Abstract
Background
The incidence of knife-related injuries is rising across the UK. This study aimed to determine the spectrum of knife-related injuries in a major UK city, with regards to patient and injury characteristics. A secondary aim was to quantify their impact on secondary care resources.
Methods
Observational study of patients aged 16+ years admitted to a major trauma centre following knife-related injuries resulting from interpersonal violence (May 2015 to April 2018). Patients were identified using Emergency Department and discharge coding, blood bank and UK national Trauma Audit and Research prospective registries. Patient and injury characteristics, outcome and resource utilisation were collected from ambulance and hospital records.
Findings
532 patients were identified; 93% male, median age 26 years (IQR 20–35). Median injury severity score was 9 (IQR 3–13). 346 (65%) underwent surgery; 133 (25%) required intensive care; 95 (17·9%) received blood transfusion. Median length of stay was 3·3 days (IQR 1·7–6·0). In-hospital mortality was 10/532 (1·9%). 98 patients (18·5%) had previous attendance with violence-related injuries. 24/37 females (64·9%) were injured in a domestic setting. Intoxication with alcohol (19·2%) and illicit drugs (17·6%) was common. Causative weapon was household knife in 9%, knife (other/unspecified) in 38·0%, machete in 13·9%, small folding blade (2·8%) and, unrecorded in 36·3%.
Interpretation
Knife injuries constitute 12·9% of trauma team workload. Violence recidivism and intoxication are common, and females are predominantly injured in a domestic setting, presenting opportunities for targeted violence reduction interventions. 13·9% of injuries involved machetes, with implications for law enforcement strategies.
Research in context.
Evidence before this study
The incidence of knife-related injuries has recently risen dramatically in the United Kingdom, particularly in urban centres outside of London.
Added value of this study
This study provides a comprehensive description of patient and injury characteristics; recent increases in admissions due to knife injuries occurred in males under 25 years of age. Nearly one in five patients are recidivists and female knife-injured patients are most likely to be injured in a setting of domestic violence. One in five of our study population required involvement of cardiothoracic surgeons. Limb injuries, whilst not often life threatening, consume significant resources including substantial emergency operating theatre utilisation. A comprehensive breakdown of weapons is presented, demonstrating that 14% of injuries were attributable to machetes, possibly associated with gang-related criminal activity. The national TARN registry recognised fewer than half of knife-related admissions.
Implications of all the available evidence
These data can inform resource planning within Major Trauma Centres and networks. The frequency of thoracic stabbing injuries should mandate co-location of cardiothoracic services within MTCs. Healthcare-based research with specific data capture has identified opportunities for targeted injury prevention, particularly recidivism and intimate partner violence prevention. Health workers must engage with law enforcement strategies as part of a multi-agency effort to combat the recent surge in knife-related crime. Development of a regional or national registry encompassing all knife injuries is strongly warranted in order to objectively report prevalence and trends and measure the impact of injury prevention strategies.
Alt-text: Unlabelled box
1. Introduction
Knife-related incidents are a significant public and political concern in the UK. Across England and Wales, in the year ending March 2019, there were 47,136 recorded offences involving a knife; the highest figure since recording began in 1946 [1]. The West Midlands has the fourth highest national rate of crime involving a knife or sharp instrument (111 per 100,000 population) [1]. Although knives and sharp objects account for the greatest proportion (39–45%) of homicides in the UK, the true burden of injury is more obscure [2]. The rise in knife crime is multifactorial. Contributory factors are thought to include income inequality and deprivation, school exclusion, adverse childhood environments and changes in the illicit drug trade [3,4]. Police data demonstrate a national upward trend with all forms of violent crime; knife injuries account for only 4% of violence with injury but are associated with significantly higher mortality [1,5]. UK in-hospital mortality from knife injuries ranges between 0·5–8%, with deaths most commonly attributable to penetrating cardiac injuries [6], [7], [8], [9]. Crucially, the incidence of knife crime appears to be rising despite considerable efforts at injury prevention.
The only national infrastructure that records knife-related injuries is the national Trauma Audit and Research Network (TARN) registry, with a focus on severe or multisystem injuries [10]. No UK organisation makes publicly available a breakdown of the type of knives implicated in injuries, limiting evidence-based approaches to reducing knife-related violence. Several media reports cite machetes as the causative weapon in knife assaults, but the true incidence of their use in unknown [11,12]. In the UK, studies pertaining to knife injuries have largely been based in inner city London and the extent to which these findings are generalisable in other large urban areas, such as the Midlands and North of England, is unclear [9,13,14]. Studies indicate that assaults involving knives typically affect young men living in deprived, urban areas [6,13,15]. A public health approach to knife crime has been advocated on the basis that there are identifiable demographic and social risk factors, which may be amenable to intervention [16]. Government has proposed the imposition of Knife Crime Prevention Orders, involving a supervised programme of preventive rather than punitive measures [17]. This will include some prohibitions, such as a curfew, geographical and restriction of association, as well as positive elements such as educational courses, life skills programmes and targeted interventions [7,18]. There remains an urgent need to identify opportunities for targeted injury prevention and law enforcement strategies as part of a multi-agency effort to reduce knife injuries.
