Abstract
Background
Sexual harassment of women in academic medicine may impede advancement and productivity. This study analyzes the longitudinal effects of sexual harassment on academic advancement and productivity among women.
Methods
We undertook a longitudinal analysis to predict effects of sexual harassment reported in 1995 on career outcomes measured in 2012–13, among a sample of women in academic medicine (N = 1273) recruited from 24 U.S. medical schools. Measures included survey data from 1995 on sexual harassment (predictor), and 2012–2013 data on retention in academic medicine, rank, leadership positions, and refereed publications (outcomes), captured from surveys and public records. We used multivariable models to test effects of sexual harassment on study outcomes, adjusting for socio-demographics, employment-related variables, and gender discrimination.
Findings
In 1995, 54% of women reported any workplace sexual harassment, and 32% of women reported severe harassment (e.g., threats or coercive sexual advances) in the workplace. Multivariable regression models showed no significant effects of sexual harassment. However, severe sexual harassment was associated with higher odds of attaining full professorship by 2012–2013 (AOR: 1·70; 95% CI 1·03, 2·80; p = 0·04).
Interpretation
Contrary to our hypothesis, women reporting severe workplace harassment in 1995 were more rather than less likely to advance to full professor. Women seeking advancement may be more vulnerable to sexual harassment in academic medicine vis a vis greater exposure to those who abuse their position of authority.
Funding
NIvH R01GM088470; Doris Duke Foundation 2016D007145; BMGF OPP1163682
Keywords: Sexual harassment, Academic medicine, Faculty, Gender discrimination
Research in Context.
Evidence before this study
The #MeToo movement has brought to light the pervasiveness of sexual harassment of women in the workplace across fields, including academic medicine, but little research with academic medical faculty in the United States (U.S.) exist on the topic. A multi-institutional study of academic medical faculty in 1995 found that 52% of women and 5% of men had experienced sexual harassment in the course of their professional career. A 2014 study of junior faculty in academic medicine found that 30% of women and 4% of men had experienced workplace sexual harassment, suggesting a decline in these abuses though still too prevalence for women. No research has analyzed this issue longitudinally to assess whether it may affect productivity and advancement.
Added value of this study
This study builds on previous research by offering the first longitudinal study of sexual harassment among women in academic medicine. We assessed the associations between women's reports of sexual harassment in 1995 on advancement and productivity as measured in 2012-–13, among a sample of women (N = 1273) recruited from 24 U.S. medical schools.
Implications of all the available evidence
This longitudinal study of women in academic medicine demonstrates that women with a history of severe sexual harassment have increased odds of attaining full professorship. Women pursuing career advancement may be in more vulnerable positions vis-à-vis greater exposure to men in authority who engage in abuse of power. Alternatively, women recognizing/labeling experiences of severe harassment may be better able to cope and advance professionally. Importantly, those experiencing early career sexual harassment remain at greater risk for these abuses even after achieving seniority. Systematic change in the hierarchical and gender-biased culture and climate of academic medicine is needed, because opportunity for advancement in this male-dominated field should not require women to be more resilient or tolerant in the face of assault.
Alt-text: Unlabelled box
1. Introduction
There is increased national attention to the issue of sexual harassment, including a report from the U.S. National Academies of Science, Engineering, and Medicine (NASEM) demanding reduced institutional tolerance of such abuse [1]. Historic trends do suggest a decline in sexual harassment in academic medicine in the U.S. from 1995 to 2014 [2,3]. A 1995 multi-institutional study of academic medicine found that 52% of women and 5% of men had experienced sexual harassment in the course of their professional careers [2]. Using similar measures, a 2014 survey of K-awardees (junior faculty grant awards in the United States providing mentored transition to research independence) in academic medicine found that 30% of women and 4% of men had experienced workplace sexual harassment [3]. While this decline is laudable, these findings still indicate that almost one in three women in academic medicine have been sexually harassed at work. Further, recent research with female residents highlights great variation in risk for harassment across specialty, with lowest risk reported among pediatric residents and highest risk among surgeons [4], which notably corresponds with sex parity imbalances in these fields (i.e., pediatrics is female-dominated and surgery male-dominated) [5]. Overall, these data point to ongoing need to address this issue in academic medicine.
Potential professional harms of workplace sexual harassment are substantial, including stress, lower productivity and even loss of employment [6,7]. A 2018 report from NASEM indicates that job stress and mental/physical health consequences of workplace sexual harassment are linked to declines in employee performance, advancement, and retention [1]. The hierarchical nature of academic medicine facilitates these abuses, both normalizing harassment and allowing perpetrators to act with impunity [2,8,9]. In such contexts fears of retaliation and of loss of opportunity or employment maintain low reporting of sexual harassment [10]. Women in academic medicine who have experienced this workplace harassment also report perceived negative effects of it on professional confidence and career advancement [3]. However, a similar cross-sectional study assessing associations between sexual harassment and productivity and career advancement did not yield significant associations [2]. A recent cross-sectional study with female residents did find an association of sexual harassment with stress [4], and qualitative research suggests that this may affect productivity over time [11]. Longitudinal analysis of this issue may provide greater insight, and would allow for assessment of the potential longer-term effects of sexual harassment over a woman's career trajectory. Unfortunately, there is limited access to longitudinal data on this topic in academic medicine. The aforementioned 1995 study, however, did include follow-up data from 2012–2013 for a subsample of participants who agreed to follow-up for assessments of longer-term tracking of career outcomes. These data offer, to our knowledge, the only available longitudinal data allowing for analysis of longer term career effects of sexual harassment among academic medical faculty.
In this study, we assess longitudinally whether sexual harassment predicts career advancement outcomes among women in academic medicine from across 24 medical schools in the United States from the period of 1995 to 2012–13. While outcome data were collected prior to the #MeToo movement and are not necessarily reflective of issues of sexual harassment for junior faculty today, they provide insight into the realities and experiences of senior female faculty in academic medicine, many of whom continue to work in the field.
2. Methods
This study uses longitudinal data from a cohort of academic medical faculty recruited across 24 medical schools in the United States, as part of the National Faculty Survey in 1995; study participants consenting to follow-up were re-surveyed in the 2012–2013 academic year.
