Abstract
Low- and middle-income countries have been undertaking health finance reforms to address shortages of medicines. However, data are lacking on how medicine availability and stock-outs influence access to health services in Tanzania. The current study assesses the effects of medicine availability and stock-outs on healthcare utilization in Dodoma region, Tanzania. We conducted a cross-sectional study that combined information from households and healthcare facility surveys. A total of 4 hospitals and 89 public primary health facilities were surveyed. The facility surveys included observation, record review over a 3-month period prior to survey date, and interviews with key staff. In addition, 1237 households within the health facility catchment areas were interviewed. Data from the facility survey were linked with data from the household survey. Descriptive analysis and multivariate logistic regressions models were used to assess the effects of medicine availability and stock-outs on utilization patterns and to identify additional household-level factors associated with health service utilization. Eighteen medicines were selected as ‘tracers’ to assess availability more generally, and these were continuously available in ∼70% of the time in facilities across all districts over 3 months of review. The main analysis showed that household’s healthcare utilization was positively and significantly associated with continuous availability of all essential medicines for the surveyed facilities [odds ratio (OR) 3.49, 95% confidence interval (CI) 1.02–12.04; P = 0.047]. Healthcare utilization was positively associated with household membership in the community health insurance funds (OR 1.97, 95% CI 1.23–3.17; P = 0.005) and exposure to healthcare education (OR 2.75, 95% CI 1.84–4.08; P = 0.000). These results highlight the importance of medicine availability in promoting access to health services in low-income settings. Effective planning and medicine supply management from national to health facility level is an important component of quality health services.
Keywords: Medicines availability, healthcare utilization, Dodoma, Tanzania
Key Messages
The availability of quality medicines in the provision of healthcare service is an integral part of universal health coverage, shapes health service delivery as well as household healthcare utilization.
Availability of most tracer medicines was relatively good, with frequent stock-outs of a few medicines and variation across level of care and across districts.
Better forecasting of upcoming medicine needs and timely ordering at health facilities, along with the improved availability of medicines at the medical store department, could help prevent stock-outs and improve availability.
Introduction
The availability of quality medicines in the provision of healthcare service is an integral part of universal health coverage (UHC; Prinja et al., 2015). Evidence suggests that the availability of medicines is essential for healthcare service delivery (Obare et al., 2014; Bigdeli et al., 2015). In low- and middle-income countries (LMICs) the availability of essential medicines in public health facilities ranges from 17.9% to 87.1% (WHO, 2014). The proportion of total health expenditure spent on medicines in low-income countries ranges widely from 7.7% to 67.6% (Lu et al., 2011). In addition, a limited proportion of funds for medicines is allocated to primary health facilities in these countries (Kusemererwa et al., 2016). Coupled with frequent supply chain management problems (Cameron et al., 2009; YALE, 2011), access to quality medicines is often limited, contributing to inequalities and deficits in access to health services and ultimately influencing health outcomes (Chen et al., 2014; Masters et al., 2014). The lack of medicines in health facilities fosters the use of over-the-counter medicines or products from unqualified sources, exposing consumers to the risks of using counterfeit or substandard products (Jia et al., 2016). In addition, a large proportion of medicines is paid for out-of-pocket, potentially exposing households to financial hardship (Lu et al., 2011; Prinja et al., 2015; Luiza et al., 2016).
Several LMICs have undertaken or are undertaking health finance reforms (Mtei et al., 2007; Fenny et al., 2018) aimed at increasing the availability of medicines at an affordable cost. The emphasis of some reforms has been on expansion of social health insurance schemes (Mcintyre et al., 2013; Fenny et al., 2018) and direct health facility financing (Kapologwe et al., 2019) as a means of generating more revenue to purchase medicines and to protect citizens from the risk of catastrophic health expenditure (Saksena et al., 2011; Kusi et al., 2015; Ataguba and Ingabire, 2016). Furthermore, other initiatives undertaken include the strengthening of public–private partnerships as a means of ensuring healthcare facilities have sufficient medicines to carter for the population needs throughout the year (WHO, 2000; Rutta et al., 2015; Embrey et al., 2016; USAID, 2016).
The continuous availability of essential medicines within primary healthcare facilities plays an important role in promoting access to and utilization of health services. On the other hand, frequent stock-outs of medicines have been shown to influence healthcare utilization (Mwabu et al., 1993; Anselmi et al., 2015). In Uganda, the continued absence of medicines in public health facilities was found to influence healthcare utilization and individual decisions to consult health service providers (Shaikh and Hatcher, 2005; Musoke et al., 2014). The availability of medicines positively affects patient trust in healthcare providers (Shan et al., 2016), while medicine stock-outs in facilities foster distrust in healthcare providers and contributes to low utilization of the formal healthcare system (Mkoka et al., 2014). Trust in healthcare providers is important; it shapes household healthcare utilization patterns, it influences medication adherence (Brennan et al., 2013) and it fosters communication with service providers (Al-Mandhary et al., 2007). A number of other factors have also been found to influence household healthcare-seeking behaviour. In rural areas, long distances to reach a formal healthcare provider results in the underuse of health services (Tran et al., 2016). The availability of sufficient transport systems and close geographic proximity to healthcare facilities positively influences healthcare service utilization (Shaikh and Hatcher, 2005; Feikin et al., 2009). In addition, affordability of healthcare services influences household’s healthcare-seeking behaviour; evidence suggest that health insurance increases the probability of households seeking care (Saksena et al., 2011; Chomi et al., 2014; Ahmed et al., 2018; Atnafu et al., 2018) and protects them against impoverishment from out-of-pocket expenditures (Saksena et al., 2011; Spaan et al., 2012).
To our knowledge, most studies assessing how medicine availability influences healthcare utilization in Tanzania have focused on specific diseases such as diarrhoea, fever/malaria, tuberculosis, chronic diseases and acute respiratory infection (Mikkelsen-Lopez et al., 2013; Kante et al., 2015; Nnko et al., 2015; Senkoro et al., 2015); on special vulnerable populations such as people who inject drugs; or on the influence of health insurance systems overall (Chomi et al., 2014; Mlunde et al., 2016). However, no study investigated how medicine availability and stock-outs influence healthcare utilization in the general population by integrating information from the healthcare facility and households. This study assesses the effects of medicine availability and stock-outs on healthcare utilization in Dodoma region, Tanzania by combining data of households and health facilities survey.
Study setting
Tanzania has a decentralized health system which gives district councils authority to manage available resources district healthcare facilities. The central government, in turn, allocates funds to the medical store department (MSD), the main supplier of medicines, medical equipment and medical supplies to public healthcare facilities. However, several barriers challenge MSD’s effectiveness in supplying medicines to the health facilities, including inadequate funds for medicines, delays in disbursement of allocated funds, inaccurate forecasting of medicines at the facility and national level, thefts, stock-outs at the national MSD warehouse and ineffective systems for fulfilling back-ordered items (YALE, 2011). Nevertheless, health facilities and districts have funds available that are earmarked for purchasing supplementary medicines from the private sector when MSD is out-of-stock (HPSS, 2014). Funding for complementary medicines and supplies is closely linked with fiscal decentralization of public financial management and the community health fund (CHF ‘iliyoboreshwa’) system. These medicines are paid from the regular sources of complementary funds available such as those of the CHF, of the national health insurance fund (NHIF), of user fees, and the basket funds provided by the government, the donors and the private sector. However, the availability of medicines within the public sector in district-level facilities tends to be insufficient, in turn, affecting the quality of services. A survey conducted in 2012 in Dodoma region reported a stock-out rate of 46% and an order fulfilment rate of 59% from MSD (HPSS, 2011). The purchase of supplementary medicines has been reported to be fragmented, unco-ordinated, inefficient and lacking transparency (HPSS, 2014). In 2014, regional authority and district councils started implementing a complementary pharmaceutical supply system funded by Swiss Agency for Development and Cooperation through the Health Promotion and Systems Strengthening (HPSS) project known as Jazia Prime Vendor system (Jazia PVS). The aim of Jazia PVS is to improve the availability of medicines in the Dodoma region by complementing MSD supply. Jazia PVS is a unique public–private partnership between the health authorities of the Dodoma region and a private supplier (HPSS, 2014). The Jazia PVS consolidates and pools orders for supplementary medicines from all public healthcare facilities at the district level and purchases from one contracted supplier, the Prime Vendor. Medicines are paid for using the funds collected through national insurance schemes (CHF and NHIF), user fees and basket funds (Mushi, 2014). Jazia PVS was designed to address shortages of medicines in primary-level public health facilities by pooling the limited resources available from districts councils. Healthcare decision-makers require information on the effectiveness of the Jazia PVS, including the effect on medicines availability and stock-outs and on household healthcare utilization.
