Abstract
In this paper, we report on the development of an analytical model and a decision support tool for meeting the complex challenge of scheduling dialysis patients. The tool has two optimization objectives: First, waiting times for the start of the dialysis after the patients’ arrivals must be minimized. Second, the minimization of lateness after the scheduled finish time, which is relevant for transport services, are pursued. We model the problem as a mathematical program considering clinical pathways, a limited number of nurses managing the patients, and dialysis stations. Furthermore, information about patients’ drop-off and pick-up time windows at/from the dialysis unit are considered. We develop a platform in Microsoft Excel and implement the analytical model using an Open Source optimization solver. A case study from a dialysis unit in the UK shows that a user can compute a schedule efficiently and the results provide useful information for patients, caregivers, clinicians and transport services.
Introduction
Recent research has reported an increasing prevalence of chronic kidney disease worldwide1. Patients who are in the end stage of chronic kidney disease (ESRD) rely on dialysis treatments to survive. Hemodialysis is a common approach to manage the condition. It is typically performed in a clinical setting three times a week for several hours, where the patient is connected to a machine via a vascular access. Patients seeking treatment in dialysis units have individual characteristics which can be distinguished on a variety of metrics such as blood flow rate, dialysate flow rate and composition, volume of fluid to be removed and size of dialyzer. Regular laboratory tests of the patient’s blood help the physicians to determine a suitable treatment plan. Patients may have many preferences, including the desire for short treatment times and preferred starting times during the day. Dialysis facilities, on the contrary, pursue planning the treatment efficiently by optimizing resource utilization for the best patient outcomes. Patient scheduling which is done in dialysis units world-wide, can be defined as assigning patients to scarce resources and time slots to maximize some objective2.
In this paper, we develop an analytical approach to deliver a patient-centric scheduling platform for dialysis patients. Individual patients’ characteristics are taken into account, such as the patient’s clinical pathway, alongside the consideration of the availability of scarce resources that are required. We formulate the scheduling problem as a mathematical program which includes the scheduling decisions around the patients’ availability time windows. Using Microsoft Excel, a manager of a dialysis unit can specify parameters in our tool. The manager selects the waiting time objective and obtains feasible solutions based on the objective function and constraints which are implemented using the Open Source solver back-end of our tool. In doing so, patient schedules can be obtained effectively and efficiently such that waiting-times for patients can be minimized. Finally, the optimal schedules can be shared with patients, caregivers, clinicians and transport services.
The remainder of this paper is structured as follows. In the next section, we provide an overview of related patient scheduling work followed by the presentation of the analytical model, demonstration of the platform and discussion, and conclusions.
Related Work
Patient scheduling is the process of assigning individual patients and/or patients’ activities to time and/or health-care resources2 on the operational decision level. In contrast, appointment scheduling defines a blueprint of patients’ appointments on a tactical level. While some reviews focus exclusively on patient scheduling2,3, appointment scheduling problems have been reviewed by several authors4,7. In this section, we position our paper in the relevant patient scheduling literature and focus on patient-related objectives as shown in Table 1.
Table 1:
Patient-related objectives
| Minimize | ||
| penalties | 8-14 | |
| waiting time of (prioritized) patients | 9-11,15-30 | |
| welfare loss | 31 | |
| number of night treatments | 32 | |
| quality of life proxies | 33 | |
| Maximize | ||
| # patients to be scheduled | 19,34-38 | |
| patients’ satisfaction / preferences | 17,18,22,32,39 | |
The table reveals that most of the research focus has been on one single patient-related objective which is the minimization of patient waiting times which is similar to the objective of the collaborating dialysis unit. The difference of our work is, however, that we consider patient waiting times which occur before the start of the treatment and after the end of the treatment.