2.1. Baseline survey
The baseline survey was conducted with a representative sample of academic medical faculty from each of 24 randomly selected continental U.S. medical schools. Medical schools eligible for selection were those with 200 or more faculty (≥50 women and ≥10 underrepresented minority faculty). Schools were balanced for public and private status and across four national regions (Northeast, South, Midwest, West). Within each school, the original study investigator team randomly selected six faculty in each of the 24 cells: graduation cohorts (before 1970, 1970–1980, after 1980), sex (male, female), and areas of medical specialization (generalist, medical specialties, surgical specialties, basic science). Women who graduated before 1970 and underrepresented minorities were oversampled in the original study to ensure adequate numbers of faculty for analysis, as the original study focused on cross-sectional analysis of sex and racial/ethnic differences in advancement and promotion of academic medical faculty in the United States. While the original study was not focused on sexual harassment or gender discrimination, these data were collected with the 1995 cohort, allowing opportunity to analyze longitudinally whether these experiences predicted advancement outcomes among women.
2.2. Sample
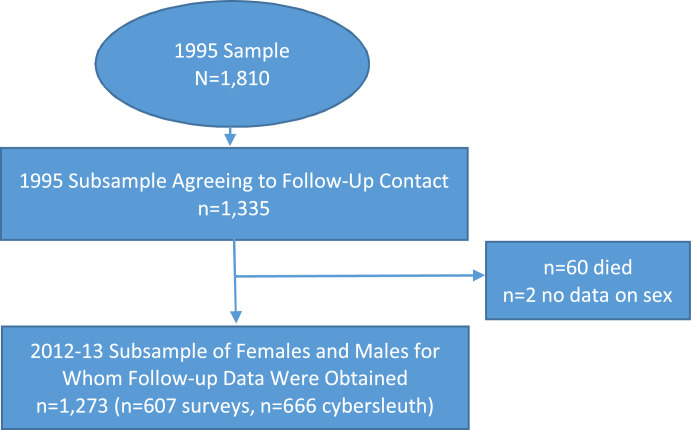
Approximately 60% of all invited faculty responded and participated in the initial mail-in questionnaire (N = 1810); of these respondents, 1335 (74%) consented to participate in follow-up research. We were able to obtain follow-up data for 1273 (95%); 60 participants had died and two did not provide information on sex. Of our sample (N = 1273), we were able to obtain follow-up survey data for 607 (48%); for the remaining (n = 666), outcome variables were obtained from publicly available databases (Fig. 1).
Fig. 1.
Flowchart on Original Study Sample and Analytic Subsamples.
The original baseline participants providing sexual harassment and gender discrimination data were majority white (81% for males and females) and over age 40 (for males: 24% <40, 39% 40–49, 37% 50+; for females: 32% <40, 36% 40–49, 32% 50+) in 1995 [2]. In the initial survey, half of women were at the assistant professor (45%) or instructor level (6%), where less than half of men were at these levels (35% assistant profession, 4% instructor) [2]. Approximately one-quarter of men (26%) and women (27%) were associate professors in the 1995 survey, and mean number of publications was 23 for women and 39 for men [2]. Subsequent studies with the sample document sustained sex differences in promotion to full professor and publication productivity over time [8,12]. Participants were 30% generalist, 28% medical specialists, 25% basic scientists, and 16% surgical specialists [2]. We compared our analytic subsample to participants in the original sexual harassment study and found no significant differences between groups on these indicators.
2.3. Baseline measures
The survey included items on sexual harassment at work as well as items on socio-demographics, respondents’ professional profile and institutional characteristics, and gender discrimination (i.e., differential treatment based on sex but due to gender norms and expectations attached to sex) at work.
A single yes/no item assessed whether the participant had ever encountered sexual harassment, which we defined as having experienced unwanted sexual comments, attention, or advances by a superior or colleague in their professional career. This item was developed based on a standard definition of sexual harassment at training institutions [2,13,14]. Those responding yes to sexual harassment in their career were then asked, again using yes/no questions, if they had ever experienced specific forms of more “severe” sexual harassment. Items assessed behaviors indicative of greater levels of pressure or humiliation, consistent with definitions used by the NASEM [15]: unwanted sexual advances, subtle bribery to engage in sexual behavior, threats to engage in sexual behavior, or coercive advances. We categorized participants reporting yes on any item as having experienced severe sexual harassment [14,16,17].
Covariates included were baseline demographic and employment-related variables known to be associated with outcomes of interest based on our prior research using these data [2,8,12,18,19]. Items on socio-demographics included age, race/ethnicity (dichotomized as non-white and white), marital status (dichotomized as married/partnered versus other), and parental status (dichotomized as ≥1 children versus other). Items related to the respondent's professional profile included academic department (categorized as generalist, surgical specialties, medical specialties, and basic sciences); years since first faculty appointment; and percentage of time spent in administration, research, clinical work, and teaching. Geographic region of the institution was also included (Northeast, South, Midwest, and West). Mean years since first faculty appointment was re-calculated to yield 2012–13 data, using the reported years since appointment reported in 1995 and the date at which follow-up data were obtained from the participant in 2012–13.
Age was subsequently excluded from covariates in all adjusted models due to collinearity with years since first faculty appointment.
Gender discrimination was assessed via two items using five-point Likert scales anchored by “no, never,” and “yes, frequently.”[2] The first item asked whether the respondent perceived any gender bias or obstacles to career success or satisfaction. A second item asked if the respondent had ever been left out of professional advancement opportunities due to gender/sex. We created a composite dichotomous gender discrimination variable where “yes” was defined as a faculty member responding yes/possibly/probably to either perceived gender-specific bias or discrimination in professional advancement questions. We viewed this variable as a potential covariate based on observed association with sexual harassment [2]. We use the terms gender discrimination and gender bias, rather than sex discrimination and sex bias, to account for the fact that these forms of discrimination and bias are rooted in socially constructed gender norms and expectations that hold individuals to a socially defined gender binary (i.e., male and female).
2.4. Follow-up data
We conducted a second survey in the 2012–2013 academic year among those who agreed to participate in follow-up studies. We compared the 1995 cohort with this follow-up subsample and found no significant differences in outcomes by sex [20]. We invited participants to complete the follow-up survey either online or via mail. To ensure baseline and follow-up data were correctly linked to the same participant, we collected demographic information (sex, year of birth, and race/ethnicity) again for purposes of verification; surveys also included all items from the baseline survey on sexual harassment and gender discrimination as well as outcomes of interest: academic rank, senior leadership, retention in academia, and number of refereed publications. Sexual harassment and discrimination items were assessed for the period of 1995 to time of interview, in order to assess whether these abuses occurred in the period since last interview. We provided individual remuneration ($100) to faculty completing the follow-up survey.
