Abstract
The underutilization of primary care in urban China threatens the efficiency and effectiveness of the Chinese health system. To guide patient flow to primary care, the Chinese government has rolled out a sequence of health care reforms which improve the affordability, the infrastructure and workforce of the primary care system. However, these measures have not yielded the desired effect on the utilization of primary care, which is lowest in urban areas. It is unclear how the factors identified to influence facility choice in urban China are actually impacting choice behaviour. We conducted a discrete choice experiment to elicit the quantitative impact of facility attributes when choosing a health care facility for first visit and analysed how the stated choice varies with these attributes. We found that the respondents placed different weights on the identified attributes, depending on whether they perceived their condition to be minor or severe. For conditions perceived as minor, the respondents valued visit time, equipment and medical skill most. For conditions perceived as severe, they placed most importance on equipment, travel time and facility size. We found that for conditions perceived as minor, only 14% preferred visiting a facility over opting out, a percentage which would more than double to 37% if community health centres were maximally improved. For conditions perceived as severe, improvements in community health centres may almost double first visits to primary care, mostly from patients who would otherwise choose higher-level facilities. Our findings suggest that for both severity conditions, improvements to medical equipment and medical skill at community health centres in urban China can effectively direct patient flow to primary care and promote the efficiency and effectiveness of the urban health system.
Keywords: Health care seeking behaviour, health care utilization, priority setting, health systems, hospitals, decision-making
Key Messages
Residents placed different weights on hospital characteristics depending on whether they perceived their disease conditions to be minor or severe.
For primary care hospitals, short visit time and lower out-of-pocket are the most attractive characteristics for conditions perceived as minor and severe, respectively.
Latent demand for health care converted to visits at primary care hospitals if they were improved.
Improvements on medical equipment and medical skill at primary care hospitals can effectively direct patient flow to primary care and promote the efficiency and effectiveness of the Chinese health system
Introduction
The Chinese health care system contains three levels. Patients may directly access health care facilities at all these levels (National Health Commission, 2011; Eggleston, 2012). In urban China, level-one health care facilities are known as community health centres (CHCs). As the core of the urban primary care system, CHCs provide primary care and public health services, as well as technical support to their branch facilities (Ministry of Health, 2006; The State Council, 2006). Urban patients often have easy access to secondary and tertiary hospitals as they are typically located in urban areas (Chen et al., 2014; Cai et al., 2018a). They tend to bypass primary care and choose these higher-level facilities regardless of disease severity (Yip and Hsiao, 2014; Wu and Lam, 2016; Li et al., 2017). Follow-up visits to primary care facilities after the first visit to higher-level facilities are uncommon (Liu et al., 2018c). Altogether, this leads to underutilization of primary care and congestion in secondary and tertiary hospitals, threatening the efficiency and effectiveness of the Chinese health system (Zhang et al., 2017). The situation may further worsen, as rapid urbanization and talent flow towards metropolitan cities increase the size of the urban population and corresponding demand for health care (Miao and Wu, 2016; Gu et al., 2019). Between 2007 and 2017, the population of Shanghai increased from 20.6 to 24.2 million and the number of consultations in the health care system per year increased from 132.2 to 273.4 million (Shanghai Bureau of Statistics, 2008, 2018).
To address these challenges, it is important for policymakers to understand the factors influencing urban patients’ facility choice, particularly their relative importance. A systematic literature review reported a considerable body of studies that have identified factors influencing facility choice in China (Liu et al., 2018b). They can be categorized as individual, facility, context and composite factors. The literature also reports that these factors vary with the patient-perceived severity of their condition (Wu et al., 2017; Liu et al., 2018c). Moreover, urban patients often revert to self-care (such as purchasing self-prescribed medicine from pharmacies or forms of self-treatment at home) or take no action instead of visiting a facility (Li et al., 2012; Liu et al., 2018c). While a variety of factors has been identified, the literature does not provide rigorous quantitative evidence on the importance attached to these factors by urban residents. To the best of our knowledge, the only study reporting on the quantitative impact of the factors influencing health care facility choice is from rural China (Liu et al., 2019). However, the factors considered differ considerably between rural and urban residents (Liu et al. 2018c). For example, rural residents considered drug availability as an important factor for first visit, whereas urban residents did not. To advance understanding of the importance of factors influencing facility choice, this study firstly aims to understand how the urban residents evaluate facility attributes for first visit under different perceived disease severities.
As the initial point of contact with the health care system, primary care should be located close to where people live and work and be able to address main health problems in the community (Primary Health Care: Declaration of Alma-Ata, 1978). A strong primary care system can improve population health and health care affordability (Starfield et al., 2005; Kringos et al., 2013; Hansen et al., 2015). In China, the recent health reforms in 2009 and 2015 have prioritized strengthening the primary care system, with the objective of diverting patient flow to primary care facilities (The State Council, 2015; Liu et al., 2017). Specifically, the percentage of patients who choose primary care facilities for the first visit is targeted to reach at least 70% (The State Council, 2015). From 2007 to 2017, subsidies to primary care system have increased from 19 to 181 billion RMB to improve the infrastructure and workforce (Li et al., 2017; Ministry of Finance, 2018). In addition, funding targeted for educating and training general practitioners in the primary care system has been made available (Ministry of Finance, 2018). Notably, substantial efforts have been made to improve demand-side incentives, such as a higher reimbursement rate at the primary level and the establishment of the essential medicine system (Li et al., 2017; Ministry of Finance, 2018).
These measures have shown limited effects (Li et al., 2017). Primary care visits by the urban population have not increased significantly (National Health Commission, 2017) and the outpatients who could have been serviced appropriately in primary care still tend to choose higher-level facilities (Yip et al., 2012; Wu and Lam, 2016; Liu et al., 2018a). Therefore, our second aim in this study is to understand how facility choice is affected by policy interventions to modify facility attributes under different perceived disease severities, taking the options ‘self-care’ or ‘no action’ into account.
To address these research aims, we conducted a discrete choice experiment (DCE) among the general population of a district in Shanghai.
Methods
This section described the selection of attributes, data collection and the analysis of the DCE. For an important part, it follows the methods of a related study conducted in rural China (Liu et al., 2019). This study received ethical approval from Medical Ethical Review Committee of the author’s institute [No. 2017 KY207].
Selection of attributes and DCE design
The DCE attributes and levels were selected based on the outcomes of a systematic literature review (Liu et al., 2018b) and subsequent qualitative research conducted for this purpose (Liu et al., 2018c). Seven facility attributes have been identified to influence health care facility choices of urban residents. In addition, the perceived disease severity played an important role in the choice process (Liu et al., 2018c). Table 1 shows the seven attributes, the corresponding levels and a description of the perceived severity scenarios included in the DCE.
Table 1.
