Abstract
Sick building syndrome (SBS) and building-related illnesses are omnipresent in modern high-rise buildings. The SBS is a complex spectrum of ill health symptoms, such as mucous membrane irritation, asthma, neurotoxic effects, gastrointestinal disturbance, skin dryness, sensitivity to odours that may appear among occupants in office and public buildings, schools and hospitals. Studies on large office buildings from USA, UK, Sweden, Finland, Japan, Germany, Canada, China, India, Netherlands, Malaysia, Taiwan, and Thailand, substantiate the occurrence of SBS phenomena. The accumulated effects of a multitude of factors, such as the indoor environmental quality, building characteristics, building dampness, and activities of occupants attribute to SBS. A building occupant manifests at least one symptom of SBS, the onset of two or more symptoms at least twice, and rapid resolution of symptoms following moving away from the workstation or building may be defined as having SBS. Based on the peer-reviewed documentation, this chapter elaborates the magnitude of building-related health consequences due to measurable environmental causations, and the size of the population affected. The mechanisms and causative factors of SBS and illnesses include, for example, the oxidative stress resulting from indoor pollutants, VOCs, office work-related stressors, humidification, odours associated with moisture and bioaerosol exposure. Related regulatory standards and strategies for management of SBS and other illnesses are elaborated.
Introduction
Outbreaks of building-related illnesses, collectively termed as sick building syndrome (SBS) among building occupants reported in the recent decades, draw remarkable resemblance to early events of epidemic hysteria. Tarantism, the dancing mania of peasant women (animal-like squealing, obscene shouting, laughing, or weeping) during the fifteenth to seventeenth century, St. John’s or St. Vitus’ dances in Northern Europe, the hysterical fits of women due to smells from hemp steeped in water (Ramazzini 1713) , industrial outbreak among workers in a cotton mill in the eighteenth century England ( Gentleman’s Magazine 1787), are historically recorded events. Many other early psychogenic illnesses reported from schools, hospitals, prisons, and in warfare, exemplify the results of various reasons, like prominent social concerns and exposure to physical, biological, or chemical agents (Bartholomew and Wessely 2002; Sirois 2013) .
The SBS manifests as the complex spectrum of ill health symptoms, such as mucous membrane irritation (rhinorrhea, nasal congestion, sore throat, eye irritation), asthma symptoms (chest tightness, wheezing), neurotoxic effects ( a headache, fatigue, irritability), gastrointestinal disturbance, skin dryness, sensitivity to odours. These symptoms may appear among occupants in office buildings, schools, public buildings, hospitals, and recreational facilities. The rapid spread of symptoms often leads to the virtual closure of the facility, and resolution of the illness also takes place within a short time after leaving the facility (Laumbach 2008; Takeda et al. 2009) .
Building-related illnesses have been viewed as ubiquitous in modern high-rise buildings. These are designed to be airtight on energy-saving consideration—windows remain sealed, deprived of natural ventilation and daylighting, and HVAC system re-circulates the air in the building, with the minimal replacement of fresh air. Concerns about human health due to deteriorating indoor environmental quality are steadily increasing with a public outcry among the building occupants and also challenging lawsuits to redress grievances. The term SBS has been in use for some time now and widely recognized, in spite of suggestions for alternative names, such as problem buildings, building-related occupant complaint syndrome, abused building syndrome. Acknowledging that the incidences of SBS symptoms are straightforward, its characterization and linkages to an indoor exposure require more in-depth analysis. An impediment towards this effort is to make the primary distinction as to whether the problem is chemical, biological, physical, or psychogenic. The questions to examine are the mechanism how workplace or environmental processes trigger physical health symptoms, and whether some individuals are more prone to illnesses. Further, it calls for a review on the kind of critical work settings that precipitate illness conditions, and how the work or environmental aspects influence building occupant’s psychophysiological threshold, making oneself hypersensitive even to mild irritants. Priority is placed on exploring organizational interventions to restrict the spread of the syndrome and efficiently manage causes of building-related illnesses.
Several researchers indicate the SBS as a phenomenon that occurs among building occupants, perhaps one out of five building occupants reports symptoms associated with their respective place of work and attributed to the IAQ. The interactions of a multitude of factors, such as the site, climate, building system, construction materials, building dampness, contaminant sources, activities of occupants, affect the quality of indoor air. Typically, maintaining allowable IAQ in office buildings depends on effective ventilation systems in operation. Ineffective or inadequate ventilation systems result in inefficient removal of pollutants from indoor air and display signs of SBS among the occupants.
Questionnaire Survey
Health impact assessment addresses qualitative or quantitative evaluation of the magnitude of health consequences due to measurable environmental causation or metric, and the size of the population affected (Fehr et al. 2012; Mesa-Frias et al. 2014) . Apparent relationships exist between the external stimuli, kinds of human responses and about the type of building environment. Therefore, the discomfort and symptoms of occupants in the building require acknowledging that an exposure scenario exists, and the discomfort and disease have a strong association with psychologic or physiological components. A structured questionnaire (Table 3.1) may be used to ascertain the SBS of the respondents in an office building. The office workers who had at least one symptom of SBS and onset of two or more symptoms at least twice weekly, overnight resolution of symptoms after leaving the workstation or building, and the absence of known medical causes, may be defined as having SBS (Ooi et al. 1998). The prevalence of symptoms among building occupants is linked to personal exposure to the indoor environment. The symptoms may vary during the day, in the course of changes in the concentrations of indoor pollutants. Further, the prevalence of syndrome might differ with the specificity of criteria for the definitive diagnosis of a case. Accordingly, there may be a shift in the frequency distribution of affected workers when the requirements were changed to one symptom, instead of two or more symptoms (Ooi et al. 1998).
Table 3.1.
Questionnaire on SBS (Adapted from Ooi et al. 1998)
| Demographic details of the building occupant | Socio-economic aspects | |||
| Workplace characteristics (office plan) | Work experience; working schedule (including overtime and night work) | |||
| During the past four weeks | ||||
| Health and well-being symptoms | Daily | 2–3 times weekly | Less | |
| Fatigue | ||||
| Headache | ||||
| Drowsiness | ||||
| Dizziness | ||||
| Shortness of breath | ||||
| Nausea/ vomiting | ||||
| Stuffy nose | ||||
| Dry throat | ||||
| Skin dryness/rash | ||||
| Eye irritation | ||||
| Time of occurrence | ||||
| Do the complaints occur? | Morning | Afternoon | No noticeable trend | |
| Does relief occur from complaints? | On leaving workstation | On leaving building | Never | |
| Medical conditions | Yes | On medication (Yes) | Not on medication | No |
| Allergy | ||||
| Sinus | ||||
| Asthma | ||||
| Migraine | ||||
| Others (specify) | ||||
For measuring the concentration of indoor air pollutants, one may adopt area sampling by placing an environmental monitoring device in general building locations and placing a personal sampling device close to the nose of the person that better represents the inhaled dose of individuals. Chapter 10.1007/978-981-13-2577-9_10 is dedicated to indoor environmental quality (IEQ) assessment, concerning primary exposures. The exposure assessment based on area sampling and recording of symptoms of occupants from the vicinity of the samplers may indicate some dose–response relationships between exposures and symptoms. However, there are limitations to extrapolate the relation to other buildings, since the problem situations in buildings are unlikely to be similar.
SBS Epidemiology
Epidemiological evidence is abundant of the occurrence of SBS in real-world settings all over the world. Within the limited scope, and the author’s comprehension on the subject, only a selected number of cross-sectional studies that have been reported in the recent years are briefly summarized in Table 3.2. Different research groups emphasized on the association of prevalence of SBS symptoms among the office workers with the organic floor dust concentration, the floor covering of the workplaces, the age of the building, and the kind of ventilation system in operation. The size of the office and the number of occupants in the office were critical, presumably because of likely rise of pollutants during the day. The shelf factor was identified as a risk factor for mucosal irritation, and the fleece factor, such as fleecy surfaces, paper, and cardboard was recognized for general symptoms in the office buildings (Skov et al. 1990; Mølhave 2011) . Despite that carpets give a cozy atmosphere and an aesthetic acoustic environment in a building, carpet fibres and accumulated dust, especially the organic part of the dust, have been found to be associated with SBS, namely mucosal irritation. Further details of work and building-related respiratory illnesses are elaborated elsewhere in the chapter.
Table 3.2.
Cross-sectional studies on SBS
| References | Sample population | Questionnaire survey/objective measurement | Results |
|---|---|---|---|
| Burge et al. (1987) | 4373 office workers in 42 office buildings in the UK | SBS | Workers had more SBS symptoms in buildings that were humidified or air-conditioned. Complaint: lethargy (57%), nasal congestion (47%), dry throat (46%), headache (46%). Symptoms (mean building sickness index) were more in women than in men and were independently more frequent in clerical workers, secretaries than in technical and professional employees and managers |
| Skov et al. (1989) | 4369 workers in 14 town halls and affiliated buildings in Denmark | SBS, ambient climate, CO2, formaldehyde, VOCs, airborne dust, fibres, lighting, micro-organism, static electricity, noise, housekeeping; analysis of building material, materials used in office equipment | Employees in mechanically ventilated buildings had highest rates of mucous membrane irritation, headache, fatigue; clerical and social workers had more complaints than those of professional workers. Increased incidence of mucous irritation from exposure to photograph printing, carbonless paper, and VDT. Females had a higher prevalence of mucosal irritation and general symptoms than males |
| Richards et al. (1993) | 2598 combat troops stationed in Saudi Arabia during the Gulf War | Investigation of respiratory illness | The type of housing (air-conditioned buildings, non-air-conditioned buildings, open warehouses, and tents) influenced the prevalence of symptoms. Ever vs. never housed in an air-conditioned building was associated with ~37% greater prevalence of a sore throat, and 19% greater prevalence of a cough |
| Ooi et al. (1998) | 2856 office workers in 56 public and private sector buildings in Singapore | A self-administered questionnaire introduced on SBS and perception of the physical and psychosocial environment, measurement of ambient climate, respirable dust, chemicals, bioaerosol, and other variables | Health complaints included neurotoxic reactions (fatigue, headache, drowsiness, dizziness), eye irritation, irritation of the nose, throat, and airway (stuffy nose, dry throat, shortness of breath), skin irritation (dryness, rash), and other complaints (nausea, vomiting). Associations of the physical environment and work-related stress with the history of health ailments among the building occupants. SBS symptoms became more apparent over the work shift and resolved upon leaving the premises |
| Milton et al. (2000) | 3720 workers from 40 buildings with a total of 110 independently-ventilated floors | Recorded short-term absence from work and incidences of acute respiratory illnesses. | Based on analysis of ventilation system design, occupancy, and end-of-day CO2 measurements, the ventilation rates of buildings were classified as moderate (~12 L/sec) or high ventilation (~24 L/sec per occupant). The absence rate was 35% lower in the high-ventilation buildings |
| Brasche et al. (2001) | 1464 (60% females) in 14 office buildings from the German ProKlimA-Project | SBS survey and ergonomics data on working conditions and job characteristics | Gender-specific SBS prevalence rates differ for the whole sample; complaints were significantly higher in females. Independent of personal, work-related and building factors, ~36% of females with the most favourable job characteristic suffered SBS (male: ~19%), 53% of females with the most unfavourable job characteristic suffered SBS (males: ~33%) |
| Reijula and Sundman-Digert (2004) | 11154 office workers from 122 workplaces in Finland during the period of 1996–99 | SBS |
Most common indoor problems as reported by respondents: dry air (35%), stuffy air (34%), dust or dirt in the indoor environment (25%), and draught (22%) Common work-related symptoms: irritated, stuffy, or running nose (20%), itching, burning, or eye irritation (17%), and fatigue (16%) Women reported symptoms more often than men. Allergic persons and smokers reported indoor air problems and work-related symptoms more often than non-allergic persons and non-smokers |
| Apte and Erdmann (2003) | US EPA Building Assessment Survey and Evaluation (BASE) study of 100 large office buildings during the period of 1994 to 1998 | Environmental parameters (e.g., CO2, CO, VOCs, air temperature, and RH), including data of jobs, perceptions about indoor environment, health, and well-being. SBS related to mucous membrane (irritation of eyes, stuffy nose/sinus, and sore throat), lower respiratory (chest tightness, shortness of breath, cough or wheezing), fatigue, headache, and dry or itchy skin | The analysis covered 36 VOC compounds (41 buildings), formaldehyde (100 buildings) and acetaldehyde (86 buildings), as analysed by gas chromatography–mass spectrometry (GC-MS). Multivariate logistic regression analyses revealed dose-dependent associations for dry eyes, sore throat, nose/sinus congestion, and wheeze symptoms with the delta change in indoor and outdoor CO2 concentrations. VOC sources had a direct association with mucous membrane and lower respiratory irritation |
| Marmot et al. (2006) | 4052 male and female participants from 44 office buildings in longitudinal Whitehall II SBS study in the UK | Self-reported ten SBS symptoms (i.e., headache, cough, dry eyes, blocked/runny nose, tired for no reason, rashes/itches, cold/flu, dry throat, sore throat, and wheeziness) | 25% of men and 15% of women reported no symptoms, whereas 14% of men and 19% of women reported five or more symptoms. There was positive (non‐significant) relationship between the aspects of the local physical environment (airborne bacteria, inhalable dust, air temperature, RH) and SBS symptoms prevalence. More significant effects were found with features of the psychosocial work environment, such as high job demands and low support |
| Karjalainen (2007) | 3094 (50% females) in the home environment; 1000 (52% females) in an office environment | Telephonic interview; thermal satisfaction | In general, men reported higher thermal satisfaction. The relative percentage of people voted to uncomfortably hot or cold votes was consistently higher in females |
| Syazwan et al. (2009) | 176 office workers in two buildings (new and old) at Kuala Lumpur | SBS and IAQ | These buildings had the same centralized air-conditioning unit, and the office was dependent only on the general ventilation. Nearly ~69% of office workers from old building recorded SBS, in comparison with 36% of office workers in the new building |
| Aries et al. (2010) | 333 occupants (42% females) from 10 office buildings in the Netherlands | SBS, office layout, lighting, physical and psychological discomfort | The significant relationship observed between gender and office lighting, including desk lighting, physical and psychological discomfort, such as concentration problem, dullness, headache, bad vision, and dry throat/eyes |
| Zalejska-Jonsson and Wilhelmsson (2013) | 5660 (53% female) in residential buildings in Sweden | Questionnaire; thermal comfort, IAQ, acoustics | Thermal comfort and overall IEQ satisfaction are greater among female occupants. Problems associated with IEQ (stuffy air, draught, and dust) were more among females than males |
The US EPA Building Assessment Survey and Evaluation ( BASE) study (Apte and Erdmann 2003) is a landmark study covering 100 large office buildings and extensive measurements of both SBS symptoms and environmental monitoring. The occupant must have reported an occurrence of one SBS symptom, at least 1–3 days per week during the month, and resolution of the symptoms when the occupant moves away from work. Analysis indicated dose-dependent associations in many of SBS symptoms with the delta change in indoor and outdoor CO2 concentrations. VOC sources had a direct association with mucous membrane and lower respiratory irritation.
The Whitehall II SBS study is a longitudinal health survey of UK office-based civil servants, commenced with 10308 males and females, exploring the significance of the physical and psychosocial work environment to the occurrence of SBS. Analysing ten SBS symptoms among 4052 participants from 44 buildings, Marmot et al. (2006) did not observe the significant relation between most aspects of the physical work environment and SBS symptom prevalence. The features of the psychosocial work environment, such as high job demands and low support, appear to be more determining in explaining differences in the prevalence of SBS symptoms, than those attributed to local aspects of the physical environment of office buildings.
Jaakkola et al. (2007) examined the occurrence of SBS related symptoms, chronic respiratory symptoms, and respiratory infections, using a questionnaire survey of 342 office workers in Finland. A case definition of SBS was taken as symptoms of nasal (dryness or itching of nose, blocked or a runny nose, or sneezing), eye (dryness and irritation, watering, or redness), throat (dry irritative cough, sore throat, or hoarseness), skin (dryness, irritation, redness patches, itching, sore skin, or urticaria), and non-specific symptoms (headache and fatigue), which might have occurred during the past year, at least 1–3 days per week and mainly during workdays or work shifts. There were significant health effects due to office work exposures, adjusting confounders such as psychosocial factors at work. Exposures to paper dust and carbonless paper that contains solvents and colour-forming chemicals increase the risk of a headache and fatigue, chronic breathlessness, and chronic bronchitis (a chronic cough and phlegm production). Exposure to carbonless paper through its touching can cause sinus infections, middle ear infections, and increased risk of eye symptoms and diarrhoea.
Gupta et al. (2007) undertook a questionnaire-based investigation on the prevalence of the SBS at a multi-story centrally air-conditioned Airport Authority of India building in New Delhi. Qualitative analysis included the relationships between SBS score, CO2 and other parameters related to building and work environment. Quantitative analysis included monitoring of pollutants, namely NOx, SO2, CO, and suspended particulate matter. Despite that the concentrations of pollutants complied with IAQ standards were generally within limits, the prevalence of SBS ( a headache—51%, lethargy—50%, and dryness in body mucous—33%) was higher in the third floor as compared to other floors and the control tower. The third floor and the control tower of the airport were affected by infiltration, mainly from entrance doors.
Hengpraprom et al. (2010) showed the influence of airborne fungi on allergic rhinitis among office occupants (49%) of a high-rise building in Bangkok. Allergic rhinitis was defined as having the symptoms of nasal congestion, an itchy nose, sneezing, and running nose without a cold in the past 12 months (Teeratakulpisarn et al. 2000) . Work-related allergic rhinitis was defined as (a) having the above symptoms with a cold at least twice in the past month; (b) expressing the manifestation at work or seeing it worsen at work; and (c) the frequency of manifestation occurred at least 1–3 days per week. Indoor humidity was strongly correlated with airborne fungi concentrations. However, the fungal concentration was not associated with work-related allergic rhinitis. Asthma and asthma-like symptoms among office workers, respiratory sensitization with exposure to hot or cold weather, the presence of visible mould, and carpeting resulted in a positive association with allergic rhinitis.
Syazwan et al. (2009) compared the data of SBS and IAQ of 176 office workers in old and new buildings in Kuala Lumpur City. The investigators suggested that improvement in ventilation effectiveness and increase in ventilation rates per person may reflect on the reduction of indoor pollutants and also reduction in the prevalence of SBS in buildings. Norhidayah et al. (2013) investigated associations between IAQ parameters and SBS in three buildings in Malaysia. The prevalence of SBS symptoms, having 1 to 3 symptoms per week, was similar in the buildings. The CO concentration and fungal counts were not significantly different between the buildings. However, the observed CO2 concentration and climatic factors suggest that the predictors of SBS might be ventilation and accumulation of contaminants within the indoor environment.
Many abiotic agents from building materials and interiors like wall coverings, synthetic paints (a&b—pinene), thinners, glue, floor coatings of linoleum and PVC, solvents, such as formaldehyde, hairspray, perfume, photocopiers and printers, disinfectants and detergents (members of linear alkylbenzene sulphonates), and soap as cleaning agent (sodium or potassium salts mixed with fatty acids) add to air pollution to cause SBS symptoms (Guo 2011; McDonnell and Burke 2011) . Therefore, it may be reiterated from reviewing voluminous literature that no one single cause explains most SBS complaints, but instead assumes that multiple factors interact to manifest occupant complaints. The symptoms typically grow worse during the workday and disappear or diminish after the person leaves the building.
Gender Difference in SBS
Women appeared to show a higher prevalence of SBS symptoms as compared to men in the same buildings. Individual characteristics, such as education level, working conditions, job characteristics, and other psychosocial factors, can also influence SBS prevalence positively or negatively in men and women. The technical factors associated with the increased prevalence of SBS are the building factors, such as the age of the building, indoor dampness, presence of some photocopiers and humidifiers in the building (Sundell 1996) . Zweers et al. (1992) examined 7043 occupants (65% female) in 61 office buildings in the Netherlands and noted that occurrence of SBS symptoms was related to air conditioning and humidification in buildings. Females had more prevalence of SBS (e.g., skin/eye/nasal symptoms) and complaints of indoor climate, such as temperature, air quality, lighting, and noise. Carrying out of study on 4943 office workers (53% female) in Sweden, Stenberg and Wall (1995) observed a higher prevalence of SBS among females (OR = 3.4) than males.
