Abstract
Background:
Inconclusive noninvasive tests (NITs) complicate the care of patients with suspected coronary artery disease, but their prevalence and impact on management, outcomes, and costs are not well described.
Methods:
PROMISE patients were randomized to stress testing (n=4533) or CT angiography (CTA) (n=4677). We assessed relationships between inconclusive results, subsequent testing, a composite outcome (death, myocardial infarction, or hospitalization for unstable angina), and healthcare expenditures.
Results:
Overall, 8.0% of tests were inconclusive (9.7% stress, 6.4% CTA). Compared with negative tests, inconclusive tests were more often referred to a second NIT (stress: 14.6% vs. 8.5%, OR 1.91; CTA: 36.5% vs. 8.4%, OR 5.95, p<0.001) and catheterization (stress: 5.5% vs. 2.4%, OR 2.36; CTA: 23.4% vs. 4.1%, OR 6.49, p<0.001), and composite outcomes were higher for both inconclusive tests (stress: 3.7% vs. 2.0%, HR 1.81, p=0.034; CTA: 5.0% vs. 2.2%, HR 1.85, p=0.044) and positive tests (stress: 8.3% vs. 2.0%, HR 3.50; CTA: 9.2% vs. 2.2%, HR 3.66, p<0.001). 24-month costs were higher for inconclusive tests than negative tests by $2905 (stress) and $4030 (CTA).
Conclusion:
Among patients with stable chest pain undergoing an NIT, inconclusive results occurred in 6% of CTA and 10% of stress tests. Compared to those with conclusive negative tests, individuals with inconclusive results more often underwent subsequent testing, had increased medical costs and experienced worse outcomes.
Journal Subject Terms: Diagnostic Testing, Exercise Testing, Coronary Artery Disease, Cost-Effectiveness
Keywords: Non-Invasive Testing, CT Angiography, Stress Testing, Inconclusive Results, Cost-Effectiveness
Clinical Summary
Evaluation of suspected coronary artery disease with noninvasive testing can sometimes yield inconclusive results. The current study sought to characterize the frequency of such inconclusive results and their implications on subsequent testing, clinical outcomes, and costs stratified by a randomized assignment to functional (stress) or anatomic (CT angiography) testing strategy. We found that about 1 in 12 noninvasive tests were inconclusive; when compared to negative tests, inconclusive tests led to more secondary noninvasive and invasive testing, with higher 24-month costs regardless of testing strategy. Patients with inconclusive results had worse clinical outcomes (all-cause mortality, myocardial infarction, or hospitalization for unstable angina) when compared to those with negative noninvasive tests even after adjustment for important clinical variables. Although we cannot directly address the reasons for these worse outcomes, only one third of patients went on to receive additional testing. Our findings highlight the possibility that in current real-world practice, patients with an inconclusive noninvasive test are at higher risk than those with a negative test, and may therefore warrant consideration for follow-up testing or further investigation, as clinically appropriate.
Introduction
Stable chest pain triggering suspicion of obstructive coronary artery disease (CAD) is often managed by noninvasive testing (NITs)1–3 and is associated with over $500 million in United States annual healthcare expenditures.4,5 Although data from the Prospective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE) indicated that the type of NIT chosen (anatomic vs. functional stress testing) did not affect midterm clinical outcomes,6 different types of tests may vary in their ability to provide conclusive, diagnostic information among different patient populations. Obtaining conclusive results from NITs is important to guide proper diagnosis, risk stratification and management and enhances patient satisfaction by providing a conclusive “answer” to the cause of their symptoms. Despite this, little has been published on the prevalence and predictors of inconclusive diagnostic testing, and on the impact inconclusive results have on downstream management, clinical outcomes, and healthcare expenditures.
The PROMISE trial randomized patients with stable chest pain undergoing evaluation for suspected CAD to either functional stress testing or anatomic testing with coronary computed tomographic angiography (CTA).6 The trial followed patients over a median of 25 months, allowing for an in-depth evaluation of the prevalence and impact of NIT results. The purpose of the current study is to 1) assess the prevalence of inconclusive NIT results and patient characteristics associated with inconclusive results; 2) determine the association between inconclusive tests, subsequent patient management, and clinical outcomes across testing modality; and 3) estimate the economic impact of inconclusive results.
Methods
The complete data set for the PROMISE trial has been deposited with the National Institutes of Health and is publicly available (https://biolincc.nhlbi.nih.gov/studies/promise/).
Study Cohort and Design
The PROMISE trial recruited outpatients without known CAD who presented with stable angina between July 2010 and September 2013 across 193 sites in North America.6,7 In brief, after obtaining informed written consent, the trial randomized 10,003 patients to anatomic evaluation (CTA with ≥64-slice multidetector scanning) versus functional stress testing (with the modality at the sites’ discretion including: exercise electrocardiography [ECG], exercise or pharmacologic stress echocardiography, or exercise or pharmacologic stress nuclear testing). For both arms, the local clinician was responsible for performing the test, its interpretation, and any subsequent clinical decision making. Local or central institutional review board at each center and enrolling site approved the study protocol.
For this per-protocol analysis, we included all patients in the primary PROMISE analysis except those who were not tested as randomized (n=770) or were missing key information regarding conclusiveness (n=23) (see Figure I in the Data Supplement). An intention-to-treat sensitivity analysis was also performed for comparative purposes (see Tables I and II in the Data Supplement) which excluded those who did not have the randomized test or had missing data (n=464). The relationships between test results (positive, negative, and inconclusive), NIT type, subsequent testing, and a composite outcome of all-cause death, myocardial infarction (MI), and unstable angina hospitalization (UAH) were assessed, and conclusive negative results were used as the reference group for comparisons with either inconclusive or positive results. In addition, the economic impact of inconclusive versus conclusive negative testing was evaluated.
