Abstract
Purpose
Increasing evidence suggests that fibromyalgia most likely represents a neurological dysfunction. We previously hypothesized that at least some fibromyalgia cases may be caused by irritation of nerve root fibers and sensory neurons due to moderately increased cerebrospinal pressure. Because of the rostro-caudal hydrostatic pressure gradient, neurogenic abnormalities are expected to be most pronounced in sacral nerve roots. The purpose was to review electrodiagnostic tests of patients with fibromyalgia.
Methods
A retrospective review of electrodiagnostic test results, including the lumbar and sacral nerve root myotomes of patients diagnosed with fibromyalgia according to the 1990 criteria of the American College of Rheumatology was done.
Results
All 17 patients were female. Sural nerve responses could not be elicited in 12% and S1-Hoffmann reflex latencies were increased in 41%. In 12% of the patients, fibular motor nerve distal latency and conduction velocity were outside normal limits. Needle-EMG revealed neurogenic motor unit potentials in 0% of L2, 6% of L3, 29% of L4, 71% of L5, 47% of S1, 94% of S2, and 76% of S3-S4 myotomes. S3-S4 nerve-supplied anal reflexes were delayed in 94%.
Conclusion
This is the first time that electrodiagnostic data of both lumbar and sacral nerve root myotomes in fibromyalgia patients are presented. All patients showed neurogenic abnormalities that were more pronounced in the sacral than in the lumbar myotomes with a rather patchy distribution pattern. We propose that, in addition to skin punch biopsies to assess small fiber neuropathy, assessment of the anal reflex may be a useful part of the diagnostic pathway in patients with fibromyalgia.
Keywords: large fiber neuropathy, anal reflex, sacral nerves, nerve conduction studies, needle EMG
Introduction
The cause of fibromyalgia (FM) remains elusive. Increasing evidence, however, indicates that at least some FM cases are probably due to a neurological dysfunction. Up to 94% of patients with FM (PFM) present with neurological complaints, such as paresthesia (prickling, needles, numbness), electric shocks and bursts, evoked pain when wearing tight clothes or when touching the skin, hot and burning pain sensations, sensitivity to temperature, severe pressure pain, and weakness in the arms and legs.1–3
Moreover, in PFM, multiple objective neurological symptoms can be detected, such as sensory abnormalities (impairments in vibration, temperature, or pinprick sensation), elevated temperature and mechanical detection thresholds, muscle weakness, poor balance, and walking difficulties (sensory ataxia).1,2,4–8
Since 2013, microscopic studies of skin biopsies, corneal confocal microscopy and electrodiagnostic (EDX) studies have detected small fiber neuropathy (SFNP) in up to 50% of PFM.5,6,9–14 Recently, EDX evidence for large nerve involvement in 90% of PFM was reported.2
Previously, we hypothesized that at least some FM cases may be caused by moderately longstanding or intermittently increased cerebrospinal fluid pressure, forcing cerebrospinal fluid (CSF) into the nerve root sheaths. This increased pressure inside the nerve root sheaths may irritate or damage the nerve root fibers and the sensory neurons in the dorsal root ganglion (DRG), causing widespread radicular pain.15 Because of the human upright position, hydrostatic pressure is the highest in the lowest nerve roots; therefore, according to this hypothesis, EDX abnormalities are expected to be more pronounced in sacral nerve roots.
The aim of this study was to retrospectively review EDX tests of PFM, which included lumbar and sacral nerve roots.
Materials and Methods
The electronic database of a physiatrist outpatient clinic for patients consulting for musculoskeletal pain was searched to identify patients previously diagnosed with FM according to the 1990 criteria of the American College of Rheumatology.
Patients were referred because of pain and/or paresthesia in the low back, the pelvis, the legs and/or perineal pain. None of the patients showed EDX evidence of polyneuropathy or suffered diabetes.
Only those who had undergone EDX tests of the lumbar and sacral nerve root myotomes conducted by the same expert electrophysiologist skilled in pelvic floor and foot muscle EDX (FB) were selected.
A Natus Synergy EMG machine (Natus Medical Incorporated 6701 Koll Center Parkway, Suite 120, Pleasanton, CA 94566 USA) with filter settings from 20 hertz (low) to 20,000 hertz (high) and Natus disposable concentric needle electrodes, 25 mm in length and 30G, 0.33 mm in diameter, were used.
