Abstract
Aims
Large population-based studies have demonstrated increased prevalence of rotator cuff disease amongst diabetics. Recent studies have suggested comparable clinical outcomes from rotator cuff repair despite suggestions of increased complication rates amongst diabetics. However, there is a relative paucity of studies considering the effect of diabetes upon complication rate. We aim to report and quantify the effect of diabetes on complication rates following arthroscopic rotator cuff repair.
Materials and methods
A retrospective review of a consecutive series of patients undergoing arthroscopic rotator cuff repair between January 2011 and December 2014 was performed. Diabetic status and complication data defined as infection, frozen shoulder, re-tear or re-operation were collected and interrogated.
Results
A total of 462 patients were included at median follow-up of 5.6 years. Diabetics were significantly more likely to experience frozen shoulder (15.8% vs. 4.4%, p = 0.001), re-tear (26.3% vs. 15.6%, p = 0.042) or at least one complication following surgery (35.1% vs. 22.7%, p = 0.041) compared to non-diabetics. These equated to odds ratios of 4.03, 1.94 and 1.84, respectively.
Conclusions
Diabetic patients are almost twice as likely to experience complications following arthroscopic rotator cuff repair, including double the risk of repair failure and more than four times the risk of frozen shoulder.
Keywords: arthroscopy, complications, diabetes, rotator cuff, shoulder
Introduction
Rotator cuff disease is a common source of morbidity. Large population-based cohort studies have suggested diabetic patients are twice as likely to develop rotator cuff pathology1 and over 1.5 times more likely to undergo surgical rotator cuff repair2 than non-diabetics. Further, there is evidence that increased glycaemia – even within the normoglycaemic range – may be associated with rotator cuff disease.3
Although some series have reported inferior functional outcomes and range of motion in diabetics following rotator cuff repair,4 subsequent studies have suggested comparable clinical outcomes.5,6 This is despite suggestions of increased postoperative complications amongst diabetics.6,7 However, there is a paucity of contemporary studies evaluating the association between diabetes and postoperative complications. We aim to report and quantify the effect of diabetes on complication rates following arthroscopic rotator cuff repair.
Methods
A prospectively maintained database was interrogated to provide a single-centre consecutive series of patients. Inclusion criteria were all patients undergoing primary rotator cuff repair at our institution between January 2011 and December 2014. This time period was selected to provide adequate minimum follow-up whilst satisfying an a priori power calculation performed from a pilot study presented elsewhere. It was concluded that a cohort of 366 patients, of whom 47 were diabetic, would provide 95% power to detect differences in overall complication rate at a significance level of 0.01. Exclusion criteria comprised revision procedure, open procedure and those in whom rotator cuff repair was attempted but deemed inoperable at arthroscopic assessment.
Data collection was by retrospective analysis of the electronic patient notes at our institution. The primary outcome was collection of diabetic status and complication data. Diabetic status at the time of surgery was recorded dichotomously from the patient notes and corroborated against the preoperative glycated haemoglobin (HBA1C), which was also recorded. Patients who were not diabetic at the time of surgery, but have subsequently developed diabetes, were highlighted for subgroup analysis. Complication data were defined as: infection requiring intravenous antibiotics or surgical management; clinically significant frozen shoulder; clinically significant re-tear confirmed radiologically with ultrasonography or MRI; or re-operation/revision.
Statistical analysis was with the SPSS Statistics (IBM) software package. Continuous data were tested for parametricity using the Shapiro–Wilks test and groups subsequently compared with the Mann–Whitney test. Categorical data were interrogated with Fisher’s exact or Chi-square tests as appropriate. In all cases, significant was set at p < 0.05.
Results
Four hundred and sixty-three cases met the inclusion criteria. One patient died from an unrelated cause at one postoperative month and was therefore excluded. This left 462 cases for analysis at a median follow-up of 5.6 years (interquartile range (IQR) 4.7–6.4 years). Fifty-seven (12.3%) were diabetic. Follow-up and gender distribution did not differ between diabetic and non-diabetic cohorts, but age at surgery was slightly increased in the diabetic group (Table 1).
Table 1.
