Abstract
Background
We report functional outcomes at six years in patients with varying degrees of fatty infiltration and atrophy of the rotator cuff muscles who have undergone anatomic total shoulder replacement.
Methods
A retrospective analysis of case notes and magnetic resonance imaging scans of patients undergoing total shoulder replacement for primary glenohumeral arthritis was performed. Patients were grouped based upon their pre-operative magnetic resonance imaging findings for fatty infiltration, muscle area and tendinopathy. Post-operative functional outcomes were assessed using the Oxford Shoulder Score and Quick Disabilities of the Arm, Shoulder and Hand score. Post-operative measurements were made for active shoulder movements.
Results
Thirty-two patients were reviewed at a mean of 67 months following surgery. All patients demonstrated fatty infiltration on their pre-operative magnetic resonance imaging scan. Muscle atrophy was shown in 22 patients and 12 had tendinopathy. Multiple regression analysis showed no correlation between the Oxford Shoulder Score (p = 0.443), the Quick Disabilities of the Arm, Shoulder and Hand score (p = 0.419), forward flexion (p = 0.170), external rotation (p = 0.755) and any of the pre-operative independent variables.
Discussion
The degree of fatty infiltration, muscle atrophy and tendinopathy of the rotator cuff muscle on pre-operative magnetic resonance imaging scanning is not associated with functional outcome score or functional movement at medium-term follow-up following total shoulder replacement.
Level of evidence
IV
Keywords: glenohumeral osteoarthritis, rotator cuff tear, total shoulder arthroplasty, fatty infiltration, muscle atrophy, magnetic resonance imaging
Introduction
Total shoulder replacement (TSR) is an effective treatment for glenohumeral arthritis. The anatomic TSR aims to restore the normal shoulder biomechanics by replicating the native anatomy.1 The majority of patients who undergo this procedure achieve both a reduction in pain and an improvement in range of motion. The stability of the joint and the restoration of joint kinematics is thought to be reliant on an intact and functional rotator cuff.2 Aside from the commonly noted complications of joint arthroplasty such as infection, aseptic loosening, dislocation and peri-prosthetic fracture, anatomic shoulder replacement is unique in that the gradual attrition of the surrounding rotator cuff poses one of the greatest risks for subsequent revision.1,3–6 Furthermore, it is the functionality of these muscles that will dictate the behaviour of the implant in situ. Hence an understanding of the integrity of the rotator cuff is critical prior to undertaking surgery.
Rotator cuff fatty infiltration and muscle atrophy are both indicative of chronic rotator cuff dysfunction and have been shown to increase the likelihood of a poor outcome in the treatment of rotator cuff tears.7–11 Thus, the management of patients who have a concomitant rotator cuff tendinopathy at the time of arthroplasty remains controversial.12–14 It is perceived that the degree of fatty infiltration and atrophy in the rotator cuff muscles in the pre-operative osteoarthritic shoulder affects functional outcome and has perhaps attributed to the rise in the use of reverse geometry prosthesis for glenohumeral osteoarthritis.14 However, recent investigation has suggested that fatty infiltration of the rotator cuff is a reversible process in patients undergoing elective anatomic shoulder replacement for arthritis at 12-month follow-up suggesting that restoration of active movement negates the effects of chronic immobilisation secondary to joint arthropathy.8
Appropriate patient selection is essential prior to TSR to optimise outcomes and reduce the risk of complication. It requires careful pre-operative assessment of the quality of the rotator cuff tendon and muscle. Magnetic resonance imaging (MRI) is a critical investigation that allows for the assessment of multiple parameters relevant to the procedure. It not only permits accurate appreciation of the soft tissue integrity and quality, but is also valuable for the analysis of glenoid bone stock and orientation.15
The aim of this study was to investigate whether the presence of rotator cuff muscle atrophy, fatty infiltration and rotator cuff tendinopathy on pre-operative MRI scanning was associated with functional outcome measurement and active shoulder movements following anatomic TSR at medium-term follow-up.
