Highlights
-
•
A significant reduction in psychological impact 4 weeks after COVID outbreak.
-
•
The mean scores of respondents in both surveys were above PTSD cut-offs.
-
•
Female gender, physical symptoms associated with a higher psychological impact.
-
•
Hand hygiene, mask-wearing & confidence in doctors reduced psychological impact.
-
•
Online trauma-focused psychotherapy may be helpful to public during COVID-19.
Keywords: Anxiety, Coronavirus, COVID-19, Depression, Epidemic, Longitudinal, Stress, Pandemic, Precaution, Post-traumatic stress disorder
Abstract
In addition to being a public physical health emergency, Coronavirus disease 2019 (COVID-19) affected global mental health, as evidenced by panic-buying worldwide as cases soared. Little is known about changes in levels of psychological impact, stress, anxiety and depression during this pandemic. This longitudinal study surveyed the general population twice - during the initial outbreak, and the epidemic's peak four weeks later, surveying demographics, symptoms, knowledge, concerns, and precautionary measures against COVID-19. There were 1738 respondents from 190 Chinese cities (1210 first-survey respondents, 861 s-survey respondents; 333 respondents participated in both). Psychological impact and mental health status were assessed by the Impact of Event Scale-Revised (IES-R) and the Depression, Anxiety and Stress Scale (DASS-21), respectively. IES-R measures PTSD symptoms in survivorship after an event. DASS -21 is based on tripartite model of psychopathology that comprise a general distress construct with distinct characteristics. This study found that there was a statistically significant longitudinal reduction in mean IES-R scores (from 32.98 to 30.76, p < 0.01) after 4 weeks. Nevertheless, the mean IES-R score of the first- and second-survey respondents were above the cut-off scores (>24) for PTSD symptoms, suggesting that the reduction in scores was not clinically significant. During the initial evaluation, moderate-to-severe stress, anxiety and depression were noted in 8.1%, 28.8% and 16.5%, respectively and there were no significant longitudinal changes in stress, anxiety and depression levels (p > 0.05). Protective factors included high level of confidence in doctors, perceived survival likelihood and low risk of contracting COVID-19, satisfaction with health information, personal precautionary measures. As countries around the world brace for an escalation in cases, Governments should focus on effective methods of disseminating unbiased COVID-19 knowledge, teaching correct containment methods, ensuring availability of essential services/commodities, and providing sufficient financial support.
1. Introduction
China was the first country that identified the novel coronavirus disease (COVID-19) as the cause of the outbreak. On January 23, Chinese authorities imposed lockdown measures on ten cities in an unprecedented effort to contain the COVID-19 outbreak. The World Health Organization (WHO) declared the COVID-19 outbreak an international public health emergency on January 30, 2020 (Mahase, 2020) and a pandemic on March 11, 2020 (Who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march, 020). Subsequently, rapid surge in the number of COVID-19 cases was observed during March 2020 in Iran, Italy, South Korea, Europe and United States (WHO team arrives in Iran, 2020, Europe on Lockdown From COVID-19, 2020). Increasing menace of the epidemic led to a global atmosphere of anxiety and depression due to disrupted travel plans, social isolation, media information overload and panic buying of necessity goods (Ho et al., 2020). A recent study in China found that the vicarious traumatization scores of the general public were significantly higher than those of the front-line nurses (Li et al., 2020). As a result, governments and public health authorities urgently need guidance and actionable information on effective public health and psychological interventions that can safeguard the mental health of the general public (Rubin et al., 2020). Recent mental health studies on COVID-19 were cross-sectional (Wang et al., 2020), focusing on health professionals (Kang et al., 2020, Tan et al., 2020, Joob and Wiwanitkit, 2020) or a particular age group (Cao et al., 2020) and lack of in-depth analysis to identify risk or protective factors for mental health (Qiu et al., 2020). Currently, there is no known information about the longitudinal change of mental health status throughout the COVID-19 epidemic and factors that would influence psychological impact and mental health status with the implementation of public health measures of such unprecedented magnitude. The novelty of this longitudinal study was to evaluate the temporal psychological impact and adverse mental health status during the initial outbreak and peak of COVID-19 epidemic and identity risk and protective factors among the general population in China.
2. Methods
2.1. Study design and study population
This longitudinal study was conducted from January 31 to February 2 (first survey) and February 28 to March 1, 2020 (second survey). Both surveys were conducted during weekends to ensure maximum participation. Our snowball sampling strategy focused on recruiting the general public living in mainland China during the COVID-19 outbreak.
2.2. Procedure
When the Chinese Government recommended the public to minimize face-to-face interaction and isolate themselves, information about this study was posted on the university website. In addition to their own participation, a respondent was encouraged to invite new respondents from his or her contacts. A questionnaire was completed through an online survey platform (‘SurveyStar’, Changsha Ranxing Science and Technology, Shanghai, China). Ethics approval was obtained from the Institutional Review Board of the Huaibei Normal University (HBU-IRB-2020-001). All respondents provided informed consent.
2.3. Outcomes
This study used the National University of Singapore COVID-19 questionnaire, which evaluated its psychometric properties in the initial phase of the COVID-19 epidemic (Wang et al., 2020). The National University of Singapore COVID-19 questionnaire consisted of questions related to (1) demographic data; (2) physical symptoms during past 14 days; (3) contact history with a COVID-19 patient in past 14 days; (4) knowledge and concerns about COVID-19 and (5) precautionary measures against COVID-19 in the past 14 days. The psychological impact of COVID-19 was measured using the Impact of Event Scale-Revised (IES-R) (Christianson and Marren, 2012). IES-R measures PTSD symptoms in survivorship after an event (Hosey et al., 2019). The mental health status of respondents was measured using the Depression, Anxiety and Stress Scale (DASS-21) (Norton, 2007). DASS -21 is based on tripartite model of psychopathology that comprise a general distress construct with distinct characteristics (Zanon et al., 2020). IES-R and DASS were previously used in research related to the COVID-19 epidemic (Wang et al., 2020, Tan et al., 2020, Hao et al., 2019, Tan et al., 2019)
2.4. Statistical analysis
To analyze the differences in psychological impact, levels of depression, anxiety and stress, the independent sample t-test was used to compare the mean score between the first and second survey. Percentages of response to other questions were calculated according to the number of respondents per response to the number of total responses of a question and presented as categorical variables. The chi-squared test was used to analyze the differences in categorical variables between the first and second surveys. We used linear regressions to calculate the univariate associations between independent variables and dependent variables for the first and second survey separately. All tests were two-tailed, with a significance level of p < 0·05. Statistical analysis was performed on SPSS Statistic 21.0.
3. Results
3.1. Development of the COVID-19 epidemic in China during the two recruitment periods
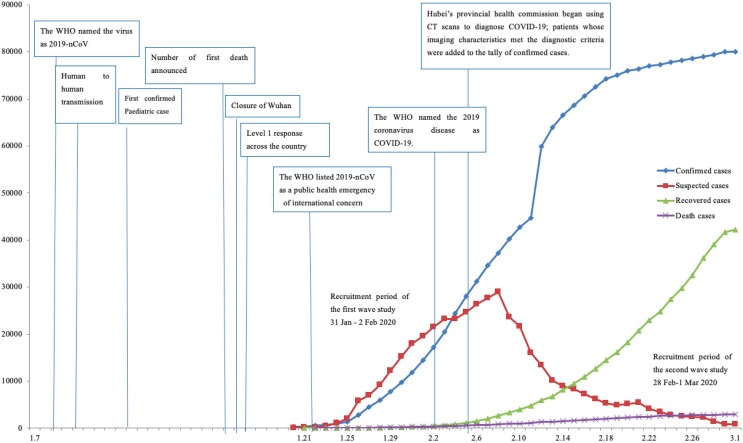
Fig. 1 shows the evolution of the COVID-19 epidemic in China from January 7 to March 1, 2020. The first survey conducted between January 31 and February 2, when China was going through a phase of rapid increase in the number of newly diagnosed COVID-19 cases and related deaths. After February 8, 2020, there was a rapid decline in the number of new and suspected cases and the downward trend continued thereafter. Simultaneously, the number of recovered patients showed a substantial increase during this period. The second survey was conducted from February 28 to March 1, 2020.
