New York State had its first case of novel coronavirus (COVID-19) caused by SARS-CoV-2 on March 1, 2020, a health-care worker returning from Iran. The second confirmed case was on March 2 and was thought to be the first caused by community spread. As of March 19, 18 days after the first confirmed case, New York City had 2,469 confirmed cases, and the state had 4,152. We aim to describe our early experience with patients with COVID-19 at a large, tertiary health-care system in the New York metropolitan region so that other health systems in the country are fully prepared to handle the influx of patients with COVID-19 at their hospitals.
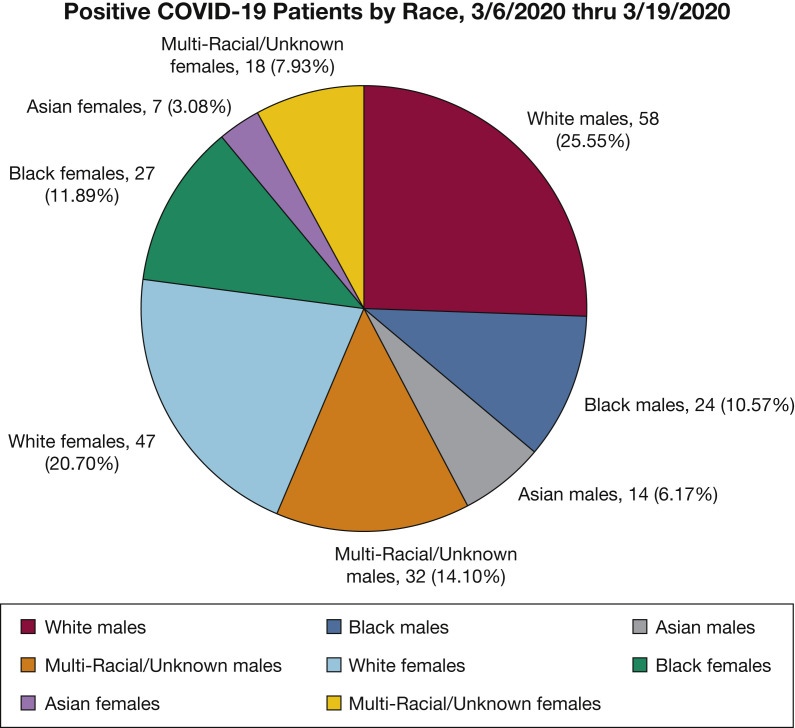
Our health system’s first case was on March 6, 2020. Since then, because of an increase in our testing capabilities, there have been 1,443 people tested for COVID-19 (as of March 19). There are 889 tests pending. There have been 227 positive cases, of which 209 patients have been admitted to one of our system hospitals. The average age of these patients is 62.6 years, with 99 women (43.6%) and 128 men (56.4%). The breakdown by race is shown in Figure 1 . Figure 2 shows the comorbidities for patients who are COVID-19-positive.
Figure 1.
Positive COVID-19 results by race.
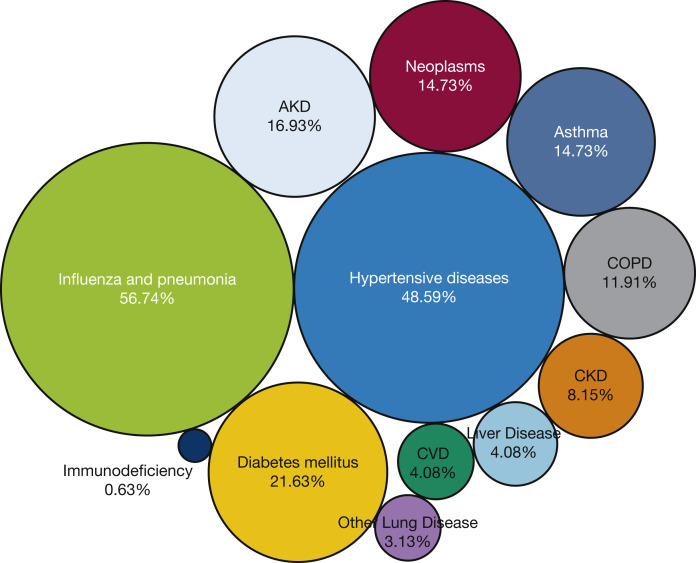
Figure 2.