Materials and methods
The STROBE methodology for observational studies was followed.16
A retrospective analysis was performed on a group of 51 consecutive patients with primary glenohumeral arthritis who had undergone elective TSR between June 2006 and August 2011. Patients were identified by operative procedure code from computerised theatre records. The radiological investigations were available via the Picture Archiving and Communications System (PACS) Centricity® Web software (GE Healthcare, Chalfont St Giles, UK). The inclusion criterion for this study was primary anatomic TSR for glenohumeral osteoarthritis. Exclusion criteria included hemiarthroplasty, reverse TSR for cuff tear arthropathy and TSR for fracture. All surgeries were performed by, or under the direct supervision of the senior author using the EPOCA (Synthes, Paoli, Pennsylvania, USA) modular prosthesis via a standard operative technique utilising a lesser tuberosity osteotomy and a standard post-operative rehabilitation programme (see Figure 1). At the time of surgery an assessment of the integrity of the rotator cuff tendon was made; if the tendons were macroscopically torn then the operative plan was changed and then a reverse geometry prosthesis used instead.
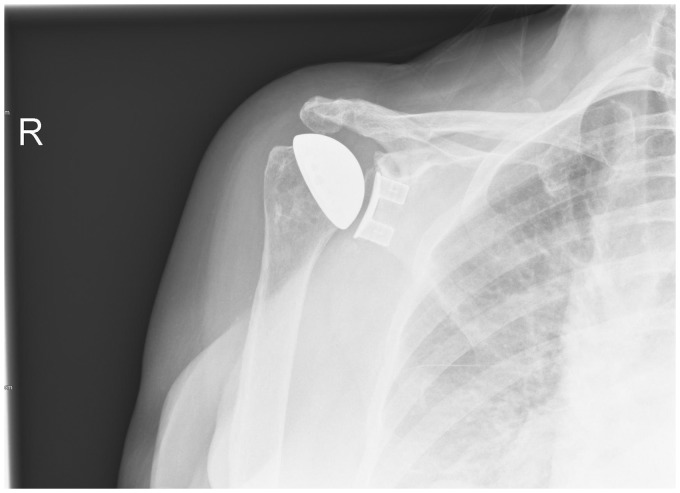
Figure 1.
Plain radiograph demonstrating Epoca resurfacing prosthesis.
All patients underwent a pre-operative MRI scan of the affected shoulder, reported by consultant musculoskeletal radiologists. The imaging and reports were reviewed for the presence and grade of tendinopathy, fatty infiltration and rotator cuff atrophy.
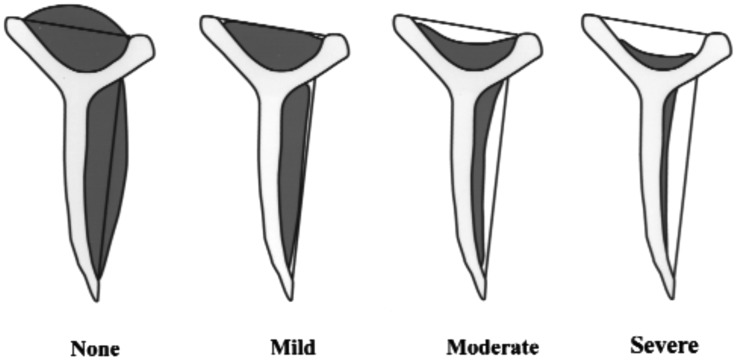
The patients were grouped by their MRI findings as per the Fuchs grading system for fatty infiltration (see Table 1), the Warner atrophy grade (see Figure 2) and finally in to either normal rotator cuff, rotator cuff tendinopathy or partial thickness tear of the rotator cuff tendons.17,18 The Warner atrophy grade is a four-category scale describing atrophy as none, mild, moderate or severe.18 None indicates that the supraspinatus muscle extends superior to a line extending between the superior tip of the coracoid and the superior tip of the scapular spine; mild indicates that the supraspinatus muscle extends to but not beyond this line; moderate and severe indicate higher degrees of muscle atrophy. These scales were converted to numerical scales for the purposes of statistical analysis. (1 = none, 4 = severe)
Table 1.