Fig. 1.
National epidemic trend of 2019 coronavirus disease (COVID-19) outbreak in China from January 7 to March 1, 2020.
3.2. Comparison of respondents and mental health status between the first and second survey
Of the 1406 invited participants from 194 cities in China, 1304 (92.7%) completed the questionnaire during the first survey. Although there were 865 participants from 159 cities during the second survey, only 861 (99.5%) questionnaires were complete, which were included in the study. Importantly, 333 respondents during the second survey (27·5% of the first-survey respondents and 38·7% of the second-survey respondents) had also participated in the first survey. Therefore, a total of 1738 individual respondents participated in this longitudinal study.
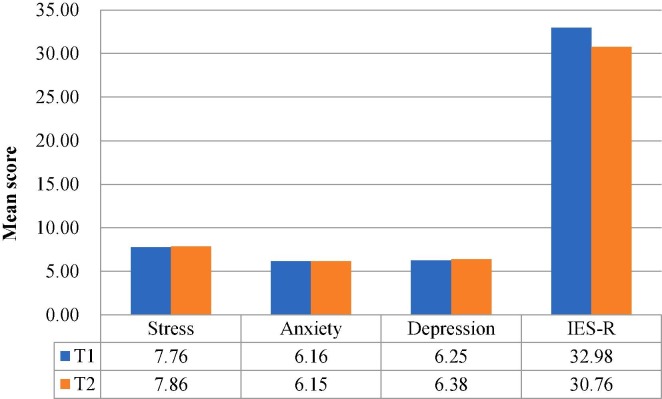
Fig. 2 compares the mean scores of DASS-stress, anxiety and depression subscales and IES-R scores between the first- and second-survey respondents. The mean score (standard deviation, SD) for DASS-stress subscale was 7·76 (7·74) for the first-survey respondents and 7·86 (7·93) for the second-survey respondents (t = −0·30, p > 0·05, 95% CI −0·79 to 0·58). Similar non-significant differences were noted between the two surveys for the DASS-anxiety subscale [6·16 (6·57) versus 6·15 (6·94); t = 0·36, p > 0·05, 95% CI −0·58 to 0·60] and DASS-depression subscale [6.25 (7.16) versus 6·38 (7.39); t = −0·41, p > 0·05, 95% CI −0·77 to 0·50)] mean scores. However, the mean IES-R score of the second-survey respondents [30·76 (16·34)] was significantly lower than the first-survey respondents [32·98 (15·42); t = 3·125, p < 0·01, 95% CI 0·83 to 3·62]. Most importantly, the overall mean IES-R scores for respondents in both surveys were more than 24 points, indicating the presence of PTSD symptoms and the reduction in IES-R scores was not clinically significant.
Fig. 2.
Comparison of the mean scores of DASS-stress, anxiety and depression subscales as well as IES-R scores between the first (T1) and second (T2) survey.
3.3. Demographic characteristics and their association with psychological impact and adverse mental health status
Majority of first-survey respondents were women (67·3%), of younger age group of 21·4 to 30·8 years (53·1%), married (76·4%), having a household size of 3–5 people (80·7%), having children (67·4%), being students (52·8%) and well educated (87·9% with at least a bachelor degree). Similarly, the majority of second-survey respondents were women (75%), of young adulthood with age 21·4 to 30·8 years (46·5%), married (83·5%), having a household size of 3–5 people (80·4%), having children (68·6%), students (62·8%) and well educated (87·6%≥ bachelor degree). The differences in the association between demographic characteristics and IES-R scores are represented in Table 1 . Briefly, the second survey respondents aged 12 to 21·4 years demonstrated significantly higher score of IES-R as compared to respondents aged 49·6-59 years (B = 0·77, t = 2·28, p < 0·05). Similarly, the second-survey respondents staying in a household with 3–5 people (B = 1·32, t = 2·04, p < 0·05) and more than 6 people (B = 1·44, t = 2·20, p < 0·05) had significantly higher score of IES-R as compared to respondents who stayed alone. Interestingly, these findings were not observed among the first survey respondents.
Table 1.
Association between demographic variables and the psychological impact as well as adverse mental health status during the first and second surveys (n = 1738).
| Demographic variables | The first survey (January 31 – February 2, 2020) (N = 1210) |
The second survey (February 28 – March 1, 2020) (N = 861) |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Impact of event |
Stress |
Anxiety |
Depression |
Impact of event |
Stress |
Anxiety |
Depression |
|||||||||
| B | T | B | t | B | t | B | T | B | T | B | T | B | t | B | t | |
| Gender | ||||||||||||||||
| Male | −0.20 | −2.56* | 0.10 | 2.33* | 0.19 | 2.64** | 0.12 | 2.13* | −0.26 | −2.61** | 0.08 | 1.38 | 0.18 | 1.90 | 0.22 | 2.89** |
| Female | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Age range | ||||||||||||||||
| 12–21.4 years | 0.21 | 1.00 | 0.08 | 0.65 | 0.10 | 0.51 | 0.06 | 0.39 | 0.77 | 2.28* | −0.03 | −0.16 | 0.29 | 0.92 | −0.02 | −0.07 |
| 21.4–30.8 years | 0.09 | 0.45 | 0.12 | 1.01 | 0.07 | 0.36 | 0.18 | 1.15 | 0.59 | 1.75 | 0.02 | 0.08 | 0.36 | 1.17 | 0.10 | 0.36 |
| 30.8–40.2 years | −0.17 | −0.73 | −0.07 | −0.52 | −0.16 | −0.72 | −0.06 | −0.36 | 0.63 | 1.62 | 0.03* | −0.15 | 0.29 | 0.80 | 0.03 | 0.12 |
| 40.2–49.6 years | −0.16 | −0.69 | −0.12 | −0.82 | −0.23 | −1.05 | −0.16 | −0.89 | 0.26 | 0.70 | −0.15 | −0.70 | −0.02 | −0.05 | −0.18 | −0.63 |
| 49.6–59 years | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Status as a parent | ||||||||||||||||
| Has a child 16 years or below | 0.04 | 0.43 | −0.02 | −0.37 | 0.08 | 0.86 | 0.05 | 0.70 | 0.12 | 0.94 | 0.03 | 0.34 | 0.11 | 0.87 | 0.09 | 0.88 |
| Has a child older than 16 years | −0.06 | −0.78 | −0.07 | −1.50 | −0.08 | −1.10 | −0.06 | −1.03 | 0.10 | 0.96 | 0.003 | 0.06 | −0.03 | −0.34 | −0.02 | −0.29 |
| No children | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Marital status | ||||||||||||||||
| Single | −0.04 | −0.05 | 0.02 | 0.05 | 0.71 | 1.06 | 0.45 | 0.84 | 1.06 | 1.41 | 0.41 | 0.94 | 0.60 | 0.87 | 0.48 | 0.84 |
| Married | 0.09 | 0.12 | 0.12 | 0.29 | 0.80 | 1.20 | 0.56 | 1.03 | 1.27 | 1.71 | 0.46 | 1.06 | 0.80 | 1.17 | 0.58 | 1.02 |
| Divorced/separated | 0.11 | 0.13 | <0.001 | <0.001 | 0.44 | 0.58 | 0.44 | 0.72 | 1.27 | 1.35 | 0.60 | 1.10 | 1.00 | 1.16 | 0.60 | 0.84 |