Comorbidities of the early patients who were COVID-19-positive (does not account for overlapping conditions). AKD = acute kidney disease; CKD = chronic kidney disease; CVD = cardiovascular disease.
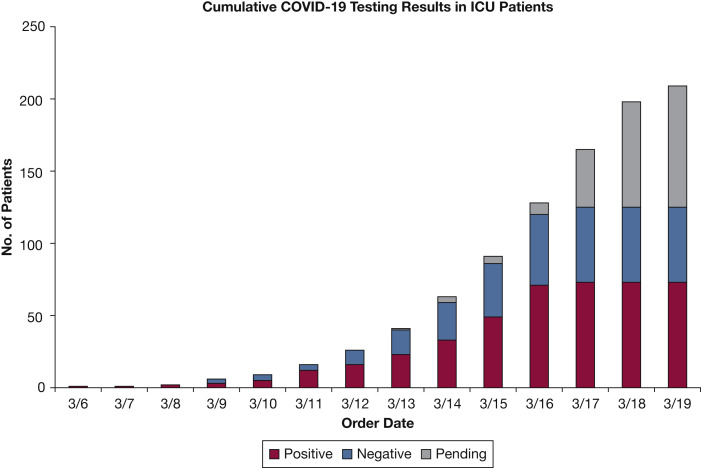
As of March 19, 209 patients were in the ICU that have confirmed COVID-19 (n = 73, 34.9%), have results pending (n = 84, 40.2%), or are negative for COVID-19 (n = 52, 24.9%). Of those 157 patients in the ICU that are COVID-19-positive or have results pending, 33 are ≤ 50 years of age. These patients have taken up most of our ICU capacity and staffing, and many are intubated. Figure 3 shows the cumulative testing results of the patients in the ICU, being mindful of a delay in reporting.
Figure 3.
Cumulative COVID-19 testing results in patients in the ICU.
These data are already outdated by the time of publication because the numbers rise hour by hour. It is imperative that health systems across the country anticipate this oncoming wave of patients to properly prepare staff, change staffing models, and prepare more ICU beds. We describe here our disaster planning.
Emergency Planning: Lessons Learned
In planning for this influx of patients, we divided leadership teams into operations teams, clinical advisory teams, human resource teams, and finance teams. We were able to divide the work into one of those groups and reported out to the whole leadership team daily. Things pertinent to ICU care included the concept of cohorted units for patients who were COVID-19-positive and COVID-19-pending, surge plans to create hospital floor beds and ICU beds, intubation strategies, surge staffing plans, and supply issues. The supply issues involved personal protective equipment, ventilators, ventilator supplies (high-efficiency particulate air filters, tubing, bag-valve masks, etc), medications, tubing, and so forth. Surge plans should happen in stages as the surge progresses. More radical increases in space should be planned for in case of extreme circumstances.
Lessons learned include the following: planning for the inevitable loss of employees because of exposures, loss of employees because of school closures, the need for hospital-aided backup childcare plans, and stock and supply chain losses because of the closure of factories. Care should be taken to establish teams for ICU care if the traditional ICU teams are overextended. We included other subspecialties, such as anesthesia and surgical teams, because all elective surgeries were cancelled and other teams were less busy. This also helped to open up other ICU beds.
Because we are a network of tertiary care centers and community hospitals, we started training community sites to handle ARDS prior to the local start of the pandemic. We also have the luxury of a telehealth network that connects all of our ICUs, so our team had the ability to evaluate and coordinate care easily across our hospital system. This technology also enabled our extracorporeal membrane oxygenation (ECMO)-to-Go team to evaluate ECMO candidates across our system and help those teams manage extreme cases of acute lung injury that were not ECMO candidates. This enabled us to deploy ECMO, a limited resource, in a fair and thoughtful manner. It also helped reduce transfers to other centers when not absolutely necessary.
A well thought-out plan will avoid chaos and panic when surge occurs. We strongly suggest the aforementioned elements are addressed as you face this pandemic.
Footnotes
FINANCIAL/NONFINANCIAL DISCLOSURES: None declared.
Supplementary Data
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.