Highlights
-
•
Rural residents in central China were exposed to high levels of PM1.
-
•
PM1 exposure was related to increased TC and LDL-C, and decreased TG and HDL-C.
-
•
High levels of PM1 was associated with higher risk of dyslipidemias.
-
•
Males, older and overweight participants were vulnerable to adverse effects of PM1.
Keywords: PM1, Dyslipidemia, Blood lipids, Rural areas, Cohort study
Abstract
Background
Air pollution has been shown to be associated with blood lipid levels. However, studies on long-term ambient particulate matter with aerodynamic diameter ≤1 μm (PM1) exposure in high-exposure areas are still limited. This study aimed to explore the associations among long-term PM1 exposure, blood lipids and dyslipidemias.
Methods
Baseline data of The Henan Rural Cohort study was used in present study, including a total of 39,259 participants aged from 18 to 79 years. Daily levels of PM1 were estimated by a spatiotemporal model using ground-level measurements of PM1, satellite remote sensing data and other predictors, according to participants' home addresses. Individual exposure to PM1 was the 3-year average before baseline investigation. Linear regression and logistic regression models were applied to examine the associations among PM1, blood lipids ((total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL-C) and low-density lipoprotein cholesterol (LDL-C)), and prevalence of dyslipidemias.
Results
The 3-year concentration of PM1 was 55.7 ± 2.1 μg/m3. Each 1 μg/m3 increment of PM1 was associated with an increase of 0.21% (95% confidence interval (CI): 0.11%–0.31%) in TC and 0.75% (95% CI: 0.61%–0.90%) in LDL-C, while decrease of 2.68% (95% CI: 2.43%–2.93%) in TG and 0.47% (95% CI: 0.35%–0.59%) in HDL-C. Each 1 μg/m3 increase in PM1 was associated with 6% (95% CI: 4%–8%), 3% (95% CI: 2%–5%) and 5% (95% CI: 3%–7%) higher risks of hypercholesterolemia, hyperbetalipoproteinemia and hypoalphalipoproteinemia. Sex, age and BMI statistically modified the associations between PM1 with blood lipid levels and dyslipidemias.
Conclusions
Higher PM1 exposure was associated with adverse changes of blood lipid levels and dyslipidemias. Males, older and overweight participants were susceptive to the adverse effects of PM1.
1. Introduction
The prevalence of dyslipidemia has been increasing and hyperbetalipoproteinemia remained one of the primary causes of risk-attributable death from 1990 to 2017 around the world (GBD, 2018). China Chronic Disease and Risk Factor Surveillance (CCDRFS) reported that the prevalence of hypercholesterolemia, hypertriglyceridemia, hypoalphalipoproteinemia and hyperbetalipoproteinemia in 2012 had significantly increased to 6.9%, 13.8%, 20.4%, and 8.1%, compared with that in 2002 (2.9%, 11.9%, 7.4% and 2.5%) (Longde, 2005, Zhang et al., 2018a). Epidemiological studies have shown abnormal lipid metabolism and blood lipids were related to total mortality, cardiovascular disease mortality, and risk of cardiovascular diseases (CVDs) (Anderson et al., 1987, Liu et al., 2001, Tirschwell et al., 2004).
Ambient particulate matter (PM) remained an increasingly crucial public health issue worldwide. Many studies indicated PM exposure can exacerbate abnormal lipid metabolism and lead to adverse health effects in China (Wang et al., 2018, Yang et al., 2018a), U.S.(McGuinn et al., 2019, Shanley et al., 2016, Yeatts et al., 2007), Iran (Poursafa et al., 2014) and Israel (Yitshak Sade et al., 2016). For instance, McGuinn et al. (2019) reported higher PM with diameter ≤ 2.5 μm (PM2.5) exposure corresponded to increased total cholesterol (TC), triglyceride (TG), low-density lipoprotein cholesterol (LDL-C) and high-density lipoprotein cholesterol (HDL-C). In addition, a longitudinal study in U.S. demonstrated that increased PM2.5 exposure accounted for higher risk for hypertriglyceridemia (Wallwork et al., 2017). PM with diameter ≤ 1.0 μm (PM1) is a major constituent of PM2.5, which accounts for over 80% of PM2.5 mass in China (Chen et al., 2018a, Yang et al., 2018b). PM1 has a bigger surface-to-mass ratio than PM2.5, suggesting that PM1 may have worse effects on human health as it contains more biological and/or chemical toxins, infiltrates deeper into lung alveoli and avoids the alveolar phagocytes(Brown et al., 2001, Delfino et al., 2011). Compared with the adverse effect of PM2.5 on hypertension and metabolic syndrome, similar adverse effects of PM1 were reported (Yang et al., 2018b, Yang et al., 2018c).
To date, most studies focused on the adverse effects of PM2.5 and PM10 on blood lipids and dyslipidemia, while few studies addressed the effects of PM1. A study based on an urban population reported that PM1 exposure was associated with higher risk of hypercholesterolemia, hypoalphalipoproteinemia and hyperbetalipoproteinemia (Yang et al., 2018a). Variation among living environment, food, household cooking energy, healthcare care services and economics contributed to different susceptibilities between urban and rural populations (Li et al., 2018, Liu et al., 2016). However, evidence of PM1 and blood lipid levels in rural populations are still lacking. Thereby, accurate estimation of adverse effect of PM1 exposure to dyslipidemia in rural population are urgently needed, especially in Chinese populations whose prevalence of dyslipidemia had reached to 40.8% (Zhang et al., 2018a).
This study was designed to explore the associations between long-term PM1 exposure, blood lipids and the prevalence of dyslipidemias in a rural population using the baseline data from The Henan Rural Cohort study.
2. Material and methods
2.1. Study population
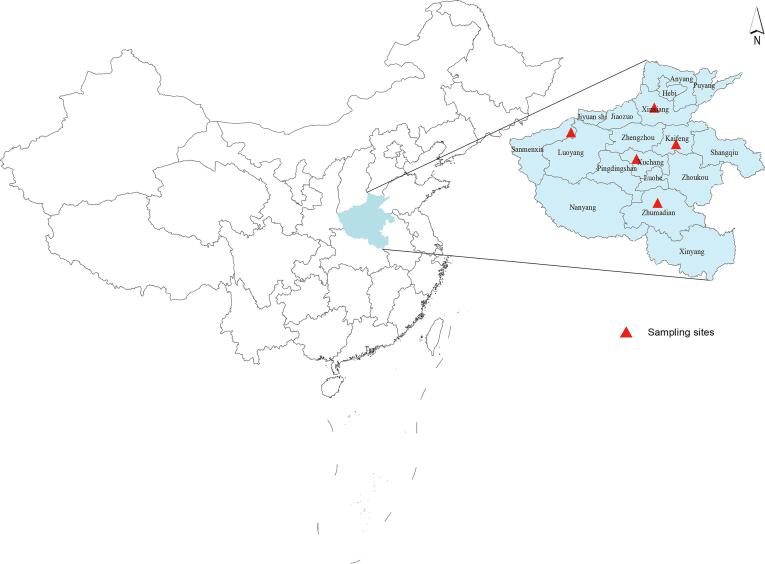
Study population was derived from The Henan Rural Cohort study (Registration number: ChiCTR-OOC-15006699). Specific information has been reported in previous studies (Liu et al., 2019, Liu et al., 2018, Tian et al., 2018). In brief, multistage stratified random cluster sampling method was adopted to recruit the eligible participants in five rural areas (Zhumadian, Xuchang, Xinxiang, Kaifeng and Sanmenxia) in Henan province, China. The locations of sampling sites were shown in Fig. 1. A total of 39,259 permanent residents aged from 18 to 79 years were collected during 2015–2017, with a response rate of 93.7%. Individuals with severe physical or mental disease were excluded. We excluded individuals with missing lipids data (n = 138) and key demographic characteristics (n = 64). Finally, 39,057 participants were included in our analysis. Zhengzhou University Life Science Ethics Committee approved The Henan Rural Cohort study (Code: [2015] MEC (S128)). Informed consents were signed before investigation.
