Abstract
Hospitalized patients and their caregivers often access technologies like patient portals to understand what happens during their hospital stay. Although this access can lead to more patient engagement and positive health outcomes, many find that the technology does not support their needs. As a first step toward improving patient-facing technologies we create personas for hospitalized patients and their caregivers by following the Q Methodology, a technique for quantifying subjective opinion. We clustered 28 hospitalized patients’ and 19 caregivers’ attitudes towards receiving and managing information and working with their care team. We contribute three patient personas: patients who are (1) accommodating information seekers, (2) involved safety guardians, and (3) self-managing participators. We identify three caregiver personas: (1) cooperative information seekers, (2) vocal participators, and (3) hands-off safety guardians. These personas can inform future tools designed to support communication and information management for hospitalized patients and caregivers.
Introduction
Allowing patients to access their health information while in the hospital enables them to be active participants in their care1, to have increased satisfaction, to engage in healthy behaviors, and to have improved understanding of their care2,3. Patients want to understand many different aspects of their care, including their medications, the plan of care, and the workflow of activities4,5. However, patients and caregivers (i.e., friends or family members who help or accompany the patient during their hospital stay) face substantial barriers to receiving information and engaging in their care while in the hospital. These challenges include the lack of supportive tools4, poor setup of their hospital room4, challenges communicating with their care team4,6, cognitive challenges from treatment as well as their illness, and ergonomic limitations due to their environment7.
Research thus far has highlighted the needs of patients and the difference between their needs and the needs of clinicians. Missing from existing work is an understanding of how patients’ needs differ from each other, and how patient-facing technologies should be designed to accommodate those differences. Researchers have found that hospitalized patients differ in their interest and approach to engagement with their care8, and that people managing a chronic disease differ in their use of technology9. Yet, more work is needed to understand how hospitalized patients’ and caregivers’ values and priorities differ, and how the design of patient-facing technologies can better support those differences. A common approach to designing for such different types of users is to use personas10,11. To identify personas in order to support the information needs of hospitalized patients, we use the Q methodology and semi-structured interviews12,13.
We identify hospitalized patient and caregiver user groups based on how they prioritize information in the hospital and how they want to work with their care team. We base those user groups on our study with 28 hospitalized patients and 19 caregivers. Through this work, we contribute (1) an explanation of six distinct personas that represent hospitalized patients and caregivers, and (2) implications for the design of tools that support the varied information and communication needs of hospitalized patients and caregivers.
Related Work
In a hospital environment, patients and their caregivers find it challenging to maintain up-to-date awareness of the patient’s’ health status and plans of care14, managing their information and communicating with their care team. We briefly summarize this research and how creating personas for patients and caregivers contributes new insights.
Patient and Caregiver Information Needs in the Hospital
Patients want to receive a variety of information about their care such as the plan of care, the schedule of activities, information about their vitals, food, and providers on their care team4. Patients also want to know that information such as their allergies or preferences is effectively communicated to their care team. They want to ensure that information they communicate is properly propagated to the care system, for example that their current clinical team knows their allergy information15 or contextual information about their treatment routine16, and that such information is properly transferred to clinical staff from one shift to another to achieve continuity of care16.
Caregivers play an important role in managing care. Caregivers act as a proxy in the care of patients to make treatment decisions17,18, or to communicate on behalf of the patient17. They also provide social support in transition periods or when the patient faces cognitive challenges16, normalize the patient experiences19,20, and act as companion, assistant, representative, navigator, and planner for pediatric patients17. In a critical care environment, patients and families have limited cognitive resources to be able to process and manage their health information. Patients may forget 40-80% of what was said during a medical consultation almost immediately21. The order and modality in which information is presented, perceived importance, and health context can all impact the patient’s likelihood of remembering information21.
In addition to needing to receive a variety of types of information, patients and their caregivers want to effectively manage, capture, and communicate information to the care team16. Without tools to accomplish this, patients would have to remember all the information providers share and be responsible for keeping their providers aware of their needs during shift changes and transitions in care16. Further, critically ill patients often need substantial help from caregivers for managing information from clinicians22.
This prior work has helped identify the multitude of information needs that patients and caregivers have. Our study adds to this knowledge by investigating how patients and caregivers prioritize different information needs and how they cluster together based on shared priorities.
Patient and Caregiver Communication with the Care Team
The Institute of Medicine has emphasized that providers should engage in patient-centric care, “responsive to individual patient preferences, needs and values and ensuring that patient values guide all the clinical decisions”23. Even though patient and caregiver engagement in the hospital is important, it can be heavily impacted by the relationship they have with their care team. A high-quality relationship with the provider might make people more comfortable communicating certain questions to providers, such as information seeking questions about medication24, and more interested in engaging with their care team around improving safety issues6. A good quality relationship is associated with lower disease burden and greater uses of preventative care services25. When patients have an increase in perceived control and communication with the provider, it leads to improvements in trust in their provider26. But when the relationship with the care team is not as strong, patients encounter significant barriers in communicating with their care team, such as asymmetrical power dynamics that are typically dominated by the physician27, fear of being perceived as a “difficult” patient27, and lack of comfort asking challenging questions such as asking if a health care provider washed their hands6.
The patient’s level of engagement in their care and their attitudes to their care team play a role in the information they receive in the hospital and how they engage with it. In this work we contribute empirical findings about how patients and caregivers prioritize and balance relationships and communication with their care team relative to their information needs.
