Abstract
Coronal shear fractures of the distal humerus are a unique subset of distal humeral fractures which entail partial or complete articular fractures of the distal humerus without involvement of the columns. The very distal nature of these fragments, their small size and propensity for comminution render them challenging to treat surgically. The purpose of this article is to describe the classification, outcomes and surgical techniques currently used for the treatment of these fractures using the available literature and authors' clinical experience.
Keywords: capitellum, coronal, fixation, fractures, shear, trochlea
Introduction
Coronal shear fractures of the distal humerus are a challenging subset of fractures that affect the distal humeral articular surface. These fractures usually involve the capitellum with frequent extension into the trochlea. The spectrum of severity ranges from relatively simple fractures with uni-planar fracture lines to highly comminuted multi-planar fractures with bony impaction and associated ligamentous injuries.
Increasing articular and posterior column comminution is associated with worsening outcome because of difficulty achieving anatomic, stable fixation.1,2 Possible sequalae include stiffness, pain, avascular necrosis and post-traumatic arthritis. Consequently, these fractures require careful pre-operative evaluation and an individualised approach to treatment with respect to surgical approach, fixation principles and implant choice.
The aim of this article is to outline a systematic approach to treatment of these injuries based on the pertinent characteristics of each fracture. The described techniques are specifically for isolated coronal shear fractures of the articular surface rather than condylar distal humeral fractures with a coronal shear component.
Epidemiology
Coronal shear fractures of the distal humerus account for 1% of elbow fractures and 6% of distal humeral fractures.3 They occur in both adults and children, with the elderly prone to more comminuted fractures.4
The most common injury mechanism in females is a low energy fall onto an outstretched hand, particularly in older individuals. Higher energy fractures such as motor vehicle accidents or falls from height tend to occur in younger or male patient.1,5,6 The characteristic coronal plane fracture most likely occurs from combined axial loading of the articular surface with a ‘shearing’ injury caused by transient dislocation or subluxation of the radial head and coronoid. This mechanism also explains the high rate of associated elbow injuries which most frequently include lateral collateral ligament (LCL) tears and fractures of the radial head.1,7–11
Pre-operative planning
Clinical assessment
Patients with high-energy injuries should be treated in accordance with Advanced Trauma Life Support guidelines.
With regard to elbow, there should be an awareness and scrutiny for potential associated bony and soft tissue injuries, particularly in the setting of a dislocation. Longitudinal instability of the forearm should be considered in the presence of a radial head and capitellar fracture, and in this scenario, the wrist should be examined carefully. Although rare, neurovascular injuries and compartment syndrome should also be screened for.
Radiographic assessment
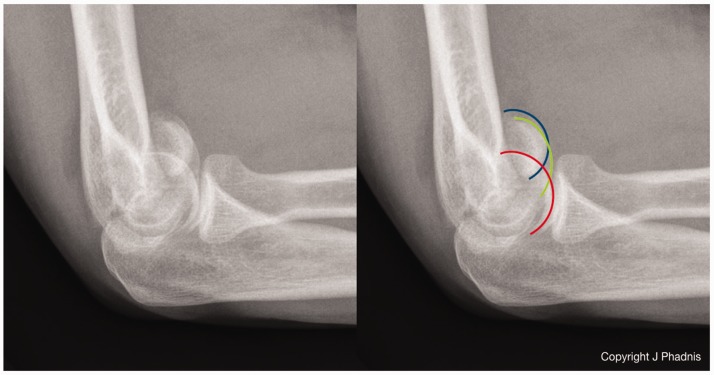
Standard antero-posterior (AP) and lateral elbow radiographs should be obtained; however, these are known to underestimate the fracture extent. A ‘double-arc sign’ seen on the lateral view indicates more extensive involvement of the articular surface than just the capitellum. This sign represents the subchondral bone of the capitellum and lateral trochlear ridge, rotated and displaced in continuity with each other.6 In more comminuted fractures, a ‘triple arc sign’ is visible (Figure 1). This represents a more extensive fracture where the articular elements may not be in continuity with each other.5,6,12 AP radiographs are often difficult to interpret because of the flexed position of the fragments but may show additional sagittal plane fracture lines representing further comminution of the articular surface.
Figure 1.
A triple arc sign indicating extensive involvement of the articular surface with significant comminution likely.
The difficulties with radiographic interpretation and the impact this has on surgical treatment mean that there should be a very low threshold for CT scanning in the assessment of these injuries. 3D CT scanning has been demonstrated to correlate strongly with intra-operative findings and allows accurate assessment of surgically relevant factors such as articular comminution, fracture line orientation and posterior comminution. This allows meticulous pre-operative planning which is likely to improve patient outcome.6,13,14
Classification
Several classification systems have been presented, although most are descriptive with limited value in predicting clinical outcomes.5,15,16
Bryan and Morrey focused on the capitellum describing three subtypes of fracture. Type 1 (Hahn–Steinthal fracture) involves a thick hemispherical fragment; Type 2 (Kocher–Lorenz fracture) is a thin osteochondral injury and Type 3 are comminuted fractures.15 McKee et al. subsequently added a Type 4 fracture in recognition of the frequent extension into the lateral trochlea.6
The Ring classification combined intra-operative findings with pre-operative X-rays to create five subtypes with recognition of epicondylar involvement and posterior impaction as a common feature of these fractures.5
More recently, Dubberley et al. described a classification system based on 28 patients who underwent internal fixation. This system is of particular value, as it incorporates information on the fracture's anatomic pattern, the number of fragments and the extent of posterior comminution, all of which affect surgical decision making and provide prognostic value based on their series of patients.1 Type 1 fractures involve the capitellum, with or without the lateral trochlea ridge; Type 2 involves the capitellum in continuity with more extensive extension into the trochlea and Type 3 describes separate capitellar and trochlea fragments. Each type is further divided into subtype A (no posterior comminution) and subtype B (posterior comminution).