Definitions of Conclusive and Inconclusive Testing
All “positive” and “negative” tests were considered to be conclusive (see result classification algorithms for each test type in Supplemental Figures II-VII). In brief, a positive exercise ECG (non-imaging) was defined as ST-segment changes consistent with ischemia during stress or early termination (<3 minutes) due to symptom reproduction, hypotension, and/or arrhythmia. Positive stress nuclear and stress echocardiography testing were defined as inducible ischemia in at least one of either anterior, inferior, or lateral territory corresponding to an expected, left anterior descending, right coronary, or left circumflex artery distribution or if an exercise stress test was terminated early (<3 minutes) due to ST-segment changes consistent with ischemia, symptom reproduction, hypotension, and/or arrhythmia. A positive CTA was defined as ≥70% stenosis in at least one epicardial artery or ≥50% stenosis in the left main artery. A negative test was defined as the absence of the above criteria in an otherwise technically conclusive study; for the purposes of this study, scar alone was insufficient for a positive result as this can arise from etiologies other than CAD.
Inconclusive test results were defined as a non-positive test considered by the site to be non-diagnostic or if maximum achieved heart rate with exercise or dobutamine stress was <85% age-predicted without evidence of ischemia. In addition, exercise ECG testing was considered to be inconclusive if the stress ECG was deemed borderline or indeterminate by the site due to poor technical quality. To maximize generalizability to a real-world clinic setting, all tests were performed and interpreted by each individual site. Reasons for inconclusiveness are heterogeneous (Supplemental Figures II-VII). Positive invasive coronary angiography (ICA) was defined as site interpretation with ≥70% stenosis in at least one epicardial artery or ≥50% stenosis in the left main artery.
Statistical Analyses
All analyses were performed on a per-protocol basis, except for the intention-to-treat sensitivity analyses (Supplemental Tables I and II). Baseline characteristics including demographics, cardiac risk factors, likelihood of CAD, and type of NIT were described using the median (25th, 75th percentile) for continuous variables and percentages for categorical variables. Descriptive statistical testing included the Wilcoxon rank sum test for continuous variables and chi-square testing for categorical variables. An unadjusted logistic regression model was used to assess the association between randomized NIT modality (functional testing vs. CTA), NIT type, and NIT inconclusiveness. Unadjusted logistic regression was also used to assess the association between NIT inconclusiveness and referral to second NIT and ICA. A multivariable logistic regression model assessed these associations after adjusting with prespecified variables including age, sex, race, body mass index, diabetes, smoking status/history, CAD equivalent, site characterization of chest pain (e.g. typical, atypical, or non-cardiac), provider estimation of likelihood of obstructive epicardial disease (high or very high), hypertension, dyslipidemia, family history of premature CAD, participation in physical activity, Framingham Risk Score (2008), and Diamond-Forrester score (2011). The linearity assumption was used for all continuous adjustment variables, and an appropriate nonlinear form was used in cases where the assumption did not hold..
The frequency and raw rate of the primary clinical event (time to all-cause death, MI, or UAH) was tabulated by comparison groups. An unadjusted Cox proportional hazards model was fitted to assess the association between NIT inconclusiveness and clinical outcomes. Proportional hazards assumptions were assessed for NIT inconclusiveness. If a substantial violation was found, measures were taken to identify an appropriate time-dependent representation that was used throughout. A multivariable Cox regression model was fitted to assess this association after adjustment for confounding variables as above. Both logistic regression and Cox regression models used patients with conclusive negative tests as the reference cohort.
Cost Analyses
Cost estimates were derived from 1) Premier Research Database for diagnostic testing, 2) hospital billing data, and 3) 2014 Medicare reimbursement schedule for physician costs. An adjusted repeated measures, mixed model was used to assess the association between inconclusive test results and costs over the first 24 months as previously described (see also the Data Supplement).8
Results
Baseline Characteristics
Among the 9210 patients in the PROMISE trial receiving testing, 737 (8.0%) had an inconclusive result (6.4% CTA, 9.7% stress). By stress modality, inconclusive frequency was 23.7% for exercise ECG, 11.9% for stress echocardiography, and 6.9% for stress nuclear. Among stress echocardiography and nuclear testing, the frequency of inconclusive results by stressor was 3.3% for pharmacologic stress and 10.5% for exercise stress (p<0.001). The CTA test result groups varied significantly with respect to age, race, sex, body mass index, smoking status, CAD risk equivalent, site characterization of chest pain, provider assessment of obstructive epicardial disease, ASCVD risk, Framingham risk score, Diamond-Forrester score, and prevalence of diabetes, hypertension, and dyslipidemia (p<0.01) (Table 1). Median coronary artery calcium (CAC) score was 402 (31, 1109) in inconclusive CTA results compared to 387 (131, 771) and 9 (0, 95) in conclusive positive and negative CTA results, respectively (p<0.001). The stress test result groups also varied significantly with respect to age, sex, smoking status, CAD risk equivalent, site characterization of chest pain, provider assessment of obstructive epicardial disease, ASCVD risk, Framingham risk score, Diamond-Forrester score, and prevalence of hypertension and diabetes (p<0.05) (Table 1). Notably, inconclusiveness was most often attributed to submaximal heart rate for stress tests, and calcifications and motion artifact for CTA (Table 2).