This study was carried out in six district councils in the Dodoma region in Tanzania where the Jazia PVS was implemented: Kondoa, Kongwa, Dodoma city council, Bahi, Mpwapwa and Chemba. Table 1 presents information about the included districts in Dodoma region. The region has a population of 2 083 588. Of the six district councils, Dodoma municipal has the largest population (410 956) whereas Bahi district council has the smallest population (221 645). Bahi has the largest average number of primary healthcare facilities per 10 000 population (1.8), followed by Chemba and Kongwa district councils (1.4) and Dodoma city council has the fewest (0.8).
Table 1.
Districts council basic information
| District council variable | Kondoa | Kongwa | Dodoma city | Bahi | Mpwapwa | Chemba |
|---|---|---|---|---|---|---|
| Populationa | 269 704 | 309 973 | 410 956 | 221 645 | 305 056 | 235 711 |
| Area coverage (km2) | 5921 | 4041 | 2576 | 5948 | 7479 | 7289 |
| Number of public health centresb | 2 | 4 | 7 | 6 | 2 | 4 |
| Number of public dispensariesb | 27 | 40 | 27 | 35 | 39 | 30 |
| Number of private health facilitiesb | 11 | 8 | 29 | 2 | 5 | 4 |
| Number of primary care facilities per 10 000 population | 1.1 | 1.4 | 0.8 | 1.8 | 1.3 | 1.4 |
| Number of primary health facilities surveyed | ||||||
| Hospital | 1 | 1 | 1 | 0 | 1 | 0 |
| Health centres | 2 | 1 | 1 | 3 | 1 | 3 |
| Dispensaries | 6 | 16 | 13 | 12 | 18 | 13 |
| Total staffing in the surveyed health centre | ||||||
| Clinical cadrec | 3 | 2 | 2 | 9 | 2 | 2 |
| Nurse cadred | 14 | 4 | 0 | 39 | 4 | 4 |
| Pharmacists cadree | 0 | 0 | 0 | 1 | 0 | 0 |
| Total staffing in the surveyed dispensary clinical cadre | 1 | 7 | 8 | 4 | 5 | 3 |
| Nurse cadre | 15 | 18 | 29 | 45 | 27 | 22 |
| Pharmacists cadre | 0 | 0 | 0 | 0 | 0 | 0 |
| Household interviews | ||||||
| Household selected (n = 1264) | 194 | 223 | 296 | 160 | 221 | 170 |
| Household interviewed (n = 1237) | 195 | 220 | 281 | 168 | 201 | 172 |
| Household response rate (%) (98.5)f | 100.5 | 98.7 | 94.9 | 105 | 91.0 | 101.2 |
NBS, Tanzania National Bureau of Statistics; Population and Housing Census 2013.
http://hfrportal.ehealth.go.tz/ (accessed 15 January 2018; only operating facilities).
Composed of Medical Doctor (MD), Assistant Medical Officer (AMO) and Clinical Officer (CO).
Composed of Medical Attendant (Nurse Assistant), Nurse Midwife and Nurse Officer.
Composed of Pharmacist, Pharmaceutical Assistant and Pharmaceutical Technician.
Variation of household response rates by district was due to the fact that some of sampled iCHF households members have permanently/temporarily migrated out of the sampled villages as it was a harvesting time and some villages had changed their administrative boundaries hence the names of households do not appear in the sampled villages, therefore, there was a need to sample extra households.
Methods
Study design
Two cross-sectional surveys were conducted in May 2017 in Dodoma region: (1) a household survey and (2) a healthcare facility survey. The two surveys covered the same areas and were then combined together to assess the effects of medicines availability and stock-outs on household healthcare utilization.
Health facility survey
The sample size for the healthcare facilities was 50% of all government health facilities (267) covered by the Health Promotion and System Strengthening programme in Dodoma region. The health facilities were stratified into three categories, namely hospitals, health centres and dispensaries. A probability proportional to size sampling design was utilized, whereby the number of health facilities selected was adjusted based on the number of healthcare facilities in the district. Thus districts with larger numbers of health facilities had a greater number of health facilities included in the sample. A total of 4 hospitals and 89 public primary healthcare facilities (11 health centres and 78 dispensaries) were randomly selected and surveyed in May 2017 across the seven districts. Surveys included observation, record review and interview with key staff at each health facility selected. Healthcare facility staff was interviewed to collect data on medicine availability, frequency and duration of medication stock-outs, reasons for stock-outs and facility staffing levels (Supplementary material S2: Sample of health facility survey tool). The survey addressed the previous 3-month period of February to April 2017.
The availability of 18 tracer medicines was examined from existing health facility records (Supplementary Table S1). The 18 tracer medicines were selected to align with the medications targeted by the HPSS-Jazia PVS. A pharmacist and an enumerator verified the availability and stock-outs of medications using a review of facility records from the previous 3 months (90 days) prior to the survey. The average number of days a facility had experienced stock-outs for each of 18 medicines was recorded (Supplementary Table S2). We categorized health facilities as those with and without any stock-outs over the observation period of 3 months prior to the survey date and this variable was included in the final regression model.
Household survey
A multi-stage sampling approach was used in the selection of wards and villages from the councils. In the first stage, a list of wards was obtained and three wards from each district were randomly selected. The second stage of selection involved the random selection of two villages from each ward. In total, 42 villages were chosen across the district councils. The sample size was obtained by adopting a formula from Cochran with consideration of households who had enrolled in CHF and those who are not enrolled (Cochran, 1977). A random sample of 1237 households was interviewed from the villages. At the village level, households were categorized into two categories, the first group consisted of those who were previously enrolled in the CHF ‘iliyoboreshwa’ scheme (415 households) that were randomly selected for interview from the Insurance Management Information System database. While the second group were non-CHF members (822 households) that were randomly selected from a list of all households in the village, obtained from a village chairperson. At each household, the head of the household or his/her representative was interviewed to collect information on household demographic and economic characteristics, healthcare access and utilization. Demographic and economic characteristics included ownership of assets, household income and expenditure and health insurance status. Recent healthcare utilization, illness episodes and health problems, reasons for not consulting health services; waiting times at healthcare facilities where care was sought, distance from the closest healthcare facility, trust to healthcare providers and exposure to health education were also assessed. Potential respondents aged 18 years and above were eligible to participate. In this study, health education has been conceptualized as one of the strategies of health promotion intended to raise community awareness of relevant health issues and enhance knowledge in improving health such as preventing illness and seeking timely and appropriate health assistance.
Data collection and management
A team of six experienced supervisors, 5 district pharmacists and 21 enumerators were recruited for field data collection. In each district, a pharmacist and one enumerator conducted the health facility survey. Four enumerators implemented the household’s survey. All supervisors, pharmacists and enumerators together with research scientists underwent a 3 days training session. Health facility and household survey tools were pre-tested villages in Dodoma rural district council that were included in the study sample. Open Data Kit technologies on Android mobile devices were used for data collection and management in both surveys. Data from both surveys were exported and analysed in STATA version 13.0. The household and healthcare facility response rate across all the district councils was 98.5% and 100%, respectively.
Data from facility surveys were linked with data from household surveys conducted in the same geographical location. To this end, we first used the household information on place of residence (such as village and ward/street) to match households with facilities in the same village or area. Secondly, we then matched the two surveys using global positioning system co-ordinates of both health facilities and households’ village to visualize the spatial distribution of households and health facilities using the ArcGIS software v10.5 (ESRI, Redland, CA, USA). The shapefiles of Dodoma region were obtained from the National Bureau of Statistics (http://www.nbs.go.tz/) and geo-processing was used to dissolve to the district level. The results for the second stage are presented in Supplementary Figure S1: Map of Dodoma showing the distribution of healthcare facilities and households surveyed. A total of 577 households out of 1237 (47%) surveyed households were successfully linked across six out of the seven district councils. We could not include one district, Chamwino, in the study due to the fact that none of the 20 facilities surveyed was in the catchment area of the households surveyed (232).
