Abstract
We are continuously exposed to many pathogens through inhalation, ingestion, and touch. The immune system protects us from the majority of these pathogens as flatworms, bacteria, fungi, and viruses. We have also witnessed tremendous progress in the prevention and treatment of infectious diseases; still, they remain a major challenge and are responsible for major cause of death and disability worldwide. The immune system’s memory response and vaccination have resulted in complete eradication of many diseases. Our immune system is very adaptive and consists of a variety of cells and molecules, which play an active role in protecting us. It not only protects us from the outside pathogenic agents but also is also capable of recognizing the body’s own components. It recognizes them as self and does not induce response against them. It is known as self-/non-self-discrimination. Sometimes due to certain defects or other reasons when the immune system is not able to differentiate self, then it mounts an attack on self-components leading to autoimmunity. The importance of the immune system was recognized by early work of Dr. Edward Jenner and Louis Pasteur; they recognized the abilities of the immune system, and since then the system was gradually being explored and it laid the foundation of immunology.
However, day-by-day microbes are also posing health risks as new strains are continuously being evolved. Many chemotherapeutic agents have been developed to control the spread and infections. However, microbes are also continuously developing the ability of their survival with emergence of new strains and properties. Antibiotic resistance is occurring with all classes of microbes posing a serious clinical problem in managing infections. The diseases like tuberculosis, cholera, and rheumatic fever, which were believed to be eradicated, have ferociously reemerged. The reemergence and new pathogenic agents might be the result of mutations in their genome and changes occurring in the environment. In this chapter, basic concept of the immune system and some of the diseases of the skin, gastrointestinal tract, nervous system, and respiratory system caused by microorganisms are discussed along with sexually transmitted diseases and characterization of pathogens.
Keywords: Human Immunodeficiency Virus, Adaptive Immune Response, Bacterial Vaginosis, Chlamydia Trachomatis, Pelvic Inflammatory Disease
Introduction
We are continuously exposed to many pathogens through inhalation, ingestion, and touch. The immune system protects us from the majority of these pathogens as flatworms, bacteria, fungi, and viruses. We have also witnessed tremendous progress in the prevention and treatment of infectious diseases; still, they remain a major challenge and are responsible for major cause of death and disability worldwide. The immune system’s memory response and vaccination have resulted in complete eradication of many diseases. Our immune system is very adaptive and consists of a variety of cells and molecules, which play an active role in protecting us. It not only protects us from the outside pathogenic agents but also is also capable of recognizing the body’s own components. It recognizes them as self and does not induce response against them. It is known as self-/non-self-discrimination. Sometimes due to certain defects or other reasons when the immune system is not able to differentiate self, then it mounts an attack on self-components leading to autoimmunity.
The importance of the immune system was recognized by early work of Dr. Edward Jenner and Louis Pasteur; they recognized the abilities of the immune system, and since then the system was gradually being explored and it laid the foundation of immunology.
However, day-by-day microbes are also posing health risks as new strains are continuously being evolved. Many chemotherapeutic agents have been developed, but on the other hand, microbes are continuously developing the ability of their survival with emergence of new strains and properties. Antibiotic resistance is occurring with all classes of microbes posing a serious clinical problem in managing infections. The diseases like tuberculosis, cholera, and rheumatic fever, which were believed to be eradicated, have ferociously reemerged. The reemergence and new pathogenic agents might be the result of mutations in their genome and changes occurring in the environment. In this chapter, basic concept of the immune system and some of the diseases caused by microorganisms and characterization of pathogens are discussed.
Introduction to the Immune System
Immune system first recognizes the pathogen and then gives a response against that pathogen. Thus, upon recognition of the pathogenic agent, it triggers the effector response which helps in the elimination of the pathogen.
In our body there are distinct effector responses for pathogens; thus, there are two kinds of immune responses: the innate immune response and adaptive or acquired immune response (Fig. 8.1). Though self-/non-self-recognition is the hallmark of the two responses, the adaptive immune system is much more diverse, is specific, and has memory in contrast to innate immune responses. The innate immune system recognizes and responds nonspecifically against pathogen, while adaptive or acquired immune system mediates specific response and remembers the pathogen after interacting with it [6].
Fig. 8.1.

The figure shows the outline of innate and adaptive immune responses
Immunology and Medical Microbiology
The study of immunology led to the growth of medical microbiology, which deals with identification, and mechanism of action of infectious agents. The disease-causing organisms are called pathogens and their mode of attacking the host and its effects on host is pathogenesis. The major human pathogens are viruses, bacteria, fungi, and parasites which are causative agents of many diseases. The immune system responds differently for these pathogenic agents. Unlike bacteria, fungi, and parasites which are capable of independent growth, the viruses require the host cell for the multiplication.
Whenever there is a state of misfunctioning of any immune components because of genetic defects or because of acquired disease as acquired immunodeficiency syndrome (AIDS) caused by human immunodeficiency virus (HIV-1 and HIV-2), the immune system is not able to respond naturally to infectious agents. These conditions are termed as immunodeficiency where the pathogens that are prevalent in the external environment but do not cause any harm in normal individual result in severe diseases in these patients, for example, Candida albicans. These are known as opportunistic pathogens. Therefore getting infections from these opportunistic agents show the compromised immune system.
Thus, the immune system deals with the majority of pathogenic agents and is well equipped with many cells and molecules to combat them.
Innate and Adaptive Immune Responses
Innate immunity is the first line of defense system which gives nonspecific response. The immunity is natural (by birth) and quick when the body encounters the pathogen. On the other hand, adaptive immunity is an acquired immunity and takes sometime to mediate the response; the response is highly specific and with memory. When adaptive immune components react for the first time with pathogen, the response is primary; when same pathogen is encountered again by the body, the response is via memory cells with specificity, in less time and heightened as compared to primary response.
Due to memory response of adaptive immune system, the body is given exposure with either weakened or killed or subunit of pathogen. This exposure leads to active clearance of the pathogen by adaptive immunity and induces the formation of memory cells, which prevent subsequent infection with the same pathogen. This is the basis of the field of vaccinology (see Chap. 10.1007/978-981-10-0875-7_14); it has led to vigorous decrease in the incidences of the childhood diseases like measles, mumps, and polio and complete eradication of small pox [6].
Innate Immunity
Innate immunity is the first line of defense system of our body which does not give a very specific response. The immunity is natural that is preexisting, is quick, and occurs when the body encounters the pathogens. The innate immune components comprise cells and soluble molecules. The system has physical, chemical, and cellular barriers. The physical barriers include the skin and mucous membrane. The mucous lining includes the mucosal epithelia lining respiratory and genitourinary and gastrointestinal tracts; the mucous which is secreted contains substances like defensins that are capable of killing pathogens or inhibiting their growth.
The skin’s outermost layer has dead cells filled with waterproof substance called keratin which does not let viruses to infect and multiply on our body. The skin also has psoriasin, which is capable of lysing E. coli. The places from where these pathogens can invade our body have the mucous membrane and have a number of nonspecific mechanisms. Saliva is present in our mouth, tears in eyes, secretion of mucus by epithelial cells and movement of cilia on some of the cells at the lower respiratory tract, and acid and digestive enzymes in the gastric tract. The presence of many nonpathogenic microorganisms as commensals is protective, as they compete with pathogenic agents.
The chemical barriers are various cytokines and soluble proteins. The innate immune components are capable of self-/non-self-discrimination and are able to recognize some specific, conserved, and unique pattern associated with a particular class of microorganisms [6].
These patterns are not present in our body but are typically associated with pathogens and are called pathogen-associated molecular patterns (PAMPs). These PAMPs may be a combination of sugars, certain proteins, lipids, or nucleic acids as peptidoglycan in the bacterial cell wall, flagella of bacteria, lipopolysaccharide (LPS) on gram-negative bacteria, teichoic acids on gram-positive bacteria, chitin, glucans, and zymosan on fungi. These are recognized by some receptors present on our body called as pattern recognition receptors (PRRs) (Fig. 8.2).
Fig. 8.2.