Fig. 1.
The locations of sampling sites in the Henan Rural Cohort Study.
2.2. Data collection
A standardized questionnaire was designed to gather information on demographic characteristics (age, sex, marital status, incomes, education, etc.), lifestyle characteristics (smoking, alcohol drinking, diet habits, etc.) and family history (diabetes, hypertension, dyslipidemia, etc.). The survey was conducted by face-to-face interviews with well-trained workers. Moreover, a physical examination was conducted. Height (to 0.1 cm) and weight (to 0.1 kg) of each subjects were measured twice, then body mass index (BMI, kg/m2) was calculated. Details of the measurements and definitions have been reported in previous publications (Liu et al., 2019, Liu et al., 2018, Tian et al., 2018).
Venous blood samples were obtained from individuals after at least 8 h overnight fasting by well-trained physicians and nurses. Serum was immediately centrifuged at 3000 rpm for 10 min, 4 °C. TC, HDL-C, LDL-C and TG were measured by enzymatic methods with a chemistry analyzer (Cobas C501, Roche Diagnostics GmbH, Switzerland).
2.3. PM1 expose measurement
Concentrations of PM1 were estimated by a spatiotemporal model using satellite remote sensing, meteorological data and land use information at a 0.1-degree spatial resolution. Details of estimation method had been reported in previous publications (Chen et al., 2018a, Chen et al., 2018b). Briefly, we employed a general additive model to predict PM1 concentrations using ground-monitored PM1 data, two types of Moderate Resolution Imaging Spectroradiometer (MODIS) Collection 6 aerosol optical depth (AOD) data, Dark Target (DT) and Deep Blue (DB) and other spatiotemporal predictors (e.g., afforested cover, temperature, and rainfall). The adjusted coefficient of determination (R2) and Root Mean Squared Error (RMSE) for daily prediction was 0.58 and 21.7 µg/m3. Annual PM1 concentrations for each object were estimated according to residential addresses. Three-year average PM1 exposures of participants were used as an indicator of long-term PM1 exposure in this study, while one-year and five-year average PM1 exposures were used in sensitivity analyses.
2.4. Definition of dyslipidemias
According to the Guidelines on Prevention and Treatment of Dyslipidemia for Chinese Adults (2007), hypercholesterolemia was defined as TC ≥ 6.22 mmol/L; hypertriglyceridemia was defined as TG ≥ 2.26 mmol/L; hypoalphalipoproteinemia was defined as HDL-C < 1.04 mmol/L) and hyperbetalipoproteinemia was defined as LDL-C ≥ 4.14 mmol/L; dyslipidemia was defined as the presence of one or more abnormal blood lipid concentrations or accepting lipid-lowering medicines over the past two weeks.
2.5. Models and covariates
According to previous studies (McGuinn et al., 2019, Poursafa et al., 2014, Wallwork et al., 2017, Yang et al., 2018a), we include age, sex and body mass index (BMI, kg/m2) as covariates in baseline model. Then, we added these following factors in adjusted model, including marital status(married/cohabitation, unmarried/divorced/widowed), monthly income(<500 RMB, 500–1000 RMB, ≥1000 RMB), education level(elementary school or below, junior high school, high school or higher), smoking(never, former, current), alcohol drinking(never, former, current), family history of dyslipidemia (yes, no), high-fat diet(>75 g/day of meat from livestock and poultry) (yes, no), adequate fruit and vegetable intake(>500 g/day) (yes, no), and physical exercise(low, moderate, high).
2.6. Statistical analysis
Multiple linear regression analyses were performed to evaluate associations between PM1 exposure (per 1 μg/m3 increase) and naturally log-transformed blood lipids (TC, TG, LDL-C, and HDL-C), which was transformed to achieve normal distribution. And then percent differences with corresponding 95% CIs were computed by back-transforming effect estimates using 100 × [exp (β) − 1] (Yang et al., 2018a). Odds ratios (ORs) and 95% CIs were acquired from logistic regression models for dyslipidemias in respect of per 1 μg/m3 increment of PM1.
To examine potential modification effects, we performed a series of interactive analyses by including potential effect confounder, such as sex, age (<45 years, 45–60 years and ≥ 60 years), BMI (<24 kg/m2, 24–28 kg/m2 and ≥ 28 kg/m2) and lifestyle characteristics.
A string of sensitivity analyses were conducted to test the steadiness of our findings based on adjusted model. Associations of PM1 with blood lipid levels and dyslipidemias were estimated by excluding individuals who were taking lipid-lowering drugs and participants with diabetes. We also examined associations of 1-year and 5-year PM1 exposure with blood lipid levels and dyslipidemias.
We regarded P < 0.05 as statistical significance for main effects and interactions. All statistical analyses were conducted in SAS software 9.4.
3. Results
3.1. Descriptive statistics
Basic characteristics of all participants are shown in Table 1. A total of 15,365 males and 23,692 females were included in the study. The mean age of participants was 55.6 and the average BMI was 24.8 kg/m2. The mean level of TC, TG, HDL-C, and LDL-C was 4.75 mmol/L, 1.68 mmol/L, 1.33 mmol/L, and 2.87 mmol/L, respectively. The prevalence of hypercholesterolemia, hypertriglyceridemia, hypoalphalipoproteinemia, hyperbetalipoproteinemia and dyslipidemia in this rural population was 7.2%, 18.8%, 19.1%, 6.7% and 37.4%, respectively. The long-term PM1 exposure in our study was 55.6 ± 2.1 μg/m3, ranging from 48.1 μg/m3 to 70.9 μg/m3.
Table 1.
