Abstract
As healthcare organizations continue to grow and evolve, migrations from one commercial electronic health record (EHR) system to another are likely to become more common. However, little is known about front-line clinicians’ and staff’s perceptions of such changes. Our study addresses this gap through an organization-wide survey of employees immediately prior to the transition to a new commercial EHR. We found that almost all front-line clinicians and staff were aware of the upcoming migration, and that most felt positive or neutral about the change, with only about 11% indicating that they were uncomfortable with the migration. Reasons for discomfort included the beliefs that the new EHR will be more time consuming to use and that moving to a new EHR is too costly, as well as concerns about the migration process. Attitudes differed by demographic characteristics and satisfaction with the current EHR. We discuss the implications of these results.
Introduction
While the investments made through the 2009 HITECH Act have resulted in significant progress in the adoption of electronic health record (EHR) systems in the U.S. over the last decade, this progress has come with some growing pains.1,2 Many healthcare organizations have now not only implemented an EHR but have also migrated from one EHR to another. The extant literature suggests that these migrations have met numerous challenges and that these challenges can put patient safety at risk.3 For instance, studies have found that technical issues (e.g., converting data to a new format) can create new work for users and result in continued parallel reliance on the old system.e.g.,4 In addition, physicians often perceive such changes negatively, for example, reporting that the new EHR is less efficient.5–7 In fact, Hanauer et al. reported that, even up to two years after migrating to a popular commercial EHR system, many physicians’ attitudes towards the new EHR were surprisingly negative.5
Existing studies have largely focused on migrations from locally developed, “homegrown,” EHRs to commercial systems.e.g.,4–7 In these cases, healthcare organizations are switching from an EHR that has been designed specifically for their particular context, but that may not be a comprehensive system with the more advanced functionalities offered by a mature commercial tool (e.g., clinical decision support). However, in recent years, it has become increasingly common for healthcare organizations to migrate from one commercial EHR to another commercial system. Like the aforementioned transitions, these migrations may be motivated by the need for a commercial tool with more advanced functionalities. In other cases, though, healthcare organizations have come to realize that the comprehensive commercial tool that they adopted is not optimal for their situation, prompting them to switch to a more suitable comprehensive commercial EHR.
Less is known about commercial-to-commercial migrations, especially how front-line clinicians and staff perceive the change.8,9 Our study addresses this gap through a survey assessing the attitudes and beliefs of employees at a large academic health system immediately prior to such a transition. The results of this survey have important implications for the migration at the study institution, as well as those considering or planning for a similar transition.
Methods
Institutional Setting
University of California, Irvine Health (UCI Health) is a large academic health system. In November 2017, UCI Health migrated from their existing comprehensive commercial EHR, Quest (Allscripts, Chicago, IL, USA), to another comprehensive commercial EHR, Epic (Epic Systems, Verona, WI, USA). UCI Health prepared clinicians and staff for this change in a number of ways such as in-person and online trainings.
Survey Development and Deployment
We developed a short survey to understand clinician and staff perceptions related to the upcoming migration from Quest to Epic. Specifically, we included structured questions to understand their satisfaction with Quest, awareness of and comfort with the upcoming migration to Epic, and reasons for their attitudes. Respondents were also able to provide unstructured (free-text) responses to several of the questions. The technology acceptance model (TAM) was used to guide survey development.
To minimize the burden on participants, we designed a skip pattern that ensured that they were only asked to respond to questions that were appropriate based on their previous answers. For instance, if a participant indicated that they did not know what Quest was, they were not asked to complete any additional questions. After the survey instrument was finalized, the questions and survey logic were entered into REDCap. The initial invitation email was sent through REDCap to 7,361 UCI Health employees on September 12, 2017. Two reminder emails were subsequently sent to non-respondents over the five weeks the survey remained open.
EHR Account Status and Demographics
In addition to the survey results, we also had an EHR account status dataset and a demographics dataset for all UCI Health employees. The former dataset included an identifier, Epic account status (active or inactive), date of last access, and provider type. The latter included the following variables: an identifier, department, years at UCI Health (as of the date they took the survey or, for non-respondents, September 18, 2017), FTE, shift, job title, and job family (i.e., job type).