The analytical approach proposed in this paper can be categorized into and differentiated from the literature on patient scheduling as follows. One relevant paper focuses on hemodialysis scheduling but on a tactical decision level32. The authors schedule patients’ treatments across several days and not within a day as we do. Furthermore, we provide a decision support tool that allows managers to accommodate patient availability and schedule patients more efficiently. In another relevant paper, therapy jobs are scheduled hospital-wide15. The difference to our work is, again, that we provide a decision support tool that is based on an Open Source solver as compared to a commercial solver. Using Microsoft Excel and Open Source software increases the usability in the National Health Service because most of the computers have Microsoft Excel pre-installed, users are familiar with it and the Open Source package can be downloaded free and installed as a plugin. Another difference is that dialysis stations are considered as a scarce resource and patients’ clinical pathways consist of a setup, dialysis and a finish activity as our next section will reveal.
An Analytical Model
In what follows, we will introduce the parameters for our analytical model, the decision variables, objective function and constraints. Finally, an example schedule is given.
Parameters
Planning horizon, patients and activities
Let T :={1, 2,…,T} be the set of 15-minute slots with planning horizon T. In practice, we start the day at 7:00am and finish it at 11:00pm so that the planning horizon comes up to T = 64 periods enumerated using the set T := {1, 2, … , 64}. Dialysis patients are denoted by set P. A denotes the set of all clinical activities to be scheduled and denotes the subset of activities for patient .
Hospital resources, capacity and demand
Nurses and stations have a capacity Rtnurse and Rtstation, respectively, in period . For example, R1nurse= 1 means that 1 nurse is available between 7:00am and 7:15am. The demand of activity on nurses and stations is denoted by rinurse and ristation, respectively. This parameter will be used in the clinical pathways which are introduced next.
Clinical pathways
In our model, clinical pathways represent standardized, typically evidence-based health care processes as defined by van De Klundert et al.40. For more definitions and a literature review on clinical pathway modelling, see Aspland et al.41. We depict the clinical pathway of a patient as an activity-on-node graph in which the set of nodes represents the clinical activities. Weighted arcs represent minimum time lags between clinical activities3 and we write the activities’ capacity requirements below the nodes, see the legend in Figure 1.
Figure 1:
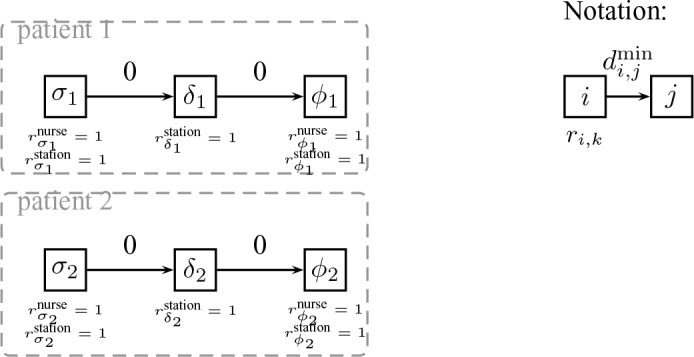
Clinical pathways for two dialysis patients
Consider, for example, patients’ set of dialysis activities which are the setup, dialysis and the finish activity, depicted by , respectively shown in Figure 1. means that the patients’ setup activity requires 1 nurse who is busy with the patient setting her up on the dialysis machine.
Let denote the set of all minimum time lags between clinical activities. A minimum time lag (i, j) of weight stipulates that activity j has to be scheduled at least periods later than activity i. Given the graph , the earliest and latest start of activities, denoted by Ei and Li, respectively can be calculated using longest path methods (see, for example,42). Let Wi := {Ei, Ei + 1, … , Li} denote the time window of activity i. Once we have calculated the latest time slot in which the dialysis activities can be scheduled, the index of the last period can be calculated by T = max Li. Table 2 provides an overview of all parameters and decision variables. The latter will be introduced next.
Table 2:
Sets, indices, constants and decision variables
| Parameter | Description | ||
| Set of activities | |||
| Set of activities corresponding to patient | |||
| Dialysis activity of patient p which excludes the setup and finish. They are modelled as separate activities. | |||
| Minimum time lag for precedence relation | |||
| Set of precedence relations | |||
| Earliest period to schedule activity | |||
| Latest period to schedule activity | |||
| Set of patients | |||
| Dialysis finish activity of patient | |||
| Duration of activity i | |||
| Nurse demand by activity | |||
| Station demand by activity | |||
| Nurse capacity in period (e.g. 1 nurse available in period 1) | |||
| Station capacity in period (e.g. 1 station available in period 1) | |||
| Dialysis setup activity of patient | |||
| Set of periods | |||
| Set of consecutive periods to schedule activity | |||
| Decision Variable | Description | ||
| 1, if activity i starts in period |
Decision variables
We use binary activity-to-period assignment variables, a concept which has been used successfully in other scheduling literature, see43. Accordingly,
Objective function
Having introduced all necessary parameters and decision variables, the objective functions are given by Equations (1) and (2).
