Abstract
The purpose of this study was to describe prior use of detoxification and addiction treatment programs among injection drug users (IDUs) in Kabul, Afghanistan. From 2005–2006, IDUs (n=464) recruited into this cross-sectional study completed an interviewer-administered questionnaire and whole blood rapid testing with fingerstick samples for HIV, syphilis, and hepatitis C antibody and B surface antigen testing. Participants were predominantly male (99.8%), Afghan (98.9%), and had little formal education. Correlates of detoxification and addiction treatment were identified with logistic regression. The majority (94.0%, n=435) felt great/ urgent need for treatment, of whom, 56.3% (n=245) reported inability to access treatment. Prior detoxification was associated with new needle use with each injection (AOR=1.91, 95% CI: 1.12 – 3.26) and prior incarceration (AOR=1.81, 95% CI: 1.04 – 3.13). The study’s limitations are noted. Rapid scale-up and subsidy of needle and syringe programs and opioid agonist treatment is urgently needed in Kabul.
Keywords: Afghanistan, detoxification, injecting drug user, addiction treatment, needle exchange program
Background
Opium has been used both recreationally and medicinally in Afghanistan for centuries (Chouvy, 2002). In recent years, opiate use, and injection drug use in particular, has increased (UNODC, 2005). A recent nationwide study indicates that drug use is increasing in most areas of Afghanistan, with approximately 920,000 active drug users (3.8% of the population) estimated to reside within the country (UNODC, 2005). This number is expected to increase further as refugees from surrounding countries, where many first started using illicit substances, repatriate in the near future (UNODC, 2005). Reasons postulated for the increasing numbers of users are large-scale opium production creating a ready drug supply within the country, poor socioeconomic opportunities, and repatriation of individuals influenced by residence in countries with higher prevalence of drug use (Hankins, 2002; Strathdee, 2006). Availability of opium and heroin may expand as production increases. Current projections indicate that Afghanistan provided 92% of the global opium supply in 2006; 10% of the total production is estimated to be consumed within the country (UNODC, 2005; UNODC, 2006).
In an environment of increasing drug use and high risk drug and sexual practices among drug users, effective harm reduction and addiction treatment programs need to be widely available to prevent or stabilize epidemics of blood-borne infection (WHO/UNAIDS/UNODC, 2006). For the purpose of this paper, needle and syringe programs (NSPs) were considered to be any program distributing, exchanging, and collecting injection equipment at no cost to the client and from any site, whether fixed or field-based for the purposes of this paper. Utilization of NSPs and addiction treatment, particularly opioid substitution therapy, has been associated with decreasing HIV seroprevalence and incidence and injecting behaviors among injection drug users (IDUs) in international settings (Wodak, 2006; Bastos, 2000; Kerr, 2004). Drug treatment, particularly opioid substitution therapy, has been consistently associated with decreases in HIV risk behaviors and overdose-related morbidity and mortality (Kerr, 2004; Caplehorn, 1996; Metzger, 1993). Among HIV-infected IDU, methadone and buprenorphine maintenance has been associated with increased uptake of antiretroviral therapy (Antela, 1997; Moatti, 2000). In light of these data, methadone and buprenorphine have been added to the World Health Organization’s essential drug list (WHO, 2006).
Addiction treatment and detoxification programs have been present in Afghanistan for several decades, though methods are currently limited to acute treatment of withdrawal symptoms for detoxification, which may or may not be combined with inpatient or outpatient counseling (UNODC, 2005; Todd, 2005). Methadone and buprenorphine have not been approved for medical use within Afghanistan to date. The approval process lies with the Ministry of Public Health and this approval is necessary prior to importation or use of any medication by the government or affiliated medical services. In the 2005 nationwide drug use survey, no more than 100 inpatient beds for either drug treatment or detoxification programs were identified, suggesting that coverage of these programs to drug users potentially in need of treatment was only 0.25% (UNODC, 2005).