Fuchs grading system.17
| Grade | Rotator cuff fat content |
| Minimal | No to minimal fat |
| Moderate | More muscle than fat |
| Severe | Amount of fat is equal/greater than muscle |
Figure 2.
Warner atrophy grade.
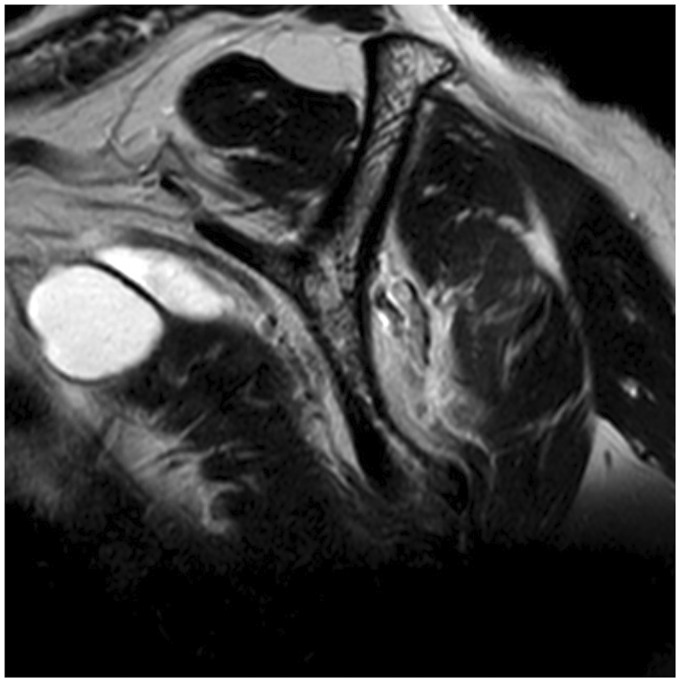
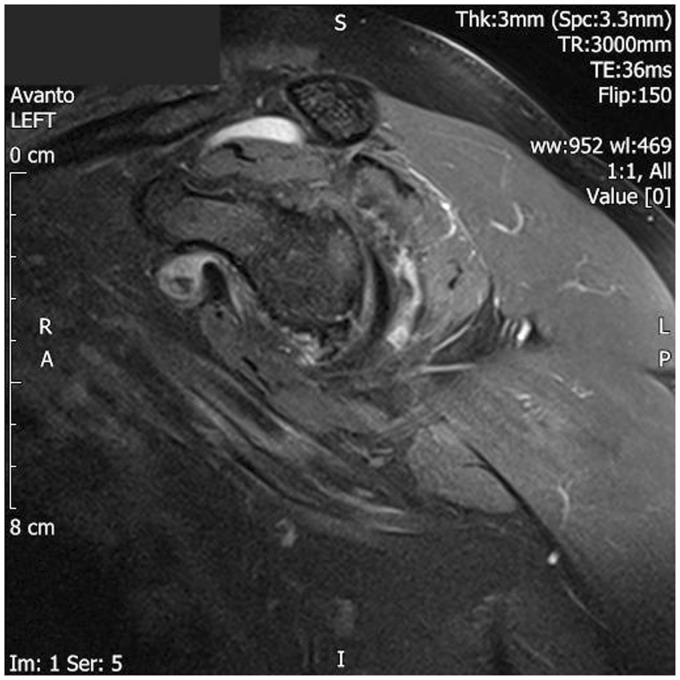
The muscles were graded on the most lateral parasagittal image on which the scapular spine was in contact with the scapular body. Adjacent images were used to clarify the anatomic relationships where required. The cross-sectional area of the supraspinatus fossa was assessed at this point as per the grading system described by Fuchs et al.17 (see Figure 3). The degree of muscle atrophy was also assessed on the same sagittal slice as per the grading system described by Warner et al.18 (see Figure 4).
Figure 3.