Table 1:
Patient Characteristics at Baseline by Inconclusiveness and Test Modality
| CTA (N=4677) | Stress Test (N=4533) | |||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | Inconclusive (N=299) | Conclusive Positive (N=534) | Conclusive Negative (N=3844) | P-value | Inconclusive (N=438) | Conclusive Positive (N=564) | Conclusive Negative (N=3531) | P-value |
| Demographics | ||||||||
| Age (Years) | 62.9 (57.0, 68.7) | 62.5 (56.5, 68.6) | 59.1 (53.9, 65.3) | <0.001 | 59.6 (54.6, 65.4) | 62.6 (56.9, 68.1) | 60.1 (54.6, 66.0) | <0.001 |
| Female sex | 140 (46.8%) | 184 (34.5%) | 2078 (54.1%) | <0.001 | 215 (49.1%) | 274 (48.6%) | 1932 (54.7%) | 0.004 |
| Race | 0.004 | 0.389 | ||||||
| Multi-Racial | 7 (2.4%) | 2 (0.4%) | 50 (1.3%) | 5 (1.2%) | 4 (0.7%) | 22 (0.6%) | ||
| White | 236 (79.5%) | 471 (89.5%) | 3187 (83.6%) | 355 (82.0%) | 479 (84.9%) | 3009 (86.0%) | ||
| Black | 42 (14.1%) | 31 (5.9%) | 426 (11.2%) | 59 (13.6%) | 61 (10.8%) | 360 (10.3%) | ||
| Asian | 10 (3.4%) | 17 (3.2%) | 109 (2.9%) | 8 (1.8%) | 13 (2.3%) | 74 (2.1%) | ||
| Indian | 2 (0.7%) | 3 (0.6%) | 31 (0.8%) | 2 (0.5%) | 5 (0.9%) | 22 (0.6%) | ||
| Hawaiian | 0 (0.0%) | 2 (0.4%) | 9 (0.2%) | 4 (0.9%) | 2 (0.4%) | 12 (0.3%) | ||
| BMI (kg/m2) | 30.1 (27.1, 35.9) | 30.0 (26.7, 33.9) | 29.4 (26.3, 33.8) | 0.010 | 29.8 (25.9, 33.9) | 30.0 (26.5, 35.1) | 29.8 (26.4, 33.7) | 0.186 |
| Cardiac Risk Factors | ||||||||
| Diabetes | 83 (27.8%) | 139 (26.0%) | 764 (19.9%) | <0.001 | 90 (20.5%) | 150 (26.6%) | 746 (21.1%) | 0.011 |
| Smoking (ever) | 130 (43.5%) | 217 (40.6%) | 1936 (50.4%) | <0.001 | 179 (40.9%) | 261 (46.3%) | 1764 (50.0%) | <0.001 |
| CAD risk equivalent | 96 (32.1%) | 160 (30.0%) | 900 (23.4%) | <0.001 | 113 (25.8%) | 178 (31.6%) | 883 (25.0%) | 0.004 |
| Site characterization of chest pain | <0.001 | 0.031 | ||||||
| Typical | 42 (14.0%) | 88 (16.5%) | 419 (10.9%) | 51 (11.6%) | 83 (14.7%) | 379 (10.7%) | ||
| Atypical | 227 (75.9%) | 404 (75.7%) | 3003 (78.1%) | 330 (75.3%) | 424 (75.2%) | 2782 (78.8%) | ||
| Non-cardiac | 30 (10.0%) | 42 (7.9%) | 422 (11.0%) | 57 (13.0%) | 57 (10.1%) | 370 (10.5%) | ||
| Provider estimation of likelihood of obstructive epicardial disease (High or Very High) | 24 (8.0%) | 57 (10.7%) | 138 (3.6%) | <0.001 | 29 (6.6%) | 64 (11.4%) | 127 (3.6%) | <0.001 |
| Hypertension | 218 (72.9%) | 362 (67.8%) | 2448 (63.7%) | 0.002 | 304 (69.4%) | 404 (71.6%) | 2255 (63.9%) | <0.001 |
| Dyslipidemia | 217 (72.6%) | 384 (71.9%) | 2561 (66.6%) | 0.008 | 306 (69.9%) | 383 (67.9%) | 2398 (67.9%) | 0.707 |
| Family history of premature CAD | 100 (33.7%) | 185 (34.8%) | 1239 (32.3%) | 0.493 | 130 (29.7%) | 160 (28.4%) | 1112 (31.6%) | 0.257 |
| Participate in physical activity | 165 (55.2%) | 263 (49.3%) | 1992 (51.9%) | 0.262 | 220 (50.3%) | 273 (48.4%) | 1840 (52.2%) | 0.211 |
| 10-Year CVD Risk | ||||||||
| Framingham Risk Score (2008) | 23.3 (13.3, 40.3) | 24.8 (15.7, 39.3) | 16.0 (10.0, 26.1) | <0.001 | 18.9 (11.4, 32.7) | 20.8 (12.9, 36.4) | 16.6 (10.3, 27.6) | <0.001 |
| ASCVD (2013) | 16.3 (8.6, 27.6) | 16.5 (9.2, 26.9) | 10.3 (5.8, 17.8) | <0.001 | 11.9 (6.6, 21.5) | 14.7 (8.6, 24.0) | 11.2 (6.0, 19.3) | <0.001 |
| Likelihood of CAD | ||||||||
| Diamond-Forrester (2011) | 47.4 (27.7, 59.4) | 48.9 (33.6, 59.4) | 37.0 (23.8, 48.9) | <0.001 | 38.4 (24.8, 57.7) | 47.1 (27.7, 59.4) | 37.0 (24.8, 48.9) | <0.001 |
| Calcium Scores (CTA Only) | ||||||||
| Calcium Score | 402.0 (31.0, 1108.5) | 386.5 (130.8, 771.0) | 8.5 (0.0, 94.5) | <0.001 | ||||
| Calcium ≥400 | 136 (50.0%) | 237 (48.8%) | 265 (7.7%) | <0.001 | ||||
Continuous variables are described using median (25th, 75th percentile). Categorical variables are described using frequency (%). Wilcoxon rank sum tests are used for continuous variables, and chi-square tests are used for categorical variables. BMI = body mass index, CTA = computed tomographic angiogram, CAD = coronary artery disease, CVD = cardiovascular disease, ASCVD = atherosclerotic cardiovascular disease.
Table 2:
Frequency of Conclusive/Inconclusive Results by Test Type
| Reason | Frequency |
|---|---|
| Overall Stress | |
| Conclusive Positive | 564 (12.4%) |
| Conclusive Negative | 3531 (77.9%) |
| Inconclusive | 438 (9.7%) |
| Exercise ECG | |
| Conclusive Positive | 54 (12.3%) |
| Conclusive Negative | 280 (63.9%) |
| Inconclusive | 104 (23.7%) |
| Target heart rate not attained | 34 (32.7%) |
| Borderline or indeterminate ECG Result | 70 (67.3%) |
| Stress Echo | |
| Conclusive Positive | 75 (7.5%) |
| Conclusive Negative | 805 (80.6%) |
| Inconclusive | 119 (11.9%) |
| Target heart rate not attained | 80 (67.2%) |
| Respiratory artifact | 1 (0.8%) |
| Poor sound transmission | 8 (6.7%) |
| Other | 30 (25.2%) |
| Stress Nuclear | |
| Conclusive Positive | 435 (14.1%) |
| Conclusive Negative | 2446 (79.0%) |
| Inconclusive | 215 (6.9%) |
| Target heart rate not attained | 152 (70.7%) |
| Motion artifact | 6 (2.8%) |
| Attenuation | 45 (20.9%) |
| GI uptake | 5 (2.3%) |
| Missing | 7 (3.3%) |
| CTA | |
| Conclusive Positive | 534 (11.4%) |
| Conclusive Negative | 3844 (82.2%) |
| Inconclusive | 299 (6.4%) |
| Motion artifact | 100 (33.4%) |
| Calcification | 131 (43.8%) |
| Image Noise | 18 (6.0%) |
| Other | 32 (10.7%) |
| Missing | 18 (6.0%) |
| Total | |
| Conclusive Positive | 1098 (11.9%) |
| Conclusive Negative | 7375 (80.1%) |
| Inconclusive | 737 (8.0%) |
ECG = electrocardiogram.