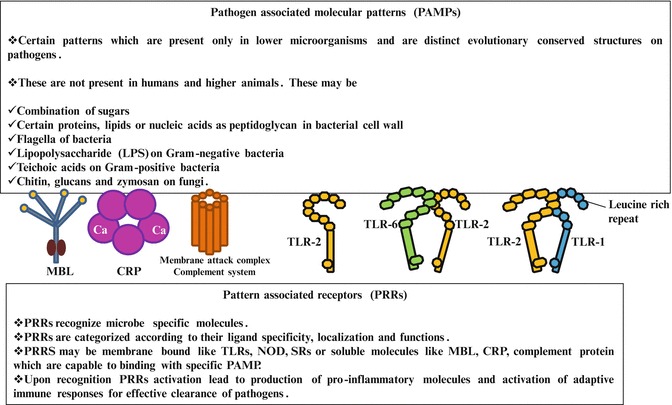
The figure shows various pathogen-associated molecular patterns, which are present exclusively on pathogens. PRRs are present in our body which are capable of recognizing and binding PAMPs. PRRs may be soluble as mannose-binding lectin (MBL), C-reactive protein (CRP), and complement components or may be membrane bound like toll-like receptors (TLRs), NOD, or SRs. Humans have ten kinds of TLRs which are capable of interacting with different PAMPs. TLRs may also form unique binding by interacting with each other as TLR2 and TLR6 and TLR1 and TLR2. TLR have leucine-rich repeats on their extracellular domain
PRRs may be soluble or membrane bound. Cell surface PRRs are members of the toll-like receptor (TLR) family. Humans have at least ten TLRs which play important roles in innate immune responses (Fig. 8.3).
Fig. 8.3.
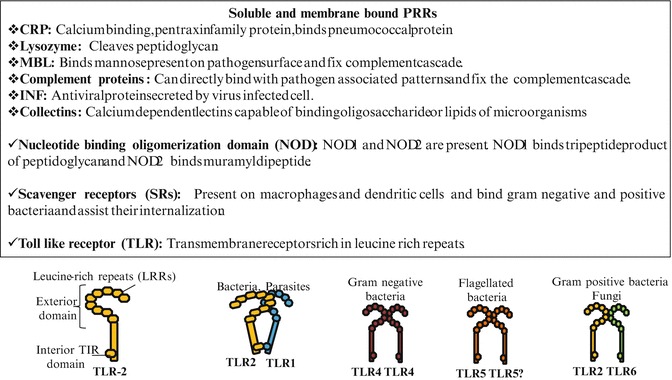
The figure shows the soluble receptor and membrane receptors of innate immunity. CRP is C-reactive protein, MBL is mannose-binding lectin, INF is interferon. NOD, SR, and TLRs belong to the family of membrane receptors. TLR may exist singly or may form homodimer (TLR4) and heterodimer (TLR2 and TLR1)
Toll-Like Receptors
The protein toll was discovered in mutant flies (unable to establish dorsal–ventral axis). Toll is a transmembrane signal receptor protein whose related molecules function in innate immune response and are called as toll-like receptors (TLRs). Toll-like receptors are transmembrane innate immune receptors which are present on cells. These receptors are responsible for binding nonspecifically to many pathogenic patterns. These can also interact among them to form new binding sites for other PAMPs. Major membrane-bound PRR as TLRs have leucine-rich repeat (LRR) motif and IL-1 receptor homology domain. TLRs are divided according to their PAMPs. TLR1, TLR2, TLR4, and TLR6 recognize lipids; TLR3, TLR7, TLR8, and TLR9 recognize nucleic acids.
TLRs recognize PAMPs either directly or via an intermediate PAMP-binding molecule.
TLR1: Is responsible for recognizing triacyl lipopeptide of Mycobacteria
TLR2: Recognize peptidoglycans of gram-positive bacteria, GPI-linked proteins of trypanosomes, lipopeptide of Mycobacteria, and zymosan of fungi
TLR3: Recognize double-stranded RNA of viruses
TLR4: Recognize lipopolysaccharide of gram-negative bacteria and F-protein of respiratory syncytial virus (RSV)
TLR5: Bind to flagellin of bacteria
TLR6: Bind to diacyl lipopeptide of Mycobacteria and zymosan of yeast and fungi
TLR7 and TLR8: Bind with single-stranded RNA of viruses
TLR9: Binds with CpG unmethylated dinucleotides of bacterial DNA and herpesvirus
-
TLR10, TLR11:
Several TLRs also function as dimers of which TLR4 can form homodimers and others can form heterodimers. The dimerization of TLRs affects their specificities also. TLR1/TLR2, TLR3, and TLR9 can bind triacylated lipopeptides, double-stranded RNA (dsRNA), and CpG DNA.
Lectins: Lectins facilitate cell–cell contact. They can bind carbohydrate units. Lectins present on one cell can interact with different carbohydrates which are displayed on the surface of another cell. Their interaction is specific but weak thus many interactions occur. Lectins are divided on the basis of their amino acid sequence and properties. C-type lectins are calcium requiring and bind carbohydrates. For example, selectins are present in three forms: L-form on lymph node vessels, E-form on the endothelium, and P-form on activated platelets.
The variety of soluble factors are shown in Fig. 8.3:
Lysozyme: It is a hydrolytic enzyme capable of cleaving bacterial cell wall peptidoglycan, present in tears and mucous secretions.
Interferons: Are group of antiviral proteins.
-
Complement: A group of around 20 serum proteins synthesized by the liver which remain in inactive state. They are converted into active form and ultimately form membrane attack complex (ability to damage the membrane of pathogenic organisms) and in the process release proteins which act as anaphylatoxins (enhance inflammation). Complement system can be activated by itself or by innate immune components (MBL) or by adaptive immunity ( antibody)
The white blood cells or leukocytes participate in innate and adaptive immunity. Lymphocytes (T lymphocytes and B lymphocytes) are involved in adaptive immune responses, and other leukocytes as neutrophils, eosinophils, basophils, monocytes, dendritic cells, and natural killer cells are important cells of innate immunity (Fig. 8.4). They are again divided into granulocytes and agranulocytes [6]. The cells containing granules have a variety of digestive enzymes in them for pathogen clearance, while agranulocytes have other modes of action.
Neutrophils: Are called polymorphonuclear cells, take both the acidic and basic stains, are first cells to respond for infections, and are predominant cells involved in inflammation.
Eosinophils: Take up acidic dye eosin. They are cells which respond against parasitic infections. They are phagocytic and also involved in allergic reactions.
Basophils: They take up basic dye methylene blue and have high-affinity receptors of IgE antibody. When they migrate to tissue, they are known as mast cells. They release variety of allergic mediators and are responsible for allergic reactions.
Monocytes and Macrophages: Monocytes are blood phagocytic cells. They have many enzymes which breakdown the pathogenic cells. When monocytes move into tissue, they are known as macrophages. The various macrophages are microglial cells (brain), mesangial cells (kidney), Kupffer cells (liver), osteoclast cells (bone), alveolar macrophages (lungs), and histiocytes (connective tissue).
Natural killer cells: They have the natural capability to kill virus-infected cells. They are mainly responsible for removal of virus-infected and tumor cells.
Fig. 8.4.
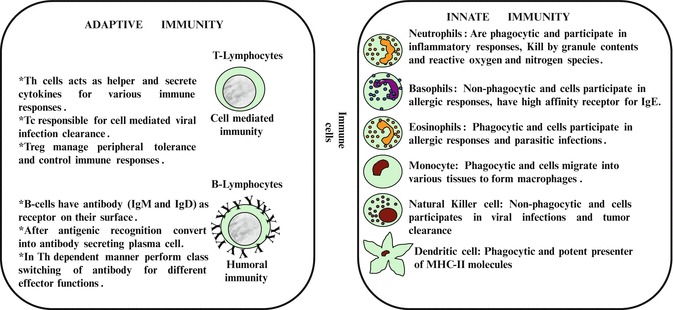
The figure shows various cells involved in innate immunity and adaptive immunity along with their important properties and functions
Some Terms
Antigen: The molecular entities capable of generating immune responses or foreign substances like toxins, pathogens which can bind to the antibodies, or other receptors.
Hapten: Some compounds are antigenic (can bind with antibodies) but are not capable by themselves of inducing a specific immune response, thus are non-immunogenic. Thus, hapten is coupled to an immunogenic carrier, and hapten–carrier conjugate triggers immune responses for hapten antigens , carrier antigens, and new epitopes formed due to hapten–carrier interactions. Dinitrophenol (DNP) is a hapten which cannot elicit antibody response.
Immunogen: Antigen which is capable of mounting adaptive immune responses. An antigen may or may not be an immunogen, but an immunogen is always an antigen. Immunogenicity is determined by four properties like foreignness, molecular size, chemical composition, and complexity.