| Widowed | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Household size | ||||||||||||||||
| 6 people or more | 0.38 | 0.97 | −0.23 | −0.99 | −0.17 | −0.46 | −0.19 | −0.67 | 1.44 | 2.20* | 0.50 | 1.32 | 0.84 | 1.40 | 0.12 | 0.24 |
| 3–5 people | 0.25 | 0.65 | −0.20 | −0.88 | −0.12 | −0.35 | 0.09* | −0.31 | 1.32 | 2.04* | 0.45 | 1.19 | 0.77 | 1.29 | 0.06 | 0.13 |
| 2 people | 0.41 | 0.99 | −0.33 | −1.35 | −0.18 | −0.46 | −0.21 | −0.69 | 1.19 | 1.76 | 0.44 | 1.12 | 0.61 | 0.99 | −0.16 | −0.31 |
| Stay alone | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Education Level | ||||||||||||||||
| None | −0.07 | −0.08 | 0.76 | 1.40 | 1.02 | 1.19 | 1.81 | 2.64** | −1.00 | −1.17 | −0.33 | −0.67 | −0.33 | −0.42 | −0.56 | −0.86 |
| Preschool | 0.67 | 0.78 | −0.33 | −0.67 | −0.33 | −0.42 | −0.56 | −0.86 | ||||||||
| Primary school | −1.07 | −2.07* | −0.11 | −0.37 | −0.10 | −0.21 | −0.07 | −0.17 | −0.75 | −0.97 | 0.17 | 0.37 | 0.67 | 0.94 | 0.44 | 0.76 |
| Lower secondary school | 0.21 | 0.66 | 0.20 | 1.05 | 0.38 | 1.27 | 0.41 | 1.72 | 0.43 | 0.93 | 0.08 | 0.29 | 0.41 | 0.97 | 0.01 | 0.04 |
| Upper secondary school | 0.01 | 0.03 | 0.16 | 0.87 | 0.36 | 1.28 | 0.34 | 1.50 | 0.24 | 0.51 | 0.23 | 0.85 | 0.60 | 1.40 | 0.14 | 0.39 |
| University – Bachelor | 0.19 | 0.67 | 0.21 | 1.28 | 0.32 | 1.25 | 0.35 | 1.70 | 0.63 | 1.46 | 0.11 | 0.42 | 0.40 | 1.00 | −0.03 | −0.08 |
| University – Master | 0.14 | 0.49 | 0.18 | 1.09 | 0.24 | 0.90 | 0.33 | 1.55 | 0.58 | 1.30 | 0.19 | 0.73 | 0.65 | 1.58 | 0.13 | 0.39 |
| University – Doctorate | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
†There were 333 respondents who participated in both the first and second surveys.
*p < 0·05, **p < 0·01, ***p < 0·001.
3.4. Physical symptoms, health status and its association with psychological impact and adverse mental health status
Physical symptoms and health status findings of the participants during the two surveys is shown in Table A.1. Briefly, significantly lower proportion of the second-survey respondents reported chills, headache, cough, dizziness, coryza and sore throat. Similarly, significantly lower consultations with a doctor occurred among the second survey participants. In contrast, significantly higher proportion of the second-survey respondents underwent home quarantined as compared to the first-survey respondents. There were no significant differences in recent testing of COVID-19 and medical insurance coverage between the first- and second-survey respondents.
In both surveys, physical symptoms, very poor self-rating of health status, and history of chronic illness were significantly associated with higher IES-R scores, DASS stress, anxiety or depression subscale scores (Table 2 ). In the second survey, the presence of symptoms such as fever with cough or breathing difficulty and recent quarantine were significantly associated with DASS stress, anxiety and depression scores, which was not observed among the first survey participants. Interestingly, gastrointestinal symptoms were significantly associated with DASS stress, anxiety and depression scores during the second survey.
Table 2.
Association between physical health status and the psychological impact as well as adverse mental health status during the first and second survey (n = 1738).
| The first survey (January 31 – February 2, 2020) (N = 1210) † |
The second survey (February 28 – March 1, 2020) (N = 861) † |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Physical symptoms and health status | Impact of event |
Stress |
Anxiety |
Depression |
Impact of event |
Stress |
Anxiety |
Depression |
||||||||
| B | t | B | t | B | t | B | T | B | t | B | t | B | t | B | t | |
| Persistent fever | ||||||||||||||||
| Yes | −0.23 | −0.44 | 0.40 | 1.34 | 1.23 | 2.60* | 0.98 | 2.57* | 1.43 | 1.11 | 3.55 | 4.81*** | 3.24 | 2.75** | 3.44 | 3.56*** |
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Chills | ||||||||||||||||
| Yes | 0.46 | 2.34* | 0.44 | 3.84*** | 0.60 | 3.31** | 0.41 | 2.84** | 0.69 | 1.84 | 0.90 | 4.16*** | 0.83 | 2.42* | 0.87 | 3.08** |
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Headache | ||||||||||||||||
| Yes | 0.37 | 3.07** | 0.12 | 1.65 | 0.36 | 3.20** | 0.23 | 2.52* | 0.59 | 3.02** | 0.46 | 4.07*** | 0.76 | 4.26*** | 0.51 | 3.45** |
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Myalgia | ||||||||||||||||
| Yes | 0.63 | 4.77*** | 0.43 | 5.60*** | 0.69 | 5.61*** | 0.50 | 5.08*** | 0.50 | 2.83** | 0.42 | 4.13*** | 0.59 | 3.67*** | 0.58 | 4.42*** |
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Cough | ||||||||||||||||
| Yes | 0.33 | 3.23** | 0.19 | 3.11** | 0.29 | 2.97** | 0.21 | 2.69** | 0.48 | 1.95 | 0.61 | 4.25*** | 0.69 | 3.03** | 0.68 | 3.64*** |
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Breathing difficulty | ||||||||||||||||
| Yes | 0.88 | 1.58 | 0.57 | 1.74 | 1.63 | 3.15** | 1.28 | 3.08** | 0.77 | 1.46 | 1.06 | 3.47** | 1.08 | 2.23* | 1.45 | 3.66*** |
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Dizziness | ||||||||||||||||
| Yes | 0.54 | 3.95*** | 0.33 | 4.09*** | 0.63 | 4.97** | 0.42 | 4.13*** | 0.98 | 4.20*** | 0.80 | 6.00*** | 0.95 | 4.42*** | 0.66 | 3.72*** |
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Coryza | ||||||||||||||||
| Yes | 0.39 | 4.11*** | 0.25 | 4.46*** | 0.46 | 5.18*** | 0.33 | 4.70*** | 0.66 | 3.40** | 0.33 | 2.90** | 0.52 | 2.94** | 0.53 | 3.64*** |
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Sore throat | ||||||||||||||||