Characteristics of participants in The Henan Rural Study.
| Variables | Total (N = 39,057) |
Men (n = 15,365) |
Women (n = 23,692) |
|---|---|---|---|
| Age (years), mean (SD) | 55.6 (12.2) | 56.7 (12.3) | 54.9 (12.1) |
| BMI (kg/m2), mean (SD) | 24.8 (3.6) | 24.5 (3.5) | 25.0 (3.6) |
| Marital status, n (%) | |||
| Married/cohabitation | 35,059 (89.8) | 13,819 (90.0) | 21,240 (89.6) |
| Unmarried/divorced/widowed | 3998 (10.2) | 1546 (10.0) | 2452 (10.4) |
| Monthly income, n (%) | |||
| <500 Yuan | 13,950 (35.7) | 5571 (36.3) | 8379 (35.4) |
| 500 Yuan ~ | 12,849 (32.9) | 4891 (31.8) | 7958 (33.6) |
| ≥1000 Yuan | 12,258 (31.4) | 4903 (31.9) | 7355 (31.0) |
| Education attainment, n (%) | |||
| Primary school or below | 17,504 (44.8) | 5202 (33.9) | 12,302 (51.9) |
| Middle school | 15,556 (39.8) | 7100 (46.2) | 8456 (35.7) |
| High school or above | 5997 (15.4) | 3063 (19.9) | 2934 (12.4) |
| Smoking status, n (%) | |||
| Never | 28,470 (72.9) | 4866 (31.7) | 23,604 (99.6) |
| Former | 3165 (8.1) | 3142 (20.4) | 23 (0.1) |
| Current | 7422 (19.0) | 7357 (47.9) | 65 (0.3) |
| Alcohol drinking status, n. (%) | |||
| Never | 30,234 (77.4) | 7219 (47.0) | 23,015 (97.1) |
| Former | 1822 (4.7) | 1758 (11.4) | 64 (0.3) |
| Current | 7001 (17.9) | 6388 (41.6) | 613 (2.6) |
| High fat diet, n (%) | 7419 (19.0) | 3825 (24.9) | 3594 (15.2) |
| Adequate vegetable and fruit intake, n(%) | 16,292 (41.7) | 6560 (42.7) | 9732 (41.1) |
| Physical activity, n (%) | |||
| Low | 12,627 (32.3) | 5468 (35.6) | 7159 (30.2) |
| Moderate | 14,745 (37.8) | 4275 (27.8) | 10,470 (44.2) |
| High | 11,685 (29.9) | 5622 (36.6) | 6063 (25.6) |
| Family history of hyperlipidemia, n (%) | 1379 (3.5) | 447 (2.9) | 932 (3.9) |
| TC, mean (SD), mmol/L | 4.75 (0.98) | 4.63 (0.94) | 4.83 (0.99) |
| TG, mean (SD), mmol/L | 1.68 (1.12) | 1.66 (1.15) | 1.69 (1.10) |
| HDL-C, mean (SD), mmol/L | 1.33 (0.33) | 1.26 (0.32) | 1.37 (0.33) |
| LDL-C, mean (SD), mmol/L | 2.87 (0.82) | 2.83 (0.80) | 2.90 (0.83) |
| Dyslipidemia, n (%) | 14,602 (37.4) | 6123 (39.9) | 8479 (35.8) |
| Hypercholesterolemia, n (%) | 2825 (7.2) | 831 (5.4) | 1994 (8.4) |
| Hypertriglyceridemia, n (%) | 7330 (18.8) | 2815 (18.3) | 4515 (19.1) |
| Hypoalphalipoproteinemia, n (%) | 7477 (19.1) | 3910 (25.5) | 3567 (15.1) |
| Hyperbetalipoproteinemia, n (%) | 2624 (6.7) | 890 (5.8) | 1734 (7.3) |
Abbreviations: SD, standard deviation; BMI, body mass index; TC, total cholesterol; TG, triglyceride; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol.
3.2. Associations between PM1 and blood lipids
Table 2 summarizes associations between PM1 and blood lipids. In baseline and adjusted models, higher PM1 exposure was associated with elevated levels of TC and LDL-C, and decreased levels of TG and HDL-C levels. In adjusted model, every 1 μg/m3 PM1 increase was associated with 0.21% (95% CI: 0.11%–0.31%) and 0.75% (95% CI: 0.61%–0.90%) higher levels of TC and LDL-C, and 2.68% (95% CI: 2.43%–2.93%) and 0.47% (95% CI: 0.35%–0.59%) lower levels of TG and HDL-C, respectively.
Table 2.
Associations between per 1 μg/m3 increment of PM1 and blood lipid levels.
| TC | TG | HDL-C | LDL-C | |
|---|---|---|---|---|
| %Changes (95%CI) | %Changes (95%CI) | %Changes (95%CI) | %Changes (95%CI) | |
| Baseline Modela | 0.34 (0.24, 0.44) | −2.90 (−3.13, −2.66) | −0.41 (−0.52, −0.29) | 0.89 (0.75, 1.03) |
| Adjusted Modelb | 0.21 (0.11, 0.31) | −2.68 (−2.93, −2.43) | −0.47 (−0.59, −0.35) | 0.75 (0.61, 0.90) |
Abbreviations: CI, confidence interval; TC, total cholesterol; TG, triglyceride; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol.
Covariates included age, sex and BMI.
Covariates included age, sex, BMI, education, marital status, family income, smoking, alcohol drinking, high fat diet, adequate vegetable and fruit intake, physical activities and family history of dyslipidemia.
We have examined interactions of sex, age, BMI and lifestyle characteristics (see Fig. 2 and Table S1 in the Supplements). The estimated effects of PM1 were stronger in males than females (P < 0.05). The interactions of age were presented in associations between PM1 with TC, TG and LDL-C. The association between PM1 and TC among participants over 60 years old (0.52%) was statistically higher than those<45 years old (0.03%). Higher effect of PM1 on TG was observed among participants aged from 45 to 60 compared to younger participants. Furthermore, the adverse effects of PM1 on LDL-C were getting worse along with the increasing of age and BMI. The modification of BMI on the effects of PM1 was presented on LDL-C only. Our results also showed that high-fat diet can mitigate the associations of PM1 with TC and TG. Adequate Vegetable and fruit intake modified the associations of PM1 with TG and LDL-C.
Fig. 2.
Interactions of sex, age, BMI and lifestyle characteristics on associations between a 1 μg/m3 increment of PM1 and blood lipid levels. Abbreviations: CI, confidence interval; TC, total cholesterol; TG, triglyceride; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol. Covariates included age, sex, BMI, education, marital status, family income, smoking, alcohol drinking, high fat diet, adequate vegetable and fruit intake, physical activities and family history of dyslipidemia.
3.3. Associations between PM1 and dyslipidemias
Fig. 3 presents the associations between PM1 and dyslipidemias. In baseline and adjusted models, increased PM1 exposure was associated with increased risk of hypercholesterolemia, hyperbetalipoproteinemia and hypoalphalipoproteinemia, and reduced risk of dyslipidemia and hypertriglyceridemia (see Fig. 3 and Table S2 in the Supplements). In adjusted model, the odds ratio of dyslipidemia, hypercholesterolemia, hyperbetalipoproteinemia, hypoalphalipoproteinemia, and hypertriglyceridemia was 0.99 (95% CI: 0.97–0.99), 1.06 (95% CI: 1.04–1.08), 1.03 (95% CI: 1.02–1.05), 1.05 (95% CI: 1.03–1.07), and 0.92 (95% CI: 0.91–0.93), respectively.
Fig. 3.
Associations between per 1 μg/m3 increment of PM1 and dyslipidemias. Abbreviations: OR, odds ratio; CI, confidence interval. Baseline Model: Covariates included age, sex and BMI; Adjusted Model: Covariates included age, sex, BMI, education, marital status, family income, smoking, alcohol drinking, high fat diet, adequate vegetable and fruit intake, physical activities and family history of dyslipidemia.