Epitope: Antigenic determinant or epitope is that specific part of antigen which interacts with complementarity-determining region of an antibody. B cell binds surface regions of antigens as they bind directly; however, T cells recognize processed antigen in association with MHC; thus, TCR recognizes hidden or intracellular moieties.
Antibody: Antibodies are effectors of humoral immune responses. It is a Y-shaped glycoprotein present on B cells as part of its receptor and is also secreted to bind to antigenic determinants. It neutralizes the antigen by activating various immune components. There are five classes of immunoglobulins based upon their effector functions: IgM, IgD (both present on B cell as B-cell receptor), IgG, IgE, and IgA.
Toll-like receptors: Toll-like receptors (TLRs) are a class of proteins that play a key role in the innate immune system. They are transmembrane proteins with extracellular domain of leucine-rich repeats (LRRs). Ten human TLRs have been characterized which play an important role in binding to different PAMPs.
Opsonization: When any antigenic molecule is surrounded and bound by antibody from all sides, the binding of antibody triggers phagocytic cells to readily phagocytose the antigen; the coated particles or antibodies are known as opsonins and the process is called opsonization (Fig. 8.5a).
Antibody-dependent cell-mediated cytotoxicity (ADCC): Natural killer (NK) cells express a membrane receptor (CD16) for a specific portion of the antibody molecule, allowing them to attach to the antibody bound with target. Attachment of NK initiates the cascade of events resulting in the destruction of target cell (Fig. 8.5b). Its granules release perforin and granzyme. Pores formed by perforin assist the entry of granzyme which triggers fragmentation of DNA including viral DNA and cell death.
Fig. 8.5.

The figure shows two important effector functions of antibody. (a) It shows the process of opsonization. When antibody coats a particular pathogen, the process of phagocytosis is facilitated as macrophages have receptor for antibody. It is important for pathogens which resist phagocytosis. The antibody in this is referred as opsonin. (b) It shows ADCC response of antibody. Natural killer cells have receptor for constant region of antibody; thus, they can be recruited for elimination of pathogen. The antibody-bound pathogen is rapidly induced for apoptotic cell death like the response mediated by CTL
Adaptive Immune Responses
The adaptive immune response occurs when recognized pathogen challenge occurs. The response can be elicited by many different unique receptors that have variability in antigen-binding regions and conservation in the remaining regions. Thus, the reactions are highly diverse, are highly specific, and are associated with memory (Fig. 8.4). It occurs after 5–7 days of initial antigen exposure. Thus unlike innate immunity which mounts quick response, it takes time. Adaptive immunity is triggered by innate immunity; thus, response is highly interactive with many co-involvements and cooperation to eliminate pathogen effectively. Thus, adaptive immune response can do self-/non-self-discrimination and is highly specific against a variety of pathogens with tremendous diverse memory [6].
Any substance capable of eliciting an adaptive immune response is referred to as an antigen ( antibody generator). Adaptive responses can be either cell-mediated or humoral immune responses. Both are mediated by white blood cells called lymphocytes. There are two classes of lymphocytes: the T lymphocytes responsible for cell-mediated immunity and B lymphocytes responsible for humoral immunity whose ultimate effectors are antibodies or immunoglobulins.
The humoral branch is mediated by antibodies secreted by activated B cells (called as plasma cells) after they bind any antigenic molecule. The antibodies can be secreted, and binding of antibodies on the viruses and bacteria can either make them very prone for phagocytosis ( opsonization), or they can be destroyed by complement-mediated lysis or through antibody-dependent cell-mediated cytotoxicity ( ADCC). The B cells after recognition of antigen are activated, and in the presence of cytokines derived from Th cell (Th2 which secretes IL-4, IL-5, IL-6, IL-10, and IL-13) and contact with Th cell, they form antibody-secreting plasma cell, start class switching of antibody, and form memory cells [6].
Cell-mediated response occurs when antigen is presented by cells of the body to T lymphocytes. T cells may be CD4+ T-helper (Th) cells, CD8+ T-cytotoxic (Tc) cells, and CD4 and CD25+ T-regulatory (Treg) cells. Treg plays an important role in the regulation of immune responses. Th and TC can recognize antigen only when it is presented on another group of polymorphic proteins known as major histocompatibility complex (MHC). MHC-I is responsible for presentation of virus-specific antigens to Tc cells; thus, all the nucleated cells can activate Tc cells which are capable of killing virus-infected cell. MHC-II is specifically presented on antigen-presenting cells (APCs) which activate Th cells which recruit a number of other immune components to clear these pathogens (Fig. 8.6).
Fig. 8.6.

The figure shows that after antigen is encountered by macrophages and B cells, they present it on MHC-II molecule. Antigen-MHC-II is recognized by T-cell receptor (TCR) of Th cells. Th cells produce Th2 population which is helper cell for B-cell response. In the presence of cytokines derived from Th2 and physical contact with T cell, B cell converts into antibody-secreting plasma cell and memory cell and produces all classes of antibody in response to the antigen. Virally infected cell presents endogenous antigen on MHC-I molecule which is recognized by TCR of T-cytotoxic cell. Th cells in the form of Th1 secrete cytokines for CTL. In the presence of Th1-derived cytokines, Tc converts into activated cytotoxic T lymphocytes (CTLs) which activates procaspase cascade and thus kills the virus-infected cell
Upon recognition of antigen associated with MHC-I, the Tc is activated and forms CTL which releases its granule content rich in perforin and granzyme. This induces the target cell to undergo apoptotic cell death.
Medical Microbiology
The research is increasingly showing the role of pathogen in several diseases which in earlier days were believed to be noninfectious disease. The usage of nucleic acid amplification technique is able to show the involvement of pathogenic agent in several nervous system disorders which otherwise were considered nonpathogenic (Table 8.1).
Table 8.1.
Shows the involvement of pathogenic agents in the diseases which were earlier believed to be non infectious diseases
| Papillomavirus | Invasive cervical cancer |
| Helicobacter pylori | Peptic ulcers |
| Herpesvirus types | Kaposi’s sarcoma |
| Epstein–Barr virus | Hodgkin’s disease and certain lymphomas |
The ongoing research might possibly indicate the role of infectious agent in the etiology of rheumatoid arthritis, sarcoidosis or inflammatory bowel disease, and atherosclerosis.
There is emergence of new diseases resulting from changes in the pathogenic agent like changes in coronavirus and onset of severe acute respiratory syndrome (SARS) in 2003 and H5N1 avian influenza virus from poultry farms to humans. These pose a threat as well as challenge to humankind. The understanding of emergence of the disease requires host– pathogen interaction, which is influenced by geography, environment, age, and nutritional status [5].
There is essential requirement of record of the history, behavioral parameters, traveling information, etc. for the effective and early management of the disease. For example, a patient has encountered a pathogenic strain from a geographical area where antibiotic- or drug-resistant strains are predominant. In case a patient has acquired the disease from that region, then the normal medicines would unknowingly delay the intervention in the life cycle of the pathogen resulting in serious condition or death. However, history would provide information about the prevalence of pathogenic strains from that niche for appropriate treatment.
The clinical laboratory or hospital laboratory which undertakes testing of microorganisms should have safety features so that health-care workers remain safe from these infectious agents:
Microorganisms are studied in clinical hospital laboratories, reference laboratories, and research facilities.
There should be appropriate posting of signs regarding safety. These are very important to ensure safety.
Handling of sample with highly contagious microorganism would require high security, appropriate masks, and working in biosafety hoods to avoid splashing or inhaling.
The laboratory should have well-defined compartments, equipped for each kind of application along with efficient energy-based refrigeration unit for sample and reagent storage. This is important to get accurate results.
In a hospital microbiology laboratory, the blood cultures are incubated and monitored electronically for bacterial and fungus growth. High-tech instruments are used to aid in the identification of microorganisms. Teamwork is essential in all types of laboratories [5].
The invasion of pathogen can be described in three steps:
Colonization: Pathogen presence in or on the host
Infection: Attachment and penetration of pathogen inside the host; bypass defense responses of the host immune system
Disease: Is caused by action of endotoxin/exotoxin/metabolites secreted by the pathogen in the host
The onset of disease often results in clinical signs and symptoms.
Adhesives of Pathogens
The bacterial pathogens often use pili, flagella, or lipopolysaccharide for binding to various host receptors. The virus uses variety of adhesive which can bind to multiple components of the host (Table 8.2).
Table 8.2.
