Abstract
The pathophysiology of irritable bowel syndrome (IBS) is not completely understood. However, several factors are known to play a role in pathophysiology of IBS such as genetics, diet, gut microbiota, gut endocrine cells, stress and low-grade inflammation. Understanding the pathophysiology of IBS may open the way for new treatment approaches. Low density of intestinal stem cells and low differentiation toward enteroendocrine cells has been reported recently in patients with IBS. These abnormalities are believed to be the cause of the low density of enteroendocrine cells seen in patients with IBS. Enteroendocrine cells regulate gastrointestinal motility, secretion, absorption and visceral sensitivity. Gastrointestinal dysmotility, abnormal absorption/secretion and visceral hypersensitivity are all seen in patients with IBS and haven been attributed to the low density the intestinal enteroendocrine cells in these patients. The present review conducted a literature search in Medline (PubMed) covering the last ten years until November 2019, where articles in English were included. Articles about the intestinal stem cells and their possible role in the pathophysiology of IBS are discussed in the present review. The present review discusses the assumption that intestinal stem cells play a central role in the pathophysiology of IBS and that the other factors known to contribute to the pathophysiology of IBS such as genetics, diet gut microbiota, stress, and low-grade inflammation exert their effects through affecting the intestinal stem cells. It reports further the data that support this assumption on genetics, diet, gut microbiota, stress with depletion of glutamine, and inflammation.
Keywords: Diet, Gut enteroendocrine cells, Gut microbiota, Low grade inflammation, Stress
Core tip: The pathophysiology of irritable bowel syndrome (IBS) is not completely understood. Understanding the pathophysiology of IBS may enable us to find an effective treatment for this disorder. The density of intestinal stem cells is low in patients with IBS. Moreover, the differentiation of stem cells into enteroendocrine cells is abnormal. It seems that these abnormalities in intestinal stem cells is the cause of the low density of enteroendocrine cells seen in patients with IBS. It is believed that the low density of enteroendocrine cells is behind the gastrointestinal dysmotility, abnormal secretion/absorption and hypersensitivity observed in patients with IBS. This review presents the observations that suggest that the factors known to contribute to the pathophysiology of IBS may exert their effects through affecting the intestinal stem cells.
INTRODUCTION
Irritable bowel syndrome (IBS) is a wide spread condition affecting 12.1% of the world population[1,2]. The prevalence of IBS differs considerably between different parts of the world with the lowest prevalence in Asia and the highest in South America[1]. The cardinal symptom of IBS is intermittent abdominal pain accompanied by altered bowel habits and abdominal bloating/distention[3]. There is no biochemical, radiological or clinical test/examination for diagnosing IBS and the IBS diagnosis is based on symptoms assessment[4]. IBS reduces significantly the patients’ quality of life in the same degree as major chronic diseases such heart failure, renal failure, diabetes, and inflammatory bowel disease[2,3]. It has been reported that 12%-14% of primary care patient visit, and 28% of referrals to gastroenterologists are IBS patients[5-7] and consequently IBS patients are more common in the healthcare than patients with diabetes, hypertension or asthma[8,9]. There is no effective treatment for IBS and the available treatment in clinic is directed to symptom relief[4].
Several factors are known to play pivot role in pathophysiology of IBS. These factors are genetics, diet, gut microbiota, gut endocrine cells, stress and low-grade inflammation[2,10]. Abnormalities in the intestinal stem cells has been reported recently[11-13]. The present review aimed at discussing the possibility that the factors known to contribute to the pathophysiology of IBS may exert their effects through affecting the intestinal stem cells. The present review conducted a literature search in MEDLINE (PubMed) covering the last ten years until November 2019, where articles in English were included. Articles about the intestinal stem cells and their possible role in the pathophysiology of IBS are discussed.
FCACORS INVOLVED IN THE PATHOPHYSIOLOGY OF IBS
Genetics
Studies of family history and family cluster as well as twin studies provided strong evidences that IBS is hereditary[14-21]. However, the possible mutant gene(s) responsible for IBS is/are not found yet[2].
Diet
Patients with IBS avoid certain food items as they believe they worsen/trigger their symptoms[22-26]. However, there is no difference in intake of calories, or the meal patterns between IBS patients and community controls[23,27,28].
The effect of diet on IBS symptoms cannot be explained by food allergy/ intolerance[29]. However, it is generally accepted that poorly absorbed carbohydrates and fibers play an important role in development IBS symptoms[29,30]. The intake of low fermentable oligo-, di-, monosaccharides and polyols-diet and National Institute for Health and Care Excellence-modified diet improve both symptoms and quality of life in IBS patients[22,29,31,32]. However, a recent review and meta-analysis showed that there is very low quality evidence showing that low fermentable oligo-, di-, monosaccharides and polyols diet reliefs IBS symptoms[33].
Based on a case report published in 1978, non-celiac gluten sensitivity was coined[34-36]. In this case, a patient without celiac disease, suffered from abdominal pain and diarrhea who experienced symptoms improved when she used gluten-free diet. Several studies showed that withdrawal of wheat products in patients with non-celiac IBS-like symptoms improve these symptoms[37-42]. However, a double-blind placebo-controlled study showed that it is fructan in the wheat rather than gluten that trigger IBS symptoms[43]. In a recently published meta-analysis concluded that there is insufficient evidence that gluten-free diet improves IBS symptoms[33].
Gut microbiota
The gastrointestinal microbiota comprises 12 different bacteria phyla, but most of the gut bacteria belongs to the Proteobacteria, Firmicutes, Actinobacteria and Bacteroidetes[44,45]. The anaerobic Firmicutes and Bacteroidetes phyla dominate the bacterial population in the intestinal of healthy adults, with a few members from of the Proteobacteria and Actinobacteria phyla[45,46]. A low microbial diversity in the gut (dysbiosis) has been reported to be associated with several diseases[47,48].
In healthy subjects, the intestinal microbiota composition is affected by the individual genetic composition and environmental factors one is exposed for[44,48]. The intestinal microbiota in IBS patients differs from that of healthy subjects[48-51], and have a lower diversity (dysbiosis)[48-51]. It is believed that this difference in the intestinal microbiota plays a pivot role in the pathophysiology of IBS[49].
Gastrointestinal endocrine cells
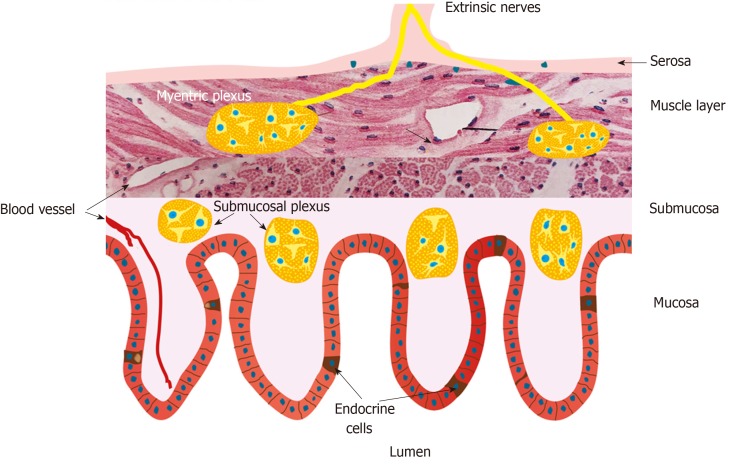
The gastrointestinal endocrine cells are scattered in-between the epithelial cells facing the gut lumen (Figure 1)[52-54].These cells are localized to the stomach, small-and large intestine[53]. Among the different segments of the gastrointestinal tract the density of the endocrine cells is highest in the duodenum (Figure 2)[25]. These cells secret over 10 different hormones that interact and integrate with the enteric, autonomic and central nervous system to regulate: Gastrointestinal motility, secretion of enzymes and bile acid, absorption of nutrients, visceral sensation, gastrointestinal cell proliferation, local immune defense and appetite[3,22,52,55-69]. These cells have sensory microvilli that project into the gastrointestinal lumen that sense gastrointestinal lumen contents and respond by releasing their hormones into the lamina propria[70-82]. These hormones can act locally on the nearby structures (paracrine mode of action) or reach the blood stream and act on far structure (endocrine mode of action)[70-82].