Personas in Health Domains
Although some technologies exist to support patients’ needs for information about their care and engagement with the care team14, existing tools insufficiently support tailored, patient-specific information14. To understand how technologies might offer tailored support to patients and caregivers with different needs, we seek to identify different patient and caregiver personas based on their information and collaboration needs. Personas are user archetypes that characterize users based on their attitudes, goals and behaviors11. They are informed by a variety of types of data and methods, from qualitative insights on user goals11 to data driven personas based on behaviors33. Personas are used during the design process to help: build empathy towards users10; facilitate communication about design choices10; reduce conflicts about what the perceived user goals are10,11; and summarize data about users and their needs. Personas have helped characterize users in many health domains such as heart failure self-management28, home healthcare technologies29,30, child cancer survivors31, or older adults32. Based on the demonstrated usefulness of personas in these health domains, we characterize users of patient facing technologies based on attitudes towards information and communication needs.
Methods
We used a mixed methods approach to identify the attitudes and opinions of patients and caregivers around information needs, information engagement, information management, and the relationships and social perceptions surrounding care delivery in the hospital. We used the Q methodology34 to structure data collection with the patient and caregiver, and interviewed the participants twice, first during the study session, and second during a follow up a week after discharge. The study was approved by the researchers’ institutional review board.
Q Methodology
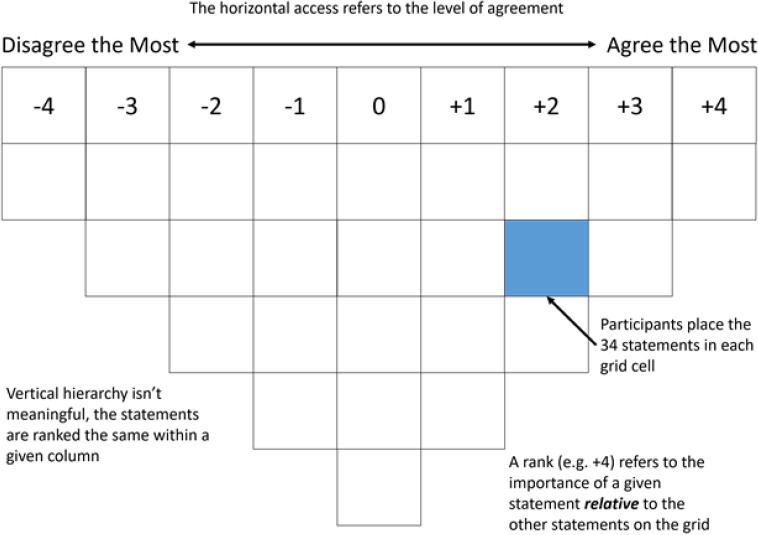
To understand how patients prioritize and make sense of getting and managing information while hospitalized, we used the Q Methodology12,34 to structure our data collection and analyze our data. The method quantifies subjective opinions through two key features – a set of statements about a topic, and a grid for ranking those statements in the shape of a normal distribution (Figure 1). By quantifying subjective opinions, the Q Methodology leads to the creation of personas by understanding what people feel most strongly about. It provides many of the advantages of qualitative methods, such as discovering themes in rich subjective data. The Q methodology is a small-sample technique that offers statistical validity to the qualitative interpretation of subjective data, making it useful for small samples (<50 people)12. The Q methodology has increasingly been used to cluster types of users based on beliefs and reactions to technology12, and to describe the tradeoffs and attitudes individuals have about health technology in a structured way9,13. This method showed how common attitudes towards health and technology supersede typical demographic segmentations like gender, age, and ethnicity in the context of a chronic disease population9.
Figure 1.
Force distribution for ranking statements
The Q methodology requires participants to order a set of statements relative to one another using a grid like the one shown in Figure 1. Researchers created a set of 34 statements, as described below. To identify patient priorities, we use the Q sorting activity: a highly structured data collection activity in which participants need to organize the subjective statements in a grid shaped like a normal distribution. The extremes of the distribution are the statements that participants agree or disagree with the most, with Neutral in the middle. The statements placed at the extremes receive the most weight in the quantitative data analysis. Based on this distribution, we can compare each person’s ranking with the statistical technique of factor analysis, and thus, identify patterns of subjective opinions.
Participants were asked to read through the statements and place them into a grid based on how much they agree or disagree with the statement relative to all the other statements. The researchers then probed the participants to explain their reasoning for the placement of statements and their general opinion about the statements. After participants organized all the 34 statements into the grid, we interviewed them about topics such as their routines during their hospital stay, communication with staff, families and friends, or the use of technology while hospitalized. A follow up phone interview was conducted within 7 days of the discharge. The patients and caregivers conducted the Q sorting activity and interviews separately, then discussed together, and took breaks as needed. The information from interviews is used to complement participant agreement with statements by adding qualitative insights.
Creating the Q Statement Set
For the Q sorting process we started with a set of 89 statements that described different attitudes related to interacting with information and people in the hospital environment, based on prior research on patient-provider communication, patient information needs, and based on data from prior surveys on patients and caregivers4,14. These statements pertained to communication preferences, empowerment, information management, information needs and relationships. Based on pilots with children and adults, we narrowed down the Q set to 34 statements https://patientsassafeguards.ischool.uw.edu/wp-content/uploads/2019/07/AMIA19Q.pdf, such as “(6) It’s important to speak up to doctors and nurses when I have a question”, “(3) It’s important to know why each medication is given to me”, or “(12) It’s important that I am not a bother to my doctors and nurses”. Caregiver statements were almost identical, with adjustments to the pronoun where appropriate. Since caregivers and patients can play different roles in care, using identical Q statements between these two populations allowed us to find where caregivers and patients converged and diverged from each other.