Association by NIT Type and Inconclusive Results
Stress testing overall was more likely to produce inconclusive results compared with CTA (adjusted OR 1.56, 95% CI 1.33–1.82, p<0.001) (Table 3). Specifically, exercise ECG (adjusted OR 4.78, 95% CI 3.69–6.20, p<0.001) and stress echocardiography (adjusted OR 2.11, 95% CI 1.68–2.66, p<0.001) more frequently had inconclusive results compared with CTA, but not nuclear testing (adjusted OR 1.06, 95% CI 0.88–1.27, p=0.564) (Supplemental Figure VIII). Both stress nuclear (adjusted OR 0.23, 95% CI 0.17–0.30, p<0.001) and stress echocardiography (adjusted OR 0.44, 95% CI 0.32–0.59, p<0.001) were less likely than exercise ECG to have inconclusive results (Supplemental Table III and Figure IX). A sensitivity analysis was performed using an intention-to-treat definition of treatment group, which showed similar results (Supplemental Data, Tables I and II).
Table 3:
Associations between NIT Type, Modality, and Inconclusiveness
| Frequency of Inconclusiveness (# Events/Sample Size) | Unadjusted* | Adjusted† | ||||
|---|---|---|---|---|---|---|
| Comparison of NIT Modality | Stress Test | CTA | Odds Ratio (95% CI) | P-value | Odds Ratio (95% CI) | P-value |
| Stress vs. CTA | 438/4533 (9.66%) | 299/4677 (6.39%) | 1.57 (1.34–1.83) | <0.001 | 1.56 (1.33–1.82) | <0.001 |
| Comparison of NIT Type | ||||||
| Stress Nuclear vs. CTA | 215/3096 (6.94%) | 299/4677 (6.39%) | 1.09 (0.91–1.31) | 0.338 | 1.06 (0.88–1.27) | 0.564 |
| Stress Echo vs. CTA | 119/999 (11.91%) | 299/4677 (6.39%) | 1.98 (1.58–2.48) | <0.001 | 2.11 (1.68–2.66) | <0.001 |
| Exercise ECG vs. CTA | 104/438 (23.74%) | 299/4677 (6.39%) | 4.56 (3.55–5.85) | <0.001 | 4.78 (3.69–6.20) | <0.001 |
NIT = noninvasive test.
Unadjusted model contains NIT modality or test type (stress nuclear, stress echo, exercise ECG vs. CTA).
Adjusted model contains NIT modality or test type (stress nuclear, stress echo, exercise ECG vs. CTA), age, sex, BMI, diabetes, smoker (ever/never), CAD equivalent, site characterization of chest pain, provider estimation of likelihood of obstructive epicardial disease (high or very high), hypertension, dyslipidemia, family history of premature CAD, participate in physical activity, Framingham Risk Score (2008), Diamond-Forrester (2011).
Subsequent Processes of Care and Clinical Outcomes
Inconclusive NIT results were more often followed with a second NIT compared with conclusive negative results for both stress and CTA (14.6% vs. 8.5%, adjusted OR 1.91, 95% CI 1.42–2.56, p<0.001; 36.5% vs. 8.4%, adjusted OR 5.95, 95% CI 4.52–7.85, p<0.001, respectively) (Table 4). Referral to ICA within 90 days was also more frequent with inconclusive versus conclusive negative stress and CTA testing (5.5% vs. 2.4%, adjusted OR 2.36, 95% CI 1.47–3.78, p<0.001; 23.4% vs. 4.1%, adjusted OR 6.49, 95% CI 4.67–9.02, p<0.001, respectively). For the composite outcome, inconclusive results had higher rates of all-cause death, MI, or UAH compared to conclusive negative results for both stress and CTA (3.7% vs. 2.0%, adjusted HR 1.81, 95% CI 1.05–3.13, p=0.034; 5.0% vs. 2.2%, adjusted HR 1.85, 95% CI 1.02–3.36, p=0.044, respectively) (Table 4). See Supplemental Tables IV and V for data on individual stress testing modalities.
