaphragmatic muscle fatigue. With worsening respiratory failure, patients become increasingly hypercarbic and acidemic, which leads to confusion, stupor, and ultimately, apnea.
Laboratory Data
Initial laboratory testing should include:
-
1
Pulse oximetry to monitor the level of hypoxemia
-
2
Chest x‐ray
The classic findings of COPD include hyperinflated lungs, flattened diaphragms, and a narrowed and lengthened mediastinum. A chest x‐ray should be obtained in all patients presenting with a COPD exacerbation because findings on radiography have been shown to change short‐term management in as many as 20% of these patients, most of whom have new pulmonary infiltrates or evidence of heart failure.
-
3
Arterial blood gas (ABG)
Most COPD exacerbations do not require ABG measurements. An ABG analysis is appropriate if the patient's distress or somnolence raises concern for acute respiratory acidosis, but the ABG should never delay intubation.
Patients with stable COPD may have a chronic respiratory acidosis from long‐standing carbon dioxide retention as a result of airway obstruction. ABG analysis in these patients shows an increased partial pressure of arterial carbon dioxide (PaCO2) but normal arterial pH, because the kidneys buffer the acid by retaining bicarbonate. Patients with a superimposed acute respiratory acidosis will have a reduced arterial pH and higher PaCO2 compared to their baseline measurements, because the kidneys are unable to buffer the acid resulting from acute carbon dioxide retention.
-
4
Electrocardiogram (ECG)
An admission ECG is recommended to rule out cardiac conditions, such as ischemia or acute myocardial infarction that may be contributing to the COPD exacerbation. Continuous cardiac monitoring is appropriate in patients with a moderate or severe COPD exacerbation, patients with a significant history of coronary artery disease, or patients with known cardiac arrhythmias, such as multifocal atrial tachycardia or atrial fibrillation.
-
5
Sputum gram stain and culture
White sputum may suggest a nonbacterial cause of the COPD exacerbation whereas green sputum may suggest a bacterial infection. However, sputum samples are notoriously unreliable, because they do not distinguish infection from colonization or oropharyngeal contamination. Therefore, sputum Gram stain and culture should be reserved for patients who do not respond to empiric therapy.
-
6
Spirometry
Spirometry is not recommended during a COPD exacerbation, because this technique does not provide a reliable measure of disease severity nor is it useful for guiding therapy.
Acute Treatment (Table 15‐1, Fig. 15‐1)
Table 15‐1.
Inpatient Management of an Acute Exacerbation of Chronic Obstructive Pulmonary Disease: Recommendations from Professional Societies
| British Thoracic Society | American College of Chest Physicians and American College of Physicians–American Society of Internal Medicine | European Respiratory Society | American Thoracic Society | Global Initiative for Chronic Obstructive Lung Disease (GOLD) | |
|---|---|---|---|---|---|
| Date of statement | 1997 | 2001 | 1995 | 1995 | 2001 |
| Type of statement | Consensus | Evidenced‐based review | Consensus | Consensus | Evidenced‐based review |
| Diagnostic testing | Chest x‐ray, arterial blood gas, complete blood count, electrolytes, ECG, sputum culture, FEV1 or peak flow | Chest x‐ray (spirometry is not recommended) | Chest x‐ray, arterial blood gas, complete blood count, electrolytes, ECG, sputum gram stain and culture, FEV1 | Sputum culture if exacerbation is severe, if condition worsens despite antibiotics, or if patient is a nursing home resident | Chest x‐ray, arterial blood gas, hematocrit, electrolytes, ECG, sputum culture |
| Bronchodilators | Beta‐agonists and anticholinergic agents. IV aminophylline if no response | Start with an anticholinergic agent. Add beta‐agonist if maximal dose of the anticholinergic is inadequate. (Methylxanthines not recommended) | Beta agonists and anticholinergic agents. IV aminophylline in severe exacerbations | Start with beta‐agonist ± anticholinergic agent. Add IV aminophylline if inadequate response | Start with beta‐agonist. Add anticholinergic agent if prompt response not evident. Oral or IV methylxanthine in severe exacerbations |
| Antibiotics | For moderate or severe exacerbations. Broader spectrum antibiotics if no response to first‐line agents* | Optimal duration unclear | Inexpensive antibiotic for 7–14 days* | “Simple” antibiotic* for abnormal mucus. Broader spectrum antibiotic for severe exacerbations | Antibiotic choice based on local sensitivity for S. pneumoniae, H. influenzae, M. catarrhalis |
| Glucocorticoids | Prednisone 30 mg daily for 7–14 days | Systemic for up to 2 weeks | Recommended, IV if severe exacerbation | Recommended, reassess use after 1–2 weeks | Oral or IV prednisolone daily for 10–14 days |
| Mucolytic drugs | Not recommended | Not recommended | Not recommended | Not recommended | Not discussed |
From Stoller JK. Acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med. 2002;346:988–994. Copyright © 2002 Massachusetts Medical Society. All rights reserved. Adapted with permission, 2005.
Examples: amoxicillin, tetracycline, doxycycline.