Analysis
Each participant’s ranking of statements was transcribed and entered into the freely available PQMethod software35. We separated the Q rankings created by patients from those created by caregivers. We used principal component analysis and rotated using the varimax method36. This analysis surfaces unique clusters where participants’ Q statements clustered together. Each identified cluster was therefore a selection of participants who unambiguously load highly in the cluster. Each cluster had a set of distinguishing statements that characterized a unique point of view, ranked from -4 (Disagree the most) to +4 (Agree the most). The distinguishing statements for each cluster are statistically significant, meaning that participants ranked those statements much higher or lower than participants in other clusters, at minimum threshold of p<0.05. In the results we will refer to the distinguishing statements by marking their relative ranking with an asterisk. For example, we will refer to knowing information about medication (+4*) to refer to a statement that participants strongly agreed with, is a statistically significant (at p<0.05), and is a distinguishing statement for that cluster. To supplement the quantitative analysis, we analyzed interviews qualitatively based on codes grounded in the original statement categories, with additional codes developed based on emergent themes identified during the content analysis.
Participants
We recruited 28 patients and 19 caregivers at two study sites: an adult tertiary care hospital and a pediatric hospital. Patients (13 male, 14 female) had a median age of 53 for adults, and 12 for children. Caregivers (2 male, 15 female) were or age: one was 18-29, seven were 30-39, six were 40-49, three were 50-59 years old, and two did not specify the age. Participants had diverse educational and racial backgrounds: Hispanic/Latino (6), American Indian/Alaska Native (2), Asian (5), Native Hawaiian/Pacific Islander (1), Black/African American (7), White/Caucasian (30).
Based on regional population demographics, we used purposeful sampling to identify eligible participants based on age, gender, race, ethnicity, and we sought an even distribution across hospital services (medical or surgical). Research coordinators approached patients who had been in the hospital for at least 24 hours, spoke English, and were able to participate in a conversation about their current care. The coordinators obtained informed consent, and conducted a verbal questionnaire to collect demographics and information about the current hospital stay. In our pediatric cohort, participants needed to be at least 7 years old and have parental consent as well as their own assent to participate. Caregivers included family members and friends who actively observed and participated in the care for the patient.
Results
The Q-sorting principal component analysis surfaced three clusters, from the PQMethod35 software analysis, for patient attitudes and three clusters for caregiver attitudes. We present these clusters described as personas in the next section. Of the 28 patient participants, two were not able to complete the Q sort process because of interruptions related to their health condition or hospital stay. Adult patient quotations are indicated by an “A” and youth quotations by a “Y”, followed by a number (e.g. A02), or “C” for caregiver, followed by the participant number (e.g. C08). A complete list of the distinguishing statements is available at https://patientsassafeguards.ischool.uw.edu/wp-content/uploads/2019/07/AMIA19Q.pdf.
The personas are different between the patient and caregiver groups, however patient and caregiver personas also share dimensions. Both patients and caregivers have safety guardian personas, but they differ in how engaged they are with the care team. Both patients and caregivers have information seeker personas, but they differ in how cooperative or accommodating they are with the care team. Both populations have personas that are interested in being active participants in their care, either holistically, or focused specifically on self-management.
Patient Personas
Patients fell into three clusters with shared attitudes towards managing and receiving information in the hospital, and collaborating with the care team. These patient clusters account for 45% of the variance in the patient group, and were relatively evenly split between Cluster 1 (n=9), 2 (n=6), and 3 (n=7). Four patients did not have significant associations with any of the clusters, or fit across multiple clusters, so they are not included in the persona descriptions below. The clusters had an even distribution between hospital sites (adult and children’s), gender, and type of service (medical vs. surgical). All patient participants cared about actively engaging with their care in that they strongly disagreed with statement #30: “I prefer to leave decisions about my medical care up to my doctor”. The patients expressed general agreement with statements about wanting to know what will happen with their care for the day (#2), the importance of speaking up when they have a question (#6), and feeling like their doctors and nurses listen to them (#21). However, key differences emerged regarding how the participants prioritized types of information, relationships, and level of engagement. Based on these differences, we describe three patient personas.
Patient Persona 1: The Accommodating Information Seeker
The persona emerging from the first cluster of the Q analysis (n=9) is distinguished by 8 statements, summarized in . We call this persona the “Accommodating Information Seeker”, based on their priority for knowing different types of information as well as their apathy in learning more about or interacting with their care team.
Table 2.
Example distinguishing statements for each attitude cluster, (P>0.05, +4=Most Agree, -4=Most Disagree)
| Patient Personas | Distinguishing Statement | Ranking |
| Accommodating | (3) “It’s important to know why each medication is given to me” | +4 |
| Information Seekers | (22) “It’s important to know how my doctors and nurses are communicating with each other at shift changes” | -3 |
| Involved Safety Guardians | (25) “It’s important to know what kinds of safety errors can happen with patients in my situation” | +3 |
| (11) “It’s important to get information in a way that I can understand” | +4 | |
| Self-Managing Participator | (17) “It’s important that I be an active participant in my healthcare” | +4 |
| (12) “It’s important that I am not a bother to my doctors and nurses” | -4 |
The “accommodating information seeker” strongly values getting information about various aspects of their care, with an emphasis on information immediately relevant for them. For example, accommodating information seekers think it important to know about their medication (+4*), about rapidly changes of situation like the severity of their condition (+4*), and the way to get information when they are worried (+3*). Many patients spoke specifically about wanting to know changes in their medications. For example: “knowledge is power and [knowing] what medications I’m taking and for what condition and is this a medication that’s just temporary related to this condition that I have or is this one of my regular medications that I take for a different condition?” (A06).