Questionnaire survey and ergonomic data from the German ProKlimA-Project (Brasche et al. 2001) also substantiated a significantly higher prevalence of SBS symptoms among women, as compared to men folks, both under the most favourable and most unfavourable job characteristics. Undoubtedly, the physical and psychological disposition, on the one hand, and work- and job-related factors, on the other hand, are risk factors on the perception of the indoor environment and the pathogenesis of complaints. With a sample size of 368 office workers (~77% females) from 6 office buildings in the USA, Reynolds et al. (2001) observed that the psychosocial factors were positively correlated with the incidences of SBS in females. However, the environmental factors were correlated with symptoms in males. By examining 877 occupants (50% female) in 12 office buildings in Quebec, Canada, Donnini et al. (1997) observed no significant differences in thermal neutrality between males (23.5 °C) and females (23.8 °C). Females expressed significantly higher thermal dissatisfaction (63% female vs. 37% male). Nakano et al. (2002) examined 406 Japanese office workers (37% females) and noted a significant difference in thermal neutrality, i.e., females (25.1 °C) and males (22.9 °C), while females reported a higher frequency of SBS symptoms, as compared to the male group. In a study on 935 office occupants (48% female), in 22 office buildings in Australia, Cena and de Dear (1999) noted the votes of thermal unacceptability, and females complained of significantly higher thermal dissatisfaction than those of males. Choi et al. (2010) had a similar observation by studying 402 office workers (~53% females) from 20 office buildings in the USA. Runeson et al. (2003) investigated the prevalence and change of SBS symptoms in buildings with suspected indoor air problems about Antonovsky’s sense of coherence (SOC), a psychological measure of life attitude. The study was conducted on a cohort of 194 workers from 19 Swedish buildings with indoor environmental problems between 1988 and 1998. Information on 16 SBS symptoms was gathered, as well as the SOC measure was administered in a postal follow-up. After adjusting for age, gender, history of atopy, and ETS, Runeson et al. (2003) noted that SBS was more common in women, younger ones, and those with a history of atopy. A low SOC was related to a higher prevalence of ocular, nasal, and throat symptoms, tiredness, and headache. Also, subjects with a low SOC developed more symptoms during the follow-up period.
Saijo et al. (2009) undertook postal self-administered questionnaire survey to 1,582 dwellings from 40 municipal, and 24 prefectural apartment buildings in the city of Asahikawa, Japan, and 480 questionnaires were finally analysed. From the questionnaire about moisture condensation and visible mould on window panes, walls, closets, bathrooms, the perception of mouldy odour, and water leakages, a building dampness index was defined as the sum of positive dampness indicators. SBS symptoms recorded for the preceding 3-month period were—fatigue, feeling heavy-headed, headache, nausea/ dizziness, difficulty in concentrating, irritation of the eyes, running nose, dry throat, cough, dry or flushed facial skin, itching of the scalp, ears, and hands. The symptoms were significantly higher among females than males. The building dampness index was also significantly related to all SBS symptoms, as also noted by Engvall et al. (2001) in the study covering 609 multi-family buildings (14,235 dwellings) in Stockholm. Saijo et al. (2009) noted allergic diseases as risk factors for SBS development, and therefore, the history of allergic diseases was taken as a confounder for SBS symptom analysis. The US NIOSH study in 80 office buildings also found a positive association between moisture and debris in the ventilation systems and lower respiratory tract symptoms (Mendell et al. 2003 ).
Kim et al. (2013) undertook a comprehensive literature survey, based on North American post-occupancy evaluation (POE) database (N = 38,257). The survey indicated that the satisfaction levels of female occupants were significantly lower than males on all fifteen IEQ factors (such as thermal comfort, air quality, lighting, acoustics, office layout, furnishings, cleanliness, and maintenance). The results were consistent, even after controlling the potential confounders, such as age and work characteristics.
Chronic Fatigue Syndrome
Chronic fatigue syndrome (CFS) manifests as a clinical entity characterized by prolonged severe and disabling fatigue (Fukuda et al. 1994). The syndrome usually occurs sporadically, but occasionally may appear as epidemics. Typically, the syndrome follows a cyclical course, alternating between periods of illness and relatively good health. The onset of CFS has been related to a variety of psychological, environmental, and behavioral factors (Pizzigallo et al. 1999), and exposure to pesticides, organophosphates, solvents, and other chemicals (Bell et al. 1998). In tropical areas, many CFS-like cases follow an episode of gastroenteritis due to food toxins from ciguatoxic fish (Pearn 1995) . Ciguatera consists of a food-chain disease that starts with a reef-dwelling dinoflagellate, Gambierdiscus toxicus (Gillespie et al. 1986), which is heat-stable. Individuals can be poisoned from eating fresh or frozen fish, or fish products. Symptomatology of some outbreaks of SBS resembles CFS, associating with building characteristics, such as old buildings, inadequate ventilation, non-functioning windows, and inefficient HVAC system (Chester and Levine 1997) . Thousands of Gulf War veterans, even 5 years after the Operation Desert Storm in 1991, remained ill with vague symptoms that resemble CFS. These veterans were exposed to an array of hazards, such as extremes of climate, dust, and smoke from oil well fires, petroleum fuels and products, depleted uranium (used in artillery shells), chemical warfare agents, pesticides, infectious diseases, and pervasive psychological and physical stress. The veterans were administered with pyridostigmine bromide (as pre-treatment for potential poison gas exposure), anthrax and botulinum toxoid vaccines (Landrigan 1997). Haley et al. (1997) identified six different syndromes among the war veterans, namely:
Syndrome 1 (impaired cognition)—reported by veterans wearing flea collars during the war than those who never wore them;
Syndrome 2 (confusion-ataxia)—reported by veterans involved in chemical exposure (e.g., pyridostigmine bromide);
Syndrome 3 (arthro-myo-neuropathy)—exposure to insecticides containing 75% DEET (N,N-diethyl-m-toluamide);
Syndrome 4 (phobia-apraxia);
Syndrome 5 (fever-adenopathy); and
Syndrome 6 (weakness-incontinence).
The case definition of CFS (Fukuda et al. 1994)
-
A.Persistent or recurrent fatigue (lasting >6 months)
- Recent and or well-defined onset;
- Not secondary to excessive physical activity;
- Not resolved by rest; and
- Inducing reduction of previous levels of physical and mental activities.
-
B.Presence of more than four symptoms (for >6 months), not previous to fatigue onset:
- Impaired memory or concentration;
- A sore throat;
- Tender cervical or axillary lymph nodes;
- Muscle pain;
- Multi-joint pain;
- New headaches;
- Unrefreshing sleep; and
- Post-exertion malaise.
If the combined number of elements of A and B present exceeds 4, a case of CFS would be considered.
Environmental Stressors Associated with SBS
The multifactorial aetiology of SBS in office buildings is yet to understand clearly. Evidence favours that the accumulated effects of building characteristics and IEQ manifest in health outcomes, including SBS symptoms, allergy, asthma, and other respiratory illnesses. The health effects, in turn, cause adverse impacts on job satisfaction, work performance, productivity, and healthcare costs (Fisk 2000). The potential environmental stressors that might be responsible for causing SBS symptoms are briefly mentioned herewith. Further details of IAQ associated with different pollutants in the indoor environment are described in Chap. 10.1007/978-981-13-2577-9_10.
Indoor air pollutants include oxides of nitrogen (NOx), CO, CO2, VOCs, and particulates, which are emitted from building materials, office equipment, and as combustion by-products. The intrusion of pollutants from the outdoor air through leakages and ventilation systems is a critical component. The build-up of CO2 may be considered as a surrogate for many occupant-generated pollutants in the indoor built environment. Review of studies of SBS symptoms in office buildings indicated increased indoor CO2 levels were associated with an increase in the prevalence of one or more SBS symptoms (Seppänen et al. 1999 ). Findings from more mechanically ventilated and air-conditioned buildings indicated a significant association between an increase in CO2 and SBS symptoms, and total symptom scores. As mentioned earlier, the BASE dataset (1994–98) yielded significant dose–response relationships between the delta change in indoor and outdoor CO2 concentrations, and the SBS symptoms, such as a sore throat, nose/sinus irritation, mucous membrane symptoms, and tight chest (Apte et al. 2000).
Headaches represent the single most common symptom in almost all indoor environmental studies (Schwartz et al. 1998). The current knowledge highlights different forms and mechanisms of a headache, such as a migraine, or a tension-type headache, or any plausible exposure to chemical toxicants, e.g., CO or pesticide poisoning. Whereas, many of the events do not provide a precise characterization of the office environment (Schneider et al. 1999), such headaches are no less significant given the productivity implications, and the potential for active intervention in the office environment.
Volatile organic compounds (VOCs)— VOCs are ubiquitous indoors, due to human activities, building product emissions, including floorings, linoleum, carpets, paints, surface coatings and furniture, and infiltration of the outdoor air. For new or renovated buildings, VOCs are primarily emitted from building products. Secondary emissions of VOCs result from ageing of building products, by chemical decomposition (e.g., moisture build-up or inadequate maintenance) or physical damage due to heat and UV light (Wolkoff 1999) . Furniture coatings release nearly 150 VOCs (aliphatic and aromatic aldehydes, aromatic hydrocarbons, ketones, esters, and glycols) (Salthammer 1997) . Office equipment and supplies, such as laser printing toners, emit VOCs, ozone, formaldehyde, resin, and other particles. Use of perfumes indoors may release VOCs. Indoor fungi are also a source for the production of VOCs. Many VOCs are known toxic compound, with potential for carcinogenicity, mutagenicity, or teratogenicity. Documented evidence strongly affirms that occurrence of SBS follows predictable dose–response relationships with increasing concentrations of mixtures of VOCs. The VOCs, such as O-xylene, styrene, d-limonene and other terpene compounds may readily react with ozone and NOx entrained from outdoors and produce highly reactive compounds, including aldehydes and ultrafine particles, leading to sensory irritant symptoms (Sarwar et al. 2002; Sundell 2004) . These effects have been observed in case of carpet emissions, latex paint off-gassing, and other office pollutants.
It has been viewed that SBS may be related to the lost VOCs, i.e., the difference in the concentration of VOCs entering the room to that leaving the room. In California Healthy Buildings Study, Brinke et al. (1998) adopted an approach in developing VOC metrics and identified relationships between SBS symptoms and clusters of VOCs by its possible emission sources. The principal component analysis (PCA) allowed to cluster VOCs into a reduced set of principal component (PC) vectors and further estimated the association between SBS symptoms and the VOC exposure metrics, using logistic regression analysis. A similar approach was taken by Apte and Daisey (1999) in exploring the causal associations between SBS and environmental stressors, using a subset of data from 28 office buildings of the US EPA BASE study. Four source-based PC vectors were derived that identify sources as photocopiers, automotive emissions, ETS, and latex paints. Regression analyses indicated significant associations between mucous membrane-related symptoms and the photocopier vector, after adjustment for age, gender, smoking status, the presence of carpeting, and thermal exposure. Sore throat symptoms were associated with the paint vector. Analysis of dataset of all 100 BASE buildings revealed 36 VOCs, formaldehyde and acetaldehyde corresponded to 41 buildings, whereas 19 VOCs were available in all buildings. The PCA yielded ten PCs identified as the VOC sources (Apte and Erdmann 2003). Seven components referred to as furniture coatings (PC1), paint (PC2), construction materials (PC3), printing materials and processes (PC4), carpet and undercarpet (PC5), parking garage (PC6), and cleaning products (PC7) met the criterion of having eigenvectors ≥1.0.
Oxidative Stress and SBS—Several studies suggest that a shallow concentration of VOCs in indoor environment may cause SBS symptoms, but how such symptoms generate disability at such low levels remains unexplained. Little is known about the likely oxidative stress that can attribute to the occurrence of SBS due to exposure risks of air pollutants or other factors of the environment. Reactive oxygen species (ROS) are components found in many of the air pollutants and can cause oxidative damage to lipids, proteins, and nucleic acids. Urinary 8-hydroxydeoxyguanosine (8- OHdG) is a known biological marker of oxidative stress on DNA. Accumulation of ETS, VOCs, formaldehyde in the building due to insufficient ventilation can result in the rise of urinary 8-OHdG levels among occupants (Calderon-Garciduenas et al. 1999). Lu et al. (2007) gathered data from self-reported questionnaires and analysis of on-site air pollutants and urinary 8-OHdG of 389 employees in 87 government offices of eight high-rise buildings in Taipei city. The urinary 8-OHdG was significantly associated with VOCs and CO2 levels in offices, and the 8-OHdG level were significantly higher among the employees with SBS symptoms than in those without such complaints. A positive dose–response effect between 8-OHdG levels and the number of symptoms was suggestive that the urinary 8-OHdG as a viable non-invasive marker can be taken as a predictor for SBS.
Office exposures and work stress—Office work-related exposure to paper dust emanated from carbonless copy paper and fumes from photocopiers and printers are health concerns, including respiratory illness among office occupants. Observations of Jaakkola et al. (2007) substantiated that the exposure to paper dust and carbonless papers carries potential risks of chronic respiratory symptoms, respiratory infections, and other health concerns in an office environment.
The stress of work, including extended hours of work, reflects as different work stressors and consequent health impacts among occupants in modern office buildings. There are multiple aspects of work, including physiological, motivation, technical, psychosocial, environmental, perceptual as well as organizational that attribute to work stress. As mentioned earlier, outbreaks of psychogenic illness (SBS) are perhaps a symptom of underlying stress at work and workplace (Selvamurthy and Ray 1996). Mizoue et al. (2001) carried out a cross-sectional survey of 1281 municipal employees from different buildings in a Japanese city. Findings indicated that both ETS exposure and overtime work contributed to the development of SBS. Working overtime for 30 or more hours per month was also associated with SBS symptoms, but the occurrence of SBS reduced by 1/5th after adjustment for variables associated with overtime work and about an-half after further adjustment for perceived work overload.
Runeson et al. (2006) undertook a postal questionnaire survey as regard to SBS on a sample of 1000 subjects (20–65 years of age), including the three-dimensional model of demand–control–support, regarding social support in actual work situations. Results indicated that males and females perceived psychosocial work conditions differently and reacted differently to job stressors. That is, the psychosocial work environment was as important as gender and atopy as a predictor of SBS symptoms.
Nag and Nag (2004) examined the work stresses of women VDT-cum-telephone operators in selected office buildings (telephone exchanges) and observed that the behavioural response to the work stressors, and health and well-being dimensions did vary with the work schedules. The PCA analysis of the ergonomics checkpoints yielded five aspects of work, as organizational (PC1―describing job design needs, workplace interventions, and constraints of VDT workstations), environmental (PC2―covering illumination-, climate-, and noise-related hazards), mechanistic (PC3―referring to job specialization, pace of work, information handling), perceptual and motor (PC4―describing visual and auditory displays and controls), and motivational (PC5―referring to personal job characteristics and core dimensions). The loading of the work stressors explained in PC1 to PC3 appeared autonomous, irrespective of the shift schedules at which the women were engaged. The operators in the rotating shift had higher sensitivity to the stressors related to PC4. The day workers responded greater to the stressors related to the core job dimensions that reflect growth needs (PC5). The sleep disturbance, flexibility to sleeping habits, and personality dimension (neuroticism) were negatively correlated with PC1. The digestive problems, social and domestic disruption, and languidity dimensions were positively correlated to PC4 and PC5. The operators in rotating shift had increased demand in the perceptual and motor, and the motivational aspects of work, and thus causing greater negative influence on physical health symptoms, and social and domestic disruption. The job design interventions tailoring to delay the morning shift and adjust the shift length based on the work and climatic load (that is, reduce work hours in the evening shift to avoid peak workload, and extend hours of day work during the hot summer months) might alleviate work stress and enhance health and well-being. Manifestations of work-related stress call for organizational analysis and job design interventions in structuring the workplace.
Thermal Discomfort—Exceedance beyond the thermal comfort range is associated with increased symptoms, such as a headache, fatigue, and mucosal irritation. Besides the relative effectiveness of ventilation systems, uses of increasing numbers of electronic devices in the offices add to the heat loads in buildings. In real-life work environment, a significant proportion of the population remains in uncomfortable situations and shows thermal discomfort. Clothing habits in different seasons may also contribute to the causes of thermal discomfort in a hotter environment.
Humidification—A sensation of air dryness and irritative symptoms from eyes, skin, and upper airways are common factors in the SBS (Stenberg et al. 1993) . By examining 104 employees from four geriatric hospital units in southern Sweden, Nordstrom et al. (1994) evaluated the effect of steam air humidification on SBS and perceived air quality during the heating season. Air humidification was raised to 40–45% RH in two units during a four-month period, whereas the other two units were maintained at 25–35% RH. After four months of air humidification during the heating season, 24% of the employees reported a weekly sensation of dryness in humidified units, compared with 73% in controls, indicating that air humidification during the heating season in colder climates can decrease symptoms of SBS and perception of dry air. In a tropical environment, RH remains at a much higher level even in an indoor office environment; therefore, incidences of SBS in such situations may be attributed to factors other than air dryness or humidification.
Odours— Odours associated with moisture and bioaerosol exposure are familiar in buildings and best considered in the context of disease with physiological indicators. The odour characteristics are the basis to investigate the possible adverse effects of moulds on human health, in what is often referred to as SBS. From mouldy buildings, the fungal VOCs (such as 1-octen-3-ol and 3-octanone) can produce a range of musty odour (Morey et al. 1997) , as listed (Table 3.3).
Table 3.3.
Odours in mouldy buildings due to fungal VOCs
| 1-Octen-3-ol | Semiochemical; earthy, mushroomy odour |
| 1-Butanol-3-, methyl-, acetate | Anti-fungal; banana odour |
| Sabinene | Unknown; peppery odour |
| 6-Pentyl-a-pyrone | Antibiotic; coconut odour |
| b-Caryophyllene | Plant-growth-promoting; woody-spicy odour |
| Isobutyric acid, 2-heptanone | Anti-fungal; cheese-like odour |
| Benzyl aldehyde | Anti-microbial; almond odour |
| 1,8-Cineole | Anti-fungal; camphor-like odour |
| 2-Methyl-1-propanol | Fungivore attractant; mild alcohol odour |
| 3-Methyl-butanol | Unknown; component of truffle odour |
Odour recognition thresholds are usually several orders of magnitude below the irritant thresholds (Cometto-Muniz and Cain 1996) . Fanger (1988) proposed an unit of pollution, olf (for olfactory) for arbitrarily defining the emission rate of air pollutants from a standard person (white male, 18–30 years of age, showering 0.7 time/day, wear no perfumes, and energy expenditure equivalent of one Met for person sitting at rest). The number of olfs is indicated on the initial perception of the odour, referring to discomfort from irritation and annoyance from odour, and overall acceptability. This method was deployed in a project assessing air quality in 20 offices/assembly halls in Copenhagen, and 54 external judges adjudged the air quality in unoccupied and occupied, and with or without ventilating systems in buildings. About 42% of the perceived defects in air quality was due to ventilation systems, 38% was due to combined occupant activities and occupants themselves, and 20% due to building materials. The stated method has limitations of efficacy since the raters assess the pollution level in a site within minutes of entering the site. The majority of the occupants may not be able to rate odours consistently, and also the odour annoyance is generally perceived most severe early on first exposure and recedes over time.
Fungi in Buildings and Health Impacts
The building professionals may be amazed at recognizing how the proliferation of fungi in buildings damages the building materials and affects the health of occupants, and more importantly to the causation of SBS and building-associated illness. Inadequacy in the ventilation system, moisture controls, and dirt management thrive microbial proliferation in the HVAC systems and office carpeting. Water incursion into the building envelope is a common cause of moisture build-up and fungal growth. There could be visible mould growth on surfaces, the wall behind wallpaper or under the floor covering, suspended ceiling panels, localized damp areas between a wall and a large item of furniture, and in cavity wall spaces (Lugauskas and Krikstaponis 2004) . Through the routes of inhalation or ingestion, propagules of fungi and bacteria may elicit symptoms of illness, like bronchial irritation and allergy (Britton 2003; Beezhold et al. 2008).
Broadly, bioaerosol contains fungal and bacterial cells and cellular fragments, and by-products of microbial metabolism build-up in the buildings. Particles that range in size from 1 to 5 µm remain suspended in the air, whereas larger particles are deposited on the surfaces (Martinez et al. 2004; Horner et al. 2004). It is not within the present scope to elaborate on the classification of fungi, which are grouped by phylum (division), class, order, family, genus, and species, in the order. Khan and Karuppayil (2012) indicated that ~600 species of fungi are in contact with humans and ~50 of them are frequently described in epidemiologic studies on indoor environments. In the present context, several fungal species have been referred to by the researchers about an infestation in building materials and contamination of the indoor environment. Some of the species are listed in Table 3.4.
Table 3.4.