Sagittal MRI sequence demonstrating normal supraspinatus muscle bulk in the supraspinatus fossa and fatty infiltration of infraspinatus.
Figure 4.
Sagittal MRI sequence demonstrating loss of supraspinatus muscle bulk.
Demographic data were collected for patients with regard to sex and age. Shoulder range of movement was recorded at the time of review for elevation, external rotation, abduction and internal rotation. Patient-reported outcome measures (PROMs) were obtained post-operatively by an Oxford Shoulder Score (OSS) and Quick Disabilities of the Arm, Shoulder and Hand score (Quick DASH).19,20 PROMs and range of motion measurements were collected at a mean of 67 months following surgery.
Statistical analyses were performed using Graph Pad InStat and Prism (GraphPad Software Inc, La Jolla, CA, USA). The distribution of continuous data was assessed with a Kolmogorov–Smirnov test. Where the data were found to be normally distributed, it is described with the mean and standard deviation (SD). Data that were not normally distributed are described with the median and interquartile ranges (IQRs). In order to determine the effect of pre-operative predictors (Fuchs grade, Warner grade, Tendinopathy grade, patient age at procedure and gender) on outcome (OSS, Quick DASH, forward flexion, external rotation, abduction and internal rotation), a multiple regression analysis was performed. Significance was determined when p < 0.05. The R2 values were inspected to determine if multicollinearity was a problem in the model; all R2 values were < 0.75 indicating that multicollinearity was not a problem and therefore no rationalisation of the independent variables was required. A post hoc power calculation was performed to determine the calculated power achieved for the model.
Results
Fifty-one patients met the inclusion criteria and underwent anatomic TSR for primary glenohumeral osteoarthritis.
At the review point, a mean time of 67 months (range 48–94 months), six patients had died of unrelated illness, six patients had incomplete data, seven patients had been lost to follow-up, and a full set of data and case notes, PACS images and PROMs was available for 32 patients. No post-operative complications were noted as of the final review date.
Procedures were carried out for 19 females and 13 males, and the mean age was 70 years (SD 7.3). Demographic details for patients included are shown in Table 2.
Table 2.
Patient demographic data classified by Fuchs fatty infiltration.
| Mild | Moderate | |
|---|---|---|
| Number | 22 | 10 |
| Mean age | 71 years | 66 years |
| Sex (male/female) | 9/13 | 4/6 |
| Warner grade (normal/mild/moderate) | 10/12/0 | 0/6/4 |
| Tendinopathy (normal/mild/partial tear) | 7/9/6 | 6/3/1 |
| Mean OSS | 42 | 44 |
| Mean Quick DASH | 14 | 8 |
OSS: Oxford Shoulder Score; Quick DASH: Quick Disabilities of the Arm, Shoulder and Hand score.
Within the cohort the presence of tendinopathy, fatty infiltration and muscle atrophy was a common finding with 12 patients demonstrating tendinopathy and seven a partial tear which was debrided at time of surgery. All 32 patients showed either mild or moderate fatty infiltration of their rotator cuff muscles, with 22 demonstrating mild changes. Fatty infiltration was noted to be broadly similar throughout the cuff muscles of each patient in keeping with previous studies, but supraspinatus was specifically analysed statistically as we believe it is clinically the most important to good outcome following TSR.8 Twenty-two patients were reported to have muscle atrophy on their MRI scans and 10 had normal muscle bulk.
The median OSS was 47 (IQR 42.5–48) and the median Quick DASH 8 (IQR 0–13.6). The median forward flexion was 150° (IQR 127.5–170), external rotation 55° (IQR 45–60), abduction 100° (IQR 90–130) and median internal rotation 90° (IQR 90–100).
The multiple regression analysis showed no correlation between the OSS (p = 0.443), the Quick DASH (p = 0.419), forward flexion (p = 0.170), external rotation (p = 0.755), abduction (p = 0.058), internal rotation (p = 0.523) and any of the pre-operative independent variables (outcome scores: Table 3 and post-operative movements: Table 4).
Table 3.