| (1) |
| (2) |
Objective function (1) minimizes the maximum waiting time for patients to start the dialysis session as follows: Each patient p has a time window to start the session which is defined for the individual’s dialysis start activity σp (see the patients’ clinical pathways shown in Figure 1). Now, one decision variable xσP,t is equal to 1, we multiply the time point t which leads to the scheduled start times across all patients. Now, the maximum value of this start time vector is minimized. Similarly, for objective function (2), we minimize the maximum scheduled finish time of the treatments.
Constraints
In what follows, we add constraints to our model which we break down by clinical pathways, nurse and machine constraints.
Clinical pathways, nurse and machine constraints
Constraints (3) use the information from the clinical pathways defined earlier and ensure that minimum time lags between all consecutive activities are guaranteed.
| (3) |
Nurse constraints (4) ensure that the demand for nurses does not exceed the nurse capacity.
| (4) |
Constraints (5) ensure that the demand for the stations does not exceed the station capacity.
| (5) |
Constraints (6) ensure that each activity is scheduled exactly once.
| (6) |
Variable definitions and their domains are given by (7).
| (7) |
Example
Table 3 shows a station and nurse allocation example based on the clinical pathways defined in Figure 1. “–” means that the variables are not defined in these periods because they are outside the activities’ time windows. We assume that the processing times of the patients’ start activities are 1, the finish activities require two time periods and the durations of the dialysis take 4 and 1 period for patients 1 and 2 respectively. Naturally, the durations are longer in reality as the next section will reveal.
Table 3:
A station and nurse allocation example
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
| 1 | 0 | 0 | - | - | - | - | ||
| - | 1 | 0 | 0 | - | - | - | ||
| - | - | - | - | - | 1 | 0 | ||
| 0 | 1 | 0 | - | - | - | - | ||
| - | 0 | 1 | 0 | - | - | - | ||
| - | - | - | 1 | 0 | 0 | - | ||
| 1 | 1 | 0 | 1 | 1 | 1 | 1 | ||
| - | - | - | 1 | 0 | 0 | - |
The example reveals that the first activity is scheduled in period t = 1 which means that the nurse is allocated in the same period. In the next period (t = 2) the second patient’s first activity (σ2, see Figure 1) is scheduled which allocates the nurse in the second period (t = 2) as can be seen in the second to last row. In period t = 3, the nurse is not assigned to tasks that involve the connection and disconnection of patients to/from machines.
The last row shows the demand profile for the capacity requirement from the dialysis stations. As can be seen, one station is allocated in period t = 1, followed by an allocation of two stations in periods t = 2, 3,… , 6. As only one patient is on the station at period t = 7, the demand profile goes down to 1.
Decision Support Tool
We created a decision support tool in Microsoft Excel. The tool is broken down into a parameters tab which is shown in Figure 2, the solver tab shown in Figure 3, and a solution tab shown in Figure 4.
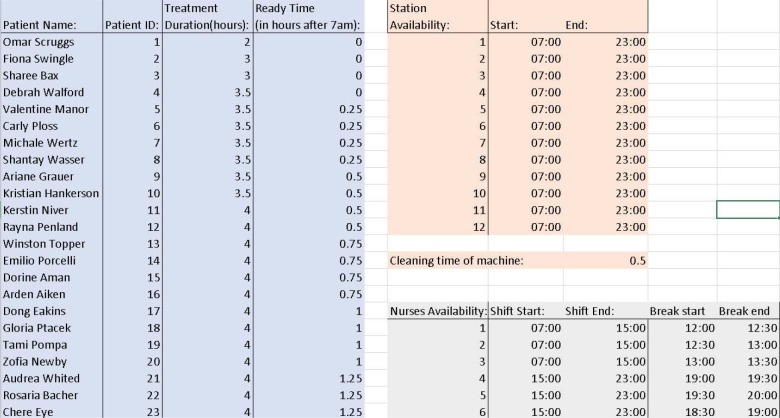
Figure 2:
Parameters for scheduling the patients in the Dialysis Unit. All patients’ names are synthetic.
