Abstract
Objective:
To identify scalable interventions for improving sexual minority mental health and health-risk behavior, this study tested the efficacy of two self-guided online writing interventions – expressive writing and self-affirmation. To reach sexual minority young adults living in high-stigma, low-resource settings, we developed and tested these interventions in Appalachian Tennessee.
Method:
In consultation with sexual minority young adults (n=10) and stakeholders (n=10) living in Appalachian Tennessee, we adapted two writing interventions that we then delivered to 108 local sexual minority young adults (Mage=23.68, SD=3.11). Participants, representing diverse sexual and gender identities and socioeconomic backgrounds, were randomly assigned to participate in a 3-session expressive writing intervention, self-affirmation intervention, or neutral control. Participants completed mental health and health-risk behavior measures at baseline, post-intervention, and 3-month follow-up.
Results:
Compared to the neutral control, expressive writing exerted 3-month improvements in depressive symptoms (d=0.48) and general psychological distress (d=0.36) whereas self-affirmation exerted improvement in suicidal ideation (d=0.62) and drug abuse (d=0.59). Participants who were exposed to greater contextual minority stressors common in rural regions (i.e., discrimination, victimization) experienced significantly greater 3-month reductions in depression from expressive writing and self-affirmation compared to control. Those who experienced greater discrimination also experienced significantly greater 3-month reductions in suicidality from self-affirmation compared to control.
Conclusions:
Brief writing interventions exert significant impact on the mental health of young adult sexual minorities, especially those exposed to minority stress. Future research can consider strategies for population-level implementation, especially in high-stigma, low-resource settings.
Public Health Significance:
This study responds to the pressing need for efficacious interventions to improve sexual minority young adult mental health and health-risk behavior. We find evidence that two brief online writing interventions – expressive writing and self-affirmation – can be tailored to meet the needs of geographically dispersed sexual minority young adults and significantly improve their mental health. Results notably provide among the first randomized controlled trial evidence for an intervention capable of reducing suicidality among sexual minorities exposed to high degrees of minority stress.
Keywords: sexual minority, lesbian, gay, bisexual, transgender, evidence-based treatment, empirically-supported treatment, rural
Sexual orientation disparities in mental health problems and health-risk behaviors begin early in development and peak in young adulthood (Irish et al., 2019; Rice, Vasilenko, Fish, & Lanza, 2019). Specifically, sexual minority young adults show substantially elevated prevalence of depression, anxiety, suicidality, alcohol and drug use, and sexual-risk behavior compared to heterosexual young adults (Everett, 2013; King et al, 2008; Talley, Hughes, Aranda, Birkett, & Marshal, 2014). Sexual minorities’ disproportionate exposure to stigma-related stress, especially in adolescence and young adulthood, represents the most plausible explanation for these disparities and their age patterning (Bränström, Hatzenbuehler, & Pachankis, 2016).
In addition to age, geography also predicts mental health problems and health-risk behaviors among sexual minorities. Compared to urban areas, many rural areas of the US contain high degrees of anti-LGBTQ structural stigma (e.g., discriminatory and unjust laws, policies, and community attitudes that preclude equal life chances for the stigmatized). Structural stigma reflects and perpetuates anti-LGBTQ sentiment in rural institutions, including in local religious communities, families, and healthcare settings (Kosciw, Greytak, & Diaz, 2009; Swank, Fahs, & Frost, 2013; Williams, Bowen, & Horvath, 2005). Although sexual minority young adults living in many rural areas of the US face chronic exposure to stigma and discrimination (Preston & D’Augelli, 2013), whose effects are amplified by socioeconomic strain (Barnes, Hatzenbuehler, Hamilton, & Keyes, 2014; McGarrity & Huebner, 2014), they also often have limited access to LGBTQ-specific coping resources (Cohn & Hastings, 2010; D’Augelli, 2006). As a result, sexual minority young adults in rural areas bear a disproportionate burden of stress-sensitive mental health problems and health-risk behaviors compared to their urban peers (Galliher, Rostosky, & Hughes, 2004; Poon & Saewyc, 2009) without ready access to identity-supportive interventions (Hatzenbuehler, Keyes, & McLaughlin, 2011).
Despite clear and consistent evidence that sexual minority young adults represent one of the highest risk populations for stress-sensitive mental health problems and health-risk behaviors, relatively few stress coping interventions have been tested for efficacy in this population (Chaudoir, Wang, & Pachankis, 2017; Pachankis, 2018). Although a few stress coping interventions for sexual minorities have been piloted in uncontrolled trials (e.g., Lucassen et al., 2015; Riggle, Gonzalez, Rostosky, & Black, 2014), even fewer have been tested in randomized controlled trials (e.g., Israel et al., 2019; Pachankis, Hatzenbeuhler, Rendina, Safren, & Parsons, 2015). The briefest and most portable of these interventions tend to yield small effect sizes limited to stigma-specific outcomes (e.g., internalized stigma; Israel et al., 2019), whereas more intensive interventions involving in-person engagement show comparatively larger effect sizes across mental health problems and health-risk behaviors (e.g., Pachankis et al., 2015). Identifying interventions that possess both efficient reach across geographies and robust effects across mental health problems and health-risk behaviors disproportionately affecting sexual minority young adults remains a high-priority public health need.
Brief Online Writing Interventions
Interventions involving written expression of stress and coping experiences, when delivered online, can potentially provide efficient help to individuals living out-of-reach of brick-and-mortar support. One such intervention – expressive writing – has received substantial empirical support across stress-exposed populations and mental health outcomes (e.g., Pennebaker & Beall, 1986). Expressive writing interventions, in which one writes about a stressful or traumatic event for about 20 minutes per day for several days, can theoretically help facilitate stress coping via exposure to and extinction of past traumatic experiences. Expressive writing interventions tend to show robust effects across mental health outcomes, but typically weak, non-significant effects across health-risk behavioral outcomes (Frattaroli, 2006). Expressive writing interventions that provide directed writing prompts and examples of the intended writing topic, rather than more general prompts, show the strongest effects, yielding moderate average effect sizes on mental health improvement across over 100 prior studies (Frattaroli, 2006).
Notably, two of the few randomized controlled trials of stress coping interventions with sexual minorities examined the efficacy of expressive writing interventions (Lewis et al., 2005; Pachankis & Goldfried, 2010). One of these studies, conducted with college student sexual minority men across the US, found that expressive writing increased positive affect and, for those with low social support, reduced depression relative to a neutral control condition (Pachankis & Goldfried, 2010). The other study, conducted with a community sample of lesbian adults, found that expressive writing reduced perceived stress for those who were less open about their sexual identity, but increased stress for those who were more open; this moderation did not exist for a neutral control condition (Lewis et al., 2005).
Despite the preliminary promise of expressive writing interventions for sexual minority mental health, several important questions remain. First, whether expressive writing interventions can benefit sexual minority young adults living in low-resource, high-stigma areas, where efficient interventions unconstrained by geographic boundaries are highly needed, remains unknown. Second, the extent to which stigma-related contextual factors common in such areas, such as discrimination and victimization, might moderate the efficacy of such interventions remains unknown. Third, also unknown is whether other writing interventions, possibly operating through other theoretical mechanisms, might reduce not only mental health problems but also health-risk behaviors that are common among sexual minorities (e.g., alcohol use, drug use, HIV-risk behavior) but less likely to be impacted by expressive writing.
Although having a smaller evidence base than expressive writing interventions, self-affirmation interventions have also shown promise for improving mental health and health-risk behavioral outcomes among stigmatized populations. Brief self-affirmation interventions build coping self-efficacy by helping members of threatened groups construe stigma-based adversity as common, temporary, and external to the self (e.g., Walton & Cohen, 2011). They are also theorized to reduce defensive responding to self-evaluative threats (Epton et al., 2015). For instance, one such intervention asked African American college students to write an essay, ostensibly for future new students, about how their experiences during their first year of college were initially challenging but ultimately surmountable (Walton & Cohen, 2011). Immediately post-intervention, participants in this intervention condition, compared to those in multiple control conditions, experienced a greatly attenuated association between adversity events and threatened sense of belonging. Three years post-intervention, these participants experienced significantly higher academic performance and fewer medical visits than control participants. Notably, by instructing recipients to provide advice to similar others, this type of “saying-is-believing” intervention reduces inadvertent perpetuation of stigma by instead communicating to recipients that they are the benefactors, rather than beneficiaries, of the intervention. To date, the efficacy of such an intervention has not been examined for sexual minority mental health and health-risk behavioral outcomes, despite theoretical promise for helping young adult sexual minorities develop self-efficacy for coping with adversity. Modified versions of such interventions have appeared as part of larger treatment packages for sexual minority men’s stigma coping (Lin & Israel, 2012; Pachankis et al., 2015). However, being packaged alongside numerous other intervention techniques prevents the type of dismantling necessary for determining the efficacy of this stand-alone brief intervention capable of broad dissemination to high-need populations of sexual minorities.
The Present Study
To address the notable gap in evidence-based interventions for sexual minorities, especially for those living in high-stigma, low-resource areas such as the rural US, the present study sought to test the efficacy of two brief online interventions holding preliminary promise. This study compared the efficacy of expressive writing and self-affirmation interventions to a neutral control. Based on prior evidence drawn from other populations, we expected that expressive writing would exert a significant impact on mental health outcomes compared to control (Frattaroli, 2006) whereas self-affirmation writing would exert a significant impact on health-risk behavioral outcomes compared to control (e.g., Walton & Cohen, 2011). The impact of expressive writing on health-risk behavioral outcomes has been repeatedly shown to be weak or non-existent (Frattaroli, 2006), which we also hypothesized here. Conversely, the impact of self-affirmation seems to be somewhat specific to behavioral outcomes (e.g., Epton, Harris, Kane, van Koningsbruggen, & Sheeran, 2015). Self-affirmation could theoretically also reduce mental health problems, although this possibility has been less frequently studied.
With the goal of identifying sexual minorities who could especially benefit from these interventions, we also examined the influence of contextual minority stress moderators of intervention efficacy relevant to sexual minorities in high-stigma, low-resource areas. Specifically, we examined whether sexual minorities who are exposed to LGBTQ-related discrimination and victimization would benefit most from these interventions. Based on past tests of intervention moderation with this population (e.g., Feinstein et al., 2018; Millar, Wang, & Pachankis, 2016), we reasoned that those who experienced more contextual minority stressors would have the most to gain from these interventions. Knowing whether and under what contexts these brief online writing interventions work can provide the treatment community with needed guidance for reaching sexual minority young adults, who despite being at risk of mental health problems and health-risk behaviors, often exist out-of-reach of identity-affirming evidence-based treatments because of structural barriers.
Method
Participants
Upon ethical review by the Yale University Human Subjects Committee (protocol number: 1512016952, “Development and preliminary trial of a brief, portable health intervention for rural sexual minority emerging adults,” we recruited, in 2017 and 2018, 108 sexual minority young adults who were living in Northeast Tennessee, a part of South Central Appalachia containing high structural stigma toward sexual minorities and few LGBTQ-specific formal support resources (Human Rights Campaign, 2018). Participants were specifically recruited from six counties (i.e., Washington, Sullivan, Carter, Unicoi, Greene, and Hawkins) through tailored advertising on geo-targeted websites (e.g., Facebook); bulletin boards and listservs of regional colleges and universities; in-person announcement and flyers at local businesses, community events, and the gay-straight alliances of area schools; and word of mouth. Participants completed a brief online survey to confirm eligibility, defined as: being age 18–29; identifying as a sexual minority (e.g., lesbian, gay, bisexual, pansexual, queer); currently living in one of the eligible six counties; and having daily personal internet access. Participants emailed a photo of an identification card, typically a driver’s license, as proof of age. Figure 1 describes the sample size throughout study phases, including exclusion and ineligibility of screened participants.