For non-respondents to the follow-up survey, we developed a methodology to access publicly available databases to assess academic rank, senior leadership, retention in academia, and number of refereed publications. Using name, departmental affiliation, year of birth, and academic institution in 1995 as personal identifiers, we searched for the subject's current academic affiliation, presence of any leadership position, and professional activities outside of academic medicine, and included data where a match occurred. We used the bibliographic database SCOPUS [21] for total number of peer-reviewed publications through 2012. We conducted a reliability assessment of self-report publication rates and SCOPUS data, which indicated good validity of data from online sources; 62% of women and 58% of men had agreement between self-report and SCOPUS within 80% of the absolute number of publications. The proportion of faculty with self-report higher than SCOPUS was the same for men and women (65%), suggesting that we did not introduce gender bias by using SCOPUS data. We used self-reported data when available, supplementing them with data obtained from publicly available sources for all analyses. This approach allowed retention of the full follow-up subsample with known sex (n = 1273). (Note: All individuals included in this study identified as either male or female.)
Outcome variables were based on combination of self-report and online data and were: academic rank, senior leadership, retention in academia, and number of referred publications. Academic rank was dichotomized as full professor versus all other (lower) ranks. We specifically focused on full professorship because the follow-up period was 17 years, which would capture stagnation at the associate professor level (or lower) and attrition from academic medicine. Retention in academia was dichotomized as retained in academia (working in an academic, foundation, or government setting, including retiring from such settings) or not (in private practice, industry, or another non-academic setting, including retiring from such settings). [Note: In the United States, academics may spend time in government or foundations, which are not tied to profit or product-focused research as would be seen in industry. Such jobs are similar in nature and scope to academic positions, and can include training of junior scholars such as post-doctoral positions, again as seen in academia [22,23].] Two investigators (PC, KF) coded all senior leadership positions (e.g., provost, dean, associate dean, department chair, center director, chief executive officer). We thencreated a dichotomized variable on senior leadership. Number of peer-reviewed publications was measured as a continuous variable.
3. Human ethics
Institutional review board approval for the study was received from Boston University, Tufts Medical Center, and - through a reliance agreement with Tufts Medical Center - Massachusetts General Hospital.
4. Statistical analyses
Only participants with complete data were included in analyses. Due to non-availability of sampling data and information on non-respondents, we did not account for the design or non-response in these analyses. We obtained summary statistics (proportions, means, and standard deviations [SDs]) for all variables, for the total sample and by sex. As appropriate, differences in the distributions of characteristics by sex and outcomes (rank, senior leadership, retention in academia, and number of publications) were conducted using Fisher's exact tests (categorical variables) or t-tests (continuous variables). Due to the small proportion of men reporting sexual harassment, subsequent analyses assessing effects of sexual harassment on career outcomes were limited to women. We conducted descriptive analyses on workplace sexual harassment and gender discrimination for the period prior to 1995 (baseline reports) and the period from 1995 to 2012–2013 (follow-up reports). We used generalized estimating equations accounting for repeated measures to detect significant change over time on these variables.
We conducted bivariate and multivariable analyses to assess associations between sexual harassment reported in 1995 with outcomes reported in 2012–2013, among women. We obtained adjusted odds ratios (AORs) and 95% confidence intervals (CIs) from multivariable logistic regression models for analyses with categorical outcomes (rank, leadership, retention), and an adjusted incident rate ratio from negative binomial regression for our continuous or count outcome (number of refereed publications). We used a backward selection process to develop parsimonious multivariable models and forced “sexual harassment” into the model, retaining covariates with p <0·10. We opted for backward rather than forward selection as some covariates are correlated, and forward selection could result in selected variables becoming non-significant upon inclusion of a subsequent variable. We also included number of publications as a covariate for our model to predict full professor, given the demonstrated association between publication record and promotion [12,20].
We conducted all analyses using SAS 9·4. All tests were two-sided, and we considered p-value <0·05 as significant.
5. Results
At baseline women were less likely than men to be married, have children, and be a full professor (p<0.05) (Table 1). In 2012–2013, women remained less likely to be full professor (59·8% vs 71·5%; p ≤ 0·0001), and were also less likely to have attained a senior leadership position (10·3% vs 21·4%;p ≤ 0·0001) or remain in academia (80·7% vs 85·3%; p = 0·03); they also had fewer peer-reviewed publications than their male counterparts [mean (SD): 49·3 (55·1) vs 69·2 (71·6); p<0·0001].
Table 1.
Demographic and faculty characteristics of participants in 1995 and advancement outcomes in 2012–2013 for the total sample and by sex [1], National Faculty Survey follow-up study.
| Variable | Total sample (N = 1273) n1 (col%) | Male (n = 641) n1 (col%) | Female (n = 632) n1 (col%) | p-value2 |
|---|---|---|---|---|
| CHARACTERISTICS2 | ||||
| Mean age in years (SD) | 45.7 (9.2) | 46.4 (9.2) | 45.1 (9.1) | 0.01 |
| Race | 0·06 | |||
| Non-white | 259 (20·3) | 144 (22·5) | 115 (18·2) | |
| White | 1014 (79·7) | 497 (77·5) | 517 (81·8) | |
| Marital status | ≤0·0001 | |||
| Other | 244 (19·3) | 78 (12·3) | 166 (26·5) | |
| Married/living with partner | 1017 (80·7) | 557 (87·7) | 460 (73·5) | |
| Parental status | ≤0·0001 | |||
| No children | 299 (23·5) | 103 (16·1) | 196 (31·1) | |
| Children | 971 (76·5) | 536 (83·9) | 435 (68·9) | |
| Region | 0·49 | |||
| Northeast | 483 (38·1) | 230 (36·1) | 253 (40·1) | |
| South | 293 (23·1) | 155 (24·3) | 138 (21·9) | |
| Midwest | 246 (19·4) | 127 (19·9) | 119 (18·9) | |
| West | 247 (19·5) | 126 (19·7) | 121 (19·2) | |
| Rank | ||||
| Instructor | 48 (3·8) | 24 (3·7) | 24 (3·8) | <0·0001 |
| Assistant Professor | 503 (39·5) | 221 (34·5) | 282 (44·6) | |
| Associate Professor | 337 (36·5) | 164 (25·6) | 173 (27·4) | |
| Full Professor | 352 (27·7) | 217 (33·9) | 135 (21·4) | |
| Other | 8 (0·6) | 3 (0·5) | 5 (0·8) | |
| Department | 0·14 | |||
| Generalist | 332 (27·3) | 156 (25·4) | 176 (29·1) | |
| Surgical specialist | 217 (17·8) | 122 (19·9) | 95 (15·7) | |
| Medical specialist | 388 (31·9) | 188 (30·7) | 200 (33·1) | |
| Basic sciences | 281 (23·1) | 147 (24·0) | 134 (22·1) | |
| Mean years since first faculty appointment (SD) (2012) | 28·9 (8·9) | 29·4 (9·2) | 28·3 (8·6) | 0·02 |
| ADVANCEMENT OUTCOMES (2012) | ||||
| Full professor3 | 710 (65·8) | 398 (71·5) | 312 (59·8) | ≤0·0001 |
| Senior leadership3 | 202 (15·9) | 137 (21·4) | 65 (10·3) | ≤0·0001 |
| Retention in academia3 | 1009 (83·0) | 524 (85·3) | 485 (80·7) | 0·03 |
| Mean number of refereed articles (SD)4 | 59·5 (64·8) | 69·2 (71·6) | 49·3 (55·1) | <0·0001 |
Percentages do not always correspond to n/N due to missing data. Missing data are excluded from the denominator.