It is estimated that violence costs the NHS £2·9 billion a year [13,16]. Indirect costs are much greater, including loss of psychological and social function to the individual, diminished community cohesion and, loss of economic productivity. A better understanding of knife-related injuries and the patients affected could facilitate targeted injury prevention strategies and aid resource planning within trauma systems of care. This study aimed to collate the epidemiological characteristics of knife-related injuries in order to further our understanding of knife crime victims. A secondary aim was to quantify the burden of knife injuries on Major Trauma Centre (MTC) resources.
2. Methods
This single-centre, observational study was designed and reported according to STROBE guidance for observational studies. Inclusion criteria were consecutive patients who required hospital admission, or died within the Emergency Department (ED), following injury with a knife as a result of interpersonal violence within a three year period (May 2015 to April 2018). A knife is defined as a cutting instrument typically in the form of a blade fitted into a handle or into machinery [19]. Patients admitted following accidental or self-inflicted knife wounds were excluded. The setting is an urban MTC in Birmingham, UK, representing the highest tier of trauma care for all patients aged 16 years and above, within a regional trauma network. The centre receives patients living within its locality, as well as those who trigger the pre-hospital Major Trauma Triage Tool across a region encompassing a population of 2·44 million [20]. Those aged under 16 years are served by a separate paediatric regional MTC.
Patients were identified using three sources. The TARN database includes consecutive patients who attend hospital after sustaining injury who meet any of the following criteria: hospital length of stay greater than 72 h, admission to intensive care or in-hospital mortality. After meeting inclusion criteria, a hospital-based TARN audit co-ordinator will record prospectively collected variables into a standardised, web-based case record form including demographic, injury-related and outcome parameters. For these TARN-eligible patients, injury descriptions are coded centrally by TARN using the Abbreviated Injury Score (determined using manual AIS2005, Updated 2008), allowing calculation of Injury Severity Score (ISS). Additionally, the hospital's blood bank maintains a prospective log of all massive transfusion protocol (MTP) activations; this log was perused to identify any trauma patients presenting within the three-year period, followed by screening of their medical records for eligibility. Furthermore, patients who attended the ED or the hospital with the discharge code “knife/sharp instrument” were identified retrospectively via the Hospital Informatics system and medical records were screened for eligibility.
Demographic and clinical data were collected from ambulance and hospital electronic medical records by four investigators and abstracted directly into a single, standardized Excel spreadsheet, monitored by one investigator. Definitions for each variable were agreed upon prior to data abstraction. Where conflicting data were found or doubt existed, these were checked by a second investigator. The following variables were recorded: age, gender, mode of arrival, incident location, circumstances of assault, time of presentation to ED, psychiatric and medical history including pregnancy, alcohol intoxication, declared use of recreational drugs and/or drug-dependence at the time of attendance. Weapon description was categorised to reflect legality as per English law and relative availability: a folding blade of three inches long or less, which is legal to possess; household knife; knife (other/unspecified) and machete. A note was made when precise weapon description was not recorded in the medical records. Folding blades of three inches or less were recognised by their common names “pen knife,” “flick knife” and “switch blade.” A machete is defined as a long heavy broad-bladed knife used as a weapon or cutting tool [19].
Previous or subsequent attendance at our ED with violence-related injuries during the period 1 April 2012 and 1 January 2019 was noted. Clinical data and resource utilisation were recorded including: trauma pre-alert; hypotension on arrival in ED (SBP<110); MTP activation; receipt of blood transfusion; number and duration of operations (knife-to-skin time); specialties involved in inpatient care; ICU admission; survival to discharge, length of stay. Co-morbidities were categorised using the Charlson Comorbidity Index. For patients who did not meet TARN eligibility criteria, Injury Severity Score was calculated by a single investigator trained in coding, using the Abbreviated Injury Score manual (AIS2005, Updated 2008). The 12-month periods were aligned with our institution's financial year to facilitate interpretation of resource utilisation. The actual cost to the hospital of the index admission was obtained, as calculated directly by the hospital costings department (not involving tariff codes). World Health Organisation age categories were applied, including late adolescence (16–19 years) and young adulthood (20–24 years) [21]. As a registered hospital audit, no further ethical approval was required.
2.1. Data analyses
Data were collected using Microsoft Excel V·15·3 (Microsoft, California, USA) and analysed using R v3·6·1 software (R Core Team, Auckland, New Zealand, 2000). Continuous data are presented as medians and interquartile ranges (IQR) and categorical data are presented as frequencies (n) and percentages. Risk ratios and associated 95% confidence intervals and p-values were obtained using unadjusted log-binomial regression models, assessing the likelihood of sustaining injury in a domestic setting for female compared with male patients. The relationship between body region and weapon type and associated 95% confidence intervals was assessed using unadjusted log-linear multinomial regression models. The p-value for the relationship between body region and weapon type was obtained through a Monte Carlo simulation of Fisher's exact test due to small cell frequencies. The relationships between weapon type and ISS and associated 95% confidence intervals and p-values were assessed using unadjusted linear regression models.