Multiple regression models investigating the association of outcome measures (OSS, Quick DASH) with pre-operative state of rotator cuff (Fuchs grade, Warner grade, tendinopathy grade), age and gender.
| Outcome | Pre-operative variable | Coefficient | 95% Confidence interval | p-value |
|---|---|---|---|---|
| OSS (p = 0.443) | Fuchs grade | 3.992 | −5.45 to 13.44 | 0.393 |
| Warner grade | −2.759 | −9.55 to 4.03 | 0.411 | |
| Tendinopathy grade | 3.970 | −0.77 to 8.71 | 0.097 | |
| Age | −0.412 | −0.90 to 0.08 | 0.094 | |
| Gender | −1.462 | −7.99 to 5.06 | 0.649 | |
| Quick DASH (p=0.419) | Fuchs grade | −5.616 | −26.28 to 15.04 | 0.581 |
| Warner grade | 2.063 | −12.79 to 16.92 | 0.778 | |
| Tendinopathy grade | −9.213 | −19.58 to 1.15 | 0.079 | |
| Age | 0.859 | −0.21 to 1.93 | 0.110 | |
| Gender | 2.286 | −11.99 to 6.56 | 0.745 |
OSS: Oxford Shoulder Score; Quick DASH: Quick Disabilities of the Arm, Shoulder and Hand score.
Table 4.
Multiple regression models investigating the association of post-operative movement (forward elevation, external rotation, abduction and internal rotation) with pre-operative state of rotator cuff (Fuchs grade, Warner grade, tendinopathy grade), age and gender.
| Outcome | Pre-operative variable | Coefficient | 95% Confidence interval | p-value |
|---|---|---|---|---|
| Forward flexion (p=0.170) | Fuchs grade | −6.468 | −35.64 to 22.71 | 0.652 |
| Warner grade | 5.804 | −15.17 to 26.78 | 0.574 | |
| Tendinopathy grade | 10.873 | −3.76 to 25.51 | 0.139 | |
| Age | −1.671 | −3.18 to −0.17 | 0.031 | |
| Gender | −6.267 | −26.42 to 13.89 | 0.528 | |
| External rotation (p=0.755) | Fuchs grade | 2.610 | −10.13 to 15.35 | 0.677 |
| Warner grade | −2.525 | −11.68 to 6.63 | 0.576 | |
| Tendinopathy grade | 2.813 | −3.57 to 9.20 | 0.374 | |
| Age | −0.246 | −0.90 to 0.41 | 0.448 | |
| Gender | −5.529 | −14.33 to 3.27 | 0.208 | |
| Abduction (p = 0.058) | Fuchs grade | −10.265 | −32.10 to 11.57 | 0.342 |
| Warner grade | 2.457 | −13.24 to 18.16 | 0.750 | |
| Tendinopathy grade | 3.653 | −7.30 to 14.61 | 0.499 | |
| Age | −0.634 | −1.76 to 0.49 | 0.258 | |
| Gender | −20.679 | −35.76 to −5.59 | 0.009 | |
| Internal rotation (p = 0.523) | Fuchs grade | −0.154 | −11.21 to 10.90 | 0.977 |
| Warner grade | 0.488 | −7.46 to 8.44 | 0.900 | |
| Tendinopathy grade | −0.894 | −6.44 to 4.65 | 0.743 | |
| Age | −0.095 | −0.67 to 0.48 | 0.734 | |
| Gender | −6.477 | −14.11 to 1.16 | 0.093 |
The calculated R2 for the model with abduction as the dependent variable and Fuchs grade, Warner grade, tendinopathy grade, patient age at procedure and gender as the independent variables was 32.3% giving a calculated effect size of 0.477. For a multiple regression model with an alpha value of 0.05, 32 patients and 5 predictor variables, this gives a calculated power of (1-beta) of 0.78 which is reasonable for this type of analysis of a retrospective cohort.