DCE attributes and attribute levels
| Scenario variable | Level |
|---|---|
| Perceived disease severity (hypothesized) | Minor (description in the choice sets: imagine you have a mild symptom, such as catching a cold, coughing, sore throat …) |
| Severea (description in the choice sets: imagine you have a situation with a health problem, which makes feel worry and anxious …) | |
|
| |
| Attribute | Level |
|
| |
| Time taken for a visit (h)b | 5c |
| 3 | |
| 1 | |
| Out-of-pocket expense for visit (RMB) | 105c |
| 88 | |
| 59 | |
| Medical professionals’ skill | Mostly junior doctorsc |
| Many senior doctors; not much experts | |
| Experts are available | |
| Personal connection in the hospital | Know nobody in personc |
| Know somebody but is not very familiar | |
| Direct personal connection | |
| Medical equipment condition | Obsoletec |
| Advanced | |
| Travel time from home to hospital (min) | 90c |
| 40 | |
| 15 | |
| Hospital size | Smallc |
| Medium | |
| Large | |
No specific symptom or disease was described for a hypothesized severe condition, as the taboo of mentioning disease in Chinese culture may decrease the respondents’ motivation to participate in the survey.
Total time to finish one visit calculated from the moment the patient steps into the hospital until the end of all procedures related to the visit.
Reference levels.
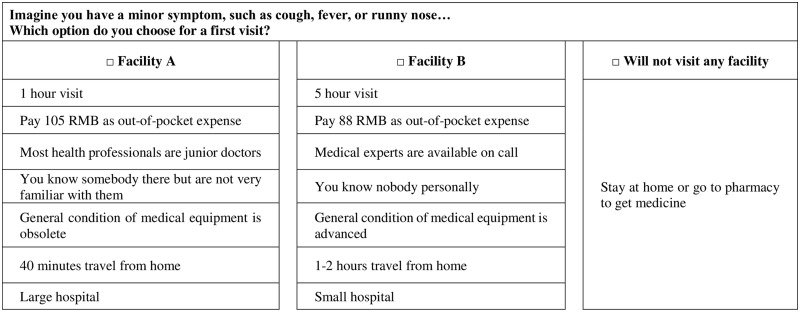
Using Ngene software (ChoiceMetrics, version 1.1.1), we generated a subset of the full Bayesian D-efficient design that includes 36 choice sets. Each choice set included two unlabelled facility alternatives and an opt-out option (Louviere and Lancsar, 2009; Veldwijk et al., 2014; see Figure 1 for an example of the choice set). A hypothesized disease severity was attributed to each choice set generated by the two-way interaction function in Ngene, which was consistent across all alternatives in each choice set. These 36 choice sets were divided into three blocks, thus each version of questionnaire included 12 choice sets. These three versions of questionnaires were evenly distributed among the respondents (Johnson et al., 2013); therefore, each respondent was asked to answer 12 choice questions. In each questionnaire, we grouped the choice questions by the two hypothesized severity scenarios. In the beginning of each group of questions, there was a short description of the severity scenario. The respondents were asked to answer each choice question based on its specified severity scenario as shown in Table 1. Respondent data on individual characteristics influencing facility choices were also collected as shown in Table 2 (Liu et al., 2018b, c). The questionnaire was piloted (N = 48) and revised to reach the final version. No signs of fatigue regarding the choice questions were noticed in the pilot study.
Figure 1.
Example of choice set (translated into English from the original Chinese version).
Table 2.
Respondents’ characteristics (n = 532)
| Characteristics | Percentage |
|---|---|
| Gender | |
| Female | 48% (pre-defined quota: 50%) |
| Male | 52% (pre-defined quota: 50%) |
| Age | |
| 18–45 years | 46% (pre-defined quota: 55%) |
| 45+ years | 54% (pre-defined quota: 45%) |
| Education | |
| Primary level or below | 1% |
| Middle or high school | 56% |
| College or above | 43% |
| Marriage | |
| Married | 85% |
| Not married | 15% |
| Employment status | |
| Not employed | 40% |
| Employed | 60% |
| Have children | |
| No | 19% |
| Yes | 81% |
| Number of family member living together | |
| 1–2 | 32% |
| ≥3 | 68% |
| Family annual income | |
| <110 000 | 56% |
| ≥110 000 | 44% |
| Insurance type | |
| UEBMI | 65% |
| URRBMI | 34% |
| No insurance | 1% |
| Hospital visiting experience | |
| Only primary | 20% |
| Only higher level | 12% |
| Both | 68% |
| Self-rated health | |
| Worse than average | 15% |
| Average | 60% |
| Better than average | 25% |
Data collection
Following the sample size calculation methods presented in de Bekker-Grob et al. (2015), we targeted a sample of 500 respondents aged 18 years and older. Pre-defined sample quota on gender and age were used to ensure sample representativeness (National Bureau of Statistics, 2017) as shown in Table 2. The respondent recruitment was supported by a local residence bureau, which assigned study co-ordinators from three residential committees. The study co-ordinators screened the residential databases to find eligible respondents. They contacted the eligible respondents in advance by phone calls to check their availability to complete the questionnaire. Before data collection, two authors (Y.L. and S.W.) trained the study co-ordinators to administer the questionnaires. Door-to-door surveys were conducted to collect data using pencil and paper from January to March 2018. Respondent recruitment continued until the predetermined sample size was met. In total, we approached 535 respondents and the sample characteristics were similar to the pre-defined quota as shown in Table 2. Of these, three respondents did not answer any choice question. Of the remaining 532 respondents who answered at least one choice question, 13 (2.4%) respondents missed at least one question. We included the data from all 532 respondents in the final analysis to ensure we obtained the response data as much as possible. Each respondent was compensated with a small monetary token (15 RMB).
Data analysis
Statistical analysis
Data analysis was conducted with Stata 15 software (StataCorp, 2017). We defined interaction terms between the main attributes and the disease severity. Effect coding was used for each of the attributes and the opt-out and interaction terms were dummy-coded (Bech and Gyrd-Hansen, 2005). We used a mixed logit model to estimate the impact of the main attributes and the interaction terms (McFadden and Train, 2000; Clark et al., 2014; Hauber et al., 2016). We tested different strategies to model the coefficients as fixed or random parameters. Based on the results, the model with the minimum Akaike Information Criterion was selected (Liu et al., 2019). It is worth noting that the coefficients of cost were modelled as fixed parameters to avoid a positive coefficient for cost (Bliemer and Rose, 2013). Normal distributions were used for the attributes modelled as random parameters. The results of this model provide information corresponding to our first research aim on the valuation of facility attributes.
For each effect-coded attribute, the level supposed to carry the lowest utility was specified as the reference level and was omitted in coding. The coefficient of this omitted level can be calculated as the negative sum of the coefficients of the non-omitted levels (Hauber et al., 2016). Relative importance of each attribute was calculated by the difference between the lowest and highest coefficient of that attribute, divided by the sum of this difference of all attributes (Lancsar et al., 2007).