Figure 1.
Schematic illustration of the enteroendocrine cells and their anatomic relation to the enteric nervous system. The enteroendocrine cells are scattered among the epithelial cells lining the intestinal lumen. They interact and intergrade with each other’s and with enteric nervous system. Reproduced from El-Salhy et al[54] by permission of the authors and the publisher.
Figure 2.
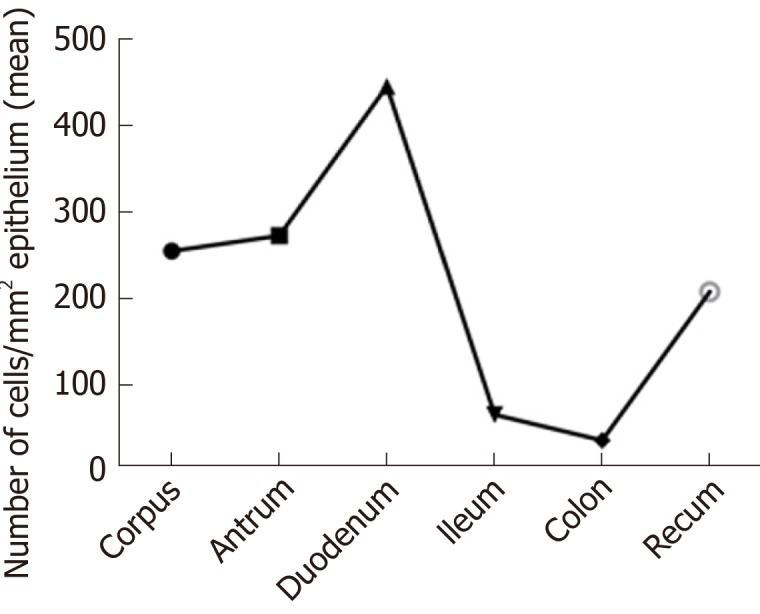
The density of gut endocrine cells as detected by chromogranin a immunoreactivity. Reproduced from El-Salhy et al[25] by permission of the authors and the publisher.
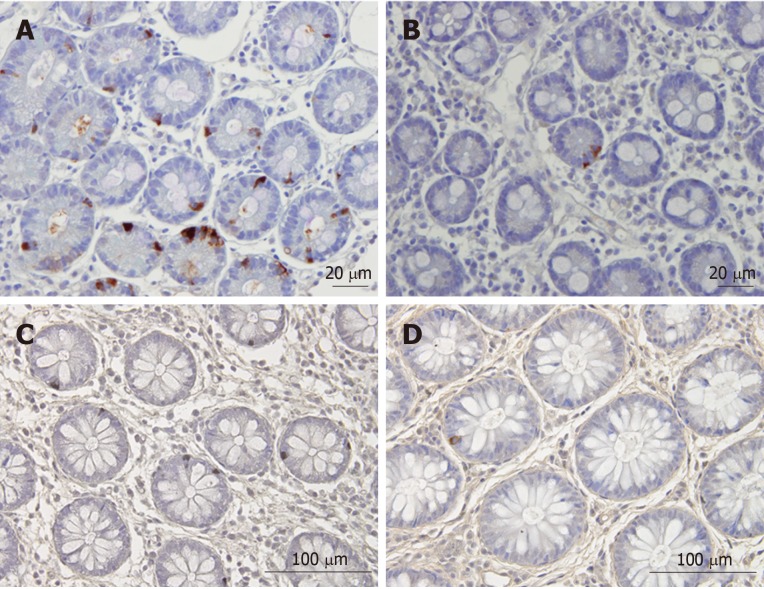
Several abnormalities in different endocrine cell types of the stomach, small- and large intestine have been described in IBS patients (Figure 3)[53,83-97]. Generally, IBS patients have a lower gut endocrine cell density than healthy subjects[52].
Figure 3.
Chromogranin immunoreactive cells in the duodenum of a healthy subject and of a patient with irritable bowel syndrome. A: Chromogranin immunoreactive cells in the duodenum of a healthy subject; B: Chromogranin immunoreactive cells in the duodenum of a patient with irritable bowel syndrome (IBS); C: Chromogranin A cells in the colon of a healthy control; D: Chromogranin A cells in the colon of a patient with IBS. Chromogranin A is a common marker for enteroendocrine cells. The density of Chromogranin A in the duodenum and colon of patients with IBS is lower than that of healthy subjects.
Stress
Stress is defined as an acute threat, real or perceived, to the homeostasis of an organism[10]. Stress is a known factor that trigger/worsen the IBS symptoms[98]. The exact mechanisms by which stress affects IBS are not exactly known. However, the negative effect of stress on IBS symptoms is believed to be caused by an interaction between the gut and the central nervous system (gut-brain axis)[10].
Low grade inflammation
Intestinal low-grade inflammation is believed to be a factor that contribute to the pathophysiology of IBS[86]. Low‐grade inflammation in the intestinal mucosa occurs only in a subset of IBS, i.e., post-infectious IBS, but not in sporadic (non-specific) IBS[86,99-102].
THE ROLE OF INTESTINAL STEM CELLS IN THE PATHOPHYSIOLOGY OF IBS
Intestinal stem cells
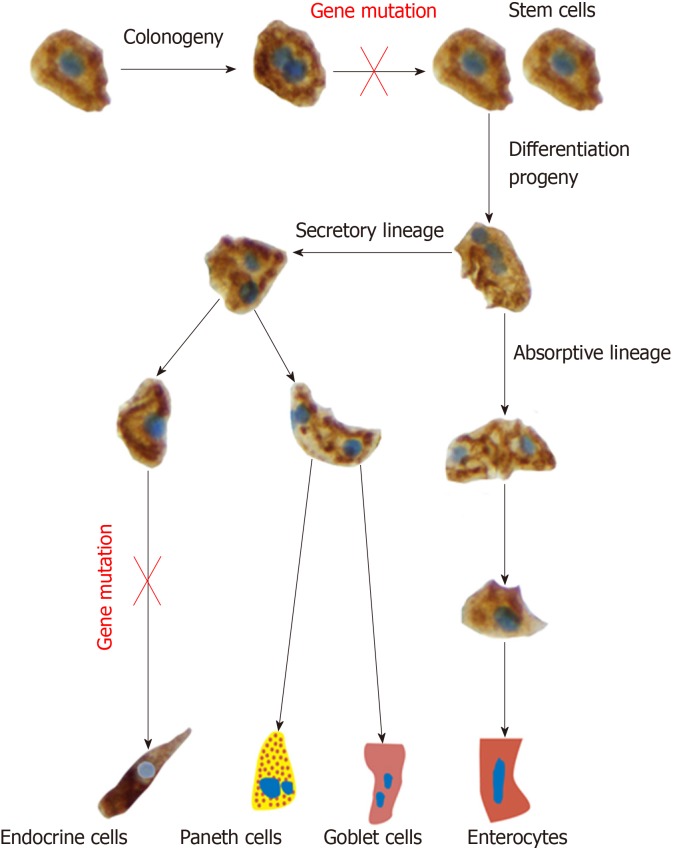
Each intestinal crypt contains four to six pluripotent (stem) cells[103]. Stem cell perform 2 activities, namely self-renewal by dividing into identical stem cell (clonogeny) to maintain a constant number of stem cells and differentiation progeny[103]. In the differentiation progeny, the stem cells differentiate into all cell types of the villus epithelium through 2 cell lineages: The secretory lineage giving raise to goblet cells, endocrine cells and Paneth cells, and the absorptive lineage giving raise to absorptive enterocytes. This differentiation takes place through a series of precursors (progenitors) (Figure 4)[68,69,104-112].
Figure 4.
The intestinal stem cell divides into 2 identical cells (clonogeny). One of these cells remain inactive, while the other stem cell differentiates into all cell types of the villus epithelium through 2 cell lineages: The secretory lineage giving raise to goblet cells, endocrine cells and Paneth cells, and the absorptive lineage giving raise to absorptive enterocytes. This differentiation occurs through a series of progenitors. The observations that the density of stem cells and progenitors for enteroendocrine cells, led to the assumption of gene mutations affecting the stem cell and neurogenin 3 gene.