Demographic and faculty characteristics were based on 1995 data as these survey data were available for all participants. Mean years since first faculty appointment was the only covariate based on 2012 data, and this was calculated using the survey data from 1995 in addition to the year at which follow-up data were collected.
Based on Fisher's Exact test.
Based on t-test; SD: Standard Deviation.
In 1995, women as compared with men reported higher rates of gender discrimination (81·7% vs. 30·7%) and sexual harassment (53·9% vs. 4·2%), and 32·1% of women reported severe sexual harassment in the forms of unwanted and coercive sexual advances, as well as bribery and threats to engage in sexual behavior (Table 2). While these baseline prevalence rates are for the full sample, they are comparable to rates for the subsample reached for follow-up survey data. Women reported lower prevalence of workplace sexual harassment for the period between baseline and follow-up, relative to what was reported at baseline (follow-up prevalence 20·7%, p < 0·0001), while men reported similar rates for both time periods (follow-up prevalence 3·9%, p = 0·84). Gender discrimination produced similar findings, with women reporting lower prevalence of workplace gender discrimination between the period of baseline and follow-up, relative to what was reported at baseline (follow-up prevalence 66·4%, p <0·0001), while men reported similar prevalence for both time periods (follow-up prevalence 29·6%, p = 0·72).
Table 2.
Prevalence of sexual harassment and gender discrimination in 1995 and 2012–131 and change prevalence over time, by sex, national faculty survey.
| Male |
Female |
|||||
|---|---|---|---|---|---|---|
| 1995 (n = 641) n (%) | 2012–13 (n = 283) n (%) | p-value2 | 1995 (n = 632) n (%) | 2012–13 (n = 296) n (%) | p-value2 | |
| Sexual harassment | 26 (4·2) | 10 (3·9) | 0·84 | 336 (53·9) | 56 (20·7) | <0·0001 |
| Severe sexual harassment | 22 (3·5) | 7 (2·7) | 0·54 | 197 (32·1) | 34 (12·6) | <0·0001 |
| Unwanted sexual advances | 21 (3·4) | 7 (2·7) | – | 186 (30·1) | 30 (11·2) | – |
| Subtle bribery to engage in sexual behavior | 2 (0·3) | 2 (0·8) | – | 56 (9·1) | 6 (2·2) | – |
| Threats to engage in sexual behavior | 1 (0·2) | 1 (0·4) | – | 9 (1·5) | 0 (0·0) | – |
| Coercive sexual advances | 4 (0·6) | 2 (0·8) | – | 49 (8·0) | 9 (3·3) | – |
| Gender discrimination | 194 (30·7) | 76 (29·6) | 0·72 | 514 (81·7) | 178 (66·4) | <0·0001 |
| Gender bias/obstacles to career success | 154 (24·3) | 68 (26·3) | – | 454 (72·4) | 165 (61·3) | – |
| Left out of professional advancement due to gender | 58 (9·2) | 27 (10·5) | – | 401 (63·7) | 140 (52·2) | – |
Percentages do not always correspond to n/N due to missing data. Missing data are excluded from the denominator.
Obtained from Generalized Estimating Equations (GEE) accounting for repeated measures.
To explore whether sexual harassment and gender discrimination reported in 1995 were associated with having experienced these abuses in period from the 1995 survey to the 2012–2013 survey, we conducted a simple post-hoc analysis with the subsample of women providing these survey data at both time points (n = 265). Among this subsample, we found that 15·5% of women (n = 41) reported harassment in 1995 and in 2012–2013 (the latter indicative of the period subsequent to the 1995 survey up to the 2012–2013 survey. Two in five (40·8%; n = 108) reported harassment only on the 1995 survey, and 4·9% (n = 13) reported sexual harassment only on the 2012 survey. More than one-third of women (38·9%; n = 103) reported no sexual harassment on either survey. Women who reported harassment in 1995 were significantly more likely to report sexual harassment in the subsequent period up to 2012–2013 (p<0·001). For the female subsample with gender discrimination data available at both time points (n = 266), 59·8% (n = 159) reported gender discrimination in 1995 and on the 2012–2013 survey (again, the latter for the period from the 1995 survey to the 2012–2013 survey). More than one in five (22·2%; n = 59) reported gender discrimination in 1995 but not on the 2012–2013 survey. Smaller percentages reported gender discrimination only on the 2012–2013 survey (6·4%, n = 17) or on neither survey (11.7%; n = 31). [Note: Sexual harassment and gender discrimination prevalence estimates for 1995 did not differ for the subsample with 2012–13 follow-up survey data on harassment and discrimination as compared to the full follow-up sample included in our main analyses (Table 2).]
5.1. Effects of sexual harassment
Bivariate analyses (Table 3) and multivariable regression models (Table 4) indicated no statistically significant associations between prior discrimination or sexual harassment and career outcomes among women. However, women who reported severe sexual harassment achieved full professorship at a higher rate [Adjusted Odds Ratio (AOR): 1·77, 95% Confidence Interval (CI): 1·10, 2·87; p = 0·02].
Table 3.
Bivariate associations between gender discrimination and sexual harassment and academic advancement of women in academic medicine, National Faculty Survey.
| Variable | Outcomes |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Full professor |
Senior leadership |
Retention in academics |
Number of refereed articles |
||||||||
| No (N = 210) | Yes (n = 312) | p-value2 | No (n = 566) | Yes (n = 65) | p-value2 | No (n = 116) | Yes (n = 485) | p-value2 | (n = 632) | p-value3 | |
| n1 (%) | n1 (%) | n1 (%) | Mean (SD4) | ||||||||
| Encountered Sexual harassment | 102 (49·0) | 176 (57·3) | 0·07 | 299 (53·7) | 37 (56·9) | 0·69 | 62 (54·9) | 253 (52·7) | 0·75 | 53·4 (57·0) | 0·09 |
| Encountered severe sexual harassment | 53 (25·9) | 116 (38·4) | <0·01 | 171 (31·2) | 26 (40·0) | 0·16 | 33 (29·2) | 153 (32·5) | 0·57 | 58·7 (56·6) | <0·01 |
Percentages do not always correspond to n/N due to missing data. Missing data are excluded from the denominator.