Demographics of diabetic and non-diabetic cohorts.
| Non-diabetic | Diabetic | Significance | |
|---|---|---|---|
| Number of patients | 405 | 57 | |
| Age at surgery (years; IQR) | 62.2 (54.1–69.3) | 66.4 (58.3–72.6) | p = 0.021a |
| Follow-up (years; IQR) | 5.57 (4.67–6.35) | 5.80 (4.82–6.35) | p = 0.445a |
| Gender distribution | 161F:244M | 28F:29M | p = 0.178b |
Note: Age and follow-up tested non-parametric with Shapiro–Wilks.
aMann–Whitney test.
bChi-square test.
In total, there were 6 (1.3%) cases of infection; 27 (5.8%) of adhesive capsulitis; 78 (16.9%) of re-tear and 61 (13.3%) of re-operation. Re-operation was revision rotator cuff repair with or without augmentation in 52 (85%), arthroscopic washout in 4 (6.6%), incision and drainage of a portal abscess in 2 (3.3%), debridement after failed revision in 2 (3.3%) and a single case of balloon interposition arthroplasty (1.6%).
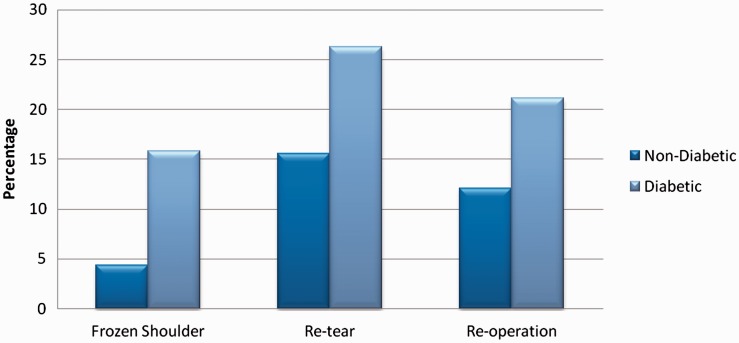
Diabetic patients were more than four times as likely to experience adhesive capsulitis (15.8% vs. 4.4%, p = 0.001, OR 4.03) and almost twice as likely to experience cuff re-tear (26.3% vs. 15.6%, p = 0.042, OR 1.94). Re-operation rate was greater in the diabetic cohort, though this did not reach statistical significance. Diabetic patients undergoing surgery were more likely to experience at least one complication (35.1% vs. 22.7%, p = 0.041, OR 1.84). These analyses are summarised in Table 2 and represented graphically in Figure 1. Excluding patients who were not diabetic at the time of surgery, but have subsequently become diabetic, ‘pre-diabetics’, yields similar results but with a trend towards increased significance and greater effect size (n = 451, Table 3).
Table 2.
Complications by cohort, significant results in boldface.
| Non-diabetic | Diabetic | Significance | Odds ratio (95% CI) | |
|---|---|---|---|---|
| Infection | 6 (1.5%) | 0 (0%) | p = 1a | – |
| Frozen shoulder | 18 (4.4%) | 9 (15.8%) | p = 0.001 b | 4.03 (1.72–9.47) |
| Re-tear | 63 (15.6%) | 15 (26.3%) | p = 0.042 b | 1.94 (.01–3.71) |
| Re-operation | 49 (12.1%) | 12 (21.1%) | p = 0.062b | 1.94 (0.96–3.91) |
| At least one complication | 92 (22.7%) | 20 (35.1%) | p = 0.041 | 1.84 (1.02–3.32) |
aFisher’s exact test.
bChi-square test.
Figure 1.
Percentage of patients experiencing frozen shoulder, re-tear or undergoing re-operation in the diabetic and non-diabetic cohorts.
Table 3.
Complications by cohort after exclusion of those considered ‘pre-diabetic’, significant results in boldface.
| Non-diabetic | Diabetic | Significance | Odds ratio (95% CI) | |
|---|---|---|---|---|
| Infection | 5 (1.3%) | 0 (0%) | p = 1a | – |
| Frozen Shoulder | 18 (4.6%) | 9 (15.8%) | p = 0.001 b | 3.92 (1.67–9.21) |
| Re-tear | 60 (15.2) | 15 (26.3%) | p = 0.036 b | 1.99 (1.04–3.81) |
| Re-operation | 47 (11.9%) | 12 (21.1%) | p = 0.056b | 1.97 (0.97–3.99) |
| At least one complication | 88 (22.3%) | 20 (35.1%) | P = 0.045 b | 1.88 (1.04–3.40) |
aFisher’s exact test.
bChi-square test.