We also tested the interaction between the attributes and the respondent characteristics by building different models for the minor and severe disease scenarios. The respondent characteristics were binary-coded and interacted with the main attributes (Supplementary Appendix SA1). The interaction terms were treated as fixed effect parameters, whereas the main attributes were coded as random effects except for the cost.
Predicted probabilities of health care facility choice
In DCEs, changes in predicted choice probability of an alternative reflect the impact of attribute modifications on the alternative (Lancsar et al., 2007; de Bekker-Grob et al., 2018). Thus, we calculated the predicted choice probabilities to address the second research aim of this study and estimated the following probabilities:
(1) The predicted probabilities of choosing any facility vs opting out, depending on facility attributes at the worst, average and best-case scenarios.
We calculated this choice probability by taking the exponent of the total utility of facility options, divided by the total utility of the available options including the opt-out. In each severity scenario, we defined an ‘average facility’ as one whose attributes are all at average levels (zero-utility levels); a ‘worst facility’ or a ‘best facility’ when all attributes are at the levels of the lowest or the highest utilities, respectively. These hypothesized facilities at the worst and best-case scenarios are characterized by the attribute levels in Table 3.
Table 3.
Attributes of the hypothesized facilities in the worst case and the best case in calculating the predicted probabilities of choosing any facility vs opting out
| Minor disease condition | Severe disease condition | |
|---|---|---|
| Worst-case facility |
|
|
| Best-case facility |
|
|
The attribute levels that are significant in each scenario.
(2) The probabilities of choosing a hypothesized CHC vs a higher-level facility (a hypothetical secondary or tertiary hospital), depending on the CHC at the worst-case, average and best-case scenarios.
We calculated this choice probability by taking the exponent of the utility of a CHC, divided by the total utility of the available options including the opt-out. For the hypothetical hospitals, we fixed all attributes at their ‘typical’ values (Liu et al., 2018c). As health care resources are relatively abundant in Shanghai, many patients can reach different levels of facilities within a relatively short distance. Therefore, the travel time to all facilities was fixed at 15 min. To quantify the effects of CHC attributes on the CHC choice probability, we firstly varied the attributes one at a time (i.e. one-way impact). In addition, we considered the worst case, resp. best-case CHC by simultaneously taking all attributes at the lowest, resp. highest utility level in each severity scenario, while keeping ‘small-sized’ and ‘travel time 15 min’ unchanged. The hypothetical ‘typical’ facilities and the hypothesized CHC at the worst case and the best case can be found in Table 4.
Table 4.
Attributes of the hypothetical ‘typical’ facilities and the hypothesized CHC at the worst case and the best case for calculating the probabilities of choosing a hypothesized CHC vs a higher-level hospital
| Hypothesized facility | Minor disease condition | Severe disease condition |
|---|---|---|
| CHC at the worst scenario | ||
| CHC at the best scenario | ||
| Typical CHC | Small-sized, 1-h visit time, OOP expense 59 RMB, mostly junior doctors, direct personal connection, obsolete equipment, travel time 15 min | |
| Typical secondary hospital | Mid-sized, 3-h visit time, OOP expense 88 RMB, many senior doctors, know nobody in person, medium-level equipment, travel time 15 min | |
| Typical tertiary hospital | Large-sized, 5-h visit time, OOP expense 105 RMB, experts are available, knows nobody personally, advanced equipment, travel time 15 min | |
The attribute levels that are significant in each scenario.
OOP, out-of-pocket; CHC, community health centre.
Results
DCE results
Table 5 presents the DCE results. The statistical significance level indicates whether the respondents considered the attribute important or not when making choices. The sign of a coefficient indicates whether the attribute had a positive or negative effect on utility. The interaction terms represent the change in utility resulting from changing perceived severity from minor to severe. The results of the interaction effects between the main attributes and the respondent characteristics can be found in Supplementary Appendix SA2.
Table 5.
Model estimates
| Attribute | Attribute level | Minor condition coefficient (95% CI) | Severe condition coefficient (95% CI) | ||
|---|---|---|---|---|---|
| Time taken for a visit (h) | 5 (ref) | −0.425*** | (−0.585, −0.266) | −0.103 | (−0.223, 0.017) |
| 3 | −0.077 | (−0.057. 0.201) | 0.096** | (0.001, 0.191) | |
| 1 | 0.502*** | (0.344. 0.659) | 0.007 | (−0.118, 0.131) | |
| OOP for visit (RMB) | 105 (ref) | −0.196*** | (−0.314, −0.077) | −0.102*** | (−0.188, −0.015) |
| 88 | 0.072 | (−0.057. 0.201) | −0.036 | (−0.152, 0.079) | |
| 59 | 0.124 | (−0.011. 0.259) | 0.138** | (0.029, 0.247) | |
| Medical professionals’ skill | Junior doctors (ref) | −0.277*** | (−0.400, −0.154) | −0.050 | (−0.155, 0.055) |
| Many senior doctors | 0.199*** | (0.067. 0.332) | −0.089** | (−0.167, −0.011) | |
| Experts available on call | 0.078 | (−0.050. 0.205) | 0.139*** | (0.039, 0.239) | |
| Personal connection within the hospital | Know nobody (ref) | 0.038 | (−0.092, 0.168) | 0.036 | (−0.053, 0.126) |
| Know somebody, not very familiar with | 0.026 | (−0.123, 0.175) | 0.059 | (−0.062, 0.180) | |
| Direct personal connection | −0.064 | (−0.199, 0.072) | −0.095 | (−0.201, 0.011) | |
| Medical equipment condition | Obsolete (ref) | −0.275*** | (−0.387, −0.162) | −0.430*** | (−0.518, −0.341) |
| Advanced | 0.275*** | (0.162, 0.387) | 0.430*** | (0.341, 0.518) | |
| Travel time (min) | 90 (ref) | −0.096 | (−0.220, 0.027) | −0.037 | (−0.133, 0.059) |
| 40 | 0.014 | (−0.128, 0.156) | −0.176*** | (−0.285, −0.067) | |
| 15 | 0.083 | (−0.063, 0.229) | 0.213*** | (0.109, 0.318) | |
| Facility size | Small (ref) | 0.050 | (−0.109, 0.209) | −0.121 | (−0.257, 0.015) |
| Medium | 0.024 | (−0.133, 0.181) | −0.095 | (−0.179, 0.029) | |
| Large | −0.074 | (−0.218, 0.070) | 0.196*** | (0.078, 0.314) | |
| Opt-out | 2.499*** | (2.075, 2.923) | −6.024*** | (−6.883, −5.165) | |
| Interaction: attribute levels × severity | 3-h visit × severity | 0.173** | (0.012, 0.334) | ||
| 1-h visit × severity | −0.495*** | (−0.690, −0.301) | |||
| Many senior doctors × severity | −0.288*** | (−0.442, −0.134) | |||
| Advanced equipment × severity | 0.155** | (0.020, 0.289) | |||
| 40-min travel × severity | −0.190** | (−0.369, −0.010) | |||
| Large size × severity | 0.270*** | (0.087, 0.453) | |||
| Not visiting a facility × severity | −8.524*** | (−9.453, −7.594) | |||
| Model fit | Akaike Information Criterion | 4539.866 | |||
| Log likelihood | 9171.732 | ||||
| Number of mixed logit iterations used = 16; choice observations = 6, 357; respondents = 532. | |||||
Coefficients for severe condition are post hoc estimates based on the coefficients for minor condition. Coefficients of the reference levels are calculated as the negative sum of the coefficients of the other levels of the attribute. In the minor condition, coefficient and SE represent the estimated results in the case of perceived minor disease; in the severe condition, coefficient and SE represent the estimated results in the case of perceived minor disease. Only the significant interaction terms are listed in the table. ** and *** denote significance at the 0.05 and 0.01 level, respectively. OOP, out-of-pocket expenses; ref, reference levels; SE, standard error.