These patients are “accommodating” to their care team in the sense that they are willing to let their clinicians go about their business without interruption. Accommodating information seekers found it less important to engage with their care team and know either the care team’s workflow (-3*), or their names and responsibilities (-2*). Despite patients’ interest in getting access to information when they are worried, patients did not think it important to feel like clinicians had time to answer their questions (-1*). Nonetheless, they were not concerned about being a bother to the care team (-1*) and were willing to assert their voices about topics they cared about, like medication (+4*): “If you’re still confused [and] nobody can help now, you worry. So you need something, like ask doctor what I have to do to keep my body continue to working” (A14).
Patient Persona 2: The Involved Safety Guardian
The persona describing the second cluster of the Q analysis (n=6) is distinguished by 8 statements, summarized in Table 2. We call this persona the “Involved Safety Guardian”, based on patients being actively involved in patient care that appears grounded in a concern about patient safety.
Participants in this cluster took a “safety guardian” role, finding it important to receive information that is critical to their safety, such as awareness of possible safety errors (+3*) or reasoning for medication (+4*). These patients also were “involved” in their care because they wanted to stay informed about how doctors and nurses communicate between shift changes (+2) and to make sure they got information in a way they could understand (+4). Some patients emphasized getting information in formats they could understand, such as pictures or video. One participant mentioned: “I’m a visual person, like you can’t just like give me a bunch of handouts and tell me to read them and that I’ll get it? … you kind of have to like show me when you’re talking to me” (A02).
Compared to other clusters, participants associated with this cluster felt that cost concerns and respecting privacy were least important. In contrast to the “accommodating information seekers”, patient participants in this group were less concerned about understanding the seriousness of their medical situation.
Patient Persona 3: The Self-Managing Participator
The third persona comprises participants in the third cluster of the Q analysis (n=7), and is distinguished by 9 statements, summarized in Table 2. We call this persona the “Self-Managing Participator”, based on patients’ interest in being active participants in their care and performing self-management of their condition.
Patients associated with this cluster placed greater emphasis on “active” participation (+4) as one of the highest ranked items in their sorting grid compared to the “Accommodating Information Seekers” (+1) and the “Involved Safety Guardians” (0). These patients found it important to know the reasoning of their doctors (+3*), and they were not concerned that they might be a bother to their care team (-4*). Patients in this cluster were also interested in the longer-term trajectory of their care, indicating “self-management” interest, such as when they would leave the hospital (+3*). One patient stated: “I’m a control freak, I like to be in control so it’s important that I am, if not totally in control, … you really want to be an active participant so that you understand the consequences later on, because you expect to be living the consequences later on” (A05). These patients cared about aspects like illness severity (+4*), similarly to the “Accommodating Information Seekers”. But this cluster focused primarily on how their illness would impact the future: “I don’t want to know if it’s worsening, but I want to know how serious it is so I can do stuff myself to help.” (Y12).
Compared to the other clusters, patients in this cluster were least concerned about the way information is communicated (0*), possibly because they appreciate information in any form. These patients rated the question about concerns with possible safety errors the lowest (-3), compared to the “accommodating information seekers” (+1) and the “involved safety guardians” (+3).
Caregiver Personas
Using the Q sort analysis, we identified three caregiver personas from the 19 caregiver participants. Our caregiver sample size was determined by the caregiver presence at the research site. All pediatric patients had at least one caregiver present (16 participants), but far fewer adult patients in this study had such active caregivers (3 participants). The three caregiver clusters identified in the Q analysis account for 59% of the variance in the caregiver group. Three participants fit across multiple clusters, so their data is not included in the analysis of the personas below. Each cluster included caregivers from the adult and the pediatric patients.
In contrast to the patients, the caregiver group had a greater consensus in attitudes, both agreement and disagreement, about the Q statement ranking. Thus, fewer statements distinguished each caregiver cluster. Some topics that caregivers commonly agreed upon included (1) giving importance to having information that’s easy to share with others (#24), and (2) having someone else help keep track of things is important (#19). Caregivers also said they wanted to feel doctors had time to answer their questions (#14) and to know about different treatment options (#7). Caregivers did not agree with the statement that they should know only what the doctors think is important (#31).
Caregiver Persona 1: The Cooperative Information Seeker
The persona resulting from the first caregiver cluster of the Q analysis (n=10) is distinguished by 8 statements, summarized in Table 3.We call this persona the “Cooperative Information Seeker” based on the caregiver’s interest in specific details and information about the care being given to the patient and their value of getting along with members of the care team.
Table 3.