Fungal species from phylum: Ascomycota
| Class | Order | Family | Genus | Species |
|---|---|---|---|---|
| Ascomycetes | Incertae sedis | Incertae sedis | Hymenula | Cephalosporium gramineum H. cerealis |
| Dothideomycetes | Pleosporales | Pleosporaceae | Alternaria | A. alternata |
| Dothideales | Aureobasidiaceae | Aureobasidium | A. pullulans | |
| Capnodiales | Davidiellaceae | Cladosporium | C. herbarum | |
| Pleosporales | Pleosporaceae | Ulocladium | Ulocladium | |
| Eurotiomycetes | Eurotiales | Trichocomaceae | Aspergillus | A. niger |
| A. Versicolor | ||||
| Aspergillus | ||||
| Paecilomyces | P. variotii | |||
| Penicillium | P. brevicompactum | |||
| P. chrysogenum | ||||
| P. expansum | ||||
| Sordariomycetes | Hypocreales | Nectriaceae | Fusarium | Fusarium |
| Gibberella | G. fujikuroi | |||
| Incertae sedis | Myrothecium | M. roridum | ||
| Stachybotryaceae | Stachybotrys | S. chartarum | ||
| Stachybotrys | ||||
| Hypocreaceae | Trichoderma | T. harzianum | ||
| Trichoderma | ||||
| Acremonium | Acremonium alternatum |
Wood, wooden building materials, and kiln dried wood surfaces are vulnerable to fungal attack, with infestation by Cladosporium and Penicillium (Penicillium brevicompactum and Penicillium expansum) (Sailer et al. 2010). Acylated wooden furniture, plywood, and polyurethanes used in wood composites for insulation are found to be susceptible to infestation by Aspergillus, Trichoderma harzianum, Paecilomyces variotii, and Penicillium species (Yazicioglu et al. 2004; Doherty et al. 2011). Prefabricated gypsum board that is used as inner wall materials in buildings favours the growth of Stachybotrys chartarum.
Sterflinger et al. (2013) examined five different indoor insulation materials, i.e., bloated perlite plaster, bloated perlite board, loam and reed, soft wooden board, and sprayed cellulose, for their biosusceptibility. A. Versicolor, Alternaria, Cladosporium, and Penicillium species grow in fibreglass insulation and ceiling tiles (Erkara et al. 2008). Galvanized steel accumulated with dust or lubricant oil residues allows the growth of fungi (Rene et al. 2010; Yau and Ng 2011) . Dampness can cause chemical degradation of polyvinyl chloride (PVC) floor coverings, including formation and emission of 2-ethyl-1-hexanol, 1-butanol (Tuomainen et al. 2004) . Acrylic painted surfaces are attacked by Alternaria, Cladosporium, and Aspergillus (Shirakawa et al. 2011), and also Aureobasidium pullulans can deteriorate the paints (Lugauskas et al. 2003) .
Moisture damage of building frames was characterized by Meklin et al. (2003), studying 17 wooden and 15 concrete or brick school buildings. Aspergillus versicolor, Stachybotrys, and Acremonium were detected in samples from moisture-damaged buildings. Observations indicate that moisture damage of the building did not alter the fungal concentrations in wooden school buildings, whereas, in concrete schools, the effect of moisture damage was seen with higher fungal concentrations. The presence of Oidiodendron and elevated concentrations of Cladosporium and actinobacteria were associated with moisture damage in concrete schools.
Most fungi are mesophilic, and the optimum temperature for fungal sporulation (number of conidiophores and conidia formed in each conidiophore) is within the range of 20–25 °C (Burge 2006). Incidently this temperature range corresponds to the human comfort indoors, at which fungi flourish in working environments (Burge 2006). The relative humidity and air currents influence the release of conidia. Fungal growth is favoured at a water activity (aw) of 0.95–0.99, which is a ratio of the partial vapour pressure of water in a substance to the standard state partial vapour pressure of water. pH range of 5–6.5 in building materials allows better growth of most of the fungi (Vacher et al. 2010; Hoang et al. 2010). The thermophilic and xerophilic (dry tolerant) fungi are found more in hot-dry climates, than in cooler wetter environments. In tropical and subtropical places, thermophilic and xerophilic fungi tend to be abundant in outdoors with optimal heat and moisture. However, an array of factors are necessary for optimal growth of different kinds of fungi.
Cladosporium, Penicillium, and Aspergillus produce high numbers of small and light spores (<10 µm in size). Penicillium and Aspergillus can grow in substrates with water activity lower than 0.80. The smaller particles can penetrate into the alveolar region when inhaled, evade phagocytosis by macrophages, and transport through systemic circulation (Reponen et al. 2007; Seo et al. 2009) , whereas the larger spores and other fragments get deposited in the nasopharynx. Kildeso et al. (2003) studied the release of particles from indoor fungi growing in wetted wallpapered gypsum boards, for 46 weeks. When Penicillium chrysogenum were subjected to air currents, only spores were released from the colonies, but with Aspergillus versicolor, both spores, and fragments were released. With Trichoderma harzianum, particles released are—groups of spores (5–6 µm), individual spores (2–3 µm) and fragments (0.7–1 µm). Seo et al. (2009) reported the release of fragments and spores from Aspergillus Versicolor and Stachybotrys chartarum growing on the surface of ceiling tiles, wallpapered gypsum board, and culture medium. The studies are suggestive that long-term mould damage in buildings may increase the contribution of fungal fragments to the overall mould exposure.
Quantitation of Fungi
In non-culture-based methods, fungal spores in samples and its morphological identification are determined by light microscopy. Components or metabolites of fungi can also be used to quantitate fungi population. Specific assays can detect extracellular polysaccharides for partial identification of fungal genera in indoor environments (Jovanovic et al. 2004). Polyclonal antibody-based assays detect a broad range of fungal antigens but cannot detect the spores (Mitchell et al. 2007) . Molecular methods for quantitation of fungi include the use of genus-/species-specific probes, polymerase chain reaction (PCR)-based methods, restriction endonuclease analysis, and karyotyping. Mitochondrial DNA can be used for restriction enzyme analysis and DNA fingerprinting for fungal identification.
Sampling Methods
The typical approach for fungal detection in a building utilizes culture and microscopy. Different surface and air sampling methods are used for detection and counting of fungi, fungal spores and fragments in ambient air and settled dust, pieces of wallboard, duct linings, carpets (Asadi et al. 2011; Reponen 2011) . Surface sampling allows determining the degree and the types of microbial growth on environmental surfaces (Cabral 2010). Adhesive tape sampling method examines the fungi and the hyphal fragments in the specimens using a compound microscope (Aydogdu et al. 2010).
In air sampling of fungi, the principles of impaction, impingement, and air filtration have been used. In the impactor method, the airstream is passed through progressively narrower slits into a culture medium and microscopic glass slides covered with an adhesive substance or tape strip is used to collect the sample, and counted by optical microscopy (Zhen et al. 2009). Andersen six-stage impactor is used for collection of particles on culture medium. In Andersen sampler, in a Petri dish could grow 400 colonies. Fast-growing colonies may grow above the slow growing and hinder in counting colonies (Stetzenbach et al. 2004) . The dichloran-glycerol-18 agar (DG-18) culture medium with fungistatic properties prevents the growth of the fast-growing fungi (Horner et al. 2004). Liquid impingers collect the samples into the fluid, and the micro-organisms are retained in the liquid until they are cultivated, or evaluated by techniques like biochemical or immunoassays (Jo 2011). Shipe sampler, AGT–30 glass impinger, midget, multi-stage, and micro impingers are common impinger devices (Gralton et al. 2011). Air filtration is used to collect the samples of indoor air in volume. In this method after sampling, the filters are agitated or sonicated in a solution (Bazaka et al. 2011).
Readers may refer to standard manuals for analytical details. However, the choice of air or surface sampling techniques depends on the purpose of measurement (Jung et al. 2011). Air sampling by impingement has some advantages over impaction on solid surfaces; for example, if the concentration of microbes in the atmosphere is too high, the liquid could be diluted before adding to the culture medium. Collection of the cells in a liquid avoids desiccation resulting from impaction on solid surfaces (Stetzenbach et al. 2004) . Impaction directly onto agar plates may maximize survival of culturable organisms. In addition to impaction and impingement, other methods like filtration by aspiration and sedimentation sampling have been used. In filtration, three types of filter media are used, such as porous fibrous filters with overlapping fibres, porous gel membrane filters, and capillary pore filters. Filter materials include glass fibre, mixed cellulose esters, polytetrafluoroethylene, polyvinyl chloride, gelatin, and polycarbonate (Martinez et al. 2004 ). Membrane filters can be placed directly on the surface of culture medium or washed with a liquid, and this added to culture medium. Specific filters (namely gelatin) are dissolvable in warm liquids, and the resulting suspension can be plated on agarized medium. That is, filtration devices are adaptable for air sampling of wall cavities or roof spaces to pinpoint foci of contamination.
Sedimentary sampling (e.g., the gravity slide and the settle plate techniques) is the simplest of all methods. In the gravity slide method, microscopic glass slides, smeared with an adhesive substance, are exposed during a specified period. In the settle plate method, open petri dishes with appropriate culture medium are left open for a given time, depending on the air contamination load. After a certain period of incubation, colonies are counted. An index of microbial air (IMA) contamination was proposed; that is, a standard petri dish (dia: 9 cm) containing plate count medium is left open to the air, for 1 h, 1 m from the floor and at least 1 m away from walls. After 48 h incubation at 36 °C, the colonies are counted, and the number of colonies is the IMA. Five IMA classes were defined, as 0–5 very good; 6–25 good; 26–50 fair; 51–75 poor; and >76 very poor.
The conventional sampling apparatus gives values for fungal particles present in the atmosphere, at the time of sampling; however, other spores and fragments can be attached to the colonies and be released later. The fungal spore source strength determines the maximum amount of fungal particles that can be released from contaminated materials by the action of air currents. From the counting of released particles, the maximum fungal load for a given indoor environment can be calculated (Gorny 2004; Sivasubramani et al. 2004a, b ).
Fungi and Respiratory Symptoms
Damp concrete floor and visible mould in buildings are constant sources of risk of respiratory tract symptoms, infections, and exacerbation of asthma (Lanier et al. 2010; Araki et al. 2010). Mucociliary clearance represents the first strategy for removal of fungi/mould from the human respiratory tract. Hypersensitivity syndromes, such as hypersensitivity pneumonitis (both acute and chronic) or extrinsic allergic alveolitis, can occur in individuals exposed to conidia, hyphae, or fungal fragments, mycotoxin (trichothecene) (Eduard 2009; Franks and Galvin 2010). Hypersensitivity pneumonitis is generally associated with high IgG antibodies concentrations in response to alveolar or bronchiolar inflammation caused by fungi or other allergens. The patients may present neutrophilic inflammation with increased production of TNFa and IL-6, and symptoms such as fever, chilliness, dry cough, dyspnoea, changes in nodular bilateral X-ray, fatigue, and headache (Eduard 2009). Aspergillus spp. develops allergic bronchopulmonary aspergillosis and pulmonary aspergilloma (Kawel et al. 2011).
Undoubtedly, exposure to fungi in indoor environments elicits an IgE-mediated hypersensitivity response that precipitates into rhinitis and other forms of the allergic syndromes, such as upper airway irritation, eye irritation, and sinusitis (Yike 2011). During this process, antigen-specific IgE is produced that attaches to receptors on mast cells which are concentrated on the gastric and respiratory mucosa. The principal fungal allergens, such as (1–3)-b-D glucan or water-soluble glycoproteins, may become airborne and when its concentration exceeds 4 ng/m3, susceptible individuals may show non-specific inflammatory airway reactions and that affect the immune system (Kalyoncu 2010; Tercelj et al. 2011) . (1–3)-b-D glucan, a cell wall component of filamentous fungi, is readily detected in moisture-damaged building materials, dust samples, and textile floor coverings (Reponen et al. 2010; Rylander 2010) . Ergosterol is found in the cell membranes of fungi, but its content varies with the fungal species (Heinrich 2011).
Besides, people who inhabit mouldy buildings (presence of S. chartarum and Aspergillus spp. in air samples) were reported with cognitive defects and difficulties in concentration (Drappatz et al. 2007). In mouldy buildings, occupants complain of dermatological symptoms, gastrointestinal problems, reproductive effects, rheumatologic, and other immune diseases. Breda et al. (2010) recorded that the rheumatic diseases (inflammation and stiffness in muscles, joints, or fibrous tissues) are exacerbated by indoor environmental conditions, including dampness and fungi infestation. Rheumatoid arthritis, ankylosing spondylitis, Sjogren’s syndrome, and psoriatic arthritis have been observed among occupants in water-damaged buildings with mould growth (Muise et al. 2010) .
Mycotoxins and SBS
Various fungi produce mycotoxins that are low molecular weight and non-volatile compounds, and potentially carcinogenic, teratogenic, and mutagenic. Mycotoxins can also be isolated from fungi-contaminated building materials and house dust (Engelhart et al. 2002). The production of mycotoxins by indoor fungi growing in building materials is usually lower than that cultivated in vitro in building materials (e.g., gypsum board, chipboard) (Nielsen 2003; Nieminen et al. 2002) . Aflatoxins, trichothecenes, and ochratoxins are common mycotoxins in indoor environments (Zain 2011; Halios and Helmis 2010). Other toxins (e.g., T-2, HT-2, deoxynivalenol (DON), nivalenol, diacetoxyscirpenol, satratoxins, trichoverrols, verrucarol, verrucarins, trichoverrins) have been described in this group. Trichothecenes are a family of mycotoxins produced by species such as Cladosporium, Aspergillus, Penicillium, Fusarium, Trichoderma, Myrothecium, Trichothecium, Stachybotrys, Cephalosporium, Giberella, Memnoniella (Tuomi et al. 2000) .
A possible causal relationship exists between mycotoxin exposure and building related illnesses (Sen and Asan 2009; Di Giulio et al. 2010) . The effects of trichothecenes exposure in humans include internal burning, vomiting, and diarrhoea with blood, cutaneous necrosis, and internal haemorrhages. Evidence gathered that exposure to higher concentrations of Penicillium and Aspergillus in the indoor environment could induce health problems and SBS symptoms. Severe asthma and acute exacerbations of asthma have been associated with Alternaria sensitivity and increased airborne concentrations of Alternaria spores (Salo et al. 2005). Vance and Weissfeld (2007) warned that the presence of S. chartarum indoors is a concern since its growth requires water saturation of cellulose-based materials such as paper, cardboard, wood, and gypsum board (Menetrez and Foarde 2004; Gottschalk et al. 2006). It is likely that plumbing and roof leaks provide the needed moisture for the fungus to grow. The small size, ellipsoid shape Stachybotrys spores can reach the lower respiratory tract (Murtoniemi et al. 2003) . The causal relationship between S. chartarum and SBS has been debated, with the view that health effects may be due to the presence of other pollutants, like VOCs ( MVOCs), endotoxins, respirable dust, and other compounds in the indoor environment (Bloom et al. 2007). DON, a trichothecene mycotoxin mainly produced by Fusarium molds, like other mycotoxins, is an immunomodulator that can enhance or suppress the immune system depending upon the dose and duration of exposure (Lee et al. 1999; Zhou et al. 1999) . The T2-toxin, which is produced by species of Fusarium and diacetoxyscirpenol, has been shown to modulate apoptosis in human promyelocytic leukaemia cells (Yoshino et al. 1996; Yang et al. 2000).
Several types of research explore the potential association of SBS with particular microbes, biotoxins, or other complex exposure mixture components observed in the water-damaged buildings (Shoemaker et al. 2005). Trichothecene mycotoxins produced by Stachybotrys, satratoxin, and roridin have been identified in serum using an ELISA assay. Generally viewed that the mixture components, including fungi, bacteria, mycotoxins, endotoxins, and lipopolysaccharides, interact synergistically, through the feedback control of pro-inflammatory cytokine production and induce SBS (Huttunen et al. 2004). The onset of SBS is typically observed following chronic exposure in water-damaged buildings, extending for many months. Needless to mention that health risk assessment for SBS has many uncertainties, such as the extent of toxin accumulation in tissues, interspecies differences in susceptibility, and threshold shifts of the repair mechanisms during chronic exposure (Shoemaker and House 2005; Shoemaker et al. 2005). There is an evident need to make the focus on innovative and effective therapeutic interventions (e.g., Cholestyramine (CSM) therapy) to remove biotoxins from the body, caused by toxic mould exposure.
Fungal VOCs and SBS
There are nearly 250 VOCs of fungal origin that often referred to as microbial VOCs ( MVOCs). These MVOCs produce mixtures of simple hydrocarbons, heterocycles, aldehydes, ketones, alcohols, phenols, thioalcohols, thioesters, and their derivatives, including benzene derivatives, and cyclohexanes (Korpi et al. 2009; Ortiz-Castro et al. 2009) . Currently, gas chromatography–mass spectrometry (GC-MS) is the primary method for the detection of MVOCs (Matysik et al. 2009). The electronic nose ( E-nose) is an alternative non-invasive technique to detect essential fungi and MVOCs. The instrument combines an array of electronic chemical sensors, a pattern recognition processing unit, and a reference library for recognizing odours (Wilson and Baietto 2009, 2011) .
Molhave (2008) emphasized the exposure to MVOCs as the aetiological agents associated with SBS, including lethargy, headache, as well as irritation of the mucous membranes. However, the types and concentrations of MVOCs in mould-infested buildings vary with the ventilation rate indoors, moisture level, the composition of mould population, and other parameters (Schleibinger et al. 2008) . For example, Penicillium, Aspergillus, and Stachybotrys are VOCs as well as mycotoxin producers (Matysik et al. 2008) . MVOCs are produced by the cells and released to the indoor environment, whereas mycotoxins are present inside the cells and fragments (Reponen et al. 2007) . In healthy individuals, the fungal spores and fragments are destroyed by cells of the immune system, but a small number of mycotoxins can still enter in the systemic circulation with possible chronic or sub-chronic toxic effects (Straus 2009) .
The fungal release of VOCs is sometimes referred to like products of secondary metabolism, and these compounds remain reasonably stable in a range of growth media and conditions (Moularat et al. 2011). Moularat et al. (2008a, b) described the assay of VOCs produced by Aspergillus niger, A. versicolor, and Penicillium brevicompactum and identified nineteen compounds resulting from fungal metabolism. MVOCs also cause indirect metabolic effects. Fungal colonization in urea formaldehyde insulation materials results in the cleavage of urea from the polymer releasing formaldehyde (Shinoj et al. 2011; Asan et al. 2010) . Like other sources of VOCs, the exposure of MVOCs even at deficient concentrations has been linked to symptoms such as a headache, nasal irritation, dizziness, fatigue, and nausea, independent of exposure to other allergenic fragments and toxins (Weinhold 2007; Burton et al. 2008) .
Respiratory Illness in Buildings
Researchers have attempted to distinguish between the SBS and building-associated illness (Jaakkola et al. 2007; Tsai et al. 2012) . As discussed, the SBS represents multiple non-specific symptoms among the building occupants, but its occurrence is correlated with some factors, such as the type of ventilation and the condensation or the leakage of water in building indoors. On the other hand, building-associated illness consists of different diseases with known aetiologies (Craig and Mindell 2011); for example, allergic alveolitis, with specific aetiologies, is usually linked to ventilation-based, wet microbial breeding places, such as humidifiers, air washers, heater/cooler units. In multifactorial causal situations, however, several components attribute to creating complex environmental conditions. Ventilation inadequacy in indoor spaces may aggravate IEQ, resulting in health symptoms, SBS or BR and other communicable respiratory illnesses, such as allergy and asthma symptoms, respiratory infections and cardiovascular diseases. The literature emphasizes association of building characteristics, IAQ, and inhaling of bioaerosol with the prevalence of respiratory illnesses among building occupants. For easy understanding by the professionals from other building sciences, some common forms of respiratory illnesses are briefly described herewith. Details of the respiratory illnesses are found in several online sources, e.g., http://www.mayoclinic.org/diseases-conditions/copd/symptoms-causes/dxc-20204886.
Asthma and Asthma-Like Disorders
Increased prevalence of asthma has long been known as the impacts of outdoor and indoor exposures to air pollutants, and lifestyle habits, as well (Eder et al. 2006). Asthma can be adult onset or occupational in origin. From a clinical point of view, bronchial asthma is a well-known lung condition, defined as a chronic inflammatory disease, due to the contraction of the bronchial muscles, increased mucous production or decreased clearance, and muscle tightening, causing variable airflow obstruction (Fig. 3.1). Coughing, wheezing, chest tightness, shortness and shallow breathing, anxiety, and tachycardia are the common signs and symptoms of asthma. The inflammation causes airway hyper-responsiveness and is the reason for the appearance of variable and reversible airflow obstruction. Occupational asthma is caused by breathing substances present at workplaces, such as chemical fumes, gases or dust which are irritating or sensitizing. Exposure to these substances develops an immune response either to respiratory irritants (gas, fume, or vapour), usually of low molecular mass at high concentration, referred to as irritant-induced occupational asthma, or to sensitizing agents (e.g., high molecular mass―glycoproteins of biological origin), referred to as sensitizer-induced occupational asthma. These exposures are characteristically associated with symptoms at work with relief on weekends and holidays. With early diagnosis and treatment, occupational asthma may be reversible. Table 3.5 includes the most common asthmagen agents.
Fig. 3.1.