Based on Fisher's Exact test.
Based on t-test; SD: Standard Deviation.
Table 4.
Adjusted odds ratios (AOR), adjusted incident rate ratio (Adj. IRR), and 95% confidence intervals (CI) from multivariable regressions to evaluate the association of gender discrimination and sexual harassment with academic advancement of women in academic medicine, National Faculty Survey1.
| Full professor2 (n = 494) | Senior leadership3 (n = 579) | Retention in academics4 (n = 561) | Number of refereed articles5 (n = 518) | |
|---|---|---|---|---|
| AOR (95% CI); p-value | Adj IRR (95% CI); p-value | |||
| Sexual harassment | 1·25 (0·80, 1·95); p = 0·32 | 0·92 (0·53, 1·59); p = 0·76 | 0·69 (0·43, 1·10); p = 0·11 | 1·12 (0·95, 1·33); p = 0·19 |
| Severe sexual harassment | 1·77 (1·10, 2·87); p = 0·02 | 1·17 (0·67, 2·04); p = 0·58 | 0·93 (0·56, 1·54); p = 0·78 | 1·16 (0·97, 1·38); p = 0·11 |
Excludes missing data.
Logistic regression adjusted for region (Northeast, South, Midwest, West), department (generalist, surgical, medical/other, basic sciences), type of institution (academic, other), years since first faculty appointment, percent of time in administration, and percent of time in research.
Logistic regression adjusted for department (generalist, surgical, medical/other, basic sciences), type of institution (academic, other), and percent of time in administration.
Logistic regression adjusted for race (white, non-white), marital status (married/living with partner, other), region (Northeast, South, Midwest, West), department (generalist, surgical, medical/other, basic sciences) and years since first faculty appointment.
Negative binomial regression adjusted for parental status (no children, have children), department (generalist, surgical, medical/other, basic sciences), type of institution (academic, other), years since first faculty appointment, percent of time in administration, and percent of time in research.
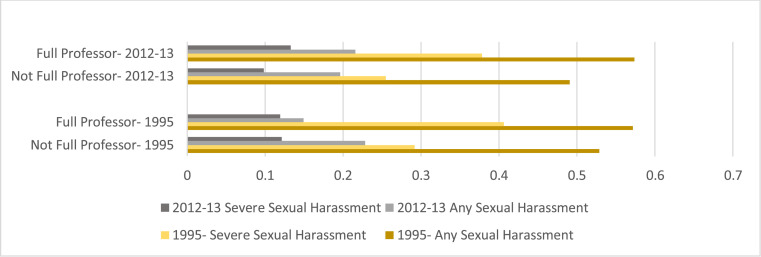
As the data on sexual harassment in 2012–13 is a secondary analysis for the smaller subsample of follow-up participants providing survey data in 2012–13, we did not create regression models to assess these cross-sectional associations. Nonetheless, we graphed reported experiences of sexual harassment among women in 1995 and in 2012–2013, by full professor/not full professor at each time point (Fig. 2). This graph reinforces our multivariable finding on the association between reports of severe sexual harassment in 1995 and achieving full professor by 2012–13, but suggests no difference by rank in terms of reports of sexual harassment at follow-up.
Fig. 2.
Sexual Harassment and Severe Sexual Harassment in Academic Medicine Reported in 1995 and for the period of 1995 to 2012–13 among Female Faculty by Rank (Full Professor or Not) in 1995 and in 2012–13.
6. Discussion
Findings from this longitudinal study of more senior women in academic medicine demonstrate that those who experienced severe sexual harassment earlier in their professional careers, about one in three of these women, were significantly more likely to advance to full professor. This finding and the lack of associations between sexual harassment and other study outcomes are contrary to that seen in prior descriptive and cross-sectional research [1,3]. These findings are also inconsistent with prior cross-sectional research with this same cohort which found no correlational association between harassment and career advancement outcomes in 1995 [2]. The difference in our findings and these prior publications may be attributable to prior research being limited to cross-sectional analyses and possibly a more limited period between the time of harassment and outcomes [1]. Our longitudinal findings may more accurately reflect that this senior cohort of women persisted and advanced in medicine despite harassment and discrimination, an unacceptable but too often required situation for women in the workplace. These findings are particularly notable given prior analysis of these data documenting that women relative to men were less likely to advance to full professor in this same timeframe [20].
A potential explanation for these findings is that women seeking advancement in male-dominated academia, with its historic tolerance of such abuses, have increased opportunity for exposure to harassment. Prior research indicates greater risk for workplace sexual harassment in male-dominated professions and environments, including medicine, where advancement opportunity depends on a hierarchical power structure (i.e., advisors and mentors) [1,2,[24], [25], [26]]. Recent research with medical residents corresponds with these findings, with higher past 24 month prevalence of sexual harassment reported in the male-dominated field of surgery relative to the female-dominated field of pediatrics [4]. Research from academic medicine similarly shows that harassment most commonly occurs from a supervisor or colleague [3], and can include “quid pro quo harassment,” making women seeking advancement more vulnerable to these abuses [1]. Our finding that 9% of women have experienced quid pro quo harassment reinforces this point. Studies indicate that across science, engineering, and medicine, medical students are at the greatest risk for sexual harassment, potentially also resulting in greater tolerance of these abuses [1,27]. Greater understanding of the frequency and chronicity of harassment and the nature of the relationship to the perpetrator, as well as of support systems used by victims, would offer more insight into our findings. Nonetheless, findings support that women are demonstrating resiliency and advancement in the context of workplaces that do not protect them from sexual harassment and gender discrimination [28].
While these findings are important, they may not necessarily hold true for newer professionals in Academic Medicine, particularly subsequent to the #MeToo movement and recent responses from the National Academies of Science, Engineering and Medicine (NASEM) offering clarity on these abuses and their unacceptability [15]. There is some research, with a convenience sample of working women, which suggests that sexual harassment in the workplace has declined since the #MeToo movement [29]. However, studies on the topic with nationally representative samples indicate no change in prevalence of sexual harassment over the period of 2014 (pre-#MeToo) to 2018 and 2019 [30], [31], [32]. This study offers important advancement over prior work by offering a longitudinal examination of the topic, but we must continue to collect data and follow-up with women and men on their experiences of sexual harassment in academic medicine today. The opportunity to use these data to promote change cannot be overstated given the substantial and growing response to pressures for change, based on the NASEM report and the larger #MeToo movement. For example, the United States National Institute of Health (NIH), the nation's federal health research body, has in response to this report set new standards for monitoring and accountability of these abuses [33], and the head of NIH has vowed not to speak on any “manels” (i.e., male-only expert panels) [34].