UCI Health categorizes career opportunities into the following job families: (i) administrative/clerical (e.g., clerks, administrative assistants), (ii) clinical professional (e.g., case managers, social workers), (iii) executive (e.g., directors), (iv) finance/information technology (e.g., programmers), (v) management (e.g., administrative nurses), (vi) nursing (e.g., clinical nurses), (vii) professional (e.g., administrative analysts), (viii) support services (e.g., medical assistants, admitting workers), (ix) technician/technologist (e.g., anesthesia technicians), and (x) trades and services (e.g., mechanics). We separated out clinical support service (e.g., medical assistants) and other support service (e.g., medical records admin) jobs to better align with the other job families and because we believed that those with a patient care role may have a different perspective than those with a more administrative role. In addition, 2,881 records were missing the job family field, including all physicians, as well as those with a professor or instructor job title. Therefore, we created two new job families: physician and non-clinical professor/instructor. The latter category only included professors or instructors without an active EHR account, indicating that they are not practicing clinicians. After doing this, only 472 were missing the job family field. These were categorized into the existing job families as appropriate. For example, 98.8% of job titles that included the word ‘supervisor’ were associated with the management job family; thus, if the job title for a record without a job family included this term, it was categorized as management.
In addition to the existing variables, we also created a new variable, which we refer to as job level. We categorized employees into one of five different job levels based on their job title and/or job family: (i) trainee (e.g., ‘resident’ or ‘intern’ in job title), (ii) early-career/entry (e.g., ‘i’ or ‘ii’ in job title as in ‘clinical nurse ii’), (iii) mid-career (e.g., ‘iii’, ‘iv’, or ‘v’ in job title as in ‘biller iv’), (iv) senior (e.g., ‘lead’ in job title), and (v) leadership (e.g., ‘executive’ job family).
Data Analysis
We combined the three datasets for analysis. Structured data were analyzed using R v.3.5.1. After conducting univariate analyses, we assessed the representativeness of our sample. We then conducted bivariate analyses to evaluate whether survey responses varied by Epic account status and/or the demographic variables, as well as to determine whether responses to certain survey questions were associated with other survey responses. For instance, we hypothesized that satisfaction with Quest would be inversely related to comfort with the migration to Epic. In other words, those dissatisfied with Quest would be more likely to be comfortable with the migration to Epic than those satisfied with or neutral about Quest (and vice versa).
For categorical independent variables we used chi-square tests for independence of all factors. We then used adjusted standardized residuals to identify where the significant differences occurred. To correct for multiple comparisons, we applied the Bonferroni p-value correction method. In addition, for continuous independent variables we performed pairwise comparisons using t-tests with pooled standard deviations, and the Holm-Bonferroni p-value correction method to account for multiple comparisons.
Free-text survey responses were analyzed with NVivo v.12.2.0. We employed an inductive qualitative analysis approach and the constant comparison method to identify emergent categories and then to classify participants’ comments.10,11 We continued this process until no new categories emerged (theoretical saturation).12
This was a quality improvement study and was, thus, exempt from institutional review board review.
Results
Of those invited, 1,674 responded to the survey (22.7%). Nine did not fill out the first question; and 47 indicated that they did not know what is “Quest.” These 56 individuals were excluded from the analysis. Unsurprisingly, among those excluded, the majority were not active EHR users (60.7%, N=56). In addition, a relatively high percentage of respondents in non-clinical jobs were excluded from analysis, including non-practicing clinical professors/instructors (Excluded: 20%, N=20) and trades and services jobs (Excluded: 14.3%, N=14). On the other hand, responding physicians (0%, N=222), finance professionals (0%, N=45), executives (0%, N=26), and nurses (0.7%, N=401) were least likely to be excluded.
Relative to the entire population of UCI Health employees, physicians are underrepresented in the analyzed sample (Analyzed: 13.7% vs. Overall: 20.6%), while nurses (Analyzed: 24.6% vs. Overall: 18.9%) and managers (Analyzed: 10.4% vs. Overall: 5.0%) are overrepresented. Furthermore, while the percentage of respondents in early-career or entry-level, mid-career, and senior positions are similar to the overall population, a relatively lower percentage of trainees (e.g., residents) were included in the analysis (Analyzed: 5.1% vs. Overall: 10.8%).