Analysis
Descriptive statistics
Descriptive statistics were generated for the health facility and household survey data. We computed frequencies and percentages of reported medicine availability/stock-outs considering facilities with and without any stock-out of medicines within the observation period of 90 days (3 months). The mean value of medicines availability in the surveyed facilities was 0.73 with the minimum–maximum value of (0.22–1.00; Supplementary Table S3).
Descriptive statistics were used to summarize household economic and demographic characteristics and healthcare utilization. We then used ‘t-tests’ to assess whether the difference in proportions between districts for each variable was statistically significant. The descriptive statistics informed the variables (covariates) included in the multivariate logistic regression model, to assess the effects of medicines availability and stock-outs on healthcare utilization.
Empirical strategy
A ‘Pearson’s correlation’ analysis was used to examine the strength and direction of the linear relationship between facilities without any stock-outs and household use of public healthcare facilities. We hypothesized that household healthcare utilization would be affected by a continuous availability of medicine and stock-outs. Other variables which could affect healthcare utilization included sociodemographic variables, CHF insurance coverage, level of trust in facility staff, receiving healthcare education, waiting time at the health facility, distance to the facility, chronic illness in at least one household member and household income (Supplementary Table S5). Backward elimination was used to arrive at the final model, a technique in which variables with the highest P-values were eliminated one by one, conditional on the P-value being bigger than some pre-determined level (P > 0.60). Furthermore, the models were subjected to a diagnostic test to ensure the model was correctly specified; we used the link test for model specification (Long and Freese, 2006). The regression analysis has been clustered at the facility level, relaxing the assumption of independence (Cameron and Miller, 2015).
We created a household wealth index including indicators relating to housing characteristics (water source, toilet type, nature of the flooring, nature of roof) and assets (electricity, radio, TV, mobile phone, car, refrigerator, bicycle) using polychoric principal component analysis (Vyas and Kumaranayake, 2006). The constructed wealth index was used as a proxy measure of the household living standard; households were ranked according to the wealth index score and generated wealth quintiles of each household, five equally sized groups. Sampled households were classified according to the five wealth quintiles.
Results
Descriptive statistics
Availability of medicines in healthcare facilities
Table 2 presents results on the availability of 18 tracer medicines in the sampled facilities along with the mean days of medicine stock-outs in the 3 months prior to the survey (Supplementary Table S2). Availability of artemether/lumefantrine (ALU) was generally high in all facilities in all districts above 85.7%. Availability of amoxicillin caps or cotrimoxazole tabs was above 70.0% in five districts, except Chemba district where availability was 57.8%. Availability of Amoxicillin syrup and cotrimoxazole suspension in all facilities in all districts was below 65%, with 73.3%, 70.6% and 68.4% of facilities in Kongwa, Bahi and Mpwapwa, respectively, experiencing stock-outs for >14 days. We found that availability of Ceftriaxone 1 g injection/250 g injection in all facilities in all districts was above 85.0% in Chemba and Kondoa districts.
Table 2.
Availability of medicine for the last 3 months prior to the date of the survey
| District name (n = number of facilities), no stock-out was observed for 90 days (%) | Kondoa (n = 8) | Kongwa (n = 17) | Dodoma city (n = 14) | Bahi (n = 15) | Mpwapwa (n = 19) | Chemba (n = 16) | Total (n = 89) |
|---|---|---|---|---|---|---|---|
| ALU orala | 100.0 | 100.0 | 85.7 | 100.0 | 94.7 | 100.0 | 96.6 |
| Quinine injection or artesunate injectionb | 62.5 | 70.6 | 64.3 | 93.3 | 89.5 | 93.7 | 80.9 |
| Amoxicillin caps or cotrimoxazole tabsa | 87.5 | 70.6 | 85.7 | 93.3 | 57.8 | 93.1 | 79.8 |
| Amoxicillin syrup or cotrimoxazole suspension | 62.5 | 29.4 | 42.9 | 20.0 | 31.6 | 56.3 | 38.2 |
| Benzyl penicillin 5 MU injectiona | 87.5 | 41.2 | 35.7 | 80.0 | 73.7 | 93.6 | 67.4 |
| Ceftriaxone 1 g injection/250 g injectionc | 87.5 | 52.9 | 64.3 | 53.3 | 52.6 | 93.6 | 65.2 |
| Mebendazole or albendazole tabsa | 87.5 | 64.7 | 78.6 | 86.7 | 52.6 | 81.3 | 73.0 |
| Griseofulvin oral or clotrimoxazole creamc | 87.5 | 17.6 | 64.3 | 60.0 | 73.7 | 75.0 | 60.7 |
| Metronidazole tabsa | 100.0 | 76.5 | 78.6 | 100.0 | 63.2 | 100.0 | 84.3 |
| ORS sacheta | 87.5 | 64.7 | 64.3 | 73.3 | 57.8 | 93.7 | 71.9 |
| Paracetamol 500 mg tabsc | 100.0 | 64.7 | 71.4 | 33.3 | 47.4 | 100.0 | 66.3 |
| Medroxyprogesterone acetate (depo) injectiona | 100.0 | 94.1 | 100.0 | 93.3 | 73.7 | 100.0 | 92.1 |
| Oxytocin injectiona | 100.0 | 100.0 | 85.7 | 100.0 | 100.0 | 100.0 | 97.8 |
| Ferrous salt and folic acidc | 50.0 | 11.8 | 50.0 | 26.7 | 31.6 | 0.0 | 25.8 |
| Vaccine, e.g. DTP vaccinea | 100.0 | 100.0 | 78.6 | 93.3 | 89.4 | 100.0 | 93.3 |
| Ophthalmologic drops or creama | 87.5 | 58.8 | 71.4 | 53.3 | 84.2 | 100.0 | 75.3 |
| Dextrose 5% or DNS or Ringer solutionc | 87.5 | 64.7 | 64.3 | 93.3 | 42.1 | 100.0 | 73.0 |
| Adrenaline injectionc | 87.5 | 52.9 | 57.1 | 80.0 | 100.0 | 93.6 | 78.6 |
Significance at 5% level.
Significance at 10% level.
Significance at 1% level.
DNS, Dextrose normal saline; ORS, Oral rehydration salts.
Availability of paracetamol 500 mg tabs was generally high in all facilities in Kondoa and Chemba reaching 100.0%. However, it was lower in Bahi and Mpwapwa, below 50.0%, with several facilities reporting stock-out for >14 days (53.3% and 31.6%, respectively). Availability of oxytocin injection was generally high in all facilities in all districts above 85.6%. A 100% availability of diphtheria, tetanus and pertussis (DTP) vaccine was reported in Kondoa, Kongwa and Chemba district councils.
Availability of ferrous salt and folic acid was below 52.0% across all the facilities in all the districts, and most facilities reported stock-outs of >14 days. About 41.2% and 35.7% of facilities in Kongwa and Dodoma city, respectively, experienced stock-out of adrenaline injection that lasted >14 days.
Availability of individual medicines by facility level over the observed period of 3 months is presented in Supplementary Table S1. The availability of most medications varied substantially across facility levels. All health centres had 100.0% availability of ALU, whereas 96.2% of the dispensaries had ALU. Mebendazole was available in 72.7% of health centres and 73.1% of dispensaries. All health centres had a 63.5% availability of paracetamol, compared with 66.7% of dispensaries. Only 28.2% of dispensaries and 9.1% of health centre had ferrous salt in stock.
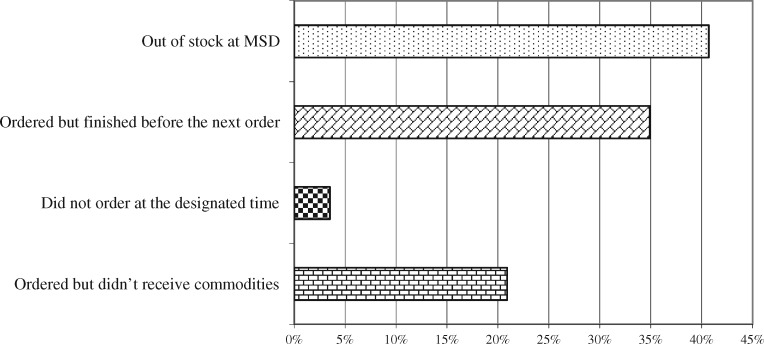
Out of 89 healthcare facility surveyed the most commonly reported reasons for the medicines stock-out were lack of availability of medication at MSD (40.7%), use of all stocked medicines before the next order arrived (34.9%), failure to receive medicines that had been ordered (20.9%) and failure of facility to send orders at designated time (3.5%; Figure 1).