The relation between the abnormalities in intestinal stem cells and enteroendocrine cells
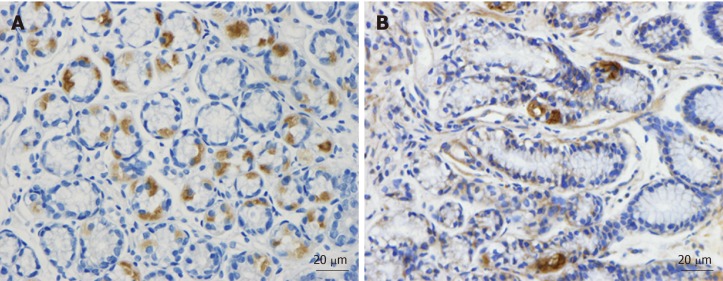
As mentioned previously, the densities of the gastrointestinal endocrine cells are lower than that of healthy subjects[53,83-97]. The cell density of Musashi 1, and neurogenin 3 immunoreactive cells in the small and large intestine of patients with IBS are lower than that of healthy subjects (Figures 5 and 6)[11-13]. Musashi 1 is marker for intestinal stem cells and their early progeny, and neurogenin 3 is expressed in early intestinal endocrine cell progenitors originated from stem cells[103,113-118]. The low densities of enteroendocrine cells in patients with IBS could be explained by the abnormalities in intestinal stem cells[119]. Thus, low densities of Msi-1 and NEUROG3 small and large intestine in IBS patients indicate that the intestinal stem cells in these patients exhibit reduced clonogenic activity and low differentiation progeny toward endocrine cells[119,120].
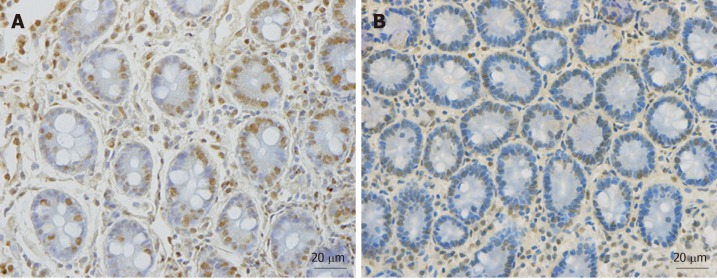
Figure 5.
Musashi 1 immunoreactive cells in duodenum. A: A healthy subject; B: A patient with irritable bowel syndrome (IBS). Musashi 1 is a marker for intestinal stem cells and their early progeny. The density of Musahi 1 cells in healthy subjects is higher than that of the IBS patients. Furthermore, Musashi 1 cells in healthy subjects appear to have more proliferation activity than that of IBS patients.
Figure 6.
Neurogenin 3 immunoreactive cells in the duodenum. A: A healthy control; B: A patient with irritable bowel syndrome. Neurogenin 3 is expressed in the nuclei (brown) of early intestinal endocrine cell progenitors. The healthy subjects have higher density of neurogenin 3 than irritable bowel syndrome patients.
HYPOTHESIS
Based on the data presented above, one may hypothesized that IBS patients may have a gene mutation controlling the number of the stem cells and/or NEUROG3 gene mutation. Furthermore, environmental factors such as diet, inflammation, stress and gut microbiota may affect the stem cells and their progeny (Figure 7). This hypothesis gets support from the following facts: (1) Low density of intestinal endocrine cells has been described in patients with congenital malabsorptive diarrhoea, which is an autosomal recessive disorder[121]. The low density of intestinal endocrine cells in this disorder is caused by loss-of-function mutations in NEUROG3 gene[121]. Similarly, low density of intestinal endocrine cells has been observed in small-intestine allograft rejection, and in NEUROG3-knockout mice[117,120]. The low density of intestinal endocrine cells in these conditions was associated with a reduction in number of intestinal neurogenin 3 cells[117,120]; (2) Changing from the common Norwegian diet to a National Institute for Health and Care Excellence-modified diet, which improved symptoms and quality of life in IBS patients is associated with changes in the densities of gastrointestinal cells[91,122-127]; (3) Modulation of the intestinal microbiota by fecal microbiota transplantation improved both symptoms and the quality of life in patients with IBS[128]. This improvement was accompanied by a change in in the densities of enteroendocrine cells[128]; (4) Glutamine is the main energy source for intestinal enterocytes and plays a major role in intestinal homeostasis and other physiological functions[129-133]. Stress, infection or inflammation cause a depletion of glutamine[129-133] In a randomized placebo-controlled study, dietary glutamine supplements improved symptoms in patients with post-infectious IBS[134]. Glutamine have a trophic effect on the intestinal stem cells and promotes stem cell differentia-tion[129,135,136]. One may speculate that stress results in the depletion of glutamine, which causes disturbance in the differentiation of the intestinal cells. This in turn would cause low density in enteroendocrine cells and the development of IBS symptoms; and (5) In animal models of human ulcerative colitis and Crohn’s disease, the changes in enteroendocrine cells have been found to be strongly correlated with changes in the intestinal stem cells and their differentiation progeny toward intestinal endocrine cells[137,138].
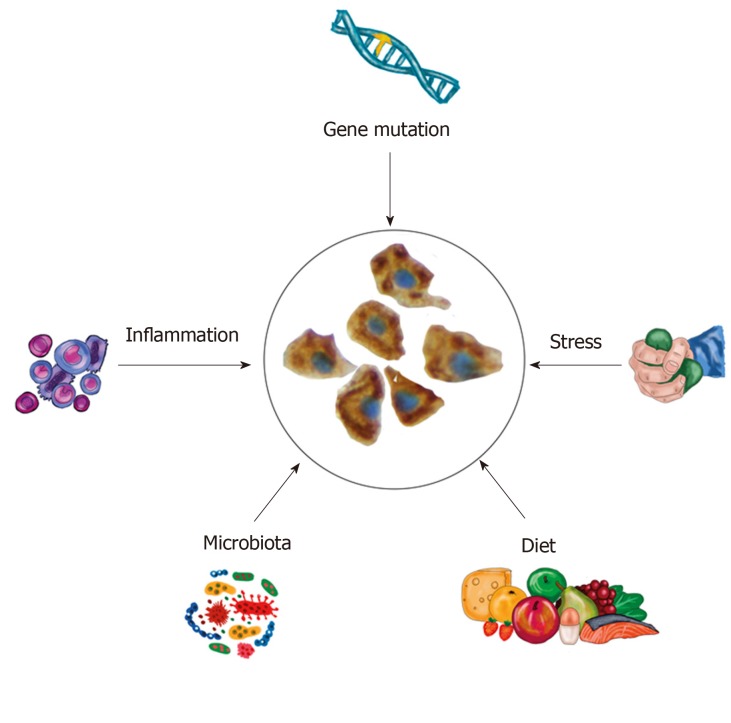
Figure 7.
Schematic drawing to illustrate the hypothesis that intestinal stem cells play a central role in the pathophysiology of irritable bowel syndrome. The abnormalities in the intestinal stem cells can be caused by gene mutation or by environmental factors such as diet, intestinal microbiota, stress and low-grade inflammation.
CLINICAL IMPLICATIONS
Assuming that IBS is caused by abnormalities in stem cells, which in turn caused by genetic and environmental factors, intestinal stem cell transplantation might be an effective tool in the treatment of IBS.
CONCLUSION
The intestinal stem cells appear to play a central role in the pathophysiology of IBS. Factors that are known to be involved in the pathophysiology of IBS exert their effects probably through affecting the intestinal stem cells.
Footnotes
Conflict-of-interest statement: Authors declare no conflict of interests for this article.