Satisfaction with the Current EHR
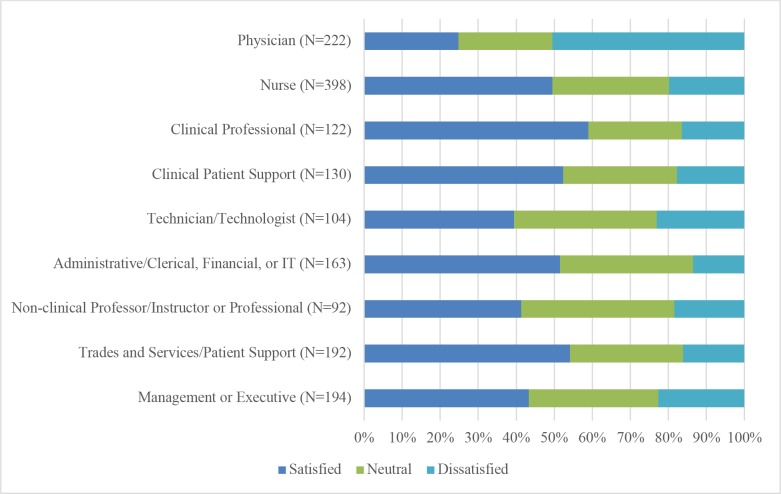
Among the analyzed sample (N=1,618), most were satisfied with Quest (45.9%), the EHR system currently used at UCI Health, or were neutral (31.0%). However, there were differences in satisfaction based on the respondent’s job type (χ2=133.41, df=16, p<0.001). Figure 1 presents a summary of these results. Upon examining the results of the post-hoc analysis (αadj=0.002, z criteria=-3.11), we found that significantly more physicians were dissatisfied with Quest than would be expected if there was no association between the two variables, and significantly fewer were satisfied than expected (N=222; Dissatisfied: 50.5%, radj=10.46; Satisfied: 24.8%, radj=-6.81).
Figure 1.
Satisfaction with the current EHR, Quest, by job type.
There was also a statistically significant association between satisfaction with Quest and job level (χ2=41.61, df=8, p<0.001). Specifically, the results show that significantly more trainees (e.g., residents) were dissatisfied with Quest than expected and significantly fewer were satisfied than expected (αadj=0.003, z criteria=-2.94; N=82; Dissatisfied: 48.8%, radj=5.69; Satisfied: 22.0%, radj=-4.48). Along these same lines, we also found that, on average, those satisfied with Quest had been employed at UCI Health longer than those who were dissatisfied with Quest (Satisfied: Mean=10.2 years, SD=7.98 vs. Dissatisfied: Mean=8.78 years, SD=7.74; p= 0.016).
Awareness of the Migration
The vast majority of respondents, 98.5%, were aware that UCI Health would soon replace the current EHR, Quest, with Epic, another electronic health record system (N=1,612). The high level of awareness was fairly uniform across demographic variables, with only negligible differences.
Attitude Toward the Migration
When asked about how they feel about UCI Health’s plan to replace Quest with Epic, most respondents indicated that they were comfortable with the migration (54.4%, N=1,601), with only 10.9% saying that they were uncomfortable. The remainder indicated that they felt neutral about the migration (34.7%).
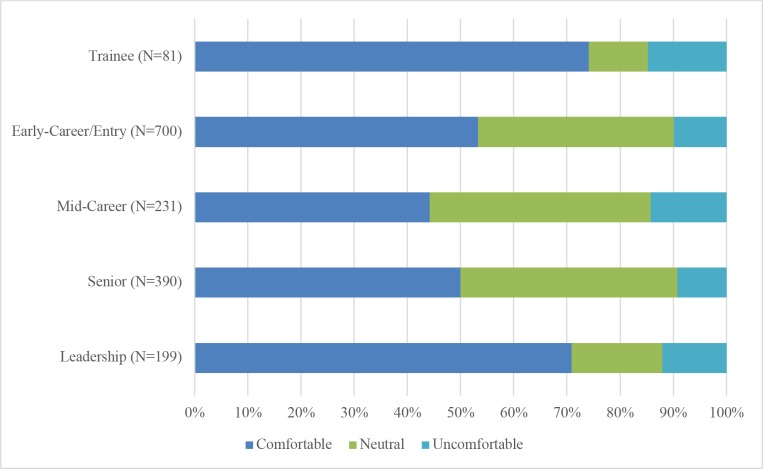
There was some variation in responses based on demographic variables, including type of job (χ2=78.6, df=16, p<0.001) and job level (χ2=66.15, df=8, p<0.001). The post-hoc analysis showed that, for job type (αadj=0.002, z criteria=-3.11), significantly more management/executives were comfortable with the migration than expected and significantly fewer than expected were neutral (N=190; Comfortable: 69.5%, radj=4.44; Neutral: 17.9%, radj=-5.19). In addition, significantly fewer physicians were neutral about the migration than expected (21.8%, N=220, radj=-4.33), while significantly more technicians/technologists were neutral about the migration than expected (53.8%, N=104, radj= 4.23).