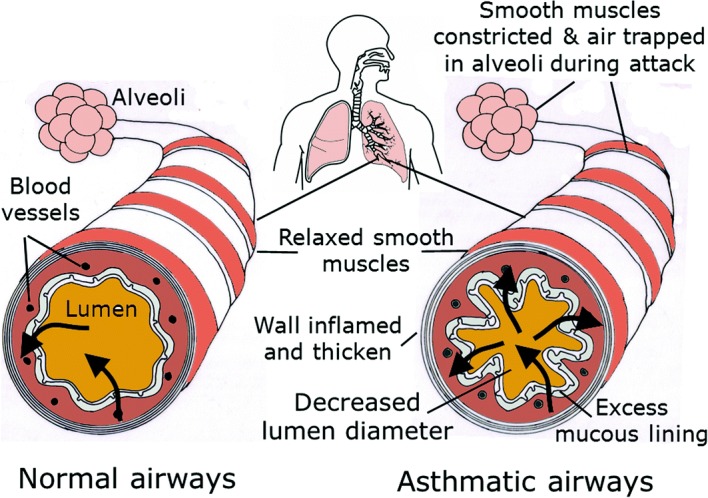
Illustrated normal and bronchial asthmatic airways
Table 3.5.
Common most asthmagen agents
| Classification | Sub-groups | Sources | Occupational activity |
|---|---|---|---|
| High-molecular-weight protein antigens | Animal-derived substances; plant-derived substances | Laboratory animals, seafood, grain mites/insects; grain dust, natural rubber/latex gloves, bacterial enzymes, vegetable gums | Animal handlers, food processing; bakeries, healthcare workers, detergent making; |
| Low-molecular-weight/chemical sensitizers | Plasticizers, paints, adhesives, wood dust, foams, metals, drugs and pharmaceuticals | Isocyanates (e.g., toluene diisocyanate), acid anhydrides (e.g., phthalic anhydride), amines (e.g., ethylenediamine), fluxes (e.g., colophony), metals (e.g., platinum salts), drugs (e.g., penicillin), plastics (e.g., acrylates), wood dust (e.g., western red cedar) | Auto-spray painting, varnishing, metal grinding, platinum refineries, pharmaceutical manufacturing, sawmill work, woodworking, |
| Other chemicals | Biocides (e.g., glutaraldehyde), polyvinyl chloride fumes, organophosphate insecticides | Janitorial work, meat packaging |
Irritant-induced acute occupational asthma (also termed as reactive airway dysfunction syndrome― RADS) may occur following a short-duration single high-level irritant exposure to substances, such as chlorine or oxides of nitrogen, or multiple exposures to gas, smoke, fume, or vapour characterized by irritant capacity. Respiratory symptoms (a cough, wheezing, chest tightness, and dyspnea) may persist for 3 months. Low-molecular mass agents probably become antigenic after conjugation with a body protein (e.g., serum albumin), and its response clinically manifest as direct epithelial cell injury. The procedure to diagnose RADS includes analysis of occupational history, inventory of exposures in the workplace, pulmonary function tests (PFT), serial peak expiratory flow measurement on work days and days off, histamine or methacholine challenge, and immunological tests, such as specific IgE and skin prick, epicutaneous tests (Fishwick et al. 2008; Tarlo et al. 2008) . The PFT may show evidence of airway obstruction (FEV1/FVC ratio less than 0.7), although the absence of airway obstruction does not exclude a diagnosis of the disease. For irritant-induced asthma due to indoor environmental exposures, specific bronchial challenges may not diagnose; also the peak expiratory flow (PEF) is not diagnostically specific. However, conventional approach of observing an elevated diurnal variation in PEF might suggest the presence of asthma. Bronchodilator response may be seen in individuals with acute irritant-induced asthma. A chest radiograph is usually normal, although it may show no specific signs associated with coexisting respiratory infection. A bronchial biopsy may indicate possible inflammation with lymphocytes and plasma cells, as a manifestation of epithelial cell injury.
Sensitizer-induced occupational asthma is characterized by a latency period, which may last from several weeks to months or years, between first occupational exposure to a respiratory sensitizer and the development of immunologically mediated symptoms. Once the subject is sensitized, asthma attacks are provoked even with exposure to a shallow concentration of the sensitizing agent. Diagnosis is typically achieved from the evidence of reversible variable airway limitations, along with asthmatic trends between periods of work and rest. PFT may become normal rapidly after the cessation of the exposure. A serial PEF (about four recordings a day) over three weeks has high specificity and sensitivity in making the diagnosis of occupational asthma. Serum-specific IgE may assist in making a diagnosis, due to its likely presence in persons exposed to allergens with high molecular weight and some chemical agents. Skin prick tests may also be positive for the workplace allergen. Increased bronchial reactivity to challenge with the agents, such as histamine, methacholine, is evidence of sensitizer-induced occupational asthma, and this may be carried out sequentially over time. Allergens that cause occupational asthma can also cause allergic rhinitis (nasal symptoms) that may precede the onset of occupational asthma symptoms or may commence at the same time as asthma symptoms.
Simoni et al. (2010) showed that upper respiratory tract symptoms were more prevalent in poorly ventilated classrooms. That is, with CO2 levels exceeding 1000 ppm had a higher risk of a dry cough and rhinitis. Increased ventilation rate (>0.7 l h−1) was associated with a decreased prevalence of allergic symptoms among college students living in dorms in China (Sun et al. 2011a) . The occurrence of wheeze decreased with the increase in ventilation rates when CO2 concentration reduced from 1359 to 915 ppm.
The prevention of occupational asthma requires environmental intervention and medical management. The primary prevention of exposure, such as improved ventilation and dust control for elimination of the formation of dust, and localized aspiration, is the direct approach towards reducing the incidences of the disease. Avoiding cold temperature and air dryness, wearing PPE, and in some cases, adopting prophylactic pharmacological treatments can mitigate asthma symptoms. Population screening for early detection is the secondary prevention.
The term Asthma-like (suspected asthma) is indicative that all asthma-like symptoms are not associated with asthma. These include chronic obstructive pulmonary disease, chronic bronchitis, chronic cough, hyperventilation, mechanical obstruction of the airways, congestive heart failure, pulmonary embolism, gastro-oesophageal reflux, multiple chemical sensitivity/idiopathic environmental illness, SBS, Sjogren’s syndrome, vocal cord dysfunction. The chronic obstructive pulmonary disease is characterized by a slowly progressive reduction of pulmonary ventilation due to a combination of emphysema and bronchiolitis with obstruction of the small airways. ETS is a critical aetiological factor. Chronic cough has different aetiologies—a cough at night or associated with physical exercise may be indications of asthma. The asthma tests such as reversibility to a bronchodilator and increased levels of exhaled nitric oxide should be positive (Chatkin et al. 1999). Hyperventilation syndrome is indicated by symptoms induced by physiologically inappropriate hyperventilation or voluntary hyperventilation. Shortness of breath, accelerated/deepened breathing, and feeling of inability to breathe deeply are asthma-like. Symptoms reproduced by a hyperventilation test and a slow recovery of CO2 in blood or expired air are the two criteria for establishing the diagnosis (Ringsberg and Akerlind 1999) . RADS is an illness with asthma-like symptoms that may occur as the direct consequence of excessive toxic inhalation exposure. The bronchial histological changes show an increase in inflammatory cells. However, eosinophils and mast cells do not dominate. Multiple chemical sensitivity (also named as idiopathic environmental intolerance) is a disease caused due to some low dose of exposure to chemical toxicants, manifesting diverse symptoms (e. g., headache, weakness, memory problems, inability to concentrate, throat soreness, abdominal pain, and discomfort). One may suffer from nasal congestion and asthma-like symptoms such as cough and chest tightness. As elaborated earlier, SBS is a complex disease caused primarily due to building characteristics of the indoor environment, including inadequacies in air-handling systems. Sjogren’s syndrome is a systemic rheumatic disease. Vocal cord dysfunction is characterized by episodic or acute attacks of breathing troubles similar to attacks of asthma. In asthma-like disorder, treatment compliance with conventional therapy is low (Schmier and Leidy 1998; Chan et al. 1998) . Medication with steroids are the most potent drugs in the treatment of asthma.
Sensory hyper-reactivity (earlier referred to as functional breathing disorder) manifests common symptoms, such as heavy breathing, cough, and increased secretion, difficulty in getting air, and chest pressure (Lowhagen et al. 1997) . The symptoms are often induced by trigger factors, such as allergens, chemical irritants, ETS and strong scents, cold air, viral infections, physical exercise (Millqvist and Lowhagen 1998). Symptoms, such as difficulty in breathing and breathlessness, which indicate asthma, may also be indicators of sensory hyper-reactivity. The diagnosis of sensory hyper-reactivity is a clinical challenge; PFT is sometimes difficult to obtain due to inability to perform an adequate forced expiration, giving a false indication of bronchoconstriction (Ringsberg et al. 1997). Asthma-like symptoms can be provoked by a sensory nerve-mediated disturbance of the respiratory pattern; for example, a capsaicin inhalation test provokes these kinds of symptoms (Millqvist et al. 1998) .
Extrinsic allergic alveolitis (EAA, also termed as hypersensitivity pneumonitis) is type III and IV hypersensitivity reaction of the alveolar and bronchiolar tissue and interstitium of the lungs, in response to inhaled antigens. A range of environmental allergens, including fungi, bacteria, plant proteins, and other reactive chemicals, may be related to the occurrence of EAA (Simon-Nobbe et al. 2008; Robertson et al. 2007) . Farmer’s lung caused by mouldy forage is a well-studied form of EAA. Microbiological contamination of air conditioners or humidifiers has been reported to cause of EAA in an office environment. The EAA may manifest as an acute, sub-acute, and chronic form. The former form is more natural to recognize, with symptoms, like a cough, chest tightness, febrile chills, and flu-like illness appear 3–8 h after exposure, fades away gradually over a few hours, and may reappear on subsequent exposure. The sub-acute form presents as progressive shortness of breath, dry cough, and weight loss. The chronic form may show the slow development of interstitial fibrosis.
Diagnosing EAA requires identifying the source of exposure to contaminants, recording exposure history, including worksite visit and environmental measurements. In physical examination, crackles in the lower fields of the lungs may be noticed. A chest X-ray may show fine interstitial infiltrates in acute and sub-acute forms of the disease, whereas in the chronic form, irregular scarring may indicate diffuse pulmonary fibrosis. In PFT, typically patients may show restrictive impairment, i.e., the FEV1/FVC ratio reduced in comparison with its normal range. The EAA is a diffuse parenchymal disease, and thus, the diffusion capacity of the lungs is affected (both DLco and Kco). Bronchoscopy with bronchoalveolar lavage (BAL) and transbronchial biopsy may be carried out when investigating a patient with suspected EAA. BAL typically shows increased total cell count, with an increased proportion of lymphocytes (>40%). T-helper to T-suppressor ratio is usually reduced to less than 1. After acute exposure, neutrophils are transiently increased. The histopathologic findings include diffuse interstitial infiltrate, scattered non-caseating granulomas, and cellular inflammation of the bronchioles. An inhalation provocation test with the specific antigen can be performed to confirm the diagnosis; a worksite challenge test is a conventional approach, with PFT before and after workplace exposure. Management of EAA primarily demands to remove the affected persons from the source of exposure. Drug intervention with corticosteroids is given at the acute episodes. Any dampness or mould problems in buildings should be repaired promptly.
Humidifier fever, like in EAA, is also termed as a disease related to bioaerosol exposure from contaminated humidifier water, often referred to as Monday morning fever. The affected person experiences fever, nausea, sweating, and myalgia, sometimes with breathlessness, about 3–8 h after exposure, which is very similar to those described in outbreaks of EAA. The symptoms diminish towards the end of the working week, and over the weekend, for example, the episode may be worse again. Humidifier fever differs from EAA in that the affected person may have specific IgG antibodies to the micro-organisms growing in water reservoirs as a sign of exposure. Regular maintenance of humidifiers and air conditioners is the best approach to prevent humidifier fever (Pal et al. 2000) .
Legionnaires’ disease presents as pneumonia, due to infection with Legionella pneumophila, a bacterial micro-organism that may be found in wet surroundings and capable of forming colonies in cooling towers and hot water systems in hospitals and office buildings. An outbreak of Legionella pneumophila in Philadelphia in 1976 (Fraser et al. 1977) with the source identified at the ventilation and humidification system of a hotel, affected 221 persons, with about 20% mortality. The incubation period of the disease is about a week. The early symptoms include illness, headache, myalgia, fever and mild cough, blood in the sputum, and watery diarrhoea (Cunha 2008). There may be a neurological symptom of severe encephalopathy. A chest X-ray may show unilateral lobe infiltrate, with rapidly progressive infiltrations of Legionella. Complete recovery of the infiltrates may take several weeks to months. Urinary antigen detection is a rapid test. However, it is less sensitive than culturing respiratory secretion. Superheating of hot water to >50 °C and flushing the water distribution systems are crucial to prevent Legionella infections.
Other Office Environment Exposures
Office environment exposures through handling of self-copying paper that contains ink, solvent and dust, acrylate glues used in flooring, PVC, phthalate compounds, and wall-to-wall carpet might induce airway inflammation in humans (Jaakkola et al. 2006; Jaakkola and Jaakkola 2007; Jaakkola and Knight 2008). Professional cleaners in buildings are regularly exposed to cleaning chemicals containing ammonium, bleach, chlorine, and some disinfecting substances, and these people may develop irritant-induced asthma (Zock 2005). Table 3.6 includes different environmental, physical, and social factors, which may cause one or more signs and symptoms related to SBS.
Table 3.6.
Environmental exposures to cause signs and symptoms related to SBS and other respiratory illnesses
| Sources | Potential exposures/factor |
|---|---|
| Physical environment | High indoor temperature (>23 °C); low relative humidity; low air change |
| Water damage or leakage | Dampness and mould |
| Paints | Toluene, propylene, glycol, ethylene glycol, butyl propionate, methyl propanol |
| Furniture (plywood, plastic) | Formaldehyde, 2-pentyl furan, benzaldehyde, hexanal, pentanal |
| Carpets | Particles, vinyl acetate, styrene, dodecanol, acetaldehyde |
| Plastic wall, PVC flooring | Phthalates |
| Photocopying | Xylenes, benzene, 2-ethyl-1-hexanol |
| Cleaning agents (Detergents) | Fatty acid salts, organic sulphonates |
| Cleaning agents (water softeners) | EDTA (ethylenediaminetetraacetic acid), tripolyphosphates |
| Cleaning agents (Alkaline agents) | Silicates, carbonates, sodium hydroxide, ammonia |
| Cleaning agents (Acids) | Phosphoric, acetic, citric, sulphamic, hydrochloric acid |
| Disinfectants | Hypochlorite, aldehydes, quaternary ammonium compounds |
| Carbonless copy paper | Crystal violet lactone, trimellitic anhydride (TMA), phenol-formaldehyde resins, azo dyes, diisopropyl naphthalenes (DIPN), formaldehyde, isocyanates, hydrocarbon-based solvents, epoxy resins, aliphatic isocyanates, Bisphenol A, diethylenetriamine |
| Smoking | Environmental tobacco smoke (ETS) |
Second-hand tobacco smoke exposure (SHS), containing irritant substances, can potentially induce mucus hypersecretion and inflammation in the airways (Jaakkola et al. 2003; Gilmour et al. 2006). In adults with asthma, SHS exposure is related to increased occurrence of respiratory symptoms, reduced lung functions, increased use of bronchodilator and steroid medications, and increased bronchial hyper-responsiveness (Jaakkola and Jaakkola 2002). Fisk et al. (2007) from a meta-analysis of 33 epidemiological studies on dampness and mould problems revealed 30–50% increased risk of asthma about indoor dampness and mould problems in buildings. The IgE-mediated hypersensitivity reactions to fungal allergens (Jaakkola et al. 2006) and mycotoxins produced by fungi and inflammatory reactions caused by fungal cell wall components (1,3-β-D-glucan, ergosterol) are the suggested mechanisms that could lead to asthma.
Airborne Transmission of Pathogens
There is a whole range of airborne pathogens, such as Aspergillus and Bacillus spp., that may be found in the built environment and also during construction or renovation activities (Balm et al. 2012; Fournel et al. 2010). Particular focus is on hospitals and healthcare buildings, to create healthy conditions. Natural ventilation and availability of sunlight in buildings serve as effective strategies in infection control of diseases, such as measles, tuberculosis, smallpox, chickenpox, influenza, SARS and H1N1 (Li et al. 2007) .
The transmission of pathogen takes place through contact, dust, respiratory droplets, and droplet nuclei, e.g., inhalation of large droplets from contagious individuals or contaminated surfaces. The transmission depends upon the number and size of particles produced, the velocity at which they are produced, micro-organisms contained within the droplets, and proximity of a susceptible target (Gralton et al. 2011). The longevity of the pathogens depends on temperature and humidity, ultraviolet (UV) radiation, and atmospheric pollutants (Tang 2009) . Depending on the size and density, residues of suspended droplet nuclei can remain suspended and penetrate deep into the lung tissues. Droplet nuclei that are exhaled during normal breathing are only a small fraction than those aerosols produced when coughing or sneezing (Gralton et al. 2011). Factors, such as local ventilation, the activity of occupants indoors, and thermal gradients produced due to office equipment influence the movement of the suspended droplets (Nielsen 2009; Eames et al. 2009; Clark and de Calcina-Goff 2009) . Towards controlling infection in healthcare and other building facilities through sunlight and natural ventilation, transmission and control of some pathogens are briefly described herewith.
Influenza is assumed to be transmitted by large droplets. However, the aerosol transmission, such as H5N1 avian influenza that demonstrates high virulence and lethality involves the lower respiratory tract (Tellier 2009; Tang and Li 2007) . Direct contact with diseased poultry and other birds may cause H5N1 transmission through the air, without recombination in an intermediate host (Herfst et al. 2012).
Severe acute respiratory syndrome (SARS) epidemic in 2003 was assumed direct contact as the primary transmission route. The Hong Kong, Amoy Gardens outbreak, is an affirmative indication of the airborne transmission of the SARS virus (McKinney et al. 2006) , such as transmission of virus-laden aerosol through inadequate ventilation, the ventilating shaft of adjacent buildings, floor drainage. Before the SARS epidemic, hantavirus transmission causing the pulmonary syndrome in humans has been demonstrated, due to the inhalation of aerosolized excreta and saliva from wild rodents (Kimmel et al. 2010; Clement et al. 2008). The primary prevention is to clean the ventilation system of buildings that show signs of rodent infestation. Norovirus that causes gastrointestinal illness is transmitted via contact with food materials, contaminated surfaces, and the spread of aerosolized particles from vomiting or liquid diarrhoea (Marshall and Bruggink 2011; Greig and Lee 2012) .
Tuberculosis is mainly contracted through airborne droplets; that is, transmission of M. tuberculosis to a non-infected person is possible if there are overcrowding and confined environment, and poor indoor ventilation (Beggs et al. 2003). Earlier it was presumed that smallpox virus spreads by face-to-face contact. However, airborne transmission of the virus is evident now. Occupants in hospital, health care, and allied facilities are at potential risk from Staphylococcus aureus (Kerr 2010) that get deposited throughout a room. Nasal cavities of susceptible adults become colonized with S. aureus by inhaling particles from the air. There are many other pathogens found in an aerial spread in building facilities, such as Escherichia coli, Klebsiella, Acinetobacter, Pseudomonas, Clostridium difficile (Wu et al. 2011) . Persons infected with C. difficile may shed spores in faeces, and therefore, when a toilet is flushed without a closed lid, aerosol production may contaminate the surrounding environment (Best et al. 2012).
SBS: Intervention and Management
Office goers and building occupants are usually not exposed to high levels of physical, chemical, or biological compounds potentially hazardous to health. Office environments have traditionally been considered as safe. However, an ample body of the literature is available on SBS and building-associated illnesses (BRI) from different kinds of studies, including epidemiological cohort and cross-sectional studies, population questionnaire surveys, and experimental studies. The risk of SBS may occur at different levels, for example, (a) building level—indoor environmental quality, different sources pollutants, and exposure to bioaerosols, (b) personal level—interpersonal differences (women, younger and the elderly people, persons predisposed with chronic disease show more SBS related complaints), and (c) workplace stressors—aspects of work and psychosocial environment of the building occupants, and ones’ ability to cope with the conditions of workplace and workspace. Since all these levels are simultaneously present, one major problem emerges in SBS and BRI is its lack of generalizability. On a simplistic way, the overall impression of the building environment may be rated by the occupants on an ordinal 100 point scale, against the stated levels of IEQ, personal characteristics, aspects of work and the psychosocial environment. The summated scores are scaled into an overall dissatisfaction score for the building occupants.