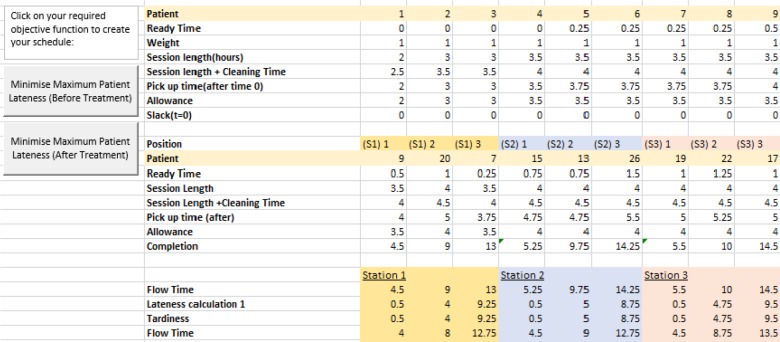
Figure 3:
Solving the problem of scheduling the patients in the Dialysis Unit
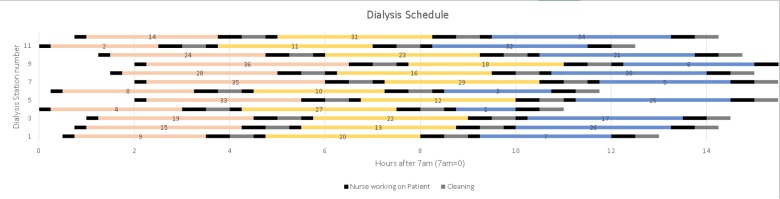
Figure 4:
Solution of scheduling the patients in the Dialysis Unit
Figure 2 shows the user interface where the manager can input each patient, along with their treatment duration and arrival time on the left-hand side. Sometimes, a station may be unavailable because of maintenance operations going on for the dialysis machine. Accordingly, the user can parametrize the station availability by using the “station availability table” on the right-hand side. The nurses’ availability and the cleaning time for the machines can also be inputted.
In Figure 3, the user can choose which objective function they wish to optimize when solving the scheduling problem. As mentioned in the modelling section, we have two patient lateness objectives, the first being the time they wait after arrival before starting their treatment, and the latter being the time a relative, Welsh ambulance or a private taxi service has to wait for the treatment to finish. Once the user selects the objective function, OpenSolver44 will use the inputted values and constraints to create a schedule which is then displayed to the clinician using metrics such as activity start times and lateness.
Figure 4 shows the output of the tool in a Gantt chart. For each station, we can see which patients have been scheduled at time t. The black bars relate to the patients’ start activity and finish activity (introduced in Figure 1). Recall that these activities require nurses in addition to the stations. The coloured bars relate to activity , where only the station is required for the actual dialysis activity .
Discussion
In several workshops we discussed the usability and acceptability of the platform with managers from the National Health Service. One major feedback to improve the usability of the platform was that we have to link our tool with the clinical information system which operates on a separate database. However, using an ODBC connection, we will be able to link Microsoft Excel with the patient data in the collaborating dialysis unit.
The usage of our platform will have several implications and benefits for different stakeholders: Using our tool, patients can be communicated an expected dialysis start time which may reduce perceived waiting time45. Nurses will be able to plan their breaks during the day which is very difficult at the moment because of the workload imposed by the unfavorable schedules: Currently, nurses struggle to take breaks during midday because patients who started the treatments in the morning finish at midday and need to be taken care of. In parallel, new patients who arrive at midday have to be setup on the machines and delays may impose overtime at the end of the nurses’ shifts. Another benefit of our structured approach is that transport services and patients’ caregivers can be informed about the scheduled dialysis finish times. Using information about the patients’ home addresses, transport services may aggregate trips for patients and provide more efficient services.