Detailed data on chronicity of sexual harassment are not available in the current study, but analysis of prevalence of sexual harassment at baseline and subsequently for the period from baseline to 2012–2013 follow-up among the subsample providing follow-up survey data do indicate a decline for women over time, though no change for men. Notably, those reporting sexual harassment at baseline were more likely to report it at follow-up as well. Similar findings are seen for gender discrimination, which is strongly linked to sexual harassment [1], [2], [3]. Importantly, these findings indicate that harassment and discrimination persist across women's career trajectories, even though some reduction is seen. Women's lower risk for sexual harassment and assault with increased age is well-documented [30,35], but workplace sexual harassment may also be declining. There is some evidence which suggests that this is the case for academic medicine [2,3]. Nonetheless, as our findings support, it remains unacceptably high even for participating women with academic seniority; more than one in five reported workplace sexual harassment in the follow-up period. Prior research documents that institutional climate and culture affect the likelihood of abusive and discriminatory behaviors, and this may explain persistence of these experiences over time [1,36]. [Climate refers to the shared perceptions of the institutional environment (e.g., allowance for dating among colleagues), where culture is the often more deep-seated norms and values of the institution that define its identity (e.g., norms related to sexual language or interactions in the workplace) [37].] Such cultures also maintain victims’ silence with direct or indirect threats of vindictive retaliation [38]. We cannot, though, assume that these findings are institution-specific, as we know that changing institutions remains common among faculty [39]. Likely this is a broader concern for the field with continued disproportionate burden to those early in career. Female medical students may learn early to navigate these risks, and perhaps all the more so when our sample was in training. As such, our cohort of female faculty may have entered our study with a pre-existing resiliency to advance despite exposure to harassment and discrimination at work, and it is possible that those who did not want to continue to endure these abuses in the academic setting opted out of academic medicine. Research demonstrates that sexual harassers are often serial abusers, maintaining their position at their institution with impunity or transferred to other organizations without notification of the abuses they perpetrated [40], and this speaks to the problem with both the abusers and the bystanders in power that allow the abuse to continue. In such contexts, it may be that those women willing and/or able to navigate these abuses are disproportionately represented in academic medicine, at least for the generation of faculty included in this study.
Study findings indicate very low rates of sexual harassment of men, but the nature of the assessment may not have sufficiently identified men's experiences. A recent national study found that the most common form of sexual harassment men experience is emasculation and homophobia [30]. Sexual and gender minorities also face greater risk for such workplace abuses [30], which the current measure may not have been sufficiently sensitive to detect. NASEM recently offered a broader definition of sexual harassment: “(One) gender harassment (verbal and nonverbal behaviors that convey hostility, objectification, exclusion, or second-class status about members of one gender), (Two) unwanted sexual attention (verbal or physical unwelcome sexual advances, which can include assault), and (Three) sexual coercion (when favorable professional or educational treatment is conditioned on sexual activity [quid pro quo]).”[1] This definition goes beyond directly targeting an individual, recognizing that a sexually hostile environment itself can be sexually harassing even if specific individuals are not directly targeted [1]. More research is needed to understand men's experiences of harassment and bullying in academic medicine.
While these longitudinal findings offer important insight, they must be considered in light of certain study limitations. Our primary predictor, sexual harassment, is based on self-report, and did not include information regarding the relationship of the respondent and perpetrator(s). Self-report data can be subject to social desirability and recall biases. Severity of sexual harassment can also be subjective, though we based our definition as used in the original study [2] and adherent to definitions from NASEM [15]. Additionally, for follow-up data on sexual harassment, low response rates may introduce bias. However, we found a similar percent of women reporting sexual harassment in 1995 as that seen among those who responded in 2012 (55–56%). Further, these data are, to our knowledge, the only data on chronicity of sexual harassment (reports of harassment over both periods) for academic medical faculty, indicating their value despite the more limited sample. Importantly, however, the data from this study are specific to later in career and life individuals, who were recruited based on their faculty position in 1995. Findings thus cannot be generalizable to junior faculty today, but may still offer a cautionary tale for these younger cohorts and the institutions in which they work, where both affected women and those who harassed may continue to work in senior faculty positions.
An additional limitation is potential selection bias related to sexual harassment for participants in the original baseline study versus non-responders. Our sample from 1995 had a 60% participation rate, and the untapped 40% may have been more or less likely to have experienced sexual harassment or gender discrimination. We unfortunately have no data on non-respondents and thus cannot assess whether selection bias is a concern for the sample. While these data exist in the AAMC's Faculty Roster Survey [41], they are unavailable for analysis due to confidentiality concerns. Nonetheless, our sample is largely demographically comparable to academic medicine faculty according to the AAMC report [41], suggesting a lower risk for selection bias. An additional concern is our inability to understand the institutional context of these data. The original 1995 data anonymized schools for their protection, so while we can compare differences across schools, we cannot know institutional indicators that may affect harassment, such as the proportions of female faculty or faculty leaders in a given school in 1995 or currently. Future research should examine this issue.
Generalizability of our sample is also limited to female academic medical professionals in the United States, and from a period prior to the #MeToo movement. Greater public awareness and intolerance of sexual harassment may yield different findings regarding prevalence of sexual harassment today and with younger cohorts, and possibly with cohorts of clinicians and health researchers who do not pursue positions in academic medicine. Unfortunately, past year data from graduating medical students indicate that 4% received unwanted sexual advances and 15% were subjected to offensive sexist remarks during medical training (sex disaggregated data are unavailable) [42], suggesting that the issue of sexual harassment, even if declining, persists and occurs early in career. Importantly, we did not assess mental health outcomes; depression is a well-recognized effect of harassment that can potentially mediate effects of harassment on advancement [3,15,30,35]. Further research with mental health considerations is needed.
Additionally, demographic and occupational related risks for sexual harassment could not be a focus of this study to the relatively small cell sizes that would result from splitting data further. More research is needed to consider intersectional vulnerability to sexual harassment, including vulnerability based on subspecialty and the male dominance of that subspecialty, as well as differences by demographic indicators related to marginalization (race/ethnicity, geographic region, disability, and sexual minority identification). Replication of this study with a larger sample would offer an important opportunity to understand these issues better.