For job level (αadj=0.003, z criteria=-2.94; See Figure 2), we found that the results for the leadership category were very similar to the management/executive job type category. We also found that significantly fewer in mid-career were comfortable with the migration than expected (44.2%, N=231, radj=-3.38). On the other hand, significantly more trainees were comfortable with the migration than expected and significantly fewer than expected were neutral (N=81; Comfortable: 74.1%, radj= 3.65; Neutral: 11.1%, radj=-4.58).
Figure 2.
Attitude toward the Epic migration by job level.
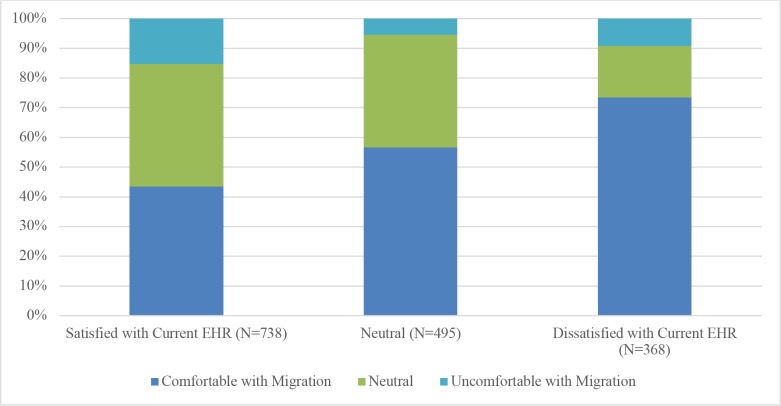
There was also a statistically significant difference in attitude toward the Epic migration based on satisfaction with Quest (χ2=110.79, df=4, p<0.001). These results are highlighted in Figure 3. Perhaps unsurprisingly, the post-hoc analysis (αadj=0.006, z criteria=-2.77) revealed that there were significantly more participants who were dissatisfied with Quest and comfortable with the migration than expected (73.4%, N=368, radj=8.32), while there were significantly fewer individuals satisfied with Quest and comfortable with the migration than expected (43.5%, N=738, radj=-8.10). In addition, participants who reported being satisfied with Quest and uncomfortable with the migration were observed significantly more than expected (15.3%, N=738, radj=5.28) and those neutral about Quest and uncomfortable with the migration were observed significantly less than expected (5.5%, N=495, radj=-4.66).
Figure 3.
Attitude toward the Epic migration by satisfaction with the current EHR, Quest.
Those who felt comfortable with migrating to Epic (N=871) were asked to provide a reason(s) for this perception (see Table 1). Among the 858 participants that selected at least one of the options, over half indicated that they believe that Epic will better support their clinical work (60.4%), will be less time consuming to use (58.7%), will make it easier to retrieve data (57.6%), and that Epic’s user interface is easier to learn and use (54.1%).
Table 1.
Respondents’ reasons for feeling comfortable or uncomfortable with the migration to Epic.
| Reason for Feeling Comfortable | Percentage of Participants (N=858) | Reason for Feeling Uncomfortable | Percentage of Participants (N=153) | ||||
| Epic will better support my clinical work | 60.4% | Epic will not support my clinical work as well | 24.8% | ||||
| Epic will be less time consuming to use | 58.7% | Epic will be more time consuming to use | 41.8% | ||||
| - | - | Moving to a new electronic medical records system is too expensive | 38.6% | ||||
| Epic will make it easier to retrieve data | 57.6% | Epic will make it more difficult to retrieve data | 22.2% | ||||
| Epic’s user interface is easier to learn and use | 54.1% | Epic’s user interface is more difficult to learn and use | 29.4% | ||||
| Epic will better support quality improvement | 33.6% | Epic will not support quality improvement as well | 16.3% | ||||
| Epic will better support population health management | 17.7% | Epic will not support population health management as well | 4.6% | ||||
| Epic will less likely interfere with my interaction with patients | 14.6% | Epic will more likely interfere with my interaction with patients | 14.4% | ||||
| Epic will better support research | 12.8% | Epic will not support research as well | 3.3% | ||||
| Epic has fewer patient safety risks | 11.4% | Epic has more patient safety risks | 11.8% | ||||
| Epic will better support the learning of medical students, residents, and fellows | 11.4% | - | - |
Those who felt uncomfortable with migrating to Epic (N=174) were also asked to provide a reason(s) why they felt this way (see Table 1). Although none of the response options were selected by fifty percent or more of the 153 participants that chose at least one reason, the four most commonly reported attitudes were that Epic will be more time consuming to use (41.8%), that moving to a new electronic medical records system is too expensive (38.6%), that Epic’s user interface is more difficult to learn and use (29.4%), and that Epic will not support their clinical work as well (24.8%).