Figure 1.
Reasons for the out of stock for the past 3 months.
Household’s demographic and socioeconomic characteristics
Table 3 presents information on the participant’s demographic and socioeconomic characteristics. The majority of the surveyed households were male-headed (68.6%). The average age of respondents was 49.6 years [standard deviation (SD): 16.2]. Most heads of the households were aged between 46 and 64 years (31.3%), or between 36 and 45 years (26.2%). Few households were headed by someone below 25 years of age (5.2%). Most of the heads of households (68.3%) had attended primary school up to grade five while few (5.7%), had secondary education and above, and 26.0% had not attended formal education. About half (48.9%) heads of households were farmers, 24.3% were not employed and very few (2.4%) were employed in a formal sector position. The majority (58.4%) of respondents were not married. About 75.6% of respondents reported their health as ‘good’ while few (1.9%) reported ‘bad’ health status. The average household size across all the district councils was 4.5 people (SD: 1.9; Table 3).
Table 3.
Demographic and socioeconomic characteristics of the respondents included in the analysis
| Variable | Kondoa (n = 79) | Kongwa (n = 24) | Dodoma city (n = 200) | Bahi (n = 65) | Mpwapwa (n = 129) | Chemba (n = 80) | Total (n = 577) |
|---|---|---|---|---|---|---|---|
| Gender of head of household, n (%) | |||||||
| Male | 45 (56.0) | 8 (33.3) | 123 (61.5) | 53 (81.5) | 93 (72.1) | 66 (82.5) | 396 (68.6) |
| Female | 34 (43.9) | 16 (66.7) | 77 (38.5) | 12 (18.5) | 36 (27.9) | 14 (17.5) | 181 (31.4) |
| Age categories of head of household | |||||||
| ≤25, n (%) | 0 (0.0) | 3 (12.5) | 13 (6.5) | 5 (7.7) | 5 (3.9) | 4 (5.0) | 30 (5.2) |
| 26–35, n (%) | 5 (6.3) | 3 (12.5) | 39 (19.5) | 14 (21.5) | 23 (17.8) | 15 (18.7) | 99 (17.2) |
| 36–45, n (%) | 17 (21.5) | 6 (25.0) | 47 (23.5) | 18 (27.7) | 40 (31.0) | 23 (28.7) | 151 (26.2) |
| 46–64, n (%) | 27 (34.2) | 12 (50.0) | 58 (29.0) | 21 (32.3) | 34 (26.4) | 29 (26.3) | 181 (31.4) |
| ≥65, n (%) | 30 (38.0) | 0 (0.0) | 43 (21.5) | 7 (10.8) | 27 (20.9) | 9 (11.3) | 116 (20.0) |
| Mean (years) (SD) | 60 (17.9) | 45 (10.4) | 49 (16.2) | 45 (14.0) | 48 (115.8) | 46 (13.3) | 49.6 (16.2) |
| Education level of head of household, n (%) | |||||||
| No education | 35 (44.3) | 5 (20.8) | 42 (21.0) | 24 (36.9) | 32 (24.8) | 12 (15.0) | 150 (26.0) |
| Primary up to grade five | 43 (54.4) | 18 (75.0) | 133 (66.5) | 41 (63.1) | 95 (73.6) | 64 (80.0) | 394 (68.3) |
| Secondary and above | 1 (1.3) | 1 (4.2) | 25 (12.5) | 0 (0.0) | 2 (1.6) | 4 (5.0) | 33 (5.7) |
| Occupation of head of household, n (%) | |||||||
| Formal employed | 0 (0.0) | 0 (0.0) | 7 (3.5) | 1 (1.5) | 3 (2.3) | 3 (3.7) | 14 (2.4) |
| Farmer | 39 (49.4) | 21 (87.5) | 39 (19.5) | 57 (87.7) | 73 (56.6) | 53 (66.3) | 282 (48.9) |
| Self-business | 8 (10.1) | 0 (0.0) | 94 (47.0) | 1 (1.5) | 27 (20.9) | 11 (13.7) | 141 (24.4) |
| Not employed | 32 (40.5) | 3 (12.5) | 60 (30.0) | 6 (9.2) | 26 (20.2) | 13 (16.3) | 140 (24.3) |
| Marital status, n (%) | |||||||
| Married | 57 (72.2) | 13 (54.2) | 74 (37.0) | 39 (60.0) | 43 (33.3) | 51 (63.7) | 240 (41.6) |
| Not married | 22 (27.8) | 11 (45.8) | 126 (63.0) | 26 (40.0) | 86 (66.7) | 29 (36.3) | 337 (58.4) |
| Health status of head of household, n (%) | |||||||
| Good | 53 (67.1) | 19 (79.2) | 143 (71.5) | 53 (81.5) | 105 (79.1) | 66 (82.5) | 436 (75.6) |
| Average | 25 (31.6) | 5 (20.8) | 50 (25.0) | 11 (16.9) | 25 (19.4) | 14 (17.5) | 130 (22.5) |
| Bad | 1 (1.3) | 0 (0.0) | 7 (3.5) | 1 (1.5) | 2 (1.5) | 0 (0.0) | 11 (1.9) |
| Number of people in the household | |||||||
| ≤2, n (%) | 17 (21.5) | 1 (4.2) | 33 (16.5) | 4 (6.2) | 17 (13.2) | 14 (17.5) | 86 (14.9) |
| 3–4, n (%) | 30 (38.0) | 6 (25.0) | 75 (37.5) | 18 (27.7) | 66 (51.2) | 30 (37.5) | 225 (38.9) |
| 5–6, n (%) | 23 (29.1) | 13 (54.2) | 55 (27.5) | 32 (49.2) | 31 (24.0) | 27 (33.7) | 181 (31.4) |
| ≥7, n (%) | 9 (11.4) | 4 (16.6) | 37 (18.5) | 11 (16.9) | 15 (11.6) | 9 (11.3) | 85 (14.7) |
| Average house hold size (SD) | 4.2 (1.8) | 5.0 (1.4) | 4.6 (2.0) | 5.0 (1.7) | 4.2 (1.7) | 4.4 (2.1) | 4.5 (1.9) |
| CHF insurance status, n (%) | |||||||
| CHF insured | 72 (91.1) | 9 (37.5) | 41 (20.5) | 8 (12.3) | 25 (19.4) | 2 (2.5) | 157 (27.2) |
| Not insured | 7 (8.9) | 15 (62.5) | 159 (79.5) | 57 (87.7) | 104 (80.6) | 78 (97.5) | 420 (72.8) |
| Social economic status (%), n (%) | |||||||
| S1 (poorest) | 35 (44.3) | 1 (4.2) | 48 (24.0) | 5 (7.7) | 24 (18.6) | 12 (15.0) | 125 (21.7) |
| S2 | 13 (16.5) | 7 (29.2) | 21 (10.5) | 25 (38.5) | 7 (5.4) | 22 (27.5) | 95 (16.5) |
| S3 | 10 (12.7) | 9 (37.5) | 30 (15.0) | 24 (36.9) | 44 (34.1) | 31 (38.7) | 148 (25.6) |
| S4 | 9 (11.4) | 5 (20.8) | 38 (19.0) | 7 (10.8) | 34 (26.4) | 8 (10.0) | 101 (17.5) |
| S5 (non-poor) | 12 (15.1) | 2 (8.3) | 63 (31.5) | 4 (6.2) | 20 (15.5) | 7 (8.8) | 108 (18.7) |
Household healthcare utilization
Among the households which were successfully linked with the health facility providing services in their region, 255 (44.2%) reported an illness episode of a household member in the last 3 months prior to the survey. The reported causes of illness were chest and related diseases (20.3%), malaria (18.0%) and typhoid and stomach-related diseases (12.9%). Out of 255 households, ∼7.8% reported a member with non-communicable diseases (NCDs—point prevalence) such as cancer, hypertension and diabetes (7.8%), fever (5.5%), illness related to eyes and ears (3.9%), urinary tract infection (3.1%), while the health problem could not be specified for 12.2% (Table 4).
Table 4.