This is our preferred classification system because of its influence on surgical decision making. In addition, we propose addition of a ‘Type 4 fracture’ which represents a Type 3 fracture with associated sagittal and axial plane fracture lines, creating multiple small fragments of the capitellum and trochlea (Figure 2). This fracture pattern is a rare but particularly challenging variant seen most often in osteoporotic bone and may require alternate surgical management, which is discussed later in this article.
Figure 2.
Modified Dubberley Classification of capitellar fractures illustrating the addition of a Type 4 fracture defined by the presence of multiple sagittal and coronal plane fracture lines.
Two further factors which affect surgical decision making and outcome that should be considered in pre-operative planning are the amount of subchondral bone stock within the fragments and evidence of associated bony and ligamentous injuries. Subchondral bone within the major fragments can be seen on CT imaging and influences implant choice, while the presence of elbow instability can be inferred from the patient's history and imaging and requires treatment to prevent adverse outcome.
Management
Non-operative treatment
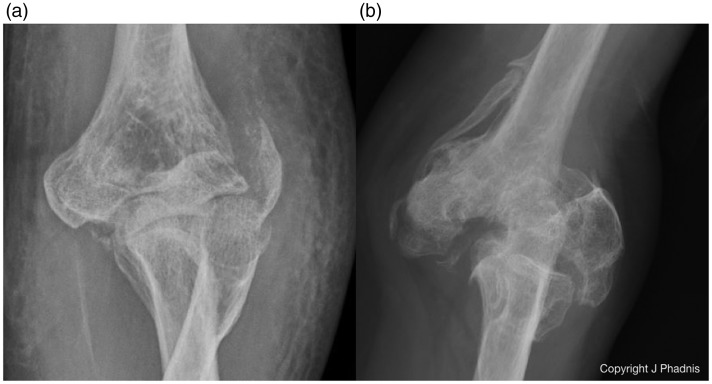
Conservative management of these fractures should be considered for older patients with low functional demands or pre-existing cognitive or physical impairments. Good results have been reported for the treatment of distal humerus fractures in select older patients by several authors; however, there is little information on the outcome after coronal shear fractures specifically. Desloges et al. reported two displaced coronal shear fractures in their series of non-operatively treated distal humeral fractures.17 One patient with an undisplaced trochlea fracture did well, whereas the other who had a proximally displaced trochlea fragment did poorly. Similarly, for fractures involving the columns, they found that patients with a stable medial column and secondary ulnohumeral congruity fared better than those with medial column displacement. In coronal shear fractures, the columns are intact by definition, and although it is possible for some patients to develop secondary congruency and achieve a satisfactory outcome with non-surgical management, this treatment is reserved for select patients that are not good candidates for surgery (Figure 3).
Figure 3.
A Type 3B fracture treated non-surgically in a patient with significant medical co-morbidities. (a) Three years later, there is secondary radiographic congruency and a satisfactory outcome despite some restriction in motion and no further treatment was required.
Closed reduction and immobilisation
Several authors have reported satisfactory outcomes with closed reduction and plaster immobilisation. Reduction is achieved through traction with gradual flexion, and direct pressure on the flexed fragments to aid reduction. Supination and varus stress during these manoeuvres may also be of value in aiding reduction.10,18–22 Late displacement is a recognised complication of closed reduction which is more likely in comminuted fractures or significantly displaced fractures with disruption of the anterior superior periosteal hinge.10
Surgical treatment
Patient positioning and consideration of skin incisions
The supine position allows circumferential access to place incisions around the whole elbow for any chosen approach. The arm is placed on a hand table to perform medial or lateral approaches and over the patient's chest for posterior approaches. In the supine position, both AP or posterior to anterior (PA) fixation of lateral and medial fragments can be readily performed.
A lateral position is beneficial if a posterior skin incision is chosen. Fasciocutaneous flaps can be elevated and muscular intervals used to access all aspects of the elbow, although it is more difficult to place AP screws while in the lateral position particularly if these are required for the trochlea. Prone positioning compounds this problem and is also awkward for anaesthesia.
If both sides of the elbow need to be exposed, separate lateral and medial incisions may be preferable to avoid the risk of seroma formation with a posterior skin incision and reduce the risk of flap necrosis.
Anterolateral approach
This inter-nervous approach between the brachialis and brachioradialis provides ‘face on’ access to the capitellum and is appropriate for simple Type 1 and 2 fractures. The disadvantage is that it is not extensile, requires dissection and retraction of the radial nerve and does not allow visualisation of the posterior aspect of the capitellum which means it is unsuitable for cases with posterior comminution. While placement of AP fixation is straightforward, it is not possible to place PA fixation or posterolateral plates through this approach.