The submitted study was approved by the institutional review board AZ Rivierenland Bornem. Because of the retrospective nature of the study, patient consent to review their medical records was not required by the AZ Rivierenland Bornem IRB. Patient data were anonymized and were treated in compliance with the Declaration of Helsinki.
Nerve Conduction Studies
Nerve conduction studies included the sural nerves (containing fibers from nerve roots S1 and S2), the motor fibular nerves and the S1 Hoffmann reflexes (the electrophysiological equivalent of the Achilles tendon reflex).
For the sural nerves, the stimulation site was slightly lateral to the calf midline, 14 cm from the detecting electrode, which was placed posteroinferior to the lateral malleolus. The local skin temperature was ≥ 30°C. The latencies to onset and onset-to-peak amplitude were calculated. The reference values for normal latency were < 3.6 milliseconds (ms) and amplitude ≥ 6 microvolts (µV).
For the motor fibularis profundus nerve, the detecting electrode was placed on the extensor digitorum brevis muscle. The stimulating site at the ankle was 5–8 cm proximal to the recording electrode, lateral to the tendon of the m. tibialis anterior muscle and below the knee, and 2–5 cm distal to the proximal part of the caput fibulae. Distal motor latencies, baseline-to-peak amplitudes, and nerve conduction velocities were recorded. The reference values for normal conduction velocity were ≥ 39 m/sec, latency < 6 ms and amplitude ≥ 1000 µV.16
To obtain the S1 Hoffmann reflex, the stimulating electrode was placed over the popliteal tibial nerve in the popliteal fossa with the leg stretched and the recording electrode placed on the medial head of the gastrocnemius muscle. The reference values were a latency < 32 ms for body length ≤1.80 m, or a left-right difference of ≤ 2 ms.17
Needle Electromyography (EMG)
Needle EMG included lumbar and sacral myotomes: vastus medialis muscle (L3); vastus lateralis muscle (L4); extensor digitorum longus muscle (L5); tibialis anterior muscle (L4-L5); medial head of the gastrocnemius muscle (S1); tibial nerve-supplied intrinsic foot muscles (S2); and external anal sphincter (S3-S4).
During needle EMG, the presence of abnormal spontaneous activity during muscle relaxation as a sign of axonal motor irritation or denervation and/or the presence of at least 50% polyphasic motor unit potentials (MUPs) during muscle contraction were considered abnormal. Most muscles normally show only 5–25% polyphasic MUPs.18,19
We doubled the highest amount to 50% polyphasic MUPs as the cutoff value to avoid overestimating the findings at 25%.
Anal Reflex
The S3-S4 nerve-supplied external anal sphincter guarding reflex (anal reflex) is the electrophysiological equivalent of the anocutaneous reflex, a reflexive contraction of the external anal sphincter upon stroking the perianal skin. The anal reflex is imperative for bowel continence. A reflex arc consists of both a motor (efferent) and a sensory (afferent) limb. Needle EMG of the anal sphincter evaluates only the motor limb, whereas when assessing the anal reflex, the sensory limb would also be included. Because both the external anal sphincter and urethral sphincter are innervated by the S3-S4 nerves, this perineal reflex also indirectly provides information about the urethral sphincter.20
The patients lay on their left side. The needle was first inserted on the left side and then on the right side of the sphincter (3 and 9 o’clock positions) at the mucocutaneous junction at a depth of approximately 3 mm. Electrical stimulation with a maximal pulse (300 V, 35mA) and 1-ms duration on the midline of the sacrum, just caudal of the sacrococcygeal joint, evokes a reflex contraction of the external anal sphincter mediated via the sacral nerve roots 3 and 4. The latency was measured from the onset of the stimulation artifact to the onset of the clearly defined reflex response at the external anal sphincter (Figure 1). The reference value for a normal latency was <40 ms (or < 45 ms in women who had given vaginal birth) and/or a left-right difference < 6.0 ms or left-right difference in amplitude < 500 µV.21
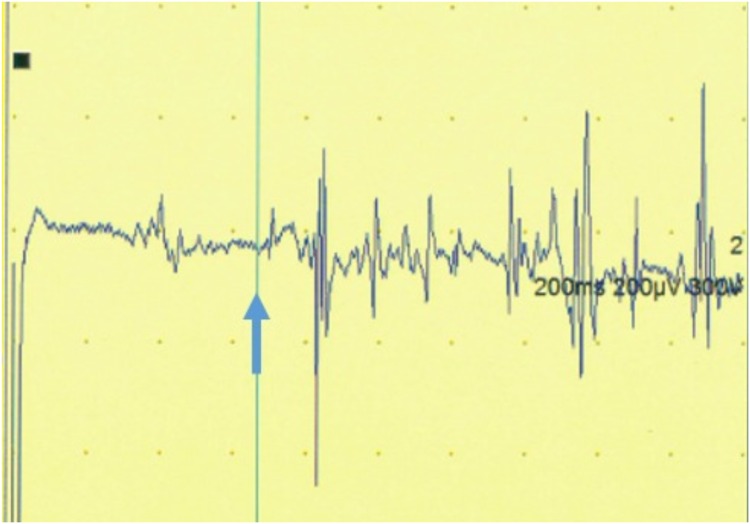
Figure 1.