Figure 1.
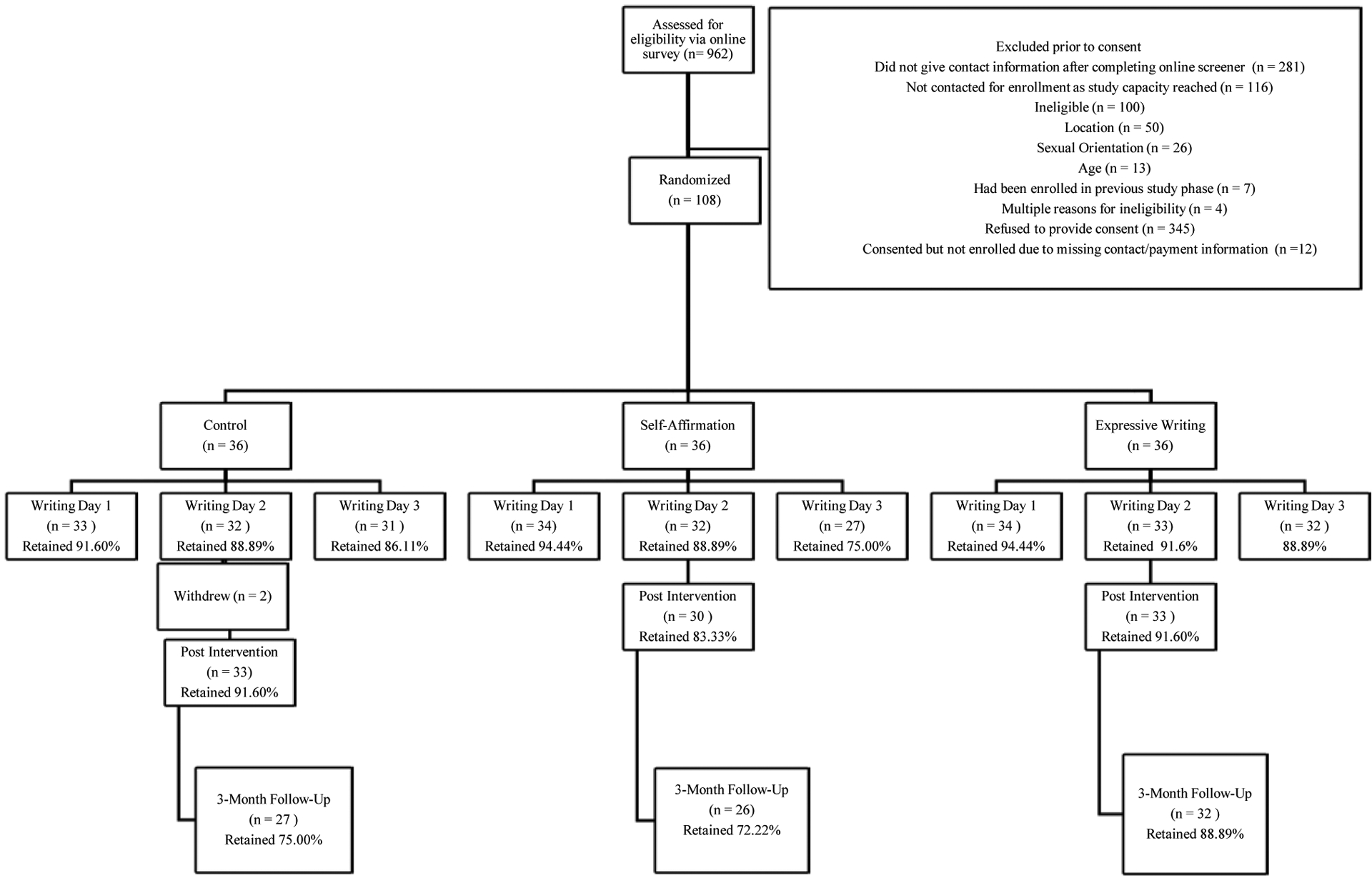
Flow diagram of participants’ progress through study phases.
Participants were on average age 23.68 (SD = 3.11). The majority were white (87.1%), reflecting the demographic makeup of South Central Appalachia (Pollard & Jacobson, 2018). The majority also reported being assigned a female sex at birth (70.4%) and currently identified as women (55.6%). Notably, gender minority participants who also identified as sexual minorities were not excluded from the study: 24.1% of participants identified as transgender or gender non-conforming. A slight majority (51.9%) identified as gay or lesbian; many also identified as bisexual (27.8%) and pansexual (13.9%). About half had a college degree (46.3%) and most were employed (80.6%), although many earned less than $10,000 per year (38.0%). The majority came from a background described as lower middle class, working class, or poor (63.9%). Most were in a relationship (67.6%).
As a reflection of the structural climate surrounding sexual minorities in rural Appalachia, 39 (36.1%) reported not being out to at least one parent, 18 (16.7%) reported healthcare avoidance in the past year due to fears of sexual orientation discrimination, and a significant number (i.e., 19; 17.6%) indicated that a professional (such as a psychologist, counselor, or religious advisor) had attempted to change their sexual orientation.
Measures
At baseline, participants completed an online assessment of demographic factors and potential contextual moderators. Outcomes were assessed at baseline, one week after the last writing day (i.e., post-intervention), and at a 3-month follow-up. In primary analyses, we only utilized the baseline and 3-month follow-up assessments given the incomparability of timeframes for the baseline and 3-month follow-up assessments (i.e., past 3 months) compared to the post-intervention assessment (i.e., past week). In supplemental analyses, we also compare post-intervention to baseline assessments with the caveat that such analyses must be interpreted in light of the fact that different timeframes were assessed at post-intervention rendering them incomparable to the baseline or 3-month follow-up assessments.
Outcomes.
Center for Epidemiological Studies -- Depression Scale (CESD; Radloff, 1977).
The CESD is a 20-item scale that asks individuals to report how often they have experienced symptoms of depression in the past week (e.g., “I was bothered by things that usually don’t bother me,” “I felt depressed”) on a 4-point scale ranging from 1 (Rarely or none of the time [less than 1 day]) to 4 (Most or all of the time [5–7 days]). At baseline and 3-month follow-up assessments, participants completed the CESD in reference to the past 3 months. At the post-intervention assessment, individuals were asked these questions in reference to the past week (Cronbach’s α at baseline = .92).
Brief Symptom Inventory (BSI; Derogatis & Melisaratos, 1983; Meijer, de Vries, & van Bruggen, 2011).
The present study used the 18-item version of the BSI, which asks individuals to report how much they have been distressed or bothered by depressive, anxious, and somatic symptoms (e.g., “feeling no interest in things,” “feeling tense or keyed up”). Responses are on a 5-point scale and range from 0 (Not at all) to 4 (Extremely). At baseline and 3-month follow-up assessments, individuals were asked these questions about the past 3 months At the post-intervention assessment, individuals were asked these questions in reference to the past week (Cronbach’s α at baseline = .93).
Beck Anxiety Inventory (BAI; Beck, Epstein, Brown, & Steer, 1988).
The BAI is a 21-item scale that asks individuals to report how much they have been bothered by symptoms of anxiety in the past week (e.g., “terrified or afraid,” “faint/lightheaded”). Responses are on a 4-point scale ranging from 0 (Not at all) to 3 (Severely – it bothered me a lot). At baseline and 3-month follow-up assessments, individuals were asked these questions about the past 3 months. At the post-intervention assessment, individuals were asked these questions about the past week (Cronbach’s α at baseline = .98).
Suicidal Ideation Attributes Scale (SIDAS; Spijker et al., 2014).
The SIDAS is a 5-item scale that asks individuals about frequency of thoughts of suicide, controllability of these thoughts, how close they have come to making a suicide attempt, distress resulting from thoughts of suicide, and degree to which thoughts of suicide have interfered with daily life. Responses are on an 11-point scale ranging from 0 (Never or Not at All) to 10 (Always or Extremely). At baseline and 3-month follow-up assessments, individuals were asked these questions about the past 3 months. At the post-intervention assessment, individuals were asked these questions in reference to the past week. Participants who indicated no thoughts about suicide over the past three months were not asked the subsequent questions (Cronbach’s α at baseline = .91).
Alcohol Use Disorders Identification (AUDIT; Saunders, Aasland, Babor, de la Fuente, & Grant, 1993).
The AUDIT is a 10-item scale used to assess hazardous drinking in the past 3 months (e.g., “how often did you have a drink containing alcohol?”). Responses are on a 5-point scale (i.e., 0 [Never] to 4 [daily or almost daily]) and a score of 8 or higher serves as a clinical cut-off indicating hazardous or harmful alcohol use (Cronbach’s α at baseline = .83).
Short Inventory of Problems-Modified for Drug Use (SIP-DU) (Allensworth Davies, Cheng, Smith, Samet, & Saitz, 2012).
The SIP-DU is a 15-item scale that assesses the social, physical, interpersonal and intrapersonal effects of drugs use on participants (e.g. “I have been unhappy because of my drug use”). Participants endorse whether each item is true (i.e., 0 [no], 1 [yes]). At baseline and 3-month follow-up assessments, individuals were asked these questions about the past 3 months. At the post-intervention assessment, individuals were asked these questions in reference to the past week (Cronbach’s α at baseline = .88).
HIV-risk Behavior.
This questionnaire, created for this study based on the approach used in previous studies of sexual risk among sexual minority young adults (e.g., Pachankis, Eldahan, & Golub, 2016), asked participants to report their HIV status (i.e., negative, positive, or unknown), pre-exposure prophylaxis (PrEP) usage, relevant characteristics of all past-3-month partners (i.e., main vs. casual; gender), partner HIV status (i.e., negative, positive, or unknown), partner PrEP usage, types of sex acts and frequency of each (i.e., mutual masturbation, oral, anal, and vaginal/frontal), condom usage, prosthetic usage, and sexual position (i.e., insertive or receptive). Reflecting the biomedical realities of HIV transmission risk in this population, HIV risk was defined as condomless anal or vaginal/frontal sex (not counting the sole use of prosthetics) in the absence of PrEP, with any HIV+ partner (except primary HIV+ partners with a known undetectable viral load) or status-unknown partner. HIV-risk behavior was treated as a count of these acts. At baseline and 3-month follow-up assessments, individuals were asked to report their HIV risk in the past 3 months. At the post-intervention assessment, individuals were asked these questions in reference to the past week.
Contextual Moderators.
Everyday discrimination (Cochran & Mays, 2001; Williams, Yu, Jackson, & Anderson, 1997).
The Everyday Discrimination Scale assesses participants’ perceived discrimination due to their sexual orientation (e.g., “you are treated with less courtesy than other people”). Responses are on a 6-point Likert scale ranging from 1 (Never) to 6 (Almost every day). This scale was adapted from the everyday discrimination scale used to assess experiences with racism (Williams et al., 1997) and has been previously used to assess sexual orientation related discrimination (e.g., Cochran & Mays, 2001; Cronbach’s α at baseline = .93).
LGBTQ victimization (Birkett, Newcomb, & Mustanski, 2015; D’Augelli, Hershberger, & Pilkington, 1998).
We used a 10-item measure that asks individuals to assess their past-3-month experiences with victimization related to their LGBTQ identity (e.g., “threatened with physical violence”) on a 4-point scale ranging from 0 (Never) to 3 (3 or more times) (Cronbach’s α at baseline = .86).