Manuscript source: Invited Manuscript
Peer-review started: December 3, 2019
First decision: January 13, 2020
Article in press: March 14, 2020
Specialty type: Gastroenterology and hepatology
Country of origin: Norway
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Finsterer J, Gregorio BM S-Editor: Tang JZ L-Editor: A E-Editor: Ma YJ
References
- 1.Canavan C, West J, Card T. The epidemiology of irritable bowel syndrome. Clin Epidemiol. 2014;6:71–80. doi: 10.2147/CLEP.S40245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.El-Salhy M. Recent developments in the pathophysiology of irritable bowel syndrome. World J Gastroenterol. 2015;21:7621–7636. doi: 10.3748/wjg.v21.i25.7621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.El-Salhy M. Irritable bowel syndrome: diagnosis and pathogenesis. World J Gastroenterol. 2012;18:5151–5163. doi: 10.3748/wjg.v18.i37.5151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.El-Salhy M, Gilja OH, Hatlebakk JG. Overlapping of irritable bowel syndrome with erosive esophagitis and the performance of Rome criteria in diagnosing IBS in a clinical setting. Mol Med Rep. 2019;20:787–794. doi: 10.3892/mmr.2019.10284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Talley NJ, Gabriel SE, Harmsen WS, Zinsmeister AR, Evans RW. Medical costs in community subjects with irritable bowel syndrome. Gastroenterology. 1995;109:1736–1741. doi: 10.1016/0016-5085(95)90738-6. [DOI] [PubMed] [Google Scholar]
- 6.Jones R, Lydeard S. Irritable bowel syndrome in the general population. BMJ. 1992;304:87–90. doi: 10.1136/bmj.304.6819.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hungin AP, Whorwell PJ, Tack J, Mearin F. The prevalence, patterns and impact of irritable bowel syndrome: an international survey of 40,000 subjects. Aliment Pharmacol Ther. 2003;17:643–650. doi: 10.1046/j.1365-2036.2003.01456.x. [DOI] [PubMed] [Google Scholar]
- 8.Schuster MM. Defining and diagnosing irritable bowel syndrome. Am J Manag Care. 2001;7:S246–S251. [PubMed] [Google Scholar]
- 9.Mitchell CM, Drossman DA. Survey of the AGA membership relating to patients with functional gastrointestinal disorders. Gastroenterology. 1987;92:1282–1284. doi: 10.1016/s0016-5085(87)91099-7. [DOI] [PubMed] [Google Scholar]
- 10.Konturek PC, Brzozowski T, Konturek SJ. Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options. J Physiol Pharmacol. 2011;62:591–599. [PubMed] [Google Scholar]
- 11.El-Salhy M, Gilja OH. Abnormalities in ileal stem, neurogenin 3, and enteroendocrine cells in patients with irritable bowel syndrome. BMC Gastroenterol. 2017;17:90. doi: 10.1186/s12876-017-0643-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.El-Salhy M, Hatlebakk JG, Hausken T. Reduction in duodenal endocrine cells in irritable bowel syndrome is associated with stem cell abnormalities. World J Gastroenterol. 2015;21:9577–9587. doi: 10.3748/wjg.v21.i32.9577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.El-Salhy M, Patcharatrakul T, Hatlebakk JG, Hausken T, Gilja OH, Gonlachanvit S. Enteroendocrine, Musashi 1 and neurogenin 3 cells in the large intestine of Thai and Norwegian patients with irritable bowel syndrome. Scand J Gastroenterol. 2017;52:1331–1339. doi: 10.1080/00365521.2017.1371793. [DOI] [PubMed] [Google Scholar]
- 14.Locke GR, 3rd, Zinsmeister AR, Talley NJ, Fett SL, Melton LJ., 3rd Familial association in adults with functional gastrointestinal disorders. Mayo Clin Proc. 2000;75:907–912. doi: 10.4065/75.9.907. [DOI] [PubMed] [Google Scholar]
- 15.Kalantar JS, Locke GR, 3rd, Zinsmeister AR, Beighley CM, Talley NJ. Familial aggregation of irritable bowel syndrome: a prospective study. Gut. 2003;52:1703–1707. doi: 10.1136/gut.52.12.1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kanazawa M, Endo Y, Whitehead WE, Kano M, Hongo M, Fukudo S. Patients and nonconsulters with irritable bowel syndrome reporting a parental history of bowel problems have more impaired psychological distress. Dig Dis Sci. 2004;49:1046–1053. doi: 10.1023/b:ddas.0000034570.52305.10. [DOI] [PubMed] [Google Scholar]
- 17.Morris-Yates A, Talley NJ, Boyce PM, Nandurkar S, Andrews G. Evidence of a genetic contribution to functional bowel disorder. Am J Gastroenterol. 1998;93:1311–1317. doi: 10.1111/j.1572-0241.1998.440_j.x. [DOI] [PubMed] [Google Scholar]
- 18.Levy RL, Jones KR, Whitehead WE, Feld SI, Talley NJ, Corey LA. Irritable bowel syndrome in twins: heredity and social learning both contribute to etiology. Gastroenterology. 2001;121:799–804. doi: 10.1053/gast.2001.27995. [DOI] [PubMed] [Google Scholar]
- 19.Lembo A, Zaman M, Jones M, Talley NJ. Influence of genetics on irritable bowel syndrome, gastro-oesophageal reflux and dyspepsia: a twin study. Aliment Pharmacol Ther. 2007;25:1343–1350. doi: 10.1111/j.1365-2036.2007.03326.x. [DOI] [PubMed] [Google Scholar]
- 20.Wojczynski MK, North KE, Pedersen NL, Sullivan PF. Irritable bowel syndrome: a co-twin control analysis. Am J Gastroenterol. 2007;102:2220–2229. doi: 10.1111/j.1572-0241.2007.01479.x. [DOI] [PubMed] [Google Scholar]
- 21.Bengtson MB, Rønning T, Vatn MH, Harris JR. Irritable bowel syndrome in twins: genes and environment. Gut. 2006;55:1754–1759. doi: 10.1136/gut.2006.097287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.El-Salhy M, Ostgaard H, Gundersen D, Hatlebakk JG, Hausken T. The role of diet in the pathogenesis and management of irritable bowel syndrome (Review) Int J Mol Med. 2012;29:723–731. doi: 10.3892/ijmm.2012.926. [DOI] [PubMed] [Google Scholar]
- 23.Ostgaard H, Hausken T, Gundersen D, El-Salhy M. Diet and effects of diet management on quality of life and symptoms in patients with irritable bowel syndrome. Mol Med Rep. 2012;5:1382–1390. doi: 10.3892/mmr.2012.843. [DOI] [PubMed] [Google Scholar]
- 24.El-Salhy M, Gilja OH, Gundersen D, Hatlebakk JG, Hausken T. Interaction between ingested nutrients and gut endocrine cells in patients with irritable bowel syndrome (review) Int J Mol Med. 2014;34:363–371. doi: 10.3892/ijmm.2014.1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.El-Salhy M, Mazzawi T, Hausken T, Hatlebakk JG. Interaction between diet and gastrointestinal endocrine cells. Biomed Rep. 2016;4:651–656. doi: 10.3892/br.2016.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.El-Salhy M, Lilbo E, Reinemo A, Salmeøid L, Hausken T. Effects of a health program comprising reassurance, diet management, probiotic administration and regular exercise on symptoms and quality of life in patients with irritable bowel syndrome. Gastroenterology Insights. 2010;2:21–26. [Google Scholar]
- 27.Jarrett M, Heitkemper MM, Bond EF, Georges J. Comparison of diet composition in women with and without functional bowel disorder. Gastroenterol Nurs. 1994;16:253–258. doi: 10.1097/00001610-199406000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Saito YA, Locke GR, 3rd, Weaver AL, Zinsmeister AR, Talley NJ. Diet and functional gastrointestinal disorders: a population-based case-control study. Am J Gastroenterol. 2005;100:2743–2748. doi: 10.1111/j.1572-0241.2005.00288.x. [DOI] [PubMed] [Google Scholar]