Example of a significantly delayed anal reflex response of 66.80 ms (cutoff for latency < 40 ms or < 45 ms in women who had given vaginal birth). The blue vertical cursor indicates the onset of the anal reflex response.
Figure 1 shows an example of a significantly delayed anal reflex response of 66.80 ms.
Results
EDX studies that included lumbar and sacral nerve root myotomes of seventeen patients (all female) were retrieved. The mean age was 45.8 ± 9.9 years (range: 35–67 years). Table 1 shows the results of the nerve conduction studies and needle EMG.
Table 1.
Results of Nerve Conduction Studies and Needle EMG in Patients with Fibromyalgia
| Nerves | Number and Percentage of Patients with EMG Abnormalities (Total N =17) | |
|---|---|---|
| Nerve Conduction Studies | ||
|
Sural nerve Latency: >3.6 ms (14 cm) |
2 | 12% |
|
Fibular nerve Conduction velocity: <39 m/sec; latency: >6 ms; amplitude: <1000 µV |
2 | 12% |
|
Hoffmann reflex Latency: >32 ms; left/right difference >2 ms |
7 | 41% |
|
Anal reflex Latency: >40 ms or >45 ms in women who had given vaginal birth; left/right difference > 6 ms; amplitude: left-right difference ≥500 µV |
16 | 94% |
|
Needle EMG ≥50% neurogenic motor unit potentials | ||
| L2 | 0 | 0% |
| L3 | 1 | 6% |
| L4 | 5 | 29% |
| L5 | 12 | 71% |
| S1 | 8 | 47% |
| S2 | 16 | 94% |
| S3-S4 | 13 | 76% |
Nerve Conduction Studies
The sural nerve response could not be elicited in 12% of the PFM. In 88% of the patients, the amplitude was ≤ 12 µV.
Hoffmann reflex latencies were delayed in 41% (35% unilaterally and 6% bilaterally).
In 12% of the patients, fibular motor nerve conduction latency and conduction velocity were not within normal limits.
Needle EMG
Neurogenic MUPs were observed in 0% of L2 myotomes, 6% of L3 myotomes, 29% of L4 myotomes, 71% of L5 myotomes, 47% of S1 myotomes, 94% of S2 myotomes, and 76% of S3-S4 myotomes.
Abnormal spontaneous activity, including prolonged insertional activity, fibrillation potentials, positive sharp waves, and isolated or repetitive fasciculation potentials, was detected in 82% of S2 myotomes, in 6% of L5 myotomes and in 18% of S1 myotomes.
Anal Reflex
Ninety-four percent of the PFM showed delayed S3-S4 nerve root-supplied anal reflexes: unilaterally delayed in 47% and bilaterally delayed in 47%.
Three of the patients with a unilaterally delayed anal reflex did not show significant needle EMG abnormalities in the external anal sphincter on that side.
Discussion
This review of EDX studies of a cohort of 17 PFM revealed nerve conduction and needle EMG abnormalities in multiple lumbar and sacral myotomes in all patients. All but one patient showed delayed S3-S4 nerve root-supplied anal reflex. Because the sacral nerve roots are more affected than the lumbar nerve roots, these findings indicated that the abnormalities may have been caused by increased hydrostatic pressure in the nerve root sheaths.