Procedure
One week after completing baseline questionnaires, participants received an email link containing access to and instructions for the first writing session. On the morning after completing a writing session, participants would receive a link for the subsequent writing session, up to three sessions across three consecutive days. In the event of missed sessions, participants could not advance to a subsequent writing session until they had completed the one that was overdue. Participants who missed a writing session received reminder emails once per day, for up to two weeks, until they completed the writing session. Participants received $10 for each writing session and $90 for completing all three assessments (see Figure 1 for participants’ progress through study phases).
Participant engagement and intervention adherence.
The online writing conditions contained a timer feature that required participants to spend 20 minutes addressing the writing prompt. Average word count per submission was 503 words for expressive writing, 454 for self-affirmation, and 453 words for control. A study staff member read each submission for participant safety (e.g., references to suicidality) and adherence (e.g., to the respective writing prompt). No safety-related issues were detected in the review. All submissions (100%) adhered to the assigned prompt in terms of 1) writing about an LGBTQ-related stressor for the expressive writing submissions, 2) addressing each of the self-affirmation prompts (e.g., parental rejection, religious rejection, peer rejection), or 3) describing daily events for the control submissions.
Intervention adaptation process.
While expressive writing and self-affirmation interventions are well-established for delivery with the general population and other minority populations (Frattaroli, 2006; Walton & Cohen, 2011), neither intervention has benefited from LGBTQ-resonant writing prompts derived in consultation with sexual minority community members themselves. Therefore, in order to create culturally relevant writing prompts for these interventions, we consulted 20 sexual minority young adults and community member stakeholders in Northeast Tennessee across two in-person focus groups and, for those unavailable for or uncomfortable with a group format, five individual interviews.
Ten interviewees were sexual minority young adults (Mage = 23.00, SD = 2.75) recruited from geo-targeted websites, LGBTQ community listservs, and flyers at local businesses and university. Ten were community stakeholders (Mage = 46.40, SD = 13.99) affiliated with online-or community-based organizations that provide services to sexual minority emerging adults in Northeast Tennessee; they were recruited through in-person or email invitations to local LGBTQ advocates and service providers with experience working with sexual minority young adults (e.g., counselors, teachers, social service providers). Of the 10 sexual minority young adults, 50% identified as female, 20% identified as male, 30% identified as non-binary or gender non-conforming; 40% as bisexual; 30% as lesbian; 20% as gay; and 10% as pansexual. Of the 10 stakeholders, 50% identified as female and 50% identified as male; 40% identified as gay; 20% as lesbian; 10% as bisexual; 10% as bi/pansexual, 10% as heterosexual, and 10% did not specify. All 10 young adults and nine of the stakeholders identified their race/ethnicity as white. One stakeholder identified as Hispanic/Latinx.
Interviewees were asked to describe stressors that sexual minority young adults in their area experience as a result of being a sexual minority. The first, second, and sixth authors reviewed transcripts of the interviews to derive the most typical stress experiences reported in order to use those examples in the writing prompts.
Expressive writing prompts.
To adapt expressive writing prompts for sexual minority young adults, we derived a general list of the types of stressors and contexts commonly described across interviewees as characterizing sexual minority stress in Northeast Tennessee. Based on a meta-analysis finding that providing examples of the intended writing topic enhances expressive writing efficacy (Frattaroli, 2006), this general list was provided to participants assigned to the expressive writing condition as an example of the types of stressors about which to focus in their writing (see Appendix A for actual instructions). Participants assigned to the expressive writing condition were asked to write for 20 minutes once per day for three consecutive days.
Self-affirmation prompts.
For self-affirmation, we created three vignettes based on modal examples of severe sexual minority stress shared across interviewees. The three vignettes respectively described family rejection, rejection by one’s religious community, and school-based victimization experienced by a late adolescent or young adult sexual minority person living in East Tennessee. While fictional, these vignettes represented an amalgam of the actual stress stories shared by interviewees (see Appendix A for actual instructions).
Self-affirmation participants received one distinct vignette per day. Presented vignettes were identical across participants, although they were matched to each participant’s sexual identity, gender identity, and race/ethnicity. Upon reading a vignette of the sexual minority young person experiencing severe stress, participants were asked how they themselves would advise this person based on their own experience as a sexual minority. Participants assigned to the self-affirmation condition were asked to write for 20 minutes once per day for three consecutive days.
Control prompts.
For the control condition, participants were asked to write for 20 minutes once per day about their daily activities since waking up that day (see Appendix A for actual instructions).
The study protocol was reviewed by the Yale University Human Subjects Committee. All participants provided consent by phone for eligibility screening and online for the full study. The study was pre-registered as a clinical trial (ClinicalTrials.gov identifier: NCT03751020).
Data Analysis Plan
Efficacy analyses compared expressive writing with the control condition and self-affirmation with the control condition utilizing an intent-to-treat approach, including all randomized participants (n = 108). Symptom-based outcomes (i.e., depression, psychological distress, anxiety) were analyzed with the full sample; indeed, nearly the entire sample endorsed non-zero levels of these outcomes (i.e., depression: n = 107; psychological distress: n = 106; anxiety: n = 107). For those outcomes that were not as consistently endorsed at baseline (i.e., suicidality, alcohol abuse, drug abuse, and HIV-risk behaviors), analyses were limited to those participants who did endorse them at baseline. This decision is empirically supported by the fact that very few participants who reported zero alcohol abuse (n = 2), drug abuse (n = 6), HIV-risk behavior (n = 2), or suicidality (n = 6) at baseline went on to develop those problems at 3-month follow-up. This decision is conceptually supported by the fact that participants were not recruited into this study as a function of their engagement in these health-risk behaviors as they would have been if this were a prevention study and by the fact that the intervention was not expected to result in an increase in these behaviors among those who did not engage in them at baseline. We did, however, conduct supplemental analyses that included all participants regardless of their endorsement of such behavior at baseline.
We first used t-tests and chi-square tests to examine demographic differences among the three intervention conditions (Table 1). Employment status trended toward statistically significant group differences across conditions at baseline (χ2 = 11.46, p = .08) and was therefore used as a covariate in all analyses. The covariance structure within participants was modeled as unstructured and effect sizes were calculated using pooled pretest standard deviations for weighting differences between the baseline and follow-up means to account for repeated measures (Lenhard & Lenhard, 2016; Morris, 2008).
Table 1.
Demographic variables
| Control n = 36 |
Expressive writing n = 36 |
Self-affirmation n = 36 |
Condition comparisons | |||||
|---|---|---|---|---|---|---|---|---|
| Variable | n | % | n | % | n | % | ||
| Age, years | ||||||||
| Mean | 23.47 | 23.42 | F = 0.60 | p = 0.55 | ||||
| SD | 3.24 | 2.88 | 3.25 | |||||
| Race | ||||||||
| American Indian/Alaskan Native | 0 | 0.00 | 2 | 5.56 | 0 | 0.00 | χ2 = 0.16 | p = 0.92 |
| Asian | 1 | 2.78 | 0 | 0.00 | 0 | 0.00 | ||
| Black/African American | 2 | 5.56 | 4 | 11.11 | 4 | 11.11 | ||
| Native Hawaiian/Pacific Islander | 1 | 2.78 | 0 | 0.00 | 0 | 0.00 | ||
| White | 33 | 91.67 | 33 | 91.67 | 34 | 94.44 | ||
| Other | 1 | 2.78 | 0 | 0.00 | 0 | 0.00 | ||
| Hispanic/Latino | ||||||||
| No | 35 | 97.20 | 36 | 100 | 35 | 97.20 | χ2 = 102 | p = 0.60 |
| Yes | 1 | 2.78 | 0 | 0.00 | 1 | 2.78 | ||
| Sex assigned at birth | ||||||||
| Male | 11 | 30.60 | 10 | 27.80 | 10 | 27.80 | χ2 = 0.09 | p = 0.96 |
| Female | 25 | 69.40 | 26 | 72.20 | 26 | 72.20 | ||
| Gender Identity | ||||||||
| Man | 10 | 27.78 | 12 | 33.33 | 9 | 25.00 | χ2 = 193 | p = 0.38 |
| Woman | 20 | 55.56 | 21 | 58.33 | 19 | 52.78 | ||
| Transgender man | 1 | 2.78 | 3 | 8.33 | 3 | 8.33 | ||
| Transgender woman | 1 | 2.78 | 0 | 0.00 | 0 | 0.00 | ||
| Genderqueer | 4 | 11.11 | 2 | 5.56 | 4 | 11.11 | ||
| Gender non-conforming/-binary | 3 | 8.33 | 3 | 8.33 | 4 | 11.11 | ||
| Two-spirit | 0 | 0.00 | 0 | 0.00 | 1 | 2.78 | ||
| Hijra | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | ||
| Other | 2 | 5.56 | 2 | 5.56 | 1 | 2.78 | ||
| Sexual Orientation | ||||||||
| Asexual | 0 | 0.00 | 1 | 2.78 | 1 | 2.78 | χ2 = 0.30 | p = 0.86 |
| Bisexual | 13 | 36.11 | 9 | 25.00 | 8 | 22.22 | ||
| Gay | 8 | 22.22 | 9 | 25.00 | 9 | 25.00 | ||
| Lesbian | 12 | 33.33 | 9 | 25.00 | 9 | 25.00 | ||
| Pansexual | 3 | 8.33 | 6 | 16.67 | 6 | 16.67 | ||
| Questioning | 0 | 0.00 | 0 | 0.00 | 1 | 2.78 | ||
| Other | 0 | 0.00 | 2 | 5.56 | 2 | 5.56 | ||
| Education | ||||||||
| Less than college | 18 | 50 | 19 | 52.8 | 21 | 58.3 | χ2 = 0.52 | p = 077 |
| College degree | 18 | 50 | 17 | 47.2 | 15 | 41.7 | ||
| Employment Status | ||||||||
| Full-time | 14 | 38.9 | 13 | 36.1 | 14 | 38.9 | χ2 = 11.46 | p = 0.08 |
| Part-time | 21 | 58.3 | 13 | 36.1 | 12 | 33.3 | ||
| Student (employed) | 0 | 0.00 | 5 | 13.9 | 6 | 16.7 | ||
| Unemployed | 1 | 2.8 | 5 | 13.9 | 4 | 11.1 | ||
| Personal Income (past year) | ||||||||
| Less than $10,000 | 11 | 26.8 | 17 | 47.2 | 13 | 36.1 | χ2 = 2.20 | p = 033 |
| More than $10,000 | 25 | 69.4 | 19 | 52.8 | 23 | 63.9 | ||
| Family Class Background | ||||||||
| Poor | 3 | 8.3 | 7 | 19.4 | 6 | 16.7 | χ2 = 4.53 | p = 081 |
| Working class | 12 | 33.3 | 11 | 30.6 | 13 | 36.1 | ||
| Lower middle class | 8 | 22.2 | 4 | 11.1 | 5 | 13.9 | ||
| Middle class | 10 | 27.8 | 11 | 30.6 | 11 | 30.6 | ||
| Upper middle class | 3 | 8.3 | 3 | 8.3 | 1 | 2.8 | ||
| Relationship Status | ||||||||
| Single | 11 | 30.6 | 10 | 27.8 | 14 | 38.9 | χ2 = 1.10 | p = 058 |
| In a relationship | 25 | 69.4 | 26 | 72.2 | 22 | 61.1 | ||
Note. Race, gender, and sexual orientation variables were dichotomized as follows when conducting condition comparisons: race (white versus person of color), gender (cisgender/transgender versus gender non-conforming), sexual orientation (gay or lesbian versus not gay or lesbian).