- 29.El-Salhy M, Gundersen D. Diet in irritable bowel syndrome. Nutr J. 2015;14:36. doi: 10.1186/s12937-015-0022-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.El-Salhy M, Hatlebakk JG, Gilja OH, Hausken T. The relation between celiac disease, nonceliac gluten sensitivity and irritable bowel syndrome. Nutr J. 2015;14:92. doi: 10.1186/s12937-015-0080-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.El-Salhy M, Gundersen D, Hatlebakk JG, Hausken T. Diet and irritable bowel syndrome, with a focus on appetite-regulating hormones. In: Watson RR. Nutrition in the prevention and treatment of abdominal obesity. San Diego: Elsevier. In: Watson RR, editor. 2014. pp. 5–16. [Google Scholar]
- 32.El-Salhy M. Diet in the pathophysiology and management of irritable bowel syndrome. Cleve Clin J Med. 2016;83:663–664. doi: 10.3949/ccjm.83a.16019. [DOI] [PubMed] [Google Scholar]
- 33.Dionne J, Ford AC, Yuan Y, Chey WD, Lacy BE, Saito YA, Quigley EMM, Moayyedi P. A Systematic Review and Meta-Analysis Evaluating the Efficacy of a Gluten-Free Diet and a Low FODMAPs Diet in Treating Symptoms of Irritable Bowel Syndrome. Am J Gastroenterol. 2018;113:1290–1300. doi: 10.1038/s41395-018-0195-4. [DOI] [PubMed] [Google Scholar]
- 34.Ellis A, Linaker BD. Non-coeliac gluten sensitivity? Lancet. 1978;1:1358–1359. doi: 10.1016/s0140-6736(78)92427-3. [DOI] [PubMed] [Google Scholar]
- 35.Boettcher E, Crowe SE. Dietary proteins and functional gastrointestinal disorders. Am J Gastroenterol. 2013;108:728–736. doi: 10.1038/ajg.2013.97. [DOI] [PubMed] [Google Scholar]
- 36.Sapone A, Bai JC, Ciacci C, Dolinsek J, Green PH, Hadjivassiliou M, Kaukinen K, Rostami K, Sanders DS, Schumann M, Ullrich R, Villalta D, Volta U, Catassi C, Fasano A. Spectrum of gluten-related disorders: consensus on new nomenclature and classification. BMC Med. 2012;10:13. doi: 10.1186/1741-7015-10-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Campanella J, Biagi F, Bianchi PI, Zanellati G, Marchese A, Corazza GR. Clinical response to gluten withdrawal is not an indicator of coeliac disease. Scand J Gastroenterol. 2008;43:1311–1314. doi: 10.1080/00365520802200036. [DOI] [PubMed] [Google Scholar]
- 38.Vazquez-Roque MI, Camilleri M, Smyrk T, Murray JA, Marietta E, O'Neill J, Carlson P, Lamsam J, Janzow D, Eckert D, Burton D, Zinsmeister AR. A controlled trial of gluten-free diet in patients with irritable bowel syndrome-diarrhea: effects on bowel frequency and intestinal function. Gastroenterology. 2013;144:903–911.e3. doi: 10.1053/j.gastro.2013.01.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kaukinen K, Turjanmaa K, Mäki M, Partanen J, Venäläinen R, Reunala T, Collin P. Intolerance to cereals is not specific for coeliac disease. Scand J Gastroenterol. 2000;35:942–946. doi: 10.1080/003655200750022995. [DOI] [PubMed] [Google Scholar]
- 40.Carroccio A, Mansueto P, Iacono G, Soresi M, D'Alcamo A, Cavataio F, Brusca I, Florena AM, Ambrosiano G, Seidita A, Pirrone G, Rini GB. Non-celiac wheat sensitivity diagnosed by double-blind placebo-controlled challenge: exploring a new clinical entity. Am J Gastroenterol. 2012;107:1898–1906. doi: 10.1038/ajg.2012.236. [DOI] [PubMed] [Google Scholar]
- 41.Biesiekierski JR, Newnham ED, Irving PM, Barrett JS, Haines M, Doecke JD, Shepherd SJ, Muir JG, Gibson PR. Gluten causes gastrointestinal symptoms in subjects without celiac disease: a double-blind randomized placebo-controlled trial. Am J Gastroenterol. 2011;106:508–514. doi: 10.1038/ajg.2010.487. [DOI] [PubMed] [Google Scholar]
- 42.Shahbazkhani B, Sadeghi A, Malekzadeh R, Khatavi F, Etemadi M, Kalantri E, Rostami-Nejad M, Rostami K. Non-Celiac Gluten Sensitivity Has Narrowed the Spectrum of Irritable Bowel Syndrome: A Double-Blind Randomized Placebo-Controlled Trial. Nutrients. 2015;7:4542–4554. doi: 10.3390/nu7064542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Skodje GI, Sarna VK, Minelle IH, Rolfsen KL, Muir JG, Gibson PR, Veierød MB, Henriksen C, Lundin KEA. Fructan, Rather Than Gluten, Induces Symptoms in Patients With Self-Reported Non-Celiac Gluten Sensitivity. Gastroenterology. 2018;154:529–539. doi: 10.1053/j.gastro.2017.10.040. [DOI] [PubMed] [Google Scholar]
- 44.Thursby E, Juge N. Introduction to the human gut microbiota. Biochem J. 2017;474:1823–1836. doi: 10.1042/BCJ20160510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hugon P, Dufour JC, Colson P, Fournier PE, Sallah K, Raoult D. A comprehensive repertoire of prokaryotic species identified in human beings. Lancet Infect Dis. 2015;15:1211–1219. doi: 10.1016/S1473-3099(15)00293-5. [DOI] [PubMed] [Google Scholar]
- 46.Ley RE, Hamady M, Lozupone C, Turnbaugh PJ, Ramey RR, Bircher JS, Schlegel ML, Tucker TA, Schrenzel MD, Knight R, Gordon JI. Evolution of mammals and their gut microbes. Science. 2008;320:1647–1651. doi: 10.1126/science.1155725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kriss M, Hazleton KZ, Nusbacher NM, Martin CG, Lozupone CA. Low diversity gut microbiota dysbiosis: drivers, functional implications and recovery. Curr Opin Microbiol. 2018;44:34–40. doi: 10.1016/j.mib.2018.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wilson BC, Vatanen T, Cutfield WS, O'Sullivan JM. The Super-Donor Phenomenon in Fecal Microbiota Transplantation. Front Cell Infect Microbiol. 2019;9:2. doi: 10.3389/fcimb.2019.00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.El-Salhy M, Mazzawi T. Fecal microbiota transplantation for managing irritable bowel syndrome. Expert Rev Gastroenterol Hepatol. 2018;12:439–445. doi: 10.1080/17474124.2018.1447380. [DOI] [PubMed] [Google Scholar]
- 50.Casén C, Vebø HC, Sekelja M, Hegge FT, Karlsson MK, Ciemniejewska E, Dzankovic S, Frøyland C, Nestestog R, Engstrand L, Munkholm P, Nielsen OH, Rogler G, Simrén M, Öhman L, Vatn MH, Rudi K. Deviations in human gut microbiota: a novel diagnostic test for determining dysbiosis in patients with IBS or IBD. Aliment Pharmacol Ther. 2015;42:71–83. doi: 10.1111/apt.13236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Enck P, Mazurak N. Dysbiosis in Functional Bowel Disorders. Ann Nutr Metab. 2018;72:296–306. doi: 10.1159/000488773. [DOI] [PubMed] [Google Scholar]
- 52.El-Salhy M, Seim I, Chopin L, Gundersen D, Hatlebakk JG, Hausken T. Irritable bowel syndrome: the role of gut neuroendocrine peptides. Front Biosci (Elite Ed) 2012;4:2783–2800. doi: 10.2741/e583. [DOI] [PubMed] [Google Scholar]
- 53.El-Salhy M, Gundersen D, Hatlebakk JG, Hausken T. Irritable bowel syndrome: diagnosis, pathogenesis and treatment options. New York: Nova Science Publishers, 2012: 35-78. [Google Scholar]
- 54.El-Salhy M, Hatlebakk JG, Hausken T. Diet in Irritable Bowel Syndrome (IBS): Interaction with Gut Microbiota and Gut Hormones. Nutrients. 2019;11:pii: E1824. doi: 10.3390/nu11081824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mawe GM, Coates MD, Moses PL. Review article: intestinal serotonin signalling in irritable bowel syndrome. Aliment Pharmacol Ther. 2006;23:1067–1076. doi: 10.1111/j.1365-2036.2006.02858.x. [DOI] [PubMed] [Google Scholar]