Table 3 displays the interaction analyses between PM1 and dyslipidemias of sex, age, BMI and lifestyle characteristics. Similar to the associations between PM1 and blood lipid levels. Males were more susceptible to PM1 exposure than females. For example, compared with the effect of PM1 on hypercholesterolemia in females (OR = 1.04, 95% CI: 1.02–1.07), higher effect in males (OR = 1.11, 95% CI: 1.08–1.15) was observed. The effects of PM1 on dyslipidemia and hyperbetalipoproteinemia were significantly modified by age. The effect of PM1 on hyperbetalipoproteinemia among participants aged over 60 years old (OR = 1.08, 95% CI: 1.04–1.12) was higher than the effect on younger participants (≤45 years old) (OR = 1.01, 95% CI: 0.95–1.07). Additionally, associations between PM1 and hypertriglyceridemia among overweight and obese participants were slightly weaker than the other participants. Vegetable and fruit intake modified the associations of PM1 with hypercholesterolemia and hypertriglyceridemia.
Table 3.
Interactions of sex, age and BMI on associations between a 1 μg/m3 increment of PM1 and dyslipidemias.
| Dyslipidemia | Pinteraction | Hypercholesterolemia | Pinteraction | Hypertriglyceridemia | Pinteraction | Hypoalphalipo-proteinemia | Pinteraction | Hyperbetalipo-proteinemia | Pinteraction | |
|---|---|---|---|---|---|---|---|---|---|---|
| OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | ||||||
| Sex | ||||||||||
| Men | 1.03 (1.02, 1.05) | 1.11 (1.08, 1.15) | 0.96 (0.94, 0.98) | 1.05 (1.03, 1.07) | 1.10 (1.06, 1.13) | |||||
| Women | 0.96 (0.95, 0.97) | <0.001 | 1.04 (1.02, 1.07) | 0.001 | 0.91 (0.89, 0.92) | <0.001 | 1.03 (1.01, 1.05) | 0.097 | 1.03 (0.99, 1.05) | <0.001 |
| Age | ||||||||||
| <45 years | 1.00 (0.98, 1.03) | 1.05 (0.99, 1.11) | 0.94 (0.91, 0.97) | 1.04 (1.01, 1.07) | 1.01 (0.95, 1.07) | |||||
| 45–60 years | 0.97 (0.96, 0.99) | 0.035 | 1.03 (1.00, 1.07) | 0.618 | 0.92 (0.90, 0.94) | 0.300 | 1.04 (1.02, 1.06) | 0.859 | 1.02 (0.98, 1.05) | 0.808 |
| ≥60 years | 1.00 (0.99, 1.02) | 0.931 | 1.09 (1.06, 1.12) | 0.294 | 0.93 (0.91, 0.95) | 0.470 | 1.04 (1.02, 1.06) | 0.847 | 1.08 (1.05, 1.11) | 0.036 |
| BMI | ||||||||||
| <24 kg/m2 | 0.99 (0.97, 1.01) | 1.08 (1.05, 1.12) | 0.90 (0.88, 0.93) | 1.03 (1.00, 1.05) | 1.04 (1.01, 1.08) | |||||
| 24–28 kg/m2 | 0.99 (0.97, 1.00) | 0.733 | 1.06 (1.03, 1.09) | 0.406 | 0.93 (0.91, 0.95) | 0.116 | 1.04 (1.02, 1.06) | 0.558 | 1.04 (1.01, 1.07) | 0.897 |
| ≥28 kg/m2 | 0.99 (0.97, 1.02) | 0.942 | 1.04 (1.00, 1.09) | 0.179 | 0.95 (0.93, 0.97) | 0.006 | 1.05 (1.03, 1.08) | 0.147 | 1.08 (1.03, 1.12) | 0.231 |
| High fat diet | ||||||||||
| No | 0.99 (0.97, 0.99) | 1.06 (1.04, 1.08) | 0.92 (0.91, 0.94) | 1.04 (1.02, 1.05) | 1.05 (1.03, 1.07) | |||||
| Yes | 1.06 (0.98, 1.03) | 0.112 | 1.09 (1.04, 1.14) | 0.278 | 0.95 (0.92, 0.97) | 0.096 | 1.04 (1.01, 1.07) | 0.835 | 1.05 (1.00, 1.10) | 0.906 |
| Adequate vegetable and fruit intake | ||||||||||
| No | 1.00 (0.98, 1.01) | 1.04 (1.01, 1.06) | 0.95 (0.93, 0.96) | 1.04 (1.02, 1.06) | 1.05 (1.02, 1.08) | |||||
| Adequate | 0.98 (0.96, 0.99) | 0.092 | 1.11 (1.07, 1.15) | 0.001 | 0.90 (0.88, 0.92) | <0.001 | 1.04 (1.02, 1.06) | 0.859 | 1.06 (1.02, 1.09) | 0.692 |
Covariates included age, sex, BMI, education, marital status, family income, smoking, alcohol drinking, high fat diet, adequate vegetable and fruit intake, physical activities and family history of dyslipidemia.
3.4. Sensitivity analyses
Compared with the results of previous data analyses, associations of PM1 with blood lipid levels and dyslipidemias were consistent in sensitivity analyses (see Table S3 and Table S4 in the Supplements), where participants taking lipid lowering drugs and participants with diabetes were excluded, and 1-year and 5-year PM1 exposure were used. Table S3 and Table S4 showed the detailed results.
4. Discussion
This large-scale study on Chinese rural populations provides new evidence on adverse health effects of long-term PM1 exposure. In general, higher long-term PM1 exposure was associated with increased TC and LDL-C, and decreased TG and HDL-C. Higher PM1 exposure was associated with increased risk of hypercholesterolemia, hyperbetalipoproteinemia and hypoalphalipoproteinemia, while reduced risk of dyslipidemia and hypertriglyceridemia. Our stratified analyses suggested that males, older and overweight participants were more vulnerable to the adverse effects of PM1 exposure.
As PM1 is a major component of PM2.5, PM1 have similar adverse effects with PM2.5 on dyslipidemias and blood lipid levels. Compared with previous studies, the positive associations between PM, TC and LDL-C were almost accordant, but not the same. The current results were comparable but higher than Yang et al’ s findings (Yang et al., 2018a). They found every 1 μg/m3 increment in PM1 and PM2.5 corresponded to 0.16% (95% CI: 0.11%–0.20%) and 0.11% (95% CI: 0.08%–0.14%) increase in TC, 0.32% (95% CI: 0.26%–0.39%) and 0.29% (95% CI: 0.24%–0.35%) increase in LDL-C, and 0.14% (95% CI: 0.09%–0.18%) and 0.11% (95% CI: 0.08%–0.14%) decrease in HDL-C based on an urban population of northeast China, while our study showed that every 1 μg/m3 increase of PM1 was associated with 0.21% higher levels of TC and 0.75% of LDL-C, while 0.47% lower levels of HDL-C. This difference suggested that the rural population may be more vulnerable to PM1 than urban population. As far as we acknowledged, there were no other studies evaluated the associations between PM1 and blood lipids, and most studies focused on PM2.5. For example, the CATHGEN study in U.S. demonstrated that a 1 μg/m3 increment of PM2.5 was associated with an increase of 1.62%, 3.29%, and 1.70% in TC, TG, and LDL-C (McGuinn et al., 2019). Studies in the Europe (Sorensen et al., 2015) and Israel (Yitshak Sade et al., 2016) also observed that higher PM2.5 was associated with 0.78 mg/dL per 1 μg/m3 and 0.22% per 1 μg/m3 increased TC and LDL-C, respectively. A quantile regression analysis in U.S. suggested that participants with higher lipid levels were more vulnerable to adverse effects of PM2.5 (Bind et al., 2016).