In addition to the structured questions, participants had several opportunities to share unstructured comments. These free-text responses revealed additional insights into participants’ attitudes towards the migration to Epic and fell into two main categories – attitudes towards (1) the technologies (Quest and/or Epic) and (2) the migration process. First, as suggested by the quantitative results, many participants were positive about transitioning to Epic. This was generally either due to negative perceptions about Quest or positive perceptions about Epic. For instance, one person with little knowledge about Epic stated, “It couldn’t be any worse [than Quest].” Other participant comments focused on their positive beliefs or expectations about Epic, including that it will improve coordination and communication; has better system design, functionality, or usability; offers a process efficiency or otherwise better supports their work; or will improve outcomes such as increased patient safety (see Table 2). Participants indicated that their positive beliefs about Epic were largely based on their knowledge of the EHR market (e.g., “it is an industry standard”), personal experience with Epic at another institution, co-workers’ experiences with Epic, or organizational trust (e.g., “I am sure UCI has done enough research , and if it shows medical record improvement with Epic, why not”).
Table 2.
Summary of free-text survey results.
| Category | Example(s) | |
| Technologies | ||
| Negative Perceptions about Current EHR | • “I don’t know enough about Epic to know whether any of the above [reason feel comfortable question options] are true, but there’s no way that it won’t be better than Quest.” • “I believe Epic it’s from this century, not like Quest.” • “Currently, we use 3 to 4 different systems for our patients.” | |
| Positive Perceptions about New EHR | ||
| Improves Coordination and Communication• | • “Will have access of patient medical records chart across EPIC system” • “Epic will make coding easier in regards to work assignment…” | |
| Better System Design, Functionality, or Usability | “better reporting - real time” • “Epic gives more control to the user by more versatile” • “better and faster note template and loading” | |
| Offers Process Efficiency or Otherwise Better Supports Work | • “Automatically generates cost vs me having to manually input billing” • “Epic does not use the same Script as QUEST and the interface is set up like a Word document as opposed to the windows seen in QUEST so multitasking by writing notes and looking up labs is easier and more efficient” | |
| Improves Outcomes | “After Epic implementation, Epic alone will include these 3 to 4 systems to where nursing and radiology are using the same system, decreasing duplication of work, and increasing patient safety.” | |
| Migration Process | ||
| Insufficient Communication | “EPIC’s functionality and how it differs from Quest has not been made known to us…” | |
| Insufficient Training | “the training had an incomplete buildout and still a lot of unanswered questions. We need more training than is supplied in the on-line modules and the single face to face session.” | |
| Negative Perceptions about Migration Leadership | “The consultants that were hired to direct this project are ineffective.” | |
| Problems with Planning | • “I think the push to meet a target date is a little foolhardy. We should make sure the system works first, not worry about the calendar.” • “Why does administration think that the conversion from Quest to Epic will not impact our clinical practice and that we do not need to adjust patient volumes?” | |
Second, while some participants were not actually opposed to migrating to Epic, they did feel that certain aspects of the migration process had been problematic, including training, planning, communication, and leadership (see Table 2). Of these, insufficient training and the perception of poor planning were the most commonly mentioned. Several respondents felt that they were not adequately trained to use Epic and, thus, felt ill prepared for the upcoming change. For instance, one participant stated, “training end users with incomplete workflows that can impact patient care patient’s financial status. I do not feel we are ready for Go Live…” In addition, issues with the migration plan, especially the timeline, were also relatively common. For example, one person stated, “Concept is good, but timeline is too aggressive…” Finally, some respondents cited insufficient communication and negative perceptions of the migration leadership as sources of uncertainty or concern. For example, one participant stated, “EPIC’s functionality and how it differs from Quest has not been made known to us…” Another respondent commented, “The consultants that were hired to direct this project are ineffective.”