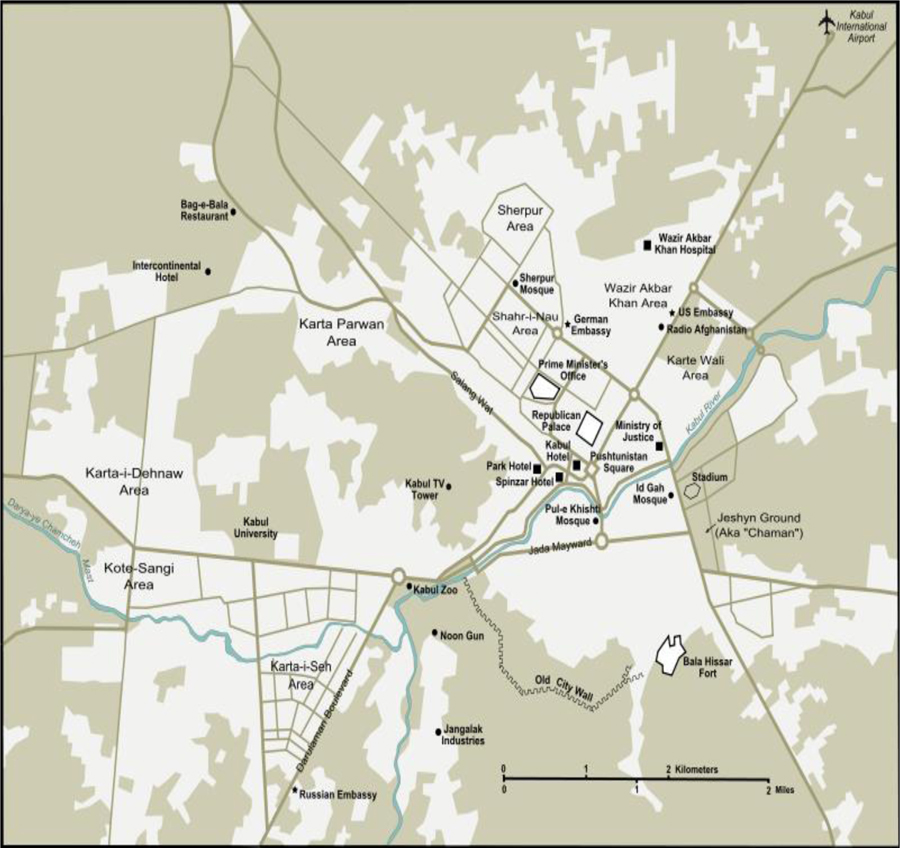
At the time of the study, Kabul, the capital of Afghanistan, had one fixed site NSP and three public drug treatment programs functioning. Kabul has been the site of prior surveys that estimated number of drug users, types of drugs used, and drug treatment program utilization (UNODC, 2005; UNODC, 2003) (Figure 1). Treatment modalities in Kabul, where the largest number of treatment programs exist, are largely abstinence-based counseling programs and treatment of acute withdrawal symptoms with benzodiazepines or other psychotropic medications. Inpatient treatment is possible but waiting lists often exceed six months due to the small number of available beds.
Figure 1.
City map of Kabul, Afghanistan.
*Available at http://en.wikipedia.org/wiki/Image:Kabul_City_Map.svg
The purpose of this paper is to assess prevalence and correlates of prior utilization of detoxification, and addiction treatment programs among IDUs in Kabul. These data are meant to provide the perspectives of drug users that may be used to tailor services of harm reduction and addiction treatment programs in this setting to the needs of intended clientele.
Methods
Setting
Kabul, the capital of Afghanistan, has experienced rapid population growth in the last five years, with an estimated 2.5 million current residents (CSO, 2007). This sudden influx is due to returned refugees from neighboring countries and internally-displaced people feeing either instability or drought (North, 2005; IRIN, 2002) In Afghanistan, the unemployment rate is currently estimated at 40% with 53% of the population living below the poverty line; these conditions are certainly true of and potentially exacerbated in Kabul due to crowding (CIA, 2005). It is estimated that the greatest density of heroin users are in Kabul, estimated at 16,500 users (UNODC, 2005).
Study Design and Participants
We conducted a cross-sectional study of IDUs in Kabul, Afghanistan, between June, 2005 and June, 2006 through the Voluntary Counseling and Testing (VCT) Center at the Central Polyclinic, an Afghan Ministry of Public Health facility. Eligible participants were those reporting injecting drugs within the past six months (confirmed through injection stigmata), aged 18 years or greater, and able to provide informed consent. Participants were recruited by outreach workers from harm reduction programs or were referred by prior participants. Prior to enrollment, the research study was approved by both domestic and international investigational review boards.