Adhesive proteins used by virus for binding to host cell via host receptor
| Agent | Adherence factor | Host receptor |
|---|---|---|
| HIV | Envelope glycoprotein (gp120) | CD4 and chemokine receptor CXCR4 |
| Measles virus | Hemagglutinin (H) glycoprotein | CD46 and membrane-organizing protein moesin |
| Herpes simplex virus | Glycoprotein C (gpC) | Heparan sulfate |
| Influenza virus | Hemagglutinin, neuraminidase | Sialic acid |
| Epstein–Barr virus | Surface protein | CD21 |
| Adenovirus | Fiber protein | Integrins (vitronectin receptors) |
Gram-Positive and Gram- Negative Infections
Gram staining: This method is based upon the fact that crystal violet is capable of irreversible staining of some bacteria which are referred as gram positive (Bacillus, Staphylococcus, Streptococcus, Enterococcus, Diplococcus, etc.), and in others the stain can be washed off, that is, they are decolorized and take up counterstain and are referred as gram negative. The stain is taken up due to the cell wall components present in the microorganisms. This test is rapid and gives a good indication about the infectious agent so that before exact identification is done, a choice antibiotic therapy may be started [5].
The culture positivity or negativity confirmation along with antibiotic sensitivity results in better selection of antibiotic so that infection can be efficiently managed. Many modifications of gram staining are now in use to efficiently detect the pathogenic strain.
Tables 8.3 and 8.4 show some gram-positive and gram-negative microorganisms, respectively, along with the consequences of their infections. Their microscopic appearance has been shown for some gram-positive and gram-negative bacteria in Figs. 8.7 and 8.8, respectively.
Table 8.3.
Gram-positive infections and causative organisms
| Gram-positive infections | Pathogenic strains | Diseases and symptoms | Morphology |
|---|---|---|---|
| Pneumococcal infections | Streptococcus pneumoniae | Otitis media, acute purulent rhinosinusitis, pneumonia, meningitis | Grows in chain |
| Staphylococcal infections | Streptococcus aureus | Toxin- and non-toxin-mediated infections, surgical wound infections, primary bacteremia | Forms grapelike clusters |
| Streptococcal infections | Group A Streptococcus pyogenes | Pharyngitis, post-infectious symptoms of acute rheumatic fever, and glomerulonephritis | Spherical to ovoid, grow in chains |
| Group B Streptococcus agalactiae | Bacterial sepsis, meningitis in newborns, endometritis, and fever in parturient females | ||
| Enterococci (group D streptococci) | Enterococcus faecalis, E. faecium | Urinary tract infections, nosocomial bacteremia, endocarditis | |
| Corynebacterial infections | Corynebacterium diphtheriae | Nasopharyngeal and skin infections, toxin causes systemic toxicity, myocarditis, polyneuropathy | Club-shaped bacillary appearance forming clusters |
| Listeria | Listeria monocytogenes | Food-borne pathogen, causes serious infections in immunocompromised individuals | Rod shaped |
| Clostridial infections | Clostridium tetani | Tetanus: neurologic disorder, increased muscle tone, and spasms due to tetanospasmin (toxin) | Resembles tennis racket |
| Clostridium botulinum | Botulism: paralytic disease due to neurotoxins, proceeds with cranial nerve involvement | ||
| Clostridium perfringens | Gas gangrene (bacteremia) due to active tissue and enterotoxins |
Table 8.4.
Gram- negative infections and causative organisms
| Gram-negative infections | Pathogenic strains | Diseases and symptoms | Morphology |
|---|---|---|---|
| Meningococcal infections | Neisseria meningitidis | Causes life-threatening meningococcal meningitis and fulminant meningococcemia | Gram-negative aerobic capsular diplococci |
| Gonococcal infections | Neisseria gonorrhoeae | Causes sexually transmitted infections as gonorrhea which manifests as cervicitis, urethritis, conjunctivitis | Monococci or diplococci |
| Haemophilus infections | Haemophilus influenzae | Local invasion of mucosal surfaces; otitis media (middle ear through Eustachian tube) | Has variable shape (coccobacillus) |
| HACEK group infections | Haemophilus sp. | Reside in oral cavity and cause local infections of the mouth, sometimes severe systemic infections as bacterial endocarditis | HACEK are fastidious, gram-negative, slow growing, carbon dioxide-requiring organisms |
| Actinobacillus actinomycetemcomitans | |||
| Cardiobacterium hominis | |||
| Eikenella corrodens | |||
| Kingella kingae | |||
| Pertussis | Bordetella pertussis | Causes violent cough; inspiratory sound at the end of coughing gives the common name as whooping cough for the illness | Aerobic bacilli |
| Enteric bacilli | Escherichia coli | Global pathogens; oropharyngeal colonization may lead to pneumonia | Have extracytoplasmic outer membrane, lipopolysaccharides |
| Klebsiella | |||
| Proteus, Enterobacter | |||
| Serratia | |||
| Citrobacter | |||
| Pseudomonas | Pseudomonas aeruginosa | Infections in hospital patients |
Fig. 8.7.
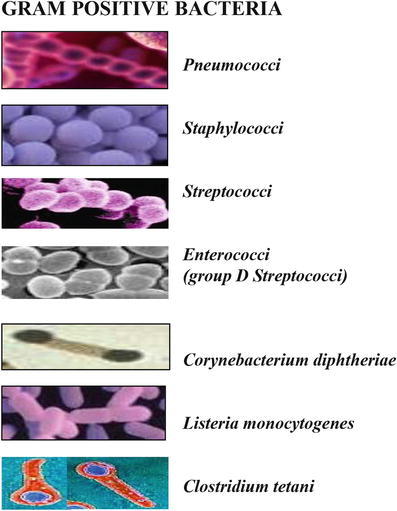
The figure shows the microscopic shape and pattern of various gram-positive bacteria which are causative agent of many human diseases
Fig. 8.8.
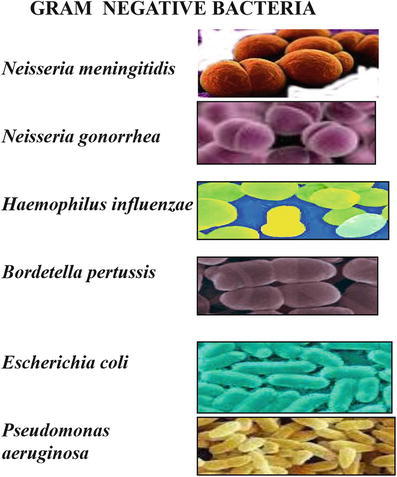
The figure shows the microscopic shape and pattern of various gram-negative bacteria which are causative agent of many human diseases
Pyrexial Illness
Pyrexia is a physiological response of illness. Pyrexia is also known as fever or hyperthermia and is manifested as elevated temperature. It is due to increase in thermal set point, that is, above the normal body temperature of 97.7–99.5 °F. Fever is a useful defense mechanism, as immune response of the body mediates its response effectively at high temperature. During fever, muscle tone of the body is increased, which presents as chills. Fever is presented by many diseases as tropical or environmental diseases, but one should remember that many common infections like influenza and tuberculosis also occur in the tropics or may be acquired en route to and from. Exotic local febrile patient may also be due to autoimmune or malignant condition. The causes of fever may be bacterial or viral or fungal infections or autoimmune condition or malignancy or folate deficiency:
Pathophysiology: Temperature is ultimately regulated by the hypothalamus; it triggers the fever by inducing pyrogens. The hypothalamus is acted upon by prostaglandin E2, generating systemic response in the body causing heat-creating effect to match a new temperature level.
Pyrogen: Pyrogen is a substance which induces fever; it may be endogenous or exogenous. Exogenous pyrogen may be bacterial lipopolysaccharide (LPS), and endogenous pyrogens are various cytokines like IL-1 (α and β), IL-6, IL-8, TNF-β, macrophage inflammatory protein β, interferon-α, and interferon-β.
Diagnosis of pyrexia: Diagnosis is made by clinical symptoms as increase of temperature, chills, rigor, and increase in muscle tone. For pattern of temperature, diagnosis is confirmed by blood and serological examination (TLC, DLC, ESR, CRP) or by culture and sensitivity test. Pyrexia is managed by treating the cause and antipyretics [5].
Infections of the Gastrointestinal System
The diseases affect the digestive organs because of infectious agents as certain bacteria (Escherichia coli (E. coli), Vibrio cholerae, Salmonella, and Shigella)), protozoa (Entamoeba histolytica), or viruses. Parasites causing gastrointestinal tract infections and infestations are Entamoeba histolytica, Ascaris lumbricoides, Taenia saginata, Taenia solium, Hymenolepis nana, Giardia, Cryptosporidium, etc. These infections are often associated with nausea, vomiting, diarrhea, and other gastrointestinal symptoms like dysentery or bleeding diarrhea and may last for 5 or 7 days. The infections may be mild to severe and are either through contaminated food (raw, undercooked, or uncovered food) and/or water (contaminated water).