Table 4:
Associations between Inconclusive Test Results and Process of Care and Outcomes by Test Type
| Frequency of Event (# Events/Sample Size) | Unadjusted | Adjusted* | ||||
|---|---|---|---|---|---|---|
| Process of Care | Conclusive Positive or Inconclusive | Conclusive Negative | Odds Ratio (95% CI) | P-value | Odds Ratio (95% CI) | P-value |
| Overall Stress | ||||||
| Referral to second NIT within 90 days of first NIT | ||||||
| Conclusive Positive vs. Conclusive Negative | 145/564 (25.71%) | 299/3531 (8.47%) | 3.74 (2.99–4.68) | <0.001 | 3.59 (2.85–4.53) | <0.001 |
| Inconclusive vs. Conclusive Negative | 64/438 (14.61%) | 299/3531 (8.47%) | 1.85 (1.38–2.47) | <0.001 | 1.91 (1.42–2.56) | <0.001 |
| Referral to ICA within 90 days of Randomization | ||||||
| Conclusive Positive vs. Conclusive Negative | 263/564 (46.63%) | 85/3531 (2.41%) | 35.43 (27.00–46.47) | <0.001 | 34.62 (26.08–45.98) | <0.001 |
| Inconclusive vs. Conclusive Negative | 24/438 (5.48%) | 85/3531 (2.41%) | 2.35 (1.48–3.74) | <0.001 | 2.36 (1.47–3.78) | <0.001 |
| CTA | ||||||
| Referral to second NIT within 90 days of first NIT | ||||||
| Conclusive Positive vs. Conclusive Negative | 124/534 (23.22%) | 324/3844 (8.43%) | 3.29 (2.61–4.14) | <0.001 | 2.97 (2.32–3.78) | <0.001 |
| Inconclusive vs. Conclusive Negative | 109/299 (36.45%) | 324/3844 (8.43%) | 6.23 (4.80–8.10) | <0.001 | 5.95 (4.52–7.85) | <0.001 |
| Referral to ICA within 90 days of Randomization | ||||||
| Conclusive Positive vs. Conclusive Negative | 354/534 (66.29%) | 159/3844 (4.14%) | 45.57 (35.87–57.91) | <0.001 | 42.81 (33.18–55.24) | <0.001 |
| Inconclusive vs. Conclusive Negative | 70/299 (23.41%) | 159/3844 (4.14%) | 7.08 (5.19–9.67) | <0.001 | 6.49 (4.67–9.02) | <0.001 |
| Outcome | Hazard Ratio (95% CI) | P-value | Hazard Ratio (95% CI) | P-value | ||
| Overall Stress | ||||||
| All-cause death/MI/UAH | ||||||
| Conclusive Positive vs. Conclusive Negative | 47/564 (8.33%) | 69/3531 (1.95%) | 4.45 (3.07–6.45) | <0.001 | 3.50 (2.38–5.15) | <0.001 |
| Inconclusive vs. Conclusive Negative | 16/438 (3.65%) | 69/3531 (1.95%) | 1.90 (1.10–3.28) | 0.021 | 1.81 (1.05–3.13) | 0.034 |
| CV Death/MI | ||||||
| Conclusive Positive vs. Conclusive Negative | 19/564 (3.37%) | 43/3531 (1.22%) | 2.74 (1.60–4.71) | <0.001 | 1.96 (1.11–3.46) | 0.019 |
| Inconclusive vs. Conclusive Negative | 11/438 (2.51%) | 43/3531 (1.22%) | 2.09 (1.08–4.06) | 0.029 | 2.04 (1.05–3.97) | 0.037 |
| CTA | ||||||
| All-cause death/MI/UAH | ||||||
| Conclusive Positive vs. Conclusive Negative | 49/534 (9.18%) | 83/3844 (2.16%) | 4.48 (3.15–6.38) | <0.001 | 3.66 (2.51–5.35) | <0.001 |
| Inconclusive vs. Conclusive Negative | 15/299 (5.02%) | 83/3844 (2.16%) | 2.43 (1.40–4.20) | 0.002 | 1.85 (1.02–3.36) | 0.044 |
| CV Death/MI | ||||||
| Conclusive Positive vs. Conclusive Negative | 14/534 (2.62%) | 45/3844 (1.17%) | 2.26 (1.24–4.12) | 0.008 | 1.66 (0.88–3.15) | 0.120 |
| Inconclusive vs. Conclusive Negative | 4/299 (1.34%) | 45/3844 (1.17%) | 1.18 (0.43–3.29) | 0.746 | 0.74 (0.23–2.43) | 0.623 |
ICA = invasive coronary angiography, MI = myocardial infarction, UAH = unstable angina hospitalization.
Adjusted model controls for NIT modality (stress test vs. CTA), age, sex, BMI, diabetes, smoker (ever), CAD equivalent, site characterization of chest pain, provider estimation of likelihood of obstructive epicardial disease (high or very high), hypertension, dyslipidemia, family history of premature CAD, participate in physical activity, Framingham Risk Score (2008), and Diamond-Forrester (2011).
Compared to conclusive negative stress and CTA tests, conclusive positive tests had higher referral to second NIT (25.7% vs. 8.5%, adjusted OR 3.59, 95% CI 2.85–4.53, p<0.001; 23.2% vs. 8.4%, adjusted OR 2.97, 95% CI 2.32–3.78, p<0.001, respectively) and ICA within 90 days (46.6% vs. 2.4%, adjusted OR 34.62, 95% CI 26.08–45.98, p<0.001; 66.3% vs. 4.1%, adjusted OR 42.81, 95% CI 33.18–55.24, p<0.001, respectively) (Table 4). Compared to conclusive negative stress and CTA tests, conclusive positive tests had higher composite outcomes of death, MI, or UAH (8.3% vs. 2.0%, adjusted HR 3.50, 95% CI 2.38–5.15, p<0.001; 9.2% vs. 2.2%, adjusted HR 3.66, 95% CI 2.51–5.35, p<0.001, respectively) (Table 4).
Of the 737 patients with inconclusive results, 67.7% did not receive any additional testing (46.5% CTA; 82.2% stress). These patients had lower average ASCVD and Framingham risk scores and lower pretest probability for CAD (p<0.001) when compared to those who did receive additional testing (Supplemental Table VI).
Economic Impact of Inconclusive Results
Cumulative medical costs at 24 months of follow up for patients with an inconclusive versus conclusive negative stress test were 38% higher (mean cost difference $2905, 95% CI $1197-$4614, p<0.001; Figure 1 and Supplemental Table VII). Patients with an inconclusive CTA had 140% higher mean cumulative medical costs than those with a conclusive negative result (mean cost difference $4030, 95% CI $1656-$6404, p<0.001), with a significant difference first seen at the 3-month time point, after which costs continued to diverge (Figure 1).