ECG, electrocardiogram; FEV1, forced expiratory volume in 1 second.
Figure 15‐1.
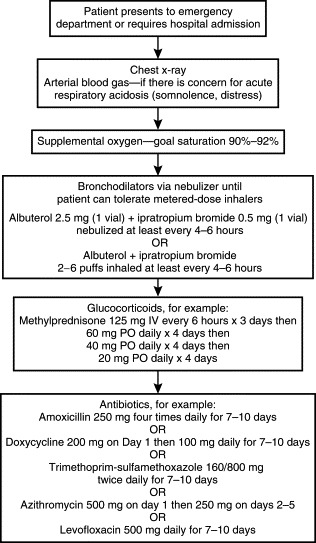
Initial treatment of an acute exacerbation of chronic obstructive pulmonary disease requiring hospitalization. Combination therapy is typically used in clinical practice but does not appear to confer substantial benefit over monotherapy with either agent alone.
Supplemental Oxygen
Supplemental oxygen is appropriate if the COPD exacerbation is accompanied by hypoxemia. Oxygen saturation should be maintained between 90% and 92% with a corresponding partial pressure of arterial oxygen (PaO2) of 60 to 65 mm Hg. These targets ensure near‐maximal hemoglobin saturation. Higher oxygen saturations may cause hypercarbia by reducing the respiratory drive and promoting ventilation–perfusion mismatching.
There are several methods for delivering supplemental oxygen. Nasal cannula provides up to 6 L of oxygen per minute, although the actual percentage of oxygen inspired will depend on other factors, such as mouth‐breathing. The concentration of oxygen in room air is 21%. As a general rule of thumb, for every 1 L of oxygen delivered per minute via nasal cannula, the inspired fraction of oxygen increases by 4%. The maximum oxygen delivery via nasal cannula is approximately 40%.
Non‐rebreather face masks provide tighter control of inspired oxygen than nasal cannula. A partial non‐rebreather mask has a reservoir that typically delivers 60% to 80% inspired oxygen. The reservoir bag is filled with oxygen that is emptied with inspiration. Exhalation fills the reservoir with the first portion of expired gas, which contains a high oxygen concentration derived from the dead space of the upper airway. A true non‐rebreather mask contains two types of valves and can deliver close to 100% oxygen. One valve prevents exhaled gas from entering the reservoir bag. The second type of valve permits exhalation and prevents ambient air from entering the inhalation circuit.
Bronchodilators
Beta2‐agonists (albuterol) and anticholinergic agents (ipratropium bromide) are bronchodilators that are equally effective at improving airflow during a COPD exacerbation. These medications are commonly used together, although combination therapy does not appear to confer substantial benefit over monotherapy with either agent alone. Metered‐dose inhalers (MDIs) and nebulizers appear to achieve equivalent bronchodilation, but MDIs cost less.
Aminophylline, a methylxanthine bronchodilator, has unclear efficacy and potential toxicity. Therefore, the role of this medication in the setting of a COPD exacerbation is unclear.
Glucocorticoids
Several good quality randomized trials have shown that systemic glucocorticoids are beneficial during an acute COPD exacerbation. Systemic glucocorticoids improve FEV1 and reduce treatment failure rates and length of hospitalization. The shortest useful duration of therapy is unknown, but there appears to be no additional advantage when glucocorticoids are given for more than 2 weeks. Oral and parenteral glucocorticoids appear to have similar efficacy. Improved outcomes have been demonstrated with doses ranging from 40 mg of oral prednisone daily in outpatient and emergency department settings to 125 mg of intravenous methylprednisone every 6 hours for 3 days, followed by 60 mg of oral prednisone daily for 4 days and then a gradual tapering of the dose with discontinuation on Day 15 in hospitalized patients. However, the optimal dose, route, and duration of therapy are unknown and vary among physicians and patients.
Hyperglycemia is an important side effect of short‐term glucocorticoid treatment. Patients with frequent exacerbations may also experience bone loss from repeated courses of glucocorticoids. Infection is unlikely with short‐term treatment.
Antibiotics
Bacterial infections may contribute to acute COPD exacerbations. Several randomized trials have shown that patients with severe COPD exacerbations are the most likely to benefit from antibiotics, although the effect of antibiotics on the duration and severity of the exacerbation appears minimal. Trials have most commonly prescribed tetracyclines, amoxicillin, or trimethoprim‐sulfamethoxazole for 3 to 14 days to cover the three most common causal pathogens: S. pneumoniae, M. catarrhalis, and H. influenzae. Nowadays, more broad‐spectrum antibiotics, such as levofloxacin, are commonly used in clinical practice because of emerging antibiotic resistance (especially among S. pneumoniae). The superiority of these newer, broader‐spectrum antibiotics has not been established. There are also no definitive data regarding optimal duration of therapy, so most physicians prescribe antibiotics for 5 to 10 days.
Mucolytic Agents
Several studies have shown no beneficial effects of mucolytic agents or mechanical chest percussion in patients with a COPD exacerbation.