Gastrointestinal infections present commonly with diarrhea characterized by frequent and watery bowel movement. Virus-induced diarrhea is known as viral gastroenteritis and may be due to Rotavirus. Usual GI symptoms are abdominal cramping, followed by diarrhea, fever, loss of appetite, nausea, vomiting, weight loss, dehydration, and mucous or blood in stool. These symptoms typically last for a few days or longer. Viral diarrhea usually goes away without treatment by drinking plenty of fluid to avoid dehydration, while some types of diarrhea require antibiotic treatment to eliminate the causative agents.
Infections of the Skin and Nail
The skin is the outermost covering of the body which consists of an outermost layer called the epidermis and inner layer the dermis. The epidermis is thin having several layers of epithelial cells of which the stratum corneum being the outermost is composed of dead cells with waterproof protein keratin and creates an effective physical barrier. The inner layer dermis consists of connective tissue and hair follicles, sweat gland, and oil gland duct, containing salt, lysozyme, and sebum (secreted by oil glands) that prevent skin from drying out and also serve as nutrients for certain microorganisms.
Normal microbiota of the skin contains a large number of gram-positive bacteria as Staphylococcus and Micrococcus which survive antimicrobial properties and his salt concentration of the skin. Microorganisms also reside in the hair follicles and sweat glands. The moistured parts like armpits and legs have higher population of microbes. Other organisms contributing to microbiota are gram-positive pleomorphic rods called diphtheroids like Propionibacterium acnes which reside in hair follicles and are anaerobic [5].
Lesions on the skin indicate the microbial disease. They are:
Vesicles: Small, fluid-filled lesions
Bullae: Vesicles larger than 1 cm in diameter
Macules: Flat reddened lesion
Papules: Raised lesions
Pustules: Raised lesions with pus
The important infectious agent may be bacteria or viruses or fungi or parasites. The important bacterial diseases are:
Acne: Common skin disease resulting in inflammatory lesion due to blockage of channels for the passage of sebum to the skin surface. Acne is usually treated with azelaic acid (Azelex), salicylic acid preparation, or retinoids. Inflammatory acne resulting in appearance of pustules and papules is caused by Propionibacterium acnes, an anaerobic diphtheroid present on the skin. The treatment for these is phenyl peroxide (available as Benzamycin), antibiotic erythromycin or isotretinoin, or clear light system.
Erysipelas: Appears after Streptococcus pyogenes (gram-positive bacteria) infects the dermal layer of the skin. The disease shows eruption of the skin into reddish patches with raised margins. The risk of this may be its progress to local tissue destruction followed by entry into the blood vessel resulting into sepsis. The treatment is β-lactam antibiotics.
Necrotizing fascitis: The invasion of streptococci with excessive tissue destruction results in necrotizing fascitis. It might be caused by exotoxin A, which acts as super antigen. The treatment is penicillin.
Impetigo: Commonly in hospitals, pathogenic strain staphylococci produce enterotoxins, leukocidins, and exfoliative toxins resulting in impetigo of the newborn. Symptoms are thin-walled isolated vesicles that rupture and later crust over. Treatment is hexachlorophene containing skin lotions.
Folliculitis: Caused by Staphylococcus and the most common skin microbiota. S. aureus enters through the opening in the skin and the hair follicle passage. Infection of hair follicle occurs as pimple on the skin and sty of eyelashes. Serious hair follicle infection is furuncle which is abscess surrounded by inflamed tissue. In case neighboring tissue is invaded, this results in excessive damage (carbuncle) with the symptoms of generalized illness with fever. The invasion of infectious agent to underlying tissue and entry into the bloodstream are serious health risks associated with Staphylococcus infection.
Pseudomonas dermatitis and otitis externa result from infection of Pseudomonas aeruginosa leading to superficial rash. In otitis externa, infection of the external ear canal occurs. The treatment is fluoroquinolones.
The common viral diseases of the skin are:
Measles: Also known as rubeola in which virus spreads through respiratory route and is highly contagious; the symptoms appear after 10–14 days of virus exposure. The symptoms are reddish macules appearing on the face and spreading to the trunk and extremities. Vaccine of measles, mumps, and rubella (MMR) has almost eliminated the measles.
Rubella (German measles) is caused by Rubella virus. The disease has symptoms like measles but is mild and less extensive which usually disappears in 3 days.
Small pox: Caused by variola virus. The effective vaccination has almost eradicated the disease. The symptoms are confluent pustules on the skin; the later stage may affect internal organs.
-
Chicken pox: Results from infection by varicella zoster virus. The symptoms are vesicles present on the face, throat, and lower back. The therapy is virostatic drugs. Shingles is caused by herpes zoster. The symptoms are appearance of vesicles on one side of the waist, face or scalp, or upper chest.
Herpes simplex virus type I infection results in cold sores in which vesicles around the mouth are visible.
-
Fungal diseases
Ringworm also known as tinea results from infection of Microsporum, Trichophyton, or Epidermophyton species. The symptoms are skin lesions of varied appearance. The treatment is antibiotic griseofulvin or topical applications of miconazole or clotrimazole.
Candidiasis: Results from Candida albicans which usually infects the mucous membrane or moist areas of the skin. The topical application of miconazole and clotrimazole is effective.
The other common parasitic infections are scabies (Sarcoptes scabiei (mite)). Symptoms are appearance of papules and the treatment is gamma benzene hexachloride or permethrin.
Infections of the Respiratory System
Diseases of the respiratory system are often manifested by symptoms of dyspnea (shortness of breath), or cough, or chest pain, or abnormality on a chest radiograph. As the symptoms often overlap in various respiratory diseases, the differential diagnosis is required from the history, physical examination, pulmonary function testing, etc., and they may or may not be associated with sputum. The most abundant microflora of the respiratory tract suppresses the growth of the pathogenic bacteria in the upper respiratory tract. There are a variety of symptoms because of infections of various regions of the respiratory system [5].
Pharyngitis: Inflammation of the mucous membranes of the throat or sore throat.
Laryngitis: Infection of larynx.
Tonsillitis: Inflamed tonsils.
Sinuses: Nasal sinuses are cavities in certain cranial bones that open into the nasal cavity lined with a continuous mucous membrane. Infection of the sinus leads to inflamed mucous membrane resulting in heavy nasal discharge, a condition called sinusitis. Blockage of the sinus leaves to internal presence causing pain or sinus headache.
Strep Throat
This is caused due to Streptococcus pyogenes (group A beta hemolytic bacteria). The symptoms of the disease are inflammation of the mucous membrane along with fever. Lymph nodes located in the neck are enlarged and tender. The disease is diagnosed by indirect agglutination and treated by penicillin.
Diphtheria
Caused by Corynebacterium diphtheriae. Exotoxin is the cause of symptoms which inhibits translation resulting in tissue and organ damage. The antitoxin therapy and antibiotics are used to cure the disease.
Otitis media
This is caused by Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, Streptococcus pyogenes, and Staphylococcus aureus. In this ear, ache occurs after nose and throat infections. Pus accumulation causes pressure on the eardrum. Treatment is amoxicillin (broad-spectrum penicillin).
Common cold
Results from infection of 200 different viruses. Symptoms include sneezing, nasal secretions, and congestion.
Pertussis (whooping cough)
Caused by Bordetella pertussis. The disease symptoms are because of congestion of the trachea and bronchi due to accumulation of mucous. The bacteria produce toxins and destroy the ciliated cells of the trachea. Vaccination is very effective in reducing the incidences of the disease.
Tuberculosis
The causative agent for tuberculosis (TB) is Mycobacterium tuberculosis. The bacteria contain lots of lipids which aids in their resistance to drying and antimicrobial agents. M. tuberculosis forms lesions known as tubercles. These lesions along with macrophages might calcify and appear clearly on X-ray films. Infection progresses when lesion ruptures releasing bacteria into the lung airways, lymphatics, and cardiovascular system leading to military tuberculosis. In this, the patient suffers from weight loss, cough sometimes with blood, and loss of appetite. Initially effective drug for TB was streptomycin. Currently, the patient is administered with multiple drugs as isoniazid, rifampin, and pyrazinamide. Noncompliance to medication during treatment in part is responsible for emergence of multiple drug-resistant strains which are posing serious problem. The Bacillus Calmette–Guerin (BCG; frequent in humans which affects the bones or lymphatics) is being widely used in the world as vaccine.