For conditions perceived as minor, three of the seven attributes were not significant: personal connection, travel time and facility size. For conditions perceived as severe, all attributes were significant, except for personal connection.
For a condition perceived as severe, the respondents were more tolerant of a long visit time, showed a strong preference for a 3-h visit, a larger hospital and a strong aversion to opting out. Medical experts were most preferred among the three types of doctors and only medical experts generated a positive effect in utility. However, junior doctors were preferred to senior doctors, although the difference in utility between these two types of doctors is small.
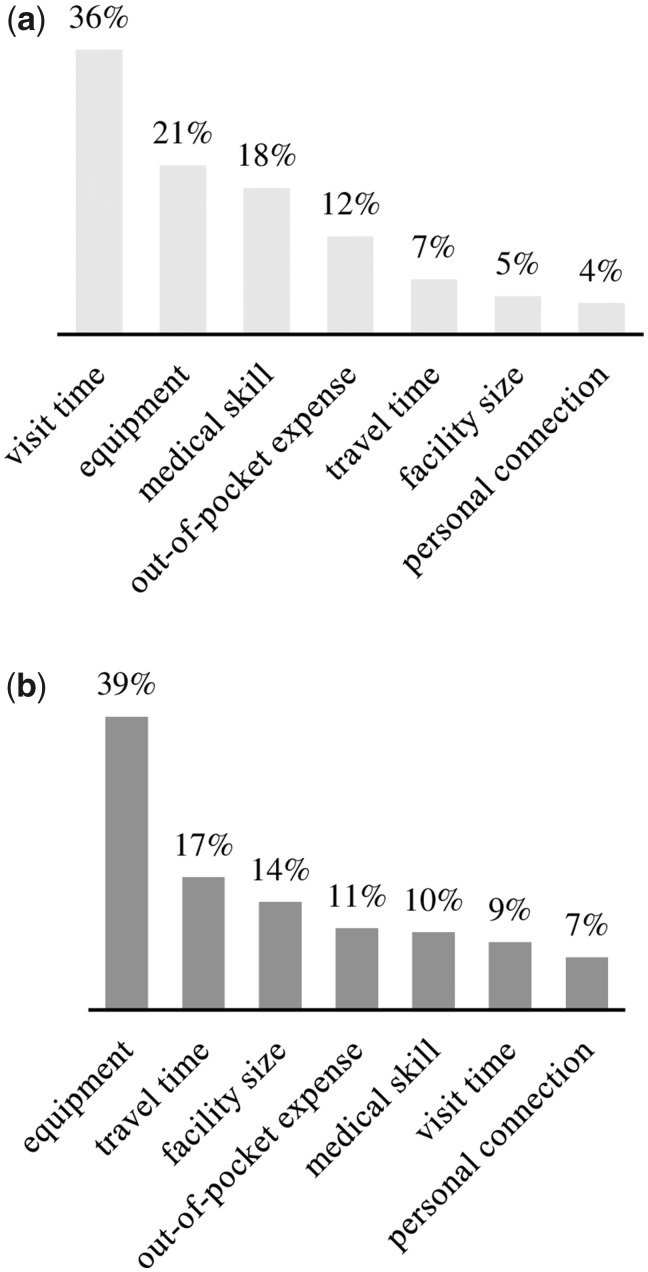
Figure 2 presents the results of the relative importance. The respondents attached different relative importance to the factors depending on perceived disease severity. For conditions perceived as minor, they gave most importance to visit time, followed by equipment, medical skill and out-of-pocket (OOP) expense. For conditions perceived as severe, they attached highest importance to equipment, followed by travel time, facility size, OOP expense, medical professionals’ skill and visit time.
Figure 2.
Relative importance of attributes under (a) perceived minor disease and (b) perceived severe disease.