Nerve Conduction Studies
Sural nerve responses could not be elicited in 12%. In 88% of the PFM, the amplitude was ≤ 12 µV. In an EMG study in patients clinically suspected of having SFNP, a relationship was observed between mild degrees of large fiber dysfunction and small fiber loss. According to the authors, this indicated that in patients with SFNP, small fiber dysfunction was accompanied by discrete alterations in large fiber function that fell within normal ranges. For example, in their study, a sural nerve action potential ≤12 µV was associated with SFNP, although the amplitude was >6 µV. This threshold value of ≤12 µV defined SFNP cases with 80% sensitivity and 72% specificity.22 Similarly, Caro et al2 found mixed small and large fiber neuropathy in most PFM. An explanation may be that intraepidermal nerve fibers are unmyelinated axons extending from small DRG neurons. Indeed, patients with sensory neuronopathy (sensory neuron disease) can show a loss of the small fibers at the limbs.23
Martínez-Lavín14 proposed that an alternative hypothesis for FM is stress-related dysautonomia with neuropathic pain features rather than centralized pain syndrome. The author assumed that the DRG may be the key autonomic-nociceptive short-circuit site.14 This assumption is partly in accordance with our hypothesis in which we proposed that neuropathic pain features are caused by increased cerebrospinal pressure inside the DRG. Longstanding moderately or intermittently increased cerebral and spinal pressure forces CSF into the nerve root sheaths, thereby irritating or compressing the nerve fibers (axons) in the nerve roots and the sensory neurons in the DRG. Due to the upright position, hydrostatic pressure is highest in the sacral dural sac.3 Therefore, according to our hypothesis, the sacral nerves would be predominantly affected, which would be reflected in more prevalent EMG abnormalities in the lowest nerve root myotomes. This pattern of findings was confirmed in our EDX study.
We detected discrete abnormalities in the fibular nerve conduction latency and amplitude in 2 PFM (12%). This percentage is in accordance with the nerve conduction studies of Ersoz,24 who found significantly prolonged fibular distal motor latencies and decreased fibular motor conduction in 5 of 33 (15%) PFM. The fibularis longus muscle is innervated by L5. According to Ersoz,24 these findings may have been due to nerve entrapment from multifactorial origins. The position of the fibular nerve at the fibular head and at the ankle are superficial and covered only by subcutaneous tissue and skin. Thus, the fibular nerve is more vulnerable to external compression, such as prolonged periods of immobilization or incorrect positioning of the legs, which may be more common in these patients.24
Additionally, in our cohort, S1-innervated Hoffmann reflexes were delayed in 41% of the PFM, which was in accordance with the findings of Caro et al,2 who detected delayed Hoffmann reflexes in 35% of PFM. Delayed Hoffmann reflexes may be due to sensory S1 radiculopathy. According to our hypothesis, this delay may be caused by increased pressure in the DRG containing the sensory neurons of S1 nerve roots.
Needle EMG
Needle EMG examination is more sensitive to axonal loss than nerve conduction studies.25 Needle EMG examination of the sacral nerve roots is an underutilized tool. Electrophysiologists are uncertain of how to interpret observed abnormalities in the S2-supplied intrinsic foot muscles, especially in the absence of external compressive pathology, eg, cauda equina syndrome. The major reason is that earlier published studies have reported abnormalities in the intrinsic foot muscles of normal subjects in the form of prolonged insertional activity.26–28 However, none of these studies had demonstrated sustained positive sharp waves or fibrillation potentials, which are the only true denervated spontaneous single muscle fiber discharge configurations. A later published EMG study by Dumitru et al29 examining intrinsic foot muscles in 50 asymptomatic subjects demonstrated these sustained fibrillation potentials and positive sharp waves in only 2% (1/50) of the subjects.30
Another type of pathological activity that may be found in relaxed muscles during needle EMG is fasciculation potentials. These fasciculation potentials may be a sign of irritation of the axons but not a sign of denervation, as the axons are not interrupted. They can be seen in radiculopathies due to compression causing irritation without interruption of the axons.31 We found fasciculation potentials in the foot muscles in 41% of PFM.