2.2. Role of funding
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
2.3. Data sharing statement
De-identified participant data may be requested via email from the corresponding author following publication (nabeelamalik@nhs.net).
2.4. Patient consent
Not required.
2.5. Ethics approval
Not required, project registered with the Hospital Audit Department.
3. Results
3.1. Epidemiology of violence-related knife injuries
532 patients were admitted to hospital following a knife injury as a result of interpersonal violence during the three year period. TARN identified 225 of these (42·2%). Of the 532 patients, 495 (93·0%) were male. Median age was 26 years (IQR 20–35). Most patients (86%) had no significant co-morbidity with a median Charlson Co-morbidity score of 0 (IQR 0–0).
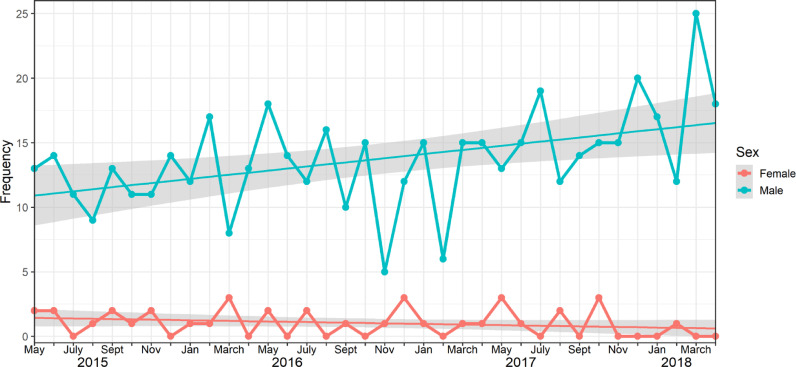
Patient and injury characteristics are summarised in Table 1. A rise in annual incidence was seen over the three-year period studied, with the increase accounted for by those aged 16–25 years (Fig. 1). A specific pattern of variation by month of the year was observed in male patients, with a peak in the months of May to July in each year and a trough in February. The incidence of knife injuries amongst females did not rise over the three-year period (Fig. 2). Patients were injured in a domestic setting in 87 (16·4%) cases. Female patients were injured in a domestic setting in 24 (64·9%) cases (p<0·0001, Fisher's Exact test). 6 of the 37 (16·2%) females presented during pregnancy, all of whom were injured in a domestic setting. The relative risk ratio of sustaining injury in a domestic setting for female patients compared to male patients was 5·1 (95% CI: 3·6 to 7·0).
Table 1.
Patient and injury characteristics.
| n | % | ||
|---|---|---|---|
| Gender | Male | 495 | 93·0 |
| Female | 37 | 7·0 | |
| Missing | 0 | 0·0 | |
| Age (years), median (IQR) | 26 (20, 35) | ||
| Previous ED attendance due to interpersonal violence* | Yes | 98 | 18·5 |
| No | 434 | 81·5 | |
| Missing | 0 | 0·0 | |
| Alcohol intoxication at presentation | Yes | 102 | 19·2 |
| No | 65 | 12·2 | |
| Missing | 365 | 68·6 | |
| History of illicit drug use at presentation and/or known drug dependence. | Yes | 95 | 17·6 |
| No | 58 | 10·9 | |
| Missing | 379 | 71·2 | |
| Drug used: n,% | Cannabinoids | 22 | 4·9 |
| Cocaine | 9 | 1·7 | |
| Heroin | 25 | 4·7 | |
| Combined Opiates | 9 | 1·7 | |
| Unspecified | 30 | 5·7 | |
| Charlson Co-morbidity Index | 0 | 458 | 86·0 |
| 1 | 67 | 12·6 | |
| ≥2 | 7 | 1·0 | |
| Missing | 0 | 0·0 | |
| Psychiatric history (as per ED notes) | Yes | 84 | 15·8 |
| No | 409 | 76·9 | |
| Missing | 39 | 7·3 | |
| Psychiatric diagnoses: n,% | Schizophrenia | 9 | 0·2 |
| Depression | 32 | 6·1 | |
| Mixed anxiety and depressive disorder | 9 | 0·2 | |
| Anxiety (including agoraphobia) | 5 | 0·9 | |
| Other/unspecified | 6 | 1·2 | |
| Causative weapon | Household knife | 48 | 9·0 |
| Knife (other/unspecified) | 202 | 38·0 | |
| Machete | 74 | 13·9 | |
| Folding blade ≤ 3 inches | 15 | 2·8 | |
| Not recorded | 193 | 36·3 | |
| Injured in a domestic setting | Yes | 87 | 16·4 |
| No | 274 | 51·5 | |
| Missing | 171 | 32·1 | |
| By Gender | |||
| Male | 63/495 | 12·7 | |
| Females | 24/37 | 64·9% |
with blunt or penetrating injuries, between 1 April 2012 – 1 Jan 2019.