Example distinguishing statements for each attitude cluster, (P>0.05, +4=Most Agree, -4=Most Disagree)
| Caregiver Personas | Distinguishing Statement | Ranking |
| Cooperative | (15) “It’s important to know how serious the patient’s illness is” | +4 |
| Information Seekers | (27) “It’s important that I have a positive relationship with the doctors and nurses” | +2 |
| (20) “I like to keep track of things by just paying attention and remembering” | -3 | |
| Vocal Participators | (17) “It’s important that I be an active participant in the patient’s healthcare” | +4 |
| (12) “It’s important that I am not a bother to the doctors and nurses” | -4 | |
| Hands-off Safety Guardians | (25)”It’s important to know what kinds of safety errors can happen with patients in our situation” | +2 |
| (30) “I prefer to leave decisions about the patient’s medical care up to the doctor.” | 0 | |
| (32) “It’s important to get information at a time when I can focus” | -4 |
These caregivers were “information seekers”, wanting to know how serious the patient’s condition is (+4*), having medications explained to them (+4), and knowing different treatment options (+3). These caregivers also found it important to be an active participant in the patient care (+2). These caregivers disagreed with “only want[ing] to know what the doctor thinks is important” (-4), or leaving the decisions about the patient to the care team (-2). These caregivers wanted to be “cooperative” with the care team, to have a positive relationships with the care team (+2*), and, that it is important to feel like doctors have time to answer their questions (+3). One caregiver placed the responsibility of a good relationship to the care team, instead of the patient-caregiver team. In a statement reflecting their own role as patient proxy, they said: “a bad start is a bad start. And that’s why it’s good rapport, and I think as a patient, I don’t need to worry about that. Nurses and doctors need to” (C08).
This caregiver cluster is different from the other caregiver clusters in terms of interest in tracking. They expressed greater agreement with statements around the importance of information tracking (0), compared to the second cluster, the “Vocal Participators” (-3), and the third cluster, the “Entrusting Safety Guardians” (-3). These caregivers also strongly disagreed with relying on memory (-3), compared to the “Vocal Participators” (+1) and “Entrusting Safety Guardians” (0). The information seeker caregivers were relatively neutral in their attitudes about information management, compared to cluster 2 and cluster 3 who strongly disagreed with statements about tracking (#18).
Caregiver Persona 2: The Vocal Participator
The second caregiver persona is based on the second caregiver cluster of the Q analysis (n=3), and is distinguished by 8 statements, summarized in Table 3. We call this persona the “Vocal Participator” because the place the greatest importance on the idea of being an active participant.
Caregivers in this cluster are “Vocal participators”. Across clusters, caregivers ranked statement #17, about being an active participant in the patient’s healthcare as the most important statement in the entire Q set (+4*), but participants in this caregiver cluster ranked it significantly higher than those in other clusters. They agreed with other statements such as being listened to by doctors and nurses (+4*), or speaking up when they have a question (+3*). This group strongly disagreed the most with the statement about leaving decision-making solely up to the clinicians (-4*). One caregiver summarized this sentiment: “I’m very active in her care, so I really don’t prefer to leave any of it all the way up to the doctor. Her doctor, specific doctor who we don’t get to see all the time because he’s not on call, but always asks me my opinion first because he knows that I read up on the disease” (C03). These caregivers place importance on knowing the names and responsibilities of the doctors and nurses (+2*), and were not concerned about being a bother to their care team (-4*).
Caregiver Persona 3: The Hands-off Safety Guardian
The third persona resulting from the third caregiver cluster of the Q analysis (n=3) is distinguished by 6 statements, summarized in Table 3. One of the most representative statements for these “safety guardians” is to know about safety errors (+2*), to understand the doctor’s reasoning when making a decision (+4), severity of patient illness (+4), medication information (+3). We call this persona the “Hands-off Safety Guardian” based on their focus on concerns about safety but neutral in controlling the patient’s care or even receiving information at their own convenience.
However, the caregivers in this cluster are more hands-off regarding their role relative to clinicians. They did not strongly agree or disagree with statements about leaving decisions about the patient care to the doctors (0*), and knowing only what the doctor feels is relevant (-1*). These caregivers are more balanced in leaving decisions to the care team (0*) than the “Cooperative Information Seekers” (-2) and the “Vocal Participators” (-4), who explicitly prioritized not leaving decisions to the care teams. Consistent with a more hands-off engagement, are the distinguishing statements that these caregivers do not find it important to get information at a time when they can focus (-4*), or that the care team needs to listen to them (-2*).
Discussion
This study demonstrates that using a mixed method approach for clustering patients and caregivers can identify different persona types for how hospitalized patients and their caregivers want to engage with their care and prioritize information. Although other work has described personas for people managing chronic conditions—such as heart failure, or cancer28,31—this work adds insights into the type of personas we encounter in the hospital environment, for both patients and caregivers. Our analysis contributes knowledge that individual patients and caregivers place different relative values on three types of needs: information seeking about their care (e.g. updates about care, information about self-management), patient safety, and the active engagement in self-care and communication with the care team. Our personas demonstrate how, while individual patients and caregivers may care about all three types of needs, they prioritize each of these needs differently. This difference in relative values means that patient-facing technologies must include features to support a variety of approaches to receiving and engaging with information and communication in the hospital. We describe a variety of features based on prior work that patient facing technology might include to support the multitude of priorities highlighted by the personas.