Intervention Effects
We used linear mixed models with maximum likelihood estimation to test condition, time, and condition × time interaction effects for all continuous outcomes (i.e., measures of depression, psychological distress, anxiety, suicidality, alcohol abuse, and drug abuse) and generalized linear mixed models with negative binomial distribution, log link, and maximum likelihood estimation to test these effects for the count outcome (i.e., past 90-day number of HIV-transmission-risk sex acts). For the sex-risk analysis, following recommended practice (Rendina et al., 2017), we used an offset equal to the log of the total number of anal and vaginal sex acts in follow-up period. Employing this offset adjusts for the overall number of sex acts.
For the empirical and conceptual reasons above, primary models of health-risk behavioral outcomes (i.e., suicidality, alcohol abuse, drug abuse, HIV-risk behavior) did not include those participants who did not endorse the respective behavior at baseline (i.e., n = 6 for suicidality, n = 2 for alcohol abuse, n = 6 for drug abuse, n = 2 for HIV-risk behavior). We also conducted supplement analyses containing all participants regardless of their engagement in these behaviors at baseline.
Moderated Effects
For both moderators (i.e., everyday discrimination, LGBTQ victimization), a linear mixed model analysis was performed for all continuous outcomes, and a separate generalized linear mixed model analysis was performed for the count outcome. Moderation analysis models included terms for condition, time, moderator, condition × time, condition × moderator, time × moderator, and condition × time × moderator. To probe significant three-way interactions, we performed simple slopes analyses and differences in slopes were compared using z-score transformations (Preacher, Curran & Bauer, 2006). Analyses were conducted using SAS v9.4.
Results
Main Intervention Effects
Examining changes from baseline to 3-month follow-up assessments between expressive writing and the control condition, we found significant condition × time interactions, suggesting improvements in depression (d = 0.48) and psychological distress (d = 0.36) (Table 2, Figure 2.) For the self-affirmation condition, there were moderate improvements in suicidal ideation (d = 0.41) and drug abuse (d = 0.59) at 3-month follow-up trending toward statistical significance (Table 1).
Table 2.
Changes in Primary Mental Health and Health-risk Behavioral Outcomes as a Function of Intervention Condition (Baseline to 3-month Follow-up)
| Control | Expressive Writing (EW) | Condition × Time EW vs. Control | Control | Self-Affirmation (SA) | Condition × Time SA vs. Control | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | M (SE) | M (SE) | Est. | 95% CI | p | d | M (SE) | M (SE) | Est. | 95% CI | p | d |
| Depression (CESD) | 0.48 | 0.21 | ||||||||||
| Baseline | 24.70 (2.36) | 25.24 (2.05) | - | - | - | 24.83 (3.02) | 28.91 (2.86) | - | - | - | ||
| 3-month follow-up | 24.06 (2.45) | 18.25 (2.04) | −6.34 | −11.03, −1.64 | 0.01** | 24.59 (3.29) | 25.00 (3.01) | −3.67 | −9.00, 1.66 | 0.17 | ||
| Distress (BSI) | 0.36 | 0.04 | ||||||||||
| Baseline | 2.31 (0.16) | 2.22 (0.14) | - | - | - | 2.20 (0.19) | 2.54 (0.18) | |||||
| 3-month follow-up | 2.21 (0.16) | 1.79 (0.14) | −0.33 | −0.62, −0.03 | 0.03** | 2.13 (0.20) | 2.43 (0.19) | −0.04 | −0.34, 0.26 | 0.79 | ||
| Anxiety (BAI)a | 0.29 | 0.10 | ||||||||||
| Baseline | 21.31 (2.54) | 20.09 (2.27) | - | - | - | 18.40 (3.51) | 23.92 (3.17) | - | - | - | ||
| 3-month follow-up | 18.60 (2.38) | 13.36 (2.00) | −4.03 | −8.55, 0.47 | 0.07+ | 15.93 (3.38) | 19.43 (3.04) | −2.02 | −5.77, 1.74 | 0.29 | ||
| Suicidality (SIDAS)b | −0.12 | 0.62 | ||||||||||
| Baseline | 12.23 (2.64) | 8.28 (2.29) | - | - | - | 12.90 (2.82) | 15.98 (2.30) | - | - | - | ||
| 3-month follow-up | 10.22 (3.06) | 7.54 (2.32) | 1.12 | −6.48, 8.77 | 0.73 | 10.43 (2.64) | 6.46 (2.29) | −7.05 | −14.47, 0.38 | 0.06+ | ||
| Alcohol abuse (AUDIT)c | 0.29 | 0.15 | ||||||||||
| Baseline | 4.48 (0.79) | 4.09 (0.71) | - | - | - | 7.81 (1.05) | 9.32 (1.03) | - | - | - | ||
| 3-month follow-up | 4.57 (0.85) | 2.91 (0.73) | −1.28 | −2.80, 0.24 | 0.10 | 7.89 (1.16) | 8.46 (1.11) | −0.94 | −2.54, 0.67 | 0.25 | ||
| Drug abuse (SIP-DU)d | −0.13 | 0.59 | ||||||||||
| Baseline | 2.41 (0.52) | 2.32 (0.60) | - | - | - | 2.00 (1.15) | 4.82 (0.92) | - | - | - | ||
| 3-month follow-up | 2.19 (0.89) | 2.28 (1.02) | 0.09 | −1.19, 1.57 | 0.76 | 1.61 (1.89) | 2.60 (1.39) | −2.24 | −4.57, 0.09 | 0.06+ | ||
| HIV-risk behaviore | 0.26 | −0.07 | ||||||||||
| Baseline | 7.79 (2.43) | 5.53 (1.38) | - | - | - | 4.87 (1.60) | 2.98 (0.82) | - | - | - | ||
| 3-month follow-up | 8.05 (2.63) | 3.76 (0.88) | −0.42 | 0.66, 0.38 | 0.125 | 4.88 (1.87) | 3.28 (1.43) | 0.09 | 0.34, 3.50 | 0.87 | ||
Note. Est.= model term coefficient; CI= confidence interval; CES-D = Center for Epidemiological Studies – Depression Scale; BSI = Brief Symptom Inventory; BAI = Beck Anxiety Inventory; SIDAS = Suicidal Ideation Attributes Scale; AUDIT = Alcohol Use Disorders Identification Test; SIP-DU = Shortened Inventory of Problems – Drug Use.
p < 0.10,
p < 0.01
All models include employment status as a covariate (see Table 1).
Anxiety analyses based on 107 participants providing BAI data at baseline (n = 1 missing).
Suicidality analyses based on 58 participants who endorsed suicidality at baseline.
Alcohol abuse analyses based on 102 participants who reported using alcohol at baseline.
Drug abuse analyses based on 23 participants who reported using drugs at baseline.
HIV risk analyses based on 39 participants who reported HIV transmission-risk behavior at baseline.
Figure 2.
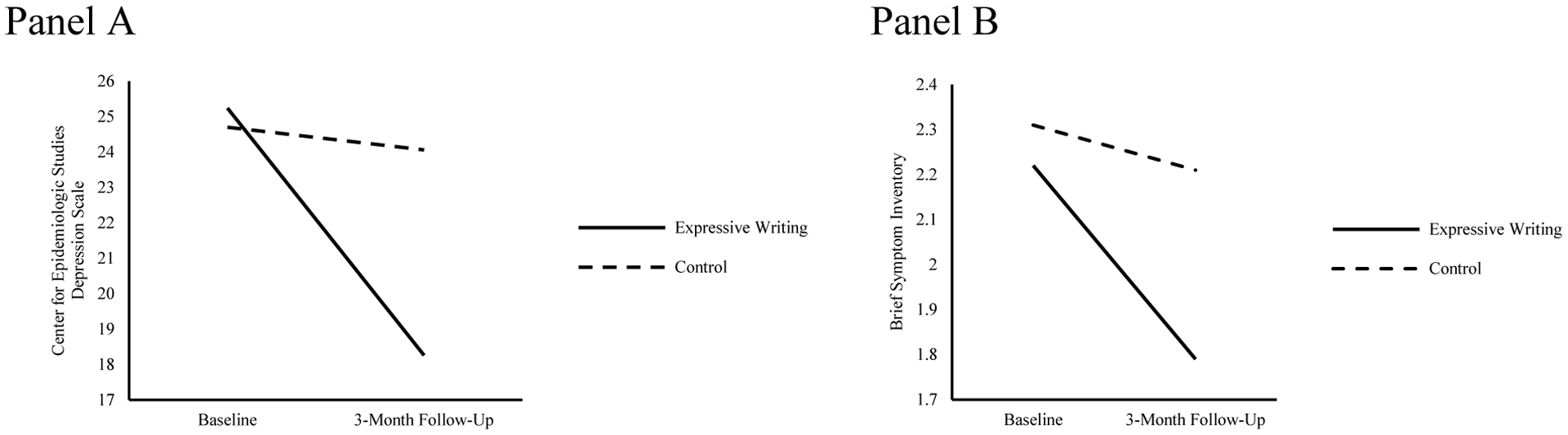
Changes in mental health outcomes over time between expressive writing and control conditions.
Appendix B also reports change from baseline to immediate post-intervention. The only significant effect found at post-intervention was a significantly greater reduction in drug abuse for participants assigned to the self-affirmation condition compared to control, but we caution that these results must be interpreted in light of the planned incomparable assessment periods chosen to balance the need to avoid overlapping timeframes across assessment points with the need to examine intervention persistence over three months. In supplemental analyses that included participants who were not included in the main analyses because of their lack of endorsement of the various health-risk behaviors at baseline, we find the same overall pattern of effects as in the primary analyses with two exceptions: 1) for expressive writing, the effect size for drug abuse became larger (and in the unexpected direction – a greater increase in the self-affirmation condition compared to control), although still not significant and 2) for self-affirmation, the effect sizes were smaller for suicidal ideation and drug abuse (in the expected direction), although they became significant for suicidal ideation in the supplemental analyses (i.e., the confidence interval no longer included 0; Appendices C and D).
Moderated Effects
Expressive writing.
The impact of the expressive writing condition on depression was moderated by discrimination (F = 6.89, n = 72, p = .01) and victimization (F = 4.53, n = 72, p = .04). As described below and depicted in Figure 3, tests of simple slopes showed significant interactions such that at higher levels (i.e., one standard deviation above the mean) of discrimination and victimization, the expressive writing condition showed greater improvements at 3-month follow-up compared to control in the respective outcomes.
Figure 3.