Fig. 1.
Incidence of knife-related injuries over three years, including age category.
Fig. 2.
Variation in presentation to ED by month over the three-year period.
Weapon descriptions were documented in patient records in 63·7% of cases. The most common weapon implicated was a “knife” (38%) with no further descriptive details. The second most common was machete, accounting for 13·9% of cases. 18·4% of patients had attended our ED previously or subsequently with blunt or penetrating violence-related injuries. Patients presented to ED on every day of the week, with 378 (71%) patients presenting between 7pm and 7am (Fig. 3). 243 (46%) presented between 7pm on Friday and 7am on Monday morning. Alcohol intoxication was reported in 19·2% of patients and 17.6% of patients reported illicit drug use, with the most common drug cited as heroin.
Fig. 3.
Time of presentation to ED with a knife injury: Variation by time of day and day of the week.
3.2. Clinical characteristics, outcome and impact on MTC resources
Over the three year study period, there were 342,560 ED attendances, of which 3354 (1%) received trauma team activation. Trauma team activation occurred in 431/532 (81%), constituting 12·9% of the workload of our major trauma team. This figure does not include self-inflicted and accidental knife injuries, or penetrating trauma of other aetiology. In-hospital mortality was 1·9% (10/532), all were male. Five (50%) of these died from knife injuries to the thorax, four of whom underwent resuscitative thoracotomy prior to arriving in hospital. The remainder of patients died of haemorrhage from abdominal injuries (3 cases) and injury to the neck (2 cases). In 7/10 deaths, the precise causative weapon was unknown. All fatalities were captured by TARN and, as such, mortality amongst the TARN eligible patients was 4·4%.
Hypotension (SBP<110 mmHg) was present in 245 patients (46%). The MTP was activated in 99 patients (18·6%). Ninety-five (17·9%) received blood transfusion. Median Injury Severity Score (ISS) was 9 (IQR 3–12). A detailed breakdown of resource utilisation per body region injured is presented in Table 2. In 22% of cases, patients presented with injuries that were isolated to the limb(s), these patients had the lowest average injury severity (median ISS 4, IQR 1–7) and shortest length of stay (median LOS 2 days, IQR 1·3–3·8) however they required more operations per patient (median of 1·0 operations per patient, IQR 1·0–1·0) compared to patients with injuries isolated to the abdomen and thorax. Four in ten patients presented with multiple body regions injured. The highest ISS occurred in patients with thoracic injuries (median ISS 9, IQR 9–16) and those with multiple body regions injured (median ISS 10, IQR 4–17).
Table 2.
Comparison of injury severity, weapon implicated and resource utilisation by body region injured.
| N (%) | ISS Median (IQR) |
No. of emergency operations, Median (IQR) |
Operating time**(h:mm). Median (IQR) | Hospital LOS (days). Median (IQR) |
ITU Admission. N (%) |
Cost of index admission (£). Median (IQR)* | ||
|---|---|---|---|---|---|---|---|---|
| All patients | 532 (100%) | 9 (3, 13) | 1·0 (0·0–1·0) | 2:22 (1:42–4:15) | 3·3 (1·7, 6) | 133 (25%) | £4375 (2574–8490) | |
| Single anatomical region injured: | ||||||||
| Limb(s) | 115 (22%) | 4 (1, 7) | 1·0 (1·0–1·0) | 2:06 (1:39–3:10) | 2 (1·3, 3·8) | 9 (8%) | £3693 (2506–6377) | |
| Head and Neck | 41 (8%) | 4 (1, 11) | 1·0 (1·0–1·0) | 3:02 (1:36–3:54) | 3·3 (1·7, 8·5) | 13 (32%) | £5487 (3485–8416) | |
| Abdomen | 57 (11%) | 4 (1, 9) | 0·5 (0·0–1·0) | 2:50 (2:03–3:22) | 4·8 (2, 7) | 20 (35%) | £5424 (3037–9000) | |
| Thorax | 98 (18%) | 9 (9, 16) | 0·0 (0·0–1·0) | 2:04 (1:37–2:12) | 3·0 (2·6, 5·0) | 27 (28%) | £2911 (2074–6020) | |
| Multiple anatomical regions injured | ||||||||
| 221 (42%) | 10 (4, 17) | 1·0 (0·0–1·0) | 2:22 (1:42–4:15) | 4·0 (2·3, 7·0) | 64 (29%) | £4924 (2646–9954) | ||
calculated based on 359 of 532 patients (cost data missing in 173 patients).
calculated on those patients who underwent surgical intervention (data available for 224/346 patients).