Healthcare utilization
| Illness episode last 3 months | Kondoa (n = 79), n (%) | Kongwa (n = 24), n(%) | Dodoma city (n = 200), n (%) | Bahi (n = 65), n (%) | Mpwapwa (n = 129), n (%) | Chemba (n = 80), n (%) | Total (n = 577), n (%) |
|---|---|---|---|---|---|---|---|
| Household reported any illness case | 44 (55.7) | 10 (41.7) | 78 (39.0) | 33 (50.8) | 55 (42.6) | 35 (43.7) | 255 (44.2) |
| Type of Illness episode reported | |||||||
| Malaria | 10 (22.7) | 3 (30.0) | 9 (11.5) | 3 (9.1) | 12 (21.8) | 9 (25.7) | 46 (18.0) |
| Urinary tract infection | 1 (2.3) | 1 (10.0) | 3 (3.8) | 0 (0.0) | 1 (1.8) | 2 (5.7) | 8 (3.1) |
| Eyes and ears | 3 (6.8) | 0 (0.0) | 4 (5.1) | 1 (3.0) | 2 (3.6) | 0 (0.0) | 10 (3.9) |
| Fever | 5 (11.4) | 0 (0.0) | 3 (3.8) | 3 (9.1) | 1 (1.8) | 2 (5.7) | 14 (5.5) |
| Typhoid and stomach-related diseases | 6 (13.6) | 1 (10.0) | 14 (17.9) | 4 (12.1) | 2 (3.6) | 6 (17.1) | 33 (12.9) |
| Chest-related diseases | 13 (29.6) | 3 (30.0) | 12 (15.4) | 4 (12.1) | 10 (18.2) | 11 (31.4) | 53 (20.3) |
| Cancer, pressure and diabetes (NCDs) | 1 (2.3) | 0 (0.0) | 15 (19.2) | 0 (0.0) | 3 (5.5) | 1 (2.8) | 20 (7.8) |
| Others | 5 (11.4) | 2 (0.0) | 17 (21.8) | 2 (6.1) | 10 (18.2) | 4 (11.4) | 40 (15.7) |
| No information on the type of illness | 0 (0.0) | 0 (0.0) | 1 (1.3) | 16 (48.5) | 14 (25.5) | 0 (0.0) | 31 (12.2) |
| Household sought help | 36 (81.8) | 10 (100) | 70 (89.7) | 15 (45.5) | 37 (67.3) | 32 (91.4) | 200 (78.4) |
| Where did she/he go for treatment | |||||||
| Public dispensary or health centre | 30 (81.1) | 8 (80.0) | 16 (22.9) | 9 (60.0) | 22 (61.1) | 19 (59.4) | 104 (52.0) |
| Private doctor/clinic | 0 (0.0) | 0 (0.0) | 7 (10.0) | 0 (0.0) | 5 (13.9) | 0 (0.0) | 12 (6.0) |
| Public hospital | 2 (5.41) | 0 (0.0) | 20 (28.6) | 3 (20.0) | 5 (13.9) | 4 (12.5) | 34 (17.0) |
| NGO or trust hospital/clinic | 0 (0.0) | 0 (0.0) | 1 (1.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.5) |
| Private hospital | 0 (0.0) | 0 (0.0) | 10 (14.3) | 1 (6.7) | 0 (0.0) | 1 (3.1) | 12 (6.0) |
| Traditional healer | 0 (0.0) | 0 (0.0) | 1 (1.4) | 1 (6.7) | 3 (8.3) | 0 (0.0) | 5 (2.5) |
| Pharmacy/drugstore | 5 (13.5) | 2 (20.0) | 14 (20.0) | 1 (6.7) | 0 (0.0) | 6 (18.7) | 28 (14.0) |
| Home treatment | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Local doctor | 0 (0.0) | 0 (0.0) | 1 (1.4) | 0 (0.0) | 1 (2.8) | 2 (6.3) | 4 (2.0) |
| The reason that the sufferer not sought care | |||||||
| Ailment not considered serious | 1 (14.3) | 0 (0.0) | 0 (0.0) | 1 (5.6) | 1 (5.6) | 0 (0.0) | 3 (5.5) |
| Expected to become better without treatment | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (5.6) | 0 (0.0) | 1 (1.8) |
| No drugs available in the area | 1 (14.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (11.1) | 0 (0.0) | 3 (5.5) |
| Did not believe it would help | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Consultation and drugs too expensive | 0 (0.0) | 0 (0.0) | 3 (37.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3 (5.5) |
| Took self-treatment | 4 (57.1) | 0 (0.0) | 4 (50.0) | 1 (5.6) | 1 (5.6) | 3 (100) | 13 (23.6) |
| No reason given | 2 (14.3) | 0 (0.0) | 1 (12.5) | 16 (88.8) | 13 (72.2) | 0 (0.0) | 32 (58.2) |
NGO, Non-governmental organization.
Of the 255 who reported illness, 200 (78.4%) sought care from a healthcare provider. About 52.0% of them sought healthcare from public dispensary or health centre, whereas 17.0% from public hospital, 14.0% sought care from pharmacy/drugstore, 6.0% from private hospital, 6.0% sought care from private doctor/clinic, 2.0% sought care from local doctor and 2% sought care from traditional healer (Table 4).
The reasons given for not seeking care were the health problem was not considered serious (5.5%); no drugs were available in the area (5.5%); participant perceived that consultation and drugs were too expensive (5.5%); participant expected to recover without treatment (1.8%); individual had knowledge on how to deal with the health problem and took self-treatment (23.6); and the remaining 58.2% did not report a reason for not seeking care with illness (Table 4).
Multivariate logistic regression
The link test showed that the model was correctly specified (Supplementary Table S6). Table 5 presents a multivariate logistic regression analysis on the effects of medicine availability on the household’s healthcare utilization. Results show that households with self-reported good health status were two times [odds ratio (OR) 1.80, 95% confidence interval (CI) 1.06–3.05; P = 0.029] as likely to seek care from formal healthcare providers compared with respondents that reported bad health status. Households that had received health education interventions were >2.7 times as likely (OR 2.75, 95% CI 1.84–4.08; P = 0.000) to seek healthcare services as were those who had not received health education. Results on pairwise correlation matrix showed a positive and significant association between the healthcare utilization and with facilities without any stock-outs (0.197) together with less waiting time at the facility (0.136), while a negative association was observed with minutes taken to reach at the healthcare facility when accessing healthcare services (−0.040) (Supplementary Table S4). Regression results showed that households that reported <60 min of wait time during the previous healthcare facility visit were more likely to have sought care than those that waited >60 min (OR 2.02, 95% CI 0.75–5.44; P = 0.167). In addition, households that were member of a community health insurance fund (CHF) were two times as likely to seek care from a formal provider than those not registered (OR 1.97, 95% CI 1.23–3.17; P = 0.000).
Table 5.
Multivariate logistic regression on the effects of medicines availability and stock-outs healthcare utilization
| Variable, odds ratio (confidence interval) | Univariate analysis (255) |
Multivariate analysis (255) |
||
|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P-value | |
| Age of respondents | 0.998 (0.98–1.02) | 0.869 | 0.992 (0.97–1.01) | 0.441 |
| Household head being male | 1.185 (0.69–2.03) | 0.538 | 1.365 (0.43–4.25) | 0.591 |
| Household head being married | 0.629 (0.33–1.20) | 0.161 | 0.532 (0.24–1.15) | 0.107 |
| Household self-reported good health statusa | 1.737 (1.08–2.78) | 0.021 | 1.801 (1.06–3.05) | 0.029 |
| Household being a CHF membershipa | 2.212 (1.11–4.42) | 0.024 | 1.974 (1.23–3.17) | 0.005 |
| Level of trust to facility staffs being great | 1.359 (0.82–2.25) | 0.234 | 1.307 (0.76–2.24) | 0.338 |
| Household head received healthcare educationb | 1.912 (1.23–2.98) | 0.004 | 2.745 (1.84–4.08) | 0.000 |
| Waiting time at the health facility <60 min | 1.783 (0.85–3.74) | 0.126 | 2.015 (0.75–5.44) | 0.167 |
| Distance to the facility <5 km | 1.107 (0.56–2.19) | 0.769 | 1.624 (0.74–3.54) | 0.225 |
| Minutes to the closest facility | 0.998 (0.99–1.00) | 0.558 | ||
| Household with at least one person with chronic illness | 0.856 (0.60–1.22) | 0.397 | 0.872 (0.54–1.40) | 0.575 |
| Facilities without any stock-outs for the past 3 monthsa | 4.869 (1.75–20.18) | 0.029 | 3.496 (1.02–12.04) | 0.047 |
| Household size | 0.994 (0.89–1.11) | 0.909 | 0.986 (0.77–1.26) | 0.908 |
| Wealth index value (proxy of income) | 0.868 (0.76–0.99) | 0.043 | 0.908 (0.80–1.02) | 0.116 |
| Total number of staffs | 1.089 (0.79–1.49) | 0.596 | ||
| TASAF beneficiary | 1.856 (0.79–4.35) | 0.154 | 0.991 (0.50–1.95) | 0.978 |
| Waiver/exemption of any household member | 1.117 (0.56–2.21) | 0.751 | 1.056 (0.49–2.28) | 0.889 |
| Constant | 0.131 (0.03–0.59) | 0.010 | ||
| Number of observations | 251 | |||
| Wald chi2 (14) | 1596.77 | |||
| Prob > chi2 | 0.000 | |||
| Pseudo R2 | 0.1117 | |||
Significance at 5% level (corresponds to the multivariate results).