Designing for Information Seeking
Two of the personas we identified prioritize access to information over a strong active participation in their care, so technology should be proactive in providing information, without people having to seek it out. Inpatient-facing systems need to offer a range of detailed information, including the status of the patient, often related to the immediate care in the hospital, plan of care, medication, changes in their condition, or information about severity of the patient’s condition. For medication information, systems should provide patients with information about what the medicine is, why they are taking the medicine, how to take and how much of the medicine to take, or what alternatives exist. Because both the patient (Accommodating Information Seeker) and caregiver personas (Cooperative Information Seeker) reflect a need to have a good relationship with providers or to not be a burden, information should be delivered in a way that is very easy for them to understand it. For example, the provided information could adapt to the level of health literacy of the patient and use delivery modalities like audio and video37,38.
To prioritize caregiver’s needs, inpatient portals could support sharing features or the ability to have several caregivers interact with the portal. For example, technology should enable collaboration between several caregivers in tracking data about what is happening in the hospital, such as symptoms, or what the providers communicate about patient care. These features should be designed with special considerations for maintaining privacy between the patient and caregiver when appropriate39.
The different priorities in being an Accommodating Information Seeker patient versus a Cooperative Information Seeker caregiver leads to different design implications for how these personas want to engage with the care team. Because caregivers are not as worried about being a burden to providers, systems can facilitate cooperation with the care team by sharing the names, photos, roles, and schedules of individual care team members. This can make it easier for the caregiver to engage with the team. To support the Accommodating patient, systems can enable the patient to communicate their needs while providing flexibility in the modality of this communication. Systems can prioritize asynchronous electronic communication, and flag which questions are urgent to the care team, to reduce patient concerns about being a bother and allow them to perform question “triage”40. To make patients more comfortable in contacting specific providers to ask questions, systems can include information about how each member of the care team prefers to be messaged, or the ability to choose which member of the care team they contact.
Designing for Safety
Being a safety guardian is often associated with being a vigilant monitor, in particular of communication with clinicians41,42. Systems should include a variety of features to support the different levels of involvement that Safety Guardians want to have. The needs reflected by the Involved Safety Guardian patient suggest that patient-facing portals should include features that promote active participation from patients, and enable keeping patients aware of safety issues, medication, and errors that can occur. Systems could support patients in actively reviewing their medication and preventing errors40,43. Through active engagement, patients could use checklists where to monitor whether they are getting the correct medication, alerts and reminders to monitor provider’s hygiene, and other potential hazards.
For the Hands-Off Safety Guardian caregiver persona, who is less engaged in managing safety issues, systems can provide ways to monitor their safety that do not introduce greater cognitive or physical burdens, such as FAQs about safety, common questions by patients like me, notification about important safety issues (e.g., changes in medication), or issues to watch for when taking medication. By including a variety of features, patient-facing technology can appeal to patients and caregivers with varied levels of engagement in care.
Designing for Active Participation
Being an active participator in one’s care involves a high interest in both information about care and in engaging with the care team, thus systems should be designed to actively support patients in participating in their care. To support the Self-Managing Participator patient, patient facing portals should be proactive in offering information about the patient’s care and self-management of their condition, such as changes occurring in their care, changes in medication, severity of their condition, or plan of care. To help patients prepare for discharge and managing care outside of hospital, technology can help patients build up knowledge about how to manage their health, and techniques to build self-efficacy towards managing their health44.
The Vocal Participator caregiver persona prioritized a high level of engagement with the care team. Systems can support them with features that enable high engagement: requesting a second opinion, engaging with doctors and nurses at times that are convenient not only for the clinicians but also for the patient and caregiver, notifications about when their doctor is due to arrive for consultation, what each care provider is in charge of for their care, or the ability to give feedback to the provider about what they did well or what could be improved. This information is of importance to caregivers, because that can help them be present for important communication events such as during rounds or when important decisions are discussed.
Limitations and Future Work
Although personas are a commonly used tool to help designers make decisions, they will not capture every user’s needs; rather, personas are meant to identify archetypes of a variety of users. People might have additional needs beyond what has been identified in prior work4,14. In addition, our sample was designed for breadth rather than depth in understanding how the needs and values of patients and caregivers differ between hospital settings or units within a hospital. Our approach offers a broad holistic view of hospitalized patient and caregiver priorities, but it is possible that if medical and surgical patients’ data were analyzed separately there might be a different prioritization of needs across personas. Also, we assessed how patients and caregivers prioritized information and communication needs at one point in time, but patient or caregiver priorities could change during their stay in the hospital. Further research is needed to understand whether these personas can be applied broadly across all hospital contexts, or if certain care contexts bring with them certain priorities. We have found distinctions between the patient and caregiver personas, but more work is needed to understand how the differences in priorities of participants in our study transfer to different population groups, including based on demographics, disease type, settings, or across different types of caregivers.
Conclusion
Our work contributes a new understanding of information management and communication priorities of hospitalized patients and caregivers. Through our mixed-methods approach, we identified three patient personas: accommodating information seekers, involved safety guardians, and self-managing participators. We also identified three caregiver personas: cooperative information seekers, vocal participators, hands-off safety guardians. These personas could be used by designers of technologies to ensure that during the design process the personas facilitate design choices10 that support the needs of different kinds of people, with different priorities and needs. We hope that versatile technology will support a variety of patients and caregivers to have their needs met with inpatient technologies, and to help them understand their hospital care and enable them to play an active role in safeguarding their hospital stay.
Acknowledgements
This work was supported by the Agency for Healthcare Research and Quality [1R01HS022894] and in part by the National Library of Medicine [T15LM007442].
