Abstract
Background
Periodontitis is reported to be associated with preterm birth (spontaneous preterm labor and birth). Gastroesophageal reflux disease (GERD) is common during pregnancy and is expected to be related to periodontitis. However, little research has been done on the association among preterm birth, GERD and periodontitis. This study uses popular machine learning methods for analyzing preterm birth, GERD and periodontitis.
Methods
Data came from Anam Hospital in Seoul, Korea, with 731 obstetric patients during January 5, 1995 - August 28, 2018. Six machine learning methods were applied and compared for the prediction of preterm birth. Variable importance, the effect of a variable on model performance, was used for identifying major determinants of preterm birth.
Results
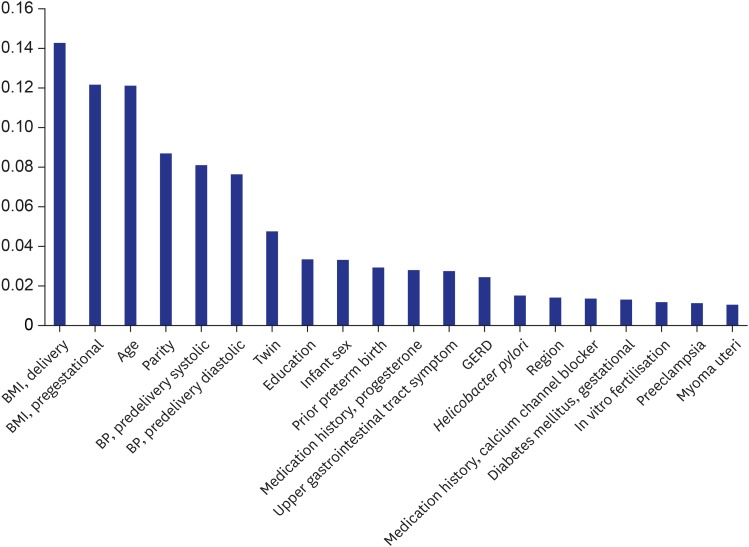
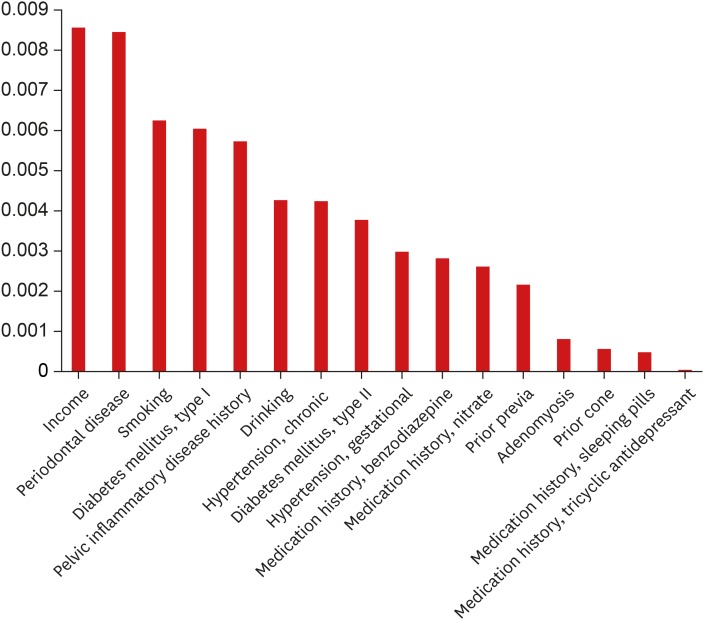
In terms of accuracy, the random forest (0.8681) was similar with logistic regression (0.8736). Based on variable importance from the random forest, major determinants of preterm birth are delivery and pregestational body mass indexes (BMI) (0.1426 and 0.1215), age (0.1211), parity (0.0868), predelivery systolic and diastolic blood pressure (0.0809 and 0.0763), twin (0.0476), education (0.0332) as well as infant sex (0.0331), prior preterm birth (0.0290), progesterone medication history (0.0279), upper gastrointestinal tract symptom (0.0274), GERD (0.0242), Helicobacter pylori (0.0151), region (0.0139), calcium-channel-blocker medication history (0.0135) and gestational diabetes mellitus (0.0130). Periodontitis ranked 22nd (0.0084).