Significance at 1% level (corresponds to the multivariate results).
TASAF, Tanzania Social Action Fund.
Distance to the healthcare facility was found to influence the likelihood of seeking healthcare services: households residing <5 km from a facility were 1.6 times more likely to seek care than those residing >5 km from the healthcare facility though not statistically significant (OR 1.62, 95% CI 0.74–5.44; P = 0.225). Lastly, household healthcare utilization was positively and significantly associated with continuous availability of all essential medicines for the surveyed facilities (OR 3.49, 95% CI 1.02–12.04; P = 0.047).
Discussion
This study assessed medicine availability and stock-outs in public health facilities and examined the effects of medicines availability on healthcare utilization in six districts of Dodoma region in Tanzania. We found that the availability of most tracer medicines was relatively good, with continuous availability of ∼70% of the medicines assessed over a 3 months period, much higher compared with the findings in Malawi where overall availability of medicines in public facilities was <50% (Khuluza and Haefele-Abah, 2019). Frequent stock-outs (5/18) were found for a few medicines, such as amoxicillin syrup or cotrimoxazole suspension, paracetamol tabs and ferrous salt and folic acid. This trend varied across facility types and across the districts. Medicine stock-outs at facilities were frequently due to the failure of the health facility to plan for needed refills and to stock-outs at the central MSD.
Medicines such as paracetamol, ferrous salt and folic acid availability were low compared with the reported estimated in LMIC countries such as Nigeria (Sun et al., 2018), Malawi (Khuluza and Haefele-Abah, 2019) and Ethiopia (Sado and Sufa, 2016). The reported causes for regular stock-outs at health facility level were related to procurement inefficiencies, staff ability to forecast needs and requisitioning of medical commodities (Walker and Ozawa, 2011). Therefore, improvements in communication, forecasting and ordering procedures at healthcare facilities are necessary for addressing such inefficiencies (Soyiri and Reidpath, 2013).
We found that the majority of households reported having sought care from public healthcare facilities, similarly to the findings of other studies (Basu et al., 2012; Ngugi et al., 2017). This finding shows the importance of the public sector in the provision of healthcare services, especially for the marginalized population. Among the prerequisites for UHC include ensuring availability of high-quality medicines in the public facilities, rational prescribing, strengthening the community and peripheral health facility level (WHO, 2012). The results of these studies indicated that the continued availability of essential medicines at the facility may influence the use of public health facility services.
The association between distance from a health facility and the use of health services was not statistically significant. Other recent studies found that living in the proximity (<1 h walking time) of a health facility increases the probability of household healthcare utilization(Buor, 2002; Anselmi et al., 2015; Khuluza and Haefele-Abah, 2019), whereas in Vietnam those living <1 km were three times likely to utilize healthcare services compared with those residing >1 km from the facility (Tran et al., 2016).
Waiting time was found to influence healthcare utilization as reported in other settings (Afolabi et al., 2013; Sado and Sufa, 2016). In our analysis, we assessed waiting time as measured in terms of how long a client normally wait until s/he gets treatment contrary to that of Nigeria which was measured in terms of a four point’s Likert-scale (Afolabi et al., 2013) and Laos which participants rated long clinic waiting time as one of the barriers in seeking treatment at the facilities (Phrasisombath et al., 2012). Irrespective of the methodology used to assess the effect of waiting time on healthcare utilization, findings tend to be similar. In contrast, easy access, shorter waiting time and longer or flexible opening hours have been demonstrated to increase the use of formal healthcare services (Shaikh and Hatcher, 2005; Sado and Sufa, 2016).
We could not find an association between trust in healthcare providers and use of health services as it was found by other studies (Trachtenberg et al., 2005; Dawson-Rose et al., 2016). Trust in providers influences both healthcare-seeking, and influences patient engagement, participation in care and treatment adherence (Mkoka et al., 2014). A high level of trust between the client and the provider induces people to utilize healthcare services from a given facility (Russell, 2005). Trust is defined as the household’s perceived technical competence of the healthcare provider (face-to-face interaction) (Russell, 2005; Dawson-Rose et al., 2016) as well as inter-personal dimensions of quality of care (Russell, 2005). Stock-outs of medicines at the healthcare facility affects the quality of healthcare services which, in turn, undermine the trust which the population has in the health services influencing health-seeking behaviour (Mkoka et al., 2014).
We found an association between health education and healthcare utilization from the study area. As documented elsewhere, health education impacts household knowledge and willingness to seek healthcare services from formal healthcare providers (Oladipo, 2014; Jibril et al., 2017). Raising community awareness of health issues, illness prevention and encouragement of timely care-seeking, in turn, improve health outcomes.
Similar to the findings of other studies (Ahmed et al., 2018; Atnafu et al., 2018), we have found that CHF beneficiaries were more likely to seek healthcare in formal settings as compared with non-insured households. Financial protection is crucial in achieving UHC, implying the absence of (substantial) out-of-pocket payments when accessing healthcare services (Abiiro et al., 2014; Ataguba and Ingabire, 2016). Insured households are less likely to delay care-seeking, borrow or sell their valuable assets or incur income loss when accessing care (Abiiro et al., 2014). The government of Tanzania within its Health Sector Strategic Plan for 2015–2020 made commitments towards universal healthcare through social health insurance (URT, 2015). The health financing strategy includes the scale-up the coverage of redesigned CHFs (the so-called ‘CHF iliyoboreshwa’) with the aim of reaching all households. It is anticipated that the uptake of CHF iliyoboreshwa will improve household access to care as well as facility revenue. In turn, facilities could use the CHFs revenue, together with other cost-sharing mechanisms, to improve quality-of-care through procurement of medical commodities (medicines, medical equipment and medical supplies; Wiedenmayer et al., 2019).
The results presented here should be considered alongside a few important limitations. First, we were unable to link data from many of the households with facility level data. This might lead to potential selection bias if the households we were able to link are systematically different from households we were unable to link. It could also influence the generalizability of the findings across the region. In addition, our study focused specifically on facilities in the public sector although households may seek care and services from the private sector too. The study focused only on the availability of medicines, as medical supplies and equipment data were limited. Lastly, respondents provided responses based on their past experiences and it is possible that responses were subject to some recall errors.
Conclusion
This study showed that the availability of most tracer medicines was relatively good (compared with other studies in the region), although there were frequent stock-outs of a few medicines and wide variation across health facilities and district councils. Medicine availability was associated with higher use of healthcare services indicating it may play an important role in influencing household utilization of healthcare services in Tanzania. The results of this study highlight the importance of efficient co-ordination, planning and medicine supply management between the facility and the national supply chain. A better understanding of factors contributing to the performance of the Jazia PVS is crucial for improvement in medicines availability at the facilities. In addition, providers should consider the availability of healthcare services within a reasonable time as a way of shortening waiting time at the point of service. Moreover, healthcare providers should continue to provide healthcare education to the community in order to raise community awareness of relevant health issues and enhance knowledge in seeking timely and appropriate health assistance, along with community sensitization on the importance of health insurance in accessing healthcare services and avoiding health-related financial hardship.