Where weapon type was grouped into two categories (any recorded weapon versus no weapon recorded), the mean ISS was 4·17 (95% CI: 2·50 to 5·84; p-value <0·001) higher for casualties with no weapon recorded compared to those with any weapon recorded (see Supple-mentary Table 1). Injuries with no recorded weapon most commonly involved multiple regions (Supplementary data Table 2). The risk ratio of having multiple regions injured compared to an isolated limb injury is 2·43 (95% CI: 1·36 to 4·34; p-value 0·003) for casualties in whom no weapon was recorded compared to those injured with a knife (other/unspecified). An association was seen between machete use and isolated limb injuries or multiple regions injured (Supplementary data Fig. 1). The risk ratio of having multiple injuries compared to an isolated limb injury is 0·67 (95% CI: 0·37 to 1·21; p-value 0·187) for casualties injured with a machete compared to a knife (other/unspecified).
Surgical intervention was required by 346/532 (65%) patients; the median number of operative procedures per patient was 1·0 (IQR 0·0–1·0) with 70/532 (13·1%) patients requiring multiple operations. There were 459 emergency operations over the 3-year study period. Those with isolated thoracic injuries were managed non-operatively in the majority of cases (median of 0·0 operations per patient, IQR 0·0–1·0). 133 patients (25%) were admitted to ICU with a median stay of 2 days (IQR 1–3). One third of patients admitted with abdominal injuries and head and neck injuries required ICU admission compared with only 8% in those with isolated limb injuries. The median total hospital length of stay per patient was 3·3 days (IQR 1·7–6). The longest total length of stay occurred in patients with abdominal injuries (median 4·8 days, IQR 2–7) and those with multiple regions injured (median 4 days, IQR 2·3–7). Involvement of multiple specialties during inpatient care was frequent (Table 3). Plastic surgery was involved in inpatient care of the greatest proportion of knife-injured patients (35%), followed by cardiothoracic surgery (23%) and general surgery (22%). Median cost of index admission per patient was £4375 (IQR 2573–8489). The highest median cost was seen in those with isolated head and neck injuries (median cost £5487, IQR 3485–8416) and isolated abdominal injuries (median cost £5423, IQR 3037–9000).
Table 3.
Surgical specialty involvement per anatomical region injured.
| Surgical specialty |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Anatomical Region of Injury | Plastic Surgery | Cardiothoracic Surgery | General Surgery | Trauma & Orthopaedic Surgery | ENT* Surgery | Vascular Surgery | Maxillofacial Surgery | Neuro surgery | |
| Single-region injuries | Limb (n = 115) | 90 (78%) | 2 (2%) | 3 (3%) | 26 (23%) | 1 (1%) | 11 (10%) | 1 (1%) | 0 (0%) |
| Head & Neck (n = 41) | 3 (7%) | 1 (2%) | 0 (0%) | 2 (5%) | 28 (68%) | 3 (7%) | 6 (15%) | 4 (10%) | |
| Abdomen (n = 57) | 0 (0%) | 1 (2%) | 43 (75%) | 1 (2%) | 1 (2%) | 1 (2%) | 1 (2%) | 1 (2%) | |
| Thorax (n = 98) | 8 (8%) | 56 (57%) | 10 (10%) | 7 (7%) | 1 (1%) | 3 (3%) | 0 (0%) | 2 (2%) | |
| Multiple regions injured (n = 221) |
87 (39%) | 60 (27%) | 62 (28%) | 37(17%) | 25 (11%) | 8 (4%) | 13 (6%) | 8 (4%) | |
| Total number seen by each specialty(as a% of total patients in study=532) | 187 (35%) | 120 (23%) | 118 (22%) | 73 (14%) | 56 (11%) | 26 (5%) | 21 (4%) | 15 (3%) | |
ENT = Ear, Nose and Throat
Percentages utilise the anatomical region of injury as the denominator e.g. 78% of all patients with limb injuries were seen by Plastic Surgery (90/115).
4. Discussion
In keeping with the national upward trend, there has been an increase in incidence of knife-related admissions in our Birmingham MTC over the last three years, particularly in male patients aged less than 25 years [1]. TARN captured less than 50% of all patients admitted with knife injuries resulting from interpersonal violence. Knife injuries amongst women most commonly occurred within a domestic setting (65%), highlighting the problem of intimate partner violence. Injuries were attributable to machete use in 13·9% of patients. Our study also demonstrates a significant degree of violence recidivism, with nearly one in 5 patients presenting to our centre previously or subsequently with violence-related injuries during the observed period.