Conclusion
GERD is more important than periodontitis for predicting and preventing preterm birth. For preventing preterm birth, preventive measures for hypertension, GERD and diabetes mellitus would be needed alongside the promotion of effective BMI management and appropriate progesterone and calcium-channel-blocker medications.
Keywords: Premature Birth, Gastroesophageal Reflux, Periodontitis
Graphical Abstract
INTRODUCTION
Preterm birth, i.e., birth between 20 and 37 weeks of gestation, is the leading cause of disease burden for infants and children in the world.1,2,3,4 Preterm birth affected one of every 10 newborns in the United States during 2003–2012, that is, 5,042,982 (12.2%) of 41,206,315 births.1 The proportion of preterm births registered a rapid growth from 4.3% to 6.0% in Korea between 2001–2010.2 These national patterns are consistent with their global counterparts. Every year 15 million births are preterm births, which are the leading cause of neonatal and childhood mortality in the world, responsible for 965,000 neonatal deaths and an additional 125,000 deaths among those aged one to five years. It is also estimated that 75% of this mortality can be prevented with cost-effective interventions.3,4
Meanwhile, 46% of adults in the United States suffer from chronic periodontitis, a set of inflammatory conditions affecting the tissues surrounding the teeth.5 A recent review implies an association between periodontitis and preterm birth through the development of an immune inflammatory response and the local suppression of growth factors in the fetal-placental unit.6 Gastroesophageal reflux disease (GERD) is defined as symptoms or complications caused by reflux of stomach contents, such as heartburn, regurgitation and dysphagia.7,8 Among GERD patients, 25.5% showed periodontitis and 44% dental erosion in a clinicopathologic study.9 Among GERD patients with long-term proton pump inhibitor medication, more erosive GERD patients suffered from severe periodontitis than did their non-erosive counterparts in a clinical trial.10 And GERD is reported to be common during pregnancy, i.e., 40% to 85% of pregnant women.11 These studies made independent suggestions on a positive linkage between GERD and periodontitis and on a positive relationship between periodontitis and preterm birth. In a similar context, one would expect a positive association between GERD and preterm birth but no research has been done on this issue.
The causes of spontaneous preterm labor and birth as a type of preterm birth (which is referred to as “preterm birth” hereafter for notational convenience) are still unclear in general. However, one previous study used popular machine learning methods for analyzing preterm birth and its major determinants.12 Data for the study came from Anam Hospital in Seoul, Korea, with 596 obstetric patients during March 27, 2014 - August 21, 2018. Six machine learning methods were applied and compared for the prediction of preterm birth. Variable importance, the effect of a variable on model performance, was used for identifying major determinants of preterm birth. Based on the results of the study, the accuracy of the artificial neural network (0.9115) was similar with those of logistic regression and the random forest (0.9180 and 0.8918, respectively). Based on variable importance from the artificial neural network, major determinants of preterm birth are body mass index (BMI) (0.0164), hypertension (0.0131) and diabetes mellitus (0.0099) as well as prior cone biopsy (0.0099), prior placenta previa (0.0099), parity (0.0033), cervical length (0.0001), age (0.0001), prior preterm birth (0.0001) and myomas & adenomyosis (0.0001). The results of the study agreed with existing literature in general,13,14,15,16 drawing the following policy implication: For preventing preterm birth, preventive measures for hypertension and diabetes mellitus would be needed alongside the promotion of cervical-length screening with different guidelines across the scope/type of prior conization.
However, the previous study above excluded many possible determinants of preterm birth including education, income, periodontitis, GERD, pelvic inflammatory disease history and medication history. It also suffered from the lack of information on the types of BMI, diabetes mellitus, hypertension and parity. This study extends the previous study by increasing the sample size, including more determinants and drawing additional clinical implications. Firstly, this study considers socioeconomic factors (education, income) and other possible obstetric variables such as periodontitis, upper gastrointestinal tract symptoms, GERD and Helicobacter pylori. Secondly, this study is characterized by the inclusion of pelvic inflammatory disease history and detailed information on the types of BMI (pregestational, delivery), diabetes mellitus (type I, type II, gestational), hypertension (chronic, gestational), and parity (full-term births, preterm births, abortions, children alive). Thirdly, this study pays due attention to medication history for progesterone, calcium channel blocker, nitrate, tricyclic antidepressant, benzodiazepine, and sleeping pills.