Predicted choice probabilities
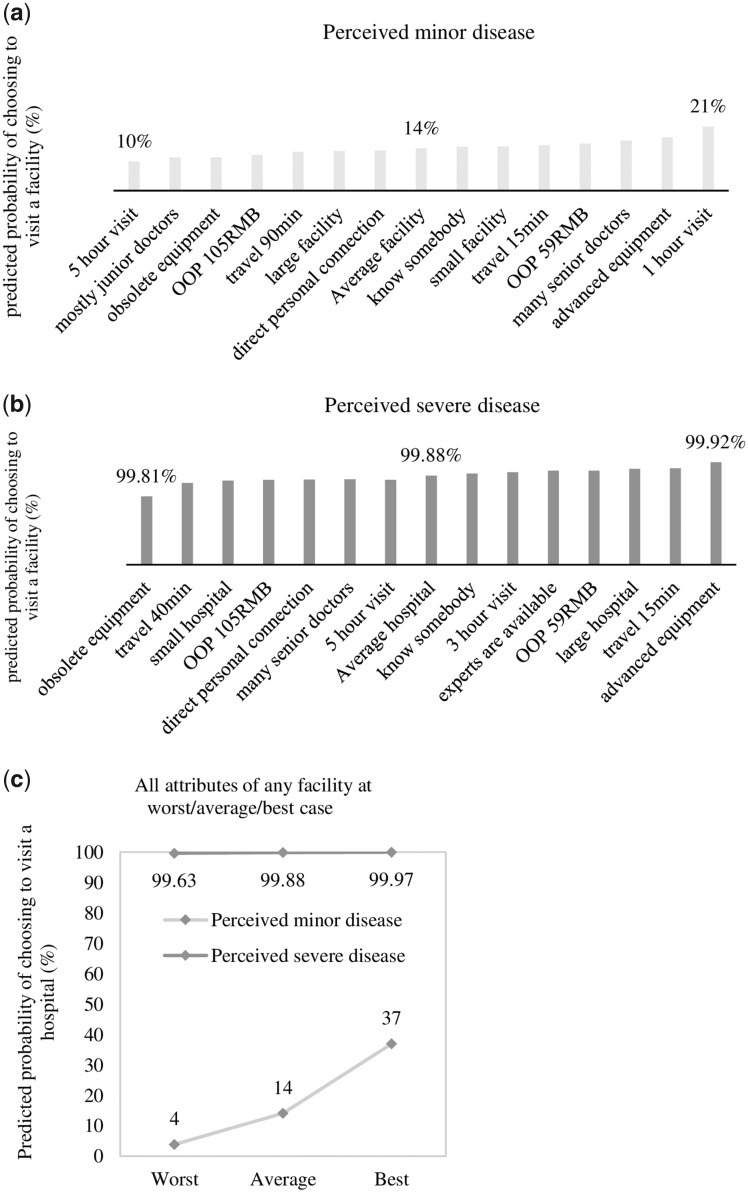
Choosing a facility vs opting out
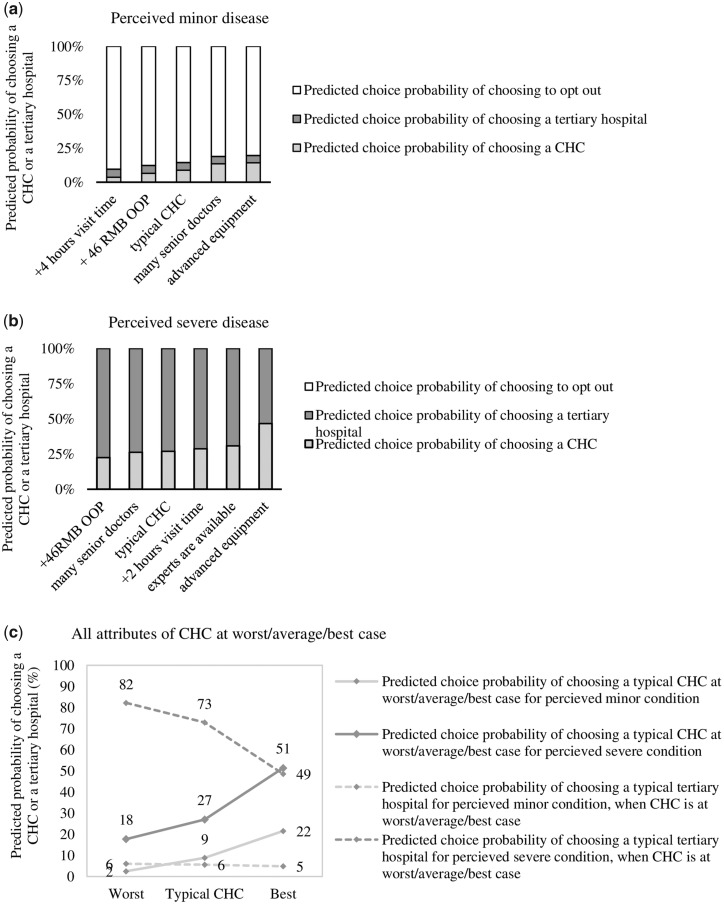
At 86% for perceived minor conditions and 0.12% for perceived severe conditions, the probabilities of choosing to opt out are notable (Figure 3a and b). When attribute levels were changed one at a time to the lowest and highest values, these probabilities ranged between 90% and 79% for perceived minor conditions: the predicted probability of choosing a facility was 10% at the lowest and more than doubled to a maximum of 21% for the one-way changes. For conditions perceived as severe, the range of the predicted choice probabilities was much smaller in absolute terms, between 0.19% and 0.08%, for the one-way changes. The relative change in the probabilities, however, was as large as that for the perceived minor conditions.
Figure 3.
(a) One-way impact of the attributes on the predicted probabilities of choosing an average hospital over opting out under out for perceived minor condition; (b) one-way impact of the attributes on the predicted probabilities of choosing and average hospital over opting out for perceived severe condition; (c) predicted choice probabilities of choosing to visit an average hospital at its worst, average and best attribute levels over opting out under different disease severity scenarios for the first visit. OOP, out-of-pocket expense per visit.
Now let us consider the best and worst cases attainable when changing all factors simultaneously rather than one at a time (Figure 3c). For a condition perceived as minor, the predicted probabilities of choosing a facility under the worst scenario were only 4% (96% preferring to opt out) and it increased substantially to 37% under the best scenario. For a condition perceived as severe, the predicted probabilities of choosing opt-out ranged from 0.37% to 0.03%, a 92% difference in the relative probability.
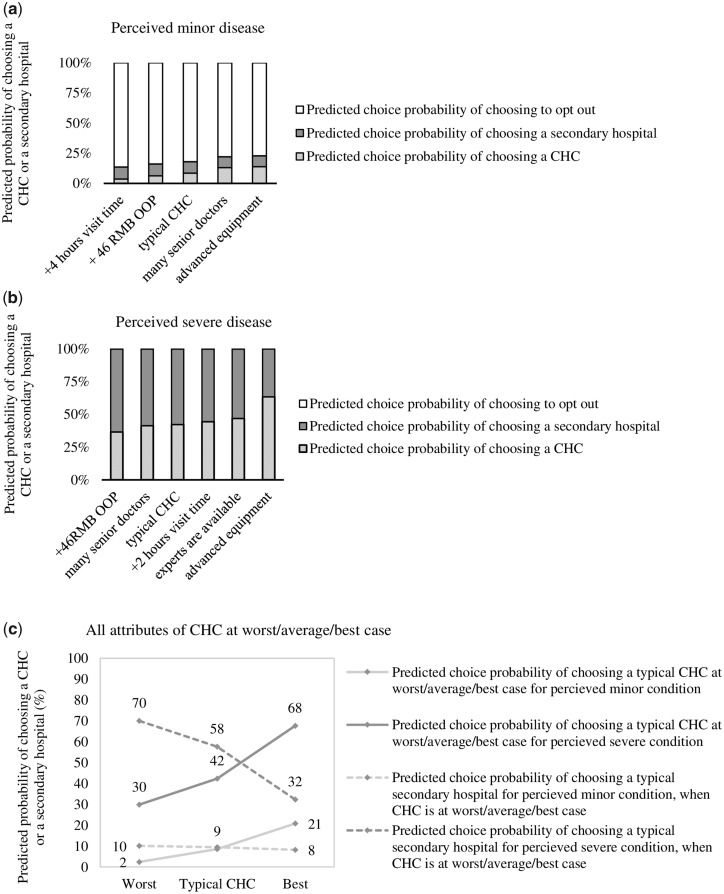
Choosing a community health centre vs a typical secondary hospital
For conditions perceived as minor, the predicted probability of choosing a secondary hospital was higher than that of a CHC. When changing one factor at a time, the secondary hospital still had a higher probability of being chosen, unless the level of medical skills or equipment of the CHC was improved (Figure 4a). The change in choice probabilities for conditions perceived as severe was as follows: only when the equipment at the CHC was improved to the advanced level was the choice probability of the CHC higher than that of a secondary hospital (Figure 4b).