- 56.Wade PR, Chen J, Jaffe B, Kassem IS, Blakely RD, Gershon MD. Localization and function of a 5-HT transporter in crypt epithelia of the gastrointestinal tract. J Neurosci. 1996;16:2352–2364. doi: 10.1523/JNEUROSCI.16-07-02352.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gershon MD, Tack J. The serotonin signaling system: from basic understanding to drug development for functional GI disorders. Gastroenterology. 2007;132:397–414. doi: 10.1053/j.gastro.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 58.Gershon MD. 5-Hydroxytryptamine (serotonin) in the gastrointestinal tract. Curr Opin Endocrinol Diabetes Obes. 2013;20:14–21. doi: 10.1097/MED.0b013e32835bc703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gershon MD. Serotonin is a sword and a shield of the bowel: serotonin plays offense and defense. Trans Am Clin Climatol Assoc. 2012;123:268–280. [PMC free article] [PubMed] [Google Scholar]
- 60.El-Salhy M, Mazzawi T, Gundersen D, Hatlebakk JG, Hausken T. The role of peptide YY in gastrointestinal diseases and disorders (review) Int J Mol Med. 2013;31:275–282. doi: 10.3892/ijmm.2012.1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dubrasquet M, Bataille D, Gespach C. Oxyntomodulin (glucagon-37 or bioactive enteroglucagon): a potent inhibitor of pentagastrin-stimulated acid secretion in rats. Biosci Rep. 1982;2:391–395. doi: 10.1007/BF01119301. [DOI] [PubMed] [Google Scholar]
- 62.Schjoldager BT, Baldissera FG, Mortensen PE, Holst JJ, Christiansen J. Oxyntomodulin: a potential hormone from the distal gut. Pharmacokinetics and effects on gastric acid and insulin secretion in man. Eur J Clin Invest. 1988;18:499–503. doi: 10.1111/j.1365-2362.1988.tb01046.x. [DOI] [PubMed] [Google Scholar]
- 63.Schjoldager B, Mortensen PE, Myhre J, Christiansen J, Holst JJ. Oxyntomodulin from distal gut. Role in regulation of gastric and pancreatic functions. Dig Dis Sci. 1989;34:1411–1419. doi: 10.1007/BF01538078. [DOI] [PubMed] [Google Scholar]
- 64.Dakin CL, Small CJ, Batterham RL, Neary NM, Cohen MA, Patterson M, Ghatei MA, Bloom SR. Peripheral oxyntomodulin reduces food intake and body weight gain in rats. Endocrinology. 2004;145:2687–2695. doi: 10.1210/en.2003-1338. [DOI] [PubMed] [Google Scholar]
- 65.Wynne K, Park AJ, Small CJ, Patterson M, Ellis SM, Murphy KG, Wren AM, Frost GS, Meeran K, Ghatei MA, Bloom SR. Subcutaneous oxyntomodulin reduces body weight in overweight and obese subjects: a double-blind, randomized, controlled trial. Diabetes. 2005;54:2390–2395. doi: 10.2337/diabetes.54.8.2390. [DOI] [PubMed] [Google Scholar]
- 66.Camilleri M. Peripheral mechanisms in irritable bowel syndrome. N Engl J Med. 2012;367:1626–1635. doi: 10.1056/NEJMra1207068. [DOI] [PubMed] [Google Scholar]
- 67.Jianu MCS, Fossmark R, Syversen U, Hauso Ø, Waldum HL. A meal test improves the specificity of chromogranin A as a marker of neuroendocrine neoplasia. Tumour Biol. 2010;31:373–380. doi: 10.1007/s13277-010-0045-5. [DOI] [PubMed] [Google Scholar]
- 68.Gunawardene AR, Corfe BM, Staton CA. Classification and functions of enteroendocrine cells of the lower gastrointestinal tract. Int J Exp Pathol. 2011;92:219–231. doi: 10.1111/j.1365-2613.2011.00767.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.May CL, Kaestner KH. Gut endocrine cell development. Mol Cell Endocrinol. 2010;323:70–75. doi: 10.1016/j.mce.2009.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sandström O, El-Salhy M. Ageing and endocrine cells of human duodenum. Mech Ageing Dev. 1999;108:39–48. doi: 10.1016/s0047-6374(98)00154-7. [DOI] [PubMed] [Google Scholar]
- 71.El-Salhy M. Ghrelin in gastrointestinal diseases and disorders: a possible role in the pathophysiology and clinical implications (review) Int J Mol Med. 2009;24:727–732. doi: 10.3892/ijmm_00000285. [DOI] [PubMed] [Google Scholar]
- 72.Tolhurst G, Reimann F, Gribble FM. Intestinal sensing of nutrients. Handb Exp Pharmacol. 2012:309–335. doi: 10.1007/978-3-642-24716-3_14. [DOI] [PubMed] [Google Scholar]
- 73.Lee J, Cummings BP, Martin E, Sharp JW, Graham JL, Stanhope KL, Havel PJ, Raybould HE. Glucose sensing by gut endocrine cells and activation of the vagal afferent pathway is impaired in a rodent model of type 2 diabetes mellitus. Am J Physiol Regul Integr Comp Physiol. 2012;302:R657–R666. doi: 10.1152/ajpregu.00345.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Parker HE, Reimann F, Gribble FM. Molecular mechanisms underlying nutrient-stimulated incretin secretion. Expert Rev Mol Med. 2010;12:e1. doi: 10.1017/S146239940900132X. [DOI] [PubMed] [Google Scholar]
- 75.Raybould HE. Nutrient sensing in the gastrointestinal tract: possible role for nutrient transporters. J Physiol Biochem. 2008;64:349–356. doi: 10.1007/BF03174091. [DOI] [PubMed] [Google Scholar]
- 76.San Gabriel A, Nakamura E, Uneyama H, Torii K. Taste, visceral information and exocrine reflexes with glutamate through umami receptors. J Med Invest. 2009;56 Suppl:209–217. doi: 10.2152/jmi.56.209. [DOI] [PubMed] [Google Scholar]
- 77.Rudholm T, Wallin B, Theodorsson E, Näslund E, Hellström PM. Release of regulatory gut peptides somatostatin, neurotensin and vasoactive intestinal peptide by acid and hyperosmolal solutions in the intestine in conscious rats. Regul Pept. 2009;152:8–12. doi: 10.1016/j.regpep.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 78.Sternini C, Anselmi L, Rozengurt E. Enteroendocrine cells: a site of 'taste' in gastrointestinal chemosensing. Curr Opin Endocrinol Diabetes Obes. 2008;15:73–78. doi: 10.1097/MED.0b013e3282f43a73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sternini C. Taste receptors in the gastrointestinal tract. IV. Functional implications of bitter taste receptors in gastrointestinal chemosensing. Am J Physiol Gastrointest Liver Physiol. 2007;292:G457–G461. doi: 10.1152/ajpgi.00411.2006. [DOI] [PubMed] [Google Scholar]
- 80.Buchan AM. Nutrient Tasting and Signaling Mechanisms in the Gut III. Endocrine cell recognition of luminal nutrients. Am J Physiol. 1999;277:G1103–G1107. doi: 10.1152/ajpgi.1999.277.6.G1103. [DOI] [PubMed] [Google Scholar]
- 81.Montero-Hadjadje M, Elias S, Chevalier L, Benard M, Tanguy Y, Turquier V, Galas L, Yon L, Malagon MM, Driouich A, Gasman S, Anouar Y. Chromogranin A promotes peptide hormone sorting to mobile granules in constitutively and regulated secreting cells: role of conserved N- and C-terminal peptides. J Biol Chem. 2009;284:12420–12431. doi: 10.1074/jbc.M805607200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Shooshtarizadeh P, Zhang D, Chich JF, Gasnier C, Schneider F, Haïkel Y, Aunis D, Metz-Boutigue MH. The antimicrobial peptides derived from chromogranin/secretogranin family, new actors of innate immunity. Regul Pept. 2010;165:102–110. doi: 10.1016/j.regpep.2009.11.014. [DOI] [PubMed] [Google Scholar]
- 83.Wendelbo I, Mazzawi T, El-Salhy M. Increased serotonin transporter immunoreactivity intensity in the ileum of patients with irritable bowel disease. Mol Med Rep. 2014;9:180–184. doi: 10.3892/mmr.2013.1784. [DOI] [PubMed] [Google Scholar]