Figures & Table
References
- 1.Greenfield S, Kaplan SH, Ware JE, Yano EM, Frank HJ. Patients’ participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med. 3(5):448–457. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- 2.Street RL, Millay B. Analyzing Patient Participation in Medical Encounters. Health Commun. 2001;13(1):61–73. doi: 10.1207/S15327027HC1301_06. [DOI] [PubMed] [Google Scholar]
- 3.Greene J, Hibbard JH, Sacks R, Overton V. When Seeing The Same Physician, Highly Activated Patients Have Better Care Experiences Than Less Activated Patients. Health Aff. 2013;32(7):1299–1305. doi: 10.1377/hlthaff.2012.1409. [DOI] [PubMed] [Google Scholar]
- 4.Kendall L, Mishra SR, Pollack A, Aaronson B, Pratt W. Making background work visible: opportunities to address patient information needs in the hospital AMIA. Annu Symp proceedings AMIA Symp. 2015:1957–1966. [PMC free article] [PubMed] [Google Scholar]
- 5.Benham-Hutchins M, Staggers N, Mackert M, Johnson AH, deBronkart D. “I want to know everything”: a qualitative study of perspectives from patients with chronic diseases on sharing health information during hospitalization. BMC Health Serv Res. 2017;17(1):529. doi: 10.1186/s12913-017-2487-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Waterman AD, Gallagher TH, Garbutt J, Waterman BM, Fraser V, Burroughs TE. Brief report: Hospitalized patients’ attitudes about and participation in error prevention. J Gen Intern Med. 2006;21(4):367–370. doi: 10.1111/j.1525-1497.2005.00385.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morris D, Karlson A. Dynamic Accessibility Requirements for Hospital Patients. 2011 [Google Scholar]
- 8.Mishra SR, Haldar S, Pollack AH, et al. In: CHI ’16. New York, NY, USA: ACM; 2016. “Not Just a Receiver”: Understanding Patient Behavior in the Hospital Environment; pp. 3103–3114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’Leary K, Vizer L, Eschler J, Ralston J, Pratt W. Understanding patients’ health and technology attitudes for tailoring self-management interventions. AMIA. Annu Symp proceedings AMIA Symp. 2015:991–1000. [PMC free article] [PubMed] [Google Scholar]
- 10.Pruitt J, Grudin J. In: Proceedings of the 2003 Conference on Designing for User Experiences - DUX ’03. Vol. 1. New York, New York, USA: ACM Press; 2003. Personas: practice and theory. [Google Scholar]
- 11.Cooper A, Reimann R, Cronin D, Noessel C. About Face: The Essentials of Interaction Design [Google Scholar]
- 12.O’Leary K, Wobbrock JO, Riskin EA. In: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems - CHI ’13. ACM Press; 2013. Q-methodology as a research and design tool for HCI; p. 1941. [Google Scholar]
- 13.O’Leary K, Eschler J, Kendall L, Vizer LM, Ralston JD, Pratt W. In: Proceedings of the 33rd Annual ACM Conference on Human Factors in Computing Systems - CHI ’15. Vol 2015. New York, New York, USA: ACM Pres; 2015. Understanding Design Tradeoffs for Health Technologies; pp. 4151–4160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prey JE, Woollen J, Wilcox L, et al. Patient engagement in the inpatient setting: a systematic review. J Am Med Informatics Assoc. 2014;21(4):742–750. doi: 10.1136/amiajnl-2013-002141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilcox L, Morris D, Tan D, Gatewood J. In: Proceedings of the 28th International Conference on Human Factors in Computing Systems - CHI ’10. ACM Press; 2010. Designing patient-centric information displays for hospitals; p. 2123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pratt W, Unruh K, Civan A, Skeels M. Personal health information management. Commun ACM. 2006;49(1):51. [PMC free article] [PubMed] [Google Scholar]
- 17.Miller AD, Mishra SR, Kendall L, Haldar S, Pollack AH, Pratt W. Partners in Care: Design Considerations for Caregivers and Patients During a Hospital Stay. In Proceedings of the 19th ACM Conference on Computer-Supported Cooperative Work & Social Computing, CSCW ‘16; ACM Press; 2016. pp. 754–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hong MK, Wilcox L, Machado D, Olson TA, Simoneaux SF. Care Partnerships: Toward Technology to Support Teens’ Participation in Their Health Care. In: ACM. 2016:5337–5349. doi: 10.1145/2858036.2858508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaziunas E, Buyuktur AG, Jones J, Choi SW, Hanauer DA, Ackerman MS. Transition and Reflection in the Use of Health Information. In: Proceedings of the 18th ACM Conference on Computer Supported Cooperative Work & Social Computing, CSCW ’15; ACM Press; 2015. pp. 1763–1774. [Google Scholar]
- 20.Liu LS, Inkpen KM, Pratt W. “I’m Not Like My Friends”: Understanding How Children with a Chronic Illness Use Technology to Maintain Normalcy. In: Proceedings of the 18th ACM Conference on Computer Supported Cooperative Work & Social Computing - CSCW ’15; ACM Press; 2015. pp. 1527–1539. [Google Scholar]