It can be argued that the S2-innervated plantar foot muscles show more EMG abnormalities because foot muscles are prone to normal “wear and tear” from walking and standing. However, abnormalities should be symmetrical in both feet. In our patients, EMG abnormalities in the intrinsic foot muscles were more pronounced in one foot compared to the other in 10 (60%) of PFM, suggesting a more proximal pathology.
Because of the above relative difficulties with the interpretation of needle EMG, it is a prerequisite that the electrophysiologist is experienced in EMG of sacral nerve root myotomes, as was the case in our study.
In our retrospective study, in the S2-innervated intrinsic foot muscles, irritation of the nerve roots was detected in 94% (all except one) of the PFM. This percentage of PFM showing EMG abnormalities was higher than that in the EMG study of Caro et al.2 However, the authors had not examined the S2 and S3-S4 myotomes.
Caro et al2 studied two insertions in the lumbar myotomes: the tibialis anterior and quadriceps femoris muscle, and detected abnormal spontaneous activity in 61% of 28 patients. This percentage is much higher than in our EMG study of the leg muscles. We found abnormal spontaneous activity in only 1 (6%) patient in the L5 myotomes and in 3 (17%) patients in the S1 myotomes (total of 23%). The explanation is possibly that our study group was 11–13 years younger on average. Our oldest patient was 67 years old, whereas in the study by Caro et al,2 the eldest patients were 84 and 90 years old. In fact, the only patient with abnormal spontaneous activity in the L5-innervated muscle in our study was 67 years old. During aging, FM pain involves an increasing number of body areas,32 probably because neurogenic abnormalities emerge after years of nerve irritation.
According to our hypothesis, our higher percentage of EDX abnormalities in the S2 myotomes compared to the lumbar myotomes may be explained by the rostro-caudal gradient of increased hydrostatic pressure in the dural sac, causing higher pressure inside the sacral nerve root sheaths.
In our study, EMG abnormalities during muscle contraction were more pronounced in the sacral than in the lumbar nerve root myotomes. However, neurogenic abnormalities in L5 myotomes were more prevalent than in S1 myotomes. One explanation may be that the gastrocnemius muscle is a large muscle. Therefore, more denervated nerve fibers are needed to detect abnormalities with the EMG needle. Another explanation based on our hypothesis may be the anatomical position of the DRG in the lateral recessus and the neural foramen. The L5 DRG has an intraforaminal location in 76% of individuals, and the S1 DRG has an intraforaminal location only in 4–14% of individuals.33 Thus, the lateral recessus of the L5 DRG is narrower compared to the wider space available for the S1 DRG. According to our hypothesis, when hydrostatic pressure forces CSF into the S1 nerve root sheath and the DRG, this sheath has the capability to distend more easily, as it is not hindered by the bony foramen. Consequently, the pressure inside the S1 DRG may not rise as high as the pressure in the L5 DRG, resulting in less irritation or compression of S1 nerve root fibers and neurons.
Further supporting the hypothesis of increased cerebrospinal pressure in PFM is that several authors have reported on radicular pain in idiopathic intracranial hypertension patients.34–37 Moreover, nerve roots can be markedly dilated, as has been observed in a patient with intracranial hypertension during CT myelography as well as during surgery.34 In a study of 101 patients with idiopathic intracranial hypertension, pain, paresthesia, and lower back pain resolved immediately following lumbar puncture with spinal fluid evacuation.38 In a study in PFM, spinal fluid evacuation immediately relieved radicular pain for a few hours to a few weeks in 70% of the patients.39
Additionally, several authors have reported radiculopathy and delayed F-waves in the median, fibular and tibial nerves in patients with intracranial hypertension.37 F-waves are responses produced by motor neurons activated by antidromic peripheral nerve stimulation and are particularly convenient for the diagnosis of polyneuropathies at a very early stage and for the diagnosis of proximal nerve lesions (near the DRG).40 Caro et al2 detected abnormal F-waves in 21% of PFM. Unfortunately, F-waves were not assessed in our retrospective study.
According to our hypothesis, absent or delayed F-waves in PFM may indicate that increased intracranial pressure is transmitted to the dural sac and to the subarachnoid space of the peripheral nerves at the dorsal root ganglion, irritating the axons inside the nerve root sheaths.