Neither increasing age nor follow-up had significant associations with the exception of age and re-tear rate (Table 4, p = 0.004). Binary logistic regression subsequently demonstrates age as significantly associated with increased re-tear risk (pseudo-r2 0.034, p = 0.003).
Table 4.
Significance values of association between age and follow-up with occurrence of complications.
| Age | Follow-up | |
|---|---|---|
| Infection | p = 0.445 | p = 0.460 |
| Frozen shoulder | p = 0.152 | p = 0.416 |
| Re-tear | p = 0.004 | p = 0.201 |
| Re-operation | p = 0.926 | p = 0.828 |
| At least one complication | p = 0.237 | p = 0.529 |
Note: All analyses were independent Mann–Whitney tests. Significant results in boldface.
Median HbA1C within the diabetic cohort was 49 mmol/mol (IQR 45–57). Increasing HbA1C was not found to be associated with higher risk of frozen shoulder (p = 0.816), re-tear (p = 0.347) or re-operation rates (p = 0.314) on binary logistic regression modelling.
Discussion
The association between rotator cuff disease and diabetes mellitus is well established, as is the association between diabetes and adhesive capsulitis.8,9 The pathophysiology is complex and incompletely understood. Although thorough review of the pathogenesis is beyond the scope of this report, impaired microcirculation, proinflammatory environment secondary to cytokine overexpression, altered gene regulation, structural alterations secondary to glycosylation and perturbation of tendon-derived stem cells have all been implicated.10–13 A number of animal models, including one specific to surgically repaired rotator cuff, have demonstrated impaired healing and mechanically deficient tendon in diabetics.8,14–16
Our study has demonstrated that diabetes is associated with a notable increase in postoperative complications following arthroscopic rotator cuff repair. This is particularly pertinent given the increased prevalence of both rotator cuff disease and increasing trend for surgical repair in this cohort. Similar associations have been described following shoulder arthroplasty, where diabetes has been shown to be an independent risk factor for perioperative morbidity, increased complications and increased length of stay.17,18
We were unable to demonstrate an association between glycaemic control and increased complication rate within the diabetic cohort, as has been demonstrated elsewhere.6 However, we suspect this is due to the relatively small number of diabetics in our study making it underpowered to detect such a relationship. Similarly, exclusion of patients who subsequently became diabetic increased the majority of observed effect sizes, and therefore we hypothesise that this could represent increased risk in pre-diabetics. We advocate rigorous glycaemic control for those in whom rotator cuff repair is being considered.
There are a number of limitations to our study. We were unable to consistently gather co-variables such as smoking status, body mass index, type of diabetes and size of the rotator cuff tear from the electronic records and these were therefore excluded from the study protocol. The confounding effect of these variables is unclear. Furthermore, age was demonstrated as significantly associated with increased re-tear rate and given the increased age of the diabetic cohort this represents a source of bias. Finally, though able to comment on the incidence of frozen shoulder postoperatively, we lack the data to comment on the permanency of symptoms or responsiveness to management. Nevertheless, our data consistently demonstrate an association between diabetes and increased postoperative complications and has implications on surgical decision making and patient counselling in addition to the obvious cost implications.
Conclusion
Diabetic patients are almost twice as likely to experience complications following arthroscopic rotator cuff repair, including double the risk of repair failure and more than four times the risk of frozen shoulder. This must be borne in mind in all cases where surgical intervention is being considered in diabetic patients with rotator cuff tears, and the patient counselled accordingly.