The significant degree of violence recidivism (18·5%) has not been reported in previous UK-based studies. A US-based study undertaken in an urban trauma centre demonstrated that 15·7% of those presenting with penetrating trauma were recidivists [22]. The true degree of recidivism may be higher than that demonstrated in our single-centre study. This finding of significant violence recidivism highlights an opportunity for secondary prevention and identifies the secondary care setting for delivery. The government-endorsed youth violence charity, RedThread has partnered with six NHS Hospital Trusts, most recently our own [23]. Following referral by a doctor or nurse, a RedThread youth worker builds rapport with the young victim of violence during their vulnerable period in the ED, at which point they may be receptive to engagement [23]. This is followed by efforts to enhance social factors that are deemed protective against violence, such as identifying avenues into education and employment, as well as signposting services such as housing and substance abuse programmes. Multi-agency collaboration between healthcare, local government and law enforcement has proved effective in Cardiff, Wales, where evidence has shown that the routine sharing of anonymised ED patient data with law enforcement to inform policing strategies has been associated with reductions in violent crime [24,25]. The community-focussed Cure Violence initiative has demonstrated similar results across several US cities [26]. As a minimum requirement, the General Medical Council specifies that clinicians have a statutory duty to report all knife injuries to the police [27]. Further research is required to determine whether the newly proposed Knife Crime Prevention Orders, issued by law enforcement alongside criminal conviction, are effective in reducing knife injuries [18].
Our study demonstrates that 13·9% of patients were injured using a machete; conferring a heavy burden on limb reconstructive services. The association between machete use and limb injuries, particularly the upper limbs, has been demonstrated internationally [28]. Weapon description was unrecorded in 36·3% of patients and these patients were found to have a higher Injury Severity Score than those in whom precise causative weapon was recorded. Possible explanations for this finding are that patients with more severe injuries were less able to provide a detailed history of events, or that clinicians did not pursue or record weapon details when dealing with more severely injured patients. Whilst folding blades of three inches or less are currently legal to possess, they accounted for 40% of head and neck injuries in the study population, imposing major additional demands on healthcare resources; further studies to measure their involvement in violent crime in other regions are required and a review of their legal status is recommended. In August 2019, the Offensive Weapons Act 2019 specifically recognises the doubled-edged “zombie” and “cyclone” knives as offensive weapons, however no mention is made of machetes, which may be easily distinguished by their size [17,18]. The authors recommend that law enforcement agencies develop strategies to limit the availability of machetes and to view the possession of machetes in the UK as a serious crime, as it is likely that these have been purposefully acquired for use as weapons.
Female patients were injured in a domestic setting in 65% of cases [1,29]. Of particular concern was the relatively high proportion of pregnant women sustaining stab wounds. Clinicians caring for female patients with knife injuries should routinely enquire about the identity of the perpetrator, particularly in those who present during pregnancy, and ensure that the necessary referral to law enforcement agencies and domestic abuse services is offered.
The UK national registry (TARN) captured only 42% of patients in our cohort, underestimating the true burden of knife injuries. TARN does not routinely include patients admitted for less than 72 h, hence it will systematically exclude those patients with isolated limb injuries (median LOS 2 days, IQR 1·3–3·8 days), as well as some patients with thoracic trauma (median LOS 3 days, IQR 2·6–5·0 days), two-thirds of whom are managed non-operatively. Notably, TARN also does not record deaths occurring pre-hospital or those patients who attend ED without requiring admission [14]. In order to objectively report prevalence and trends in violent injuries and, crucially, to measure the impact of any preventative strategies, the development of a regional or national registry including all knife injuries is urgently warranted.
In-hospital mortality in our cohort was relatively low at 1·9%; this is comparable to mortality of 1.08% to 2% recently reported at London MTCs [9,14]. Multiple specialists are often involved in the care of knife-injured patients, with favourable in-hospital mortality figures suggesting that care is well co-ordinated in the context of our regional major trauma network. The majority of deaths in our cohort were attributable to penetrating chest injuries, consistent with previous studies [6,9]. Thoracic trauma is common, occurring in 18% of patients, and often severe. For policy makers, this finding should provide impetus for co-locating cardiothoracic surgical services within MTCs. Whilst our in-hospital mortality is low, homicide data suggest that there have been almost four times the number of knife-related deaths within our region during our study period [1]. Further research is needed to determine the current injury pattern in those who die before reaching hospital, in order to elucidate the means by which these deaths may be prevented.
Temporal patterns in admission after trauma of all aetiologies have been well established internationally. As observed by others, in addition to noting a diurnal variation with most admissions occurring ‘after hours,’ we have seen a peak in incidence between May and July in Birmingham, associated with relatively warm weather and holiday periods [14,30]. These findings reinforce the need for senior ED clinicians and surgeons to be readily available out of hours and during the summer months to tend to these patients, who have a high likelihood of requiring operative intervention (65%), as demonstrated in this study.
The prevalence of a formal mental health diagnosis in our cohort did not exceed that seen in the general population but may represent under reporting bias; however, alcohol and drug intoxication was common[31]. Intoxication with heroin was recorded in 4·7% of patients and cocaine in 1·7%. Whilst overall drug use appeared relatively unchanged during the period in which knife-related crime has increased, it is thought that changes in the drugs market, such as extension of heroin and cocaine distribution outside of urban areas into ‘county lines’ by drug-dealing gangs, have contributed to the increase in serious violence [3,32]. Knowledge of drug and alcohol intoxication is clinically relevant as this may impact upon patients’ neurological status and physiology, as well as their ability to give consent, with implications for anaesthesia/analgesia and the need for detoxification.