Supplementary Material
Acknowledgements
We would like to acknowledge the assistance of the Health Promotion and Systems Strengthening (HPSS) team; Manfred Stoermer, Prof Manoris Meshack, Miss Fiona Chiluda, Vicky-Sidney Msamba and other team members. We would like to thank Dr Marina Antillon and Dr Gillian Levine, for their critical review of the paper as well as Mr Yeromin Mlacha for his support in generating the image for visualization of household and health facilities; District Executive Directors (DED), District Medical Officers (DMOs) and the facility in-charges from the sampled facilities in each of the districts for their support during the study. We also acknowledge Swiss Programme for Research on Global Issues for Development (r4d); Swiss Agency for Development and Cooperation (SDC); Swiss National Science Foundation (SNF) for funding the study. This manuscript is an output from the project: Health systems governance for an inclusive and sustainable social health protection in Ghana and Tanzania funded by the Swiss Programme for Research on Global Issues for Development (r4d programme). The project involved a consortium of five partners: Swiss Tropical and Public Health Institute, ETH Zurich, University of Applied Sciences and Arts of Southern Switzerland (SUPSI), Ifakara Health Institute Tanzania, University of Ghana.
Availability of data and material
The dataset(s) supporting the conclusions of this article is owned by Health Promotion and System Strengthening (HPSS) project and available upon request.
Conflict of interest statement. None declared.
Ethical approval. Ethical clearance for this study was obtained from the Ifakara Health Institute Institutional Review Board (IHI/IRB/No. 21-2017) and the Tanzanian National Institute for Medical Research (NIMR/HQ/R.8a/Vol. IX/2720). District managers and health facility in-charges were informed about the study and written informed consent was obtained from household heads or his/her representatives as long as participant was aged 18 years and above.
Exchange rate
1 US$= 2137 TZS
References
- Abiiro GA, Mbera GB, DE Allegri M.. 2014. Gaps in universal health coverage in Malawi: a qualitative study in rural communities. BMC Health Services Research 14: 234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Afolabi MO, Daropale VO, Irinoye AI, Adegoke AA.. 2013. Health-seeking behaviour and student perception of health care services in a university community in Nigeria. Health 5: 817–24. [Google Scholar]
- Ahmed S, Sarker AR, Sultana M. et al. 2018. The impact of community-based health insurance on the utilization of medically trained healthcare providers among informal workers in Bangladesh. PLoS One 13: e0200265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Mandhary A, Al-Zakwani I, Afifi M.. 2007. Primary health care consumers’ acceptance, trust and gender preferences towards Omani doctors. Oman Medical Journal 22: 51–6. [PMC free article] [PubMed] [Google Scholar]
- Anselmi L, Lagarde M, Hanson K.. 2015. Health service availability and health seeking behaviour in resource poor settings: evidence from Mozambique. Health Economics Review 5: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ataguba JE, Ingabire MG.. 2016. Universal health coverage: assessing service coverage and financial protection for all. American Journal of Public Health 106: 1780–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atnafu DD, Tilahun H, Alemu YM.. 2018. Community-based health insurance and healthcare service utilisation, North-West. BMJ Open 8: e019613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu S, Andrews J, Kishore S, Panjabi R, Stuckler D.. 2012. Comparative performance of private and public healthcare systems in low- and middle-income countries: a systematic review. PLoS Medicine 9: e1001244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bigdeli M, Laing R, Tomson G, Babar ZU.. 2015. Medicines and universal health coverage: challenges and opportunities. Journal of Pharmaceutical Policy and Practice 8: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan N, Barnes R, Calnan M. et al. 2013. Trust in the health-care provider–patient relationship: a systematic mapping review of the evidence base. International Journal for Quality in Health Care 25: 682–8. [DOI] [PubMed] [Google Scholar]
- Buor D. 2002. Distance as a predominant factor in the utilisation of health services in the Kumasi metropolis. GeoJournal 56: 145–57. [Google Scholar]
- Cameron A, Ewen M, Ross-Degnan D, Ball D, Laing R.. 2009. Medicine prices, availability, and affordability in 36 developing and middle-income countries: a secondary analysis. The Lancet 373: 240–9. [DOI] [PubMed] [Google Scholar]
- Cameron C, Miller D.. 2015. A practitioner’s guide to cluster-robust inference. Journal of Human Resources 50: 317–72. [Google Scholar]
- Chen C-C, Blank RH, Cheng S-H.. 2014. Medication supply, healthcare outcomes and healthcare expenses: longitudinal analyses of patients with type 2 diabetes and hypertension. Health Policy 117: 374–81. [DOI] [PubMed] [Google Scholar]
- Chomi EN, Mujinja PGM, Enemark U, Hansen K, Kiwara AD.. 2014. Health care seeking behaviour and utilisation in a multiple health insurance system: does insurance affiliation matter? International Journal for Equity in Health 13: 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran WG. 1977. Sampling Techniques, 3rd edn New York: John Wiley & Sons. [Google Scholar]
- Dawson-Rose C, Cuca YP, Webel AR. et al. 2016. Building trust and relationships between patients and providers: an essential complement to health literacy in HIV care. Journal of the Association of Nurses in Aids Care 27: 574–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Embrey M, Vialle-Valentin C, Dillip A. et al. 2016. Understanding the role of accredited drug dispensing outlets in Tanzania’s health system. PLoS One 11: e0164332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feikin DR, Nguyen LM, Adazu K. et al. 2009. The impact of distance of residence from a peripheral health facility on pediatric health utilisation in rural western Kenya. Tropical Medicine & International Health 14: 54–61. [DOI] [PubMed] [Google Scholar]
- Fenny AP, Yates R, Thompson R.. 2018. Social health insurance schemes in Africa leave out the poor. International Health 10: 1–3. [DOI] [PubMed] [Google Scholar]
- HPSS. 2011. News and Announcements Launch of a New Regional Prime Vendor System for Supplementary Medicines and Supplies in Dodoma Region [Online] http://www.hpss.or.tz/index.php/66-news/318-launch-of-a-new-regional-prime-vendor-system-for-supplementary-medicines-and-supplies-in-dodoma-region, accessed 30 November 2016.
- HPSS. 2014. Complementing the Medicines Supply Gap with a Regional Prime Vendor System in Dodoma Region. Dodoma: Swiss TPH. [Google Scholar]
- Jia LL, Lou XY, Guo Y, Leung KS, Zeng EY.. 2016. Occurrence of phthalate esters in over-the-counter medicines from China and its implications for human exposure. Environment International 98:137–42. [DOI] [PubMed] [Google Scholar]
- Jibril U, Saleh G, Lafolayan J. et al. 2017. Impact of health education intervention on knowledge and utilization of postnatal care services among women in Edu Local Government of Kwara State, Nigeria. Journal of Basic and Clinical Reproductive Sciences 6. doi: 10.4103/2278-960X.194496. [Google Scholar]
- Kante AM, Gutierrez HR, Larsen AM. et al. 2015. Childhood illness prevalence and health seeking behavior patterns in rural Tanzania. BMC Public Health 15: 951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapologwe NA, Kalolo A, Kibusi SM. et al. 2019. Understanding the implementation of Direct Health Facility Financing and its effect on health system performance in Tanzania: a non-controlled before and after mixed method study protocol. Health Research Policy and Systems 17: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khuluza F, Haefele-Abah C.. 2019. The availability, prices and affordability of essential medicines in Malawi: a cross-sectional study. PLoS One 14: e0212125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kusemererwa D, Alban A, Obua OT, Trap B.. 2016. An exploratory study on equity in funding allocation for essential medicines and health supplies in Uganda’s public sector. BMC Health Services Research 16: 453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kusi A, Hansen KS, Asante FA, Enemark U.. 2015. Does the National Health Insurance Scheme provide financial protection to households in Ghana? BMC Health Services Research 15: 331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long S, Freese J.. 2006. Regression Models for Categorical Dependent Variables Using Stata, 2nd edn Thousand Oaks, California: Stata Press. [Google Scholar]
- Lu Y, Hernandez P, Abegunde D, Edejer T.. 2011. Medicine expenditures In: The World Medicines Situation 2011. Geneva: World Health Organization; http://apps.who.int/medicinedocs/documents/s18767en/s18767en.pdf, accessed 5 October 2016. [Google Scholar]
- Luiza VL, Tavares NUL, Oliveira MA. et al. 2016. Catastrophic expenditure on medicines in Brazil. Revista de Saúde Pública 50: 15s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masters SH, Burstein R, Decenso B. et al. 2014. Pharmaceutical availability across levels of care: evidence from facility surveys in Ghana, Kenya, and Uganda. PLoS One 9: e114762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcintyre D, Ranson MK, Aulakh BK, Honda A.. 2013. Promoting universal financial protection: evidence from seven low- and middle-income countries on factors facilitating or hindering progress. Health Research Policy and Systems 11: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikkelsen-Lopez I, Tediosi F, Abdallah G. et al. 2013. Beyond antimalarial stock-outs: implications of health provider compliance on out-of-pocket expenditure during care-seeking for fever in South East Tanzania. BMC Health Services Research 13: 444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mkoka DA, Goicolea I, Kiwara A, Mwangu M, Hurtig A-K.. 2014. Availability of drugs and medical supplies for emergency obstetric care: experience of health facility managers in a rural District of Tanzania. BMC Pregnancy and Childbirth 14: 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mlunde LB, Sunguya BF, Mbwambo JK. et al. 2016. Correlates of health care seeking behaviour among people who inject drugs in Dar es Salaam, Tanzania. International Journal of Drug Policy 30: 66–73. [DOI] [PubMed] [Google Scholar]
- Mtei G, Mulligan J, Palmer N. et al. 2007. An assessment of the health financing system in Tanzania: implications for equity and social health insurance: report on shield work package 1. iHEA 2007 6th World Congress: Explorations in Health Economics Paper Available at SSRN: https://ssrn.com/abstract=993421, accessed 21 December 2019.