Lateral approaches
For Type 1 and 2 fractures, a lateral approach is most commonly used. The medial component of fractures that extend into the trochlea can be reduced indirectly because the fragment is in continuity with the capitellum. In Type 3 fractures where a separate trochlea fracture fragment is present, a more extensile variation of the lateral approach may also be suitable; however, it can be challenging to reliably visualise, reduce and stabilise a separate trochlea fragment, which lies medial to the trochlea groove through a lateral approach alone.
There are several variations of the lateral approach depending on how extensile the exposure needs to be. Isolated capitellar fractures (Type 1) can be accessed by elevating the extensor carpi radialis longus (ECRL) and anterior capsule from the lateral column. The common extensor origin is split longitudinally anterior to the LCL. The approach can be extended as far distally as the posterior interosseous nerve and as far proximally as the radial nerve. Concomitant LCL injuries should be looked for and addressed during this approach.
Osteotomy of the lateral epicondyle or reflection of the LCL origin provides more extensile exposure as the elbow can be hinged open on the intact medial collateral ligament. CT evaluation of high-grade fractures frequently shows the lateral epicondyle to be a separate fragment which can be utilised as an osteotomy if present (Figure 4). It is essential to restore the integrity of the LCL by repairing the ligament if it has been reflected or to incorporate the fractured/osteotomised epicondyle into the final fixation to prevent posterolateral rotatory instability.
Figure 4.
A Type 3B fracture treated through an extensile lateral approach. The lateral epicondyle fragment which is a consistent fragment in these fractures was used to reflect the lateral collateral ligament and allow the elbow to be hinged open. Hybrid fixation with a posterolateral plate and independent buried k wires was performed.
AP or PA screw fixation and posterolateral plating can be performed through the lateral approaches. In addition, posterior articular impaction can be addressed through these approaches, and if necessary, bone graft from the lateral olecranon may be taken through the same skin incision.
Hence, the majority of coronal shear fractures can be addressed through an extensile lateral approach; however, surgeons must be aware of the fracture patterns that are more difficult to treat through this approach and recognise these during pre-operative planning.
Combined medial and lateral approaches
For Type 3 and 4 fractures, where better visualisation of the trochlea fracture reduction is required, a separate medial approach can be added. A medial approach will also provide an improved angle of fixation for medial trochlea fragments. An ‘over the top’ approach, as described by Hotchkiss, is useful, as it preserves the MCL and is extensile enough to allow fixation.23 This approach provides good access to the anterior third of the medial trochlea but requires quite an extensive dissection and does not allow easy visualisation of the posterior trochlea because of the intact coronoid and greater sigmoid notch. The more posteriorly based medial approach described by Taylor and Scham is more extensile but requires much more soft tissue stripping and is still limited by the intact coronoid and greater sigmoid notch which cover the trochlea articular surface.24
Posterior approaches – Olecranon osteotomy
Type 3 and 4 fractures, particularly those with posterior comminution, can be exposed through an olecranon osteotomy. The advantage of an osteotomy is preservation of the medial and LCLs with wide exposure of the majority of the articular surface. It is important to emphasise that an olecranon osteotomy on its own, does not provide full exposure, as the anterior articular surface and anterior hinge (where the cartilage meets the anterior distal humerus) are not clearly exposed even with maximal elbow flexion. In order to visualise this area, which is a critical reference point for anterior reduction, it is necessary to either create a further lateral window by elevating the ECRL, anterior capsule and brachialis from the humerus.
Posterior approaches – Triceps sparing
A triceps sparing approach, such a para-olecranon or para-tricipital approach, combined with subperiosteal elevation of the collateral ligaments and dislocation of the humerus, allows circumferential access to the articular surface for Type 3 and 4 fractures which is superior to that seen through an olecranon osteotomy (Figure 5). Preservation of the extensor mechanism is advantageous for rehabilitation, strength and at minimising re-operations seen with osteotomies. It is paramount that the collateral ligaments are repaired soundly enough to maintain joint stability and permit early range of motion when using this approach.
Figure 5.
A Type 4B fracture treated using a lateral para-olecranon approach. The whole distal humerus has been subluxated through the lateral triceps split leaving the triceps tendon attached to the olecranon (black asterisk). Circumferential access allows anatomic reduction of all fracture fragments.
These approaches are also recommended over olecranon osteotomy if an arthroplasty may be required in order to prevent compromise of the olecranon articular surface (hemiarthroplasty) or the ulna component fixation (total elbow arthroplasty (TEA)).
Other posterior approaches such as a triceps tongue or triceps reflecting approach may be considered but are not performed in the authors' practice.