Anal Reflex
The anal reflex is supplied by nerve roots S3 and S4. The anal reflex response was delayed in almost all (94%) of our PFM. A delayed anal reflex response compromises bowel continence.
In a study in 100 PFM and 100 controls, significantly more PFM reported fecal incontinence (45% versus 25%) and more anorectal pain (43% versus 6%) than controls.41 The EMG abnormalities found in the anal sphincter in our patients may indicate that anal pain in FM has a neuropathic component from irritated or compressed axons or sensory neurons.
Nerve roots S3 and S4 also supply the external urinary sphincter and the pelvic floor muscles. This finding of a delayed S3,S4-supplied anal reflex response may also explain why a higher percentage of PFM suffer urinary incontinence compared to age-matched women. In a study in 62 PFM and 64 controls between 19 and 65 years of age, PFM exhibited weaker pelvic floor muscle strength compared to controls. Additionally, 64% of PFM reported urinary incontinence versus 26% of controls.42
Three of our PFM showed a significantly delayed anal reflex response without significant needle EMG abnormalities in the external anal sphincter. This can only be explained by damage to the sensory (afferent) limb of the reflex arc. This is in accordance with the assumption that FM is a neuropathy affecting the small fibers and/or the sensory nerves.14,15
From these retrospective findings of prevalent anal reflex abnormalities in PFM, we propose that the anal reflex may be an additional objective diagnostic marker for the diagnosis of FM. The test is minimally invasive and is easier to interpret than needle EMG of the external anal sphincter and is capable of detecting sensory abnormalities of the S3-S4 reflex arc. Future prospective studies should link the findings of this delayed anal reflex response with symptoms of anal and urinary incontinence, neuropathic anal pain (such as stabbing pain, painful pressure and anal spasms) and clinical assessment of perianal sensitivity.
Limitations
Though the current study highlights a potentially important role of nerve conduction studies and needle EMG in the determination of diagnostic protocols in PFM, it does have limitations.
First, this was a retrospective study that was susceptible to selection bias. However, we considered all available EDX tests of patients in whom both the lumbar and sacral myotomes were assessed.
Second, the sample size was rather small, and there was no control group. However, our data were compared to reference data obtained from healthy subjects from the literature. In future prospective studies, a matched control group of healthy subjects or subjects with low back, pelvic and/or leg pain due to other conditions, such as spondylarthropathy or disc hernia, should be included.
Third, we were not able to link the EMG findings to the patients’ complaints and clinical symptoms, such as sphincter continence, anal pain, sensitivity and strength of the lumbar and sacral nerve root myotomes. Unfortunately, these clinical data were lacking. Linking these data to blinded assessed EDX results would be useful for future prospective research.
Fourth, EDX studies of the upper limbs that were executed by the same expert electrophysiologist were lacking. Evaluating the findings of upper limb EDX is essential in studying the presence of a rostro-caudal gradient.
Conclusions
This is the first time that data from EDX studies of both lumbar and sacral nerve root myotomes in PFM have been presented. In these myotomes, all PFM showed neurogenic abnormalities in a patchy distribution that were more pronounced in the sacral than in the lumbar myotomes. Most striking was the delay of the anal reflex response in all but one patient.
We propose that in addition to skin punch biopsies to assess SFNP, assessment of the anal reflex may be a useful diagnostic pathway in PFM.
Funding Statement
This research did not receive any grants from funding.
Abbreviations
CSF, Cerebrospinal Fluid; DRG, Dorsal Root Ganglion; EDX, Electrodiagnostic; EMG, Electromyography; FM, Fibromyalgia; µV, µ-Volts; MUPs, Motor Unit Potentials; ms, Milli-seconds; PFM, Patients with Fibromyalgia; SFNP, Small Fiber Neuropathy.
Ethics and Consent Statement
The submitted study was approved by the institutional review board AZ Rivierenland Bornem. Because of the retrospective nature of the study, patient consent to review their medical records was not required by the AZ Rivierenland Bornem IRB. Patient data were anonymized and were treated in compliance with the Declaration of Helsinki.