The median estimated cost of the index admission in our cohort was £4375 (IQR 2574–8490). This is lower than that reported by Christensen et al. (£7983), whose TARN-based study was focussed on more severely injured patients and also included cost of prehospital care [6]. Challenges in the way that data are collected, both within healthcare and externally, make identification of the true direct and indirect costs associated with knife injuries difficult.
The main strength and novelty of this study is that it provides a comprehensive characterisation of the knife-injured patient and their injuries from a multi-agency perspective, extending beyond the usual remit of secondary care. The detailed consideration of risk factors for violence exceeds that afforded through other UK secondary-care based studies, several of which were based on trauma registry data [6,9,14]. This study represents the more severe end of the knife injury spectrum by virtue of its major trauma centre setting. The findings may be more generalizable to urban centres in the Midlands and North of England as compared with previous London-based studies, as these cities share demographic similarities and have all experienced a sudden increase in knife crime in the last 5 years [1]. An inherent weakness of this study include its retrospective nature and that the study was based in an adult MTC. With growing public concern regarding the involvement of minors in knife-related incidences, as highlighted in the media and national hospital admission reports, future studies should include specialist children's hospitals [2,5,11].
Knife-related injuries consume a large amount of secondary care resources, constituting 12·9% of the trauma team workload at our MTC. A thorough understanding of patient and injury characteristics will be beneficial in future resource planning. Our study has illustrated that knife injuries predominantly affect young men under the age of 25 years and that the overall increase in incidence is accounted for by this demographic. Reliance on the national major trauma database significantly under-represents the true burden of knife injuries. Our novel findings of a significant degree of violence recidivism and machete use have several potential implications for targeted violence-reduction and law enforcement strategies. An important minority of knife-injured patients are women injured by intimate partners. There is an urgent requirement to generate a national collaborative database to inform multi-agency strategies in the prevention and treatment of violent penetrating injury. Healthcare must continue to play an important role as part of a multi-agency approach to better understand and address the important public health issue of knife crime.
4.1. Transparency statement
NM guarantees that the manuscript is an honest, accurate, and transparent account of the study being reported. No important aspects of the study have been omitted.
Declaration of Competing Interest
None declared.
Acknowledgments
Acknowledgments
We are grateful to Katie Gavin (TARN systems analyst/co-ordinator) for providing TARN data from our institution.
Funding
This study was part funded by the National Institute for Health Research (NIHR) Surgical Reconstruction and Microbiological Research Centre (SRMRC) and the University Hospitals Birmingham. One author (GG) acknowledges support from the NIHR Birmingham ECMC, the NIHR Birmingham Biomedical Research Centre and the MRC HDR UK (HDRUK/CFC/01), an initiative funded by UK Research and Innovation, Department of Health and Social Care (England) and the devolved administrations, and leading medical research charities. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Footnotes
Funding: NIHR.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2020.100296.
Appendix. Supplementary materials
References
- 1.Statistics OoN . 2019. Police force area tables, crime in England & Wales, year ending March 2019. Released July 2019 (accessed 30 October 2019) [Google Scholar]
- 2.BBC. Killed in 2019: the UK's first 100 victims 2019. https://www.bbc.co.uk/news/uk-47476217. [Accessed 30 October 2019].
- 3.Roger Grimshaw M.F. Young people, violence and knives - revisiting the evidence and policy discussions. UK Justice Policy Review Focus; 2018. https://www.crimeandjustice.org.uk/sites/crimeandjustice.org.uk/files/Knife%20crime.%20November.pdf. [Accessed 30 October 2019].
- 4.Crime A-ppgoK. Back to school? Breaking the link between school exclusions and knife crime; 2019. [Accessed 30 October 2019].
- 5.Digital HESN . 2018. Hospital admitted patient care activity; 2017-18. [Accessed 30 October 2019] [Google Scholar]
- 6.Christensen M.C., Nielsen T.G., Ridley S., Lecky F.E., Morris S. Outcomes and costs of penetrating trauma injury in England and Wales. Injury. 2008;39(9):1013–1025. doi: 10.1016/j.injury.2008.01.012. [DOI] [PubMed] [Google Scholar]
- 7.Webb E W.J., Henry J., Busuttil A. A comparison of fatal with non-fatal knife injuries in Edinburgh. Forensic Sci Int. 1999;99:179–187. doi: 10.1016/s0379-0738(98)00189-3. [DOI] [PubMed] [Google Scholar]
- 8.Clarke D.L., Quazi M.A., Reddy K., Thomson S.R. Emergency operation for penetrating thoracic trauma in a metropolitan surgical service in South Africa. J Thorac Cardiovasc Surg. 2011;142(3):563–568. doi: 10.1016/j.jtcvs.2011.03.034. [DOI] [PubMed] [Google Scholar]
- 9.Vulliamy P., Faulkner M., Kirkwood G. Temporal and geographic patterns of stab injuries in young people: a retrospective cohort study from a UK major trauma centre. BMJ Open. 2018;8(10) doi: 10.1136/bmjopen-2018-023114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.TARN. The trauma audit and research network - About us 2006. https://www.tarn.ac.uk/Content.aspx?ca=2 [Accessed 30 October 2019].