Procedures
Potential participants were identified by outreach workers and others knowledgeable about the drug user community in Kabul. The outreach workers were either current or former employees of harm reduction programs or pharmacists or others acquainted with and trusted by social networks of drug users. Outreach workers, seven of eight of whom were male, approached IDU of their acquaintance in areas of the city where drug users are known to congregate. Outreach workers asked potential participants if they were interested in participating in a study that provided medical testing for hepatitis and HIV. The number of IDU declining to accompany the outreach worker was not measured. IDU interested in study participation accompanied an outreach worker to the VCT Center, the site of enrollment. At the center, a trained study representative explained the study in a confidential setting and obtained informed consent. Each participant was assigned a unique study number. Participants were interviewed by a trained study representative of the same gender for completion of the questionnaire. Two participants elected to discontinue study activities and their information and consents were destroyed and not considered in analysis. Participants received a small gift of hygiene items (e.g. soap, toothbrush) of approximately U.S.$4 value; this gift was not advertised during recruitment or the consent process to avoid coercion. Provision of free counseling and testing was available to all drug users who visited the VCT Center with an outreach worker, regardless of study entry.
Pre- and post-test counseling and rapid whole blood testing for HIV, syphilis, hepatitis C antibody, and hepatitis B surface antigen was subsequently performed with preliminary positive tests. Confirmatory testing with Western Blot (HIV BLOT 2.2®, GeneLabs Diagnostics, Singapore) for HIV, T. pallidum plasma agglutination (TPPA, Fujirebio Diagnostics, Malvern, PA, USA), a second, serum-based rapid test (Standard Diagnostics HBV, Standard Diagnostics Laboratories, Korea) for hepatitis B, and RIBA (RIBA 3.0 SIA®, Chiron Corporation, Emeryville, CA, USA) for HCV was performed at the VCT Center in Kabul.. All participants received risk reduction counseling, condoms and sterile syringes, with referrals for treatment, voluntary detoxification programs, and NSPs upon request.
Measurement of variables and outcomes of interest
The questionnaire was pilot-tested for accuracy of translation and relevance of content with five IDU in Kabul and reviewed by all investigators to finalize content. The questionnaire included questions pertaining to sociodemographics, travel, incarceration, and medical histories, and drug use and sexual behaviors. Usual sources of injecting equipment were assessed. Multiple choices for prior treatment programming were provided, which encompassed both detoxification and treatment. Prior detoxification was divided into voluntary or non-voluntary (“lock-up”) programs, either with or without medication for withdrawal symptoms. Treatment choices included inpatient or outpatient programs with or without treatment of withdrawal symptoms. Programs incorporating group activities and counseling on either inpatient or outpatient basis were also included.
Detoxification was analyzed separately from treatment. Prior detoxification and treatment of addiction were determined through affirmative responses to the question,“Have you ever received treatment for a drug problem?”. Treatment was distinguished from detoxification by a multiple choice question assessing type of prior program, with the possible answers being lock-up (forced detoxification), detoxification without medication (“cold turkey”), detoxification with medication, residential treatment program, outpatient center at hospital (treatment), substitution therapy as inpatient or outpatient (methadone, buprenorphine, or other opiate), or other type of treatment with the answer specified. Multiple answers were allowed from those who reported more than one prior episode of treatment of detoxification, with utilization based on the total reported number of episodes. Responses for frequency and duration of prior addiction treatment were similarly measured in months and days, respectively. Participants were also queried about perceived need for and barriers to addiction treatment.
Statistical Analysis
The outcomes of interest for this analysis are prior utilization of addiction treatment and/or detoxification. Prevalence and correlates of prior addiction treatment and detoxification were assessed separately. Data analysis was performed six months after data collection and the manuscript written within two months of completing data analysis.
Continuous variables, such as age of initiating injection use, were dichotomized using the median age as the cut-off point. Correlates of prior treatment and detoxification were assessed with univariable logistic regression. Simultaneous multivariable logistic regression was performed to identify independent associations; inclusion of variables was determined using the likelihood ratio test considering all variables with p≤0.10 in univariable analysis. A p-value of 0.05 was required for inclusion in the final regression model.