Discussion
This study investigates the effect of pre-operative rotator cuff fatty infiltration, muscle atrophy and tendinopathy on post-operative TSR functional scores and active range of motion. We postulated that infiltration of the rotator cuff muscles with fat, atrophy of the rotator cuff musculature and/or presence of tendinopathy on pre-operative MRI scanning would adversely affect the functional outcome measurements and movements following anatomic TSR. However, this study has shown that the presence of fatty infiltration, muscle atrophy and tendinopathy on pre-operative MRI has no significant effect on post-operative functional scores following TSR and that post-operative movement is well preserved at medium-term follow-up.
Fatty degeneration or infiltration of the rotator cuff muscles is a degenerative condition of the tendon–muscle unit, which is defined by atrophy of the muscle fibres, fibrosis and fatty accumulation within and around the muscles.21 Fatty infiltration is observed after tears of the rotator cuff tendons.17 Originally described by Goutallier, it is most commonly seen in the elderly and is most often associated with age-related reduction of the healing potential of the rotator cuff tendons.22 It is also seen in the arthritic shoulder resulting from inactivity and reduced range of motion secondary to the arthritic pain and loss of joint congruity.8
The prevalence of partial cuff tearing in this series of almost a quarter of the patients is significantly lower than previously reported studies for patients of a similar age both in an asymptomatic population and also in a similar population to that reported here undergoing TSR.23,24
Features of muscle degeneration, namely fatty infiltration and muscle atrophy influence several clinical parameters such as outcome and strength and has been associated with adverse outcome measurements following rotator cuff repair.25–29 The association between the condition of the rotator cuff muscles pre-operatively and function and quality of life post shoulder replacement in the arthritic shoulder is less well understood.8 Many previous studies have suggested that the presence of rotator cuff pathology is associated with a higher risk of failure in TSR; however, these studies to date have included multiple diagnoses and variable pathology.1,6,30
An association between increasing degree of infraspinatus fatty infiltration and poorer Constant scores in patients undergoing shoulder replacement was noted by Edwards et al.31 The authors of this study demonstrated on CT scans that moderate and severe fatty degeneration of the infraspinatus, in the presence of partial and full thickness rotator cuff tear were associated with poorer outcomes, satisfaction and movement.31 This finding is supported by Moineau et al.32 who noted that patients with post-traumatic humeral head collapse or necrosis with fatty infiltration of the rotator cuff muscles treated with anatomic shoulder replacement had poorer functional outcome. Lapner et al.8 demonstrated that the fatty infiltration of the rotator cuff muscles on post-operative CT scanning may decrease following shoulder replacement but that the muscle area did not change significantly. However, the presence of moderate to high pre-operative fatty infiltration did not correlate with poorer patient-reported outcome scores at one-year follow-up.8
Choate et al.24 demonstrated that the presence of rotator cuff pathology, including tear status and Goutallier grade did not correlate with post-operative functional outcome scores; however, the presence of fatty infiltration of the infraspinatus negatively correlated with post-operative forward elevation and external rotation. The current study supports their findings that pre-operative fatty infiltration has no significant association with post-operative PROMs; however, our study found no significant correlation between fatty infiltration of the rotator cuff and post-operative elevation and external rotation. This may be explained by our analysis of fatty infiltration being of supraspinatus rather than infraspinatus or the longer period of our follow-up. Furthermore, it is important to note that the study by Choate et al.24 and other studies with similar findings did not have a standardised operative technique, analysed multiple surgeons and implants, and included patients with rheumatoid arthritis and significant partial or full thickness supraspinatus tendon tears, none of which the current study does.8,31 Our study presents a single surgeon series with the same implant, rather than multiple surgeons using variable implants which was noted by Choate et al.24 as being a potential confounding variable with regard to the results in their study.
There are several limitations of this study, including those associated with a retrospective analysis of data with potential selection bias being acknowledged. The nature of the study design means that we can explore association, but it is not possible to definitively establish causation. Furthermore, only 63% of our original cohort had full data available for analysis; however, the achieved power from the power calculation is reasonable for consideration of association in a retrospective cohort such as this. Another limitation is that we do not have post-operative imaging to allow quantitative and qualitative analysis of the rotator cuff musculotendinous junction over time following TSR.