| Yes | 0.34 | 2.99** | 0.16 | 2.45* | 0.35 | 3.35** | 0.17 | 2.08* | 0.35 | 1.50 | 0.60 | 4.53*** | 0.80 | 3.77*** | 0.75 | 4.31*** |
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Persistent fever and cough or difficulty breathing | ||||||||||||||||
| Yes | −0.23 | −0.36 | 0.32 | 0.87 | 0.98 | 1.68 | 0.22 | 0.48 | 1.43 | 1.11 | 3.55 | 4.81*** | 3.24 | 2.75** | 3.44 | 3.56*** |
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Gastrointestinal symptoms such as nausea, vomiting, diarrhea | ||||||||||||||||
| Yes | NA | NA | NA | NA | 0.72 | 1.48 | 1.27 | 4.54*** | 1.39 | 3.11** | 1.31 | 3.56*** | ||||
| No | Reference | Reference | Reference | Reference | ||||||||||||
| Consultation with a doctor in the clinic in the past 14 days | ||||||||||||||||
| Yes | −0.06 | −0.31 | 0.17 | 1.47 | 0.38 | 2.08* | 0.22 | 1.48 | 0.44 | 1.21 | 0.25 | 1.17 | 0.39 | 1.20 | 0.29 | 1.07 |
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Recent testing for COVID-19 in the past 14 days | ||||||||||||||||
| Yes | −0.18 | −0.48 | −0.07 | −0.31 | 0.22 | 0.64 | 0.02 | 0.06 | −0.32 | −0.50 | −0.20 | −0.54 | −0.02 | −0.03 | −0.06 | −0.12 |
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Recent quarantine in the past 14 days | ||||||||||||||||
| Yes | 0.32 | 1.30 | −0.01 | −0.06 | 0.03 | 0.13 | −0.11 | −0.59 | 0.35 | 1.73 | 0.25 | 2.14* | 0.55 | 2.94** | 0.39 | 2.52* |
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Current self-rating health status | ||||||||||||||||
| Very poor | 1.39 | 1.13 | 3.63 | 5.03*** | 3.35 | 2.94** | 3.56 | 3.88*** | −0.44 | −0.91 | 0.64 | 2.29* | 0.82 | 1.86 | 0.73 | 2.01* |
| Poor | 0.69 | 1.77 | 0.13 | 0.57 | 0.65 | 1.81 | 0.36 | 1.23 | 1.56 | 3.23** | 1.21 | 4.34*** | 1.68 | 3.81*** | 1.30 | 3.59*** |
| Average | 0.37 | 4.73*** | 0.19 | 4.28*** | 0.41 | 5.70*** | 0.26 | 4.63*** | 0.37 | 3.99*** | 0.23 | 4.21*** | 0.42 | 4.94*** | 0.39 | 5.64*** |
| Good/Very good | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Chronic illness | ||||||||||||||||
| Yes | 0.29 | 2.02* | 0.24 | 2.77** | 0.48 | 3.58*** | 0.38 | 3.51*** | 0.45 | 2.25* | 0.24 | 2.02* | 0.25 | 1.34 | 0.27 | 1.76 |
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
| Medical insurance coverage | ||||||||||||||||
| Yes | 0.09 | 0.67 | −0.003 | −0.04 | −0.04 | −0.32 | 0.02 | 0.20 | 0.02 | 0.13 | −0.17 | −1.89 | −0.34 | −2.43* | −0.21 | −1.79 |
| No | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||||||||
†There were 333 respondents who participated in both the first and second surveys.
* p < 0·05, **p < 0·01, ***p < 0·001.
3.5. Knowledge and concerns about COVID-19 and its association with psychological impact and adverse mental health status
Compared to the first-survey respondents, significantly higher proportion of the second-survey respondents were uncertain about the transmission of COVID-19 by droplets but their views on transmission of the virus by being airborne or through the contacts with a contaminated object were not different (Table A.2). Importantly, significantly higher proportion of the second-survey respondents expressed very high level of confidence in their doctors’ ability to diagnose or recognize COVID-19), more likely to survive COVID-19 and satisfaction with health information on COVID-19 as compared to the first-survey respondents. Unfortunately, about one-third of the second-survey respondents felt that the Chinese had been discriminated in other countries during the COVID-19 pandemic. More than half (58.4%) experienced a shortage of necessity goods (except face masks), about one-third (31·4%) spent more than 2 h per day viewing information about COVID-19 on media and a quarter (26·4%) reported a significant reduction in household income.·These four questions were asked from only second-survey participants.
Knowledge about COVID-19 transmission and its association with psychological parameters is represented in Table 3 . Among the first-survey respondents, the belief that COVID-19 transmission occurs via droplet was significantly associated with DASS depression scores. During both surveys, participants’ confidence in their doctor’s ability to diagnose or recognize COVID-19, very low perceived likelihood of contracting COVID-19, very high likelihood of survival and high satisfaction with health information were significantly associated with lower IES-R, DASS stress, anxiety or depression scores. The dissemination of health information on COVID-19 via radio was associated with higher DASS anxiety and depression scores among participants of both surveys.
Table 3.
Association of knowledge and concerns related to COVID-19 and the psychological impact as well as adverse mental health status during the first and second survey (n = 1738).
| Knowledge and concerns related to COVID-19 | The first survey (January 31– February 2, 2020) (N = 1210) † |
The second survey (February 28 – March 1, 2020) (N = 861) † |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Impact of event |
Stress |
Anxiety |
Depression |
Impact of event |
Stress |
Anxiety |
Depression |
||||||||||
| B | t | B | t | B | t | B | t | B | t | B | t | B | t | B | t | ||
| Route of transmission | |||||||||||||||||
| Droplets | |||||||||||||||||
| Agree | 0.21 | 1.49 | 0.15 | 1.79 | 0.17 | 1.26 | 0.27 | 2.53* | 0.07 | 0.45 | −0.11 | −1.36 | −0.12 | −0.91 | −0.15 | −1.33 | |
| Disagree | 0.48 | 1.28 | 0.09 | 0.42 | 0.22 | 0.65 | 0.18 | 0.66 | 0.13 | 0.30 | 0.46 | 1.91 | 0.68 | 1.81 | 0.50 | 1.61 | |
| Do not know | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | |||||||||