Results
Of the 464 IDUs in this study, all but one was male and the majority (99%) were Afghan. The sole female participant was excluded from subsequent analysis. Most participants (88.1%) reported being currently employed, of whom the majority reported being day laborers (77.9%). One third reported no formal education and 22.0% had five years or less of formal education. Monthly earnings varied greatly, with approximately half of participants (49.3%) reporting earning 3000 Afghanis (1 U.S.$=49 Afghanis). Half were married and only four participants reported being homeless.
Only one participant (0.2%) reported ever receiving syringes from an NSP; no participants mentioned NSP as their usual source for syringes during their lifetime or in the last six months. The majority (94.0%) felt great or urgent need for addiction therapy, of whom, 56.3% reported being unable to access treatment. The chief reasons for inability to receive treatment were perceived financial limitations and no available beds at the center (Table 1). The small number of subjects utilizing NSP precluded subsequent analysis investigating correlates of its use.
Table 1.
Characteristics of prior addiction treatment among injection drug users in Kabul, Afghanistan.
| Variable | N | % |
|---|---|---|
| Prior treatment/ detox program enrollment (n=458): | ||
| None | 292 | 63.8% |
| Types of prior program (193 total answers, multiple answers allowed): | ||
| Hospital outpatient counseling program | 88 | 45.6% |
| Detoxification with treatment of withdrawal symptoms | 21 | 10.9% |
| Detoxification without treatment of withdrawal symptoms | 16 | 8.3% |
| Imprisonment/ Lock-up | 15 | 7.8% |
| Residential Program | 13 | 4.4% |
| Opioid Substitution Therapy | 2 | 1.0% |
| Other | 5 | 2.6% |
| Payment for Prior Treatment or Detoxification (n=166): | ||
| Yes | 130 | 78.3% |
| Location of Treatment or Detoxification (n=155): | ||
| Afghanistan: | 87 | |
| Iran: | 49 | |
| Pakistan: | 18 | |
| Number of Prior Treatment Courses (n=47): | ||
| One | 25 | 53.2% |
| Two | 11 | 23.4% |
| Three or more | 11 | 23.4% |
| Number of Prior Detoxification Courses (n=44): | ||
| One | 28 | 63.6% |
| Two | 7 | 15.9% |
| Three or more | 9 | 20.5% |
| Median | IQR | |
| Treatment Duration: | 10 days | 2 – 20 days |
| Detoxification Duration: | 9 days | 2 – 30 days |
| Time Elapsed Since Last Treatment: | 7 mos | 2 – 9 mos |
| Time Elapsed Since Last Detox: | 9 mos | 4 – 12 mos |
Only 14.9% of participants had ever undergone prior detoxification lasting a median of nine days. Prior detoxification was associated with using a new syringe with each injection (OR=1.81, 95% CI: 1.07–3.08) in univariable analysis. In multivariable analysis, prior detoxification was independently associated with using a new needle with each injection (AOR=1.91, 95% CI: 1.12 – 3.26) and with prior incarceration (AOR=1.81, 95% CI: 1.04 – 3.13).
Approximately one fourth (24.0%) of all participants reported prior treatment for addiction, with a median of ten months since the last treatment episode (Table 1). Outpatient programs were the most common addiction treatment reported and Kabul was the most frequent site for addiction treatment. In univariable analyses, prior addiction treatment was significantly associated with perceived difficulty attaining a new syringe (OR=1.91, 95% CI: 1.24 – 2.94). Other high risk injection and sexual behaviors were not significantly different between those who had prior treatment and those not reporting prior treatment. Multivariable analysis was not performed since no other variables met our criteria for consideration (i.e., p<0.10).
Discussion
The public health infrastructure of Afghanistan is rebuilding after decades of conflict; treatment of drug addiction has not been a priority area within the nascent health care system. However, rising numbers of IDUs and emergence of HIV and other blood-borne infections within the IDU population indicate the need for increasing availability of and services offered to drug users in Kabul (UNODC, 2005; UNAIDS, 2006). The most important findings of this study are the urgent need and unmet demand for treatment programs among this high risk population, consistent with the 2005 UNODC survey findings (UNODC, 2005). Although more than one-third of participants had previously undergone treatment or detoxification, most perceived great need for treatment and at least half felt they were unable to access treatment, lending further support for expansion of treatment programs.