Disclosure
Ingeborg Stalmans reports professional fees to the institution from Aerie, professional fees from Alcon, Allergan, EyeTechCare, Santen, and Théa pharma outside the submitted work. The authors reports no other potential conflicts of interest in this work.
References
- 1.Watson NF, Buchwald D, Goldberg J, Noonan C, Ellenbogen RG. Neurologic signs and symptoms in fibromyalgia. Arthritis Rheum. 2009;60(9):2839–2844. doi: 10.1002/art.24772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Caro XJ, Galbraith RG, Winter EF. Evidence of peripheral large nerve involvement in fibromyalgia: a retrospective review of EMG and nerve conduction findings in 55 FM subjects. Eur J Rheumatol. 2018;5(2):104–110. doi: 10.5152/eurjrheum.2018.17109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hulens M, Dankaerts W, Stalmans I, et al. Fibromyalgia and unexplained widespread pain: the idiopathic cerebrospinal pressure dysregulation hypothesis. Med Hypotheses. 2018;110:150–154. doi: 10.1016/j.mehy.2017.12.006 [DOI] [PubMed] [Google Scholar]
- 4.Caro XJ, Winter E. Evidence of abnormal epidermal nerve fiber density (ENFD) in fibromyalgia. Arthritis Rheum. 2008;58(9):S388. doi: 10.1002/art.23794 [DOI] [PubMed] [Google Scholar]
- 5.Üçeyler N, Sommer C. Objective evidence that small-fiber polyneuropathy underlies some illnesses currently labeled as fibromyalgia. Pain. 2013;154(11):2569. doi: 10.1016/j.pain.2013.06.037 [DOI] [PubMed] [Google Scholar]
- 6.Oaklander AL, Herzog ZD, Downs HM, Klein MM. Objective evidence that small-fiber polyneuropathy underlies some illnesses currently labeled as fibromyalgia. Pain. 2013;154(11):2310–2316. doi: 10.1016/j.pain.2013.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garcia-Martin E, Garcia-Campayo J, Puebla-Guedea M, et al. Fibromyalgia is correlated with retinal nerve fiber layer thinning. PLoS One. 2016;11(9):e0161574. doi: 10.1371/journal.pone.0161574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lawson VH, Grewal J, Hackshaw KV, Mongiovi PC, Stino AM. Fibromyalgia syndrome and small fiber, early or mild sensory polyneuropathy. Muscle Nerve. 2018;58(5):625–630. doi: 10.1002/mus.26131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Serra J, Collado A, Solà R, et al. Hyperexcitable C nociceptors in fibromyalgia. Ann Neurol. 2014;75(2):196–208. doi: 10.1002/ana.24065 [DOI] [PubMed] [Google Scholar]
- 10.Doppler K, Rittner HL, Deckart M, Sommer C. Reduced dermal nerve fiber diameter in skin biopsies of patients with fibromyalgia. Pain. 2015;156(11):2319–2325. doi: 10.1097/j.pain.0000000000000285 [DOI] [PubMed] [Google Scholar]
- 11.Leinders M, Doppler K, Klein T, et al. Increased cutaneous miR-let-7d expression correlates with small nerve fiber pathology in patients with fibromyalgia syndrome. Pain. 2016;157(11):2493–2503. doi: 10.1097/j.pain.0000000000000668 [DOI] [PubMed] [Google Scholar]
- 12.Erkan KT, Kocabeyoglu S, Unal-Cevik I, Bezci F, Akinci A, Irkec M. Ocular surface alterations in the context of corneal in vivo confocal microscopic characteristics in patients with fibromyalgia. Cornea. 2018;37(2):205–210. doi: 10.1097/ICO.0000000000001447 [DOI] [PubMed] [Google Scholar]
- 13.Ramírez M, Martínez-Martínez L-A, Hernández-Quintela E, Velazco-Casapía J, Vargas A, Martínez-Lavín M. Small fiber neuropathy in women with fibromyalgia. An in vivo assessment using corneal confocal bio-microscopy. Semin Arthritis Rheum. 2015;45(2):214–219. doi: 10.1016/j.semarthrit.2015.03.003 [DOI] [PubMed] [Google Scholar]