- 84.El-Salhy M, Wendelbo IH, Gundersen D. Reduced chromogranin A cell density in the ileum of patients with irritable bowel syndrome. Mol Med Rep. 2013;7:1241–1244. doi: 10.3892/mmr.2013.1325. [DOI] [PubMed] [Google Scholar]
- 85.El-Salhy M, Vaali K, Dizdar V, Hausken T. Abnormal small-intestinal endocrine cells in patients with irritable bowel syndrome. Dig Dis Sci. 2010;55:3508–3513. doi: 10.1007/s10620-010-1169-6. [DOI] [PubMed] [Google Scholar]
- 86.El-Salhy M, Mazzawi T, Gundersen D, Hausken T. Chromogranin A cell density in the rectum of patients with irritable bowel syndrome. Mol Med Rep. 2012;6:1223–1225. doi: 10.3892/mmr.2012.1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.El-Salhy M, Lomholt-Beck B, Hausken T. Chromogranin A as a possible tool in the diagnosis of irritable bowel syndrome. Scand J Gastroenterol. 2010;45:1435–1439. doi: 10.3109/00365521.2010.503965. [DOI] [PubMed] [Google Scholar]
- 88.El-Salhy M, Lillebø E, Reinemo A, Salmelid L. Ghrelin in patients with irritable bowel syndrome. Int J Mol Med. 2009;23:703–707. doi: 10.3892/ijmm_00000183. [DOI] [PubMed] [Google Scholar]
- 89.El-Salhy M, Gilja OH, Gundersen D, Hausken T. Endocrine cells in the oxyntic mucosa of the stomach in patients with irritable bowel syndrome. World J Gastrointest Endosc. 2014;6:176–185. doi: 10.4253/wjge.v6.i5.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.El-Salhy M, Gundersen D, Hatlebakk JG, Hausken T. Chromogranin A cell density as a diagnostic marker for lymphocytic colitis. Dig Dis Sci. 2012;57:3154–3159. doi: 10.1007/s10620-012-2249-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mazzawi T, Hausken T, Gundersen D, El-Salhy M. Effects of dietary guidance on the symptoms, quality of life and habitual dietary intake of patients with irritable bowel syndrome. Mol Med Rep. 2013;8:845–852. doi: 10.3892/mmr.2013.1565. [DOI] [PubMed] [Google Scholar]
- 92.El-Salhy M, Gilja OH, Hatlebakk JG, Hausken T. Stomach antral endocrine cells in patients with irritable bowel syndrome. Int J Mol Med. 2014;34:967–974. doi: 10.3892/ijmm.2014.1887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sjölund K, Ekman R, Wierup N. Covariation of plasma ghrelin and motilin in irritable bowel syndrome. Peptides. 2010;31:1109–1112. doi: 10.1016/j.peptides.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 94.Wang SH, Dong L, Luo JY, Gong J, Li L, Lu XL, Han SP. Decreased expression of serotonin in the jejunum and increased numbers of mast cells in the terminal ileum in patients with irritable bowel syndrome. World J Gastroenterol. 2007;13:6041–6047. doi: 10.3748/wjg.v13.45.6041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Park JH, Rhee PL, Kim G, Lee JH, Kim YH, Kim JJ, Rhee JC, Song SY. Enteroendocrine cell counts correlate with visceral hypersensitivity in patients with diarrhoea-predominant irritable bowel syndrome. Neurogastroenterol Motil. 2006;18:539–546. doi: 10.1111/j.1365-2982.2006.00771.x. [DOI] [PubMed] [Google Scholar]
- 96.Coates MD, Mahoney CR, Linden DR, Sampson JE, Chen J, Blaszyk H, Crowell MD, Sharkey KA, Gershon MD, Mawe GM, Moses PL. Molecular defects in mucosal serotonin content and decreased serotonin reuptake transporter in ulcerative colitis and irritable bowel syndrome. Gastroenterology. 2004;126:1657–1664. doi: 10.1053/j.gastro.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 97.El-Salhy M, Wendelbo I, Gundersen D. Serotonin and serotonin transporter in the rectum of patients with irritable bowel disease. Mol Med Rep. 2013;8:451–455. doi: 10.3892/mmr.2013.1525. [DOI] [PubMed] [Google Scholar]
- 98.Soares RL. Irritable bowel syndrome: a clinical review. World J Gastroenterol. 2014;20:12144–12160. doi: 10.3748/wjg.v20.i34.12144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Weston AP, Biddle WL, Bhatia PS, Miner PB., Jr Terminal ileal mucosal mast cells in irritable bowel syndrome. Dig Dis Sci. 1993;38:1590–1595. doi: 10.1007/BF01303164. [DOI] [PubMed] [Google Scholar]
- 100.O'Sullivan M, Clayton N, Breslin NP, Harman I, Bountra C, McLaren A, O'Morain CA. Increased mast cells in the irritable bowel syndrome. Neurogastroenterol Motil. 2000;12:449–457. doi: 10.1046/j.1365-2982.2000.00221.x. [DOI] [PubMed] [Google Scholar]
- 101.Barbara G, De Giorgio R, Stanghellini V, Cremon C, Corinaldesi R. A role for inflammation in irritable bowel syndrome? Gut. 2002;51 Suppl 1:i41–i44. doi: 10.1136/gut.51.suppl_1.i41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Barbara G, Stanghellini V, De Giorgio R, Cremon C, Cottrell GS, Santini D, Pasquinelli G, Morselli-Labate AM, Grady EF, Bunnett NW, Collins SM, Corinaldesi R. Activated mast cells in proximity to colonic nerves correlate with abdominal pain in irritable bowel syndrome. Gastroenterology. 2004;126:693–702. doi: 10.1053/j.gastro.2003.11.055. [DOI] [PubMed] [Google Scholar]
- 103.Montgomery RK, Breault DT. Small intestinal stem cell markers. J Anat. 2008;213:52–58. doi: 10.1111/j.1469-7580.2008.00925.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Barker N, Clevers H. Tracking down the stem cells of the intestine: strategies to identify adult stem cells. Gastroenterology. 2007;133:1755–1760. doi: 10.1053/j.gastro.2007.10.029. [DOI] [PubMed] [Google Scholar]
- 105.Barker N, van de Wetering M, Clevers H. The intestinal stem cell. Genes Dev. 2008;22:1856–1864. doi: 10.1101/gad.1674008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Barker N, van Es JH, Kuipers J, Kujala P, van den Born M, Cozijnsen M, Haegebarth A, Korving J, Begthel H, Peters PJ, Clevers H. Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature. 2007;449:1003–1007. doi: 10.1038/nature06196. [DOI] [PubMed] [Google Scholar]
- 107.Korinek V, Barker N, Moerer P, van Donselaar E, Huls G, Peters PJ, Clevers H. Depletion of epithelial stem-cell compartments in the small intestine of mice lacking Tcf-4. Nat Genet. 1998;19:379–383. doi: 10.1038/1270. [DOI] [PubMed] [Google Scholar]
- 108.Cheng H, Leblond CP. Origin, differentiation and renewal of the four main epithelial cell types in the mouse small intestine. V. Unitarian Theory of the origin of the four epithelial cell types. Am J Anat. 1974;141:537–561. doi: 10.1002/aja.1001410407. [DOI] [PubMed] [Google Scholar]
- 109.Le Douarin NM, Teillet MA. The migration of neural crest cells to the wall of the digestive tract in avian embryo. J Embryol Exp Morphol. 1973;30:31–48. [PubMed] [Google Scholar]
- 110.Rawdon BB, Andrew A. Origin and differentiation of gut endocrine cells. Histol Histopathol. 1993;8:567–580. [PubMed] [Google Scholar]
- 111.Hoffman J, Kuhnert F, Davis CR, Kuo CJ. Wnts as essential growth factors for the adult small intestine and colon. Cell Cycle. 2004;3:554–557. [PubMed] [Google Scholar]
- 112.Lee CS, Kaestner KH. Clinical endocrinology and metabolism. Development of gut endocrine cells. Best Pract Res Clin Endocrinol Metab. 2004;18:453–462. doi: 10.1016/j.beem.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 113.Potten CS, Booth C, Tudor GL, Booth D, Brady G, Hurley P, Ashton G, Clarke R, Sakakibara S, Okano H. Identification of a putative intestinal stem cell and early lineage marker; musashi-1. Differentiation. 2003;71:28–41. doi: 10.1046/j.1432-0436.2003.700603.x. [DOI] [PubMed] [Google Scholar]