Discussion
Through a large survey of front-line clinicians and staff at UCI Health, we found that almost all were aware of the upcoming migration to a new comprehensive commercial EHR, and that most were fairly positive about this change. However, there was some variation in attitudes towards the migration based on satisfaction with the current comprehensive commercial EHR. In addition, we found that satisfaction with the current EHR varied based on job type, with a higher proportion of physicians being dissatisfied compared to other types of jobs. Qualitative results provided additional insights showing that positive attitudes towards the migration tended to either be based on dissatisfaction with the current EHR or on positive beliefs or expectations about the new system, while negative attitudes were not always related to the technology but, rather, sometimes stemmed from dissatisfaction with the migration process.
Overall, our results are more positive than the findings from studies that have focused on migrations from homegrown EHRs to commercial systems.e.g.,4–7 This may suggest relatively lower levels of clinician and staff resistance to transitions from one comprehensive commercial EHR to another. There could be a number of explanations for this. For instance, in homegrown-to-commercial migrations, clinicians’ loyalty to the homegrown system that was created specifically for their contexte.g.,6 and/or a general preference for simpler EHRs without advanced featurese.g.,13,14 could lead to resistance to the migration. While in the case of comprehensive commercial-to-comprehensive commercial transitions, on the other hand, clinicians and staff may not have the same loyalty to the existing system and have already adjusted to a comprehensive EHR, which could result in lower levels of resistance to change.
With that said, however, our results suggest that more could have been done to facilitate a smooth transition to the new EHR, including (1) supporting key clinical activities; (2) addressing commonly cited reasons for discomfort, and (3) improving training. These findings have implications for other healthcare organizations that are considering or planning for a similar change.
First, both among those who felt comfortable with migrating to a new EHR and those who felt uncomfortable with this change, most of the commonly reported reasons were related to day-to-day clinical practice as opposed to larger institutional goals such as supporting quality improvement. Others have suggested that misaligned clinical and organizational needs can contribute to clinician dissatisfaction with EHRs.e.g.,15 Thus, for such migrations to be successful, the new EHR needs to adequately support key clinical activities, and clinicians and staff need to be reassured of this fact (e.g., through trainings and other communications).
Second, healthcare organizations should also specifically address the commonly reported reasons that clinicians and staff feel uncomfortable with a migration. For instance, clearly communicating the differences between the current EHR and new EHR and why the investment in the new EHR is necessary, as well as incorporating clinician and staff suggestions to improve the migration process, could help to mitigate many of the concerns. In addition, it may be necessary to tailor messages about the migration to different groups who may be more resistant to the change (e.g., those who are more likely to be satisfied with the current EHR).
Finally, and as many others have noted, adequate end-user training and on-going support is essential when implementing a new EHR.e.g.,9,16 However, many of our participants perceived the training they had received thus far as insufficient – our participants wanted more personalized sessions and more opportunities to interact with the new EHR. Although there are some published training programs that end-users have found satisfactory,e.g.,16 more research is needed to understand which components are most helpful and how trainings can be effectively adapted for different contexts.
Although this survey was conducted at a single institution, it included a number of different perspectives, including physicians (from both inpatient and ambulatory care), nurses, other clinical professionals, and staff. Further research is needed to validate our findings across other institutions. In addition, future studies should consider a longitudinal approach to understand how front-line clinician and staff perceptions change once they have used the new comprehensive commercial EHR in practice. Existing research suggests that, in order to see physician satisfaction rise above baseline, follow-up may need to occur more than two years after migrating from a homegrown EHR to a commercial system.8 However, it remains to be seen if that will be the case for comprehensive commercial-to-comprehensive commercial migrations.
Conclusion
We found that, immediately prior to the transition, front-line clinicians and staff were more positive about the migration from one comprehensive commercial EHR to another than had been reported in the literature on migrations from homegrown EHRs to commercial systems. However, there were still some employees who were uncomfortable with the migration. Addressing the reasons for this discomfort could reduce resistance and increase satisfaction with the new EHR once it is implemented. Further research is needed to understand how clinician and staff perspectives change after this type of migration.