METHODS
Participants
Data came from Anam Hospital in Seoul, Korea, with 731 obstetric patients during January 5, 1995 - August 28, 2018. The data included some of the 596 participants in the previous study.12 The class label (or dependent variable) was spontaneous preterm labor and birth (or preterm birth, i.e., birth between 20 and 37 weeks of gestation, coded as “no” vs.“yes”). Here, labor was defined as regular uterine contraction with cervical change. The cases of indicated preterm birth were excluded. For this purpose, vaginal deliveries with the induction of labor were excluded, and cesarean deliveries were included in cases when women suffered from labor. And the following attributes (or independent variables) were included in this study: 1) demographic/socioeconomic factors, i.e., age, education (at/above vs. below high school graduation), income (no vs. yes for public insurance/Medicaid only), and region (rural, urban); 2) periodontitis (no, yes), upper gastrointestinal tract symptom (no, yes), GERD (no, yes), and H. pylori (no, yes); 3) other health-related determinants such as pregestational and delivery BMI, predelivery systolic and diastolic blood pressure (mmHg), smoking (no, yes), drinking (no, yes), type I, type II, and gestational diabetes mellitus (no vs. yes for each type), chronic and gestational hypertension (no vs. yes for each type), medication history (no vs. yes for each of progesterone, calcium channel blocker, nitrate, tricyclic antidepressant, benzodiazepine, sleeping pills), parity (full-term births, preterm births, abortions, children alive), prior preterm birth (no, yes), twin (no, yes), myoma uteri (no, yes), adenomyosis (no, yes), preeclampsia (no, yes), in vitro fertilization (no, yes), prior previa (no, yes), prior cone (no, yes), pelvic inflammatory disease history (no, yes), and infant sex (male, female). Here, periodontitis and GERD were screened from International Classification of Diseases-10 codes first and then confirmed by the review of medical records. As described above, periodontitis is defined as a set of inflammatory conditions affecting the tissues surrounding the teeth. Likewise, GERD is defined as symptoms or complications caused by reflux of stomach contents, such as heartburn, regurgitation and dysphagia.
Analysis
Six machine learning approaches were used for the prediction of preterm birth: logistic regression, decision tree, naïve Bayes, random forest, support vector machine and artificial neural network.12,17 Data on 731 participants were divided into training and validation sets with a 50:50 ratio. The models were built (or trained) based on the training set with 365 observations then the models trained were validated based on the validation set with 365 observations. Accuracy, a ratio of correct predictions among 365 observations, was introduced as a criterion for validating the models trained. Variable importance from the random forest, a mean-impurity gap between a complete model and a model excluding a certain variable, was adopted for identifying major determinants of preterm birth (mean impurity, or the degree of data being mixed at a node on average, is disproportional to accuracy). The greater “mean-impurity increase” is defined as the greater variable importance.12,17 Python 3.52 was employed for the analysis on June 2019.
Ethics statement
This retrospective study complied with the tenets of the Helsinki Declaration and was approved by the Institutional Review Board (IRB) of Korea University Anam Hospital on November 5, 2018 (2018AN0365). Informed consent was waived by the IRB.
RESULTS
Tables 1 and 2 show descriptive statistics for participants' preterm birth and attributes. Among 731 participants, 123 (16.8%), 244 (33.4%), 214 (29.3%), and 52 (7.1%) had preterm birth, upper gastrointestinal tract symptoms, GERD and periodontitis, respectively. On average, indeed, the age, pregestational BMI and delivery BMI of the participants were 30.5, 21.2, and 26.3, respectively. In terms of accuracy, the random forest (0.8681) was similar with logistic regression (0.8736) (Table 3). Based on variable importance from the random forest, major determinants of preterm birth are delivery and pregestational BMI (0.1426 and 0.1215), age (0.1211), parity (0.0868), predelivery systolic and diastolic blood pressure (0.0809 and 0.0763), twin (0.0476), education (0.0332) as well as infant sex (0.0331), prior preterm birth (0.0290), progesterone medication history (0.0279), upper gastrointestinal tract symptom (0.0274), GERD (0.0242), H. pylori (0.0151), region (0.0139), calcium-channel-blocker medication history (0.0135), and gestational diabetes mellitus (0.0130). Periodontitis ranked 22nd (0.0084) (Table 4, Figs. 1 and 2).