In 2006, the Ministry of Counter Narcotics reported that approximately U.S.$5 million has been invested in demand reduction programming in Afghanistan, including educational programs, NSP, and addiction treatment (personal communication, Dr. Mohammad Zafar). Of the public, no-cost treatment programs currently operating in Kabul, the oldest has been present for 21 years. The treatment philosophy has abstinence as the over-arching goal, with a measured progression towards abstinence in the program starting with motivational counseling sessions and reduction in daily drug dose to an inpatient detoxification program. The duration of the programs vary, with attendance in the outpatient group sessions ranging between one and three months, before detoxification (GTZ, 2006). Several of the treatment programs have been founded by local NGOs with experience with addiction treatment programs in Pakistan or international NGOs with experience in Europe. Data on overall program retention rates and outcomes in Afghanistan are not available, but one program reports a relapse rate of 35% within one year.(personal communication, Dr. S. Wali) Many of the current addiction treatment programs in Kabul are expanding their services to include NSPs and voluntary counseling and testing services on site, emulating successful harm reduction programming in culturally-similar settings like Iran (Vazirian, 2005; WHO, 2004a). The “triangular clinic” model of Iran unifies opioid substitution therapy, blood-borne infection counseling and testing for blood borne infections, needle, syringe and condom distribution, and antiretroviral treatment and support for those living with HIV/AIDS and their families (WHO, 2004a). This model has been found to be acceptable to both drug using clients and to the community in which the clinic is located, supported by qualitative testimony from service clients (WHO, 2004a). We speculate that this combination of treatment and harm reduction services, including opioid substitution therapy, may also be acceptable in Kabul; follow-up of current efforts is warranted to determine multiservice acceptability in this setting.
Another noteworthy finding of this study is the near absent utilization of NSP and lack of opioid agonist treatment or maintenance programs. Ample evidence supports the benefits of these programs, particularly for preventing an HIV epidemic, and the opportunity to do so in this setting will evaporate with delay (WHO/UNAIDS/UNODC, 2004b; Wodak, 2006; Bastos, 2000; Kerr, 2004). During the six month period between participant entry and the writing of this manuscript (six months), two additional NSPs with primary distribution and collection through outreach workers have opened in Kabul. However, opioid agonist treatment is currently unavailable; methadone and buprenorphine are not included on the list of medications approved for importation at this time. However, a pilot opioid substitution program is being considered. Opioid substitution therapy has been implemented in Central and South Asian countries and may be beneficial in Afghanistan (WHO/UNAIDS/UNODC, 2004b; Azim, 2005; Frantz, 2000).
Only perceived difficulty accessing a new syringe was associated with a prior treatment episode. During treatment episodes, IDU may be isolated from their usual syringe sources, being others in their social networks. This isolation may lead to perceived difficulty accessing syringes for those who resume injecting. No association between previous treatment and income level was detected, despite financial reasons being the most commonly reported barrier to treatment. This may be because the direct and indirect costs for services, particularly in the private sector, are so high that no one in this IDU population can afford them. Even free treatment contains indirect financial barriers, as those who are currently working must be absent from their jobs to attend motivational sessions and inpatient detoxification.
There were three no-cost treatment centers in Kabul operating at the time of the study, one more has since been added. However, before patients may be admitted for inpatient stay, several programs maintain the policy that the patient must attend a daily motivational program at the center for one to three months. This daily program requires daily transportation to and from the center and coverage of living and drug use expenses, which may present significant barriers to drug users living on the street or without family support. Even those IDU who were employed risk losing their job if they must attend a program daily. Private programs may cost as much as 10,000 Afghanis (approx U.S.$205) for a fifteen day detoxification program, which is prohibitive for many drug users and their families in a country whose gross national income was estimated at $250 in 2005 (UNICEF, 2007). Further study is needed to determine motivations for treatment in the Afghan setting.