- 11.BBC. Birmingham star city: arrests over cinema “machete” brawl; 2019. https://www.bbc.co.uk/news/uk-england-birmingham-50533609. [Accessed 2 January 2020].
- 12.Telegraph T. The Telegraph; 2019. Man charged after machete attack in east London where police officer was saved by his Taser. [Accessed 2 January 2020] [Google Scholar]
- 13.Lam C, Aylwin C, Khan M. Are paediatric stabbings in London related to socioeconomic status? Trauma 2019;21(4):310-6.
- 14.Pallett J.R., Sutherland E., Glucksman E., Tunnicliff M., Keep J.W. A cross-sectional study of knife injuries at a London major trauma centre. Ann R Coll Surg Engl. 2014;96(1):23–26. doi: 10.1308/003588414X13824511649616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ariel B., Weinborn C., Boyle A. Can routinely collected ambulance data about assaults contribute to reduction in community violence? Emerg Med J. 2015;32(4):308. doi: 10.1136/emermed-2013-203133. [DOI] [PubMed] [Google Scholar]
- 16.Service N.H. 2012. Protecting people, promoting health: a public health approach to violence prevention for England. [Accessed 30 October 2019] [Google Scholar]
- 17.Acts UPG . 2019. Offensive weapons act 2019. 16 may 2019 ed; 2019. [Accessed 2 January 2020) [Google Scholar]
- 18.Office H. 2019. Knife crime prevention orders guidance. [Accessed 2 January 2020] [Google Scholar]
- 19.Chambers. Chambers 21st century dictionary. chambers 21st century dictionary; 2019 [Accessed 30 October 2019].
- 20.MCCaTN. West midlands ambulance service major trauma triage tool; 2015. https://www.mcctn.org.uk/guidelines-and-protocols.html [Accessed 30 October 2019].
- 21.Organisation W.H. 2011. Youth and health risks: report from the 64th world health assembly, 2011. [Accessed 30 October 2019) [Google Scholar]
- 22.Smith G.A. Knife-related injuries treated in united states emergency departments, 1990-2008. J Emerg Med. 2013;45(3):315–323. doi: 10.1016/j.jemermed.2012.11.092. [DOI] [PubMed] [Google Scholar]
- 23.Redthread Youth Limited rc . Redthread Youth Limited, registered charity 1051260; 2015. 2011. RedThread: What we do.https://www.redthread.org.uk/what-we-do/#a&e [Accessed 30 October 2019] [Google Scholar]
- 24.Boyle A., Snelling K., White L., Ariel B., Ashelford L. External validation of the Cardiff model of information sharing to reduce community violence: natural experiment. Emerg Med J EMJ. 2012;30:1020–1023. doi: 10.1136/emermed-2012-201898. [DOI] [PubMed] [Google Scholar]
- 25.Florence C., Shepherd J., Brennan I., Simon T. Effectiveness of anonymised information sharing and use in health service, police, and local government partnership for preventing violence related injury: experimental study and time series analysis. BMJ. 2011;342:d3313. doi: 10.1136/bmj.d3313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Global C.V. 2020. Cure violence: who we are.https://cvg.org/who-we-are/ [Accessed 2 January 2020] [Google Scholar]
- 27.Council G.M. 2018. Confidentiality: reporting gunshot and knife wounds. 25 may 2018 ed. [Accessed 30 October 2019] [Google Scholar]
- 28.Omoke N.I., Madubueze C.C. Machete injuries as seen in a Nigerian teaching hospital. Injury. 2010;41(1):120–124. doi: 10.1016/j.injury.2009.08.023. [DOI] [PubMed] [Google Scholar]
- 29.Jacovides C.L., Bruns B., Holena D.N. Penetrating trauma in urban women: patterns of injury and violence. J Surg Res. 2013;184(1):592–598. doi: 10.1016/j.jss.2013.06.026. [DOI] [PubMed] [Google Scholar]
- 30.Ali A.M., Willett K. What is the effect of the weather on trauma workload? A systematic review of the literature. Injury. 2015;46(6):945–953. doi: 10.1016/j.injury.2015.03.016. [DOI] [PubMed] [Google Scholar]
- 31.Bellis M.A., Hughes K. Getting drunk safely? Night-life policy in the UK and its public health consequences. Drug Alcohol Rev. 2011;30(5):536–545. doi: 10.1111/j.1465-3362.2011.00290.x. [DOI] [PubMed] [Google Scholar]
- 32.The Home Office HG . 2018. Serious violence strategy. April 2018 ed. [Accessed 30 October 2019] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.