Table 1. Descriptive statistics for participants' preterm birth and categorical attributes.
| Categorical variables | Count, no | Count, yes | Yes, % | |
|---|---|---|---|---|
| Preterm birth | 608 | 123 | 16.8 | |
| Upper gastrointestinal tract symptom | 487 | 244 | 33.4 | |
| GERD | 517 | 214 | 29.3 | |
| Helicobacter pylori | 663 | 68 | 9.3 | |
| Periodontitis | 679 | 52 | 7.1 | |
| Education, below high school graduation | 546 | 185 | 25.3 | |
| Income, public insurance/Medicaid only | 662 | 69 | 9.4 | |
| Region, rural | 721 | 10 | 1.4 | |
| Smoking | 724 | 7 | 1.0 | |
| Drinking | 713 | 18 | 2.5 | |
| Diabetes mellitus | ||||
| Type I | 728 | 3 | 0.4 | |
| Type II | 726 | 5 | 0.7 | |
| Gestational | 686 | 45 | 6.2 | |
| Hypertension | ||||
| Chronic | 722 | 9 | 1.2 | |
| Gestational | 720 | 11 | 1.5 | |
| Medication history | ||||
| Progesterone | 534 | 197 | 26.9 | |
| Calcium channel blocker | 655 | 76 | 10.4 | |
| Nitrate | 729 | 2 | 0.3 | |
| Tricyclic antidepressant | 727 | 4 | 0.5 | |
| Benzodiazepine | 712 | 19 | 2.6 | |
| Sleeping pills | 726 | 5 | 0.7 | |
| Parity, code 0000a | 276 | 455 | 62.2 | |
| Prior preterm birth | 686 | 45 | 6.2 | |
| Twin | 715 | 16 | 2.2 | |
| Myoma uteri | 699 | 32 | 4.4 | |
| Adenomyosis | 730 | 1 | 0.1 | |
| Preeclampsia | 709 | 22 | 3.0 | |
| In vitro fertilization | 717 | 14 | 1.9 | |
| Prior previa | 726 | 5 | 0.7 | |
| Prior cone | 723 | 8 | 1.1 | |
| Pelvic inflammatory disease history | 721 | 10 | 1.4 | |
| Infant sex, female | 382 | 349 | 47.7 | |
GERD = gastroesophageal reflux disease.
a0 Full-term birth, 0 preterm birth, 0 abortion, 0 children alive.
Table 2. Descriptive statistics for participants' continuous attributes.
| Continuous variables | Mean | Min | Max | |
|---|---|---|---|---|
| Age, yr | 30.5 | 19.0 | 40.0 | |
| BMI | ||||
| Pregestational | 21.2 | 14.0 | 40.0 | |
| Delivery | 26.3 | 16.0 | 45.0 | |
| Blood pressure, mmHg | ||||
| Predelivery systolic | 113.3 | 80.0 | 190.0 | |
| Predelivery diastolic | 71.4 | 50.0 | 120.0 | |
BMI = body mass index.
Table 3. Model performance.
| Model | Accuracy/AUC |
|---|---|
| Multinomial logistic regression | 0.8736/0.76 |
| Decision tree | 0.7912/0.57 |
| Naive bayes | 0.8297/0.68 |
| Random forest-1000 trees | 0.8681/0.69 |
| Support vector machine | 0.8626/0.68 |
| Artificial neural network | 0.8626/0.54 |
AUC = area under the receiver-operating-characteristic curve.