Figure 1 –
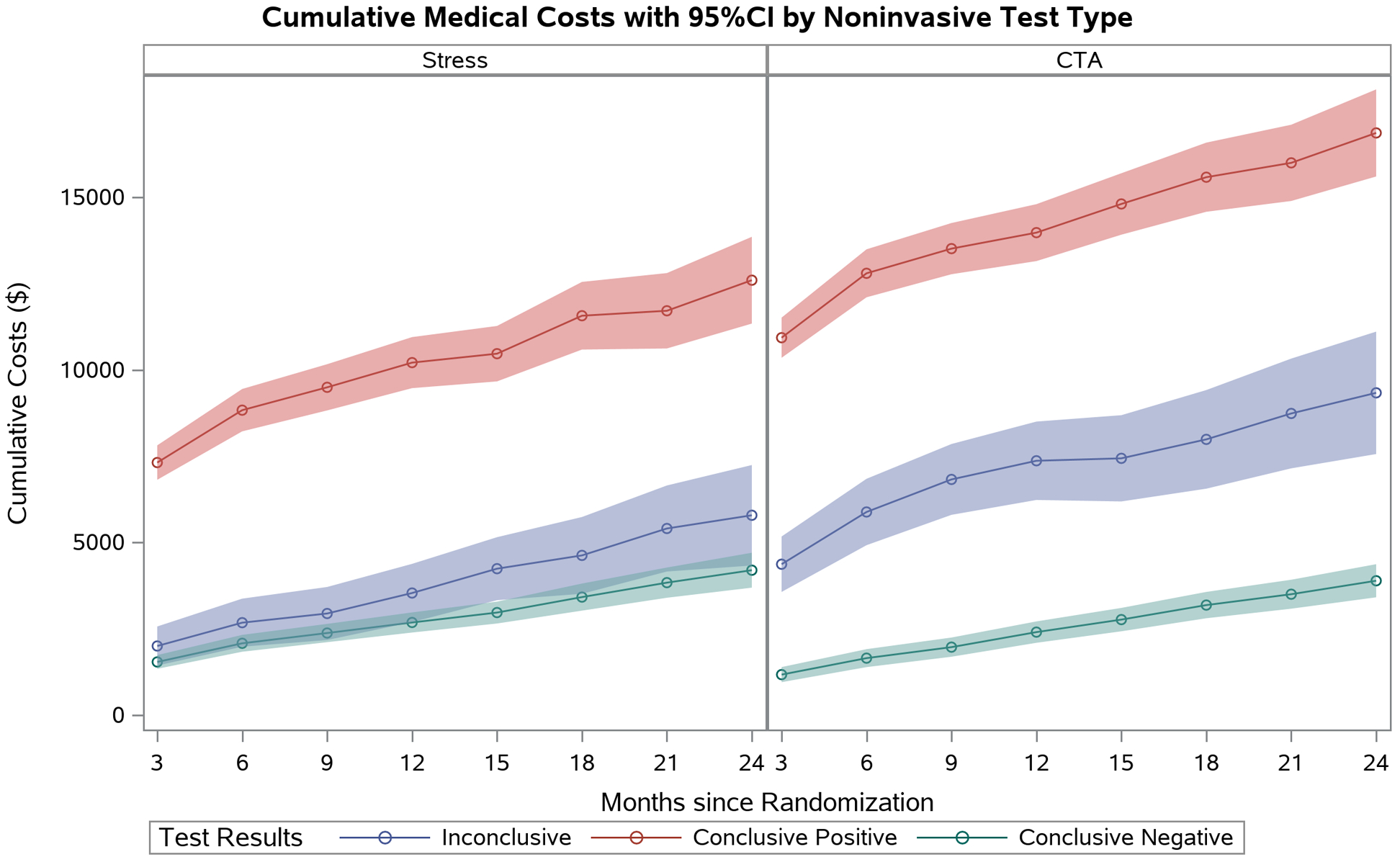
Mean cumulative medical costs with 95% CI (shaded area) by noninvasive test type. Tests are separated by conclusive positive (red line), inconclusive (blue line), or conclusive negative (green line) results.
Discussion
In this large, multicenter study of symptomatic outpatients without prior history of CAD undergoing noninvasive evaluation, we found that approximately one in 12 patients had an inconclusive result and only one third of these had subsequent testing. Compared to conclusive negative results, inconclusive stress and CTA results more often led to second NIT and ICA referral and were associated with worse clinical outcomes and up to 140% higher 24-month healthcare expenditures.
Inconclusive results were less often seen with CTA than stress testing overall, although nuclear stress and CTA had similar inconclusive rates. Evaluating individual modalities, we found that exercise ECG was most likely to yield an inconclusive result occurring in 24% of studies, 33% of which were due to submaximal heart rate. These rates are consistent with previous literature showing that 17–29% of exercise ECGs are inconclusive, with up to 57% due to submaximal heart rate.9–11 In stress echocardiography, we found an inconclusive rate of 12%, with 67% due to submaximal heart rate. Others have reported similar inconclusive rates of 15–29%, with 80–100% due to submaximal heart rate.9,12 Stress nuclear testing had a 7% inconclusive rate comparable to the rate found in previous studies.9,13–15 With regard to CTA testing, our observed inconclusive rate was 6%, similar to the 5% inconclusive rate found in the Scottish Computed Tomography of the Heart (SCOT-HEART) trial,10 but lower than the 11–13% rates found in smaller, older cohorts.16,17 The most commonly cited reasons for inconclusive CTA results are motion artifact and calcifications, which we observed in our study as well. As shown in Table 1, compared to conclusive negative results, the median CAC score for inconclusive CTAs was over forty times higher suggesting a possible anatomic rationale for the difficulty with interpretation.
Previous research on the implications of inconclusive NIT results is scant. One study by Christman et al. found that 21.6% patients with inconclusive exercise ECGs received an additional NIT. Patients with inconclusive results had adverse 3-year outcomes compared to those with negative results, but they did not evaluate other modalities.9 To our knowledge, the present study is the first to comprehensively evaluate subsequent processes of care, outcomes, and resource utilization across several NIT modalities, including CTA, and in a single cohort with uniform data collection methods. For both stress and CTA tests, patients with inconclusive results were more likely to receive a second NIT than those with a conclusive negative test. Still, approximately 80% of patients with an inconclusive stress test and 50% of patients with an inconclusive CTA did not receive additional testing (Supplemental Table VIII), even though an inconclusive result should neither increase nor decrease the pretest probability for CAD. Those with inconclusive results who did not have additional testing had slightly lower overall pretest probability of significant CAD (Supplemental Table VI) compared to those who did receive additional testing, suggesting that perhaps providers had enough clinical data to forego additional testing despite an inconclusive result. In particular, we were not able to capture the impact of “hidden” but significant information that even inconclusive results may provide (e.g., a finding of extensive or zero calcification, or excellent exercise tolerance) in spite of an overall inconclusive result, which may have an impact on additional testing decisions.