This longitudinal study of women in academic medicine demonstrates that women with a history of severe sexual harassment have increased odds of attaining full professorship. Women pursuing career advancement may be in more vulnerable positions vis-à-vis greater exposure to men in authority who engage in abuse of power. Alternatively, women recognizing/labeling experiences of severe harassment may be better able to cope and advance professionally. Importantly, among this cohort of older faculty, those experiencing early in career sexual harassment remain at greater risk for these abuses even after achieving seniority. Monitoring sexual harassment through annual surveys in academic medicine should be a priority, as should accountability structures to maintain a climate of safety [24]. Systematic change in the hierarchical and gender-biased climate and culture of academic medicine is needed [43], because opportunity for advancement in this male-dominated field should not require women to be more resilient or tolerant in the face of assault. Further, while women may be surviving these abuses, this does not mean they have no effect. They may in fact contribute to ongoing sex differences seen in advancement and productivity documented in other studies. [12,20] More prospective work is needed to determine how these findings may differ across generations of faculty, and to assess if things are getting better. While findings are specific to the United States (U.S.), they may be meaningful beyond the U.S. as the number of women entering medicine across the world increases. The time is now to stop sexual harassment in academic medicine. While findings demonstrate women's resilience despite these abuses, women's success and advancement should not require persistence in the face of ongoing mistreatment in the workplace.
Declaration of Competing Interest
Ms. McDonald reports personal fees from Partners HealthCare, outside the submitted work. The other authors have no conflicts of interest to declare.
Acknowledgments
Acknowledgements
This work was funded by the National Institutes of Health (Grant Number R01GM088470) and the Doris Duke Foundation (Grant Number 2016D007145). Support for developing the collection of supplemental papers to The Lancet Series on Gender Equality, Norms and Health, including this paper, was provided by the Bill and Melinda Gates Foundation and the Ministry of Foreign Affairs and International Cooperation of the United Arab Emirates. Study sponsors had no involvement in study design, data collection, data analysis, interpretation of findings, the writing of this paper, or the decision to submit the paper for publication.
NIH R01GM088470; Doris Duke Foundation 2016D007145.
Statement of authorship
AR and PC conceptualized the research question and hypotheses, and guided the analytic approach. AR led the literature review and writing of the introduction and result, and contributed to interpretation of study findings. PC guided discussion and interpretation of study findings. KF contributed to the refinement of the research question, guidance on variable construction, and analytic approach, and led the writing of the methods section of the paper. JM supported scientific writing and formating of the paper. All authors provided substantive review of the paper and approved the final submitted paper. AR as corresponding had full access to all the data in the study and had final responsibility for the decision to submit for publication
References
- 1.NASEM . National Academies of Sciences, Engineering, Medicine (NASEM). Policy Global Affairs Committee on Women in Science, Engineering and Medicine. Committee on the Impacts of Sexual Harassment in Academia. National Academy of Sciences. National Academies Press (US); WashingtonDC: 2018. The national academies collection: reports funded by National Institutes of Health. [Google Scholar]
- 2.Carr P.L., Ash A.S., Friedman R.H. Faculty perceptions of gender discrimination and sexual harassment in academic medicine. Ann Intern Med. 2000;132(11):889–896. doi: 10.7326/0003-4819-132-11-200006060-00007. [DOI] [PubMed] [Google Scholar]
- 3.Jagsi R., Griffith K.A., Jones R., Perumalswami C.R., Ubel P., Stewart A. Sexual harassment and discrimination experiences of academic medical faculty. JAMA. 2016;315(19):2120–2121. doi: 10.1001/jama.2016.2188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pololi L.H., Brennan R.T., Civian J.T., Shea S., Brennan-Wydra E., Evans A.T. Us too sexual harassment within academic medicine in the U.S. Am J Med. 2020;133(2):245–248. doi: 10.1016/j.amjmed.2019.06.031. [DOI] [PubMed] [Google Scholar]
- 5.AAMC . 2017. Active physicians by sex and specialty, 2017. Table 1.3. number and percentage of active physicians by sex and specialty.www.aamc.org/data/workforce/reports/492560/1-3-chart.html (accessed October 21, 2019) [Google Scholar]
- 6.Gelfand M.J. Drasgow F. measuring sexual harassment: theoretical and psychometric advances Au - Fitzgerald. Louise F, editor. Drasgow F. measuring sexual harassment: theoretical and psychometric advances Au - FitzgeraldBasic Appl Soc Psych. 1995;17(4):425–445. [Google Scholar]
- 7.Lim S., Cortina L.M. Interpersonal mistreatment in the workplace: the interface and impact of general incivility and sexual harassment. Journal of Applied Psychology. 2005;90(3):483–496. doi: 10.1037/0021-9010.90.3.483. [DOI] [PubMed] [Google Scholar]
- 8.Carr P.L., Gunn C., Raj A., Kaplan S., Freund K.M. Recruitment, promotion, and retention of women in academic medicine: how institutions are addressing gender disparities. Women's health issues: official publication of the Jacobs Institute of Women's Health. 2017;27(3):374–381. doi: 10.1016/j.whi.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stone L., Phillips C., Douglas K.A. Sexual assault and harassment of doctors, by doctors: a qualitative study. Med Educ. 2019;53(8):833–843. doi: 10.1111/medu.13912. [DOI] [PubMed] [Google Scholar]
- 10.Hersch J. 2015. Sexual harassment in the workplace.https://wol.iza.org/articles/sexual-harassment-in-workplace/long (accessed October 20, 2019) [Google Scholar]
- 11.Lindquist C., McKay T. RTI Press; Research Triangle Park (NC): June 2018. Sexual harassment experiences and consequences for women faculty in science, engineering, and medicine. RTI Press Policy Brief. 2018 Research Triangle Institute. All rights reserved. [PubMed] [Google Scholar]
- 12.Raj A., Carr P.L., Kaplan S.E., Terrin N., Breeze J.L., Freund K.M. Longitudinal analysis of gender differences in academic productivity among medical faculty across 24 medical schools in the United States. Acad Med. 2016;91(8):1074–1079. doi: 10.1097/ACM.0000000000001251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Till F. 1980. Sexual harassment: a report on the sexual harassment of students. [Google Scholar]
- 14.Fitzgerald L., Gelfand M., Drasgow F. Measuring sexual harassment: theoretical and psychometric advances. Basic Appl Soc Psych. 1995;17(4):435–445. [Google Scholar]
- 15.NASEM . 2018. Sexual harassment of women: climate, culture and consequences in academic sciences, engineering and medicine.http://sites.nationalacademies.org/shstudy/index.htm (accessed October 21, 2019) [PubMed] [Google Scholar]
- 16.1995. Sexual harassment in the federal workplace: trend, progress, continuing challenges.https://www.mspb.gov/netsearch/viewdocs.aspx?docnumber=253661&version=253948 (accessed October 21, 2019) [Google Scholar]
- 17.DLanghout R., Bergman M.E., Cortina L.M., Fitzgerald L.F., Drasgow F., Williams J.H. Sexual harassment severity: assessing situational and personal determinants and outcomes. J Appl Soc Psychol. 2005;35(5):975–1007. [Google Scholar]
- 18.Kaplan S.E., Gunn C.M., Kulukulualani A.K., Raj A., Freund K.M., Carr P.L. Challenges in recruiting, retaining and promoting racially and ethnically diverse faculty. J Natl Med Assoc. 2018;110(1):58–64. doi: 10.1016/j.jnma.2017.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blazey-Martin D., Carr P.L., Terrin N. Lower rates of promotion of generalists in academic medicine: a follow-up to the national faculty survey. J Gen Intern Med. 2017;32(7):747–752. doi: 10.1007/s11606-016-3961-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carr P.L., Raj A., Kaplan S.E., Terrin N., Breeze J.L., Freund K.M. Gender differences in academic medicine: retention, rank, and leadership comparisons from the national faculty survey. Acad Med. 2018;93(11):1694–1699. doi: 10.1097/ACM.0000000000002146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scopus. https://www.scopus.com/home.uri (accessed April 4, 2019).