Mitigation of IAQ problems may require the involvement of building management and related people of responsibility in facility operation and maintenance, housekeeping, policy-making, and staff training. Three methods have been suggested to improve the IAQ, namely source control, increase ventilation, and air cleaning. The source control is the most cost-effective approach to mitigating IAQ problems in which point sources of contaminants can be identified. Conventional pollution source control method, such as adsorption by microporous activated carbon and chemical scrubbers, has reasonable efficacy to mitigate pollutants. Thermal catalytic oxidation (Everaert and Baeyens 2004; Roark et al. 2004) and photocatalytic oxidation (Carp et al. 2004) are promising technologies for air purification. However, the former is not economically feasible at low pollutant concentrations. Photodegradation may be more cost-effective for air purification since the process takes place at room temperature and pressure. TiO2, a popular photocatalyst, is employed for removal of VOCs from indoor air (Wang et al. 2006, 2007) . By incorporating TiO2 catalyst with adsorbent may yield better results for adsorption of pollutants and oxidation efficiency. This type of catalyst, however, exhibits high catalytic activity at UV light.
Building Ventilation—Health Relationships
The literature suggests a robust affirmative link between ventilation and the respiratory health of building occupants (Seppänen and Fisk 2004) . Due to the random character of natural ventilation during different seasons of the year, emphasis among the building designers goes in installing mechanical ventilation and HVAC systems. The natural ventilation no longer provides optimal distribution of fresh air in the buildings. However, several views have been put forward with regard to mechanical ventilation systems and acute health symptoms (SBS/BR), asthma and allergy symptoms among occupants in buildings. Mendel et al. (2003, 2006), examining US NIOSH data of 80 office building, emphasized that improperly maintained ventilation systems increase the adverse health effects among the occupants, particularly the asthmatics, due to exposure to accumulated pollutants and microbiological growth. Comparing with naturally ventilated systems, the presence of air-conditioning increased respiratory symptoms in office buildings located in a hot and humid climate (Graudenz et al. 2005). Takahashi et al. (2008) reported that the presence of a ventilation system was associated with increased allergic symptoms, probably due to the entry of large quantities of pollen into the dwellings through the air ducts and other factors, not directly related to the ventilation system. Dwellings installed with air conditioners, and those had poor maintenance of ventilation systems, resulted in increased prevalence of SBS (Wong et al. 2004; Coelho et al. 2005), as compared to those in naturally ventilated dwellings. Some multidisciplinary reviews on relationships between ventilation rate and health outcomes are summarized in Table 3.7.
Table 3.7.
Case studies on the influence of indoor ventilation rate on health outcomes
| Godish and Spengler (1996) | Increasing the ventilation rate up to 10 l/s per person may be useful in reducing the prevalence of SBS symptoms and occupant dissatisfaction with air quality. The use of ventilation as a mitigation measure for IAQ problems should be dealt with factors that may limit its effectiveness |
| Seppanen et al. (1999) | Ventilation rates below 10 l/s per person in different building types were associated with significant worsening in one or more health or perceived air quality outcomes. Some studies determined that increasing ventilation rates above 10 l/s to ~20 l/s per person significantly decreases the prevalence of acute health symptoms or improvement in the perceived air quality. The SBS symptoms continued to decrease significantly with decreasing CO2 concentrations below 800 ppm |
| Wargocki et al. (2002, 2004) | Ventilation rates below 25 l/s per person increase the risk of acute health (SBS) symptoms, increase short-term sick leave, and decrease productivity |
| Mendell and Heath (2005) | No substantial evidence on the causal relationships between indoor pollutants or thermal conditions in schools and the performance of students. Suggestive evidence links low ventilation rates in buildings to decreased performance in children and adults |
| Seppanen et al. (2006) | A 1–3% improvement in average performance was associated with an increase in ventilation rate by 10 l/s per person. The performance increase per unit increase in ventilation was more substantial with ventilation rates in the range 15–17 l/s per person, and almost negligible with ventilation rates over 45 l/s per person |
| Li et al. (2007) | Strong evidence of the association between ventilation, air movements in buildings, and the transmission/spread of infectious diseases. Data insufficiency to define the ventilation rates that can reduce the spread of infectious diseases via the airborne route in hospitals, schools, offices, homes, and isolation rooms. Overcrowding is a risk factor related to the ventilation of buildings and also infection transmission via direct contact |
| Fisk et al. (2009) | Reduction in ventilation rate from 10 to 5 l/s per person led to increased prevalence of SBS symptoms by ~23% (12–32%). Increase in ventilation rate from 10 to 25 l/s per person led to the decreased prevalence of acute symptoms by 29% (15–42%) |
| Sundell et al. (2011) | Ventilation rates, up toper person, were associated with reduced prevalence of SBS symptoms in offices. Ventilation rates in homes above 0.5 ACH are associated with a reduced risk of allergic manifestations among children in a Nordic climate |
The above stated studies provide a fair understanding that ventilation (air change in a built environment) plays a central role to exhaust pollutants of both non-biological and biological agents of the occupied space or generate pollutants within systems. Chapter 10.1007/978-981-13-2577-9_12 elucidates the design, installation, operation, and maintenance of ventilation systems in buildings. Ventilation inadequacy may be due to poor building design, inadequate ventilation system, and its improper maintenance and operational strategies. Lack of control of HVAC systems aggravates the growth of micro-organisms. Besides, the quality of outdoor air, building materials, and accumulated dust are also sources of microbial contaminants in indoor environments. The presence of mould, spores, musty smell, and water intrusion are warning signs, reflecting the inefficiency of a building’s ventilation system (Radon et al. 2008) .
It is emphasized that the strength of elimination of pollutants from building space is the determinant of exposure-associated adverse health effects of occupants. In spite of differing views, ventilation rates below 10 l/s per person would increase the risk of symptoms of SBS (Jaakkola and Miettinen 1995) . The assertion from the BASE study of the association of SBS with the increasing difference in concentration of CO2 between indoor and outdoor brings forward the suggestion that a relative increase in the ventilation rates per person in an office building may reduce the prevalence of SBS symptoms. A concentration of CO2 (800 ppm) has been suggested as a control limit value. Erdmann and Apte (2004) observed a remarkable reduction in mucosal symptoms ranging from 65 to 85% when CO2 levels in offices dropped in the range from 610 to 40 ppm above outdoor levels.
Frequent contributors to biological pollutants are water damage in buildings, leaks in plumbing, roofs or air conditioners, and humidifiers (McKernan et al. 2008; Li et al. 2010) . Given that some airborne moulds may always be present in the indoor environment, various guidance limits and remediation measures have been proposed (Baubiologie Maes 2008). EC guidelines state that mould count greater than 500 CFU/m3 may be considered an intermediate level of exposure for a building occupant, whereas >1000 CFU/m3 is a high level of exposure in indoor non-industrial workplaces. Levels more than these guidelines do not necessarily imply unsafe or hazardous conditions. In the USA, there are no exposure levels for airborne concentrations of mould (US OSHA 2003) . Every country must establish the requisite legislation and environmental standards and guidance concerning building maintenance specifications.
Also, building-associated illnesses manifest in multiple forms of symptoms, and often in combinations of asthma, hypersensitivity pneumonitis, and interstitial pneumonitis (Bornehag et al. 2001). Evidence of markers for individual susceptibility might separate normal from more sensitive groups. Symptoms of allergy and asthma may be triggered by allergens in the indoor air including those from house dust mites, pets, fungi, insects, and pollens. As elaborated earlier, asthma symptoms can be evoked by irritating chemicals or sensitizing agents. There are approaches to reducing allergy and asthma symptoms via changes in buildings and indoor environments. Reductions in allergy and asthma symptoms would be expected by a substantial reduction in the associated allergens and irritants, from indoors.
Overall, intervention and management of SBS and BRI may encompass measures, as described herewith. For new buildings, the prevention measures in reducing mould contamination include, for example, (a) minimizing moisture accumulation in construction materials, (b) maintaining the integrity of building impermeable envelope, and (c) ensuring the effectiveness of HVAC system to control thermal comfort and relative humidity. In the existing buildings, corrective measures include (a) repair and maintenance of water leakage in ceilings, walls, and draining systems, (b) deep cleaning of building interiors and HVAC systems, (c) control of the reservoirs of visible mould in ceiling and carpets, and (d) periodic assessment of IAQ. Once a mould problem is established, a well-documented action plan may be followed to notify people for (a) rectifying the underlying moisture problem, (b) minimizing spread of contamination, by cleaning of ventilation pathways and enhancing ventilation to exhaust the relevant pollutants from indoors, and (c) removing mouldy materials. It is important to consider that fungal spores are continually entering into the indoor environment and a remedial measure to fungal contamination is the maintenance of dry conditions in a building. As part of remediation, an entire or part of a building may be heated to a temperature that should kill most of the fungal spores. Caution is needed that heat may not damage specific equipment and plastic materials.
Ventilation and Pathogen Infection Control
Apart from dilution of airborne pathogens, high ventilation of outdoor air results in an adverse effect on viability and virulence of micro-organisms, including influenza and the Category IV pathogen, Francisella tularensis (Hood 2009). Infection of rhinoviruses causes adults to suffer the frequent common cold. Myatt et al. (2004) provided evidence of aerosol transmission of rhinovirus in mechanically ventilated office buildings that resulted in an increased risk of inhaling infectious droplets. In student rooms having a ventilation rate of about 1 l/s per person, the frequency of common colds was six times more among 35% of the students. The number of common colds was higher in winter. Reported common colds were higher when some students shared a room. By increasing the ventilation rate to 5 l/s per person, the self-reported common colds dropped to a mere 5% (Sun et al. 2011b) , suggesting that ventilation from outdoor-to-indoor bears greater significance in diluting and dispersing virus-laden droplets (Mendell et al. 2002). Milton et al. (2000) observed a reduction in short-term sick leave among office workers when the outdoor air supply rates increased from 12 to 24 l/s per person in an office building. Mendell et al. (2013) reported the relative decrease of illness absence of about 1.6% for each additional ventilation rate of 1 l/s per person.
Natural ventilation brings many advantages, whereas entry of unfiltered air containing free contaminants such as fungal spores (Bartley et al. 2010; Phares et al. 2007) is a possible disadvantage of natural ventilation. Natural ventilation can be more effective than mechanical systems for preventing transmission (Kembel et al. 2012). Despite that an outbreak of infectious disease is an outcome of several factors, as stated above, the evidence is supportive that ventilation is a modifying factor in the transmission of infection. Following the 2001 incidents of anthrax attacks, preventive intervention is to relocate air intakes to publicly inaccessible locations, e.g., secure roofs.
Coughing and sneezing activities can carry infectious aerosols a long distance within a built environment (Zhu et al. 2006). Intervention in building ventilation airflow patterns (Chen and Zhao 2010) can thwart particle transport from a source to a receiver. The exposed concentration of aerosol from sneezing, at the breathing zone of a receiver occupant is slightly higher under displacement ventilation, DV than mixing ventilation, MV system (Seepana and Lai 2012), due to its low local air velocities. High discharge velocity air curtains provide a strong momentum to redirect coughing and sneezing jets and minimize cross infection (Aubert and Solliec 2011; Nino et al. 2011) , and also influence heat gain/loss in a facility (Foster et al. 2006). With a protected occupied zone ventilation, POV system, the intake fraction of coughed particles in the breathing zone of the receiver occupant decreased to a significant extent, as compared to an MV system (Liu et al. 2014) . A narrowly concentrated plane jet was more effective at reducing the direct exposure to expiratory particles than with multiple low-velocity jets.
Preventing Infection by Sunlight
The majority of micro-organisms that cause airborne infections cannot tolerate sunlight. Direct sunlight passing through an ordinary window can kill M. tuberculosis and Meningococci within a few hours. Streptococcus pyogenes cannot survive more than 5 min under sunlight, compared with more than an hour in diffuse daylight. Lethality of sunlight against staphylococci is due to radiation at 300–380 nm; in addition to bactericidal effect, solar radiation is mutagenic. Ordinary window glass absorbs solar radiation at <300 nm, which permits entry of solar UV-A and small amounts of UV-B. Research indicates that UV wavelengths inactivate microbes by causing cross-links between constituent nucleic acids; the formation of intra-strand cyclobutyl-pyrimidine dimers within DNA leads to mutations and cell death (Maclean et al. 2010). Exposure to high-intensity visible violet light at 405 nm is likely to be associated with photoexcitation of porphyrin molecules, resulting in the production of reactive oxidative species that are strongly bactericidal (Hamblin et al. 2005).
The contemporary modern building envelopes have an overdependence on mechanical ventilation and HVAC systems. As insulation levels increase, there is a risk of overheating and poor IAQ (Bone et al. 2010). Typically, in cold climate, the heating in new buildings is provided by warm air, whereas heating in older ones was often from a radiant source (Hobday 2011). Any exclusion of sunlight in buildings, for example, in hospital and healthcare facilities increases the risk of infection, and a variety of other health problems (Castro et al. 2011; Hobday and Dancer 2013). The design of buildings that allow increased exposure to sunlight and outdoor air may discourage survival and spread of infectious agents with considerable health benefits to occupants.
References
- Apte, M. G., & Daisey, J. M. (1999). VOCs and “sick building syndrome”: Application of a new statistical approach for SBS research to US EPA BASE study data. In Proceedings of Indoor Air, 99. The 8th International Conference on Indoor Air Quality and Climate, 8–13 August 1999, Edinburgh, Scotland (Vol. 1, pp. 117–122).
- Apte, M. G., & Erdmann, C. A. (2003). Indoor carbon dioxide concentrations, VOCs, environmental sensitivity associations with mucous membrane and lower respiratory sick building syndrome symptoms in the BASE study: Analyses of the 100 building dataset. Lawrence Berkeley National Laboratory, p 23, 2002. http://escholarship.org/uc/item/3vj5m6wj.
- Apte MG, Fisk WJ, Daisey JM. Associations between indoor CO2 concentrations and sick building syndrome symptoms in US office buildings: An analysis of the 1994–1996 BASE study data. Indoor Air. 2000;10(4):246–257. doi: 10.1034/j.1600-0668.2000.010004246.x. [DOI] [PubMed] [Google Scholar]
- Araki A, Kawai T, Eitaki Y, Kanazawa A, Morimoto K, Nakayama K, Shibata E, Tanaka M, Takigawa T, Yoshimura T, Chikara H. Relationship between selected indoor volatile organic compounds, so-called microbial VOC, and the prevalence of mucous membrane symptoms in single family homes. Science of the Total Environment. 2010;408(10):2208–2215. doi: 10.1016/j.scitotenv.2010.02.012. [DOI] [PubMed] [Google Scholar]
- Aries MB, Veitch JA, Newsham GR. Windows, view, and office characteristics predict physical and psychological discomfort. Journal of Environmental Psychology. 2010;30(4):533–541. doi: 10.1016/j.jenvp.2009.12.004. [DOI] [Google Scholar]
- Asadi E, Costa JJ, da Silva MG. Indoor air quality audit implementation in a hotel building in Portugal. Building and Environment. 2011;46(8):1617–1623. doi: 10.1016/j.buildenv.2011.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asan A, Okten SS, Sen B. Airborne and soilborne microfungi in the vicinity Hamitabat Thermic Power Plant in Kirklareli City (Turkey), their seasonal distributions and relations with climatological factors. Environmental Monitoring and Assessment. 2010;164(1–4):221–231. doi: 10.1007/s10661-009-0887-8. [DOI] [PubMed] [Google Scholar]
- Aubert A, Solliec C. Push-pull air curtain performances for VOCs containment in an industrial process. Journal of Applied Fluid Mechanics. 2011;4:43–50. [Google Scholar]
- Aydogdu H, Asan A, Otkun MT. Indoor and outdoor airborne bacteria in child day-care centers in Edirne City (Turkey), seasonal distribution and influence of meteorological factors. Environmental Monitoring and Assessment. 2010;164(1–4):53–66. doi: 10.1007/s10661-009-0874-0. [DOI] [PubMed] [Google Scholar]
- Balm MN, Jureen R, Teo C, Yeoh AE, Lin RTP, Dancer SJ, Fisher DA. Hot and steamy: Outbreak of Bacillus cereus in Singapore associated with construction work and laundry practices. Journal of Hospital Infection. 2012;81(4):224–230. doi: 10.1016/j.jhin.2012.04.022. [DOI] [PubMed] [Google Scholar]
- Bartholomew RE, Wessely S. Protean nature of mass sociogenic illness. The British Journal of Psychiatry. 2002;180(4):300–306. doi: 10.1192/bjp.180.4.300. [DOI] [PubMed] [Google Scholar]
- Bartley JM, Olmsted RN, Haas J. Current views of health care design and construction: Practical implications for safer, cleaner environments. American Journal of Infection Control. 2010;38(5):S1–S12. doi: 10.1016/j.ajic.2010.04.195. [DOI] [PubMed] [Google Scholar]
- Baubiologie Maes. (2008). Institut fur Baubiologie + Okologie IBN. In Building Biology Evaluation Guidelines for Sleeping Areas SBM-2008. http://www.maes.de/14ENGLISCH/14GUIDELINES-2008.PDF.
- Bazaka K, Jacob MV, Crawford RJ, Ivanova EP. Plasma-assisted surface modification of organic biopolymers to prevent bacterial attachment. Acta Biomaterialia. 2011;7(5):2015–2028. doi: 10.1016/j.actbio.2010.12.024. [DOI] [PubMed] [Google Scholar]
- Beezhold, D. H., Green, B. J., Blachere, F. M., Schmechel, D., Weissman, D. N., Velickoff, D., et al. (2008). Prevalence of allergic sensitization to indoor fungi in West Virginia. Allergy and Asthma Proceeding, 29(1), 29–34. OceanSide Publications, Inc. [DOI] [PubMed]
- Beggs CB, Noakes CJ, Sleigh PA, Fletcher LA, Siddiqi K. The transmission of tuberculosis in confined spaces: An analytical review of alternative epidemiological models. The International Journal of Tuberculosis and Lung Disease. 2003;7(11):1015–1026. [PubMed] [Google Scholar]
- Bell IR, Baldwin CM, Schwartz GE. Illness from low levels of environmental chemicals: Relevance to chronic fatigue syndrome and fibromyalgia. The American Journal of Medicine. 1998;105(3):74S–82S. doi: 10.1016/S0002-9343(98)00162-4. [DOI] [PubMed] [Google Scholar]
- Best EL, Sandoe JAT, Wilcox MH. Potential for aerosolization of Clostridium difficile after flushing toilets: The role of toilet lids in reducing environmental contamination risk. Journal of Hospital Infection. 2012;80(1):1–5. doi: 10.1016/j.jhin.2011.08.010. [DOI] [PubMed] [Google Scholar]
- Bloom E, Bal K, Nyman E, Must A, Larsson L. Mass spectrometry-based strategy for direct detection and quantification of some mycotoxins produced by Stachybotrys and Aspergillus spp. in indoor environments. Applied and Environmental Microbiology. 2007;73(13):4211–4217. doi: 10.1128/AEM.00343-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bone A, Murray V, Myers I, Dengel A, Crump D. Will drivers for home energy efficiency harm occupant health? Perspectives in Public Health. 2010;130(5):233–238. doi: 10.1177/1757913910369092. [DOI] [PubMed] [Google Scholar]
- Bornehag CG, Blomquist G, Gyntelberg F, Jarvholm B, Malmberg P, Nordvall L, Nielsen A, Pershagen G, Sundell J. Dampness in buildings and health. Indoor Air. 2001;11(2):72–86. doi: 10.1034/j.1600-0668.2001.110202.x. [DOI] [PubMed] [Google Scholar]
- Brasche S, Bullinger M, Morfeld M, Gebhardt HJ, Bischof W. Why do women suffer from sick building syndrome more often than men?–Subjective higher sensitivity versus objective causes. Indoor Air. 2001;11(4):217–222. doi: 10.1034/j.1600-0668.2001.110402.x. [DOI] [PubMed] [Google Scholar]
- Breda, L., Nozzi, M., De Sanctis, S., & Chiarelli, F. (2010). Laboratory tests in the diagnosis and follow-up of pediatric rheumatic diseases: An update. Seminars in Arthritis and Rheumatism, 40(1), 53–72. WB Saunders. [DOI] [PubMed]
- Brinke JT, Selvin S, Hodgson AT, Fisk WJ, Mendell MJ, Koshland CP, Daisey JM. Development of new volatile organic compound (VOC) exposure metrics and their relationship to “sick building syndrome” symptoms. Indoor Air. 1998;8(3):140–152. doi: 10.1111/j.1600-0668.1998.t01-1-00002.x. [DOI] [Google Scholar]
- Britton LA. Microbiological threats to health in the home. Clinical Lab Science. 2003;16:10–15. [PubMed] [Google Scholar]
- Burge H. (2006). How does heat affect fungi. The Environmental Reporter, 4(3).