Figure 4.
(a) One-way impact of the attributes on the predicted probabilities of choosing a CHC compared with a typically secondary hospital for perceived minor condition; (b) one-way impact of the attributes on the predicted probabilities of choosing a CHC and typical secondary hospital for perceived severe condition; (c) predicted probabilities of choosing a CHC and a typical secondary hospital under different disease severity scenarios for first visit. CHC, community health centre; OOP, out-of-pocket expense per visit.
Figure 4c shows the predicted probabilities of choosing a CHC or secondary hospital when the attributes of the CHC changed simultaneously from worst to best scenario. For conditions perceived as minor, the probability of choosing a CHC grew from 2% to 21% (>10-fold), with a decrease in the choice probability of a secondary hospital from 10% to 8%. It suggests that the large increase in the predicted probability of choosing a best-case CHC mostly came from the patients who previously preferred to opt out when the CHC is at worst case. In severe conditions, the choice probability of a CHC increased from 30% to 68% when it was improved to the best case, accompanied by a corresponding decrease in the choice probability of a secondary hospital from 70% to 32%. In this case, the patients switched to choosing a CHC from choosing secondary hospital when the CHC was improved to its best case.
Choosing a community health centre vs a typical tertiary hospital
For conditions perceived as minor, the predicted probability of choosing a CHC was always larger than that of a tertiary hospital, unless the visit time of a CHC increased from 1 to 5 h (Figure 5a). For conditions perceived as severe, the respondents were more likely to choose a tertiary hospital even if experts or advanced equipment were available at a CHC (Figure 5b).
Figure 5.
(a) One-way impact of the attributes on the predicted probabilities of choosing a CHC compared with a typical tertiary hospital for perceived minor condition; (b) one-way impact of the attributes on the predicted probabilities of choosing a CHC compared with a typical tertiary hospital for perceived severe condition; (c) predicted probabilities of choosing a CHC and typical tertiary hospital under different disease severity scenarios for first visit. CHC, community health centre; OOP, out-of-pocket expense per visit.
Figure 5c shows the predicted probabilities of choosing a CHC or tertiary hospital when the attributes of the CHC change simultaneously from the worst to the best scenario. In the minor condition, the choice probability of the CHC increased substantially from 2% to 22%. This more than 10-fold increase was predominantly due to a reduced probability of opting out. For conditions perceived as severe, the choice probabilities of the CHC and the tertiary hospital were hugely different in the worst-case scenario of the CHC (18% vs 82%), but they converged to be approximately equal (51% vs 49%) in the best-case scenario of the CHC. Thus, the predicted choice probability of a CHC at its best is almost three times higher in comparison to the worst.
Discussion
This study addressed valuations of facility attributes by urban Chinese when choosing a health care facility for first visit. We conducted a DCE in Shanghai to elicit the relative importance of facility attributes. To the best of our knowledge, this is the first study on the quantitative effects of facility attributes on facility choice for the urban population of China. The results expand the existing understanding of facility choice and provide suggestions for tailored policies to guide patient flow to primary care in urban China, thus, improving the efficiency and effectiveness of the health system.
The results showed that the urban residents weighed facility attributes differently depending on whether they perceived their condition as minor or severe. For conditions perceived as minor, they valued a rapid consultation service highly, followed by availability of advanced equipment and medical skills of doctors. However, visit time became insignificant when the condition is perceived as severe, in which case the relative importance of equipment dominated. These findings echo the literature which reports that people with severe conditions are likely to choose big hospitals for superior care and advanced equipment (Wu et al., 2017; Lin et al., 2018). Notably, the equipment factor was pivotal and in both cases had larger importance attached than the medical skills of doctors.
The results of this study can be cautiously compared with a DCE conducted in rural China (Liu et al., 2019). Rural residents also valued visit time most in conditions perceived as minor, but they did not attach large importance to equipment for conditions perceived as severe. In addition, OOP expense was considered more important under both severity scenarios for rural residents, which might be explained by their lower average income. For both urban and rural residents, facility size was never the most important factor, which implied that the popular term ‘big hospital’ may not merely refer to the physical size but rather to other attributes commonly associated with size. However, for conditions perceived as severe, urban residents valued a large-sized hospital most of the three sizes, whereas rural residents preferred a mid-sized facility. This might be due to the difficulty in navigating big hospitals reported by rural residents (Liu et al., 2018c). These findings suggest that policy measures should be tailored to the different choice behaviours for urban and rural China to enhance their effectiveness.
For conditions perceived as minor, the respondents showed a large preference for opting out, which confirms evidence of a considerable latent health care demand (Yu et al., 2017). Our results showed that this latent demand could reduce from 86% to 63% when the facilities (especially CHCs) are improved to the best case. These decreases reflect that improvement of CHC might turn presently latent demand into first visits at CHCs, more than doubling the number of first visits. Similarly, the predicted choice probability of opting out in severe condition decreased relatively by 75% (from 0.12% to 0.03%) when a CHC was improved to the best case.
We found that the health care demand for both severity conditions tended towards higher-level hospitals, although people were less likely to visit a tertiary hospital for conditions perceived as minor. Improving CHCs may reverse this situation, causing the corresponding number of first visits to primary care to grow (as we discuss below). Improvements to equipment or medical skill increase the probability of choosing a CHC more than modifying other attributes. Notably, having experts was the most preferred level of medical skill for conditions perceived as severe, while the respondents preferred senior doctors for conditions perceived as minor.
Improving CHCs could not only alter latent demand into actual medical consulting in the minor condition, but also attract a considerable portion of patients who would otherwise choose secondary (11.11%) or tertiary hospitals (16.67%) for conditions perceived as minor. Such changes in the predicted choice probability of CHCs were even more significant for conditions perceived as severe. Most notably, when people choose between CHCs and secondary hospitals—the choice probability of the secondary hospital decreased by 44.83% if the typical CHCs were improved to a best case. For tertiary hospitals, this reduction was 32.88%. These numbers too indicate that improvement of CHCs can lead to very sizable increases in patients attending CHCs for their first visit.
As the middle level of the health care system, secondary hospitals provide health services to the region across different communities and take the responsibility for receiving referrals from CHCs in urban areas (National Health Commission, 2011). However, the literature has seldom addressed the utilization of secondary hospitals. Our analysis presents the first results addressing secondary care utilization in urban China.