However, findings on HDL-C and TG were inconsistent with previous studies. Some studies showed no associations between PM, HDL-C and risk of hypoalphalipoproteinemia (Shanley et al., 2016, Wallwork et al., 2017). However, some studies indicated that higher PM exposure was associated with lower HDL-C (Bell et al., 2017, Bind et al., 2016, Chuang et al., 2010). Wang et al. reported that 1 μg/m3 increment of PM10 was associated with 0.03% increase in HDL-C (Wang et al., 2018). In addition, our study indicated that a 1 μg/m3 increment in PM1 was associated with a 2.68% decrease levels of TG and decreased prevalence of hypertriglyceridemia (OR = 0.92, 95% CI: 0.91–0.93). However, McGuinn et al. (2019) demonstrated that 1 µg/m3 increment of PM2.5 corresponded to 3.29% increase of TG; while Yang et al. (2018a) reported no associations between PM1, TG and hypertriglyceridemia. Several reasons may explain these differences. First, different concentrations, sources and compositions of PM (e.g., ions, organic compound, minerals and reactive gasses) could lead to different effects (Valavanidis et al., 2008). For example, great disparities of PM pollution existed in different regions of China. The main sources of PM pollution were industrial, secondary inorganic aerosol and dust in the central of China, while that in north China were industrial, dust, and fossil fuel (Zhu et al., 2018). Second, differences in risk factor distributions among populations may account for these difference as well, such as nation, residence, lifestyle characteristics and health conditions (Cao et al., 2011). The subjects of our study were rural population. The intake of meat, dairy, eggs, fishes and shrimps intake in rural population was insufficient compared to urban population (Guo et al., 2017). In addition, the use of lipid-lowering drugs also can affect blood lipid levels. Recently a review showed that, as one of the most widely used lipid-lowering drugs in clinic, statins can significantly reduce greater levels of TC and LDL-C than TG (Awad et al., 2017). The species of lipid-lowering drugs may be a source of the associations between PM1 and TG while we did not collect the exact species of lipid-lowering drugs.
The mechanism of lipid metabolism and air pollution exposure remains unclear. Several potential biological pathways have been proposed from existing literature. Systemic inflammation and oxidative stress were linked to inhaled air pollution, resulting in altered lipoprotein metabolism and lipoprotein oxidation (Araujo et al., 2008, Shanley et al., 2016). Moreover, lipoprotein metabolism disorders in liver consequently emerged after inflammation of visceral adipose tissue (Poursafa et al., 2014). Experimental studies also observed that induction of systemic inflammation was linked to reduced anti-inflammatory capacity, cholesterol transport by HDL-C, and circulating adipokines (e.g. adiponectin, resistin and leptin) (Shanley et al., 2016, Xu et al., 2011a, Xu et al., 2011b, Yang et al., 2018a). Another possible mechanism is that inhaled air pollution was related to DNA methylation. A human intervention study in Shanghai provided robust human evidence that PM was associated with rapidly reduction of DNA methylation and consequently mediate its effects on cardiovascular biomarkers (Chen et al., 2016). Moreover, a cohort study in U.S. found associations between air pollution and genes methylation which were relevant to lipoprotein metabolism and systemic inflammation (Bind et al., 2014). Mendez et al.’s (Mendez et al., 2013) experimental study on mouse demonstrated that chronic inhalation exposure to PM2.5 caused up-regulation of genes related to lipogenesis, lipolysis, adipocyte differentiation, and lipid droplet formation (Mendez et al., 2013, Wallwork et al., 2017).
According to exist literature, various factors can modify the adverse effects of PM on blood lipid levels. Females were found to be more vulnerable to adverse effected of PM in previous studies, while the estimated effects in the current study among males were higher than females (Bell et al., 2017, Yang et al., 2018a). Vulnerabilities of biological and lifestyle characteristics between male and female might explain this difference. First, as most participants in our study were farmers. Male farmers were accustomed to have a longer outdoor working time and expose to more PM1 than females. Besides, Lelieveld et al. (2015) found that agriculture was an important anthropogenic source of outdoor air pollution category that contributing one-fifth premature mortality. Besides, previous literature revealed that inhaled air pollution can act as an exogenous hormones, activating estrogen-disrupting effects, and playing a crucial role in reactive oxygen species generating and oxidative stress inducting (Bell et al., 2017, Chen et al., 2013, Miller, 1994). In addition, males had a higher rate of smoking and drinking, which can cause higher risk of dyslipidemias. Overweight and obese individuals were found more susceptible to the effects of PM1 in our study. A multi-city analysis of PM had similar observation that the adverse effects of PM1 among overweight participants (BMI ≥ 25 kg/m2) were stronger (Yang et al., 2018a). Sun et al. (2009) reported similar results in an animal study that adipose inflammation and visceral adiposity were significantly increased in high-fat induced male mice exposed to PM2.5. Besides, our findings showed stronger adverse effects of PM1 were presented among elderly (P < 0.05). However, studies in U.S. and Denmark showed no modification effects of age on the association between PM and blood lipid levels (Shanley et al., 2016, Sorensen et al., 2015). Health services utilization may explain this difference. The elderly had a low level of local health services utilization in China, which may bring them in a vulnerable status to the adverse effects of air pollutants (Zhang et al., 2018b).
Dietary habits were found to be a major risk factor for cardiovascular disease and blood lipid levels. Unhealthy dietary habits increased the risk of developing dyslipidemia, such as consuming excessive amounts of sugar and fats. Our current study analyzed the interactions of dietary habits on PM1 with blood lipid levels and dyslipidemias. But surprisingly, high-fat diet can mitigate the associations of PM1 with TC and TG in our current study. The same association was reported in a Taiwanese study, Lin et al., (2019) found high-fat intake inversely correlated with high TC in unadjusted model, while the correlation became not statistically significant after adjustment for some lifestyle characteristics. Vegetable and fruit intake was found to be a modified factor as well. Studies showed that intake of fruit can alleviate the adverse health effects of air pollution, which was due to the rich content of vitamin C, carotenoids, and flavonoids in dietary fruit and vegetable, given the effects of antioxidants against inflammation and oxidative stress (Bowler and Crapo, 2002, Lin et al., 2017). Adequate vegetable and fruit intake modified the associations of PM1 with TG and LDL-C, but the correlations among PM1 and dyslipidemias were not statistically significant. Chinese people are accustomed to intake cooked vegetables, it was possible that some antioxidant components in the vegetables have been destroyed during the cooking process. Besides, our study collected insufficient information about vegetable and fruit consumption. Further studies are needed to explore the potential effects of high-fat diet and intake of fruit and vegetables for those exposed to PM1.