Pneumonia
Caused by Streptococcus pneumoniae; apart from this, pneumonia may also be caused by fungi, protozoa, viruses, as well as other bacteria and is known as atypical pneumonia. Pneumonia is named after the respiratory site of the infection:
Lobar pneumonia: Lobes of lungs are infected.
Bronchopneumonia: Alveoli of the lungs are infected.
Pleurisy: Pleural membranes become painfully inflamed.
Disease caused by S. pneumoniae is known as pneumococcal pneumonia (formerly Diplococcus pneumoniae). The capsules form the basis of serological differentiation of pneumococci into 90 serotypes. The symptoms include high fever, breathing difficulty, and chest pain. Effective drugs are penicillin and fluoroquinolones. Subunit vaccine from purified capsular material of the 23 types of pneumococci has been developed [5].
Respiratory syncytial virus (RSV)
The disease is prevalent in infants and infection of the bronchial epidermis occurs during the winter and early spring. The name is derived from syncytium (cell fusion) formation in cell culture. For severe symptoms the antiviral drug ribavirin is administered.
Influenza
The disease is characterized by chills, fever, headache, and muscular aches. Recovery occurs fast and cold-like symptoms appear. Influenza virus has eight separate RNA segments with inner protein and an outer lipid bilayer. Two types of projections embedded in the lipid bilayer are hemagglutinin (H) and neuraminidase (N) spikes. H spikes (about 500 on virion) allow the virus to recognize and attach to cells of the body; this causes agglutination of RBCs. N spikes (about 100 per virus) help the virus to separate from infected cells after intracellular reproduction. Antibodies against H spikes are more important in the resistance of body to the disease. Viral strains are identified by variation in H and N antigens. Different forms of antigens are designated as H1, H2, H3, N1, and N2. The different numbers show substantial alteration in the protein composition of spikes which are referred as antigenic shifts, and they escape from the previous immunity developed in the human body. High mutation rates are characteristic of RNA viruses. The major cause of antigenic shifts is genetic recombination which might occur in infections involving more than one strain and mixing of RNA from strains of animals (swine, horses, and birds) with RNA of human strains. Swines may be infected with both human and fowl influenza, and likely animals involved in shifts therefore are referred as mixing vessels [5].
Minor variation in antigenic makeup is called antigenic drift which might reflect alteration of only single amino acid which is probably due to selective pressure of antibody. The effect of antigenic drift results in low efficacy of vaccine against a particular spike (H2) after 10 years in H2 only. Influenza viruses are also classified according to antigens of their protein coat viz., A, B, and C. A-type cause major pandemics; B viruses are geographically limited and cause mild infections.
These are the reasons that it is not possible to develop an effective vaccine for influenza that can give long-term immunity. The vaccines developed are usually multivalent with 70–90 % protection but duration of protection is not more than 3 years.
Epidemics of the flu are due to a new strain of virus which quickly propagates through population. The cause of death is not influenza virus but often it is secondary bacterial infections (H. influenza, S. aureus, S. pneumoniae).
In 1918–1919 more than 20 million people died in major pandemic of influenza with highest mortality rates in young adults, often dying within a few hours. The infection is restricted to the upper respiratory system but, due to some changes in virulence, results in invasion of the lungs causing viral pneumonia.
The antiviral drugs are amantadine and rimantadine which significantly reduce the symptoms of A-type virus. Inhibitors of neuraminidase-2 zanamivir (Relenza) which can be inhaled and oseltamivir phosphate (Tamiflu) are administered orally.
Fungal diseases: The fungal diseases of the respiratory system are histoplasmosis (inhalation of airborne conidia), coccidioidomycosis (inhalation of airborne arthrospores), and Pneumocystis pneumonia (Pneumocystis jirovecii causes inflammation and fluid buildup in lungs).
Infections of the Nervous System
The nervous system consists of the central nervous system (CNS) with the brain and spinal cord and the peripheral nervous system consisting of all the nerves that branch off from the brain and spinal cord. These nerves are the lines which send and receive the signal from the body to the brain (sensory) and from the brain to the body (motor) and thus coordinated the body. The brain and spinal cord are protected by three continuous membranes called meninges (outermost duramater, central arachnoid mater, and innermost pia mater). Between the inner and middle layer is a space called subarachnoid space in which human adults have 100–160 ml of cerebrospinal fluid (CSF).
The blood–brain barrier protects the brain by restricting components of the blood to enter the brain, but some selective substances pass through certain capillaries; lipid soluble molecules can gain entry. Though the CNS has high level of protection, still certain microorganism can gain entry because of trauma, nerve supply, blood, and lymphatics. The inflammation then occurs in the meninges ( meningitis) or brain (encephalitis) [5].
Meningitis: Meningitis may be caused by different types of pathogens including viruses, bacteria, and fungi. Its more than 70 % of cases are caused by bacterial species, as gram-positive Streptococcus pneumoniae and Neisseria meningitidis. They possess capsule that protects them from phagocytosis, and they rapidly multiply in blood and afterward enter the cerebrospinal fluid. The symptoms are fever, headache, and stiffness in the neck followed by nausea and vomiting. The diseases may progress due to the release of endotoxins of the gram-negative pathogens or the release of cell wall components (peptidoglycans and teichoic acids) of gram-positive bacteria. Quick treatment is required with broad-spectrum third-generation cephalosporins.
-
Tetanus: The disease is caused by an obligatory anaerobic, endosperm-forming, gram-positive Clostridium tetani. The symptoms are due to potent neurotoxin, tetanospasmin, which affects relaxation of muscles causing muscle spasms. The jaw muscles are the early target which prevents the mouth from opening known as lockjaw [5].
Spasms in the back muscle cause the head and heel to bow backward (opisthotonos). Death results from spasms of respiratory muscles. Effective vaccination has reduced the incidences. Both attenuated and subunit (tetanus toxoids) vaccines are available:
Botulism: The causative agent is anaerobic, endospore-forming gram-positive Clostridium botulinum. Exotoxin produced the most potent of all natural toxins which blocks the release of acetylcholines. The patient undergoes a progressively flaccid paralysis for 1–10 days and may die from respiratory and cardiac failure. Botulism toxin is used for cosmetics as Botox.
Leprosy: Due to infection of Mycobacterium leprae in the peripheral nervous system. The organism was isolated by Gerhard A. Hansen and formally known as Hansen’s disease. It usually invades cells of the peripheral nervous system. Sulfone drugs as dapsone and other drugs as rifampin and clofazimine are effective [5].
Poliomyelitis: The paralytic form of polio appears in less than 1 % of infected people, whereas majority of the cases are asymptomatic or present with mild symptoms such as headache, sore throat, fever, and nausea. The mode of transmission is through contaminated water and affects the throat (sore throat) and small intestine. The virus enters the lymph nodes and then blood and afterward penetrates the central nervous system. The virus invades and destroys motor nerve cells of the upper spinal cord; sometimes, death can result from respiratory failure. There are three different serotypes of virus. The Salk vaccine uses inactivated polio virus, whereas Sabin is oral polio which is attenuated. The use of vaccination has almost eradicated polio from the population. The use of Sabin/oral polio is not recommended as reversion to virulent state and symptoms in immunocompromised host pose a threat of the disease [5].
Rabies: (Latin, rage or madness) The disease is caused by rabies virus which is transmitted to humans by bite of infected animals (dogs, cats, bats, foxes, etc.). The virus from skeletal muscles and connective tissue moves to CNS where it causes encephalitis. The symptoms are mild and varied and sometimes thought/sight of water can result in fear called hydrophobia. The end stage of disease is due to excessive damage to the nerve cells of the brain and spinal cord. Passive vaccination is preferred as precaution [5].
Diseases Caused by Prions
Prions are abnormally folded proteins capable of inducing change in the shape of a normal protein. The disease has long incubation times with slow damage without any clinical symptoms. In humans transmissible spongiform encephalitis (spongy/porous degeneration of the brain) known as Creutzfeldt–Jakob disease (CJD) is present. CJD often occurs in families.
Sexually Transmitted Diseases (STDs) and Congenital Infection
Sexually transmitted diseases (STDs) are prevalent diseases in different parts of the world and are posing major health burden. They not only spread dramatically from one person to another, but they are also passed on to the next generation either as congenital diseases or during child birth [1–3]. Thus, before starting these diseases, one crucial thing would be prevention. Prevention can be achieved by:
Educating patients who are at risk for STDs.