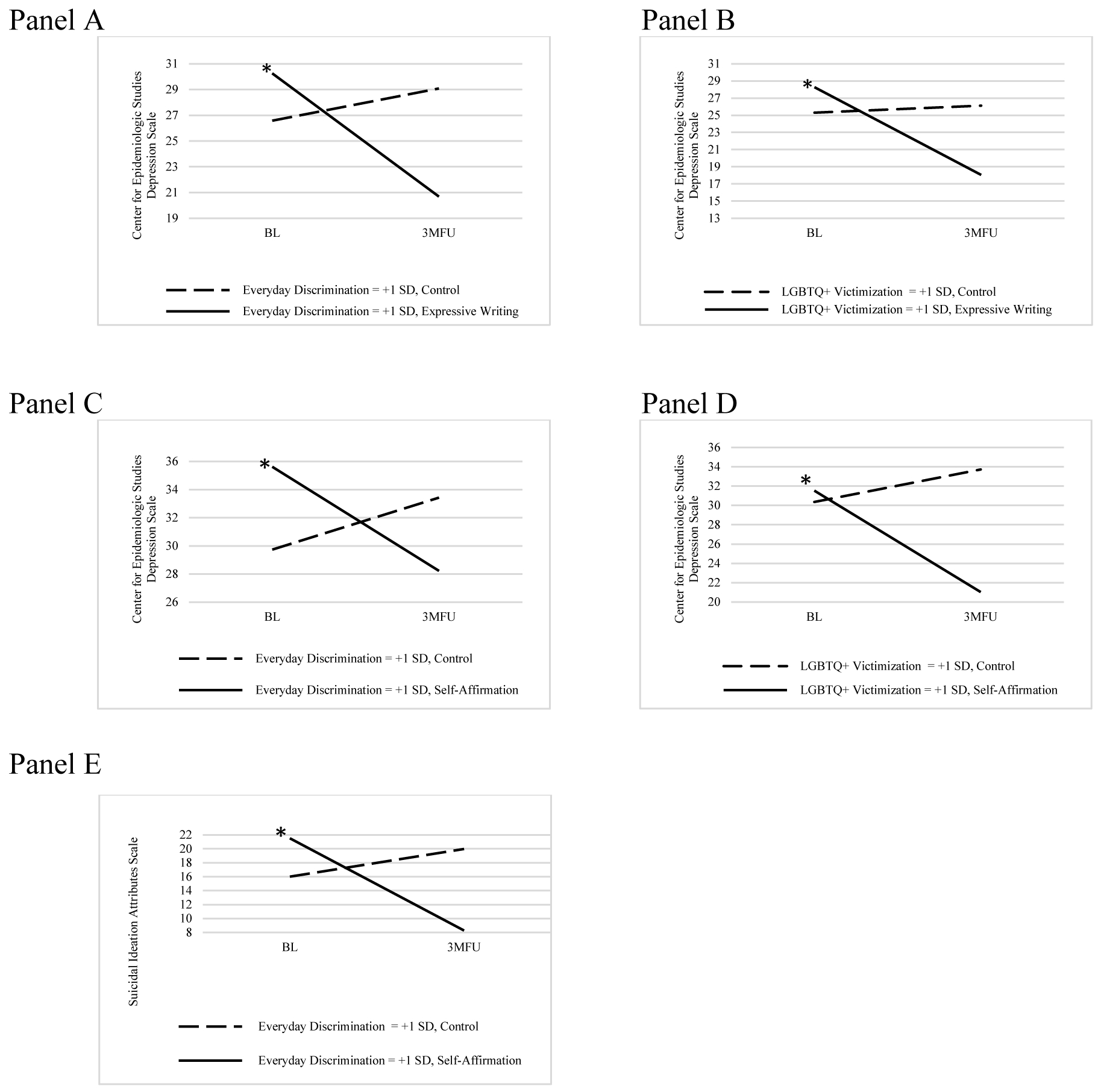
Significant moderators of effects of expressive writing and self-affirmation interventions on depression and suicidal ideation at baseline and 3-month follow-up. * p < .05
At high levels of discrimination, participants in the expressive writing condition experienced significant reductions in depression (b = −9.57, p < .01), whereas participants in the control condition did not (b = 2.50, p = .21) (Figure 3, Panel A). At high levels of LGBTQ victimization, participants in the expressive writing condition experienced significant reductions in depression (b = −10.22, p < .01), whereas participants in the control condition did not (b = 0. 82, p = .70) (Figure 3, Panel B).
Self-affirmation.
The impact of the self-affirmation on depression was moderated by discrimination (F = 8.21, n = 72, p < .01) and victimization (F = 4.23, n = 72, p = .04). The impact of self-affirmation on suicidality was also moderated by discrimination (F = 10.18, n = 40, p < .01). As described below and depicted in Figure 3, tests of simple slopes showed significant interactions such that at higher levels of discrimination and victimization (i.e., one standard deviation above the mean), the self-affirmation condition showed greater improvements at 3-month follow-up compared to control in the respective outcomes.
At high levels of discrimination, participants in the self-affirmation condition experienced significant reductions in depression at 3-month follow-up (b = −7.40, p = .01), whereas participants in the control condition did not (b = 3.69, p = .10) (Figure 3, Panel C). At high levels of victimization, participants in the self-affirmation condition experienced significant reductions in depression at 3-month follow-up (b = −10.50, p = .01), whereas participants in the control condition did not (b = 3.36, p = .40) (Figure 3, Panel D). Finally, at high levels of discrimination, participants in the self-affirmation condition experienced significantly greater decreases in suicidal ideation at 3-month follow-up (b = −13.23, p < .01), whereas participants in the control condition did not (b = 3.97, p = .27) (Figure 3, Panel E).
Discussion
Despite being at significantly greater risk of mental health problems and health-risk behaviors than their heterosexual peers, sexual minority young adults are largely without efficacious interventions tailored to their distinct stressors (Chaudoir, Wang, & Pachankis, 2017). Sexual minority young adults living in high-stigma, low-resource locales, such as rural regions of the US where this study was conducted, are in particular need of portable interventions given the high degree of structural stigma and relative lack of brick-and-mortar LGBTQ-affirmative supports that exist in these areas (Human Rights Campaign, 2018). The present study begins to remedy this lacuna by offering support for two brief, portable interventions that address LGBTQ-specific stressors and impact multiple mental health and health-risk behavioral difficulties, especially for sexual minorities who experience high levels of minority stressors common in rural regions.
As hypothesized, being asked to expressively write about a stressful or traumatic event related to being a sexual minority significantly reduced depressive symptoms and general psychological distress at 3-month follow-up. This finding extends that of the two previous trials of expressive writing for sexual minorities in notable ways. First, the present findings offer stronger support for the efficacy of expressive writing on mental health outcomes than found in the two previous studies of this intervention with this population. One previous trial of expressive writing with sexual minority male college students found that effects were limited to negative affect and depression, with depression only being reduced among those with low social support (Pachankis & Goldfried, 2010). Another trial with sexual minority women found that effects were limited to felt stress and only among those who concealed their identities (Lewis et al., 2005). On the other hand, the present study found that expressive writing yielded a significant reduction in depression and psychological distress across participants. This main effect of expressive writing suggests a more robust impact of this intervention across participants than found in previous studies. This more robust effect might be due to the fact that the present study focused on a particularly high-need sample of young adults with relatively low previous experience with or access to LGBTQ-affirmative supports. This difference between studies might also be explained by the fact that the present study created tailored writing prompts in consultation with local LGBTQ community members, not utilized in previous tests of expressive writing this population. In fact, using tailored writing prompts has been shown to enhance the efficacy of expressive writing (Frattaroli, 2006). Also extending previous studies, we examined contextual moderators of expressive writing efficacy. We specifically examined contextual minority stress factors that are relatively common in high-stigma, low-resource rural regions of the US as moderators of expressive writing’s efficacy. Participants who were exposed to high degrees of discrimination and victimization were particularly likely to benefit from the intervention in terms of reduced depression.
This first test of a stand-alone self-affirmation intervention as applied to sexual minorities further supports brief, portable interventions for this population. Compared to the neutral control, self-affirmation yielded its greatest impact on drug abuse, consistent with previous studies finding an impact of self-affirmation on health-risk behavioral outcomes (e.g., Epton et al., 2015). At the same time, self-affirmation also yielded a moderate effect on suicidality, expanding previous research on self-affirmation to this important outcome. However, self-affirmation’s efficacy trended toward statistical significance for these two outcomes and was only significant for suicidality in analyses that included all participants regardless of their baseline suicidality risk, suggesting that the marginal significance might possibly be a function of the relatively small number of participants who had experienced those problems at baseline. Like expressive writing, self-affirmation’s efficacy was significantly moderated by contextual minority stress exposures. Specifically, participants assigned to the self-affirmation condition who reported high degrees of discrimination and victimization experienced significant reductions in depression at 3-month follow-up, whereas those in the control condition who reported high degrees of discrimination and victimization did not. Participants assigned to the self-affirmation condition with high degrees of discrimination experienced significant reductions in suicidality at 3-month follow-up, also significantly greater than control. The relatively small number of participants who reported drug use precluded moderation analyses for this particular outcome.
Sexual minority young adults, especially those living in high-stigma locales, are at particularly high risk of suicide (Hatzenbuehler, 2011; Hatzenbuehler, Pachankis, & Wolff, 2012; King et al, 2008). To our knowledge, the self-affirmation intervention tested here represents one of the only LGBTQ-specific interventions tested in a randomized controlled trial with evidence for reducing suicidality among this extremely high-risk population. This elevated risk has been explained in terms of the disproportionate threats to interpersonal and societal belongingness that sexual minorities experience across the lifespan (e.g., Bränström, van der Star, & Pachankis, 2019). The self-affirmation intervention tested here—in which participants used their own stressful life experiences to advise ostensible sexual minority peers how to effectively cope with their own—might have provided a sense of interpersonal or societal belonging to participants. Perhaps self-affirmation yielded its impact by instilling within participants a sense of their belongingness to a larger sexual minority community in addition to reminding them of their ability to cope. Because we created the vignettes for this intervention in consultation with young adult sexual minorities and key stakeholders from the local community and because the vignettes reference the local community, participants may have been particularly likely to feel a part of this community by reading what might have seemed like real-life peer stories.
The exact type of self-affirmation intervention tested here, in which an individual provides advice to a similar peer in writing, while similar to previously tested interventions, differs from those in a several notable ways. First, one previous trial of self-affirmation with African American college students encouraged students to write about stigma-related stress as temporary (Walton & Cohen, 2011). However, because such stress is likely not temporary for sexual minority young adults in high-stigma locations of the US, such as Appalachian Tennessee, we did not encourage such a focus. Cognitive reframing of LGBTQ-related stress as temporary, while effective for some sexual minorities (Clyman & Pachankis, 2014), might not work against the seeming immutable stigmatizing structures surrounding sexual minorities in the rural US. Second, other tests of self-affirmation interventions have been delivered as part of larger LGBTQ-affirmative treatment packages. The present study is, to our knowledge, the first test of a stand-alone self-affirmation intervention for this population, permitting a test of its isolated impact. Third, participants in previous tests of self-affirmation for sexual minorities either watched a video of another LGBTQ peer who was struggling with a stigma-related stressful challenge (Pachankis et al., 2015) or listened to a recording of such a peer (Lin & Israel, 2012). The previous self-affirmation intervention with African American students asked participants to read their advice to a similar peer into a camera (Walton & Cohen, 2011). While these audio/video-enhanced presentations might have enhanced believability and engagement, the present study nonetheless found robust impact even without such enhancements, at least for sexual minorities who reported high levels of discrimination and victimization. Finally, future tests of self-affirmation interventions might consider whether or not participant writing instructions should be further modified, perhaps by encouraging narratives of belongingness or optimism. The present findings suggest that directing participants to focus their writing in ways that build efficacy for coping with certain contextual minority stressors (e.g., victimization) might enhance impact.
Clinically, results suggest that sexual minority young adults living in high-stigma, low-resource areas can benefit from these brief, portable interventions. The fact that these interventions require only one hour in total to complete and the fact that untreated depression and suicidality represent some of the costliest health burdens affecting sexual minorities (e.g., Hottes, Ferlatte, & Gesink, 2015) suggests that these interventions, here showing moderate effect, if disseminated broadly, can be highly cost-effective and have notable impact on this population’s health. For sexual minority young adults currently receiving mental health treatment, these interventions can potentially serve as a useful adjunct to existing treatment. For those not currently receiving treatment, mental health professionals or LGBTQ community advocates might consider ways to promote direct-to-consumer knowledge of these interventions, either as a stand-alone treatment or as one component of an integrated support package. For instance, school-based gay-straight alliances can incorporate these brief writing exercises into their social and advocacy activities to bring potentially needed evidence-based mental and behavioral health support to all members (e.g., Poteat, Scheer, Marx, Calzo, & Yoshikawa, 2015). Other existing institutional supports for sexual minority young adults, such as suicide prevention services, might also consider the adjunctive benefit of these interventions.