- 22.Glied S., Wittenberg R., Israeli A. Research in government and academia: the case of health policy. Isr J Health Policy Res. 2018;7(1):35. doi: 10.1186/s13584-018-0230-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ramsey B.W., Nepom G.T., Lonial S. Academic, foundation, and industry collaboration in finding new therapies. N Engl J Med. 2017;376(18):1762–1769. doi: 10.1056/NEJMra1612575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.VanDis J., Stadum L., Choo E. Sexual harassment is rampant in health care. Here's how to stop it. Harv Bus Rev. 2018 November 1. [Google Scholar]
- 25.Gruber J., Morgan P. Sexual harassment and male dominance: toward an ecological approach. In: Paludi M.A., editor. Vol 2. Praeger Inc; Westport, CT: 2008. (The psychology of women at work: challenges and solutions of our female workforce). [Google Scholar]
- 26.McLaughlin H., Uggen C., Blackstone A. Sexual harassment, workplace authority, and the paradox of power. Am Sociol Rev. 2012;77(4):625–647. doi: 10.1177/0003122412451728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dresden B.E., Dresden A.Y., Ridge R.D., Yamawaki N. No girls allowed: women in male-dominated majors experience increased gender harassment and bias. Psychol Rep. 2018;121(3):459–474. doi: 10.1177/0033294117730357. [DOI] [PubMed] [Google Scholar]
- 28.Day Langhout R., Bergman M., Cortina L., Fitzgerald L., Drasgow F., Hunter Williams J. Sexual harassment severity: assessing situational and personal determinants and outcome. J Appl Soc Psychol. 2006;35:975–1007. [Google Scholar]
- 29.Johnson S., Keplinger K., Kirk J., Barnes L. Has sexual harassment at work decreased. Harv Bus Rev. 2019 July 18. [Google Scholar]
- 30.SSH . February 2018. Facts behind the #MeToo movement: A national study on sexual harassment and assault.http://www.stopstreetharassment.org/wp-content/uploads/2018/01/Full-Report-2018-National-Study-on-Sexual-Harassment-and-Assault.pdf (accessed October 21, 2019) [Google Scholar]
- 31.SSH . 2014. Unsafe and harassed in public spaces: a National Street Harassment Report.http://www.stopstreetharassment.org/wp-content/uploads/2012/08/National-Street-Harassment-Report-November-29-20151.pdf 2014. (accessed October 21, 2019) [Google Scholar]
- 32.SSH Measuring #MeToo: a national study on sexual harassment and assault. 2019. Stop Street Harassment (SSH) 2019 http://www.stopstreetharassment.org/our-work/nationalstudy/2019study/ (accessed October 21, 2019) [Google Scholar]
- 33.Collins F.S., Tabak L.A., Wolinetz C., Lauer M.S., Valantine H.A. 2019. Important notice to NIH grantee and applicant institutions on sexual harassment March 26.https://www.nih.gov/sites/default/files/research-training/initiatives/sexual-harassment/20190325-notice-extramural-sexual-harassment.pdf (accessed October 21, 2019) [Google Scholar]
- 34.Collins F.S. 2019. Time to end the manel traditions.https://www.nih.gov/about-nih/who-we-are/nih-director/statements/time-end-manel-tradition June 12. (accessed October 21, 2019) [Google Scholar]
- 35.Breiding M.J., Smith S.G., Basile K.C., Walters M.L., Chen J., Merrick M.T. Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization–national intimate partner and sexual violence survey, United States, 2011. Morbid Mortal Wkl Report Surveill Summar (Washington, DC: 2002) 2014;63(8):1–18. [PMC free article] [PubMed] [Google Scholar]
- 36.Gruber J., Fineran S. Sexual harassment, bullying, and school outcomes for high school girls and boys. Violence Against Women. 2016;22(1):112–133. doi: 10.1177/1077801215599079. [DOI] [PubMed] [Google Scholar]
- 37.Hoy W. Organizational climate and culture: a conceptual analysis of the school workplace. J Educ Psychol Consult. 1990;1(2):149–168. [Google Scholar]
- 38.Binder R., Garcia P., Johnson B., Fuentes-Afflick E. Sexual harassment in medical schools: the challenge of covert retaliation as a barrier to reporting. Acad Med. 2018;93(12):1770–1773. doi: 10.1097/ACM.0000000000002302. [DOI] [PubMed] [Google Scholar]
- 39.Kaminski D., Geisler C. Survival analysis of faculty retention in science and engineering by gender. Science. 2012;335(6070):864–866. doi: 10.1126/science.1214844. [DOI] [PubMed] [Google Scholar]
- 40.Cantalupo N.C., Kidder W.A. A systematic look at a serial problem: sexual harassment of students by university faculty. Utah Law Rev. 2018;2018:671–786. June 30. [Google Scholar]
- 41.AAMC . 2018. U.S. medical school faculty.https://www.aamc.org/data/facultyroster/reports/494946/usmsf18.html 2018. (accessed October 21, 2019) [Google Scholar]
- 42.Antman K. Building on #MeToo to enhance the learning environment for US Medical Schools. JAMA. 2018;319(17):1759–1760. doi: 10.1001/jama.2018.3812. [DOI] [PubMed] [Google Scholar]
- 43.Dzau V.J., Johnson P.A. Ending sexual harassment in academic medicine. N Engl J Med. 2018;379(17):1589–1591. doi: 10.1056/NEJMp1809846. [DOI] [PubMed] [Google Scholar]