Counseling and support for the high-risk patients.
Detecting asymptomatic or symptomatic patients who are unlikely to seek treatment providing effective diagnosis and treatment of those with STDs.
Evaluating, treating, and counseling the sexual partners of those with STDs.
Immunizing patients who are at risk for STDs that are preventable by vaccination.
Testing for HIV and hepatitis in any patient diagnosed with STD, which is an important preventive measure.
Counseling about the patient’s potential risk for contracting HIV or other STDs should be done before and after testing [7].
Important STDs are syphilis, gonorrhea, HIV, hepatitis B, and chancroid. Others are chlamydial infections, genetic infections with HPV, and genital herpes which can spread very fast. They are more prevalent in individuals with frequent partner change or having multiple partners [1–3].
Syphilis
It is a bacterial disease with Treponema pallidum as the causative agent. The disease may be acquired by sexual intercourse or may be transmitted from mother to baby (congenital syphilis) or occasionally by blood transfusion or by nonsexual contacts. Effective prevention and identification of syphilis in pregnant patients requires routine serology to be performed for all pregnant patients at the time of their first prenatal visit. The pathogen causes erosion, ulcer, and vasculitis, and thereafter it may spread into regional lymph nodes. The syphilis can be divided into primary, secondary, latent, and tertiary stages. The lesion, chancre, appears as anogenital ulcer, which can also spread to extra-anogenital sites like the lip, tongue, and tonsils. Secondary syphilis presents itself with rash affecting the palms and sole which later on becomes papules. Tertiary syphilis is manifested with gummatous, cardiovascular, and neurological involvement. Syphilis is diagnosed by identifying treponemes using dark field microscopy or by serological tests. Treatment of choice is intramuscular benzathine penicillin [1–4].
Hepatitis B Virus (HBV)
Sexual transmission is responsible for 30–60 % of new cases of HBV. The risk of perinatal transmission from positive mothers to infants is as high as 85 %. Among these 90 % of infected infants progress to chronic HBV. Immunization is preventive and no other specific treatment for acute HBV exists. Interferon therapy (alpha-2b interferon (Intron A) and lamivudine (Epivir)) is available, but only 40 % is effective in eliminating HBV.
Hepatitis A Virus (HAV)
HAV is transmitted by household and sexual contacts. No treatment is available presently for acute HAV infection except supportive therapy. Passive treatment with antibodies given early can prevent 85 % of new HAV infections. Two vaccines for HAV (Havrix, Vaqta) are given in two-dose series at the interval of 6 months. The first dose gives 99–100 % response, while the second dose provides long-term immunity.
Pelvic Inflammatory Disease (PID)
PID is caused by gonorrhea and chlamydia. PID affects the upper female reproductive tract, developed in 10 % of women. During infection with PID, there are chances of its worsening due to invasion and infection with other infectious agents. PID is presented with mild or nonspecific symptoms and sometimes goes asymptomatic. Missed diagnosis leads to damage to the reproductive tract. Oral antibiotics should be used for its management. Amoxicillin–clavulanic acid (Augmentin) along with doxycycline is effective.
Genital Herpes
Mild or asymptomatic genital herpes is also a common infection in many individuals. The infection can be passed on during delivery; thus cesarean section is recommended for infected females. For the treatment of genital herpes, two new antiviral drugs, famciclovir (Famvir) and valacyclovir (Valtrex), are used in addition to established therapy with acyclovir (Zovirax). The therapy may decrease the severity and duration of a genital herpes outbreak; treatment is effective if started within 24 h of infection.
Gonococcal and Nongonococcal Urethritis
Urethritis: Urethritis can be caused by Neisseria gonorrhoeae, Chlamydia trachomatis, Mycoplasma genitalium, Ureaplasma urealyticum, Trichomonas vaginalis, herpes simplex virus (HSV), etc. In men it produced urethral discharge or dysuria, and in women it causes internal dysuria (without urinary urgency), pyuria, and absence of E. coli. Dysuria which is associated with vulvar herpes or vulvovaginal candidiasis is referred as external as it is painful when comes in contact with urine. Initial evaluation includes urethral discharge, gram staining, and test for N. gonorrhoeae and C. trachomatis. Quinolines were given for treatment of gonorrhea as quinolines are a simple, safe, and effective treatment for gonococcal infections of any severity. However, because of growing resistance of Neisseria gonorrhoeae, the guidelines suggest treatment with cefixime (Suprax) or ceftriaxone (Rocephin). In the absence of gonococci in gram stain, urethritis treatment is directed toward nongonococcal urethritis (NGU). Mycoplasma genitalium is a new etiologic agent added to the list of bacteria that cause nongonococcal urethritis (NGU) in addition to Chlamydia trachomatis. Azithromycin in a single dose or doxycycline was recommended for the treatment of NGU.
Vulvovaginal candidiasis: Caused by Candida albicans with symptoms of vulval itching with or without irritation. It is accompanied by vaginal discharge which is clumped, scanty, adherent plaques with white color. Microscopic evaluation reveals leukocytes, epithelial cells, mycelia, or pseudomycelia in 80 % of positive culture. Topical and oral antifungal like miconazole, clotrimazole or fluconazole are given.
Trichomonal vaginitis: The causative agent is Trichomonas vaginalis with symptoms of vulval itching with discharge which is homogeneous, white or yellow, profuse, and purulent and causes erythema of the vaginal and vulvar epithelium. Microscopic examination reveals leukocytes with motile trichomonads in 80–90 % of symptomatic patients. For diagnosis, nucleic acid amplification technology ( NAAT) for T. vaginalis is used and the treatment is metronidazole.
Bacterial vaginosis: Also formerly known as nonspecific vaginitis caused by Gardnerella vaginosis, various anaerobic or non-cultured bacteria, and mycoplasmas. The symptoms include moderate, white or gray, homogeneous, low viscosity, malodorous discharge. Treatment includes metronidazole and clindamycin.
Noncervical human papillomavirus: Major infections of genital human papillomavirus (HPV) infection occur annually with sexual transmission. In most patients with genital HPV, the infection is asymptomatic, subclinical, or unrecognized. The disease may be diagnosed by clinical assessment or biopsy of the lesion. The main goal of therapy for noncervical HPV infection is to treat symptomatic visible lesions by applying podofilox (Condylox) 0.5 % solution or gel. There is no evidence that treatment decreases infectivity or changes the natural course of HPV infections or the risk of development of cervical cancer.
Human immunodeficiency virus (HIV): Is caused by RNA virus of retrovirus family by human immunodeficiency virus type I (HIV-1). Acquired immunodeficiency syndrome (AIDS) is one of the most important sexually transmitted disease. Its epidemic was recognized long back, and despite major advances in prevention and treatment of the disease, the epidemic continues and has devastating effects on human society. The virus critically attacks CD4+ T cells which are active mediators of cell-mediated immunity. The end stage of the disease is severe acquired immunodeficiency with lots of infection occurring in the HIV patients. The typical case of HIV disease then manifests itself as evidenced by certain malignancies and unusual microbial infections that often attack the lungs, intestines, skin, eyes, or the central nervous system.
HIV can be detected in body fluids like blood, semen, and vaginal secretions in the patients. HIV disease spreads mainly by unprotected sexual intercourse, sharing hypodermic needles, blood transfusion, or from mother to newborn.
The prevention, detection, and treatment of STDs is very important. The recommendations of CDC should be integrated in clinical practice to reduce the morbidity and mortality because of STDs.
Characterization of Pathogens
The practice of clinical microbiology has changed with the advancement in the techniques of molecular diagnostics. The technique of PCR and the machines available are very user-friendly that helps in the detection of pathogen. For detection and characterization of pathogens, many techniques and assays are approved by the US FDA and many more are in the process of development.
In most of the cases, several tests are sought from the clinical laboratory, but occasionally the help of the laboratory is required for exclusion of certain pathogen from the sample, e.g., exclusion of HSV infection in cerebrospinal fluid sample. Help is also required for the best antimicrobial agent for the suppression of growth of pathogen and thus symptoms of the disease.
As new pathogens are evolving and many a times symptoms are confusing, thus the role of clinical microbiologist is very important because the working professional should be aware of the potential pathogens which may be present in the clinical sample.
The molecular diagnostic techniques which are used to detect and characterize the pathogens may be separated into broad categories. The aim of these methods is either to detect a pathogen or exclude the presence of the particular pathogen with an indication about the extent of the presence (titer).