Conclusion
Our study demonstrates that TSR is an effective treatment option for patients with primary glenohumeral osteoarthritis despite the presence of fatty atrophy and muscle wasting of the rotator cuff muscles. Mild-to-moderate fatty infiltration and mild-to-moderate muscle wasting of the rotator cuff muscles shoulder do not preclude patients from undergoing TSR for primary glenohumeral osteoarthritis. Longer term follow-up is ongoing and may provide an insight into the rate of rotator cuff attrition following TSR.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Review and Patient Consent
Each author certifies that all investigations were conducted in conformity with ethical principles of research. Patient consent was not sought or required as this was a retrospective review of patient records.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This study was supported by the NIHR Biomedical Research Centre at University Hospitals Bristol NHS Foundation Trust and the University of Bristol. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health and Social Care.
References
- 1.Hawkins RJ, Bell RH, Jallay B. Total shoulder arthroplasty. Clin Orthop Relat Res 1989; 242: 188–194. [PubMed] [Google Scholar]
- 2.Matsen FA, Boileau P, Walch G, et al. The reverse total shoulder arthroplasty. J Bone Joint Surg Am 2007; 89: 660–667. [DOI] [PubMed] [Google Scholar]
- 3.Khan A, Bunker TD, Kitson JB. Clinical and radiological follow-up of the Aequalis third-generation cemented total shoulder replacement: a minimum ten-year study. J Bone Joint Surg Br 2009; 91: 1594–1600. [DOI] [PubMed] [Google Scholar]
- 4.Sperling JW, Cofield RH, Rowland CM. Neer hemiarthroplasty and Neer total shoulder arthroplasty in patients fifty years old or less. Long-term results. J Bone Joint Surg Am 1998; 80: 464–473. [DOI] [PubMed] [Google Scholar]
- 5.Franklin JL, Barrett WP, Jackins SE, et al. Glenoid loosening in total shoulder arthroplasty. Association with rotator cuff deficiency. J Arthroplasty 1988; 3: 39–46. [DOI] [PubMed] [Google Scholar]
- 6.Mestdagh H, Petroff E, Maynou C, et al. [Effect of the rotator cuff condition on the results of shoulder arthroplasty]. Rev Chir Orthop Reparatrice Appar Mot 1997; 83: 522–530. [PubMed] [Google Scholar]
- 7.Goutallier D, Postel JM, Bernageau J, et al. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 1994; 304: 78–83. [PubMed] [Google Scholar]
- 8.Lapner PL, Jiang L, Zhang T, et al. Rotator cuff fatty infiltration and atrophy are associated with functional outcomes in anatomic shoulder arthroplasty. Clin Orthop Relat Res 2015; 473: 674–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Melis B, DeFranco MJ, Chuinard C, et al. Natural history of fatty infiltration and atrophy of the supraspinatus muscle in rotator cuff tears. Clin Orthop Relat Res 2010; 468: 1498–1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nakagaki K, Ozaki J, Tomita Y, et al. Function of supraspinatus muscle with torn cuff evaluated by magnetic resonance imaging. Clin Orthop Relat Res 1995; 318: 144–151. [PubMed] [Google Scholar]
- 11.Shen PH, Lien SB, Shen HC, et al. Long-term functional outcomes after repair of rotator cuff tears correlated with atrophy of the supraspinatus muscles on magnetic resonance images. J Shoulder Elbow Surg 2008; 17: 1S–7S. [DOI] [PubMed] [Google Scholar]
- 12.Galasso O, Familiari F, Gasparini G. Treatment options for irreparable postero-superior cuff tears in young patients. World J Orthop 2015; 6: 770–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Flurin PH, Roche CP, Wright TW, et al. A comparison and correlation of clinical outcome metrics in anatomic and reverse total shoulder arthroplasty. Bull Hosp Jt Dis (2013) 2015; 73: S118–S123. [PubMed] [Google Scholar]