Some limitations in this study should be noted. First, a number of possible confounders were not controlled in this study, such as passive smoking, acute infection and inflammation (Nigam, 2011, Yang et al., 2018a). These information was not available in our study, which may affect the results. Second, we did not consider the effects of other air pollutants, as some air pollutants were highly correlated (Chen et al., 2017, Chen et al., 2012). Third, the concentrations of PM1 in our areas was comparatively concentrated, the IQR of PM1 was only 2.54 µg/m3. The sensitivity of residents in high-pollution areas often tended to be reduced as the adverse effects of PM among vulnerable subjects may have reached maximum level (Cao et al., 2011). In addition, although permanent residents who have signed informed consent were selected as participants, and those people who had moved within the 3 years were excluded before investigation, we do not acknowledge the exact move records of each individual over the past three years. Furthermore, the spatial resolution was not as accurate as models (1000 m × 1000 m and 500 m × 500 m) emerged in the last two years, which may cause measurement errors.
5. Conclusions
In summary, long-term exposure to high PM1 was associated with the changed blood lipid levels, as well as higher risk of hypercholesterolemia, hyperbetalipoproteinemia and hypoalphalipoproteinemia in Chinese rural populations. In particular, males, older and overweight participants were more vulnerable to the adverse effects of PM1. Our findings add new evidence on associations between PM1 exposure and cardiovascular diseases in rural population. Further longitudinal studies based on individual PM1 exposure are urgently warranted to verify our findings.
Funding
This work was supported by the Foundation of National Key Program of Research and Development of China (Grant No: 2016YFC0900803), National Natural Science Funding of China (Grant No. 81903279), the Bill & Melinda Gates Foundation (Grant No. OOP1148464), and the Natural Science Fund of Hubei Province (Grant No: 2018CFB634). Dr. Guo is supported by Career Development Fellowship APP1107107 from the Australian National Health and Medical Research Council (NHMRC). Dr. Li is supported by Early Career Fellowship APP1109193 from the Australian NHMRC.
CRediT authorship contribution statement
Shuyuan Mao: Methodology, Formal analysis, Writing - original draft, Visualization. Shanshan Li: Resources, Data curation, Funding acquisition. Chongjian Wang: Investigation, Data curation, Project administration, Funding acquisition. Yisi Liu: Validation, Writing - review & editing. Na Li: Methodology, Software. Feifei Liu: Methodology, Software. Shuqiong Huang: Validation, Supervision. Suyang Liu: Validation, Supervision. Yuanan Lu: Validation, Supervision. Zhenxing Mao: Investigation, Resources, Data curation. Wenqian Huo: Investigation, Resources, Data curation. Gongbo Chen: Methodology, Formal analysis, Funding acquisition. Hao Xiang: Conceptualization, Methodology, Writing - review & editing, Funding acquisition. Yuming Guo: Resources, Writing - review & editing, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors acknowledge the cooperation of all the participants, staff and administrators of this study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envint.2020.105637.
Contributor Information
Gongbo Chen, Email: chen.gongbo@whu.edu.cn.
Hao Xiang, Email: xianghao@whu.edu.cn.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- Anderson K.M., Castelli W.P., Levy D. Cholesterol and mortality. 30 years of follow-up from the Framingham study. JAMA. 1987;257:2176–2180. doi: 10.1001/jama.257.16.2176. [DOI] [PubMed] [Google Scholar]
- Araujo J.A., Barajas B., Kleinman M., Wang X., Bennett B.J., Gong K.W., Navab M., Harkema J., Sioutas C., Lusis A.J., Nel A.E. Ambient particulate pollutants in the ultrafine range promote early atherosclerosis and systemic oxidative stress. Circ. Res. 2008;102:589–596. doi: 10.1161/CIRCRESAHA.107.164970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Awad K., Mikhailidis D.P., Toth P.P., Jones S.R., Moriarty P., Lip G.Y.H., Muntner P., Catapano A.L., Pencina M.J., Rosenson R.S., Rysz J., Banach M., Lipid, Blood Pressure Meta-analysis Collaboration, G. Efficacy and safety of alternate-day versus daily dosing of statins: a systematic review and meta-analysis. Cardiovasc. Drugs Ther. 2017;31:419–431. doi: 10.1007/s10557-017-6743-0. [DOI] [PubMed] [Google Scholar]
- Bell G., Mora S., Greenland P., Tsai M., Gill E., Kaufman J.D. Association of air pollution exposures with high-density lipoprotein cholesterol and particle number: the multi-ethnic study of atherosclerosis. Arterioscler. Throm. Vas. Biol. 2017;37:976–982. doi: 10.1161/ATVBAHA.116.308193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bind M.A., Lepeule J., Zanobetti A., Gasparrini A., Baccarelli A., Coull B.A., Tarantini L., Vokonas P.S., Koutrakis P., Schwartz J. Air pollution and gene-specific methylation in the Normative Aging Study: association, effect modification, and mediation analysis. Epigenetics. 2014;9:448–458. doi: 10.4161/epi.27584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bind M.A., Peters A., Koutrakis P., Coull B., Vokonas P., Schwartz J. Quantile regression analysis of the distributional effects of air pollution on blood pressure, heart rate variability, blood lipids, and biomarkers of inflammation in elderly American men: the normative aging study. Environ. Health Perspect. 2016;124:1189–1198. doi: 10.1289/ehp.1510044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowler R.P., Crapo J.D. Oxidative stress in airways: is there a role for extracellular superoxide dismutase? Am. J. Respir. Crit. Care Med. 2002;166:S38–43. doi: 10.1164/rccm.2206014. [DOI] [PubMed] [Google Scholar]
- Brown D.M., Wilson M.R., MacNee W., Stone V., Donaldson K. Size-dependent proinflammatory effects of ultrafine polystyrene particles: a role for surface area and oxidative stress in the enhanced activity of ultrafines. Toxicol. Appl. Pharmacol. 2001;175:191–199. doi: 10.1006/taap.2001.9240. [DOI] [PubMed] [Google Scholar]
- Cao J., Yang C., Li J., Chen R., Chen B., Gu D., Kan H. Association between long-term exposure to outdoor air pollution and mortality in China: a cohort study. J. Hazard. Mater. 2011;186:1594–1600. doi: 10.1016/j.jhazmat.2010.12.036. [DOI] [PubMed] [Google Scholar]