When compared to those with conclusive negative tests, individuals with inconclusive stress and CTA tests had a higher composite outcome of death, MI, or hospitalization for unstable angina. This is unlikely to be due to the higher burden of diabetes, hypertension, and dyslipidemia in the inconclusive group, since findings persisted after adjusting for these and other variables, suggesting that those with inconclusive results may be a high-risk population that warrants further clinical and research investigation.
Despite the relative frequency of inconclusive NITs, the optimal diagnostic strategy following an inconclusive result remains unclear. The most recent 2012 American College of Cardiology/American Heart Association guideline on stable ischemic heart disease gives a Class IIa recommendation for obtaining a CTA following an inconclusive functional NIT in patients with intermediate CAD pretest probability.18 This recommendation stems from an observational cohort study of 529 patients by de Azevedo et al. suggesting that an inconclusive NIT followed by CTA predicted adverse events based on stenosis severity.19 There is no stated recommendation on the optimal next test following an indeterminate CTA, but our data suggests that additional investigation is warranted in addition to risk-factor (e.g. hypertension, obesity, dyslipidemia, diabetes) optimization. Future studies should prospectively test various diagnostic algorithms following an inconclusive NIT to delineate preferred testing strategies.
Although we and other groups have evaluated comparative cost-effectiveness between imaging modalities,8,16,20–22 our study extends this discussion to consider the adverse financial implications of inconclusive results. We found higher costs in inconclusive versus conclusive negative stress and CTA results, possibly due to increased second NIT and ICA referral. For CTA tests, this cost difference started at 3 months following randomization and continued to diverge throughout the 24-month follow-up period.
Study Limitations
The trial design of PROMISE excluded patients whom clinicians opted for either conservative management or proceeded directly to ICA. Thus, the current study only addresses inconclusive results in patients between the two extremes of pretest probability for CAD. Further, the primary endpoint 2-year event rate was low at 3.0% indicating that this group was overall low risk. Given this low event rate, we were unable to make comparative statements between stress testing modalities with regard to outcomes and costs. Further, although all imaging readers were at least Level 2 trained in their respective modality, there may have been significant variability in how individual readers reported a test as conclusive. Finally, the current study does not evaluate the decision-making processes of clinicians regarding the subsequent care plan after receiving an inconclusive result
Conclusion
Inconclusive noninvasive testing is a relatively common occurrence seen in 8% of noninvasive diagnostic studies, and is less common in anatomic versus functional stress testing. Inconclusive stress and CTA test results are associated with higher cumulative healthcare expenditures, possibly driven by increased referral to additional noninvasive testing and catheterization. Patients with inconclusive results had worse clinical outcomes when compared to conclusive negative results regardless of testing modality, and may represent an under-investigated or higher-risk population or both.
Supplementary Material
Funding/Support:
This project was supported by grants R01HL098237, R01HL098236, R01HL98305, and R01HL098235 from the National Heart, Lung, and Blood Institute (NHLBI). The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper and its final contents. Akash Goyal had full access to all the data in the study and takes responsibility for its integrity and the data analysis. This paper does not necessarily represent the official views of NHLBI.
Footnotes
Disclosures:
Goyal: none.
Pagidipati: ownership – Freedom Health, Inc.; Physician Partners, LLC; RXAdvance, LLC; Florida Medical Associates, LLC.
Hill: none.
Alhanti: none.
Udelson: consultant fees/honoraria – Lantheus Medical Imaging; data safety monitoring board - Gilead, GSK; officer, director, trustee, or other fiduciary role – HFSA Executive Council; other - Abbott Laboratories, Circulation/AHA – Associate Editor, Editor – Circulation Heart Failure, Pfizer/GSK, Sunshine Heart; research/research grants – NHLBI, Otsuka.
Picard: honorarium – American Society of Echocardiography for service as Editor in Chief of the Journal of the American Society of Echocardiography.
Pellikka: grants – GE Healthcare, Lantheus Medical Imaging, OxThera, with money paid to her institution.
Hoffmann: grants – HeartFlow, Kowa Pharmaceuticals.
Mark: personal fees – Medtronic, CardioDx, and St. Jude Medical; grants – Eli Lilly, Bristol-Myers Squibb, Gilead Sciences, AGA Medical, Merck, Oxygen Biotherapeutics, AstraZeneca.
Douglas: grants – HeartFlow.
Clinical Trial Registration Information: URL: http://www.clinicaltrials.gov. Unique identifier: NCT01174550.