- 114.Kayahara T, Sawada M, Takaishi S, Fukui H, Seno H, Fukuzawa H, Suzuki K, Hiai H, Kageyama R, Okano H, Chiba T. Candidate markers for stem and early progenitor cells, Musashi-1 and Hes1, are expressed in crypt base columnar cells of mouse small intestine. FEBS Lett. 2003;535:131–135. doi: 10.1016/s0014-5793(02)03896-6. [DOI] [PubMed] [Google Scholar]
- 115.He XC, Yin T, Grindley JC, Tian Q, Sato T, Tao WA, Dirisina R, Porter-Westpfahl KS, Hembree M, Johnson T, Wiedemann LM, Barrett TA, Hood L, Wu H, Li L. PTEN-deficient intestinal stem cells initiate intestinal polyposis. Nat Genet. 2007;39:189–198. doi: 10.1038/ng1928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Fishbein TM, Novitskiy G, Lough DM, Matsumoto C, Kaufman SS, Shetty K, Zasloff M. Rejection reversibly alters enteroendocrine cell renewal in the transplanted small intestine. Am J Transplant. 2009;9:1620–1628. doi: 10.1111/j.1600-6143.2009.02681.x. [DOI] [PubMed] [Google Scholar]
- 117.Schonhoff SE, Giel-Moloney M, Leiter AB. Minireview: Development and differentiation of gut endocrine cells. Endocrinology. 2004;145:2639–2644. doi: 10.1210/en.2004-0051. [DOI] [PubMed] [Google Scholar]
- 118.Schonhoff SE, Giel-Moloney M, Leiter AB. Neurogenin 3-expressing progenitor cells in the gastrointestinal tract differentiate into both endocrine and non-endocrine cell types. Dev Biol. 2004;270:443–454. doi: 10.1016/j.ydbio.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 119.El-Salhy M, Hausken T, Gilja OH, Hatlebakk JG. The possible role of gastrointestinal endocrine cells in the pathophysiology of irritable bowel syndrome. Expert Rev Gastroenterol Hepatol. 2017;11:139–148. doi: 10.1080/17474124.2017.1269601. [DOI] [PubMed] [Google Scholar]
- 120.Jenny M, Uhl C, Roche C, Duluc I, Guillermin V, Guillemot F, Jensen J, Kedinger M, Gradwohl G. Neurogenin3 is differentially required for endocrine cell fate specification in the intestinal and gastric epithelium. EMBO J. 2002;21:6338–6347. doi: 10.1093/emboj/cdf649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wang J, Cortina G, Wu SV, Tran R, Cho JH, Tsai MJ, Bailey TJ, Jamrich M, Ament ME, Treem WR, Hill ID, Vargas JH, Gershman G, Farmer DG, Reyen L, Martín MG. Mutant neurogenin-3 in congenital malabsorptive diarrhea. N Engl J Med. 2006;355:270–280. doi: 10.1056/NEJMoa054288. [DOI] [PubMed] [Google Scholar]
- 122.Mazzawi T, El-Salhy M. Changes in small intestinal chromogranin A-immunoreactive cell densities in patients with irritable bowel syndrome after receiving dietary guidance. Int J Mol Med. 2016;37:1247–1253. doi: 10.3892/ijmm.2016.2523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Mazzawi T, El-Salhy M. Dietary guidance and ileal enteroendocrine cells in patients with irritable bowel syndrome. Exp Ther Med. 2016;12:1398–1404. doi: 10.3892/etm.2016.3491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Mazzawi T, Gundersen D, Hausken T, El-Salhy M. Increased gastric chromogranin A cell density following changes to diets of patients with irritable bowel syndrome. Mol Med Rep. 2014;10:2322–2326. doi: 10.3892/mmr.2014.2498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Mazzawi T, Gundersen D, Hausken T, El-Salhy M. Increased chromogranin a cell density in the large intestine of patients with irritable bowel syndrome after receiving dietary guidance. Gastroenterol Res Pract. 2015;2015:823897. doi: 10.1155/2015/823897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Mazzawi T, Hausken T, Gundersen D, El-Salhy M. Effect of dietary management on the gastric endocrine cells in patients with irritable bowel syndrome. Eur J Clin Nutr. 2015;69:519–524. doi: 10.1038/ejcn.2014.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Mazzawi T, Hausken T, Gundersen D, El-Salhy M. Dietary guidance normalizes large intestinal endocrine cell densities in patients with irritable bowel syndrome. Eur J Clin Nutr. 2016;70:175–181. doi: 10.1038/ejcn.2015.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Mazzawi T, Arslan G, El-Sahy M, Gilja OH, Hatlebakk JG, Hausken T. Effect of fecal microbiota transplantation on the symptoms and duodenal enteroendocrine cells in patients with irritable bowel syndrome. United Eur Gastroe. 2016;4:677–677. [Google Scholar]
- 129.Chen S, Xia Y, Zhu G, Yan J, Tan C, Deng B, Deng J, Yin Y, Ren W. Glutamine supplementation improves intestinal cell proliferation and stem cell differentiation in weanling mice. Food Nutr Res. 2018;62 doi: 10.29219/fnr.v62.1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Chen Y, Tsai YH, Tseng BJ, Tseng SH. Influence of Growth Hormone and Glutamine on Intestinal Stem Cells: A Narrative Review. Nutrients. 2019;11 doi: 10.3390/nu11081941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Chen Y, Tseng SH, Yao CL, Li C, Tsai YH. Distinct Effects of Growth Hormone and Glutamine on Activation of Intestinal Stem Cells. JPEN J Parenter Enteral Nutr. 2018;42:642–651. doi: 10.1177/0148607117709435. [DOI] [PubMed] [Google Scholar]
- 132.Kim MH, Kim H. The Roles of Glutamine in the Intestine and Its Implication in Intestinal Diseases. Int J Mol Sci. 2017;18 doi: 10.3390/ijms18051051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wang B, Wu G, Zhou Z, Dai Z, Sun Y, Ji Y, Li W, Wang W, Liu C, Han F, Wu Z. Glutamine and intestinal barrier function. Amino Acids. 2015;47:2143–2154. doi: 10.1007/s00726-014-1773-4. [DOI] [PubMed] [Google Scholar]
- 134.Zhou Q, Verne ML, Fields JZ, Lefante JJ, Basra S, Salameh H, Verne GN. Randomised placebo-controlled trial of dietary glutamine supplements for postinfectious irritable bowel syndrome. Gut. 2019;68:996–1002. doi: 10.1136/gutjnl-2017-315136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Corcoba A, Gruetter R, Do KQ, Duarte JMN. Social isolation stress and chronic glutathione deficiency have a common effect on the glutamine-to-glutamate ratio and myo-inositol concentration in the mouse frontal cortex. J Neurochem. 2017;142:767–775. doi: 10.1111/jnc.14116. [DOI] [PubMed] [Google Scholar]
- 136.Harnett NG, Wood KH, Ference EW, 3rd, Reid MA, Lahti AC, Knight AJ, Knight DC. Glutamate/glutamine concentrations in the dorsal anterior cingulate vary with Post-Traumatic Stress Disorder symptoms. J Psychiatr Res. 2017;91:169–176. doi: 10.1016/j.jpsychires.2017.04.010. [DOI] [PubMed] [Google Scholar]
- 137.El-Salhy M, Umezawa K, Hatlebakk JG, Gilja OH. Abnormal differentiation of stem cells into enteroendocrine cells in rats with DSS-induced colitis. Mol Med Rep. 2017;15:2106–2112. doi: 10.3892/mmr.2017.6266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.El-Salhy M, Mazzawi T, Umezawa K, Gilja OH. Enteroendocrine cells, stem cells and differentiation progenitors in rats with TNBS-induced colitis. Int J Mol Med. 2016;38:1743–1751. doi: 10.3892/ijmm.2016.2787. [DOI] [PMC free article] [PubMed] [Google Scholar]