- 14.Chalmers PN, Keener JD. Expanding roles for reverse shoulder arthroplasty. Curr Rev Musculoskelet Med 2016; 9: 40–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Feeley BT, Gallo RA, Craig EV. Cuff tear arthropathy: current trends in diagnosis and surgical management. J Shoulder Elbow Surg 2009; 18: 484–494. [DOI] [PubMed] [Google Scholar]
- 16.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370: 1453–1457. [DOI] [PubMed] [Google Scholar]
- 17.Fuchs B, Weishaupt D, Zanetti M, et al. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg 1999; 8: 599–605. [DOI] [PubMed] [Google Scholar]
- 18.Warner JJ, Higgins L, Parsons IM, et al. Diagnosis and treatment of anterosuperior rotator cuff tears. J Shoulder Elbow Surg 2001; 10: 37–46. [DOI] [PubMed] [Google Scholar]
- 19.Dawson J, Fitzpatrick R, Carr A. Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br 1996; 78: 593–600. [PubMed] [Google Scholar]
- 20.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med 1996; 29: 602–608. [DOI] [PubMed] [Google Scholar]
- 21.Osti L, Buda M, Del Buono A. Fatty infiltration of the shoulder: diagnosis and reversibility. Muscles Ligaments Tendons J 2013; 3: 351–354. [PMC free article] [PubMed] [Google Scholar]
- 22.Gumucio JP, Korn MA, Saripalli AL, et al. Aging-associated exacerbation in fatty degeneration and infiltration after rotator cuff tear. J Shoulder Elbow Surg 2014; 23: 99–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sher JS, Uribe JW, Posada A, et al. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am 1995; 77: 10–15. [DOI] [PubMed] [Google Scholar]
- 24.Choate WS, Shanley E, Washburn R, et al. The incidence and effect of fatty atrophy, positive tangent sign, and rotator cuff tears on outcomes after total shoulder arthroplasty. J Shoulder Elbow Surg 2017; 26: 2110–2116. [DOI] [PubMed] [Google Scholar]
- 25.Gazielly DF, Gleyze P, Montagnon C. Functional and anatomical results after rotator cuff repair. Clin Orthop Relat Res 1994; 304: 43–53. [PubMed] [Google Scholar]
- 26.Harryman DT, Mack LA, Wang KY, et al. Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am 1991; 73: 982–989. [PubMed] [Google Scholar]
- 27.Iannotti JP, Zlatkin MB, Esterhai JL, et al. Magnetic resonance imaging of the shoulder. Sensitivity, specificity, and predictive value. J Bone Joint Surg Am 1991; 73: 17–29. [PubMed] [Google Scholar]
- 28.Nakagaki K, Ozaki J, Tomita Y, et al. Alterations in the supraspinatus muscle belly with rotator cuff tearing: evaluation with magnetic resonance imaging. J Shoulder Elbow Surg 1994; 3: 88–93. [DOI] [PubMed] [Google Scholar]
- 29.Thomazeau H, Boukobza E, Morcet N, et al. Prediction of rotator cuff repair results by magnetic resonance imaging. Clin Orthop Relat Res 1997; 344: 275–283. [PubMed] [Google Scholar]
- 30.Torchia ME, Cofield RH, Settergren CR. Total shoulder arthroplasty with the Neer prosthesis: long-term results. J Shoulder Elbow Surg 1997; 6: 495–505. [DOI] [PubMed] [Google Scholar]
- 31.Edwards TB, Boulahia A, Kempf JF, et al. The influence of rotator cuff disease on the results of shoulder arthroplasty for primary osteoarthritis: results of a multicenter study. J Bone Joint Surg Am 2002; 84–A: 2240–2248. [DOI] [PubMed] [Google Scholar]
- 32.Moineau G, McClelland WB, Trojani C, et al. Prognostic factors and limitations of anatomic shoulder arthroplasty for the treatment of posttraumatic cephalic collapse or necrosis (type-1 proximal humeral fracture sequelae). J Bone Joint Surg Am 2012; 94: 2186–2194. [DOI] [PubMed] [Google Scholar]