- Chen G., Knibbs L.D., Zhang W., Li S., Cao W., Guo J., Ren H., Wang B., Wang H., Williams G., Hamm N.A.S., Guo Y. Estimating spatiotemporal distribution of PM1 concentrations in China with satellite remote sensing, meteorology, and land use information. Environ. Pollut. 2018;233:1086–1094. doi: 10.1016/j.envpol.2017.10.011. [DOI] [PubMed] [Google Scholar]
- Chen G., Li S., Zhang Y., Zhang W., Li D., Wei X., He Y., Bell M.L., Williams G., Marks G.B., Jalaludin B., Abramson M.J., Guo Y. Effects of ambient PM 1 air pollution on daily emergency hospital visits in China: an epidemiological study. Lancet Planet. Health. 2017;1:e221–e229. doi: 10.1016/S2542-5196(17)30100-6. [DOI] [PubMed] [Google Scholar]
- Chen G., Morawska L., Zhang W., Li S., Cao W., Ren H., Wang B., Wang H., Knibbs L.D., Williams G., Guo J., Guo Y. Spatiotemporal variation of PM1 pollution in China. Atmos. Environ. 2018;178:198–205. [Google Scholar]
- Chen R., Kan H., Chen B., Huang W., Bai Z., Song G., Pan G., Group C.C. Association of particulate air pollution with daily mortality: the China Air Pollution and Health Effects Study. Am. J. Epidemiol. 2012;175:1173–1181. doi: 10.1093/aje/kwr425. [DOI] [PubMed] [Google Scholar]
- Chen R., Meng X., Zhao A., Wang C., Yang C., Li H., Cai J., Zhao Z., Kan H. DNA hypomethylation and its mediation in the effects of fine particulate air pollution on cardiovascular biomarkers: a randomized crossover trial. Environ. Int. 2016;94:614–619. doi: 10.1016/j.envint.2016.06.026. [DOI] [PubMed] [Google Scholar]
- Chen S.T., Lin C.C., Liu Y.S., Lin C., Hung P.T., Jao C.W., Lin P.H. Airborne particulate collected from central Taiwan induces DNA strand breaks, Poly(ADP-ribose) polymerase-1 activation, and estrogen-disrupting activity in human breast carcinoma cell lines. J. Environ. Sci. Health. 2013;48:173–181. doi: 10.1080/10934529.2012.717809. [DOI] [PubMed] [Google Scholar]
- Chuang K.J., Yan Y.H., Cheng T.J. Effect of air pollution on blood pressure, blood lipids, and blood sugar: a population-based approach. J. Occup. Environ. Med. 2010;52:258–262. doi: 10.1097/JOM.0b013e3181ceff7a. [DOI] [PubMed] [Google Scholar]
- Delfino R.J., Staimer N., Vaziri N.D. Air pollution and circulating biomarkers of oxidative stress. Air Qual. Atmos. Health. 2011;4:37–52. doi: 10.1007/s11869-010-0095-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD, 2018. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet (London, England) 392, 1923–1994. [DOI] [PMC free article] [PubMed]
- Guo Q.Y., Zhao L.Y., He Y.N., Fang Y.H., Fang H.Y., Xu X.L., Jia F.M., Yu D.M. Survey on dietary nutrients intake of Chinese residents between 2010 and 2012. Chinese J. Epidemiol. 2017;51:519–522. doi: 10.3760/cma.j.issn.0253-9624.2017.06.012. [DOI] [PubMed] [Google Scholar]
- Joint Committee for Developing Chinese Guidelines on Prevention and Treatment of Dyslipidemia in Adults, 2007. Chinese guidelines on prevention and treatment of dyslipidemia in adults. Chinese J. Epidemiol. 35, 390–419. [PubMed]
- Lelieveld J., Evans J.S., Fnais M., Giannadaki D., Pozzer A. The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature. 2015;525:367–371. doi: 10.1038/nature15371. [DOI] [PubMed] [Google Scholar]
- Li X., Deng Y., Tang W., Sun Q., Chen Y., Yang C., Yan B., Wang Y., Wang J., Wang S., Yang F., Ding Y., Zhao G., Cao G. Urban-rural disparity in cancer incidence, mortality, and survivals in Shanghai, China, During 2002 and 2015. Front. Oncol. 2018;8:579. doi: 10.3389/fonc.2018.00579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin H., Guo Y., Zheng Y., Di Q., Liu T., Xiao J., Li X., Zeng W., Cummings-Vaughn L.A., Howard S.W., Vaughn M.G., Qian Z.M., Ma W., Wu F. Long-term effects of ambient PM2.5 on hypertension and blood pressure and attributable risk among older Chinese adults. Hypertension. 2017;69:806–812. doi: 10.1161/HYPERTENSIONAHA.116.08839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin L.Y., Hsu C.Y., Lee H.A., Wang W.H., Kurniawan A.L., Chao J.C. Dietary patterns in relation to components of dyslipidemia and fasting plasma glucose in adults with dyslipidemia and elevated fasting plasma glucose in Taiwan. Nutrients. 2019:11. doi: 10.3390/nu11040845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Zhao D., Qin L., Wang W., Wu G., Zeng Z., Wang W., Wu Z. Association of low density lipoprotein cholesterol with cardiovascular disease in a prospective study. Chin. J. Cardiol. 2001;29:561–565. [Google Scholar]
- Liu X., Li N., Liu C., Ren X., Liu D., Gao B., Liu Y. Urban-rural disparity in utilization of preventive care services in China. Medicine (Baltimore) 2016;95 doi: 10.1097/MD.0000000000004783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Mao Z., Li Y., Wu W., Zhang X., Huo W., Yu S., Shen L., Li L., Tu R., Wu H., Li H., He M., Liu L., Wei S., Li W., Wu T., Wang C. The Henan Rural Cohort: a prospective study of chronic non-communicable diseases. Int. J. Epidemiol. 2019 doi: 10.1093/ije/dyz039. [DOI] [PubMed] [Google Scholar]
- Liu X., Yu S., Mao Z., Li Y., Zhang H., Yang K., Zhang H., Liu R., Qian X., Li L., Bie R., Wang C. Dyslipidemia prevalence, awareness, treatment, control, and risk factors in Chinese rural population: the Henan rural cohort study. Lipids Health Dis. 2018;17:119. doi: 10.1186/s12944-018-0768-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longde W. People's Medical Publishing House; Beijing, China: 2005. The 2002 China National Nutrition and Health Survey(1): General Report eds. [Google Scholar]
- McGuinn L.A., Schneider A., McGarrah R.W., Ward-Caviness C., Neas L.M., Di Q., Schwartz J., Hauser E.R., Kraus W.E., Cascio W.E., Diaz-Sanchez D., Devlin R.B. Association of long-term PM2.5 exposure with traditional and novel lipid measures related to cardiovascular disease risk. Environ. Int. 2019;122:193–200. doi: 10.1016/j.envint.2018.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendez R., Zheng Z., Fan Z., Rajagopalan S., Sun Q., Zhang K. Exposure to fine airborne particulate matter induces macrophage infiltration, unfolded protein response, and lipid deposition in white adipose tissue. Am. J. Translational Res. 2013;5:224–234. [PMC free article] [PubMed] [Google Scholar]
- Miller V.T. Lipids, lipoproteins, women and cardiovascular disease. Atherosclerosis. 1994;108:S73–S82. doi: 10.1016/0021-9150(94)90154-6. [DOI] [PubMed] [Google Scholar]