The mathematical model has been formulated as a deterministic problem which means that uncertainty is not taken into account at this stage. Uncertainty may happen in patients’ no shows, late arrivals and uncertain dialysis durations. Using information from the past, however, machine learning algorithms may be used to accurately predict no-shows46 which then can be incorporated into our tool. Alternatively, a rolling-horizon procedure may be used to take into account variation during the execution of the schedule.3,47,48
Conclusions
In this paper we have presented an analytical model and a decision support tool for the problem of scheduling dialysis patients in a dialysis unit in the UK. One objective is to minimize the maximum waiting time for patients to start the dialysis session. The second objective minimizes the maximum scheduled finish time of all treatments. In doing so, the model avoids nurses’ overtime at the end of the day. Using data from a hospital we demonstrated the effectiveness of our approach and showed the solution output using a Gantt chart. This helps the dialysis unit to find out the optimal sequence of patients on the different dialysis stations.
Future work will include further patient related objective functions including patient preferences, clinician guidelines and targets, and also taking into account resource-related measures such as utilization maximization. Furthermore, we will evaluate the importance of each of the different objectives and incorporate the result into a multi-criteria optimization approach. Also, our aim is to quantify the effectiveness of the approach in practice.
Acknowledgments This research was supported by the Welsh Health Hack 2017 in collaboration with the Welsh Government, Bevan Commission, ABCi and the Wales Deanery. Additional funding was received from the Bevan Commission’s Health Technology Exemplar scheme. Also, the Data Innovation Research Institute at Cardiff University provided Seedcorn Funding to support the project and to facilitate new collaborations.
Figures & Table
References
- 1.Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298((17)):2038–2047. doi: 10.1001/jama.298.17.2038. [DOI] [PubMed] [Google Scholar]
- 2.Gartner D, Padman R. In: Wickramasinghe N, editor. Handbook of Research on Healthcare Administration and Management. IGI Global: 2017. Mathematical Programming and Heuristics for Patient Scheduling in Hospitals: A Survey. pp. p. 627–645. [Google Scholar]
- 3.Gartner D. Springer Lecture Notes in Economics and Mathematical Systems.: Heidelberg; 2015. Scheduling the hospital-wide flow of elective patients. [Google Scholar]
- 4.Hulshof PJH, Kortbeek N, Boucherie RJ, Hans EW. Taxonomic classification of planning decisions in health care: A review of the state of the art in OR/MS. Health Systems. 2012;1((2)):129–175. [Google Scholar]
- 5.Ahmadi-Javid A, Jalali Z, Klassen KJ. Outpatient appointment systems in healthcare: A review of optimization studies. European Journal of Operational Research. 2017;258((1)):3–34. [Google Scholar]
- 6.Leeftink AG, Bikker IA, Vliegen IMH, Boucherie RJ. Multi-disciplinary planning in health care: A review. Health Systems. 2018:p. 1–24. doi: 10.1080/20476965.2018.1436909. Online first. Doi: 10.1080/20476965.2018.1436909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marynissen J, Demeulemeester E. Literature review on multi-appointment scheduling problems in hospitals. European Journal of Operational Research. 2019;272((2)):407–419. [Google Scholar]
- 8.Ceschia S, Schaerf A. Dynamic patient admission scheduling with operating room constraints, flexible horizons, and patient delays. Journal of Scheduling. 2016;19((4)):377–389. [Google Scholar]
- 9.Cardoen B, Demeulemeester E. A decision support system for surgery sequencing at UZ Leuven’s day-care department. International Journal of Information Technology and Decision Making. 2011;10((3)):435–450. [Google Scholar]