Despite the strengths of this randomized controlled trial, including offering support for two brief portable interventions delivered to sexual minority young adults in a high-need region of the US, results must be interpreted in light of several limitations. First, this study was insufficiently powered to compare the two active interventions. Given that both interventions exerted relatively similar effect sizes, substantial power would be required to determine superiority of one of these interventions over the other. Knowing the comparative efficacy of the two interventions would permit more specific treatment recommendations. While not powered to compare the two active interventions to each other using tests of statistical significance, the present study finds comparable effect sizes for both interventions, with the important distinction that expressive writing showed the strongest effects for depression and psychological distress, whereas self-affirmation found larger effect sizes for drug use problems and suicidality. Participants were also more likely to complete all three days of expressive writing than self-affirmation writing and to produce more words per expressive writing submission, suggesting a hypothesis for future research – that sexual minority young adults find expressive writing to be relatively more appealing than self-affirmation.
Second, although these interventions showed moderate effect sizes across mental health and health-risk behavioral outcomes compared to a neutral control, this study does not offer evidence for how these interventions would compare to other interventions for this population. Previous intervention trials for sexual minority young adults show somewhat larger effects when compared to a weak control (e.g., Pachankis et al., 2015). Yet existing evidence-based interventions for this population are relatively time intensive (e.g., ten 60-min sessions) and have been limited to sexual minorities living in urban areas. Comparatively, the writing interventions tested here, despite showing somewhat weaker average effects, have the ability to effect such change more rapidly (i.e., three 20-min sessions) and broadly (i.e., without geographic constraints). In other trauma-exposed populations, expressive writing actually shows effects comparable to more intensive in-person cognitive-behavioral treatments (e.g., Sloan, Mark, Lee, & Resick, 2018). Thus, future implementation tests of the writing interventions tested here might show them to be particularly cost-effective, despite their lack of clinically significant effects in the present sample. To establish the relative effectiveness of the two stand-alone interventions tested here, future trials might wish to examine their efficacy and cost against existing multicomponent treatment package or against other interventions capable of transcending geographic barriers, such as tele-mental healthcare.
Third, recruitment into this study was limited to young adults between the ages of 18 and 29 living in Appalachian Tennessee. Knowing whether these interventions would work similarly for younger sexual minorities who might be at particular risk, or those living in other high-need global regions that also contain significant barriers to mental and behavioral health, remains unknown. Fourth, results should be interpreted in light of certain aspects of our measurement approach. For instance, we modified most outcome measures to capture past-3-month symptoms and health-risk behaviors, consistent with the timeframe of our follow-up window. However, this longer timeframe potentially introduces more variation and recall bias in outcomes than would shorter timeframes. Also, because of our relatively short intervention window (i.e., 2 weeks), immediate post-intervention outcome assessments only assessed past-week symptoms and behaviors, which while preventing overlap in the assessment recall periods, makes the 1-week timeframe of this assessment period incomparable to the 3-month timeframe used for baseline and 3-month follow-up. Other outcome measures captured relatively limited aspects of their respective constructs (e.g., the measure of drug use problems did not capture type, frequency, or quantity of drug use).
Finally, the present study does not shed light on these interventions’ mechanisms or suggest individualized treatment approaches. Thus, future research might consider examining shared or distinct treatment mechanisms underlying the efficacy of each of these interventions (e.g., extinction of past traumatic memories for expressive writing; reduced defensive responding to self-evaluative threats for self-affirmation). Researchers may also wish to identify the linguistic features of writing sessions that contribute to particularly beneficial outcomes. To facilitate this personalized approach, future research can determine whether writing prompts can be optimally tailored to the specific contextual minority stress exposures (e.g., family rejection, workplace discrimination) faced by sexual minority young adults in need of support against those types of specific stressors.
In conclusion, the present study finds evidence that two brief writing interventions – expressive writing and self-affirmation – represent efficacious and efficient means for reducing mental and behavioral health problems among one of the most at-risk segments of sexual minority young adults in the US. By combining local community input and technological reach, these interventions can serve an important role in empowering sexual minority young adults living in high-stigma, low-resource locales to build personal resilience against the structural challenges they face. Moreover, because young adulthood is a critical period for the development of mental illness and health-risk behaviors (Rice et al., 2019), these interventions have the potential to attenuate or halt the progression of mental health problems and health-risk behaviors into later stages of adulthood. As such, the salubrious effects of these low-cost, portable, and efficient writing interventions may persist across the lifespan.
Acknowledgments
The authors would like to thank Anthony D’Augelli for providing helpful consultation on this study. They would also like to acknowledge Abbey Mann, Timothy Sullivan, and Roxanne Winston for their help with study coordination and data collection and Alex Belser, Charles Burton, Nitzan Cohen, Zachary Rawlings, Craig Rodriguez-Seijas, Ingrid Solano, and Tenille Taggart for enacting the clinical protocol for this study.
This study was funded by the National Institute of Mental Health (R21MH113860: PIs Pachankis and Chaudoir). The content contained herein is the authors’ own and does not necessarily reflect the views of the National Institutes of Health. All data for this study are available at the NIMH Data Archive: https://nda.nih.gov. This study was also pre-registered at clinicaltrials.gov under identifier NCT03751020. Findings from this study were presented at the American Psychological Association annual conference in August 2019.
APPENDIX A
Expressive Writing Prompts
DAY 1:
As [gay/lesbian/bi/pan] individuals living in Northeast Tennessee, nearly all of us have experienced stressful life events because of who we are. Nearly everyone has a story about being the target of others’ slurs, bullying, or physical aggression. Sometimes these experiences occur in our schools, workplaces, and other public spaces. Other times, these experiences occur in our own homes and churches.
Today, please write about the most difficult or painful situation that you have encountered in your lifetime because of your sexual identity. Consider what your deepest thoughts and feelings are about this situation. Just follow your train of thought wherever it goes, without worrying about spelling, grammar, or structure. Please write for the whole 20 minutes until the timer has expired.
DAY 2:
Today, please continue writing about the most difficult or painful situation that you have encountered in your lifetime because of your sexual identity. You could continue to write about topics you addressed before, or you could write about something different. In either case, continue to really explore your very deepest emotions and thoughts about this situation.
Remember to follow your train of thought wherever it goes, without worrying about spelling, grammar, or structure. Please write for the whole 20 minutes until the timer has expired.
DAY 3:
Today is the last day of writing. Please explore your deepest thoughts and feelings about the most difficult or painful situation that you have encountered in your lifetime because of your sexual identity. Remember that this is the last day of writing, so by the end of the session, you might want to find a way to bring closure to your ideas. For example, you might write about how this situation relates to your current life or your future. Feel free to go in any direction you feel most comfortable with and delve into your deepest emotions and thoughts.
Remember to follow your train of thought wherever it goes, without worrying about spelling, grammar, or structure. Please write for the whole 20 minutes until the timer has expired.
Expressive writing prompts. Adapted from Pachankis & Goldfried, 2010.
NOTE: Scenario should be tailored to match the participant’s own sexual identity.
Self-affirmation Writing Prompts
Below is a situation a local LGBTQ+ young adult is dealing with. Please read about the situation and write your thoughts below.
DAY #1
[Meredith/Ebony/Camila/Neil/Alonzo/Angel/Pearl] is a senior [bisexual] student at a local high school in Northeast Tennessee. [NAME] recently came out to [her] dad and he responded by saying “You’re not gonna be [bisexual] under my roof!” He kicked [her] out and [she’s] been couch-surfing since. That was several months ago, and [she’s] still feeling really hopeless. [She] knew he wouldn’t take the news well, but she never expected him to freak out this badly. Now, she’s worried about being homeless forever and how [she’ll] pay for college. And, [she’s] terrified that [her] dad will never speak to [her] again.
Imagine [Meredith/Ebony/Camila/Neil/Alonzo/Angel/Pearl] comes to you for help. Based on your experiences of being [bisexual], what advice would you give [her] on how to handle this situation? Write a message to [her] for 20 minutes about what you might say. Just follow your train of thought wherever it goes, without worrying about spelling, grammar, or structure. Please write for the whole 20 minutes until the timer has expired.
DAY #2
[Carrie/Keisha/Sophia/Brendan/Theo/Daniel/Quinn] is a devout [bisexual] Christian in [his] mid-20s living in Northeast Tennessee. [He’s] belonged to his church [his] whole life and loves playing in the church band each Sunday. However, things changed since [he] came out. [His] band members told him [he’s] going to hell and kicked him out. [His] pastor asked [him] to meet so they could “pray it away.” And, everyone else at church gives [him] dirty looks like [he’s] an abomination. So, he stopped going. But, now there’s a big hole in [his] life where [his] faith life used to be and [he’s] worried whether [he’ll] ever find a church community again.
Imagine [Carrie/Keisha/Sophia/Brendan/Theo/Daniel/Quinn] comes to you for help. Based on your experiences of being [bisexual], what advice would you give [him] on how to handle this situation? Write a message to [him] for 20 minutes about what you might say. Just follow your train of thought wherever it goes, without worrying about spelling, grammar, or structure. Please write for the whole 20 minutes until the timer has expired.
DAY #3
[Sarah/Kenya/Isabella/Geoffrey/Terrance/Jose/River] is a high school student in Northeast Tennessee. A few months back, some students found out that [she] is [a lesbian] and [she] has been bullied and teased ever since. Even [her] friends constantly tell jokes about gay people. Although several teachers see what’s going on, they never intervene and none are openly LGBTQ. [She] can’t transfer schools and is feeling hopeless about ever being accepted for who [she] is.
Imagine [Sarah/Kenya/Isabella/Geoffrey/Terrance/Jose/River] comes to you for help. Based on your experiences of being [bisexual], what advice would you give [her] on how to handle this situation? Write a message to [her] for 20 minutes about what you might say. Just follow your train of thought wherever it goes, without worrying about spelling, grammar, or structure. Please write for the whole 20 minutes until the timer has expired.
Self-affirmation writing prompts. Adapted from Lin & Israel, 2012 and tailored based on interviewee feedback.
NOTE: Scenario should be tailored to match the participant’s own sexual and gender identity.
Control Prompts
ALL DAYS
Please describe in detail what you have done since you woke up this morning. It is important that you describe things exactly as they occurred. Do not mention your own emotions, feelings, or opinions. Your description should be as objective as possible—we just want to know the facts. Provide as many details as possible.
Remember to follow your train of thought wherever it goes, without worrying about spelling, grammar, or structure. Please write for the whole 20 minutes until the timer has expired.
Appendix B
Supplemental Table 2.