Prior detoxification was associated with prior incarceration and use of a new needle with each injection. The association with incarceration may reflect involuntary detoxification in prison, resulting in misclassification. While drug users are to receive treatment for the first offense by Afghan law, relapse is punishable by imprisonment (Todd, 2005). Also, IDU imprisoned for non-drug related reasons may have experienced as involuntary “detoxification” while in prison. Involuntary detoxification programs exist in Afghanistan, where IDU are committed by their families, and IDU may not distinguish between these programs and imprisonment. It is important to note the potential perception of IDU that incarceration equated detoxification; addressing this perception is critical for any programming offering detoxification services in this setting.
Reported new needle use with each injection may reflect education received from either counselors or fellow IDUs during detoxification regarding low price and availability of syringes. Reported new needle use may also reflect behavior or socially-desirable response based on information regarding reducing blood-borne infection risk received during a detoxification program. This seems unlikely as those having prior detoxification were not less likely to report sharing syringes or using condoms. Detoxification has been found to be a marker for risky injecting practices, like receptive needle sharing, but in some cases has been associated with reductions in risky injecting behavior, as observed among IDU in Thailand (Choopanya, 2003; Peters, 1998; Liu, 2006). We did not observe either such relationship; however, there may have been insufficient power to detect a relationship due to the small number of participants reporting prior detoxification.
This study has important limitations that must be considered, which are self-reporting of behaviors, low sample sizes for some analyses, portrayal of treatment programming from only one perspective, and non-random convenience sampling. Both prior treatment and high risk behaviors were based on self-report; we asked for specific details of therapy (timing and location) to improve reporting accuracy. There were relatively fewer IDU who reported prior detoxification, which reduced statistical power to detect associations. Motivations for resuming injecting drug use were not examined; these issues likely impact relapse and should be investigated in subsequent studies. Additionally, interviewing just those active IDU who had previously had treatment may provide a biased view of treatment as we only have the perspective from those who have relapsed or have not been able to access treatment. Program implementers and other stakeholders were not interviewed, so little may be said about efficacy and acceptability of addiction treatment and harm reduction programming to the Kabul community, except information collected by other surveys (UNODC 2003, UNODC 2005). Last, respondent-driven sampling methods were not possible due to concerns of compromise of participant confidentiality, thus, these results may not be applicable to all IDU in Kabul.
Conclusions
It is clear that great demand for addiction therapy exists in Kabul, which is likely to increase should the trend of increasing drug use in modern Afghanistan continue (UNODC, 2005). Lack of funding for or social barriers to expansion or continuation of treatment centers, NSPs, and other harm reduction services has been identified in several settings as a direct contributor to high rates of morbidity and mortality among substance abusers (Platt, 2004; He, 2005). Further, harm reduction programming has been found to be cost-effective due to number of HIV infections averted in a variety of limited resource settings (Vickerman, 2006; Kumaranayake, 2004). It is imperative that funding for counter-narcotic activities be equitably distributed to improve the health of drug users and prevent potential epidemics of blood-borne infections in Afghanistan. This process will need to be politically driven, and is an expected outcome of nascent political advocacy projects for HIV and harm reduction now being initiated in Afghanistan.
Acknowledgements:
The authors wish to thank the Kabul VCT Center, Zindagi Nawin and Nejat Center harm reduction programs, and their outreach workers for their contributions, Drs. Mohammad Raza Stanekzai and Mohammad Zafar Rasuli for additional input and review, the Ministries of Public Health and Counter Narcotics of the Islamic Republic of Afghanistan for their support, and, most importantly, our participants for their time and trust. This study was funded by the Walter Reed Army Institute of Research. The opinions and assertions made by the authors do not reflect the official position or opinion of the U.S. Department of the Navy or Army, or of the respective in-country National HIV/AIDS Control Programs and other Non-Governmental Organizations (NGOs). Dr. Todd appreciates support from the Fogarty International Center of the National Institutes of Health (K01TW007408).