- 10.Cardoen B, Demeulemeester E, Beliën J. Sequencing surgical cases in a day-care environment: An exact branch-and-price approach. Computers and Operations Research. 2009;36((9)):2660–2669. [Google Scholar]
- 11.Cardoen B, Demeulemeester E, Beliën J. Optimizing a multiple objective surgical case sequencing problem. International Journal of Production Economics. 2009;119((2)):354–366. [Google Scholar]
- 12.Ceschia S, Schaerf A. Local search and lower bounds for the patient admission scheduling problem. Computers & Operations Research. 2011;38((10)):1452–1463. [Google Scholar]
- 13.Demeester P, Souffriau W, De Causmaecker P, Vanden Berghe G. A hybrid tabu search algorithm for automatically assigning patients to beds. Artificial Intelligence in Medicine. 2009;48((1)):61–70. doi: 10.1016/j.artmed.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 14.Range TM, Lusby RM, Larsen J. A column generation approach for solving the patient admission scheduling problem. European Journal of Operational Research. 2014;235((1)):252–264. [Google Scholar]
- 15.Gartner D, Frey M, Kolisch R. Hospital-wide therapist scheduling and routing: Exact and heuristic methods. IIE Transactions on Healthcare Systems Engineering. 2018;8((4)):268–279. [Google Scholar]
- 16.Bakker M, Tsui KL. Dynamic resource allocation for efficient patient scheduling: A data-driven approach. Journal of Systems Science and Systems Engineering. 2017;26((4)):448–462. [Google Scholar]
- 17.Greenroyd. Maximising patient throughput using discrete-event simulation. SIMULTECH 2017 - Proceedings of the 7th International Conference on Simulation and Modeling Methodologies, Technologies and Applications. 2017:p. 204–214. [Google Scholar]
- 18.Srinivas. Systematic review of opportunities to improve Outpatient appointment systems. 67th Annual Conference and Expo of the Institute of Industrial Engineers. 2017:p. 1697–1702. [Google Scholar]
- 19.Srinivas S, Ravindran AR. Optimizing outpatient appointment system using machine learning algorithms and scheduling rules: A prescriptive analytics framework. Expert Systems with Applications. 2018;102:245–261. [Google Scholar]
- 20.Liu E, Ma X, Sauré A, Weber L, Puterman ML, Tyldesley S. Improving access to chemotherapy through enhanced capacity planning and patient scheduling. IISE Transactions on Healthcare Systems Engineering. 2019:p. 1–13. Online first. Doi: 10.1080/24725579.2018.1442376. [Google Scholar]
- 21.Chaabane S, Meskens N, Guinet A, Laurent M. Comparison of two methods of operating theatre planning: Application in Belgian hospital. Journal of Systems Science and Systems Engineering. 2008;17((2)):171–186. [Google Scholar]
- 22.Hanne T, Melo T, Nickel S. Bringing robustness to patient flow management through optimized patient transports in hospitals. Interfaces. 2009;39((3)):241–255. [Google Scholar]
- 23.Jebali A, Alouane H, Atidel B, Ladet P. Operating rooms scheduling. International Journal of Production Economics. 2006;99((1-2)):52–62. [Google Scholar]
- 24.Lamiri M, Grimaud F, Xie X. Optimization methods for a stochastic surgery planning problem. International Journal of Production Economics. 2009;120((2)):400–410. [Google Scholar]
- 25.Lamiri M, Xie X, Dolgui A, Grimaud F. A stochastic model for operating room planning with elective and emergency demand for surgery. European Journal of Operational Research. 2008;185((3)):1026–1037. [Google Scholar]
- 26.Lamiri M, Xie X, Zhang S. Column generation approach to operating theater planning with elective and emergency patients. IIE Transactions. 2008;40((9)):838–852. [Google Scholar]
- 27.Min D, Yih Y. Scheduling elective surgery under uncertainty and downstream capacity constraints. European Journal of Operational Research. 2010;206((3)):642–652. [Google Scholar]
- 28.Ogulata SN, Erol R. A Hierarchical Multiple Criteria Mathematical Programming Approach for Scheduling General Surgery Operations in Large Hospitals. Journal of Medical Systems. 2003;27((3)):259–270. doi: 10.1023/a:1022575412017. [DOI] [PubMed] [Google Scholar]