The Chinese government is making efforts to improve the primary care system. For example, as a main component to incentivize choosing primary care, the national health insurance scheme offers a higher reimbursement rate at primary care facilities (Barber and Yao, 2010). However, our results show that OOP expense was not a main factor (ranked only the fourth important factor) in either severity scenarios for our urban respondents. The effect of such costly incentives to shift patient flow to the primary level may, therefore, be modest in urban areas. To improve the medical skill in the primary care system, several provinces have rolled out a policy to motivate the doctors from higher-level hospitals to work periodically in CHCs (Beijing Municipal Health Commission, 2016). The results of our study showed that improving medical skill would work moderately effectively to shift urban patients from higher-level facilities to CHCs. Specifically, compared with having medical experts, having more senior doctors would more effectively guide patient flow to primary care. As visit time was so important in a minor disease scenario, our results suggest that accelerating the registration and treatment process may guide the patient flow more efficiently. In addition, this study conveys an important message regarding the high importance of medical equipment. Although policy measures were taken to improve the infrastructure of the primary care system, a considerable number of primary care facilities still cannot do routine procedures such as blood tests or chest X-rays (Li et al., 2017). In general, our results confirm current policies to improve medical skill and equipment as important to advance CHCs towards best case and to redirect patient flow to CHCs. In reality, these policies are constrained by budget and human resource limitations.
The high importance of medical equipment identified in our study and the exclusive availability of advanced medical equipment in higher-level hospitals can largely explain why patients tend to choose higher-level hospitals (National Health Commission, 2011; Lin et al., 2018). This may further exacerbate as competition incentivizes higher-level hospitals to invest more in equipment, a situation known as the medical arms race (Pan et al., 2016; Qian et al., 2019). In addition, studies report that competition among higher-level hospitals did not result in significant improvements on service quality or health outcomes (Pan et al., 2016; Cai et al., 2018b; Lin et al., 2018). While it may be difficult to achieve, our results show that it may be beneficial to redirect budget for investment in medical equipment from tertiary hospitals to CHCs. Frugal innovation may serve to do so at an affordable cost (Ramdorai and Herstatt, 2015; Tran and Ravaud, 2016).
It is worth noting that improvements in CHC attributes may result in considerable increases in first visits for conditions perceived as minor and for conditions perceived as severe. Such large increases may eventually cause the presently underutilized capacity of primary care facilities to become insufficient and reduce responsiveness. Therefore, research on the capacity of primary care facilities is called for to ensure these facilities are able to provide timely access to meet demand, as envisioned by the Alma-Ata agreement (Primary Health Care: Declaration of Alma-Ata, 1978).
Study limitations
One limitation of this study is that all data were collected in three adjacent residency communities in Shanghai. Therefore, the results should be interpreted with caution when generalizing to urban China at large. Moreover, the mid level of travel time (40 min) was least preferred for conditions perceived as severe. We fixed the travel time at 15 min in the major part of our analysis to limit the effect of this counter-intuitive finding. While in real life, China’s urban population can choose between three levels, the choice sets that we used limited the choice between two facilities at a time (and opting out). This was done to control the cognitive burden and promote the credibility of the choice data (Caussade et al., 2005).
Conclusion
For perceived minor and severe diseases, urban residents in China weigh facility attributes differently for first-contact facility choice. For conditions perceived as minor, the respondents valued visit time, equipment and medical skill the most, whereas for conditions perceived as severe, they placed most importance on equipment, travel time and facility size. The latent demand found is very high at 86% for conditions perceived as minor, but can be partly converted into facility visits by improving CHCs. In addition, our results strongly suggest that making appropriate improvements and innovations at CHCs can effectively guide patient flow from higher-level hospitals to primary level.
Supplementary Material
Acknowledgements
We acknowledge support from all residential committees in Hongkou district on the respondent recruitment and administrating questionnaires. We thank Prof. Guohua Wan (Shanghai Jiaotong University) for the support on organizing the task force for the recruitment. The research is supported in part by National Natural Science Foundation of China [Grants 71520107003 and 71421002].
Conflict of interest statement. None declared.
Ethical approval. This study received ethical approval from Medical Ethical Review Committee of the authors’ institute [No. 2017 KY207].
References
- Barber SL, Yao L.. 2010. Health Insurance Systems in China: A Briefing Note. World Health Report. [Google Scholar]
- Bech M, Gyrd-Hansen D.. 2005. Effects coding in discrete choice experiments. Health Economics 14: 1079–83. [DOI] [PubMed] [Google Scholar]
- Beijing Municipal Health Commission. 2016. Key Tasks of Beijing Graded Medical Treatment System Construction 2016–2017 Beijing: Beijing Municipal Health Commission. [Google Scholar]
- Bliemer MCJ, Rose JM.. 2013. Confidence intervals of willingness-to-pay for random coefficient logit models. Transportation Research Part B: Methodological 58: 199–214. [Google Scholar]
- Cai M, Liu E, Li W.. 2018. Rural versus urban patients: benchmarking the outcomes of patients with acute myocardial infarction in Shanxi, China from 2013 to 2017. International Journal of Environmental Research and Public Health 15: 1930.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai M, Liu E, Tao H. et al. 2018. Does level of hospital matter? A study of mortality of acute myocardial infarction patients in Shanxi, China. American Journal of Medical Quality 33: 185.. [DOI] [PubMed] [Google Scholar]
- Caussade S, Ortúzar J de D, Rizzi LI, Hensher DA.. 2005. Assessing the influence of design dimensions on stated choice experiment estimates. Transportation Research Part B: Methodological 39: 621–40. [Google Scholar]
- Chen Y, Yin Z, Xie Q.. 2014. Suggestions to ameliorate the inequity in urban/rural allocation of healthcare resources in China. International Journal for Equity in Health 13: 34–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark MD, Determann D, Petrou S, Moro D, de Bekker-Grob EW.. 2014. Discrete choice experiments in health economics: a review of the literature (updated). PharmacoEconomics 32: 883–902. [DOI] [PubMed] [Google Scholar]