References:
- Antela A, Casado JL, Gonzalez MJ, Perez P, Perez-Elias MJ, Montilla P, Buzon L. (1997) Influence of a methadone maintenance programme on the improved outcome of a cohort on injecting drug users with advanced HIV disease. AIDS 11:1405–6. [PubMed] [Google Scholar]
- Azim T, Hussein N, Kelly R. (2005) Effectiveness of harm reduction programmes for injecting drug users in Dhaka city. Harm Reduction Journal 2:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastos FI, Strathdee SA. (2000). Evaluating effectiveness of syringe exchange programmes: current issues and future prospects. Social Science and Medicine 51:1771–82. [DOI] [PubMed] [Google Scholar]
- Caplehorn JR, Dalton MS, Haldar F, Petrenas AM, Nisbet JG. (1996). Methadone maintenance and addicts’ risk of fatal heroin overdose. Substance Use and Misuse 31:177–96. [DOI] [PubMed] [Google Scholar]
- Central Intelligence Agency. (2005) The World Factbook: Afghanistan. [https://www.cia.gov/library/publications/the-world-factbook/geos/af.html#Econ] Downloaded August 19, 2007.
- Central Statistics Office (CSO). (2007) Annual Report, Kabul-Afghanistan. [http://www.cso.gov.af/Census/census.htm]. Central Statistics Office, Kabul, Afghanistan: Downloaded July 31, 2007. [Google Scholar]
- Choopanya K, Des Jarlais DC, Vanichseni S, Mock PA, Kitayaporn D, Sangkhum U, Prasithiphol B, Hiranrus K, van Griensven F, Tappero JW, Mastro TD. (2003). HIV risk reduction in a cohort of injecting drug users in Bangkok, Thailand. Journal of Acquired Immune Deficiency Syndrome 33:88–95. [DOI] [PubMed] [Google Scholar]
- Chouvy PA: Golden Crescent In Encyclopedia of Modern Asia. 1st Edition. Edited by Levinson D, Christensen K. Chicago: Chas. Scribner & Sons; 2002. Pg. 441. [Google Scholar]
- Frantz D. (2000). Bishkek Journal; Heroin and Needles: Battling AIDS in Central Asia. [http://query.nytimes.com/gst/fullpage.html?sec=health&res=9E03E2D7113FF935A25753C1A9669C8B63]. New York Times, New York, Downloaded February 12, 2007. [Google Scholar]
- German Technical Cooperation (GTZ). Emerging Practices for the Treatment and Prevention of Drug Dependence in Afghanistan. Integrated Drug Prevention, Treatment, and Rehabilitation Project in Afghanistan (IDPA). Wali Computer and Printing Press, Kabul, Afghanistan. [Google Scholar]
- Hankins CA, Friedman SR, Zafar T, Strathdee SA. (2002). Transmission and prevention of HIV and sexually transmitted infections in war settings: implications for current and future armed conflicts. AIDS 16:2245–2252. [DOI] [PubMed] [Google Scholar]
- He N, Detels R. (2005). The HIV epidemic in China: history, response, and challenge. Cell Research 15:825–32. [DOI] [PubMed] [Google Scholar]
- IRIN News. (2002) Afghanistan: Focused on the internally displaced. [http://www.irinnews.org/InDepthMain.aspx?InDepthId=41&ReportId=70993&Country=Yes] United Nations Office for Coordination of Humanitarian Affairs; Downloaded August 19, 2007. [Google Scholar]
- Joint United Nations Program on AIDS (UNAIDS). (2006). AIDS Epidemic Update. UNAIDS, Geneva. [Google Scholar]
- Kerr T, Wodak A, Elliott R, Montaner JS, Wood E. (2004). Opioid substitution and HIV/AIDS treatment and prevention. Lancet. 364:1918–9. [DOI] [PubMed] [Google Scholar]
- Kumaranayake L, Vickerman P, Walker D, Samoshkin S, Romantzov V, Emelyanova Z, Zviagin V, Watts C. (2004) The cost-effectiveness of HIV preventive measures among injecting drug users in Svetlogorsk, Belarus. Addiction 99:1565–76. [DOI] [PubMed] [Google Scholar]
- Liu H, Grusky O, Zhu Y, Li X. (2006). Do drug users in China who frequently receive detoxification treatment change their risky drug use practices and sexual behavior? Drug and Alcohol Dependence 84:114–21. [DOI] [PubMed] [Google Scholar]