Figures & Table
References
- 1.Adler-Milstein J, Holmgren AJ, Kralovec P, Worzala C, Searcy T, Patel V. Electronic health record adoption in US hospitals the emergence of a digital “advanced use” divide. J Am Med Inform Assoc. 2017;24(6):1142–1148. doi: 10.1093/jamia/ocx080. doi:10.1093/jamia/ocx080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adler-Milstein J, DesRoches CM, Kralovec P. Electronic Health Record Adoption In US Hospitals Progress Continues, But Challenges Persist. Health Aff (Millwood) 2015;34(12):2174–2180. doi: 10.1377/hlthaff.2015.0992. doi:10.1377/hlthaff.2015.0992. [DOI] [PubMed] [Google Scholar]
- 3.Bowman S. Impact of electronic health record systems on information integrity quality and safety implications. Perspect Health Inf Manag. 2013;10(1c) [PMC free article] [PubMed] [Google Scholar]
- 4.Gettinger A, Csatari A. Transitioning from a Legacy EHR to a Commercial Vendor-supplied, EHR One Academic Health System’s Experience. Appl Clin Inform. 2012;03(04):367–376. doi: 10.4338/ACI-2012-04-R-0014. doi:10.4338/ACI-2012-04-R-0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hanauer DA, Branford GL, Greenberg G, et al. Two-year longitudinal assessment of physicians’ perceptions after replacement of a longstanding homegrown electronic health record does a J-curve of satisfaction really exist? J Am Med Inform Assoc. 2016 Jul; doi: 10.1093/jamia/ocw077. ocw077. doi:10.1093/jamia/ocw077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abramson EL, Patel V, Malhotra S, et al. Physician experiences transitioning between an older versus newer electronic health record for electronic prescribing. Int J Med Inf. 2012;81(8):539–548. doi: 10.1016/j.ijmedinf.2012.02.010. doi:10.1016/j.ijmedinf.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 7.Pfoh ER, Abramson E, Zandieh S, Edwards A, Kaushal R. Satisfaction after the transition between electronic health record systems at six ambulatory practices. J Eval Clin Pract. 2012;18(6):1133–1139. doi: 10.1111/j.1365-2753.2011.01756.x. doi:10.1111/j.1365-2753.2011.01756.x. [DOI] [PubMed] [Google Scholar]
- 8.Saleem JJ, Herout J. Transitioning from one Electronic Health Record (EHR) to Another: A Narrative Literature Review. Proc Hum Factors Ergon Soc Annu Meet. 2018;62(1):489–493. doi:10.1177/1541931218621112. [Google Scholar]
- 9.Penrod LE. Electronic Health Record Transition Considerations. PM&R. 2017;9:S13–S18. doi: 10.1016/j.pmrj.2017.01.009. doi:10.1016/j.pmrj.2017.01.009. [DOI] [PubMed] [Google Scholar]
- 10.Charmaz K. Constructing Grounded Theory 2nd edition. London ; Thousand Oaks, Calif: Sage. 2014 [Google Scholar]
- 11.Glaser BG, Strauss AL. The Constant Comparative Method of Qualitative Analysis. The Discovery of Grounded Theory. Chicago, IL: Aldine Transaction. 1967 [Google Scholar]
- 12.Conrad CF. A Grounded Theory of Academic Change. Sociol Educ. 1978;51(2):101. doi:10.2307/2112242. [Google Scholar]
- 13.Frankel RM. Computers in the Examination Room. JAMA Intern Med. 2016;176(1):128. doi: 10.1001/jamainternmed.2015.6559. doi:10.1001/jamainternmed.2015.6559. [DOI] [PubMed] [Google Scholar]
- 14.Toll E. The Cost of Technology. JAMA. 2012;307(23) doi: 10.1001/jama.2012.4946. doi:10.1001/jama.2012.4946. [DOI] [PubMed] [Google Scholar]
- 15.Mandl KD, Kohane IS. Escaping the EHR Trap — The Future of Health IT. N Engl J Med. 2012;366(24):2240–2242. doi: 10.1056/NEJMp1203102. doi:10.1056/NEJMp1203102. [DOI] [PubMed] [Google Scholar]
- 16.Pantaleoni JL, Stevens LA, Mailes ES, Goad BA, Longhurst CA. Successful Physician Training Program for Large Scale EMR Implementation. Appl Clin Inform. 2015;06(01):80–95. doi: 10.4338/ACI-2014-09-CR-0076. doi:10.4338/ACI-2014-09-CR-0076773. [DOI] [PMC free article] [PubMed] [Google Scholar]