- Nigam P.K. Serum lipid profile: fasting or non-fasting? Indian J. Clin. Biochem. 2011;26:96–97. doi: 10.1007/s12291-010-0095-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poursafa P., Mansourian M., Motlagh M.E., Ardalan G., Kelishadi R. Is air quality index associated with cardiometabolic risk factors in adolescents? The CASPIAN-III Study. Environ. Res. 2014;134:105–109. doi: 10.1016/j.envres.2014.07.010. [DOI] [PubMed] [Google Scholar]
- Shanley R.P., Hayes R.B., Cromar K.R., Ito K., Gordon T., Ahn J. Particulate air pollution and clinical cardiovascular disease risk factors. Epidemiology. 2016;27:291–298. doi: 10.1097/EDE.0000000000000426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen M., Hjortebjerg D., Eriksen K.T., Ketzel M., Tjonneland A., Overvad K., Raaschou-Nielsen O. Exposure to long-term air pollution and road traffic noise in relation to cholesterol: a cross-sectional study. Environ. Int. 2015;85:238–243. doi: 10.1016/j.envint.2015.09.021. [DOI] [PubMed] [Google Scholar]
- Sun Q., Yue P., Deiuliis J.A., Lumeng C.N., Kampfrath T., Mikolaj M.B., Cai Y., Ostrowski M.C., Lu B., Parthasarathy S., Brook R.D., Moffatt-Bruce S.D., Chen L.C., Rajagopalan S. Ambient air pollution exaggerates adipose inflammation and insulin resistance in a mouse model of diet-induced obesity. Circulation. 2009;119:538–546. doi: 10.1161/CIRCULATIONAHA.108.799015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian Z., Li Y., Mao Z., Yu S., Wang Y., Liu X., Tu R., Zhang H., Qian X., Zhang X., Zhang L., Zhao J., Yin L., Wang C. Sex-specific relationship between visceral fat index and dyslipidemia in Chinese rural adults: The Henan Rural Cohort Study. Prev. Med. 2018;116:104–111. doi: 10.1016/j.ypmed.2018.09.009. [DOI] [PubMed] [Google Scholar]
- Tirschwell D.L., Smith N.L., Heckbert S.R., Lemaitre R.N., Longstreth W.T., Jr., Psaty B.M. Association of cholesterol with stroke risk varies in stroke subtypes and patient subgroups. Neurology. 2004;63:1868–1875. doi: 10.1212/01.wnl.0000144282.42222.da. [DOI] [PubMed] [Google Scholar]
- Valavanidis A., Fiotakis K., Vlachogianni T. Airborne particulate matter and human health: toxicological assessment and importance of size and composition of particles for oxidative damage and carcinogenic mechanisms. J. Environ. Sci. Health C Environ. Carcinog. Ecotoxicol. Rev. 2008;26:339–362. doi: 10.1080/10590500802494538. [DOI] [PubMed] [Google Scholar]
- Wallwork R.S., Colicino E., Zhong J., Kloog I., Coull B.A., Vokonas P., Schwartz J.D., Baccarelli A.A. Ambient fine particulate matter, outdoor temperature, and risk of metabolic syndrome. Am. J. Epidemiol. 2017;185:30–39. doi: 10.1093/aje/kww157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M., Zheng S., Nie Y., Weng J., Cheng N., Hu X., Ren X., Pei H., Bai Y. Association between short-term exposure to air pollution and dyslipidemias among type 2 diabetic patients in Northwest China: a population-based study. Int. J. Environ. Res. Public Health. 2018;15:631. doi: 10.3390/ijerph15040631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu X., Liu C., Xu Z., Tzan K., Zhong M., Wang A., Lippmann M., Chen L.C., Rajagopalan S., Sun Q. Long-term exposure to ambient fine particulate pollution induces insulin resistance and mitochondrial alteration in adipose tissue. Toxicol. Sci. 2011;124:88–98. doi: 10.1093/toxsci/kfr211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Z., Xu X., Zhong M., Hotchkiss I.P., Lewandowski R.P., Wagner J.G., Bramble L.A., Yang Y., Wang A., Harkema J.R., Lippmann M., Rajagopalan S., Chen L.C., Sun Q. Ambient particulate air pollution induces oxidative stress and alterations of mitochondria and gene expression in brown and white adipose tissues. Part. Fibre Toxicol. 2011;8:20. doi: 10.1186/1743-8977-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang B.Y., Bloom M.S., Markevych I., Qian Z.M., Vaughn M.G., Cummings-Vaughn L.A., Li S., Chen G., Bowatte G., Perret J.L., Dharmage S.C., Heinrich J., Yim S.H., Lin S., Tian L., Yang M., Liu K.K., Zeng X.W., Hu L.W., Guo Y., Dong G.H. Exposure to ambient air pollution and blood lipids in adults: the 33 communities Chinese health study. Environ. Int. 2018;119:485–492. doi: 10.1016/j.envint.2018.07.016. [DOI] [PubMed] [Google Scholar]
- Yang B.Y., Guo Y., Bloom M.S., Xiao X., Qian Z.M., Liu E., Howard S.W., Zhao T., Wang S.Q., Li S., Chen D.H., Ma H., Yim S.H., Liu K.K., Zeng X.W., Hu L.W., Liu R.Q., Feng D., Yang M., Xu S.L., Dong G.H. Ambient PM1 air pollution, blood pressure, and hypertension: Insights from the 33 communities Chinese Health Study. Environ. Res. 2018;170:252–259. doi: 10.1016/j.envres.2018.12.047. [DOI] [PubMed] [Google Scholar]
- Yang B.Y., Qian Z.M., Li S., Fan S., Chen G., Syberg K.M., Xian H., Wang S.Q., Ma H., Chen D.H., Yang M., Liu K.K., Zeng X.W., Hu L.W., Guo Y., Dong G.H. Long-term exposure to ambient air pollution (including PM1) and metabolic syndrome: the 33 communities Chinese Health Study (33CCHS) Environ. Res. 2018;164:204–211. doi: 10.1016/j.envres.2018.02.029. [DOI] [PubMed] [Google Scholar]
- Yeatts K., Svendsen E., Creason J., Alexis N., Herbst M., Scott J., Kupper L., Williams R., Neas L., Cascio W., Devlin R.B., Peden D.B. Coarse particulate matter (PM2.5-10) affects heart rate variability, blood lipids, and circulating eosinophils in adults with asthma. Environ. Health Perspect. 2007;115:709–714. doi: 10.1289/ehp.9499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yitshak Sade M., Kloog I., Liberty I.F., Schwartz J., Novack V. The association between air pollution exposure and glucose and lipids levels. J. Clin. Endocrinol. Metab. 2016;101:2460–2467. doi: 10.1210/jc.2016-1378. [DOI] [PubMed] [Google Scholar]
- Zhang M., Deng Q., Wang L., Huang Z., Zhou M., Li Y., Zhao Z., Zhang Y., Wang L. Prevalence of dyslipidemia and achievement of low-density lipoprotein cholesterol targets in Chinese adults: a nationally representative survey of 163,641 adults. Int. J. Cardiol. 2018;260:196–203. doi: 10.1016/j.ijcard.2017.12.069. [DOI] [PubMed] [Google Scholar]
- Zhang X., Yu B., He T., Wang P. Status and determinants of health services utilization among elderly migrants in China. Global Health Res. Policy. 2018;3:8. doi: 10.1186/s41256-018-0064-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Huang L., Li J., Ying Q., Zhang H., Liu X., Liao H., Li N., Liu Z., Mao Y., Fang H., Hu J. Sources of particulate matter in China: Insights from source apportionment studies published in 1987–2017. Environ. Int. 2018;115:343–357. doi: 10.1016/j.envint.2018.03.037. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.