Table 4. Variable importance.
| Variables (attribute) | Variable importance from the random forest |
|---|---|
| BMI, delivery | 0.1426 |
| BMI, pregestational | 0.1215 |
| Age | 0.1211 |
| Parity | 0.0868 |
| BP, predelivery systolic | 0.0809 |
| BP, predelivery diastolic | 0.0763 |
| Twin | 0.0476 |
| Education | 0.0332 |
| Infant sex | 0.0331 |
| Prior preterm birth | 0.0290 |
| Medication history, progesterone | 0.0279 |
| Upper gastrointestinal tract symptom | 0.0274 |
| GERD | 0.0242 |
| Helicobacter pylori | 0.0151 |
| Region | 0.0139 |
| Medication history, calcium channel blocker | 0.0135 |
| Diabetes mellitus, gestational | 0.0130 |
| In vitro fertilisation | 0.0116 |
| Preeclampsia | 0.0113 |
| Myoma uteri | 0.0104 |
| Income | 0.0085 |
| Periodontitis | 0.0084 |
| Smoking | 0.0062 |
| Diabetes mellitus, type I | 0.0060 |
| Pelvic inflammatory disease history | 0.0057 |
| Drinking | 0.0043 |
| Hypertension, chronic | 0.0042 |
| Diabetes mellitus, type II | 0.0038 |
| Hypertension, gestational | 0.0030 |
| Medication history, benzodiazepine | 0.0028 |
| Medication history, nitrate | 0.0026 |
| Prior previa | 0.0022 |
| Adenomyosis | 0.0008 |
| Prior cone | 0.0006 |
| Medication history, sleeping pills | 0.0005 |
| Medication history, tricyclic antidepressant | 0.0000 |
BMI = body mass index; BP = blood pressure; GERD = gastroesophageal reflux disease.
Fig. 1. Variable importance from the random forest: top 01–top 20.
BMI = body mass index, BP = blood pressure, GERD = gastroesophageal reflux disease.
Fig. 2. Variable importance from the random forest: top 21–top 36.
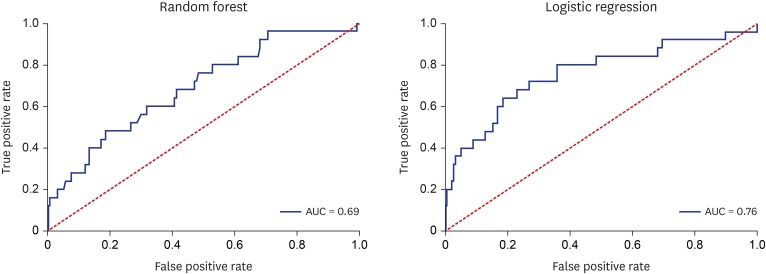
The results of logistic regression (Supplementary Table 1) provide useful information about the sign and magnitude for the effect of the major determinant on preterm birth. For example, the odds of preterm birth will increase by 4% (or 61%) if predelivery systolic blood pressure (or pregestational BMI) increases by 1 unit. Likewise, the odds of preterm birth is higher by 86% for those without calcium-channel-blocker medication history than those with it. It needs to be noted, however, that the findings of logistic regression are based on an unrealistic assumption of ceteris paribus, i.e., “all the other variables staying constant”. For this reason, the results of logistic regression need to be considered as just supplementary information to the variable importance from the random forest. Finally, Fig. 3 shows the receiver-operating-characteristic curves of the random forest and logistic regression. The area under the receiver-operating-characteristic curve (AUC) measures the power or usefulness of the model. Based on the measure, the random forest and logistic regression would be useful models: their respective AUCs, i.e., 0.69 and 0.76, are comparable to or higher than those of similar studies with 19,910 participants in the Duke University Medical Center during January 1, 1988 and June 1, 1997, i.e., 0.64–0.68.18,19,20
Fig. 3. Receiver-operating-characteristic curves.
AUC = area under the receiver-operating-characteristic curve.
DISCUSSION
In summary, the accuracy of the random forest was similar with that of logistic regression. Based on variable importance from the random forest, major determinants of preterm birth are delivery and pregestational BMI, age, parity, predelivery systolic and diastolic blood pressure, twin, education, as well as infant sex, prior preterm birth, progesterone medication history, upper gastrointestinal tract symptom, GERD, H. pylori, region, calcium-channel-blocker medication history, and gestational diabetes mellitus. Periodontitis is not likely to be a major determinant of preterm birth.