Noninvasive Positive‐Pressure Ventilation (NPPV)
NPPV unloads fatigued ventilatory muscles and reduces the rates of intubation, in‐hospital mortality, and duration of hospitalization. NPPV is appropriate for the COPD patient with acute respiratory acidosis, and worsening dyspnea and oxygenation, provided the patient is cooperative, hemodynamically stable, does not have excessive secretions, and is able to protect the airway. Patients who cannot tolerate NPPV and who have worsening oxygenation or acidemia should be intubated.
Is the Patient Ready for Hospital Discharge?
Patients are ready for hospital discharge when significant clinical improvement has occurred. A useful question to ask the patient is whether the clinical status is close to baseline. Bronchospasm should be minimal or absent, and oxygen saturation with ambulation should not fall below 88%. Patients with persistent hypoxemia despite resolution of symptoms should be discharged with supplemental oxygen via nasal cannula.
Many patients do not use MDIs correctly. Patients may experience difficulty coordinating inhalation with the release of medication from the canister. Therefore, we recommend spacers to all patients, especially when inhaled glucocorticoids are prescribed (Box 15‐2 ).
Box 15‐2. Basic Use of a Metered‐Dose Inhaler (MDI) with a Spacer.
The patient should:
-
•
Shake the inhaler and attach it to the spacer.
-
•
Breath out, then form a seal around the mouthpiece of the spacer.
-
•
Depress the canister, then breathe in slowly through the mouth.
-
•
Hold the breath for 10 seconds or as long as possible.
-
•
Wait a minute or so, then repeat the above steps, if applicable.
-
•
Rinse the mouth after using an inhaled glucocorticoid to reduce the risk of oral candidiasis.
At the followup clinic visit, smoking cessation should be discussed and the conjugated pneumococcal vaccine and influenza vaccines should be administered (if the patient is due for these vaccines). Spirometry before and after a several‐week trial of inhaled glucocorticoids should be used to assess whether the patient's COPD has a reversible component (i.e., whether the patient will benefit from long‐term glucocorticoids).
References
Review Articles and Position Papers
- 1.Palm KH, Decker WW. Acute exacerbations of chronic obstructive pulmonary disease. Emerg Med Clin North Am. 2003;21:331–352. doi: 10.1016/s0733-8627(03)00014-2. [DOI] [PubMed] [Google Scholar]
- 2.Stoller JK. Acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med. 2002;346:988–994. doi: 10.1056/NEJMcp012477. [DOI] [PubMed] [Google Scholar]
- 3.Bach PB, Brown C, Gelfand SE, McCrory DC. Management of acute exacerbations of chronic obstructive pulmonary disease: A summary and appraisal of published evidence. Ann Intern Med. 2001;134:600–620. doi: 10.7326/0003-4819-134-7-200104030-00016. [DOI] [PubMed] [Google Scholar]
Epidemiology
- Mannino DM. COPD: Epidemiology, prevalence, morbidity and mortality, and disease heterogeneity. Chest. 2002;121:121S–126S. doi: 10.1378/chest.121.5_suppl.121s. [DOI] [PubMed] [Google Scholar]
Pathogenesis of Exacerbations
- Wedzicha JA. Exacerbations: Etiology and pathophysiologic mechanisms. Chest. 2002;121:136S–141S. doi: 10.1378/chest.121.5_suppl.136S. [DOI] [PMC free article] [PubMed] [Google Scholar]
Treatment
- 1.Irwin RS, Madison JM. Systemic corticosteroids for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med. 2003;348:2679–2681. doi: 10.1056/NEJMe030034. [DOI] [PubMed] [Google Scholar]
- 2.Snow V, Lascher S, Mottur‐Pilson C. The evidence base for management of acute exacerbations of COPD: Clinical practice guideline. Chest. 2001;119:1185–1189. doi: 10.1378/chest.119.4.1185. [DOI] [PubMed] [Google Scholar]
- 3.Singh JM, Palda VA, Stanbrook MB, Chapman KR. Corticosteroid therapy for patients with acute exacerbation of chronic obstructive pulmonary disease: A systematic review. Arch Intern Med. 2002;162:2527–2536. doi: 10.1001/archinte.162.22.2527. [DOI] [PubMed] [Google Scholar]
- 4.Saint S, Bent S, Vittinghoff E, Grady D. Antibiotics in chronic obstructive pulmonary disease exacerbations: A meta‐analysis. JAMA. 1995;273:957–960. [PubMed] [Google Scholar]
- 5.Callahan CM, Dittus RS, Katz BP. Oral corticosteroid therapy for patients with stable chronic obstructive pulmonary disease: A meta‐analysis. Ann Intern Med. 1991;114:216–223. doi: 10.7326/0003-4819-114-3-216. 6. [DOI] [PubMed] [Google Scholar]
- 6.Niewoehner DE, Erbland ML, Deupree RH, Collins D. Effect of systemic glucocorticoids on exacerbations of chronic obstructive pulmonary disease. Department of Veterans Affairs Cooperative Study Group. N Engl J Med. 1999;340:1941–1947. doi: 10.1056/NEJM199906243402502. [DOI] [PubMed] [Google Scholar]