| Contact via contaminated objects | |||||||||||||||||
| Agree | 0.04 | 0.40 | −0.02 | −0.37 | −0.07 | −0.81 | 0.02 | 0.21 | −0.06 | −0.54 | −0.08 | −1.17 | −0.05 | −0.47 | −0.10 | −1.24 | |
| Disagree | −0.04 | −0.27 | −0.16 | −1.80 | −0.23 | −1.63 | −0.10 | −0.89 | 0.13 | 0.66 | 0.003 | 0.03 | −0.16 | −0.90 | −0.16 | −1.05 | |
| Do not know | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | |||||||||
| Airborne | |||||||||||||||||
| Agree | 0.11 | 1.25 | 0.04 | 0.67 | 0.12 | 1.39 | 0.08 | 1.21 | 0.06 | 0.55 | 0.04 | 0.63 | 0.03 | 0.29 | −0.03 | −0.30 | |
| Disagree | 0.17 | 1.50 | −0.002 | −0.03 | 0.04 | 0.40 | 0.03 | 0.38 | 0.02 | 0.11 | −0.05 | −0.57 | −0.04 | −0.32 | −0.08 | −0.75 | |
| Do not know | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | |||||||||
| Level of confidence in own doctor’s ability to diagnose or recognize COVID-19 | |||||||||||||||||
| Very confident | −0.20 | −0.82 | 0.05 | 0.33 | 0.02 | 0.07 | 0.02 | 0.11 | 0.12 | 0.35 | −0.33 | −1.67 | −0.42 | −1.37 | −0.85 | −3.34** | |
| Somewhat confident | 0.19 | 0.81 | 0.16 | 1.14 | 0.22 | 0.98 | 0.09 | 0.51 | 0.42 | 1.24 | −0.25 | −1.27 | −0.34 | −1.08 | −0.72 | −2.82** | |
| Not very confident | 0.19 | 0.64 | 0.18 | 1.04 | 0.38 | 1.40 | 0.10 | 0.44 | 0.48 | 1.10 | 0.03 | 0.11 | 0.11 | 0.26 | −0.43 | −1.31 | |
| Not at all confident | 0.66 | 1.34 | 1.18 | 4.04*** | 1.86 | 4.04*** | 1.66 | 4.50*** | −0.33 | −0.35 | −0.23 | −0.42 | 0.37 | 0.41 | −0.33 | −0.46 | |
| Do not know | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | |||||||||
| Likelihood of contracting COVID − 19 during the epidemic | |||||||||||||||||
| Very likely | −0.33 | −2.27* | 0.05 | 0.63 | 0.07 | 0.49 | 0.15 | 1.38 | −0.34 | −1.75 | −0.06 | −0.57 | 0.07 | 0.38 | −0.06 | −0.42 | |
| Somewhat likely | 0.15 | 1.24 | 0.06 | 0.84 | −0.02 | −0.13 | 0.04 | 0.40 | −0.03 | −0.23 | −0.14 | −1.58 | −0.03 | −0.24 | −0.14 | −1.25 | |
| Not very likely | 0.14 | 1.19 | −0.002 | −0.03 | −0.05 | −0.49 | 0.03 | 0.38 | 0.05 | 0.34 | −0.15 | −1.77 | −0.08 | −0.57 | −0.15 | −1.36 | |
| Not likely at all | −0.23 | −1.54 | −0.18 | −2.04* | −0.36 | −2.58* | −0.19 | −1.68 | −0.12 | −0.65 | −0.19 | −1.90 | −0.15 | −0.92 | −0.31 | −2.33* | |
| Do not know | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | |||||||||
| Likelihood of surviving if infected with COVID-19 | |||||||||||||||||
| Very likely | −0.19 | −1.70 | −0.02 | −0.33 | −0.06 | −0.60 | 0.01 | 0.14 | −0.32 | −2.27* | −0.14 | −1.71 | −0.18 | −1.37 | −0.23 | −2.14* | |
| Somewhat likely | 0.12 | 1.25 | 0.01 | 0.25 | −0.03 | −0.33 | −0.01 | −0.08 | 0.02 | 0.12 | −0.09 | −1.18 | −0.09 | −0.83 | −0.19 | −2.00* | |
| Not very likely | 0.23 | 1.67 | 0.18 | 2.24* | 0.18 | 1.38 | 0.15 | 1.42 | −0.01 | −0.06 | 0.06 | 0.52 | 0.39 | 2.20* | 0.21 | 1.45 | |
| Not likely at all | 0.42 | 1.45 | 0.34 | 2.02* | 0.42 | 1.55 | 0.49 | 2.28* | −0.24 | −0.69 | 0.08 | 0.39 | 0.52 | 1.62 | 0.18 | 0.67 | |
| Do not know | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | |||||||||
| Satisfaction with the amount of health information available about COVID-19 | |||||||||||||||||
| Very satisfied | 0.02 | 0.09 | −0.09 | −0.79 | −0.20 | −1.15 | −0.12 | −0.85 | −0.07 | −0.25 | −0.60 | −3.92*** | −0.69 | −2.87** | −0.72 | −3.63*** | |
| Somewhat satisfied | 0.23 | 1.26 | 0.03 | 0.25 | −0.02 | −0.13 | −0.001 | −0.004 | 0.36 | 1.40 | −0.48 | −3.21** | −0.60 | −2.55* | −0.61 | −3.13** | |
| Not very satisfied | 0.39 | 2.02* | 0.09 | 0.75 | 0.05 | 0.27 | 0.08 | 0.53 | 0.12 | 0.38 | −0.30 | −1.66 | −0.41 | −1.43 | −0.31 | −1.30 | |
| Not satisfied at all | 0.63 | 2.40* | 0.32 | 2.07* | 0.41 | 1.67 | 0.43 | 2.19* | 0.80 | 2.13* | 0.08 | 0.36 | 0.18 | 0.52 | −0.15 | −0.54 | |
| Do not know | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | |||||||||
| The primary source of health information on COVID-19 | |||||||||||||||||
| Internet | −0.46 | −0.90 | −0.25 | −0.82 | −0.57 | −1.22 | 0.19 | 0.50 | −0.33 | −0.76 | −0.11 | −0.43 | −0.70 | −1.77 | −0.47 | −1.44 | |
| Television | −0.22 | −0.40 | −0.07 | −0.22 | −0.35 | −0.71 | 0.31 | 0.79 | −0.33 | −0.68 | −0.25 | −0.91 | −0.65 | −1.50 | −0.26 | −0.72 | |
| Radio | 0.83 | 0.62 | 1.33 | 1.69 | 2.67 | 2.14* | 2.67 | 2.67** | 0.11 | 0.13 | 2.11 | 4.30*** | 1.89 | 2.42* | 2.33 | 3.64*** | |
| Family members | −0.47 | −0.73 | −0.27 | −0.71 | −0.33 | −0.56 | −0.03 | −0.07 | 0.11 | 0.17 | −0.27 | −0.73 | −0.87 | −1.48 | −0.43 | −0.89 | |
| Other sources | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | |||||||||
†There were 333 respondents who participated in both the first and second surveys.
* p < 0·05, **p < 0·01, ***p < 0·001.
3.6. Precautionary measures about COVID-19 and its association with psychological impact and adverse mental health status
Table A.3 compares the precautionary measures adopted by our study respondents. Among the second survey respondents, significantly higher proportion avoided sharing utensils during meals, washed hands with soap and water, washed hands immediately after coughing, rubbing the nose, sneezing or touching contaminated objects, used face mask regardless of the symptoms and stayed at home for 20–24 h per day. Further analyses showed that observing better hygiene practices and avoidance of sharing utensils during meals were significantly associated with lower scores in IES-R and various DASS-21 subscales among both survey participants (Table 4 ).
Table 4.
Association of precautionary measures related to COVID-19 and the psychological impact as well as adverse mental health status during the first and second survey (n = 1738).