Changes in Primary Mental Health and Health-risk Behavioral Outcomes as a Function of Intervention Condition (Baseline to Immediate Post-intervention)
| Control | Expressive Writing (EW) | Condition × Time EW vs. Control | Control | Self-Affirmation (SA) | Condition × Time SA vs. Control | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | M (SE) | M (SE) | Est. | 95% CI | p | d | M (SE) | M (SE) | Est. | 95% CI | p | d |
| Depression (CESD) | 0.29 | 0.27 | ||||||||||
| Baseline | 24.19 (2.35) | 25.07 (2.03) | - | - | - | 25.37 (2.54) | 29.78 (2.19) | - | - | - | ||
| Post-intervention | 20.71 (2.34) | 17.80 (2.05) | −3.79 | −11.56, 3.98 | 0.34 | 22.01 (2.57) | 22.61 (2.36) | −3.81 | −12.21, 4.60 | 0.37 | ||
| Distress (BSI) | −0.09 | 0.09 | ||||||||||
| Baseline | 2.27 (0.15) | 2.20 (0.13) | - | - | - | 2.28 (0.17) | 2.64 (0.17) | - | - | - | ||
| Post-intervention | 1.81 (0.15) | 1.82 (0.13) | 0.08 | −0.43, 0.58 | 0.76 | 1.83 (0.17) | 2.10 (0.16) | −0.09 | −0.65, 0.47 | 0.75 | ||
| Anxiety (BAI)a | −0.04 | 0.05 | ||||||||||
| Baseline | 21.01 (2.62) | 20.02 (2.30) | - | - | - | 20.48 (2.77) | 26.94 (2.43) | - | - | - | ||
| Post-intervention | 13.92 (2.44) | 13.56 (2.12) | 0.63 | −7.77, 9.04 | 0.88 | 14.08 (2.72) | 19.72 (2.49) | −0.82 | −9.89, 8.24 | 0.86 | ||
| Suicidality (SIDAS)b | −0.04 | 0.32 | ||||||||||
| Baseline | 11.33 (2.4) | 7.89 (2.26) | - | - | - | 15.37 (2.73) | 16.96 (2.33) | - | - | - | ||
| Post-intervention | 4.55 (1.57) | 2.18 (1.25) | 1.07 | −3.80, 5.94 | 0.66 | 8.12 (1.70) | 6.10 (0.33) | −3.61 | −11.01, 3.79 | 0.33 | ||
| Alcohol abuse (AUDIT)c | −0.04 | 0.14 | ||||||||||
| Baseline | 4.58 (0.81) | 4.09 (0.73) | - | - | - | 3.23 (1.04) | 5.21 (0.93) | - | - | - | ||
| Post-intervention | 3.77 (0.82) | 3.44 (0.75) | 0.16 | −0.85, 1.17 | 0.75 | 2.38 (1.01) | 3.54 (0.90) | −0.81 | −1.83, 0.20 | 0.11 | ||
| Drug abuse (SIP-DU)d | −1.18 | 0.88 | ||||||||||
| Baseline | 2.46 (0.60) | 2.33 (0.61) | - | - | - | 2.34 (1.41) | 4.70 (0.99) | - | - | - | ||
| Post-intervention | 2.39 (1.74) | 4.18 (1.94) | 1.92 | −3.82, 7.66 | 0.48 | 2.22 (1.29) | 1.40 (0.83) | −3.18* | −6.00, −0.37 | 0.03 | ||
| HIV-risk behaviore | 0.14 | 0.18 | ||||||||||
| Baseline | 6.69 (1.96) | 5.12 (1.20) | - | - | - | 4.01 (1.34) | 2.80 (0.80) | - | - | - | ||
| Post-intervention | 1.84 (0.50) | 1.09 (0.25) | −0.26 | −1.07, 0.56 | 0.53 | 1.11 (0.36) | 0.63 (0.23) | −0.20 | −1.10, 0.70 | 0.66 | ||
Note. Est.= model term coefficient; CI= confidence interval; CES - D = Center for Epidemiological Studies – Depression Scale; BSI = Brief Symptom Inventory; BAI = Beck Anxiety Inventory; SIDAS = Suicidal Ideation Attributes Scale; AUDIT = Alcohol Use Disorders Identification Test; SIP-DU = Shortened Inventory of Problems – Drug Use.
p ≤ 0.05. All models include employment status as a covariate (see Table 1).
Anxiety analyses based on 107 participants providing BAI data at baseline (n = 1 missing).
Suicidality analyses based on 58 participants who endorsed suicidality at baseline.
Alcohol abuse analyses based on 102 participants who reported using alcohol at baseline.
Drug abuse analyses based on 23 participants who reported using drugs at baseline
HIV risk analyses based on 39 participants who reported HIV transmission-risk behavior at baseline.
Appendix C
Supplemental Table 1.
Changes in Primary Health-risk Behavioral Outcomes as a Function of Intervention Condition (Baseline to 3-month Follow-up; Including All Participants Regardless of Baseline Risk)
| Control | Expressive Writing (EW) | Condition × Time EW vs. Control | Control | Self-Affirmation (SA) | Condition × Time SA vs. Control | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | M (SE) | M (SE) | Est. | 95% CI | p | d | M (SE) | M (SE) | Est. | 95% CI | p | d |
| Suicidality (SIDAS) | −0.18 | 0.20 | ||||||||||
| Baseline | 6.23 (1.66) | 4.42 (1.44) | - | - | - | 11.09 (2.45) | 14.53 (2.21) | - | - | - | ||
| 3-month follow-up | 4.70 (1.70) | 4.28 (1.36) | 1.39 | −4.06, 6.84 | 0.61 | 10.99 (2.33) | 11.57 (2.08) | −2.86* | −5.72, −0.003 | 0.05 | ||
| Alcohol abuse (AUDIT) | 0.32 | 0.14 | ||||||||||
| Baseline | 4.09 (0.81) | 3.76 (0.69) | - | - | - | 7.64 (1.37) | 8.59 (1.23) | - | - | - | ||
| 3-month follow-up | 4.31 (0.90) | 2.52 (0.72) | −1.45 | −4.22, 1.31 | 0.30 | 8.17 (1.43) | 8.03 (1.26) | −1.09 | 3.14, 0.96 | 0.29 | ||
| Drug abuse (SIP-DU) | −0.56 | 0.19 | ||||||||||
| Baseline | 0.25 (0.22) | 0.25 (0.18) | - | - | - | 2.78 (0.54) | 3.81 (0.48) | - | - | - | ||
| 3-month follow-up | 0.21 (0.44) | 0.82 (0.38) | 0.61 | −0.59, 1.81 | 0.32 | 2.76 (0.52) | 3.21 (0.56) | −0.58 | −1.48, 0.32 | 0.20 | ||
| HIV-risk behaviora | 0.08 | 0.00 | ||||||||||
| Baseline | 1.45 (0.53) | 1.99 (0.61) | - | - | - | 0.14 (8.50) | 0.11 (6.77) | - | - | - | ||
| 3-month follow-up | 1.26 (0.51) | 1.52 (0.49) | −0.13 | −1.36, 1.11 | 0.84 | 0.11 (7.13) | 0.05 (3.11) | −0.60 | −2.21, 1.04 | 0.46 | ||
Note. Est.= model term coefficient; CI= confidence interval; SIDAS = Suicidal Ideation Attributes Scale; AUDIT = Alcohol Use Disorders Identification Test; SIP-DU = Shortened Inventory of Problems – Drug Use.
p ≤ 0.05.
All models include employment status as a covariate (see Table 1).
HIV risk analyses based on 107 participants providing data at baseline (n = 1 missing).
Appendix D
Supplemental Table 3.
Changes in Health-risk Behavioral Outcomes as a Function of Intervention Condition (Baseline to Immediate Post-intervention; Including All Participants Regardless of Baseline Risk)
| Control | Expressive Writing (EW) | Condition × Time EW vs. Control | Control | Self-Affirmation (SA) | Condition × Time SA vs. Control | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | M (SE) | M (SE) | Est. | 95% CI | p | d | M (SE) | M (SE) | Est. | 95% CI | p | d |
| Suicidality (SIDAS) | −0.10 | 0.17 | ||||||||||
| Baseline | 5.93 (1.49) | 4.21 (1.40) | - | - | - | 9.52 (1.74) | 10.81 (1.76) | - | - | - | ||
| Post-intervention | 2.26 (0.83) | 1.42 (0.68) | 0.88 | −3.38, 5.14 | 0.68 | 4.61 (1.07) | 4.05 (0.96) | −1.86 | −6.82, 3.12 | 0.46 | ||
| Alcohol abuse (AUDIT) | 0.04 | 0.35 | ||||||||||
| Baseline | 4.53 (0.80) | 3.96 (0.69) | - | - | - | 3.79 (0.92) | 5.26 (0.79) | - | - | - | ||
| Post-intervention | 4.12 (0.83) | 3.39 (0.73) | −0.16 | −2.86, 2.55 | 0.91 | 3.37 (0.93) | 3.04 (0.86) | −1.80 | −4.84, 1.24 | 0.24 | ||
| Drug abuse (SIP-DU) | −0.34 | 0.41 | ||||||||||
| Baseline | 0.20 (0.21) | 0.22 (0.17) | - | - | - | 0.13 (0.38) | 1.33 (0.33) | - | - | - | ||
| Post-intervention | 0.20 (0.36) | 0.61 (0.34) | 0.40 | −0.63, 1.43 | 0.44 | 0.10 (0.39) | 0.42 (0.35) | −0.87 | −2.13, 0.39 | 0.17 | ||
| HIV-risk behaviora | 0.24 | 0.02 | ||||||||||
| Baseline | 1.54 (0.55) | 0.53 (0.17) | - | - | - | 1.17 (0.48) | 0.88 (0.31) | - | - | - | ||
| Post-intervention | 2.10 (0.64) | 0.49 (0.14) | −0.30 | −1.48, 0.71 | 0.49 | 0.43 (0.17) | 0.18 (0.08) | −0.56 | −1.88, 0.76 | 0.40 | ||
Note. Est.= model term coefficient; CI= confidence interval; SIDAS = Suicidal Ideation Attributes Scale; AUDIT = Alcohol Use Disorders Identification Test; SIP-DU = Shortened Inventory of Problems – Drug Use.
All models include employment status as a covariate (see Table 1).
HIV risk analyses based on 107 participants providing data at baseline (n = 1 missing).
Contributor Information
John E. Pachankis, Yale School of Public Health
Stacey L. Williams, East Tennessee State University
Kriti Behari, Yale School of Public Health.
Sarah Job, East Tennessee State University.