References
- 1.Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, et al. Heart disease and stroke statistics—2020 update: A report from the American Heart Association. Circulation. 2020;141:e000–e000. doi: 10.1161/CIR.0000000000000757 [DOI] [PubMed] [Google Scholar]
- 2.Cohn PF, Harris P, Barry WH, Rosati RA, Rosenbaum P, Waternaux C. Prognostic importance of anginal symptoms in angiographically defined coronary artery disease. Am J Cardiol. 1981;47:233–237. doi: 10.1016/0002-9149(81)90391-x. [DOI] [PubMed] [Google Scholar]
- 3.Mozaffarian D, Bryson CL, Spertus JA, McDonell MB, Fihn SD. Anginal symptoms consistently predict total mortality among outpatients with coronary artery disease. Am Heart J. 2003;146:1015–1022. doi: 10.1016/S0002-8703(03)00436-8. [DOI] [PubMed] [Google Scholar]
- 4.Ladapo JA, Blecker S, Douglas PS. Physician decision making and trends in the use of cardiac stress testing in the United States: an analysis of repeated cross-sectional data. Ann Intern Med. 2014;161:482–490. doi: 10.7326/M14-0296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iglehart JK. The new era of medical imaging--progress and pitfalls. N Engl J Med. 2006;354:2822–2828. doi: 10.1056/NEJMhpr061219. [DOI] [PubMed] [Google Scholar]
- 6.Douglas PS, Hoffmann U, Patel MR, Mark DB, Al-Khalidi HR, Cavanaugh B, Cole J, Dolor RJ, Fordyce CB, Huang M, et al. ; PROMISE Investigators. Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med. 2015;372:1291–1300. doi: 10.1056/NEJMoa1415516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Douglas PS, Hoffmann U, Lee KL, Mark DB, Al-Khalidi HR, Anstrom K, Dolor RJ, Kosinski A, Krucoff MW, Mudrick DW, et al. ; PROMISE investigators. PROspective Multicenter Imaging Study for Evaluation of chest pain: rationale and design of the PROMISE trial. Am Heart J. 2014;167:796–803 e1. doi: 10.1016/j.ahj.2014.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mark DB, Douglas PS, Daniels MR. Economic outcomes with anatomical versus functional diagnostic testing for coronary artery disease. Ann Intern Med. 2016;165:891. doi: 10.7326/L16-0482. [DOI] [PubMed] [Google Scholar]
- 9.Christman MP, Bittencourt MS, Hulten E, Saksena E, Hainer J, Skali H, Kwong RY, Forman DE, Dorbala S, O’Gara PT, et al. Yield of downstream tests after exercise treadmill testing: a prospective cohort study. J Am Coll Cardiol. 2014;63:1264–1274. doi: 10.1016/j.jacc.2013.11.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.SCOT-HEART Investigators. CT coronary angiography in patients with suspected angina due to coronary heart disease (SCOT-HEART): an open-label, parallel-group, multicentre trial. Lancet. 2015;385:2383–2391. doi: 10.1016/S0140-6736(15)60291-4. [DOI] [PubMed] [Google Scholar]
- 11.SCOT-HEART Investigators, Newby DE, Adamson PD, Berry C, Boon NA, Dweck MR, Flather M, Forbes J, Hunter A, Lewis S, et al. Coronary CT angiography and 5-year risk of myocardial infarction. N Engl J Med. 2018;379:924–933. doi: 10.1056/NEJMoa1805971. [DOI] [PubMed] [Google Scholar]
- 12.Flores-Blanco PJ, Cambronero F, Garcia-Navarro M, de la Morena G, Valdes M, Manzano-Fernandez S. Inconclusive exercise stress echocardiography in patients with chest pain: prevalence and clinical determinants. Rev Esp Cardiol (Engl Ed). 2018;71:406–408. doi: 10.1016/j.rec.2017.02.042. [DOI] [PubMed] [Google Scholar]
- 13.Schinkel AF, Elhendy A, van Domburg RT, Bax JJ, Roelandt JR, Poldermans D. Prognostic value of dobutamine-atropine stress (99m)Tc-tetrofosmin myocardial perfusion SPECT in patients with known or suspected coronary artery disease. J Nucl Med. 2002;43:767–772. [PubMed] [Google Scholar]
- 14.Greenwood JP, Maredia N, Younger JF, Brown JM, Nixon J, Everett CC, Bijsterveld P, Ridgway JP, Radjenovic A, Dickinson CJ, et al. Cardiovascular magnetic resonance and single-photon emission computed tomography for diagnosis of coronary heart disease (CE-MARC): a prospective trial. Lancet. 2012;379:453–460. doi: 10.1016/S0140-6736(11)61335-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tandon V, Hall D, Yam Y, Al-Shehri H, Chen L, Tandon K, Beanlands RS, Wells GA, Ruddy TD, Chow BJ. Rates of downstream invasive coronary angiography and revascularization: computed tomographic coronary angiography vs. Tc-99m single photon emission computed tomography. Eur Heart J. 2012;33:776–782. doi: 10.1093/eurheartj/ehr346. [DOI] [PubMed] [Google Scholar]
- 16.Nielsen LH, Olsen J, Markenvard J, Jensen JM, Norgaard BL. Effects on costs of frontline diagnostic evaluation in patients suspected of angina: coronary computed tomography angiography vs. conventional ischaemia testing. Eur Heart J Cardiovasc Imaging. 2013;14:449–455. doi: 10.1093/ehjci/jes166. [DOI] [PubMed] [Google Scholar]
- 17.Wang R, Renker M, Schoepf UJ, Wichmann JL, Fuller SR, Rier JD, Bayer RR 2nd, Steinberg DH, De Cecco CN, Baumann S. Diagnostic value of quantitative stenosis predictors with coronary CT angiography compared to invasive fractional flow reserve. Eur J Radiol. 2015;84:1509–1515. doi: 10.1016/j.ejrad.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 18.Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP, Douglas PS, Foody JM, Gerber TC, Hinderliter AL, et al. ; American College of Cardiology Foundation. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: executive summary: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012;126:3097–3137. doi: 10.1161/CIR.0b013e3182776f83. [DOI] [PubMed] [Google Scholar]
- 19.de Azevedo CF, Hadlich MS, Bezerra SG, Petriz JL, Alves RR, de Souza O, Rati M, Albuquerque DC, Moll J. Prognostic value of CT angiography in patients with inconclusive functional stress tests. JACC Cardiovasc Imaging. 2011;4:740–751. doi: 10.1016/j.jcmg.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 20.Genders TS, Petersen SE, Pugliese F, Dastidar AG, Fleischmann KE, Nieman K, Hunink MG.. The optimal imaging strategy for patients with stable chest pain: a cost-effectiveness analysis. Ann Intern Med. 2015;162:474–484. doi: 10.7326/M14-0027. [DOI] [PubMed] [Google Scholar]
- 21.van Waardhuizen CN, Khanji MY, Genders TSS, Ferket BS, Fleischmann KE, Hunink MGM, Petersen SE. Comparative cost-effectiveness of non-invasive imaging tests in patients presenting with chronic stable chest pain with suspected coronary artery disease: a systematic review. Eur Heart J Qual Care Clin Outcomes. 2016;2:245–260. doi: 10.1093/ehjqcco/qcw029. [DOI] [PubMed] [Google Scholar]
- 22.Bertoldi EG, Stella SF, Rohde LEP, Polanczyk CA. Cost-effectiveness of anatomical and functional test strategies for stable chest pain: public health perspective from a middle-income country. BMJ Open. 2017;7:e012652. doi: 10.1136/bmjopen-2016-012652. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