| Precautionary measures | The first survey (January 31– February 2, 2020) (N = 1210) † |
The second survey (February 28 – March 1, 2020) (N = 861) † |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Impact of event |
Stress |
Anxiety |
Depression |
Impact of event |
Stress |
Anxiety |
Depression |
||||||||||
| B | T | B | t | B | t | B | T | B | t | B | T | B | t | B | T | ||
| Covering mouth when coughing and sneezing | |||||||||||||||||
| Always | 0.02 | 0.08 | 0.02 | 0.19 | −0.19 | −1.15 | −0.09 | −0.64 | 0.08 | 0.39 | −0.32 | −2.65** | −0.59 | −3.11** | −0.57 | −3.64*** | |
| Most of the time | 0.18 | 0.96 | 0.09 | 0.78 | −0.09 | −0.48 | −0.04 | −0.27 | 0.35 | 1.58 | −0.35 | −2.71** | −0.56 | −2.74** | −0.46 | −2.73** | |
| Sometime | 0.40 | 1.89 | 0.12 | 0.94 | 0.09 | 0.45 | 0.02 | 0.10 | 0.47 | 1.84 | −0.22 | −1.44 | −0.55 | −2.33* | −0.40 | −2.07* | |
| Occasionally | 0.18 | 0.79 | −0.03 | −0.22 | −0.32 | −1.55 | −0.02 | −0.10 | 0.81 | 3.03** | 0.05 | 0.31 | −0.15 | −0.62 | −0.27 | −1.32 | |
| Never | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | |||||||||
| Avoidance of sharing utensils (e.g. chopsticks) during meals | |||||||||||||||||
| Always | −0.29 | −2.83** | −0.18 | −2.99** | −0.36 | −3.68*** | −0.31 | −3.92*** | −0.36 | −2.48* | −0.19 | −2.29* | −0.17 | −1.28 | −0.27 | −2.42* | |
| Most of the time | 0.17 | 1.35 | 0.01 | 0.20 | −0.03 | −0.28 | −0.07 | −0.76 | 0.12 | 0.72 | −0.18 | −1.92 | −0.06 | −0.39 | −0.18 | −1.43 | |
| Sometime | 0.23 | 1.78 | −0.02 | −0.19 | −0.13 | −1.07 | −0.20 | −1.99* | 0.18 | 1.06 | −0.16 | −1.58 | −0.06 | −0.37 | −0.23 | −1.80 | |
| Occasionally | 0.36 | 2.72** | 0.03 | 0.38 | −0.14 | −1.11 | −0.12 | −1.26 | 0.27 | 1.45 | 0.03 | 0.24 | 0.24 | 1.40 | 0.02 | 0.14 | |
| Never | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | |||||||||
| Washing hands with soap and water | |||||||||||||||||
| Always | −0.42 | −1.91 | −0.34 | −2.64** | −0.54 | −2.63** | −0.39 | −2.37* | −0.01 | −0.03 | −0.51 | −3.40** | −0.75 | −3.18** | −0.81 | −4.15*** | |
| Most of the time | −0.12 | −0.51 | −0.29 | −2.16* | −0.40 | −1.87 | −0.27 | −1.58 | 0.54 | 2.05* | −0.42 | −2.72** | −0.53 | −2.16* | −0.67 | −3.35** | |
| Sometime | 0.07 | 0.29 | −0.22 | −1.51 | −0.23 | −1.01 | −0.25 | −1.38 | 0.28 | 0.99 | −0.54 | −3.26** | −0.56 | −2.13* | −0.80 | −3.73*** | |
| Occasionally | 0.13 | 0.53 | −0.17 | −1.14 | −0.21 | −0.92 | −0.15 | −0.80 | 0.64 | 1.99* | −0.45 | −2.37* | −0.84 | −2.83** | −0.78 | −3.18** | |
| Never | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | |||||||||
| Washing hands immediaely after coughing, rubbing the nose, or sneezing | |||||||||||||||||
| Always | −0.47 | −3.11** | −0.31 | −3.42** | −0.63 | −4.43*** | −0.38 | −3.32** | −0.53 | −2.85** | −0.57 | −5.21*** | −0.67 | −3.87*** | −0.59 | −4.11*** | |
| Most of the time | 0.00 | −0.02 | −0.17 | −1.78 | −0.44 | −2.87** | −0.26 | −2.11 | 0.03 | 0.17 | −0.46 | −4.00*** | −0.48 | −2.63** | −0.47 | −3.14** | |
| Sometime | 0.02 | 0.11 | −0.12 | −1.28 | −0.41 | −2.70** | −0.18 | −1.46 | −0.04 | −0.17 | −0.47 | −3.85*** | −0.53 | −2.77** | −0.46 | −2.90** | |
| Occasionally | 0.14 | 0.83 | −0.08 | −0.81 | −0.29 | −1.84 | −0.04 | −0.35 | 0.03 | 0.15 | −0.56 | −4.31*** | −0.63 | −3.09** | −0.51 | −3.03** | |
| Never | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | |||||||||
| Wearing a face mask regarless of the presence or absence of symptoms | |||||||||||||||||
| Always | −0.19 | −0.95 | −0.21 | −1.78 | −0.43 | −2.28* | −0.37 | −2.44* | −0.43 | −1.01 | −0.80 | −3.19** | −0.96 | −2.43* | 1.05* | −3.25** | |
| Most of the time | 0.12 | 0.55 | −0.09 | −0.73 | −0.27 | −1.38 | −0.21 | −1.34 | −0.03 | −0.07 | −0.73 | −2.87** | −0.77 | −1.90 | 0.85* | −2.58* | |
| Sometime | 0.16 | 0.71 | −0.08 | −0.60 | −0.25 | −1.17 | −0.25 | −1.47 | −0.09 | −0.19 | −0.73 | −2.70** | −0.80 | −1.86 | 0.91* | −2.58* | |
| Occasionally | 0.52 | 2.11* | −0.04 | −0.27 | −0.14 | −0.62 | 0.006 | 0.03 | 0.42 | 0.80 | −0.72 | −2.33* | −0.67 | −1.36 | −0.93 | −2.31* | |
| Never | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | |||||||||
| Washing hands after touching contaminated objects | |||||||||||||||||
| Always | −0.11 | −0.37 | −0.21 | −1.23 | −0.52 | −1.90 | −0.53 | −2.40* | 0.02 | 0.04 | −0.80 | −3.20** | −1.09 | −2.76** | −1.17 | −3.61*** | |
| Most of the time | 0.19 | 0.62 | −0.15 | −0.81 | −0.37 | −1.34 | −0.41 | −1.83 | 0.41 | 0.94 | −0.75 | −2.94** | −0.87 | −2.18* | −0.99 | −3.00** | |
| Sometime | 0.40 | 1.21 | −0.01 | −0.03 | −0.03 | −0.08 | −0.27 | −1.11 | 0.63 | 1.28 | −0.65 | −2.28* | −0.71 | −1.57 | −0.95 | −2.58* | |
| Occasionally | 0.31 | 0.86 | −0.07 | −0.34 | −0.22 | −0.67 | 0.24* | −0.92 | 0.74 | 1.29 | −0.50 | −1.48 | −0.51 | −0.96 | −0.67 | −1.54 | |
| Never | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | |||||||||
| Feeling that too much unnecessary worry has been made about the COVID-19 epidemic | |||||||||||||||||
| Always | −0.47 | −4.18*** | −0.08 | −1.18 | 0.12 | 1.14 | 0.12 | 1.44 | −0.48 | −3.64*** | 0.09 | 1.15 | 0.07 | 0.60 | 0.09 | 0.91 | |
| Most of the time | −0.19 | −1.44 | −0.05 | −0.60 | 0.20 | 1.66 | 0.20 | 1.99* | −0.02 | −0.12 | 0.18 | 1.94 | 0.36 | 2.48* | 0.29 | 2.46* | |
| Sometime | −0.03 | −0.27 | −0.01 | −0.18 | 0.07 | 0.80 | 0.01 | 0.14 | −0.03 | −0.23 | −0.06 | −0.84 | −0.02 | −0.19 | 0.01 | 0.08 | |
| Occasionally | 0.13 | 1.15 | 0.03 | 0.49 | 0.12 | 1.20 | 0.10 | 1.18 | −0.08 | −0.64 | −0.05 | −0.62 | −0.01 | −0.09 | 0.06 | 0.61 | |
| Never | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | |||||||||
| The average number of hours staying at home per day to avoid COVID-19 | |||||||||||||||||
| [0–10] | −0.15 | −0.75 | −0.16 | −1.33 | −0.15 | 0.43* | −0.21 | 0.16* | −0.41 | −1.41 | 0.16 | 0.96 | 0.26 | 0.96 | 0.35 | 1.58 | |
| (10–20] | 0.11 | 1.02 | −0.03 | −0.46 | −0.06 | 0.58* | −0.08 | 0.33* | 0.22 | 1.45 | 0.10 | 1.13 | 0.17 | 1.18 | 0.01 | 0.12 | |
| (20–24] | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | |||||||||
†There were 333 respondents who participated in both the first and second survey.