Fixation techniques
Fragment excision
This was the original technique described for capitellar fractures with satisfactory results reported.10,25–28 As fixation techniques have developed, we have moved towards fragment fixation for the majority of cases; however, excision remains a viable option for small osteochondral fragments and can be performed arthroscopically to reduce morbidity.29 Cadaveric data suggest that capitellar excision does not result in instability when the remaining articular congruity is preserved and ligament constraints are intact.8,30 In contrast, excision of larger fragments that involve the lateral trochlea ridge is likely associated with inferior results because of valgus instability and secondary arthritis, pain and stiffness. Caution should be exercised if considering fragment excision because of the high incidence of associated ligament injuries often not recognised in these fractures.31
Multiple threaded k wires
The use of multiple threaded k wires alone or as an adjunct to other methods of fixation has been described as a suitable technique to stabilise fracture fragments particularly those, which are small in size32–34 (Figure 4). Threaded k wires should be used in preference to smooth wires to minimise the risk of wire migration and consideration should be given to the position of wire placement, so that they can be retrieved as easily as possible should they back out or the fragments resorb.
Independent screw fixation
This is the most common technique used for treating coronal shear fractures and is associated with good outcomes in the literature.3,9,13,35–39 This is an appropriate technique for more simple fracture patterns, where there is no posterior comminution or bone loss present (Dubberley Type 1A and 2A)3,9,36,38 (Figure 6). Despite the frequent use of independent screws, there is limited evidence regarding optimal screw type and direction of placement.40,41 Elkowitz et al. performed a cadaveric study, comparing AP and PA fixation with 4.0 mm partial threaded cancellous screws. The study demonstrated that 4.0 mm partially threaded cancellous screws used in a PA direction displaced to a lesser degree on cyclic loading, than identical screws placed in an AP direction, although there was no difference in load to failure between the two constructs. Splits were identified in the articular surface when AP screws were used; however, this may have been related to the large size of the screw tested and the force required to countersink them. In the second part of the study, AP fixation using two headless compression screws (Acutrak 4.6 mm, Acumed Hillsboro Oregon) was compared with the initially superior PA cancellous screw construct.40 This demonstrated that the headless AP fixation was superior in terms of cyclic displacement and load to failure. In a further study, the same group compared two types of headless compression screw (Acutrak & Herbert, Zimmer Biomet Warsaw Ind) placed in an AP direction, concluding that the Acutrak screws were superior.41
Figure 6.
A Type 2A fracture with associated radial head fracture treated using buried 2 mm AP locking screws. A lateral epicondyle fragment was reflected to increase exposure and incorporated into the fixation with a cortical screw (asterisk).
There are no data available on the biomechanical performance of smaller screws, multiple screws and screws placed in different orientations or the long-term effect of placing screws through the articular surface.
Independent screw fixation is frequently used for Dubberley Type 1A and 2A fractures. We prefer to use multiple small diameter AP screws placed in different orientations. AP screws are advantageous in that they reduce the need for posterior dissection, which respects the capitellar blood supply and allows stabilisation of smaller fragments with poor subchondral bone stock more effectively (Figure 6).
The most common types of screw used in the literature are either fully threaded cortical or cancellous screws, or cannulated headless compression screws. Screws with heads need to be countersunk within the articular surface. Compression of the fracture is achieved by applying a clamp to compress, while the screws are placed.
Headless compression screws are commonly used, as they seat more easily beneath the articular surface and exert compression through the screw itself. However, because of the cannulation, they tend to be larger in diameter than the smallest non-cannulated screws and therefore create a larger hole in the articular cartilage. Care is also required with shallow fragments, as headless screws may not exert compression or gain satisfactory purchase.
A novel alternative to headless, cortical or cancellous screws is the use of locking screws buried within the articular cartilage. Locking screws have a low profile compared to a cortical screw and the threads within the head allow neat countersinking of the screw while still providing a firm purchase. In addition, very small diameter screws can be used, which allow multiple screws to be placed with minimal violation of the articular cartilage (Figure 6).12
Pre-contoured locking plates
A posterolateral pre-contoured locking plate should be considered for more complex fractures with posterior comminution and bone loss (Dubberley subtype B fractures). The plate is used to ‘create a posterior cortex’ through which fixed angle PA screws are placed into the articular fragments. A posterolateral plate with a lateral extension (Figure 4) is particularly effective for Dubberley Type 2–4 fractures. The extension captures the consistent lateral epicondyle fragment and allows placement of a medially directed screw into the trochlea fragment creating a construct with multi-planar fixed angle fixation. A lateral plate may also be used if there is no significant posterior comminution in order to buttress a comminuted epicondyle fragment and still allow screw fixation into the medial trochlea (Figure 7).
Figure 7.
Dubberley Type 3A Fracture treated through an extensile lateral exposure with independent buried locking screws and a lateral buttress plate to stabilise a comminuted lateral epicondyle fragment.
Rarely, a supplementary medial peri-articular plate can be used to create an even more stable fixed angle construct with screws directed into the capitellum from the medial column.
Anti-glide plates
Anti-glide plates are a useful adjunct for highly unstable fracture fragments with no intact anterior periosteal hinge.42,43 Typically, a one third tubular plate (3.5 mm for large fragments and 2.7 mm for smaller fragments) is applied to the anterior humerus without contouring. The end of the plate is used to capture the superior edge of the articular fragment.44 A cortical screw placed proximal to the fracture is used to create an anti-glide construct which neutralises shear forces (Figure 8). Care is needed not to place the plate too distally to avoid impingement against the radial head in high flexion. Although not used frequently, this technique provides a valuable adjunct when very unstable fragments are encountered.
Figure 8.