- Burge S, Hedge A, Wilson S, Bass JH, Robertson A. Sick building syndrome: A study of 4373 office workers. The Annals of Occupational Hygiene. 1987;31(4A):493–504. doi: 10.1093/annhyg/31.4a.493. [DOI] [PubMed] [Google Scholar]
- Burton NC, Adhikari A, Iossifova Y, Grinshpun SA, Reponen T. Effect of gaseous chlorine dioxide on indoor microbial contaminants. Journal of the Air Waste Management Association. 2008;58:647–656. doi: 10.3155/1047-3289.58.5.647. [DOI] [PubMed] [Google Scholar]
- Cabral JPS. Can we use indoor fungi as bioindicators of indoor air quality? Historical perspectives and open questions. Science of the Total Environment. 2010;408:4285–4295. doi: 10.1016/j.scitotenv.2010.07.005. [DOI] [PubMed] [Google Scholar]
- Calderón-Garcidueñas L, Wen-Wang L, Zhang YJ, Rodriguez-Alcaraz A, Osnaya N, Villarreal-Calderón A, Santella RM. 8-hydroxy-2’-deoxyguanosine, a major mutagenic oxidative DNA lesion, and DNA strand breaks in nasal respiratory epithelium of children exposed to urban pollution. Environmental Health Perspectives. 1999;107(6):469. doi: 10.1289/ehp.107-1566580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carp O, Huisman CL, Reller A. Photoinduced reactivity of titanium dioxide. Progress in Solid State Chemistry. 2004;32(1):33–177. doi: 10.1016/j.progsolidstchem.2004.08.001. [DOI] [Google Scholar]
- Castro R, Angus DC, Rosengart MR. The effect of light on critical illness. Critical Care. 2011;15(2):218. doi: 10.1186/cc10000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cena K, de Dear RJ. Field study of occupant comfort and office thermal environments in a hot, arid climate. ASHRAE Transactions. 1999;105:204. [Google Scholar]
- Chan MT, Leung DY, Szefler SJ, Spahn JD. Difficult-to-control asthma: Clinical characteristics of steroid-insensitive asthma. Journal of Allergy and Clinical Immunology. 1998;101(5):594–601. doi: 10.1016/S0091-6749(98)70165-4. [DOI] [PubMed] [Google Scholar]
- Chatkin JM, Ansarin K, Silkoff PE, McCLEAN P, Gutierrez C, Zamel N, Chapman KR. Exhaled nitric oxide as a noninvasive assessment of chronic cough. American Journal of Respiratory and Critical Care Medicine. 1999;159(6):1810–1813. doi: 10.1164/ajrccm.159.6.9809047. [DOI] [PubMed] [Google Scholar]
- Chen C, Zhao B. Some questions on dispersion of human exhaled droplets in ventilation room: Answers from numerical investigation. Indoor Air. 2010;20(2):95–111. doi: 10.1111/j.1600-0668.2009.00626.x. [DOI] [PubMed] [Google Scholar]
- Chester AC, Levine PH. The natural history of concurrent sick building syndrome and chronic fatigue syndrome. Journal of Psychiatric Research. 1997;31(1):51–57. doi: 10.1016/S0022-3956(96)00054-4. [DOI] [PubMed] [Google Scholar]
- Choi J, Aziz A, Loftness V. Investigation on the impacts of different genders and ages on satisfaction with thermal environments in office buildings. Building and Environment. 2010;45(6):1529–1535. doi: 10.1016/j.buildenv.2010.01.004. [DOI] [Google Scholar]
- Clark RP, de Calcina-Goff ML. Some aspects of the airborne transmission of infection. Journal of the Royal Society, Interface. 2009;6(Suppl 6):S767–S782. doi: 10.1098/rsif.2009.0236.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clement J, Maes P, Ducoffre G, Van Loock F, Van Ranst M. Hantaviruses: Underestimated respiratory viruses? Clinical Infectious Diseases. 2008;46(3):477–479. doi: 10.1086/524896. [DOI] [PubMed] [Google Scholar]
- Coelho C, Steers M, Lutzler P, Schriver-Mazzuoli L. Indoor air pollution in old people’s homes related to some health problems: A survey study. Indoor Air. 2005;15(4):267–274. doi: 10.1111/j.1600-0668.2005.00371.x. [DOI] [PubMed] [Google Scholar]
- Cometto-Muniz JE, Cain WS. Physicochemical determinants and functional properties of the senses of irritation and smell. Indoor Air and Human Health. 1996;2:53–65. [Google Scholar]
- Craig, R., & Mindell, J. (2011). Health survey for England 2010. Respiratory health. London: NHS Information Centre.
- Cunha BA. Atypical pneumonias: current clinical concepts focusing on Legionnaires’ disease. Current Opinion in Pulmonary Medicine. 2008;14(3):183–194. doi: 10.1097/MCP.0b013e3282f79678. [DOI] [PubMed] [Google Scholar]
- Di Giulio M, Grande R, Di Campli E, Di Bartolomeo S, Cellini L. Indoor air quality in university environments. Environmental Monitoring and Assessment. 2010;170(1):509–517. doi: 10.1007/s10661-009-1252-7. [DOI] [PubMed] [Google Scholar]
- Doherty WO, Mousavioun P, Fellows CM. Value-adding to cellulosic ethanol: Lignin polymers. Industrial Crops and Products. 2011;33(2):259–276. doi: 10.1016/j.indcrop.2010.10.022. [DOI] [Google Scholar]
- Donnini G, Nguyen VH, Lai DHC, LaFlamme M, Haghighat F, Molina J, Lai HK, Martello C, Chang CY. Field study of occupant comfort and office thermal environments in a cold climate (No. CONF-970668–) ASHRAE Transactions. 1997;103:205–220. [Google Scholar]
- Drappatz J, Schiff D, Kesari S, Norden AD, Wen PY. Medical management of brain tumor patients. Neurologic Clinics. 2007;25(4):1035–1071. doi: 10.1016/j.ncl.2007.07.015. [DOI] [PubMed] [Google Scholar]
- Eames I, Shoaib D, Klettner CA, Taban V. Movement of airborne contaminants in a hospital isolation room. Journal of the Royal Society, Interface. 2009;6(Suppl 6):S757–S766. doi: 10.1098/rsif.2009.0319.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eder W, Ege MJ, von Mutius E. The asthma epidemic. New England Journal of Medicine. 2006;355(21):2226–2235. doi: 10.1056/NEJMra054308. [DOI] [PubMed] [Google Scholar]
- Eduard W. Fungal spores: A critical review of the toxicological and epidemiological evidence as a basis for occupational exposure limit setting. Critical Reviews in Toxicology. 2009;39(10):799–864. doi: 10.3109/10408440903307333. [DOI] [PubMed] [Google Scholar]
- Engelhart S, Loock A, Skutlarek D, Sagunski H, Lommel A, Färber H, Exner M. Occurrence of toxigenic Aspergillus versicolor isolates and sterigmatocystin in carpet dust from damp indoor environments. Applied and Environmental Microbiology. 2002;68(8):3886–3890. doi: 10.1128/AEM.68.8.3886-3890.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engvall K, Norrby C, Norbäck D. Sick building syndrome in relation to building dampness in multi-family residential buildings in Stockholm. International Archives of Occupational and Environmental Health. 2001;74(4):270–278. doi: 10.1007/s004200000218. [DOI] [PubMed] [Google Scholar]
- Erdmann CA, Apte MG. Mucous membrane and lower respiratory building related symptoms in relation to indoor carbon dioxide concentrations in the 100-building BASE dataset. Indoor Air. 2004;14(s8):127–134. doi: 10.1111/j.1600-0668.2004.00298.x. [DOI] [PubMed] [Google Scholar]
- Erkara IP, Asan A, Yilmaz V, Pehlivan S, Okten SS. Airborne Alternaria and Cladosporium species and relationship with meteorological conditions in Eskisehir City, Turkey. Environmental Monitoring and Assessment. 2008;144(1):31–41. doi: 10.1007/s10661-007-9939-0. [DOI] [PubMed] [Google Scholar]
- Everaert K, Baeyens J. Catalytic combustion of volatile organic compounds. Journal of Hazardous Materials. 2004;109(1):113–139. doi: 10.1016/j.jhazmat.2004.03.019. [DOI] [PubMed] [Google Scholar]
- Fanger PO. Introduction of the olf and the decipol units to quantify air pollution perceived by humans indoors and outdoors. Energy and Buildings. 1988;12(1):1–6. doi: 10.1016/0378-7788(88)90051-5. [DOI] [Google Scholar]
- Fehr R, Hurley F, Mekel OC, Mackenbach JP. Quantitative health impact assessment: taking stock and moving forward. Journal of Epidemiology and Community Health. 2012;66:1088–1091. doi: 10.1136/jech-2011-200835. [DOI] [PubMed] [Google Scholar]
- Fishwick D, Barber CM, Bradshaw LM, Harris-Roberts J, Francis M, Naylor S, Ayres J, Burge PS, Corne JM, Cullinan P, Frank TL. Standards of care for occupational asthma. Thorax. 2008;63(3):240–250. doi: 10.1136/thx.2007.083444. [DOI] [PubMed] [Google Scholar]
- Fisk WJ. Health and productivity gains from better indoor environments and their relationship with building energy efficiency. Annual Review of Energy and the Environment. 2000;25(1):537–566. doi: 10.1146/annurev.energy.25.1.537. [DOI] [Google Scholar]
- Fisk WJ, Lei-Gomez Q, Mendell MJ. Meta-analyses of the associations of respiratory health effects with dampness and mold in homes. Indoor Air. 2007;17(4):284–296. doi: 10.1111/j.1600-0668.2007.00475.x. [DOI] [PubMed] [Google Scholar]
- Fisk WJ, Mirer AG, Mendell MJ. Quantitative relationship of sick building syndrome symptoms with ventilation rates. Indoor Air. 2009;19(2):159–165. doi: 10.1111/j.1600-0668.2008.00575.x. [DOI] [PubMed] [Google Scholar]
- Foster AM, Swain MJ, Barrett R, D’agaro P, James SJ. Effectiveness and optimum jet velocity for a plane jet air curtain used to restrict cold room infiltration. International Journal of Refrigeration. 2006;29(5):692–699. doi: 10.1016/j.ijrefrig.2005.12.011. [DOI] [Google Scholar]
- Fournel I, Sautour M, Lafon I, Sixt N, L’ollivier C, Dalle F, Chavanet P, Couillaud G, Caillot D, Astruc K, Bonnin A. Airborne Aspergillus contamination during hospital construction works: Efficacy of protective measures. American Journal of Infection Control. 2010;38(3):189–194. doi: 10.1016/j.ajic.2009.07.011. [DOI] [PubMed] [Google Scholar]
- Franks TJ, Galvin JR. Hypersensitivity pneumonitis: Essential radiologic and pathologic findings. Surgical Pathology Clinics. 2010;3(1):187–198. doi: 10.1016/j.path.2010.03.005. [DOI] [PubMed] [Google Scholar]
- Fraser DW, Tsai TR, Orenstein W, Parkin WE, Beecham HJ, Sharrar RG, Harris J, Mallison GF, Martin SM, McDade JE, Shepard CC. Legionnaires’ disease: Description of an epidemic of pneumonia. New England Journal of Medicine. 1977;297(22):1189–1197. doi: 10.1056/NEJM197712012972201. [DOI] [PubMed] [Google Scholar]
- Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome: A comprehensive approach to its definition and study. Annals of Internal Medicine. 1994;121(12):953–959. doi: 10.7326/0003-4819-121-12-199412150-00009. [DOI] [PubMed] [Google Scholar]
- Gillespie NC, Lewis RJ, Pearn JH, Bourke A, Holmes MJ, Bourke JB, Shields WJ. Ciguatera in Australia. Occurrence, clinical features, pathophysiology and management. The Medical Journal of Australia. 1986;145(11–12):584–590. [PubMed] [Google Scholar]
- Gilmour MI, Jaakkola MS, London SJ, Nel AE, Rogers CA. How exposure to environmental tobacco smoke, outdoor air pollutants, and increased pollen burdens influences the incidence of asthma. Environmental Health Perspectives. 2006;114(4):627. doi: 10.1289/ehp.8380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godish T, Spengler JD. Relationships between ventilation and indoor air quality: A review. Indoor Air. 1996;6(2):135–145. doi: 10.1111/j.1600-0668.1996.00010.x. [DOI] [Google Scholar]
- Górny RL. Filamentous microorganisms and their fragments in indoor air–A review. Annals of Agricultural and Environmental Medicine: AAEM. 2004;11(2):185–197. [PubMed] [Google Scholar]
- Gottschalk C, Bauer J, Meyer K. Determination of macrocyclic trichothecenes in mouldy indoor materials by LC-MS/MS. Mycotoxin Research. 2006;22(3):189–192. doi: 10.1007/BF02959275. [DOI] [PubMed] [Google Scholar]
- Gralton J, Tovey E, McLaws ML, Rawlinson WD. The role of particle size in aerosolised pathogen transmission: A review. Journal of Infection. 2011;62(1):1–13. doi: 10.1016/j.jinf.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graudenz GS, Oliveira CH, Tribess A, Mendes C, Latorre MRDO, Kalil J. Association of air-conditioning with respiratory symptoms in office workers in tropical climate. Indoor Air. 2005;15(1):62–66. doi: 10.1111/j.1600-0668.2004.00324.x. [DOI] [PubMed] [Google Scholar]
- Greig JD, Lee MB. A review of nosocomial norovirus outbreaks: Infection control interventions found effective. Epidemiology and Infection. 2012;140(7):1151–1160. doi: 10.1017/S0950268811002731. [DOI] [PubMed] [Google Scholar]
- Guo H. Source apportionment of Volatile organic compounds in Hong Kong homes. Building and Environment. 2011;46(11):2280–2286. doi: 10.1016/j.buildenv.2011.05.008. [DOI] [Google Scholar]
- Gupta S, Khare M, Goyal R. Sick building syndrome—A case study in a multistory centrally air-conditioned building in the Delhi City. Building and Environment. 2007;42(8):2797–2809. doi: 10.1016/j.buildenv.2006.10.013. [DOI] [Google Scholar]
- Haley RW, Kurt TL, Hom J. Is there a Gulf war syndrome?: Searching for syndromes by factor analysis of symptoms. JAMA. 1997;277(3):215–222. doi: 10.1001/jama.1997.03540270041025. [DOI] [PubMed] [Google Scholar]
- Halios CH, Helmis CG. Temporal evolution of the main processes that control indoor pollution in an office microenvironment: A case study. Environmental Monitoring and Assessment. 2010;167(1):199–217. doi: 10.1007/s10661-009-1043-1. [DOI] [PubMed] [Google Scholar]
- Hamblin MR, Viveiros J, Yang C, Ahmadi A, Ganz RA, Tolkoff MJ. Helicobacter pylori accumulates photoactive porphyrins and is killed by visible light. Antimicrobial Agents and Chemotherapy. 2005;49(7):2822–2827. doi: 10.1128/AAC.49.7.2822-2827.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinrich J. Influence of indoor factors in dwellings on the development of childhood asthma. International Journal of Hygiene and Environmental Health. 2011;214(1):1–25. doi: 10.1016/j.ijheh.2010.08.009. [DOI] [PubMed] [Google Scholar]
- Hengpraprom, S., Onopparatwibul, V., Chindaporn, A., Sithisarankul, P. (2010). Indoor air quality and allergic rhinitis among office workers in a high-rise building. Journal of Environmental Health Research, 12.
- Herfst S, Schrauwen EJ, Linster M, Chutinimitkul S, de Wit E, Munster VJ, Sorrell EM, Bestebroer TM, Burke DF, Smith DJ, Rimmelzwaan GF. Airborne transmission of influenza A/H5N1 virus between ferrets. Science. 2012;336(6088):1534–1541. doi: 10.1126/science.1213362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoang CP, Kinney KA, Corsi RL, Szaniszlo PJ. Resistance of green building materials to fungal growth. International Biodeterioration and Biodegradation. 2010;64(2):104–113. doi: 10.1016/j.ibiod.2009.11.001. [DOI] [Google Scholar]
- Hobday, R. (2011). Indoor environmental quality in refurbishment. Historic Scotland Technical Paper, 12. Edinburgh
- Hobday RA, Dancer SJ. Roles of sunlight and natural ventilation for controlling infection: historical and current perspectives. Journal of Hospital Infection. 2013;84(4):271–282. doi: 10.1016/j.jhin.2013.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hood AM. The effect of open-air factors on the virulence and viability of airborne Francisella tularensis. Epidemiology and Infection. 2009;137(6):753–761. doi: 10.1017/S0950268809002076. [DOI] [PubMed] [Google Scholar]
- Horner WE, Worthan AG, Morey PR. Air-and dustborne mycoflora in houses free of water damage and fungal growth. Applied and Environmental Microbiology. 2004;70(11):6394–6400. doi: 10.1128/AEM.70.11.6394-6400.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huttunen K, Pelkonen J, Nielsen KF, Nuutinen U, Jussila J, Hirvonen MR. Synergistic interaction in simultaneous exposure to Streptomyces californicus and Stachybotrys chartarum. Environmental Health Perspectives. 2004;112(6):659. doi: 10.1289/ehp.6701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaakkola, J. J., & Jaakkola, M. S. (2002). Effects of environmental tobacco smoke on the respiratory health of children. Scandinavian Journal of Work, Environment & Health, 71–83. [PubMed]
- Jaakkola MS, Jaakkola JJ. Office work exposures and adult-onset asthma. Environmental Health Perspectives. 2007;115(7):1007–1011. doi: 10.1289/ehp.9875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaakkola JJ, Knight TL. The role of exposure to phthalates from polyvinyl chloride products in the development of asthma and allergies: A systematic review and meta-analysis. Environmental Health Perspectives. 2008;116(7):845. doi: 10.1289/ehp.10846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaakkola JJ, Miettinen P. Ventilation rate in office buildings and sick building syndrome. Occupational and Environmental Medicine. 1995;52(11):709–714. doi: 10.1136/oem.52.11.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaakkola JJ, Piipari R, Jaakkola MS. Occupation and asthma: A population-based incident case-control study. American Journal of Epidemiology. 2003;158(10):981–987. doi: 10.1093/aje/kwg238. [DOI] [PubMed] [Google Scholar]
- Jaakkola JJ, Ieromnimon A, Jaakkola MS. Interior surface materials and asthma in adults: A population-based incident case-control study. American Journal of Epidemiology. 2006;164(8):742–749. doi: 10.1093/aje/kwj249. [DOI] [PubMed] [Google Scholar]
- Jaakkola MS, Yang L, Ieromnimon A, Jaakkola JJ. Office work exposures and respiratory and sick building syndrome symptoms. Occupational and Environmental Medicine. 2007;64(3):178–184. doi: 10.1136/oem.2005.024596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jo, W. K. (2011). Bioaerosols in apartment buildings. Encyclopedia of Environmental Health (pp. 323–330).
- Jovanovic S, Felder-Kennel A, Gabrio T, Kouros B, Link B, Maisner V, Piechotowski I, Schick KH, Schrimpf M, Weidner U, Zöllner I. Indoor fungi levels in homes of children with and without allergy history. International Journal of Hygiene and Environmental Health. 2004;207(4):369–378. doi: 10.1078/1438-4639-00302. [DOI] [PubMed] [Google Scholar]
- Jung JH, Lee JE, Bae GN. Real-time measurement of UV-inactivated Escherichia coli bacterial particles by electrospray-assisted UVAPS spectrometry. Science of the Total Environment. 2011;409(17):3249–3255. doi: 10.1016/j.scitotenv.2011.05.005. [DOI] [PubMed] [Google Scholar]
- Kalyoncu F. Relationship between airborne fungal allergens and meteorological factors in Manisa City, Turkey. Environmental Monitoring and Assessment. 2010;165(1–4):553–558. doi: 10.1007/s10661-009-0966-x. [DOI] [PubMed] [Google Scholar]
- Karjalainen S. Gender differences in thermal comfort and use of thermostats in everyday thermal environments. Building and Environment. 2007;42(4):1594–1603. doi: 10.1016/j.buildenv.2006.01.009. [DOI] [Google Scholar]
- Kawel N, Schorer G, Desbiolles L, Seifert B, Marincek B, Boehm T. Discrimination between invasive pulmonary aspergillosis and pulmonary lymphoma using CT. European Journal of Radiology. 2011;77(3):417–425. doi: 10.1016/j.ejrad.2009.09.018. [DOI] [PubMed] [Google Scholar]
- Kembel SW, Jones E, Kline J, Northcutt D, Stenson J, Womack AM, Bohannan BJ, Brown GZ, Green JL. Architectural design influences the diversity and structure of the built environment microbiome. The ISME Journal. 2012;6(8):1469–1479. doi: 10.1038/ismej.2011.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr, K. G. (2010). Controlling methicillin-resistant staphylococcus aureus infection in hospitals. European Critical Care & Emergency Medicine, 2.