*p < 0·05; **p < 0·01; ***p < 0·001.
4. Discussion
Our prospective longitudinal study describes the psychological impact and mental health of the general population in a country that was first affected by the COVID-19 outbreak. Although the number of confirmed cases of COVID-19 increased sharply from the first- to the second-survey recruitment, there were no significant changes in the mean DASS-stress, anxiety and depression scores. Although the mean IES-R scores were above the cut-off score for PTSD symptoms in both surveys, a statistically but not clinically significant temporal reduction in the mean IES-R scores was observed during the study period. The reduction in IES-R score could be due to the delicate balancing between controlling the spread of COVID-19 through lockdown and establishing confidence in public health measures.
The important unexpected finding of our study is the stable levels of stress, anxiety and depression despite sharp increases in the number of COVID-19 cases between the two surveys as well as statistically but not clinically significant reduction in the psychological impact on the general population. We believe that decisive and rapid measures imposed by the Chinese government were instrumental in reducing further spread of the virus (Cyranoski, 2020) but could safeguarded mental health in the general public. Nevertheless, prolonged lockdown had several adverse impacts on mental health, especially among the second- survey respondents aged 12-21·4 years who demonstrated a higher psychological impact of COVID-19. This age group mainly comprised of students who were affected by prolonged school closure, requiring online education support and uncertainty about examinations and matriculation arrangements. Respondents from both surveys who were parents with children younger than 16 years of age were not associated with higher IES-R or DASS-21 scores. This finding corresponds to the emerging pattern of resilience to severe outcomes of COVID-19 in children (Sominsky et al., 2020) and parents were less worried as a result.
During the initial outbreak, 15.04%, 9.42% and 5.62% of respondents reported one, two or three somatic symptoms respectively. The presence of somatic symptoms prompt researchers to consider the psychoneuroimmunological (PNI) framework of COVID-19. COVID-19 can cause acute respiratory syndrome with consequent release of pro-inflammatory cytokines, including interleukin (IL)-1β and IL-6 from the respiratory tract (Conti et al., 2020). These cytokines were commonly found to be increased in major depressive disorder (Liu et al., 2012, Ng et al., 2018) and functional somatic syndromes (Viljoen and Panzer, 2005). COVID-19, depression and functional somatic syndrome share the same PNI framework. Antidepressants (e.g. fluoxetine) was found to reduce pro-inflammatory cytokines by attenuating the behavioural and neuroendocrine effects of immune activation (Lu et al., 2017). Further research is required to study the effectiveness of antidepressants as part of the anti-inflammatory strategies against COVID-19 by reducing depression and somatic symptoms.
Our study highlights some public health implications. First, the strong association between physical symptoms and the psychological impact of COVID-19 outbreak supports importance of developing a rapid diagnostic test for COVID-19 with widespread availability to alleviate the psychological impact and psychiatric symptoms experienced by general population. Second, providing proper and repeated, yet simple, health education via the Internet and media is important for inculcating good hygiene practices. We observed that significantly higher proportion (10·8%) of the second-survey respondents did not know that COVID-19 could be transmitted by droplets, which might reduce the acceptability of certain precautionary measures. Third, the dissemination of health information via radio was associated with higher levels of anxiety and depression in both surveys. This observation may help the Governments and health authorities worldwide to modify the current methods of increasing public awareness. Perhaps, increased use of television (with participation by celebrities) and Internet (for detailed information with visual graphics and videos) to disseminate important health information might be more effective methods to change knowledge, attitude and practices among the general public. Fourth, mask-wearing, as a prevention method to reduce pathogen exposure (Kim and Su, 2020); was associated with lower levels of anxiety and depression. Perhaps, this led to significantly higher face-mask use by second-survey respondents, regardless of the presence of symptoms. This is an interesting and important phenomenon due to the divided scientific opinion on protective effects of usual face masks (Tan et al., 2019, Feng et al., 2020), coupled with their scarce availability. Efforts are needed to impart an unbiased and clear guidelines on the use of face masks and their types to allay the fears, confusions and sense of inferiority (for people with no access to the masks) among general population. Fifth, about one-third of respondents experienced social discrimination due to the COVID-19 epidemic. As a result, the WHO and governments from all countries should minimize the possibility of discrimination against certain groups of people regarding the origin of COVID-19. Lastly, ensuring the availability of essential services and commodities as well as financial security are essential to prevent psychological impact of the current pandemic. Governments worldwide need to take discrete and transparent efforts to win the confidence of general public and ensure optimal mental health and avoid psychological reflexes like panic buying.
Higher IES-R scores among the participants of the two surveys reflect the presence PTSD symptoms. During the COVID-19 pandemic, face-to-face psychotherapy is not feasible due to strict quarantine and lockdown measures. Mental health providers need to consider adopting online psychotherapy. Pre-implementation training of mental health professionals with involvement of multiple relevant agencies may help in various psychological interventions targeting PTSD symptoms. One example of evidence-based treatment is trauma-focused -cognitive behavior therapy (TF-CBT) (Cao et al., 2020). TF-CBT can be modified for the COVID-19 pandemic with emphasis on 1) education on the psychological impact of the COVID-19 pandemic; 2) development of psychosocial skills to optimize emotional and behavioral adjustment during quarantine and lockdown; 3) affective expression and problem-solving to handle emotions and common problems (e.g., shortage of necessities) encountered during quarantine and lockdown; 4) cognitive formulation to illustrate the relationships among thoughts, feelings and behaviors; 5) cognitive challenge or modification of unhelpful thoughts about COVID-19 and perceived discrimination; 5) trauma narration, in which public describe their personal traumatic experiences during COVID-19 pandemic; 6) home-based relaxation techniques and stress management skills with online guidance; 7) grief therapy to handle potential loss of family members or friends who died of COVID-19; 8) online peer support group session to talk to one other about their trauma; 9) enhancing safety and precaution to reduce the risk of contracting COVID-19 and 10) exposure to trauma reminders to overcome avoidance of situations that are no longer risky when the COVID pandemic is over. Delivery of TF-CBT during the COVID-19 pandemic requires healthcare organizations to develop online readiness and engagement of other stakeholders including counselors, psychologists, doctors, insurers and the public to accept the new model of mental health service.
Our study has some limitations. The general population sampled during the two surveys were not the same respondents. Although the anonymity of the questionnaire made this sampling unavoidable, 333 respondents completed both the first and second surveys. However, owing to the anonymous nature of the data collection, we could not pair respondents at the 2- time intervals. Another limitation is due to the self-reporting of the levels of psychological impact, anxiety, depression and stress, which may not always be aligned with objective assessment by mental health professionals. Nevertheless, psychological impact, anxiety, depression and stress are based on personal feelings, and self-reporting was paramount during the COVID-19 pandemic (Tan et al., 2019). In the same vein, we could not rule out the possibility that some of the respondents might have been infected with COVID-19. There were only 0.9% of the first-survey respondents and 0.5% of second-survey respondents who received testing on COVID-19. Due to low prevalence of testing, the number of respondents who were tested positive for COVID-19 was even fewer. Nevertheless, we could not rule out the possibility that some respondents were asymptomatic carriers with mild COVID-19 symptoms (Wang et al., 2020). Finally, the understanding of COVID-19 was limited when we first designed this study. We did not measure neurological symptoms (e.g. loss of smell or taste) that were recently discovered to be associated with COVID-19 (Wu et al., 2020).