A Type 1A fracture with associated radial head and neck fracture treated with AP headless compression screws and an anterior anti-glide 1/3 tubular plate to neutralise the shear forces.
Bioabsorbable implants
Bioabsorbable implants such as darts and small screws are appealing because of their potential value in preserving articular cartilage. Complications related to these implants include implant fracture and reactive synovitis.45,46 These implants may be of value for shallow articular fragments, such as OCD lesions, but they are not routinely required for adult coronal shear fractures.
Another technique for fixation of shallow fragments that are too large to be excised is to use PDS sutures. Trans-osseous bone tunnels wide enough to accommodate a 16-gauge hypodermic needle are made in a PA direction. Number 1 PDS is then shuttled through the tunnels within a needle. The suture is passed through the articular fragment to create a mattress suture and a knot is then tied on the posterior aspect of the capitellum (Figure 9). Further peripheral sutures can be placed to neutralise rotational forces.
Figure 9.
A shallow Type 1A fracture involving the whole capitellar surface (a) treated with trans-osseous PDS sutures. The patient had an excellent outcome at one year with no sign of avascular necrosis (b).
Bone grafting
Considerable cancellous and articular impaction can occur with higher grade coronal shear fractures. Disimpaction of these fragments often leaves a void beneath the articular fragments. Bone grafting large defects may prevent collapse of the articular surface, particularly in the setting of posterior comminution. Autogenous corticocancellous or cancellous graft can be harvested from the iliac crest, lateral olecranon or distal radius. Large volume graft is rarely required; therefore, the lateral olecranon provides a safe reliable donor source which is within the surgical field.47
Arthroplasty
TEA
There is a higher complication rate related to internal fixation of Type 3 and 4 fractures, particularly in older patients with poor subchondral bone stock. These include: fixation failure, avascular necrosis, metalwork prominence, non-union and stiffness.1,2,4,48
Primary TEA is an alternative, attractive option for older active patients with these fracture patterns.49–54 Short-term functional outcomes following TEA for distal humeral fractures tend to be good, although these results deteriorate with time which is likely to be because of the more active nature of trauma patients compared to those with inflammatory arthritis. Moreover, the long-term complications such as loosening, peri-prosthetic fracture and deep infection can be very challenging to treat.48,54
Hemiarthroplasty
Hemiarthroplasty is an alternative to TEA which may be more suitable for high-grade coronal shear fractures in appropriate trauma patients, as it eliminates all complications related to an ulnar component and linked articulation55–58 (Figure 10). The anatomic, unlinked nature of these implants may reduce loosening rates in more active patients and their relative ease of revision makes them an appealing arthroplasty option. However, potential issues of native cartilage wear and instability should temper this, and although short to mid-term results with modern anatomic hemiarthroplasty implants are good, long-term and comparative studies are not yet available.58
Figure 10.
A Type 4B fracture treated with elbow hemiarthroplasty in an older active patient.
Arthroscopic-assisted fixation
Arthroscopic and arthroscopic-assisted techniques may be used for fixation of simple coronal shear fractures with satisfactory results reported in the literature.29,59,60 There may be a benefit in terms of speed of recovery and post-operative pain with an arthroscopic technique; however, a high level of arthroscopic skill is required and only simple fractures amenable to cannulated screw fixation (Dubberley 1A and 2A) are appropriate for these techniques.
Clinical outcomes
There is a paucity of high-quality evidence regarding outcomes following coronal shear fractures. Most of the existing literature is comprised of case series,1,4,6,33,38,61 and long-term outcomes are reported in one study.11 These studies suggest that inferior outcomes are evident with increasing Dubberley grade1,4,11 and the presence of posterior comminution (subtype B).4,61 In one study, the Mayo Elbow Performance Score was inferior as the number of fragments increased with > 4 fragments having the worst functional scores following internal fixation.61 Furthermore, in those studies that categorised range of motion by Dubberley grade, it seems that mean extension deficit also increases with fracture grade (Type 1: 10 °,Type 2: 16 °, Type 3: 24 °).1,4,6,61 These data support the use of this classification for prognostic purposes and decision making.
Complications
Despite the intraarticular nature and lack of soft tissue attachment of coronal shear articular fragments, avascular necrosis (AVN) is rare, although it has been reported.6,15,36 Non-union and fixation failure have also been reported with increasing incidence according to fracture type, and it may be difficult to distinguish the presence or absence of AVN as a contributing factor in these cases. Low-grade degenerative arthritis is common in longer term series with radiographic follow-up; however, this does not correlate with clinical outcome and there is no data available on the effect of placing screws through the articular surface on the development of degenerative changes. Other reported complications include heterotopic ossification, deep infection, elbow instability and ulnar or radial nerve injury.1–4,11
Reoperation rates following internal fixation are not infrequent, with a rate of 43% and 48% reported by two separate groups.1,5 The most common indication for re-operation was to perform capsulectomy for stiffness and to remove prominent metalwork, followed by revision fixation, conversion to arthroplasty and ulnar nerve decompression.
Summary
Coronal shear fractures are an uncommon but challenging subset of distal humeral fractures. Careful planning, familiarity with a variety of surgical approaches and application of numerous techniques are required to achieve good outcomes for complex fractures in particular. A surgical algorithm based on the modified Dubberley classification is suggested (Table 1) by the authors to provide a framework for planning and treatment of these injuries.