According to the empirical results above, this study draws the following clinical implications. Firstly, this study highlights the importance of predelivery hypertension, gestational diabetes mellitus and GERD as preventive measures for preterm birth. Several studies report a strong association of preterm birth with hypertension and diabetes mellitus during pregnancy.21,22,23 This study confirms these findings, suggesting that early interventions for hypertension and diabetes mellitus during pregnancy would be vital for preventing preterm birth and protecting maternal health. More effort should be made for developing the effective prevention programs based on rigorous clinical trials and promoting these programs among all risk groups. Indeed, several studies make independent suggestions on a positive linkage between GERD and periodontitis24,25 and on a positive relationship between periodontitis and preterm birth6. In a similar context, one would expect a positive association between GERD and preterm birth, and this study supports this expectation given the high importance ranking of GERD from the random forest in this study (13th). In fact, nausea, vomiting, and related oroesophageal and upper abdominal discomforts are quite common in pregnancy but pregnant women usually neglect the significant role of these common symptoms in more severe health conditions or outcomes such as preterm birth. Based on the results of this study, more active counseling for these common symptoms is really needed for effective prenatal care. Secondly, this study requests more attention to the promotion of effective BMI management and appropriate progesterone and calcium-channel-blocker medications as preventive measures for preterm birth. A systematic review states that vaginal progesterone decreases the risk of preterm birth and improves perinatal outcomes in singleton gestations with a midtrimester sonographic short cervix.26 Another systematic review indicates that calcium channel blockers for women in preterm labor have benefits over placebo or no treatment in terms of postponement of birth.27 The findings of this study agree with those of the reviews and more promotional efforts are needed in these regards.
Finally, a comment is to be made on the relationship between periodontitis and preterm birth. A recent review implies an association between the two variables through the development of an immune inflammatory response and the local suppression of growth factors in the fetal-placental unit.6 Based on variable importance from the random forest in this study, however, the importance ranking of periodontitis was low, i.e., 22nd. One possible explanation for this finding is the presence of GERD during pregnancy. Given that GERD is closely associated with periodontitis, severely refluxed gastric juice would damage periodontal tissue barriers to various pathogens such as bacteria and toxic substances, which would be related to placental colonization and systemic inflammation-associated preterm birth.
This study still had some limitations. Firstly, this study used a cross-sectional design because of limited data availability. Expanding data with a longitudinal design is expected to improve the accuracy of machine learning analysis much more. Secondly, this study did not consider possible mediating effects among variables. Thirdly, this study used data with a small sample size in a single center. Expanding this study to big data will be a good topic for future research. Fourthly, the AUCs of the random forest and logistic regression in this study (0.68 and 0.76) were comparable to or higher than those of the artificial neural networks in similar studies in the past (0.64–0.68)12,18,19,20 but it needs to be noted that there still exists some room for further improvement. Accurate classification and prediction of preterm birth are considered to be a very challenging task given a great variety of potential factors but the continued absence of reliable data on the variable. In this context, the AUCs of the random forest and logistic regression in this study would be a good starting point for further research, even though the results of this study might not be optimal as a diagnostic test yet. Fifthly, this study used the definition of preterm birth as birth between 20 and 37 weeks of gestation. However, preterm birth can be divided into several categories, e.g., previable, extremely (early), very (early), early and late preterm birth. Comparing various determinants for different categories of preterm birth will be an interesting topic for future study. Sixthly, it was beyond the scope of this study to analyze a plausible mechanism of the positive association between GERD and preterm birth. Little research has been done and more investigation is needed in this direction. Finally, further analysis of specific patients, e.g., symptomatic vs. asymptomatic, low- vs. high-risk, single vs. multiple gestation, would offer more insight on this line of research with more detailed clinical implications.
In conclusion, GERD would be more important than periodontitis for predicting and preventing preterm birth. For preventing preterm birth, preventive measures for hypertension, GERD and diabetes mellitus would be needed alongside the promotion of effective BMI management and appropriate progesterone and calcium-channel-blocker medications.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Lee KS, Song IS, Kim ES, Ahn KH.