- 21.Kessels RPC. Patients’ Memory for Medical Information. 2003;Vol 96 doi: 10.1258/jrsm.96.5.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Unruh KT, Pratt W. The Invisible Work of Being a Patient and Implications for Health Care: “[the doctor is] my business partner in the most important business in my life, staying alive.”. Ethnogr Prax Ind Conf Proc; 2008. pp. 40–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Institute of Medicine (IOM) Washington, DC: National Academy Press; 2001. Crossing the Quality Chasm. [Google Scholar]
- 24.Cumbler E, Wald H, Kutner J. Lack of patient knowledge regarding hospital medications. J Hosp Med. 2009;5(2):86–6. doi: 10.1002/jhm.566. [DOI] [PubMed] [Google Scholar]
- 25.Eton DT, Ridgeway JL, Linzer M, et al. Healthcare provider relational quality is associated with better self-management and less treatment burden in people with multiple chronic conditions. Patient Prefer Adherence. 2017;11:1635–1646. doi: 10.2147/PPA.S145942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gabay G. Perceived control over health, communication and patient–physician trust. Patient Educ Couns. 2015;98(12):1550–1557. doi: 10.1016/j.pec.2015.06.019. [DOI] [PubMed] [Google Scholar]
- 27.Doherty C, Stavropoulou C. Patients’ willingness and ability to participate actively in the reduction of clinical errors: A systematic literature review. Soc Sci Med. 2012;75(2):257–263. doi: 10.1016/j.socscimed.2012.02.056. [DOI] [PubMed] [Google Scholar]
- 28.Woods L, Cummings E, Duff J, Walker K. The development and use of personas in a user-centred mHealth design project. In: Proceedings of the 29th Australian Conference on Computer-Human Interaction - OZCHI ’17; ACM Press; New York, New York, USA. 2017. pp. 560–565. [Google Scholar]
- 29.Burrows A, Gooberman-Hill R, Coyle D. Shared Language and the Design of Home Healthcare Technology. In: Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems - CHI ’16; ACM Press; New York, New York, USA. 2016. pp. 3584–3594. [Google Scholar]
- 30.Burrows A, Gooberman-Hill R, Coyle D. Empirically derived user attributes for the design of home healthcare technologies. Pers Ubiquitous Comput. 2015;19(8):1233–1245. [Google Scholar]
- 31.Wärnestål P, Svedberg P, Nygren J, Wärnestål P, Svedberg P, Nygren J. Co-constructing child personas for health-promoting services with vulnerable children. In: Proceedings of the 32nd Annual ACM Conference on Human Factors in Computing Systems,CHI’14; ACM Press; 2014. pp. 3767–3776. [Google Scholar]
- 32.Reeder B, Zaslavksy O, Wilamowska KM, Demiris G, Thompson HJ. Modeling the oldest old: personas to design technology-based solutions for older adults. AMIA. Annu Symp proceedings AMIA Symp. 2011;2011:1166–1175. [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang X, Brown H-F, Shankar A. Data-driven Personas. In Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems, CHI’16; ACM Press; 2016. pp. 5350–5359. [Google Scholar]
- 34.Watts S, Stenner P. Doing Q Methodological Research : Theory, Method and Interpretation. Sage. 2012 [Google Scholar]
- 35.Schmolk P. PQMethod Software. 2014 [Google Scholar]
- 36.Kim J, Mueller C. Factor Analysis: Statistical Methods and Practical Issues. 1978 [Google Scholar]
- 37.Bickmore TW, Pfeifer LM, Byron D, et al. Usability of Conversational Agents by Patients with Inadequate Health Literacy: Evidence from Two Clinical Trials. J Health Commun. 2010;15(sup2):197–210. doi: 10.1080/10810730.2010.499991. [DOI] [PubMed] [Google Scholar]
- 38.Bickmore TW, Pfeifer LM, Jack BW. Taking the time to care. In: Proceedings of the 27th International Conference on Human Factors in Computing System, CHI’09; ACM Press; 2009. p. 1265. [Google Scholar]
- 39.Sharko M, Wilcox L, Hong MK, Ancker JS. Variability in adolescent portal privacy features: how the unique privacy needs of the adolescent patient create a complex decision-making process. J Am Med Informatics Assoc. 2018;25(8):1008–1017. doi: 10.1093/jamia/ocy042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wilcox L, Woollen J, Prey J, et al. Interactive tools for inpatient medication tracking: a multi-phase study with cardiothoracic surgery patients. J Am Med Informatics Assoc. 2016;23(1):144–158. doi: 10.1093/jamia/ocv160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schwappach DLB. Review: Engaging Patients as Vigilant Partners in Safety. Med Care Res Rev. 2010;67(2):119–148. doi: 10.1177/1077558709342254. [DOI] [PubMed] [Google Scholar]
- 42.Miller AD, Pollack AH, Pratt W. Bursting the Information Bubble: Identifying Opportunities for Pediatric Patient-Centered Technology. AMIA . Annu Symp proceedings AMIA Symp. 2016;2016:894–903. [PMC free article] [PubMed] [Google Scholar]
- 43.Prey JE, Polubriaginof F, Grossman L V, et al. Engaging hospital patients in the medication reconciliation process using tablet computers. J Am Med Informatics Assoc. 2018;25(11):1460–1469. doi: 10.1093/jamia/ocy115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pollack AH, Backonja U, Miller AD, et al. Closing the Gap: Supporting Patients’ Transition to Self-Management After Hospitalization. In Proceedings of the 2016 CHI Conference on Human Factors inComputing Systems, CHI’16. 2016:5324–5336. doi: 10.1145/2858036.2858240. [DOI] [PMC free article] [PubMed] [Google Scholar]