- de Bekker-Grob EW, Donkers B, Jonker MF, Stolk EA.. 2015. Sample size requirements for discrete-choice experiments in healthcare: a practical guide. The Patient 8: 373–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bekker-Grob EW, Veldwijk J, Jonker M. et al. 2018. The impact of vaccination and patient characteristics on influenza vaccination uptake of elderly people: a discrete choice experiment. Vaccine 36: 1467–76. [DOI] [PubMed] [Google Scholar]
- Eggleston K. 2012. Health care for 1.3 billion: an overview of China’s health system. The Milken Institute Review 2–28. [Google Scholar]
- Gu X, Zhang L, Tao S, Xie B.. 2019. Spatial accessibility to healthcare services in metropolitan suburbs: the case of Qingpu, Shanghai. International Journal of Environmental Research and Public Health 16: 225.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen J, Groenewegen PP, Boerma WGW, Kringos DS.. 2015. Living in a country with strong primary health is beneficial to people with chronic conditions. Health Affairs 34: 1531–7. [DOI] [PubMed] [Google Scholar]
- Hauber AB, González JM, Groothuis-Oudshoorn CGM. et al. 2016. Statistical methods for the analysis of discrete choice experiments: a report of the ISPOR conjoint analysis good research practices task force. Value in Health 19: 300–15. [DOI] [PubMed] [Google Scholar]
- Johnson FR, Lancsar E, Marshall D. et al. 2013. Constructing experimental designs for discrete-choice experiments: report of the ISPOR conjoint analysis experimental design good research practices task force. Value in Health 16: 3–13. [DOI] [PubMed] [Google Scholar]
- Kringos BDS, Boerma W, Van Der Zee J, Groenewegen P.. 2013. Health Affairs 4: 686–94. [DOI] [PubMed] [Google Scholar]
- Lancsar E, Louviere J, Flynn T.. 2007. Several methods to investigate relative attribute impact in stated preference experiments. Social Science & Medicine 64: 1738–53. [DOI] [PubMed] [Google Scholar]
- Li X, Lu J, Hu S. et al. 2017. The primary health-care system in China. The Lancet 390: 2584–94. [DOI] [PubMed] [Google Scholar]
- Li Y, Rao K, Ren X.. 2012. Use of and factors associated with self-treatment in China. BMC Public Health 12: 1.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin X, Cai M, Fu Q. et al. 2018. Does hospital competition harm inpatient quality? Empirical evidence from Shanxi, China. International Journal of Environmental Research and Public Health 15: 2283.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu G, Vortherms SA, Hong X.. 2017. China’s health reform update. Annual Review of Public Health 38: 431.. [DOI] [PubMed] [Google Scholar]
- Liu X, Tan A, Towne SD, Hou Z, Mao Z.. 2018a. Awareness of the role of general practitioners in primary care among outpatient populations: evidence from a cross-sectional survey of tertiary hospitals in China. BMJ Open 8: e020605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Kong Q, de Bekker-Grob EW.. 2019. Public preferences for health care facilities in rural China: a discrete choice experiment. Social Science & Medicine 237: 112396. [DOI] [PubMed] [Google Scholar]
- Liu Y, Kong Q, Yuan S, van de Klundert J.. 2018b. Factors influencing choice of health system access level in China—a systematic review. PLoS One 13: e0201887.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Zhong L, Yuan S, van de Klundert J.. 2018c. Why patients prefer high-level healthcare facilities: a qualitative study using focus groups in rural and urban China. BMJ Global Health 3: e000854.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Louviere JJ, Lancsar E.. 2009. Choice experiments in health: the good, the bad, the ugly and toward a brighter future. Health Economics, Policy and Law 4: 527–46. [DOI] [PubMed] [Google Scholar]
- McFadden D, Train K.. 2000. Mixed MNL models for discrete response. Journal of Applied Econometrics 15: 447–70. [Google Scholar]
- Miao J, Wu X.. 2016. Urbanization, socioeconomic status and health disparity in China. Health & Place 42: 87–95. [DOI] [PubMed] [Google Scholar]
- Ministry of Finance. 2018. State Council Report on the Distribution and Use of Financial Health Care Funds.Beijing: Ministry of Finance. [Google Scholar]
- Ministry of Health. 2006. Urban Community Health Service Agency Management Approach Beijing: Ministry of Finance. [Google Scholar]
- National Bureau of Statistics. 2017. China Statistical Yearbook. Beijing: China Statistics Press. [Google Scholar]
- National Health Commission. 2011. Interim Measures for Hospital Accreditation Beijing: National Health Commission. [Google Scholar]
- National Health Commission. 2017. Statistical Yearbook for Health and Family Planning in China Beijing: National Health Commission. [Google Scholar]
- Pan J, Qin X, Hsieh C-R.. 2016. Is the pro-competition policy an effective solution for China’s public hospital reform? Health Economics, Policy and Law 11: 337–57. [DOI] [PubMed] [Google Scholar]
- Primary health care: declaration of Alma-Ata. 1978. The Lancet 312: 1040–1. [PubMed] [Google Scholar]
- Qian J, Jingwei He A, Dean-Chen Yin J.. 2019. The medical arms race and its impact in Chinese hospitals: implications for health regulation and planning. Health Policy and Planning 34: 37–46. [DOI] [PubMed] [Google Scholar]
- Ramdorai A, Herstatt C.. 2015. Frugal Innovation in Healthcare How Targeting Low-Income Markets Leads to Disruptive Innovation.Switzerland: Springer. [Google Scholar]
- Shanghai Bureau of Statistics. 2008. Shanghai Statistical Yearbook Shanghai: Shanghai Bureau of Statistics. [Google Scholar]
- Shanghai Bureau of Statistics. 2018. Shanghai Statistical Yearbook Shanghai: Shanghai Bureau of Statistics. [Google Scholar]
- Starfield B, Shi L, Macinko J, Milbank Q.. 2005. Contribution of primary care to health systems and health. The Milbank Quarterly 83: 457–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC.
- The State Council. 2006. Guiding Opinions on the Development of Urban Community Health Services Beijing: The State Council. [Google Scholar]
- The State Council. 2015. Graded Diagnosis and Treatment Pilot Work Evaluation Criteria Beijing: The State Council. [Google Scholar]
- Tran VT, Ravaud P.. 2016. Frugal innovation in medicine for low resource settings. BMC Medicine 14: 102–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veldwijk J, Lambooij MS, De Bekker-Grob EW, Smit HA, De Wit GA.. 2014. The effect of including an opt-out option in discrete choice experiments. PLoS One 9: e111805.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu D, Lam TP.. 2016. Underuse of primary care in China: the scale, causes, and solutions. The Journal of the American Board of Family Medicine 29: 240–7. [DOI] [PubMed] [Google Scholar]
- Wu D, Lam TP, Lam KF, Zhou XD, Sun KS.. 2017. Health reforms in China: the public’s choices for first-contact care in urban areas. Family Practice 34: 194–200. [DOI] [PubMed] [Google Scholar]
- Yip W, Hsiao W.. 2014. Harnessing the privatisation of China’s fragmented health-care delivery. The Lancet 384: 805–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yip WCM, Hsiao WC, Chen W. et al. 2012. Early appraisal of China’s huge and complex health-care reforms. The Lancet 379: 833–42. [DOI] [PubMed] [Google Scholar]
- Yu W, Li M, Ye F, Xue C, Zhang L.. 2017. Patient preference and choice of healthcare providers in Shanghai, China: a cross-sectional study. BMJ Open 7: e016418.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L, Cheng G, Song S. et al. 2017. Efficiency performance of China’s health care delivery system. The International Journal of Health Planning and Management 32: 254–63. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.