Direct hybridization: These techniques allow for the rapid detection and characterization of bacteria and fungi in the blood sample. In situ hybridization uses either fluorescent probes ( fluorescence in situ hybridization (FISH)) or chromogenic probes (chromogenic in situ hybridization (CISH)):
They may be used for detection of pathogen in blood sample or other clinical samples. It can be used for rapid characterization of bacteria and fungi both in fluids and in histologic section.
This may be used to differentiate microorganisms of similar morphotypes in positive culture samples (gram-positive cocci or acid-fast bacilli).
Before its usage, the preliminary information obtained from traditional techniques is helpful as it helps to make appropriate selection of probes, e.g., differentiating gram-positive or yeast species or presence of Pseudomonas or other members of Enterobacteriaceae in case of gram-negative culture.
The FISH assays are currently available in North America to detect and differentiate S. aureus from other gram-positive cocci in clusters and Candida albicans from other yeasts.
It can detect common cause of infection in cystic fibrosis and can differentiate Mycobacteria or trypanosomes in sleeping sickness. It is also helpful in detecting Legionella pneumophila and differentiates filamentous fungi and yeast and yeastlike fungi. It can also help separate the systemic .dimorphic fungi, which appear as yeast (e.g., Histoplasma capsulatum and Blastomyces dermatitidis) or spherules (Coccidioides immitis from Candida and Cryptococcus species).
The hybrid capture (Digene) technology has been used for detection of high-risk HPV subtypes, Cytomegalovirus, HBV, Neisseria gonorrhoeae, and Chlamydia trachomatis.
Nucleic Acid Amplification Technology (NAAT)
Monoplex assays detect a single target and provide present- or absent-type result. For example, PCR performed for specific species may be used to detect presence or absence of that pathogen, e.g., Legionella pneumophila.
Used as quantitative methods, it can provide quantitative information (viral loads).
In a multiplex reaction where more targets may be detected, it allows the detection of multiple pathogens simultaneously. Multiplexing in real-time PCR setting is more useful which helps in simultaneous detection and differentiation of respiratory viral pathogens like influenza A, influenza B, and respiratory syncytial virus (RSV).
Broad-range nucleic acid amplification is also useful which is used to detect a wide variety of microorganisms. Quantitative data indicated the load of the organism, and positive result indicates the presence of one of the members of that particular group of microorganism.
PCR and NAAT technologies have large diagnostic relevance for detection of microorganisms which are difficult to culture. Samples which do not contain the target sequence (negative) will give minimal fluorescence, for example, detection of Salmonella typhi or other broad-range Salmonella assays to detect all the members. The assays have been designed to differentiate HSV types I and II, BK and JC polyomaviruses, and human herpesvirus 6 types A and B and commonly occurring Bartonella species and M. tuberculosis from nontuberculous Mycobacteria.
Microarray: In this, lots of probes are present on the chip and the sample is labeled and hybridized. The labeled sample is hybridized to the probes and detection of positive signal reveals the presence of that particular target in the sample.
Chapter End Summary
The infectious diseases are responsible for major cause of death and disability throughout the world. They are responsible for a number of diseases either involving any local organ (localized or organ specific) or whole body (systemic infections).
Our immune system is the defense system of our body which protects us from various invading pathogens. The system has two lines of immunity, the innate and adaptive immune responses. Innate immunity is nonspecific immunity and provides first line of defense. This immunity is present since birth.
Adaptive immunity is specific with specificity, diversity, and memory. Adaptive immunity has T and B lymphocytes as its main components which are responsible for cell-mediated and humoral immune responses, respectively. The main effectors of cell-mediated immune responses are T cells and humoral immune responses are antibodies.
The immune system protects us from various infections, loss of any component of immune system results in immunodeficiency (due to genetic defect or acquired during lifetime like AIDS), and failure of self-/non-self-recognition results in autoimmunity.
With the continuous evolution of new diseases and newer causative agents or emergence of mutated pathogens, they are becoming potential challenges for health-care managers. Various diseases of the gastrointestinal tract, skin, nervous system, and respiratory system and sexually transmitted diseases are caused by a number of pathogenic agents.
Infection of one agent or simultaneous infection of multiple agents is the cause and concern for major infections. With the advanced tools and techniques now, it is possible to characterize and detect these agents for therapeutic intervention.
Multiple Choice Questions
- Immune system consists of:
- Cell-mediated immunity and humoral immunity
- Innate and adaptive immunity
- Adaptive immunity
- None of these
- PAMPs are present on:
- Pathogens
- Immune cells
- Body cells of humans
- All of these
- ADCC response is shown by:
- Neutrophil
- Basophil
- Natural killer cell
- Eosinophil
- Th1 response is important in:
- Innate immune responses
- CTL-mediated responses
- Humoral immune responses
- All of the above
- TLR2 is responsible for binding:
- Peptidoglycan
- Double-stranded RNA
- Lipopolysaccharides
- Herpesvirus
- Body temperature or fever is regulated by:
- Thalamus
- Hypothalamus
- Cerebrum
- Midbrain
- Normal temperature of the body is:
- 100–101 °F
- 95–97 °F
- 103–104 °F
- 97.7–99.5 °F
- Pyrexial illness includes all except:
- PUO
- Viral fever
- Bacterial fever
- None of the above
- Syphilis lesion is known as:
- Chancroid
- Boil
- Abscess
- Laceration
- Syphilis is caused by:
- Treponema pallidum
- Treponema folliculus
- Treponema vulgaris
- Virus induced
- Dysentery is caused by all except:
- Salmonella typhi
- Shigella
- E. coli
- Entamoeba gingivitis
- All are skin lesions except:
- Macule
- Papule
- Vesicle
- Glossitis
- All are sexually transmitted diseases except:
- Syphilis
- HIV
- Malaria
- HSV
- All of these are symptoms of leprosy excluding:
- Anesthetic patch
- Thickened nerve
- Loss of sweating
- Itching
- Tuberculosis of lungs is caused by:
- Mycobacterium leprae
- Mycobacterium kansasii
- Mycobacterium tuberculosis
- Mycobacterium bovis
- If the infectious agent is present in the body in latent stage, which technique can detect its presence?
- ELISA
- DNA microarray
- NAAT
- RIA
- Influenza virus is mutating very fast which leads to emergence of new strains; mutations occur in:
- Viral glycoprotein
- Hemagglutinin
- Reverse transcriptase
- Viral coat
- MBL is an important component of:
- Adaptive immunity
- Innate immunity
- Pathogen
- Cell-mediated immunity
Answers
1. (b); 2. (a); 3. (c); 4. (b); 5. (a); 6. (b); 7. (d); 8. (d); 9. (a); 10. (a); 11. (d); 12. (d); 13. (c); 14. (d); 15. (c); 16. (c); 17. (b); 18. (b)
Questions
Q1. What is the role of the immune system in the prevention of infection?
Q2. What are soluble factors involved in immune response?
Q3. What is adaptive immune response?
Q4. Give a brief account of PRRs present in the body.
Q5. Write a short note on chancroid.
Q6. What are common cytokines involved in pyrexial illness?
Q7. Why HIV is most commonly associated with tuberculosis?
Q8. Why tubercular infections occur on the upper lobe of lungs?
Q9. Write a note on sexually transmitted diseases.
Q10. Which region is responsible in poliomyelitis?
References
- 1.Centers for Disease Control and Prevention Sexually transmitted diseases treatment guidelines. MMWR Morb Mortal Wkly Rep. 1993;42:1–102. [Google Scholar]
- 2.Centers for Disease Control and Prevention Summary of notifiable diseases, United States. MMWR Morb Mortal Wkly Rep. 1997;46:3–87. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention Guidelines for treatment of sexually transmitted diseases. MMWR Morb Mortal Wkly Rep. 1998;47:1–111. [Google Scholar]
- 4.Goh BT. Syphilis in adults. Sex Transm Infect. 2005;81:448–452. doi: 10.1136/sti.2005.015875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL (eds) (2008) Harrison’s principles of internal medicine, 17th edn. Mc Graw-Hill Medical publishers, New York
- 6.Kindt TJ, Goldsby RA, Osborne BA. KUBY immunology. 6. New York: Freeman and Company; 2007. [Google Scholar]
- 7.Miller KE, Graves JC. Update on the prevention and treatment of sexually transmitted diseases. Am Fam Physician. 2000;61:379–386. [PubMed] [Google Scholar]