Acknowledgements
Data from an earlier phase of this study were presented at the British Elbow and Shoulder Society (BESS) annual scientific meeting, Glasgow, 2018.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Lin TT, Lin CH, Chang CL, et al. The effect of diabetes, hyperlipidemia, and statins on the development of rotator cuff disease: a nationwide, 11-year, longitudinal, population-based follow-up study. Am J Sports Med 2015; 43: 2126–2132. [DOI] [PubMed] [Google Scholar]
- 2.Huang SW, Wang WT, Chou LC, et al. Diabetes mellitus increases the risk of rotator cuff tear repair surgery: a population-based cohort study. J Diabetes Complications 2016; 30: 1473–1477. [DOI] [PubMed] [Google Scholar]
- 3.Longo UG, Franceschi F, Ruzzini L, et al. Higher fasting plasma glucose levels within the normoglycaemic range and rotator cuff tears. Br J Sports Med 2009; 43: 284–287. [DOI] [PubMed] [Google Scholar]
- 4.Dhar Y, Anakwenze OA, Steele B, et al. Arthroscopic rotator cuff repair: impact of diabetes mellitus on patient outcomes. Phys Sportsmed 2013; 41: 22–29. [DOI] [PubMed] [Google Scholar]
- 5.Miyatake K, Takeda Y, Fujii K, et al. Comparable clinical and structural outcomes after arthroscopic rotator cuff repair in diabetic and non-diabetic patients. Knee Surg Sports Traumatol Arthrosc 2018; 26: 3810–3817. [DOI] [PubMed] [Google Scholar]
- 6.Cho NS, Moon SC, Jeon JW, et al. The influence of diabetes mellitus on clinical and structural outcomes after arthroscopic rotator cuff repair. Am J Sports Med 2015; 43: 991–997. [DOI] [PubMed] [Google Scholar]
- 7.Chen AL, Shapiro JA, Ahn AK, et al. Rotator cuff repair in patients with type I diabetes mellitus. J Shoulder Elbow Surg 2003; 12: 416–421. [DOI] [PubMed] [Google Scholar]
- 8.Lui PPY. Tendinopathy in diabetes mellitus patients-Epidemiology, pathogenesis, and management. Scand J Med Sci Sports 2017; 27: 776–787. [DOI] [PubMed] [Google Scholar]
- 9.Zreik NH, Malik RA, Charalambous CP. Adhesive capsulitis of the shoulder and diabetes: a meta-analysis of prevalence. Muscles Ligaments Tendons J 2016; 6: 26–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hsu C-L, Sheu WHH. Diabetes and shoulder disorders. J Diabetes Investig 2016; 7: 649–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chung SW, Choi BM, Kim JY, et al. Altered gene and protein expressions in torn rotator cuff tendon tissues in diabetic patients. Arthroscopy 2017; 33: 518–526.e1. [DOI] [PubMed] [Google Scholar]
- 12.Patel SH, Sabbaghi A, Carroll CC. Streptozotocin-induced diabetes alters transcription of multiple genes necessary for extracellular matrix remodeling in rat patellar tendon. Connect Tissue Res 2018; 59: 447–457. [DOI] [PubMed] [Google Scholar]
- 13.Lin Y-C, Li Y-J, Rui Y-F, et al. The effects of high glucose on tendon-derived stem cells: implications of the pathogenesis of diabetic tendon disorders. Oncotarget 2017; 8: 17518–17528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Connizzo BK, Bhatt PR, Liechty KW, et al. Diabetes alters mechanical properties and collagen fiber re-alignment in multiple mouse tendons. Ann Biomed Eng 2014; 42: 1880–1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bedi A, Fox AJS, Harris PE, et al. Diabetes mellitus impairs tendon-bone healing after rotator cuff repair. J Shoulder Elbow Surg 2010; 19: 978–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Egemen O, Ozkaya O, Ozturk MB, et al. The biomechanical and histological effects of diabetes on tendon healing: experimental study in rats. J Hand Microsurg 2012; 4: 60–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mahure S, Mollon B, Quien M, et al. Impact of diabetes on perioperative complications in patients undergoing elective total shoulder arthroplasty. Bull Hospital Jt Dis (2013) 2017; 75: 173–179. [PubMed] [Google Scholar]
- 18.Ponce BA, Menendez ME, Oladeji LO, et al. Diabetes as a risk factor for poorer early postoperative outcomes after shoulder arthroplasty. J Shoulder Elbow Surg 2014; 23: 671–678. [DOI] [PubMed] [Google Scholar]