Table 1.
Treatment algorithm based on the modified Dubberley classification.
| Type 1 | Type 2 | Type 3 | Type 4 | |
|---|---|---|---|---|

|

|

|

|
|
Subtype A (no posterior comminution)
|
Approach Lateral | Approach Lateral | Approach Extensile lateral Olecranon osteotomy Para-tricipital Combined medial and lateral | Approach Para-tricipital (arthroplasty may be required) |
| Fixation Independent screws ± anti-glide plate | Fixation Independent screws ± anti-glide plate | Fixation Independent screws ± anti-glide plate | Fixation Combination of all techniques. Consider arthroplasty | |
Subtype B (posterior comminution)
|
Approach Lateral | Approach Extensile lateral | Approach Extensile lateral Olecranon osteotomy Para-tricipital Combined medial and lateral | Approach Para-tricipital (arthroplasty may be required) |
| Fixation Posterolateral plate ± bone grafting | Fixation Posterolateral plate ± bone grafting | Fixation Posterolateral plate ± bone grafting ± medial/lateral plate Consider arthroplasty | Fixation Combination of all techniques Consider arthroplasty |
Acknowledgements
The authors acknowledge Mr Enis Guryel, Consultant trauma surgeon at Brighton & Sussex University Hospital for permission to use x rays in figure 8.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Review and Patient Consent
Local ethical approval was not required for composition of this article. All patients consented for use of anonymised images within the article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Dubberley JH, Faber JJ, MacDermid JC, et al. Outcome after open reduction and internal fixation of capitellar and trochlear fractures. J Bone Joint Surg Am 2006; 88: 46–54. [DOI] [PubMed] [Google Scholar]
- 2.Brouwer KM, Jupiter JB, Ring D. Nonunion of operatively treated capitellum and trochlear fractures. J Hand Surg Am 2011; 36: 804–807. [DOI] [PubMed] [Google Scholar]
- 3.Lopiz Y, Rodríguez-González A, García-Fernández C, et al. Open reduction and internal fixation of coronal fractures of the capitellum in patients older than 65 years. J Shoulder Elbow Surg 2016; 25: 369–375. [DOI] [PubMed] [Google Scholar]
- 4.Durakbasa MO, Gumussuyu G, Gungor M, et al. Distal humeral coronal plane fractures: management, complications and outcome. J Shoulder Elbow Surg 2013; 22: 560–566. [DOI] [PubMed] [Google Scholar]
- 5.Ring D, Jupiter JB, Gulotta L. Articular fractures of the distal part of the humerus. J Bone Joint Surg Am 2003; 85-A: 232–238. [DOI] [PubMed] [Google Scholar]
- 6.McKee MD, Jupiter JB, Bamberger HB. Coronal shear fractures of the distal end of the humerus. J Bone Joint Surg Am 1996; 78: 49–54. [DOI] [PubMed] [Google Scholar]
- 7.Collert S. Surgical management of fracture of the captulum humeri. Acta Orthop Scand 1977; 48: 603–606. [DOI] [PubMed] [Google Scholar]
- 8.Dushuttle RP, Coyle MP, Zadawsky JP, et al. Fractures of the capitellum. J Trauma 1985; 25: 317–321. [DOI] [PubMed] [Google Scholar]
- 9.Ruchelsman DE, Tejwani NC, Kwon YW, et al. Open reduction and internal fixation of capitellar fractures with headless screws. J Bone Joint Surg Am 2009; 91(Suppl 2): 38–49. [DOI] [PubMed] [Google Scholar]
- 10.Grantham SA, Norris TR, Bush DC. Isolated fracture of the humeral capitellum. Clin Orthop 1981; 161: 262–269. [PubMed] [Google Scholar]
- 11.Guitton TG, Doornberg JN, Raaymakers ELFB, et al. Fractures of the capitellum and trochlea. J Bone Joint Surg Am 2009; 91: 390–397. [DOI] [PubMed] [Google Scholar]
- 12.Watts AC, Morris A, Robinson CM. Fractures of the distal humeral articular surface. J Bone Joint Surg Br 2007; 89: 510–515. [DOI] [PubMed] [Google Scholar]
- 13.Singh AP, Vaishya R, Jain A, et al. Fractures of capitellum: a review of 14 cases treated by open reduction and internal fixation with Herbert screws. Int Orthop 2010; 34: 897–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doornberg J, Lindenhovius A, Kloen P, et al. Two and three-dimensional computed tomography for the classification and management of distal humeral fractures. Evaluation of reliability and diagnostic accuracy. J Bone Joint Surg Am 2006; 88: 1795–1801. [DOI] [PubMed] [Google Scholar]
- 15.Morrey BF. The elbow and its disorders, 2nd ed Philadelphia: Saunders, 1993, pp. 328–366. [Google Scholar]
- 16.Müller ME, Nazarian S, Koch P, et al. The comprehensive classification of fractures of long bones, Germany: Springer-Verlag Berlin Heidelberg, 1990, pp. 120–121. [Google Scholar]