- 29.Qu X, Peng Y, Kong N, Shi J. A two-phase approach to scheduling multi-category outpatient appointments - A case study of a women’s clinic. Health Care Management Science. 2013;16((2)):1–20. doi: 10.1007/s10729-013-9223-5. [DOI] [PubMed] [Google Scholar]
- 30.Riise A, Burke EK. Local search for the surgery admission planning problem. Journal of Heuristics. 2011;17((4)):389–414. [Google Scholar]
- 31.Testi A, Tánfani E. Tactical and operational decisions for operating room planning: Efficiency and welfare implications. Health Care Management Science. 2009;12((4)):363–373. doi: 10.1007/s10729-008-9093-4. [DOI] [PubMed] [Google Scholar]
- 32.Liu Z, Lu J, Liu Z, Liao G, Zhang HH, Dong J. Patient scheduling in hemodialysis service. Journal of Combinatorial Optimization. 2019;37((1)):337–362. [Google Scholar]
- 33.Intrevado P, Verter V, Tremblay L. Patient-centric design of long-term care networks. Health Care Management Science. 2019;22((2)):376–390. doi: 10.1007/s10729-018-9445-7. [DOI] [PubMed] [Google Scholar]
- 34.Lim C, Chodhari R. Re: A dynamic approach for outpatient scheduling. Journal of medical economics. 2017;20((11)):1126–1126. doi: 10.1080/13696998.2017.1360311. [DOI] [PubMed] [Google Scholar]
- 35.Conforti D, Guerriero F, Guido R. Non-block scheduling with priority for radiotherapy treatments. European Journal of Operational Research. 2010;201((1)):289–296. [Google Scholar]
- 36.Conforti D, Guerriero F, Guido R. Optimization models for radiotherapy patient scheduling. 4OR: A Quarterly Journal of Operations Research. 2008;6((3)):263–278. [Google Scholar]
- 37.Conforti D, Guerriero F, Guido R, Cerinic MM, Conforti ML. An optimal decision making model for supporting week hospital management. Health Care Management Science. 2011;14((1)):74–88. doi: 10.1007/s10729-010-9144-5. [DOI] [PubMed] [Google Scholar]
- 38.Schimmelpfeng K, Helber S, Kasper S. Decision support for rehabilitation hospital scheduling. OR Spectrum. 2012;34((2)):461–489. [Google Scholar]
- 39.Li X, Wang J, Fung RY. Approximate dynamic programming approaches for appointment scheduling with patient preferences. Artificial intelligence in Medicine. 2018;85:16–25. doi: 10.1016/j.artmed.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 40.van de Klundert J, Gorissen P, Zeemering S. Measuring clinical pathway adherence. Journal of Biomedical Informatics. 2010;43((6)):861–872. doi: 10.1016/j.jbi.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 41.Aspland E, Gartner D, Harper PR. Clinical Pathway Modelling: A Literature Review. Health Systems. 2019 doi: 10.1080/20476965.2019.1652547. On-line first. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Neumann K, Schwindt C, Zimmermann J. 2nd ed. Berlin:: Springer;; 2003. Project scheduling with time windows and scarce resources. [Google Scholar]
- 43.Koné O, Artigues C, Lopez P, Mongeau M. Event-based MILP models for resource-constrained project scheduling problems. Computers & Operations Research. 2011;38((1)):3–13. [Google Scholar]
- 44.Mason AJ. In: Operations Research Proceedings 2011. Springer; 2012. OpenSolver – An open source add-in to solve linear and integer progammes in Excel. pp. p. 401–406. [Google Scholar]
- 45.Gartner D, Padman R. Machine Learning for Healthcare Behavioural OR: Addressing Waiting Time Perceptions in Emergency Care. Journal of the Operational Research Society. 2019 Online first. Doi: 10.1080/01605682.2019.1571005. [Google Scholar]
- 46.Samorani M, LaGanga LR. Outpatient appointment scheduling given individual day-dependent no-show predictions. European Journal of Operational Research. 2015;240((1)):245–257. [Google Scholar]
- 47.Gartner D, Kolisch R. Scheduling the hospital-wide flow of elective patients. European Journal of Operational Research. 2014;223((3)):689–699. [Google Scholar]
- 48.Gartner D, Padman R. Flexible hospital-wide elective patient scheduling. Journal of the Operational Research Society. 2019 Online First. Doi: 10.1080/01605682.2019.1590509. [Google Scholar]