- Mushi DP. 2014. Impact of cost sharing on utilization of primary health care services: providers versus household perspectives. Malawi Medical Journal 26: 83–9. [PMC free article] [PubMed] [Google Scholar]
- Musoke D, Boynton P, Butler C, Musoke MB.. 2014. Health seeking behaviour and challenges in utilising health facilities in Wakiso district, Uganda. African Health Sciences 14: 1046–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mwabu G, Ainsworth M, Nyamete A.. 1993. Quality of medical care and choice of medical treatment in Kenya: an empirical analysis. The Journal of Human Resources 28: 838–62. [Google Scholar]
- Ngugi AK, Agoi F, Mahoney MR. et al. 2017. Utilization of health services in a resource-limited rural area in Kenya: prevalence and associated household-level factors. PLoS One 12: e0172728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nnko S, Bukenya D, Kavishe BB. et al. 2015. Chronic diseases in north-west Tanzania and southern Uganda. Public perceptions of terminologies, aetiologies, symptoms and preferred management. PLoS One 10: e0142194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obare V, Brolan CE, Hill PS.. 2014. Indicators for universal health coverage: can Kenya comply with the proposed post-2015 monitoring recommendations? International Journal for Equity in Health 13: 123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oladipo JA. 2014. Utilization of health care services in rural and urban areas: a determinant. factor in planning and managing health care delivery systems. African Health Sciences 14: 322–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phrasisombath K, Thomsen S, Sychareun V, Faxelid E.. 2012. Care seeking behaviour and barriers to accessing services for sexually transmitted infections among female sex workers in Laos: a cross-sectional study. BMC Health Services Research 12: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prinja S, Bahuguna P, Tripathy JP, Kumar R.. 2015. Availability of medicines in public sector health facilities of two North Indian States. BMC Pharmacology and Toxicology 16: 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell S. 2005. Treatment-seeking behaviour in urban Sri Lanka: trusting the state, trusting private providers. Social Science & Medicine (1982) 61: 1396–407. [DOI] [PubMed] [Google Scholar]
- Rutta E, Liana J, Embrey M. et al. 2015. Accrediting retail drug shops to strengthen Tanzania’s public health system: an ADDO case study. Journal of Pharmaceutical Policy and Practice 8: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sado E, Sufa A.. 2016. Availability and affordability of essential medicines for children in the Western part of Ethiopia: implication for access. BMC Pediatrics 16: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saksena P, Antunes AF, Xu K, Musango L, Carrin G.. 2011. Mutual health insurance in Rwanda: evidence on access to care and financial risk protection. Health Policy 99: 203–9. [DOI] [PubMed] [Google Scholar]
- Senkoro M, Hinderaker SG, Mfinanga SG. et al. 2015. Health care-seeking behaviour among people with cough in Tanzania: findings from a tuberculosis prevalence survey. The International Journal of Tuberculosis and Lung Disease 19: 640–6. [DOI] [PubMed] [Google Scholar]
- Shaikh BT, Hatcher J.. 2005. Health seeking behaviour and health service utilization in Pakistan: challenging the policy makers. Journal of Public Health 27: 49–54. [DOI] [PubMed] [Google Scholar]
- Shan L, LI Y, Ding D, Wu. et al. 2016. Patient satisfaction with hospital inpatient care: effects of trust, medical insurance and perceived quality of care. PLoS One 11: e0164366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soyiri IN, Reidpath DD.. 2013. An overview of health forecasting. Environmental Health and Preventive Medicine 18: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spaan E, Mathijssen J, Tromp N. et al. 2012. The impact of health insurance in Africa and Asia: a systematic review. Bulletin of the World Health Organization 2012. 90: 685–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun X, Wei J, Yao Y. et al. 2018. Availability, prices and affordability of essential medicines for children: a cross-sectional survey in Jiangsu Province, China. BMJ Open 8: e023646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trachtenberg F, Dugan E, Hall MA.. 2005. How patients’ trust relates to their involvement in medical care. The Journal of Family Practice 54: 344–52. [PubMed] [Google Scholar]
- Tran BX, Nguyen LH, Nong VM, Nguyen CT.. 2016. Health status and health service utilization in remote and mountainous areas in Vietnam. Health and Quality of Life Outcomes 14: 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- URT. 2015. United Republic of Tanzania Ministry of Health and Social Welfare: Health Sector Strategic Plan July 2015–June 2020 (HSSP IV): Reaching all Households with Quality Health Care. Dar es Salaam, Tanzania: Ministry of Health and Social Welfare.
- USAID. 2016. Supply Chain Management System; USAID | DELIVER PROJECT, Task Order 4; USAID | DELIVER PROJECT Task Order 7. 2016. Health Logistics in Tanzania: Timeline of Accomplishments for Supply Chain Interventions. Arlington, VA: Supply Chain Management System; USAID | DELIVER PROJECT, Task Order 4; USAID | DELIVER PROJECT, Task Order 7.
- Vyas S, Kumaranayake L.. 2006. Constructing socio-economic status indices: how to use principal components analysis. Health Policy and Planning 21: 459–68. [DOI] [PubMed] [Google Scholar]
- Walker DG, Ozawa S.. 2011. Comparison of trust in public vs private health care providers in rural Cambodia. Health Policy and Planning 26: i20–9. [DOI] [PubMed] [Google Scholar]
- WHO. 2000. WHO Medicines Strategy: Framework for Action in Essential Drugs and Medicines Policy 2000–2003. Geneva, Switzerland: World Health Organization; http://apps.who.int/medicinedocs/en/d/Jwhozip16e/, accessed November 2018. [Google Scholar]
- WHO. 2012. Universal Health Coverage: Primary Health Care towards Universal Health Coverage Report by the Director-General; EB144/12, 144th Session, Provisional Agenda Item 5.5. Geneva, Switzerland. https://apps.who.int/gb/ebwha/pdf_files/EB144/B144_12-en.pdf, accessed 6 November 2018.
- WHO. 2014. World Health Statistics 2014. Geneva: WHO. [Google Scholar]
- Wiedenmayer K, Mbwasi R, Mfuko W. et al. 2019. Jazia prime vendor system—a public-private partnership to improve medicine availability in Tanzania: from pilot to scale. Journal of Pharmaceutical Policy and Practice 12: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- YALE. 2011. The Medical Stores Department: AN Innovative Public-Private Partnership: Medical Supply Solutions in Tanzania [Online]. Yale Global Health Leadership Institute. http://nexus.som.yale.edu/ph-tanzania/?q=node/111, accessed 6 November 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset(s) supporting the conclusions of this article is owned by Health Promotion and System Strengthening (HPSS) project and available upon request.
Conflict of interest statement. None declared.
Ethical approval. Ethical clearance for this study was obtained from the Ifakara Health Institute Institutional Review Board (IHI/IRB/No. 21-2017) and the Tanzanian National Institute for Medical Research (NIMR/HQ/R.8a/Vol. IX/2720). District managers and health facility in-charges were informed about the study and written informed consent was obtained from household heads or his/her representatives as long as participant was aged 18 years and above.