- 17.Desloges W, Faber KJ, King GJW, et al. Functional outcomes of distal humeral fractures managed nonoperatively in medically unwell and lower-demand elderly patients. J Shoulder Elbow Surg 2015; 24: 1187–1196. [DOI] [PubMed] [Google Scholar]
- 18.Christopher F, Evanston I. Conservative treatment of fracture of the capitellum. J Bone Joint Surg 1935; XVII: 489–492. [Google Scholar]
- 19.Ochner RS, Bloom H, Palumbo RC, et al. Closed reduction of coronal fractures of the capitellum. J Trauma 1996; 40: 199–203. [DOI] [PubMed] [Google Scholar]
- 20.Robertson RC, Bogart FB. Fracture of the capitellum and trochlea combined with fracture of the external humeral condyl. J Bone Joint Surg Am 1933; 15: 206–213. [Google Scholar]
- 21.Kleiger B, Joseph H. Fracture of the capitellum humeri. Bull Hosp Jt Dis 1964; 25: 4–70. [PubMed] [Google Scholar]
- 22.Cutbush K, Andrews S, Siddiqui N, et al. Capitellar fractures – is open reduction and internal fixation necessary?. J Orthop Trauma 2015; 29: 50–53. [DOI] [PubMed] [Google Scholar]
- 23.Hotchkiss RN, Kasparyan GN, George N. The medial “Over the Top” approach to the elbow. Tech Orthop 2000; 15: 105–112. [Google Scholar]
- 24.Taylor TKF, Scham SM. A posteromedial approach to the proximal end of the ulna for the internal fixation of olecranon fractures. J Trauma 1969; 9: 594–602. [DOI] [PubMed] [Google Scholar]
- 25.Estell LW, Summey TJ. Fracture of the capitellum of the humerus. Ann Surg 1934; 99: 497–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grantham SA, Norris TR, Bush DC. Isolated fracture of the humeral capitellum. Clin Orthop Relat Res 1981; 161: 262–269. [PubMed]
- 27.Garner MR, Schottel P, Hotchkiss RN, et al. Capitellum fracture fragment excision: a case series. HSS J 2015; 11: 204–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fowles MB, Kassab MT. Fracture capitulum humeri treatment by excision. J Bone Joint Surg 1974; 56-A: 794–798. . [PubMed] [Google Scholar]
- 29.Feldman MD. Arthroscopic excision of type II capitellar fractures. Arthroscopy 1997; 13: 743–748. [DOI] [PubMed] [Google Scholar]
- 30.Sabo MT, Fay K, McDonald CP, et al. Effect of coronal shear fractures of the distal humerus on elbow kinematics and stability. J Shoulder Elbow Surg 2010; 19: 670–680. [DOI] [PubMed] [Google Scholar]
- 31.Mancini GB, Fiacca C, Picuti G. Resection of the radial capitellum. Long-term results. Ital J Orthop Traumatol 1989; 15: 295–302. [PubMed] [Google Scholar]
- 32.Koslowsky TC, Mader K, Kirchner S, et al. Treatment of medial malleolar fractures using fine-threaded K-wires: a new operative technique. J Trauma 2007; 62: 258–261. [DOI] [PubMed] [Google Scholar]
- 33.Heck S, Zilleken C, Pennig D, et al. Reconstruction of radial capitellar fractures using fine-threaded implants (FFS). Injury 2012; 43: 164–168. [DOI] [PubMed] [Google Scholar]
- 34.Koslowsky TC, Mader K, Gausepohl T, et al. Reconstruction of Mason type-III and type-IV radial head fractures with a new fixation device: 23 patients followed 1–4 years. Acta Orthop 2007; 78: 151–156. [DOI] [PubMed] [Google Scholar]
- 35.Sano S, Rokkaku T, Saito S, et al. Herbert screw fixation of capitellar fractures. J Shoulder Elbow Surg 2005; 14: 307–311. [DOI] [PubMed] [Google Scholar]
- 36.Mahirogullari M, Kiral A, Solakoglu C, et al. Treatment of fractures of the humeral capitellum using herbert screws. J Hand Surg Am 2006; 31: 320–325. [DOI] [PubMed] [Google Scholar]
- 37.Liberman N, Katz T, Howard CB, et al. Fixation of capitellar fractures with the Herbert screw. Arch Orthop Trauma Surg 1991; 110: 155–157. [DOI] [PubMed] [Google Scholar]
- 38.Mighell M, Virani NA, Shannon R, et al. Large coronal shear fractures of the capitellum and trochlea treated with headless compression screws. J Shoulder Elbow Surg 2010; 19: 38–45. [DOI] [PubMed] [Google Scholar]
- 39.Vaishya R, Vijay V, Jha GK, et al. Open reduction and internal fixation of capitellar fracture through anterolateral approach with headless double-threaded compression screws: a series of 16 patients. J Shoulder Elbow Surg 2016; 25: 1182–1188. [DOI] [PubMed] [Google Scholar]
- 40.Elkowitz SJ, Polatsch DB, Egol KA, et al. Capitellum fractures: a biomechanical evaluation of three fixation methods. J Orthop Trauma 2002; 16: 503–506. [DOI] [PubMed] [Google Scholar]