- Khan AH, Karuppayil SM. Fungal pollution of indoor environments and its management. Saudi Journal of Biological Sciences. 2012;19(4):405–426. doi: 10.1016/j.sjbs.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kildesø J, Würtz H, Nielsen KF, Kruse P, Wilkins K, Thrane U, Gravesen S, Nielsen PA, Schneider T. Determination of fungal spore release from wet building materials. Indoor Air. 2003;13(2):148–155. doi: 10.1034/j.1600-0668.2003.00172.x. [DOI] [PubMed] [Google Scholar]
- Kim J, de Dear R, Candido C, Zhang H, Arens E. Gender differences in office occupant perception of indoor environmental quality (IEQ) Building and Environment. 2013;70:245–256. doi: 10.1016/j.buildenv.2013.08.022. [DOI] [Google Scholar]
- Kimmel M, Braun N, Alscher DM. Should we recommend precautions during a hantavirus endemic? NDT Plus. 2010;3(4):424–426. doi: 10.1093/ndtplus/sfq093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korpi A, Järnberg J, Pasanen AL. Microbial volatile organic compounds. Critical Reviews in Toxicology. 2009;39(2):139–193. doi: 10.1080/10408440802291497. [DOI] [PubMed] [Google Scholar]
- Landrigan PJ. Illness in Gulf war veterans: Causes and consequences. JAMA. 1997;277(3):259–261. doi: 10.1001/jama.1997.03540270085031. [DOI] [PubMed] [Google Scholar]
- Lanier C, Richard E, Heutte N, Picquet R, Bouchart V, Garon D. Airborne molds and mycotoxins associated with handling of corn silage and oilseed cakes in agricultural environment. Atmospheric Environment. 2010;44(16):1980–1986. doi: 10.1016/j.atmosenv.2010.02.040. [DOI] [Google Scholar]
- Laumbach, R. J. (2008). Sick building syndrome. Intern Encyclopedia Public Health, 4–8.
- Lee MG, Li S, Jarvis BB, Pestka JJ. Effects of satratoxins and other macrocyclic trichothecenes on IL-2 production and viability of EL-4 thymoma cells. Journal of Toxicology and Environmental Health, Part A. 1999;57(7):459–474. doi: 10.1080/009841099157548. [DOI] [PubMed] [Google Scholar]
- Li Y, Leung GM, Tang JW, Yang X, Chao CYH, Lin JZ, Lu JW, Nielsen PV, Niu J, Qian H, Sleigh AC. Role of ventilation in airborne transmission of infectious agents in the built environment–A multidisciplinary systematic review. Indoor Air. 2007;17(1):2–18. doi: 10.1111/j.1600-0668.2006.00445.x. [DOI] [PubMed] [Google Scholar]
- Li A, Liu Z, Zhu X, Liu Y, Wang Q. The effect of air-conditioning parameters and deposition dust on microbial growth in supply air ducts. Energy and Buildings. 2010;42(4):449–454. doi: 10.1016/j.enbuild.2009.10.013. [DOI] [Google Scholar]
- Liu W, Ji J, Chen H, Ye C. Optimal color design of psychological counseling room by design of experiments and response surface methodology. PLoS ONE. 2014;9(3):e90646. doi: 10.1371/journal.pone.0090646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwhagen O, Ellbjär S, Jörgensen N. Asthma or asthma-like condition? Nordisk Medicin. 1997;112(4):119–121. [PubMed] [Google Scholar]
- Lu CY, Ma YC, Lin JM, Chuang CY, Sung FC. Oxidative DNA damage estimated by urinary 8-hydroxydeoxyguanosine and indoor air pollution among non-smoking office employees. Environmental Research. 2007;103(3):331–337. doi: 10.1016/j.envres.2006.08.009. [DOI] [PubMed] [Google Scholar]
- Lugauskas A, Krikštaponis A. Filamentous fungi isolated in hospitals and some medical institutions in Lithuania. Indoor and Built Environment. 2004;13(2):101–108. doi: 10.1177/1420326X04040936. [DOI] [Google Scholar]
- Lugauskas A, Levinskaite L, Peciulyte D. Micromycetes as deterioration agents of polymeric materials. International Biodeterioration Biodegradation. 2003;52(4):233–242. doi: 10.1016/S0964-8305(03)00110-0. [DOI] [Google Scholar]
- Maclean M, MacGregor SJ, Anderson JG, Woolsey GA, Coia JE, Hamilton K, Taggart I, Watson SB, Thakker B, Gettinby G. Environmental decontamination of a hospital isolation room using high-intensity narrow-spectrum light. Journal of Hospital Infection. 2010;76(3):247–251. doi: 10.1016/j.jhin.2010.07.010. [DOI] [PubMed] [Google Scholar]
- Marmot AF, Eley J, Stafford M, Stansfeld SA, Warwick E, Marmot MG. Building health: An epidemiological study of “sick building syndrome” in the Whitehall II study. Occupational and Environmental Medicine. 2006;63(4):283–289. doi: 10.1136/oem.2005.022889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall JA, Bruggink LD. The dynamics of norovirus outbreak epidemics: Recent insights. International Journal of Environmental Research and Public Health. 2011;8(4):1141–1149. doi: 10.3390/ijerph8041141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez K, Rao C, Burton N. Exposure assessment and analysis for biological agents. Grana. 2004;43(4):193–208. doi: 10.1080/00173130410000794. [DOI] [Google Scholar]
- Matysik S, Herbarth O, Mueller A. Determination of volatile metabolites originating from mould growth on wall paper and synthetic media. Journal of Microbiological Methods. 2008;75(2):182–187. doi: 10.1016/j.mimet.2008.05.027. [DOI] [PubMed] [Google Scholar]
- Matysik S, Herbarth O, Mueller A. Determination of microbial volatile organic compounds (MVOCs) by passive sampling onto charcoal sorbents. Chemosphere. 2009;76(1):114–119. doi: 10.1016/j.chemosphere.2009.02.010. [DOI] [PubMed] [Google Scholar]
- McDonnell G, Burke P. Disinfection: Is it time to reconsider Spaulding? Journal of Hospital Infection. 2011;78(3):163–170. doi: 10.1016/j.jhin.2011.05.002. [DOI] [PubMed] [Google Scholar]
- McKernan LT, Wallingford KM, Hein MJ, Burge H, Rogers CA, Herrick R. Monitoring microbial populations on wide-body commercial passenger aircraft. Annals of Occupational Hygiene. 2008;52(2):139–149. doi: 10.1093/annhyg/mem068. [DOI] [PubMed] [Google Scholar]
- McKinney KR, Gong YY, Lewis TG. Environmental transmission of SARS at Amoy Gardens. Journal of Environmental Health. 2006;68(9):26–30. [PubMed] [Google Scholar]
- Meklin T, Hyvärinen A, Toivola M, Reponen T, Koponen V, Husman T, Taskinen T, Korppi M, Nevalainen A. Effect of building frame and moisture damage on microbiological indoor air quality in school buildings. Aiha Journal. 2003;64(1):108–116. doi: 10.1080/15428110308984800. [DOI] [PubMed] [Google Scholar]
- Mendell MJ, Heath GA. Do indoor pollutants and thermal conditions in schools influence student performance? A critical review of the literature. Indoor Air. 2005;15(1):27–52. doi: 10.1111/j.1600-0668.2004.00320.x. [DOI] [PubMed] [Google Scholar]
- Mendell MJ, Fisk WJ, Kreiss K, Levin H, Alexander D, Cain WS, Girman JR, Hines CJ, Jensen PA, Milton DK, Rexroat LP. Improving the health of workers in indoor environments: priority research needs for a national occupational research agenda. American Journal of Public Health. 2002;92(9):1430–1440. doi: 10.2105/AJPH.92.9.1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendell MJ, Naco GM, Wilcox TG, Sieber WK. Environmental risk factors and work-related lower respiratory symptoms in 80 office buildings: An exploratory analysis of NIOSH data. American Journal of Industrial Medicine. 2003;43(6):630–641. doi: 10.1002/ajim.10211. [DOI] [PubMed] [Google Scholar]
- Mendell MJ, Cozen M, Lei-Gomez Q, Brightman HS, Erdmann CA, Girman JR, Womble SE. Indicators of moisture and ventilation system contamination in US office buildings as risk factors for respiratory and mucous membrane symptoms: Analyses of the EPA BASE data. Journal of Occupational and Environmental Hygiene. 2006;3(5):225–233. doi: 10.1080/15459620600628589. [DOI] [PubMed] [Google Scholar]
- Mendell MJ, Eliseeva EA, Davies MM, Spears M, Lobscheid A, Fisk WJ, Apte MG. Association of classroom ventilation with reduced illness absence: A prospective study in California elementary schools. Indoor Air. 2013;23(6):515–528. doi: 10.1111/ina.12042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menetrez MY, Foarde KK. Research and development of prevention and control measures for mold contamination. Indoor and Built Environment. 2004;13(2):109–114. doi: 10.1177/1420326X04040612. [DOI] [Google Scholar]
- Mesa-Frias M, Chalabi Z, Foss AM. Quantifying uncertainty in health impact assessment: A case-study example on indoor housing ventilation. Environment International. 2014;62:95–103. doi: 10.1016/j.envint.2013.10.007. [DOI] [PubMed] [Google Scholar]
- Millqvist E, Löwhagen O. Methacholine provocations do not reveal sensitivity to strong scents. Annals of Allergy, Asthma & Immunology. 1998;80(5):381–384. doi: 10.1016/S1081-1206(10)62987-0. [DOI] [PubMed] [Google Scholar]
- Millqvist E, Bende M, Löwhagen O. Sensory hyperreactivity–A possible mechanism underlying cough and asthma-like symptoms. Allergy. 1998;53(12):1208–1212. doi: 10.1111/j.1398-9995.1998.tb03843.x. [DOI] [PubMed] [Google Scholar]
- Milton DK, Glencross PM, Walters MD. Risk of sick leave associated with outdoor air supply rate, humidification, and occupant complaints. Indoor Air. 2000;10(4):212–221. doi: 10.1034/j.1600-0668.2000.010004212.x. [DOI] [PubMed] [Google Scholar]
- Mitchell CS, Zhang JJ, Sigsgaard T, Jantunen M, Lioy PJ, Samson R, Karol MH. Current state of the science: Health effects and indoor environmental quality. Environmental Health Perspectives. 2007;115(6):958–964. doi: 10.1289/ehp.8987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizoue T, Reijula K, Andersson K. Environmental tobacco smoke exposure and overtime work as risk factors for sick building syndrome in Japan. American Journal of Epidemiology. 2001;154(9):803–808. doi: 10.1093/aje/154.9.803. [DOI] [PubMed] [Google Scholar]
- Mølhave L. Volatile organic compounds and sick building syndrome. In: Lippmann M, editor. Environmental toxicants: Human exposures and their health effects. 3. New York: Wiley; 2008. pp. 241–256. [Google Scholar]
- Mølhave, L. (2011). Sick building syndrome. Encyclopedia of Environmental Health (pp. 61–67). Elsevier.
- Morey, P., Worthan, A., Weber, A., Horner, E., Black, M., & Muller, W. (1997). Microbial VOCs in moisture damaged buildings. In IAQ Proceedings of Healthy Buildings (pp. 245–250).
- Moularat, S., Robine, E., Ramalho, O., & Oturan, M. A. (2008a). Detection of fungal development in closed spaces through the determination of specific chemical targets. Chemosphere, 72(2), 224–232. [DOI] [PubMed]
- Moularat, S., Robine, E., Ramalho, O., & Oturan, M. A. (2008b). Detection of fungal development in a closed environment through the identification of specific VOC: demonstration of a specific VOC fingerprint for fungal development. Science of the Total Environment, 407(1), 139–146. [DOI] [PubMed]
- Moularat S, Hulin M, Robine E, Annesi-Maesano I, Caillaud D. Airborne fungal volatile organic compounds in rural and urban dwellings: Detection of mould contamination in 94 homes determined by visual inspection and airborne fungal volatile organic compounds method. Science of the Total Environment. 2011;409(11):2005–2009. doi: 10.1016/j.scitotenv.2011.02.033. [DOI] [PubMed] [Google Scholar]
- Muise B, Seo DC, Blair EE, Applegate T. Mold spore penetration through wall service outlets: A pilot study. Environmental Monitoring and Assessment. 2010;163(1):95–104. doi: 10.1007/s10661-009-0819-7. [DOI] [PubMed] [Google Scholar]
- Murtoniemi T, Nevalainen A, Hirvonen MR. Effect of plasterboard composition on Stachybotrys chartarum growth and biological activity of spores. Applied and Environmental Microbiology. 2003;69(7):3751–3757. doi: 10.1128/AEM.69.7.3751-3757.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myatt TA, Johnston SL, Zuo Z, Wand M, Kebadze T, Rudnick S, Milton DK. Detection of airborne rhinovirus and its relation to outdoor air supply in office environments. American Journal of Respiratory and Critical Care Medicine. 2004;169(11):1187–1190. doi: 10.1164/rccm.200306-760OC. [DOI] [PubMed] [Google Scholar]
- Nag A, Nag PK. Do the work stress factors of women telephone operators change with the shift schedules? International Journal of Industrial Ergonomics. 2004;33(5):449–461. doi: 10.1016/j.ergon.2003.11.004. [DOI] [Google Scholar]
- Nakano J, Tanabe SI, Kimura KI. Differences in perception of indoor environment between Japanese and non-Japanese workers. Energy and Buildings. 2002;34(6):615–621. doi: 10.1016/S0378-7788(02)00012-9. [DOI] [Google Scholar]
- Nielsen KF. Mycotoxin production by indoor molds. Fungal Genetics and Biology. 2003;39(2):103–117. doi: 10.1016/S1087-1845(03)00026-4. [DOI] [PubMed] [Google Scholar]
- Nielsen PV. Control of airborne infectious diseases in ventilated spaces. Journal of the Royal Society Interface. 2009;6(Suppl 6):S747–S755. doi: 10.1098/rsif.2009.0228.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nieminen SM, Kärki R, Auriola S, Toivola M, Laatsch H, Laatikainen R, Hyvärinen A, von Wright A. Isolation and identification of Aspergillus fumigatus mycotoxins on growth medium and some building materials. Applied and Environmental Microbiology. 2002;68(10):4871–4875. doi: 10.1128/AEM.68.10.4871-4875.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nino E, Fasanella R, Di Tommaso RM. Submerged rectangular air jets as a particulate barrier. Building and Environment. 2011;46(11):2375–2386. doi: 10.1016/j.buildenv.2011.05.020. [DOI] [Google Scholar]
- Nordström K, Norbäck D, Akselsson R. Effect of air humidification on the sick building syndrome and perceived indoor air quality in hospitals: A four month longitudinal study. Occupational and Environmental Medicine. 1994;51(10):683–688. doi: 10.1136/oem.51.10.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norhidayah, A., Chia-Kuang, L., Azhar, M. K., & Nurulwahida, S. (2013). Indoor air quality and sick building syndrome in three selected buildings. In Malaysian Technical Universities Conference on Engineering & Technology 2012, MUCET 2012 Part 3—Civil and Chemical Engineering; Procedia Engineering, 53, 93–98.
- Ooi PL, Goh KT, Phoon MH, Foo SC, Yap HM. Epidemiology of sick building syndrome and its associated risk factors in Singapore. Occupational and Environmental Medicine. 1998;55(3):188–193. doi: 10.1136/oem.55.3.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortíz-Castro R, Contreras-Cornejo HA, Macías-Rodríguez L, López-Bucio J. The role of microbial signals in plant growth and development. Plant Signaling & Behavior. 2009;4(8):701–712. doi: 10.4161/psb.4.8.9047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pal TM, de Monchy JGR, Groothoff JW, Post D. Exposure and acute exposure-effects before and after modification of a contaminated humidification system in a synthetic-fibre plant. International Archives of Occupational and Environmental Health. 2000;73(6):369–375. doi: 10.1007/s004200000131. [DOI] [PubMed] [Google Scholar]
- Pearn J. Ciguatera-a potent cause of the chronic fatigue syndrome. EOS J Immunol Immunopathol. 1995;5:63–65. [Google Scholar]
- Phares CR, Russell E, Thigpen MC, Service W, Crist MB, Salyers M, Engel J, Benson RF, Fields B, Moore MR. Legionnaires’ disease among residents of a long-term care facility: The sentinel event in a community outbreak. American Journal of Infection Control. 2007;35(5):319–323. doi: 10.1016/j.ajic.2006.09.014. [DOI] [PubMed] [Google Scholar]
- Pizzigallo E, Racciatti D, Vecchiet J. Clinical and pathophysiological aspects of chronic fatigue syndrome. Journal of Musculoskeletal Pain. 1999;7(1–2):217–224. doi: 10.1300/J094v07n01_20. [DOI] [Google Scholar]
- Radon K, Gerhardinger U, Schulze A, Zock JP, Norback D, Toren K, Jarvis D, Held L, Heinrich J, Leynaert B, Nowak D. Occupation and adult onset of rhinitis in the general population. Occupational and Environmental Medicine. 2008;65(1):38–43. doi: 10.1136/oem.2006.031542. [DOI] [PubMed] [Google Scholar]
- Ramazzini, B. (1713). The Diseases of Workers. Translated by W. Wright, (With a Portrait), 1940. Chicago, University of Chicago Press; Latin Text: De Morbis Artificum Bernardini Ramazzini Diatriba.
- Reijula K, Sundman-Digert C. Assessment of indoor air problems at work with a questionnaire. Occupational and Environmental Medicine. 2004;61(1):33–38. [PMC free article] [PubMed] [Google Scholar]
- Rene E, Montes M, Veiga MC, Kennes C. Biotreatment of gas-phase VOC mixtures from fibreglass and composite manufacturing industry. Journal of Biotechnology. 2010;150(1):218–219. doi: 10.1016/j.jbiotec.2010.09.043. [DOI] [PubMed] [Google Scholar]
- Reponen, T. (2011). Methodologies for assessing bioaerosol exposures. Encyclopedia of environmental health (pp. 722–730).
- Reponen T, Seo SC, Grimsley F, Lee T, Crawford C, Grinshpun SA. Fungal fragments in moldy houses: a field study in homes in New Orleans and Southern Ohio. Atmospheric Environment. 2007;41(37):8140–8149. doi: 10.1016/j.atmosenv.2007.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reponen T, Singh U, Schaffer C, Vesper S, Johansson E, Adhikari A, Grinshpun SA, Indugula R, Ryan P, Levin L, LeMasters G. Visually observed mold and moldy odor versus quantitatively measured microbial exposure in homes. Science of the Total Environment. 2010;408(22):5565–5574. doi: 10.1016/j.scitotenv.2010.07.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds SJ, Black DW, Borin SS, Breuer G, Burmeister LF, Fuortes LJ, Smith TF, Stein MA, Subramanian P, Thorne PS, Whitten P. Indoor environmental quality in six commercial office buildings in the midwest United States. Applied Occupational and Environmental Hygiene. 2001;16(11):1065–1077. doi: 10.1080/104732201753214170. [DOI] [PubMed] [Google Scholar]
- Richards AL, Hyams KC, Watts DM, Rozmajzl PJ, Woody JN, Merrell BR. Respiratory disease among military personnel in Saudi Arabia during Operation Desert Shield. American Journal of Public Health. 1993;83(9):1326–1329. doi: 10.2105/AJPH.83.9.1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ringsberg KC, Åkerlind I. Presence of hyperventilation in patients with asthma-like symptoms but negative asthma test responses: Provocation with voluntary hyperventilation and mental stress. Journal of Allergy and Clinical Immunology. 1999;103(4):601–608. doi: 10.1016/S0091-6749(99)70231-9. [DOI] [PubMed] [Google Scholar]
- Ringsberg KC, Wetterqvist H, Löwhagen O, Sivik T. Physical capacity and dyspnea in patients with asthma-like symptoms but negative asthma tests. Allergy. 1997;52(5):532–540. doi: 10.1111/j.1398-9995.1997.tb02596.x. [DOI] [PubMed] [Google Scholar]
- Roark SE, Cabrera-Fonseca J, Milazzo MC, White JH, Wander JD. Catalytic oxidation of volatile organic liquids. Journal of Environmental Engineering. 2004;130(3):329–337. doi: 10.1061/(ASCE)0733-9372(2004)130:3(329). [DOI] [Google Scholar]
- Robertson W, Robertson AS, Burge CB, Moore VC, Jaakkola MS, Dawkins PA, Burd M, Rawbone R, Gardner I, Kinoulty M, Crook B. Clinical investigation of an outbreak of alveolitis and asthma in a car engine manufacturing plant. Thorax. 2007;62(11):981–990. doi: 10.1136/thx.2006.072199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Runeson R, Norbäck D, Stattin H. Symptoms and sense of coherence–A follow-up study of personnel from workplace buildings with indoor air problems. International Archives of Occupational and Environmental Health. 2003;76(1):29–38. doi: 10.1007/s00420-002-0372-y. [DOI] [PubMed] [Google Scholar]
- Runeson R, Wahlstedt K, Wieslander G, Norbäck D. Personal and psychosocial factors and symptoms compatible with sick building syndrome in the Swedish workforce. Indoor Air. 2006;16(6):445–453. doi: 10.1111/j.1600-0668.2006.00438.x. [DOI] [PubMed] [Google Scholar]
- Rylander R. Organic dust induced pulmonary disease-the role of mould derived beta-glucan. Annals of Agricultural and Environmental Medicine. 2010;17(1):9–13. [PubMed] [Google Scholar]
- Saijo Y, Nakagi Y, Ito T, Sugioka Y, Endo H, Yoshida T. Relation of dampness to sick building syndrome in Japanese public apartment houses. Environmental Health and Preventive Medicine. 2009;14(1):26–35. doi: 10.1007/s12199-008-0052-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sailer MF, van Nieuwenhuijzen EJ, Knol W. Forming of a functional biofilm on wood surfaces. Ecological Engineering. 2010;36(2):163–167. doi: 10.1016/j.ecoleng.2009.02.004. [DOI] [Google Scholar]
- Salo PM, Yin M, Arbes SJ, Cohn RD, Sever M, Muilenberg M, Burge HA, London SJ, Zeldin DC. Dustborne alternaria alternata antigens in US homes: Results from the National Survey of Lead and Allergens in Housing. Journal of Allergy and Clinical Immunology. 2005;116(3):623–629. doi: 10.1016/j.jaci.2005.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salthammer T. Emission of volatile organic compounds from furniture coatings. Indoor Air. 1997;7(3):189–197. doi: 10.1111/j.1600-0668.1997.t01-1-00004.x. [DOI] [Google Scholar]
- Sarwar, G., Corsi, R., Allen, D., & Weschler, C. (2002). Production an levels of selected indoor radicals: A modeling assessment. In Proceedings of Indoor Air, The Ninth International Conference on Indoor Air Quality and Climate, June 2002 (pp. 189–197).