Erin M. McConocha, Yale School of Public Health
Stephenie R. Chaudoir, College of the Holy Cross
References
- Allensworth-Davies D, Cheng DM, Smith PC, Samet JH, & Saitz R (2012). The Short Inventory of Problems—Modified for Drug Use (SIP-DU): Validity in a primary care sample. The American Journal on Addictions, 21(3), 257–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes DM, Hatzenbuehler ML, Hamilton AD, & Keyes KM (2014). Sexual orientation disparities in mental health: The moderating role of educational attainment. Social Psychiatry and Psychiatric Epidemiology, 49(9), 1447–1454. doi: 10.1007/s00127-014-0849-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA (1988). An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology, 56, 893–897. [DOI] [PubMed] [Google Scholar]
- Birkett M, Newcomb ME, & Mustanski B (2015). Does it get better? A longitudinal analysis of psychological distress and victimization in lesbian, gay, bisexual, transgender, and questioning youth. Journal of Adolescent Health, 56, 280–285. doi: 10.1016/j.jadohealth.2014.10.275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bränström R, Hatzenbuehler ML, & Pachankis JE (2016). Sexual orientation disparities in physical health: Age and gender effects in a population-based study. Social Psychiatry and Psychiatric Epidemiology, 51(2), 289–301. doi: 10.1007/s00127-015-1116-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bränström R, van der Star A, & Pachankis JE (2019). Untethered lives: Barriers to societal integration as predictors of the sexual orientation disparity in suicidality. Social Psychiatry and Psychiatric Epidemiology. doi: 10.1007/s00127-019-01742-6 [DOI] [PubMed] [Google Scholar]
- Chaudoir SR, Wang K, & Pachankis JE (2017). What reduces sexual minority stress? A review of the intervention “toolkit”. Journal of Social Issues, 73(3), 586–617. doi: 10.1111/josi.12233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clyman JA, & Pachankis JE (2014). The relationship between objectively coded explanatory style and mental health in the stigma-related narratives of young gay men. Psychology of Men & Masculinity, 15(1), 110–115. doi: 10.1037/a0031500 [DOI] [Google Scholar]
- Cohn TJ, & Hastings SL (2010). Resilience among rural lesbian youth. Journal of Lesbian Studies, 14(1), 71–79. doi: 10.1080/10894160903060325 [DOI] [PubMed] [Google Scholar]
- D’Augelli AR (2006). Coming out, visibility, and creating change: empowering lesbian, gay, and bisexual people in a rural university community. American Journal of Community Psychology, 37(3–4), 203–210. doi: 10.1007/s10464-006-9043-6 [DOI] [PubMed] [Google Scholar]
- D’Augelli AR, Hershberger SL, & Pilkington NW (1998). Lesbian, gay, and bisexual youth and their families: Disclosure of sexual orientation and its consequences. American Journal of Orthopsychiatry, 68(3), 361–371; discussion 372–365. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N (1983). The Brief Symptom Inventory: An introductory report. Psychological Medicine, 13, 595–605. [PubMed] [Google Scholar]
- Essed P (1991). Understanding Everyday Racism. Newbury Park, California: Sage. [Google Scholar]
- Everett BG (2013). Sexual orientation disparities in sexually transmitted infections: Examining the intersection between sexual identity and sexual behavior. Archives of Sexual Behavior, 42(2), 225–236. doi: 10.1007/s10508-012-9902-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frattaroli J (2006). Experimental disclosure and its moderators: A meta-analysis. Psychology Bulletin, 132(6), 823–865. doi: 10.1037/0033-2909.132.6.823 [DOI] [PubMed] [Google Scholar]
- Galliher RV, Rostosky SS, & Hughes HK (2004). School belonging, self-esteem, and depressive symptoms in adolescents: An examination of sex, sexual attraction status, and urbanicity. Journal of youth and adolescence, 33(3), 235–245. [Google Scholar]
- Hatzenbuehler ML (2011). The social environment and suicide attempts in lesbian, gay, and bisexual youth. Pediatrics, 127(5), 896–903. doi: 10.1542/peds.2010-3020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Keyes KM, & McLaughlin KA (2011). The protective effects of social/contextual factors on psychiatric morbidity in LGB populations. International Journal of Epidemiology, 40(4), 1071–1080. doi: 10.1093/ije/dyr019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Pachankis JE, & Wolff J (2012). Religious climate and health risk behaviors in sexual minority youths: A population-based study. American Journal of Public Health, 102(4), 657–663. doi: 10.2105/ajph.2011.300517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hottes TS, Ferlatte O, & Gesink D (2015). Suicide and HIV as leading causes of death among gay and bisexual men: A comparison of estimated mortality and published research. Critical Public Health, 25(5), 513–526. doi: 10.1080/09581596.2014.946887 [DOI] [Google Scholar]
- Human Rights Campaign (2018). Municipal Equality Index: A nationwide evaluation of municipal law. Washington, DC: Human Rights Campaign; Retrieved from: https://www.hrc.org/mei [Google Scholar]
- Irish M, Solmi F, Mars B, King M, Lewis G, Pearson RM,…Lewis G (2019). Depression and self-harm from adolescence to young adulthood in sexual minorities compared with heterosexuals in the UK: A population-based cohort study. The Lancet Child & Adolescent Health, 3(2), 91–98. doi: 10.1016/s2352-4642(18)30343-2 [DOI] [PubMed] [Google Scholar]
- Israel T, Choi AY, Goodman JA, Matsuno E, Lin Y-J, Kary KG, & Merrill CRS (2019). Reducing internalized binegativity: Development and efficacy of an online intervention. Psychology of Sexual Orientation and Gender Diversity, 6(2), 149–159. doi: 10.1037/sgd0000314 [DOI] [Google Scholar]
- King M, Semlyen J, Tai SS, Killaspy H, Osborn D, Popelyuk D, & Nazareth I (2008). A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry, 8(1), 70. doi: 10.1186/1471-244X-8-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosciw JG, Greytak EA, & Diaz EM (2009). Who, what, where, when, and why: demographic and ecological factors contributing to hostile school climate for lesbian, gay, bisexual, and transgender youth. Journal of Youth and Adolescence, 38(7), 976–988. doi: 10.1007/s10964-009-9412-1 [DOI] [PubMed] [Google Scholar]
- Lenhard W & Lenhard A (2016). Calculation of effect sizes. Retrieved from: https://www.psychometrica.de/effect_size.html. Dettelbach (Germany): Psychometrica. doi: 10.13140/RG.2.1.3478.4245 [DOI] [Google Scholar]
- Lewinsohn PM, Seeley JR, Roberts RE, & Allen NB (1997). Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology and Aging, 12(2), 277–287. [DOI] [PubMed] [Google Scholar]
- Lewis RJ, Derlega VJ, Clarke EG, Kuang JC, Jacobs AM, & McElligott MD (2005). An expressive writing intervention to cope with lesbian-related stress: The moderating effects of openness about sexual orientation. Psychology of Women Quarterly, 29(2), 149–157. doi: 10.1111/j.1471-6402.2005.00177.x [DOI] [Google Scholar]
- Lin YJ, & Israel T (2012). A computer-based intervention to reduce internalized heterosexism in men. Journal of Counseling Psychology, 59(3), 458–464. doi: 10.1037/a0028282 [DOI] [PubMed] [Google Scholar]
- Lucassen MF, Hatcher S, Fleming TM, Stasiak K, Shepherd MJ, & Merry SN (2015). A qualitative study of sexual minority young people’s experiences of computerised therapy for depression. Australasian Psychiatry, 23(3), 268–273. doi: 10.1177/1039856215579542 [DOI] [PubMed] [Google Scholar]
- Mays VM, & Cochran SD (2001). Mental health correlates of perceived discrimination among lesbian, gay, and bisexual adults in the United States. American Journal of Public Health, 91(11), 1869–1876. doi: 10.2105/ajph.91.11.1869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGarrity LA, & Huebner DM (2014). Is being out about sexual orientation uniformly healthy? The moderating role of socioeconomic status in a prospective study of gay and bisexual men. Annals of Behavioral Medicine, 47(1), 28–38. doi: 10.1007/s12160-013-9575-6 [DOI] [PubMed] [Google Scholar]
- Meijer R, de Vries R, & van Bruggen V (2011). An evaluation of the Brief Symptom Inventory–18 using item response theory: Which items are most strongly related to psychological distress? Psychological Assessment, 23(1), 193–202. doi: 10.1037/a0021292. [DOI] [PubMed] [Google Scholar]
- Morris SB (2008). Estimating effect sizes from pretest-posttest-control group designs. Organizational Research Methods, 11(2), 364–386. doi: 10.1177/1094428106291059 [DOI] [Google Scholar]
- Pachankis JE (2018). The scientific pursuit of sexual and gender minority mental health treatments: Toward evidence-based affirmative practice. American Psychologist, 73(9), 1207–1219. doi: 10.1037/amp0000357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, Eldahan AI, & Golub SA (2016). New to New York: Ecological and psychological predictors of health among recently arrived young adult gay and bisexual urban migrants. Annals of Behavioral Medicine, 50(5), 692–703. doi: 10.1007/s12160-016-9794-8 [DOI] [PubMed] [Google Scholar]
- Pachankis JE, & Goldfried MR (2010). Expressive writing for gay-related stress: psychosocial benefits and mechanisms underlying improvement. Journal of Consulting and Clinical Psychology, 78(1), 98–110. doi: 10.1037/a0017580 [DOI] [PubMed] [Google Scholar]
- Pachankis JE, Hatzenbuehler ML, Rendina HJ, Safren SA, & Parsons JT (2015). LGB-affirmative cognitive-behavioral therapy for young adult gay and bisexual men: A randomized controlled trial of a transdiagnostic minority stress approach. Journal of Consulting and Clinical Psychology, 83(5), 875–889. doi: 10.1037/ccp0000037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennebaker JW, & Beall SK (1986). Confronting a traumatic event: toward an understanding of inhibition and disease. Journal of Abnormal Psychology, 95(3), 274–281. [DOI] [PubMed] [Google Scholar]
- Poon CS, & Saewyc EM (2009). Out yonder: sexual-minority adolescents in rural communities in British Columbia. American Journal of Public Health, 99(1), 118–124. doi: 10.2105/ajph.2007.122945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poteat VP, Scheer JR, Marx RA, Calzo JP, & Yoshikawa H (2015). Gay-straight alliances vary on dimensions of youth socializing and advocacy: Factors accounting for individual and setting-level differences. American Journal of Community Psychology, 55(3–4), 422–432. doi: 10.1007/s10464-015-9722-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, & Bauer DJ (2006). Computational tools for probing interaction effects in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics, 31, 437–448. doi: 10.3102/10769986031004437 [DOI] [Google Scholar]
- Preston DB, & D’Augelli AR (2013). The Challenges of Being a Rural Gay Man. New York: Routledge. [Google Scholar]
- Rendina HJ, Gamarel KE, Pachankis JE, Ventuneac A, Grov C, & Parsons JT (2016). Extending the minority stress model to incorporate HIV-positive gay and bisexual men’s experiences: A longitudinal examination of mental health and sexual risk behavior. Annals of Behavioral Medicine, 51(2), 147–158. doi: 10.1007/s12160-016-9822-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice CE, Vasilenko SA, Fish JN, & Lanza ST (2019). Sexual minority health disparities: An examination of age-related trends across adulthood in a national cross-sectional sample. Annals of Epidemiology, 31, 20–25. doi: 10.1016/j.annepidem.2019.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riggle EDB, Gonzalez KA, Rostosky SS, & Black WW (2014). Cultivating positive LGBTQA identities: An intervention study with college students. Journal of LGBT Issues in Counseling, 8(3), 264–281. doi: 10.1080/15538605.2014.933468 [DOI] [Google Scholar]
- Radloff LS (1977). The CES-D scale a self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, & Grant M (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction, 88(6), 791–804. [DOI] [PubMed] [Google Scholar]
- Sloan DM, Marx BP, Lee DJ, & Resick PA (2018). A brief exposure-based treatment vs cognitive processing therapy for posttraumatic stress disorder: A randomized noninferiority clinical trial. JAMA Psychiatry, 75(3), 233–239. doi: 10.1001/jamapsychiatry.2017.4249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spijker BAJ, Batterham PJ, Calear AL, Farrer L, Christensen H, Reynolds J, & Kerkhof AJFM (2014). The suicidal ideation attributes scale (SIDAS): Community-based validation study of a new scale for the measurement of suicidal ideation. Suicide and Life-Threatening Behavior, 44(4), 408–419. doi: 10.1111/sltb.12084 [DOI] [PubMed] [Google Scholar]
- Swank E, Fahs B, & Frost DM (2013). Region, social identities, and disclosure practices as predictors of heterosexist discrimination against sexual minorities in the United States. Sociological Inquiry, 83(2), 238–258. doi: 10.1111/soin.12004 [DOI] [Google Scholar]
- Talley AE, Hughes TL, Aranda F, Birkett M, & Marshal MP (2014). Exploring alcohol-use behaviors among heterosexual and sexual minority adolescents: Intersections with sex, age, and race/ethnicity. American Journal of Public Health, 104(2), 295–303. doi: 10.2105/ajph.2013.301627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton GM, & Cohen GL (2011). A brief social-belonging intervention improves academic and health outcomes of minority students. Science, 331(6023), 1447–1451. doi: 10.1126/science.1198364 [DOI] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, & Anderson NB (1997). Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology, 2(3), 335–351. [DOI] [PubMed] [Google Scholar]
- Williams ML, Bowen AM, & Horvath KJ (2005). The social/sexual environment of gay men residing in a rural frontier state: Implications for the development of HIV prevention programs. Journal of Rural Health, 21(1), 48–55. [DOI] [PMC free article] [PubMed] [Google Scholar]