- 41.Elkowitz SJ, Kubiak EN, Polatsch D, et al. Comparison of two headless screw designs for fixation of capitellum fractures. Bull Hosp Jt Dis 2003; 61: 123–126. [PubMed] [Google Scholar]
- 42.Felstead AJ, Phadnis J. Independent Locking Screws for Articular Fragment Fixation in the Elbow. Tech Hand Up Extrem Surg. Epub ahead of print 5 December 2018. DOI: 10.1097/BTH.0000000000000220. [DOI] [PubMed]
- 43.Schaffer JJ, Manoli A. The antiglide plate for distal fibular fixation. A biomechanical comparison with fixation with a lateral plate. J Bone Jt Surg – Ser A 1987; 69: 596–604. [PubMed] [Google Scholar]
- 44.Sen MK, Sama N, Helfet DL. Open reduction and internal fixation of coronal fractures of the capitellum. J Hand Surg Am 2007; 32: 1462–1465. [DOI] [PubMed] [Google Scholar]
- 45.Laughlin RM, Block MS, Wilk R, et al. Resorbable plates for the fixation of mandibular fractures: a prospective study. J Oral Maxillofac Surg 2007 65: 89–96. [DOI] [PubMed]
- 46.Hirvensalo E, Bostman O, Partio E, et al. Fracture of the humeral capitellum fixed with absorbable polyglycolide pins. 1-year follow-up of 8 adults. Acta Orthop Scand 1993; 64: 85–86. [DOI] [PubMed] [Google Scholar]
- 47.Micev AJ, Kalainov DM, Slikker W, et al. Comparing morbidities of bone graft harvesting from the olecranon process and the distal radius. Plast Reconstr Surg – Glob Open 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McKee MD, Veillette CJH, Hall JA, et al. A multicenter, prospective, randomized, controlled trial of open reduction-internal fixation versus total elbow arthroplasty for displaced intra-articular distal humeral fractures in elderly patients. J Shoulder Elb Surg 2009; 18: 3–12. [DOI] [PubMed] [Google Scholar]
- 49.Ray PS, Kakarlapudi K, Rajsekhar C, et al. Total elbow arthroplasty as primary treatment for distal humeral fractures in elderly patients. Injury 2000; 31: 687–692. [DOI] [PubMed] [Google Scholar]
- 50.Gambirasio R, Riand N, Stern R, et al. Total elbow replacement for complex fractures of the distal humerus. An option for the elderly patient. J Bone Joint Surg Br 2001; 83(August 1997): 974–978. [DOI] [PubMed] [Google Scholar]
- 51.Garcia JA, Mykula R, Stanley D. Complex fractures of the distal humerus in the elderly. The role of total elbow replacement as primary treatment. J Bone Joint Surg Br 2002; 84: 812–816. [DOI] [PubMed] [Google Scholar]
- 52.Kamineni S, Morrey BF. Distal humeral fractures treated with noncustom total elbow replacement. J Bone Joint Surg Am 2004; 86-A: 940–947. [DOI] [PubMed] [Google Scholar]
- 53.Frankle MA, Herscovici D, DiPasquale TG, et al. A comparison of open reduction and internal fixation and primary total elbow arthroplasty in the treatment of intraarticular distal humerus fractures in women older than age 65. J Orthop Trauma 2003; 17: 473–480. [DOI] [PubMed] [Google Scholar]
- 54.DeSimone LJ, Sanchez-Sotelo J. Total elbow arthroplasty for distal humerus fractures. Orthop Clin North Am 2013; 44: 381–387. ix–x. [DOI] [PubMed] [Google Scholar]
- 55.Street DM, Stevens PS. A humeral replacement prosthesis for the elbow: results in ten elbows. J Bone Jt Surg Am 1974; 56: 1147–1158. [PubMed] [Google Scholar]
- 56.Adolfsson L, Hammer R. Elbow hemiarthroplasty for acute reconstruction of intraarticular distal humerus fractures: a preliminary report involving 4 patients. Acta Orthop 2006; 77: 785–787. [DOI] [PubMed] [Google Scholar]
- 57.Parsons M, O'Brien RJ, Hughes JS. Elbow hemiarthroplasty for acute and salvage reconstruction of intra-articular distal humerus fractures. Techniq Shoulder Elbow Surg 2005; 6: 87–97. [Google Scholar]
- 58.Phadnis J, Watts AC, Bain GI. Elbow hemiarthroplasty for the management of distal humeral fractures: current technique, indications and results. Shoulder Elb 2016; 8: 171–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kuriyama K, Kawanishi Y, Yamamoto K. Arthroscopic-assisted reduction and percutaneous fixation for coronal shear fractures of the distal humerus: report of two cases. J Hand Surg Am 2010; 35: 1506–1509. [DOI] [PubMed] [Google Scholar]
- 60.Mitani M, Nabeshima Y, Ozaki A, et al. Arthroscopic reduction and percutaneous cannulated screw fixation of a capitellar fracture of the humerus: a case report. J Shoulder Elbow Surg 2009; 18: e6–9. DOI: 10.1016/j.jse.2008.07.007. [DOI] [PubMed]
- 61.Ashwood N, Verma M, Hamlet M, et al. Transarticular shear fractures of the distal humerus. J Shoulder Elb Surg 2010; 19: 46–52. [DOI] [PubMed] [Google Scholar]