5. Conclusion
During the initial phase and four weeks later during the COVID-19 epidemic in China, there was a statistically but not clinically significant reduction in psychological impact. There were no significant temporal changes in the levels of stress, anxiety and depression between the first and second surveys. We identified the specific target groups (young and students) prone for the psychological impact of the current COVID-19 outbreak as well as various factors that might help in safeguarding the mental health of general population. Various Governments should focus on effective methods of dissemination of unbiased knowledge about the disease, teaching correct methods for containment, ensure availability of essential services and commodities, provide sufficient financial support for the present and future in order to win the current war against COVID-19.
Author contribution
Concept and design: Cuiyan Wang, Riyu Pan, Roger Ho.
Acquisition, analysis, and interpretation of data: Cuiyan Wang, Riyu Pan, Linkang Xu, Faith Choo, Xiaoyang Wan, Yilin Tan.
Drafting of the manuscript: Cuiyan Wang, Roger Ho, Faith Choo, Vijay Sharma, Cyrus Ho.
Critical revision of the manuscript: Roger Ho, Vijay Sharma, Roger McIntyre, Bach Tran, Cyrus Ho.
Statistical analysis: Cuiyan Wang, Riyu Pan, Linkang Xu, Faith Choo, Xiaoyang Wan, Yilin Tan.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
This work was supported by grants from the Huaibei Normal University (to Cuiyan Wang), Vingroup Innovation Foundation (VINIF) COVID research grant (VINIF.2020.Covid19.DA07 to Bach Tran) and National University of Singapore, Singapore iHeathtech Other Operating Expenses (R-722-000-004-731 to Roger Ho).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bbi.2020.04.028.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Cao W., Fang Z., Hou G. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christianson S., Marren J. The impact of event scale – revised (IES-R) Medsurg. Nurs. 2012;21:321–322. [PubMed] [Google Scholar]
- Conti P., Ronconi G., Caraffa A. Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by Coronavirus-19 (COVI-19 or SARS-CoV-2): anti-inflammatory strategies. J. Biol. Regul. Homeost. Agents. 2020;34 doi: 10.23812/CONTI-E. [DOI] [PubMed] [Google Scholar]
- Cyranoski D. What China's coronavirus response can teach the rest of the world. Nature. 2020 doi: 10.1038/d41586-020-00741-x. [DOI] [PubMed] [Google Scholar]
- Europe on Lockdown From COVID-19. Jewish Journal, 2020. (Accessed March 22, 2020, at https://jewishjournal.com/commentary/opinion/312317/europe-on-lockdown-from-covid-19/).
- Feng S., Shen C., Xia N., Song W., Fan M., Cowling B.J. Rational use of face masks in the COVID-19 pandemic. Lancet Respir. Med. 2020 doi: 10.1016/S2213-2600(20)30134-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao, F.T.W., Jang, L., Zhang, L., Jiang, X., McIntyre, R.S., Zhang, Z., Sun, J., Ho, R., Ho, C., Tam, W., 2019. Psychological impact on people with and without psychiatric illnesses in Chongqing, China during the peak of 2019 coronavirus disease (COVID-19) outbreak with strict quarantine measures. In publication 2020.
- Ho C.S., Chee C.Y., Ho R.C. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann. Acad. Med. Singapore. 2020;49:1–3. [PubMed] [Google Scholar]
- Hosey M.M., Bienvenu O.J., Dinglas V.D. The IES-R remains a core outcome measure for PTSD in critical illness survivorship research. Crit. Care. 2019;23:362. doi: 10.1186/s13054-019-2630-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joob B., Wiwanitkit V. Traumatization in medical staff helping with COVID-19 control. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang L., Ma S., Chen M. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S.W., Su K.P. Using psychoneuroimmunity against COVID-19. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z., Ge J., Yang M. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Ho R.C., Mak A. Interleukin (IL)-6, tumour necrosis factor alpha (TNF-α) and soluble interleukin-2 receptors (sIL-2R) are elevated in patients with major depressive disorder: a meta-analysis and meta-regression. J. Affect. Disord. 2012;139:230–239. doi: 10.1016/j.jad.2011.08.003. [DOI] [PubMed] [Google Scholar]
- Lu Y., Ho C.S., Liu X. Chronic administration of fluoxetine and pro-inflammatory cytokine change in a rat model of depression. PloS One. 2017;12 doi: 10.1371/journal.pone.0186700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahase E. China coronavirus: WHO declares international emergency as death toll exceeds 200. BMJ. 2020;368:m408-m. doi: 10.1136/bmj.m408. [DOI] [PubMed] [Google Scholar]
- Ng A., Tam W.W., Zhang M.W. IL-1β, IL-6, TNF- α and CRP in elderly patients with depression or alzheimer's disease: systematic review and meta-analysis. Sci. Rep. 2018;8:12050. doi: 10.1038/s41598-018-30487-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton P.J. Depression Anxiety and Stress Scales (DASS-21): psychometric analysis across four racial groups. Anxiety Stress Coping. 2007;20:253–265. doi: 10.1080/10615800701309279. [DOI] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen. Psychiatr. 2020;33 doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin E.J., Baden L.R., Morrissey S., Campion E.W. Medical journals and the 2019-nCoV outbreak. N. Engl. J. Med. 2020;382:866. doi: 10.1056/NEJMe2001329. [DOI] [PubMed] [Google Scholar]
- Sominsky L., Walker D.W., Spencer S.J. One size does not fit all – patterns of vulnerability and resilience in the COVID-19 pandemic and why heterogeneity of disease matters. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan B.Y.Q., Chew N.W.S., Lee G.K.H. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann. Intern. Med. 2020 doi: 10.7326/M20-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan, W.H.F., McIntyre, R.S., Jiang, L., Jiang, X., Zhang, L., Zhao, X., Zou, Y., Hu, Y., Luo, X., Zhang, Z., 2020. Returning to Work during the Coronavirus Disease 2019 (COVID-19) Epidemic: Immediate Mental Health Status of Chinese Workforce after Strict Quarantine Measures in Chongqing, China. In publication 2020.
- Viljoen M., Panzer A. Proinflammatory cytokines: a common denominator in depression and somatic symptoms? Canad. J. Psychiatry Revue canadienne de psychiatrie. 2005;50:128. doi: 10.1177/070674370505000216. [DOI] [PubMed] [Google Scholar]
- Wang Y., Liu Y., Liu L., Wang X., Luo N., Ling L. Clinical outcome of 55 asymptomatic cases at the time of hospital admission infected with SARS-Coronavirus-2 in Shenzhen, China. J. Infect. Dis. 2020 doi: 10.1093/infdis/jiaa119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17:E1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO team arrives in Iran; COVID-19 surges in Korea, Italy. Center for Infectious Disease Research and Policy, 2020. (Accessed March 22, 2020, at http://www.cidrap.umn.edu/news-perspective/2020/03/who-team-arrives-iran-covid-19-surges-korea-italy).
- https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. World Health Organizaton, 2020. (Accessed March 22 2020, 2020, at https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020).
- Wu Y., Xu X., Chen Z. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanon C., Brenner R.E., Baptista M.N. Examining the dimensionality, reliability, and invariance of the depression, anxiety, and stress scale-21 (DASS-21) across eight countries. Assessment. 2020 doi: 10.1177/1073191119887449. 1073191119887449. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.