- Metzger DS, Woody GE, McLellan AT, O’Brien CP, Druley P, Navaline H, DePhilippis D, Stolley P, Abrutyn E. (1993) Human immunodeficiency virus seroconversion among intravenous drug users in- and out-of-treatment: an 18-month prospective follow-up. Journal of Acquired Immune Deficiency Syndrome 6:1049–56. [PubMed] [Google Scholar]
- Moatti JP, Carrieri MP, Spire B, Gastaut JA, Cassuto JP, Moreau J. (2000) Adherence to HAART in French HIV-infected injecting drug users: the contribution of buprenorphine drug maintenance treatment. The Manif 2000 study group. AIDS 14:151–5. [DOI] [PubMed] [Google Scholar]
- North A. (2005) Refugees make do in Kabul’s ruins. [http://news.bbc.co.uk/1/hi/world/south_asia/4269551.stm] BBC News, London, England: Downloaded August 19,2007. [Google Scholar]
- Peters A, Davies T, Richardson A. (1998) Multi-site samples of injecting drug users in Edinburgh: prevalence and correlates of risky injecting practices. Addiction 93:253–67. [DOI] [PubMed] [Google Scholar]
- Platt L, Hickman M, Rhodes T, Mikhailova L, Karavashkin V, Vlasov A, Tilling K, Hope V, Khutorksoy M, Renton A. (2004) The prevalence of injecting drug use in a Russian city: implications for harm reduction and coverage. Addiction 99:1430–8. [DOI] [PubMed] [Google Scholar]
- Strathdee SA, Stachowiak JA, Todd CS, Al-Delaimy WK, Wiebel W, Hankins C, Patterson TL. (2006). Complex emergencies, HIV, and substance use: no “big easy” solution. Substance Use and Misuse 41:1637–51. [DOI] [PubMed] [Google Scholar]
- Todd CS, Safi N, Strathdee SA. (2005) Drug use and harm reduction in Afghanistan. Harm Reduction Journal 2:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Childrens Fund (UNICEF). (2007). Afghanistan: statistics. Available at: http://www.unicef.org/infobycountry/afghanistan_afghanistan_statistics.html Accessed August 9, 2007.
- United Nations Office on Drugs and Crime (UNODC). (2003). Community Drug Profile #5: An assessment of problem drug use in Kabul city. UNODC, Kabul, Afghanistan. [Google Scholar]
- United Nations Office on Drugs and Crime (UNODC). (2005). Afghanistan Drug Abuse Survey 2005. UNODC, Kabul, Afghanistan. [Google Scholar]
- United Nations Office on Drugs and Crime. (2006). Afghan opium cultivation soars 59 percent in 2006, UNODC survey shows. Available at: http://www.unodc.org/unodc/press_release_2006_09_01.html Downloaded January 16, 2007.
- Vazirian M, Nassirimanesh B, Zamani S, Ono-Kihara M, Kihara M, Ravari SM, Gouya MM. (2005). Needle and syringe sharing practices of injecting drug users participating in an outreach HIV prevention program in Tehran, Iran: a cross-sectional study. Harm Reduction Journal 2:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vickerman P, Kumaranayake L, Balakireva O, Guinness L, Artyukh O, Semikop T, Yaremenko O, Watts C. (2006). The cost-effectiveness of expanding harm reduction activities for injecting drug users in Odessa, Ukraine. Sexually Transmitted Diseases 33(10 Suppl):S89–102. [DOI] [PubMed] [Google Scholar]
- Wodak A, Cooney A. (2006). Do needle syringe programs reduce HIV infection among injecting drug users: a comprehensive review of the international evidence. Substance Use and Misuse 41:777–813. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2004a). Best practice in HIV/AIDS prevention and care for injecting drug abusers: the Triangular Clinic in Kermanshah, Islamic Republic of Iran. WHO, Regional Office for the Eastern Mediterranean; Cairo. [Google Scholar]
- World Health Organization (WHO)/ United Nations Joint Commission on AIDS (UNAIDS)/ UNODC position paper. (2004b). Substitution maintenance therapy in the management of opioid dependence and HIV/AIDS prevention. WHO, Geneva. [Google Scholar]
- WHO Technical Report Series. (2006) The selection and use of essential medicines. WHO, Geneva. [Google Scholar]