- Data curation: Lee KS, Ahn KH.
- Formal analysis: Lee KS, Ahn KH.
- Investigation: Lee KS, Ahn KH.
- Methodology: Lee KS, Song IS, Kim ES, Ahn KH.
- Software: Lee KS, Ahn KH.
- Validation: Lee KS, Ahn KH.
- Writing - original draft: Lee KS, Song IS, Kim ES, Ahn KH.
- Writing - review & editing: Lee KS, Song IS, Kim ES, Ahn KH.
SUPPLEMENTARY MATERIAL
Logistic regression results
References
- 1.Magro Malosso ER, Saccone G, Simonetti B, Squillante M, Berghella V MagroMalosso ER. US trends in abortion and preterm birth. J Matern Fetal Neonatal Med. 2018;31(18):2463–2467. doi: 10.1080/14767058.2017.1344963. [DOI] [PubMed] [Google Scholar]
- 2.Lee NH. International trends and implications for preterm birth. Health Soc Welf Forum. 2013;(200):116–127. [Google Scholar]
- 3.World Health Organization. News: preterm birth. [Updated 2018]. [Accessed June 1, 2019]. http://www.who.int/news-room/fact-sheets/detail/preterm-birth.
- 4.Harrison MS, Goldenberg RL. Global burden of prematurity. Semin Fetal Neonatal Med. 2016;21(2):74–79. doi: 10.1016/j.siny.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 5.Eke PI, Dye BA, Wei L, Slade GD, Thornton-Evans GO, Borgnakke WS, et al. Update on prevalence of periodontitis in adults in the United States: NHANES 2009 to 2012. J Periodontol. 2015;86(5):611–622. doi: 10.1902/jop.2015.140520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Puertas A, Magan-Fernandez A, Blanc V, Revelles L, O'Valle F, Pozo E, et al. Association of periodontitis with preterm birth and low birth weight: a comprehensive review. J Matern Fetal Neonatal Med. 2018;31(5):597–602. doi: 10.1080/14767058.2017.1293023. [DOI] [PubMed] [Google Scholar]
- 7.Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101(8):1900–1920. doi: 10.1111/j.1572-0241.2006.00630.x. [DOI] [PubMed] [Google Scholar]
- 8.Patrick L. Gastroesophageal reflux disease (GERD): a review of conventional and alternative treatments. Altern Med Rev. 2011;16(2):116–133. [PubMed] [Google Scholar]
- 9.Vinesh E, Masthan K, Kumar MS, Jeyapriya SM, Babu A, Thinakaran M. A clinicopathologic study of oral changes in gastroesophageal reflux disease, gastritis, and ulcerative colitis. J Contemp Dent Pract. 2016;17(11):943–947. doi: 10.5005/jp-journals-10024-1959. [DOI] [PubMed] [Google Scholar]
- 10.Deppe H, Mücke T, Wagenpfeil S, Kesting M, Rozej A, Bajbouj M, et al. Erosive esophageal reflux vs. non erosive esophageal reflux: oral findings in 71 patients. BMC Oral Health. 2015;15(1):84. doi: 10.1186/s12903-015-0069-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ali RA, Egan LJ. Gastroesophageal reflux disease in pregnancy. Best Pract Res Clin Gastroenterol. 2007;21(5):793–806. doi: 10.1016/j.bpg.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 12.Lee KS, Ahn KH. Artificial neural network analysis of spontaneous preterm labor and birth and its major determinants. J Korean Med Sci. 2019;34(16):e128. doi: 10.3346/jkms.2019.34.e128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim YJ, Lee BE, Park HS, Kang JG, Kim JO, Ha EH. Risk factors for preterm birth in Korea: a multicenter prospective study. Gynecol Obstet Invest. 2005;60(4):206–212. doi: 10.1159/000087207. [DOI] [PubMed] [Google Scholar]
- 14.Di Renzo GC, Giardina I, Rosati A, Clerici G, Torricelli M, Petraglia F, et al. Maternal risk factors for preterm birth: a country-based population analysis. Eur J Obstet Gynecol Reprod Biol. 2011;159(2):342–346. doi: 10.1016/j.ejogrb.2011.09.024. [DOI] [PubMed] [Google Scholar]