- Schleibinger H, Laussmann D, Bornehag CG, Eis D, Rueden H. Microbial volatile organic compounds in the air of moldy and mold-free indoor environments. Indoor Air. 2008;18(2):113–124. doi: 10.1111/j.1600-0668.2007.00513.x. [DOI] [PubMed] [Google Scholar]
- Schmier JK, Leidy NK. The complexity of treatment adherence in adults with asthma: Challenges and opportunities. Journal of Asthma. 1998;35(6):455–472. doi: 10.3109/02770909809070999. [DOI] [PubMed] [Google Scholar]
- Schneider WJ, Furth PA, Blalock TH, Sherrill TA. A pilot study of a headache program in the workplace: The effect of education. Journal of Occupational and Environmental Medicine. 1999;41(3):202–209. doi: 10.1097/00043764-199903000-00010. [DOI] [PubMed] [Google Scholar]
- Schwartz BS, Stewart WF, Simon D, Lipton RB. Epidemiology of tension-type headache. Jama. 1998;279(5):381–383. doi: 10.1001/jama.279.5.381. [DOI] [PubMed] [Google Scholar]
- Seepana S, Lai AC. Experimental and numerical investigation of interpersonal exposure of sneezing in a full-scale chamber. Aerosol Science and Technology. 2012;46(5):485–493. doi: 10.1080/02786826.2011.640365. [DOI] [Google Scholar]
- Selvamurthy, W., Ray, U. S., Tiwary, R. S., Singh, A. P., & Ranganathan, S. (1996). Psychogenic mass illness—A case study in Calcutta telephones. In P. K. Nag (Ed.), Ergonomics and work design: Emerging issues in organizational sciences (pp. 332–347).
- Sen B, Asan A. Fungal flora in indoor and outdoor air of different residential houses in Tekirdag City (Turkey): Seasonal distribution and relationship with climatic factors. Environmental Monitoring and Assessment. 2009;151(1):209–219. doi: 10.1007/s10661-008-0262-1. [DOI] [PubMed] [Google Scholar]
- Seo SC, Reponen T, Levin L, Grinshpun SA. Size-fractionated (1 → 3)-β-D-glucan concentrations aerosolized from different moldy building materials. Science of the Total Environment. 2009;407(2):806–814. doi: 10.1016/j.scitotenv.2008.10.018. [DOI] [PubMed] [Google Scholar]
- Seppänen OA, Fisk WJ. Summary of human responses to ventilation. Indoor Air. 2004;14(s7):102–118. doi: 10.1111/j.1600-0668.2004.00279.x. [DOI] [PubMed] [Google Scholar]
- Seppänen OA, Fisk WJ, Mendell MJ. Association of ventilation rates and CO2 concentrations with health and other responses in commercial and institutional buildings. Indoor Air. 1999;9(4):226–252. doi: 10.1111/j.1600-0668.1999.00003.x. [DOI] [PubMed] [Google Scholar]
- Seppänen O, Fisk WJ, Lei QH. Ventilation and performance in office work. Indoor Air. 2006;16(1):28–36. doi: 10.1111/j.1600-0668.2005.00394.x. [DOI] [PubMed] [Google Scholar]
- Shinoj S, Visvanathan R, Panigrahi S, Kochubabu M. Oil palm fiber (OPF) and its composites: A review. Industrial Crops and Products. 2011;33(1):7–22. doi: 10.1016/j.indcrop.2010.09.009. [DOI] [Google Scholar]
- Shirakawa MA, Loh K, John VM, Silva MES, Gaylarde CC. Biodeterioration of painted mortar surfaces in tropical urban and coastal situations: Comparison of four paint formulations. International Biodeterioration & Biodegradation. 2011;65(5):669–674. doi: 10.1016/j.ibiod.2011.03.004. [DOI] [Google Scholar]
- Shoemaker RC, House DE. A time-series study of sick building syndrome: Chronic, biotoxin-associated illness from exposure to water-damaged buildings. Neurotoxicology and Teratology. 2005;27(1):29–46. doi: 10.1016/j.ntt.2004.07.005. [DOI] [PubMed] [Google Scholar]
- Shoemaker, R. C., Rash, J. M., & Simon, E. W. (2005). Sick building syndrome in water-damaged buildings: generalization of the chronic, biotoxin associated illness paradigm to indoor toxigenic fungi. In E. Johanning (Ed.), Bioaerosols, fungi, bacteria, mycotoxins and human health (pp. 66–77). Fungal Research Group Foundation Inc., Albany, NY: Eastern New York Occupational & Environmental Health Center.
- Simoni M, Annesi-Maesano I, Sigsgaard T, Norback D, Wieslander G, Nystad W, Canciani M, Sestini P, Viegi G. School air quality related to dry cough, rhinitis and nasal patency in children. European Respiratory Journal. 2010;35(4):742–749. doi: 10.1183/09031936.00016309. [DOI] [PubMed] [Google Scholar]
- Simon-Nobbe B, Denk U, Pöll V, Rid R, Breitenbach M. The spectrum of fungal allergy. International Archives of Allergy and Immunology. 2008;145(1):58–86. doi: 10.1159/000107578. [DOI] [PubMed] [Google Scholar]
- Sirois, F. (2013). Perspectives on epidemic. Mass psychogenic illness: A social psychological analysis (p. 217).
- Sivasubramani SK, Niemeier RT, Reponen T, Grinshpun SA. Assessment of the aerosolization potential for fungal spores in moldy homes. Indoor Air. 2004;14(6):405–412. doi: 10.1111/j.1600-0668.2004.00262.x. [DOI] [PubMed] [Google Scholar]
- Sivasubramani SK, Niemeier RT, Reponen T, Grinshpun SA. Fungal spore source strength tester: laboratory evaluation of a new concept. Science of the Total Environment. 2004;329(1):75–86. doi: 10.1016/j.scitotenv.2004.03.007. [DOI] [PubMed] [Google Scholar]
- Skov, P., Valbjørn, O., & Pedersen, B. V. (1989). Influence of personal characteristics, job-related factors and psychosocial factors on the sick building syndrome. Scandinavian Journal of Work, Environment & Health, 286–295. [DOI] [PubMed]
- Skov, P., Valbjørn, O., & Pedersen, B. V. (1990). Influence of indoor climate on the sick building syndrome in an office environment. Scandinavian Journal of Work, Environment & Health, 363–371. [DOI] [PubMed]
- Stenberg B, Wall S. Why do women report ’sick building symptoms’ more often than men? Social Science & Medicine. 1995;40(4):491–502. doi: 10.1016/0277-9536(94)E0104-Z. [DOI] [PubMed] [Google Scholar]
- Stenberg B, Mild KH, Sandström M, Sundell J, Wall S. A prevalence study of the sick building syndrome (SBS) and facial skin symptoms in office workers. Indoor Air. 1993;3(2):71–81. doi: 10.1111/j.1600-0668.1993.t01-2-00002.x. [DOI] [Google Scholar]
- Sterflinger K, Ettenauer J, Pinar G. Bio-susceptibility of materials and thermal insulation systems used for historical buildings. European Geosciences Union General Assembly 2013, EGU, Division Energy, Resources & the Environment. Energy Procedia. 2013;40:499–506. doi: 10.1016/j.egypro.2013.08.057. [DOI] [Google Scholar]
- Stetzenbach LD, Buttner MP, Cruz P. Detection and enumeration of airborne biocontaminants. Current Opinion in Biotechnology. 2004;15(3):170–174. doi: 10.1016/j.copbio.2004.04.009. [DOI] [PubMed] [Google Scholar]
- Straus DC. Molds, mycotoxins, and sick building syndrome. Toxicology and Industrial Health. 2009;25(9–10):617–635. doi: 10.1177/0748233709348287. [DOI] [PubMed] [Google Scholar]
- Sun Y, Wang Z, Zhang Y, Sundell J. In China, students in crowded dormitories with a low ventilation rate have more common colds: Evidence for airborne transmission. PloS one. 2011;6(11):e27140. doi: 10.1371/journal.pone.0027140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y, Zhang Y, Bao L, Fan Z, Sundell J. Ventilation and dampness in dorms and their associations with allergy among college students in China: A case–control study. Indoor Air. 2011;21(4):277–283. doi: 10.1111/j.1600-0668.2010.00699.x. [DOI] [PubMed] [Google Scholar]
- Sundell, J. (1996). What we know, and dont know about sick building syndrome. ASHRAE Journal, 38(6).
- Sundell J. On the history of indoor air quality and health. Indoor Air. 2004;14(s7):51–58. doi: 10.1111/j.1600-0668.2004.00273.x. [DOI] [PubMed] [Google Scholar]
- Sundell J, Levin H, Nazaroff WW, Cain WS, Fisk WJ, Grimsrud DT, Gyntelberg F, Li Y, Persily AK, Pickering AC, Samet JM. Ventilation rates and health: multidisciplinary review of the scientific literature. Indoor Air. 2011;21(3):191–204. doi: 10.1111/j.1600-0668.2010.00703.x. [DOI] [PubMed] [Google Scholar]
- Syazwan AI, Juliana J, Norhafizalina O, Azman ZA, Kamaruzaman J. Indoor air quality and sick building syndrome in Malaysian buildings. Global Journal of Health Science. 2009;1(2):126–135. [Google Scholar]
- Takahashi Y, Takano K, Suzuki M, Nagai S, Yokosuka M, Takeshita T, Saito A, Yasueda H, Enomoto T. Two routes for pollen entering indoors: Ventilation and clothes. Journal of Investigational Allergology and Clinical Immunology. 2008;18:382–388. [PubMed] [Google Scholar]
- Takeda M, Saijo Y, Yuasa M, Kanazawa A, Araki A, Kishi R. Relationship between sick building syndrome and indoor environmental factors in newly built Japanese dwellings. International Archives of Occupational and Environmental Health. 2009;82(5):583–593. doi: 10.1007/s00420-009-0395-8. [DOI] [PubMed] [Google Scholar]
- Tang JW. The effect of environmental parameters on the survival of airborne infectious agents. Journal of the Royal Society Interface. 2009;6(Suppl 6):S737–S746. doi: 10.1098/rsif.2009.0227.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang JW, Li Y. Transmission of influenza A in human beings. The Lancet Infectious Diseases. 2007;7(12):758–761. doi: 10.1016/S1473-3099(07)70268-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarlo, S. M., Balmes, J., Balkissoon, R., Beach, J., Beckett, W., Bernstein, D.,et al. (2008). Diagnosis and management of work-related asthma: American College of Chest Physicians Consensus Statement. CHEST Journal, 134(3_suppl), 1S–41S. [DOI] [PubMed]
- Teeratakulpisarn J, Pairojkul S, Heng S. Survey of the prevalence of asthma’, allergic rhinitis and eczema in schoolchildren from Khon Kaen, Northeast Thailand: An ISAAC Study. Asian Pacific Journal of Allergy and Immunology. 2000;18(4):187–194. [PubMed] [Google Scholar]
- Tellier R. Aerosol transmission of influenza A virus: A review of new studies. Journal of the Royal Society Interface. 2009;6(suppl 6):S783–S790. doi: 10.1098/rsif.2009.0302.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terčelj M, Salobir B, Harlander M, Rylander R. Fungal exposure in homes of patients with sarcoidosis-an environmental exposure study. Environmental Health. 2011;10(1):8. doi: 10.1186/1476-069X-10-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai DH, Lin JS, Chan CC. Office workers’ sick building syndrome and indoor carbon dioxide concentrations. Journal of Occupational and Environmental Hygiene. 2012;9(5):345–351. doi: 10.1080/15459624.2012.675291. [DOI] [PubMed] [Google Scholar]
- Tuomainen, A., Seuri, M., & Sieppi, A. (2004). Indoor air quality and health problems associated with damp floor coverings. International Archives of Occupational and Environmental Health, 77(3), 222–226. [DOI] [PubMed]
- Tuomi T, Reijula K, Johnsson T, Hemminki K, Hintikka EL, Lindroos O, Kalso S, Koukila-Kähkölä P, Mussalo-Rauhamaa H, Haahtela T. Mycotoxins in crude building materials from water-damaged buildings. Applied and Environmental Microbiology. 2000;66(5):1899–1904. doi: 10.1128/AEM.66.5.1899-1904.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US OSHA. (2003). Brief guide to mold in the workplace. Occupational Safety and Health Administration, US Department of Labor, Washington, DC. http://www.osha.gov/dts/shib/shib101003.pdf.
- Vacher S, Hernandez C, Bärtschi C, Poussereau N. Impact of paint and wall-paper on mould growth on plasterboards and aluminum. Building and Environment. 2010;45(4):916–921. doi: 10.1016/j.buildenv.2009.09.011. [DOI] [Google Scholar]
- Vance PH, Weissfeld AS. The controversies surrounding sick building syndrome. Clinical Microbiology Newsletter. 2007;29(10):73–76. doi: 10.1016/j.clinmicnews.2007.04.007. [DOI] [Google Scholar]
- Wang X, Yu JC, Chen Y, Wu L, Fu X. ZrO2-modified mesoporous nanocrystalline TiO2-x N x as efficient visible light photocatalysts. Environmental Science & Technology. 2006;40(7):2369–2374. doi: 10.1021/es052000a. [DOI] [PubMed] [Google Scholar]
- Wang S, Ang HM, Tade MO. Volatile organic compounds in indoor environment and photocatalytic oxidation: State of the art. Environment International. 2007;33(5):694–705. doi: 10.1016/j.envint.2007.02.011. [DOI] [PubMed] [Google Scholar]
- Wargocki P, Lagercrantz L, Witterseh T, Sundell J, Wyon DP, Fanger PO. Subjective perceptions, symptom intensity and performance: A comparison of two independent studies, both changing similarly the pollution load in an office. Indoor Air. 2002;12(2):74–80. doi: 10.1034/j.1600-0668.2002.01101.x. [DOI] [PubMed] [Google Scholar]
- Wargocki P, Wyon DP, Fanger PO. The performance and subjective responses of call-center operators with new and used supply air filters at two outdoor air supply rates. Indoor Air. 2004;14(s8):7–16. doi: 10.1111/j.1600-0668.2004.00304.x. [DOI] [PubMed] [Google Scholar]
- Weinhold B. A spreading concern: Inhalational health effects of mold. Environmental Health Perspectives. 2007;115(6):A300–A305. doi: 10.1289/ehp.115-a300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson AD, Baietto M. Applications and advances in electronic-nose technologies. Sensors. 2009;9(7):5099–5148. doi: 10.3390/s90705099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson AD, Baietto M. Advances in electronic-nose technologies developed for biomedical applications. Sensors. 2011;11(1):1105–1176. doi: 10.3390/s110101105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolkoff P. How to measure and evaluate volatile organic compound emissions from building products. A perspective. Science of the Total Environment. 1999;227(2):197–213. doi: 10.1016/S0048-9697(99)00019-4. [DOI] [PubMed] [Google Scholar]
- Wong TW, Lee CK, Tam W, Lau JTF, Yu TS, Lui SF, Chan PK, Li Y, Bresee JS, Sung JJ, Parashar UD. Cluster of SARS among medical students exposed to single patient. Hong Kong. Emerging Infectious Diseases. 2004;10(2):269–276. doi: 10.3201/eid1002.030452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu MJ, Feng YS, Sung WP, Surampalli RY. Quantification and analysis of airborne bacterial characteristics in a nursing care institution. Journal of the Air & Waste Management Association. 2011;61(7):732–739. doi: 10.3155/1047-3289.61.7.732. [DOI] [PubMed] [Google Scholar]
- Yang GH, Jarvis BB, Chung YJ, Pestka JJ. Apoptosis induction by the satratoxins and other trichothecene mycotoxins: relationship to ERK, p38 MAPK, and SAPK/JNK activation. Toxicology and Applied Pharmacology. 2000;164(2):149–160. doi: 10.1006/taap.1999.8888. [DOI] [PubMed] [Google Scholar]
- Yau YH, Ng WK. A comparison study on energy savings and fungus growth control using heat recovery devices in a modern tropical operating theatre. Energy Conversion and Management. 2011;52(4):1850–1860. doi: 10.1016/j.enconman.2010.12.005. [DOI] [Google Scholar]
- Yazicioglu M, Asan A, Ones U, Vatansever U, Sen B, Ture M, Bostancioglu M, Pala O. Indoor airborne fungal spores and home characteristics in asthmatic children from Edirne region of Turkey. Allergologia et Immunopathologia. 2004;32(4):197–203. doi: 10.1016/S0301-0546(04)79239-3. [DOI] [PubMed] [Google Scholar]
- Yike I. Fungal proteases and their pathophysiological effects. Mycopathologia. 2011;171(5):299–323. doi: 10.1007/s11046-010-9386-2. [DOI] [PubMed] [Google Scholar]
- Yoshino N, Takizawa M, Akiba H, Okumura H, Tashiro F, Honda M, Ueno Y. Transient elevation of intracellular calcium ion levels as an early event in T-2 toxin-induced apoptosis in human promyelotic cell line HL-60. Natural Toxins. 1996;4(5):234–241. doi: 10.1002/(SICI)(1996)4:5<234::AID-NT6>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- Zain ME. Impact of mycotoxins on humans and animals. Journal of Saudi Chemical Society. 2011;15(2):129–144. doi: 10.1016/j.jscs.2010.06.006. [DOI] [Google Scholar]
- Zalejska-Jonsson A, Wilhelmsson M. Impact of perceived indoor environment quality on overall satisfaction in Swedish dwellings. Building and Environment. 2013;63:134–144. doi: 10.1016/j.buildenv.2013.02.005. [DOI] [Google Scholar]
- Zhen S, Li K, Yin L, Yao M, Zhang H, Chen L, Zhou M, Chen X. A comparison of the efficiencies of a portable BioStage impactor and a Reuter centrifugal sampler (RCS) High flow for measuring airborne bacteria and fungi concentrations. Journal of Aerosol Science. 2009;40(6):503–513. doi: 10.1016/j.jaerosci.2009.02.003. [DOI] [Google Scholar]
- Zhou HR, Harkema JR, Yan D, Pestka JJ. Amplified proinflammatory cytokine expression and toxicity in mice coexposed to lipopolysaccharide and the trichothecene vomitoxin (deoxynivalenol) Journal of Toxicology and Environmental Health Part A. 1999;57(2):115–136. doi: 10.1080/009841099157818. [DOI] [PubMed] [Google Scholar]
- Zhu S, Kato S, Yang JH. Study on transport characteristics of saliva droplets produced by coughing in a calm indoor environment. Building and Environment. 2006;41(12):1691–1702. doi: 10.1016/j.buildenv.2005.06.024. [DOI] [Google Scholar]
- Zock JP. World at work: cleaners. Occupational and Environmental Medicine. 2005;62(8):581–584. doi: 10.1136/oem.2004.015032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zweers T, Preller L, Brunekreef B, Boleij JSM. Health and indoor climate complaints of 7043 office workers in 61 buildings in The Netherlands. Indoor Air. 1992;2(3):127–136. doi: 10.1111/j.1600-0668.1992.00001.x. [DOI] [Google Scholar]