- 15.Boghossian NS, Yeung E, Albert PS, Mendola P, Laughon SK, Hinkle SN, et al. Changes in diabetes status between pregnancies and impact on subsequent newborn outcomes. Am J Obstet Gynecol. 2014;210(5):431.e1–431.e14. doi: 10.1016/j.ajog.2013.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Premkumar A, Henry DE, Moghadassi M, Nakagawa S, Norton ME. The interaction between maternal race/ethnicity and chronic hypertension on preterm birth. Am J Obstet Gynecol. 2016;215(6):787.e1–787.e8. doi: 10.1016/j.ajog.2016.08.019. [DOI] [PubMed] [Google Scholar]
- 17.Han J, Micheline K. Data Mining: Concepts and Techniques. 2nd ed. San Francisco, CA: Elsevier; 2006. [Google Scholar]
- 18.Goodwin LK, Maher S, editors. Data mining for preterm birth prediction; Proceedings of the 2000 ACM Symposium on Applied Computing; 2000 Mar 19–21; Villa Olmo, Italy. New York: Association for Computing Machinery; 46. p. 51. [Google Scholar]
- 19.Goodwin LK, Iannacchione MA, Hammond WE, Crockett P, Maher S, Schlitz K. Data mining methods find demographic predictors of preterm birth. Nurs Res. 2001;50(6):340–345. doi: 10.1097/00006199-200111000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Goodwin LK, Iannacchione MA. Data mining methods for improving birth outcomes prediction. Outcomes Manag. 2002;6(2):80–85. [PubMed] [Google Scholar]
- 21.Sibai BM, Caritis SN, Hauth JC, MacPherson C, VanDorsten JP, Klebanoff M, et al. Preterm delivery in women with pregestational diabetes mellitus or chronic hypertension relative to women with uncomplicated pregnancies. The National Institute of Child Health and Human Development Maternal- Fetal Medicine Units Network. Am J Obstet Gynecol. 2000;183(6):1520–1524. doi: 10.1067/mob.2000.107621. [DOI] [PubMed] [Google Scholar]
- 22.Hedderson MM, Ferrara A, Sacks DA. Gestational diabetes mellitus and lesser degrees of pregnancy hyperglycemia: association with increased risk of spontaneous preterm birth. Obstet Gynecol. 2003;102(4):850–856. doi: 10.1016/s0029-7844(03)00661-6. [DOI] [PubMed] [Google Scholar]
- 23.Zhang J, Villar J, Sun W, Merialdi M, Abdel-Aleem H, Mathai M, et al. Blood pressure dynamics during pregnancy and spontaneous preterm birth. Am J Obstet Gynecol. 2007;197(2):162.e1–162.e6. doi: 10.1016/j.ajog.2007.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Song JY, Kim HH, Cho EJ, Kim TY. The relationship between gastroesophageal reflux disease and chronic periodontitis. Gut Liver. 2014;8(1):35–40. doi: 10.5009/gnl.2014.8.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Adachi K, Mishiro T, Tanaka S, Yoshikawa H, Kinoshita Y. A study on the relationship between reflux esophagitis and periodontitis. Intern Med. 2016;55(18):2523–2528. doi: 10.2169/internalmedicine.55.6898. [DOI] [PubMed] [Google Scholar]
- 26.Romero R, Conde-Agudelo A, Da Fonseca E, O'Brien JM, Cetingoz E, Creasy GW, et al. Vaginal progesterone for preventing preterm birth and adverse perinatal outcomes in singleton gestations with a short cervix: a meta-analysis of individual patient data. Am J Obstet Gynecol. 2018;218(2):161–180. doi: 10.1016/j.ajog.2017.11.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Flenady V, Wojcieszek AM, Papatsonis DN, Stock OM, Murray L, Jardine LA, et al. Calcium channel blockers for inhibiting preterm labour and birth. Cochrane Database Syst Rev. 2014;(6):CD002255. doi: 10.1002/14651858.CD002255.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Logistic regression results