- 14.Martínez-Lavín M. Fibromyalgia and small fiber neuropathy: the plot thickens! Clin Rheumtol. 2018;37(12):3167–3171. doi: 10.1007/s10067-018-4300-2 [DOI] [PubMed] [Google Scholar]
- 15.Hulens M, Rasschaert R, Vansant G, Stalmans I, Bruyninckx F, Dankaerts W. The link between idiopathic intracranial hypertension, fibromyalgia, and chronic fatigue syndrome: exploration of a shared pathophysiology. J Pain Res. 2018;11:3129–3140. doi: 10.2147/JPR.S186878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen S, Andary M, Buschbacher R, et al. Electrodiagnostic reference values for upper and lower limb nerve conduction studies in adult populations. Muscle Nerve. 2016;54(3):371–377. doi: 10.1002/mus.25203 [DOI] [PubMed] [Google Scholar]
- 17.Buschbacher RM. Normal range for H-reflex recording from the calf muscles. Am J Phys Med Rehabil. 1999;78(Supplement):S75–S79. doi: 10.1097/00002060-199911001-00014 [DOI] [PubMed] [Google Scholar]
- 18.Chu J, Bruyninckx F, Chan RC. Significance of motor unit action potential parameters in normal and neurogenic situations. Electromyogr Clin Neurophysiol. 1986;26(7):465–479. [PubMed] [Google Scholar]
- 19.Preston DC, Shapiro BE. Needle electromyography. Fundamentals, normal and abnormal patterns. Neurol Clin. 2002;20(2):361–396, vi. doi: 10.1016/S0733-8619(01)00005-6 [DOI] [PubMed] [Google Scholar]
- 20.Vodusek DB, Janko M, Lokar J. Direct and reflex responses in perineal muscles on electrical stimulation. J Neurol Neurosurg Psychiatry. 1983;46(1):67–71. doi: 10.1136/jnnp.46.1.67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Varma JS, Smith AN, McInnes A. Electrophysiological observations on the human pudendo-anal reflex. J Neurol Neurosurg Psychiatry. 1986;49(12):1411–1416. doi: 10.1136/jnnp.49.12.1411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ebadi H, Perkins BA, Katzberg HD, Lovblom LE, Bril V. Evaluation of proxy tests for SFSN: evidence for mixed small and large fiber dysfunction. PLoS One. 2012;7(8):e42208. doi: 10.1371/journal.pone.0042208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sghirlanzoni A, Pareyson D, Lauria G. Sensory neuron diseases. Lancet Neurol. 2005;4(6):349–361. doi: 10.1016/S1474-4422(05)70096-X [DOI] [PubMed] [Google Scholar]
- 24.Ersoz M. Nerve conduction tests in patients with fibromyalgia: comparison with normal controls. Rheumatol Int. 2003;23(4):166–170. doi: 10.1007/s00296-002-0271-2 [DOI] [PubMed] [Google Scholar]
- 25.Del Toro D, Nelson PA. Guiding treatment for foot pain. Phys Med Rehabil Clin N Am. 2018;29(4):783–792. doi: 10.1016/j.pmr.2018.06.012 [DOI] [PubMed] [Google Scholar]
- 26.Wiechers D, Guyton JD, Johnson EW. Electromyographic findings in the extensor digitorum brevis in a normal population. Arch Phys Med Rehabil. 1976;57(2):84–85. [PubMed] [Google Scholar]
- 27.Falck B, Alaranta H. Fibrillation potentials, positive sharp waves and fasciculation in the intrinsic muscles of the foot in healthy subjects. J Neurol Neurosurg Psychiatry. 1983;46(7):681–683. doi: 10.1136/jnnp.46.7.681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gatens PF, Saeed MA. Electromyographic findings in the intrinsic muscles of normal feet. Arch Phys Med Rehabil. 1982;63(7):317–318. [PubMed] [Google Scholar]
- 29.Dumitru D, Diaz CA, King JC. Prevalence of denervation in paraspinal and foot intrinsic musculature. Am J Phys Med Rehabil. 2001;80(7):482–490. doi: 10.1097/00002060-200107000-00002 [DOI] [PubMed] [Google Scholar]
- 30.Del Toro DR, Park TA. Needle EMG Examination of the Foot. Handouts for Workshop of the American Association of Neuromuscular & Electrodiagnostic Medicine. Vols. September, 2008 Rochester, MN: AANEM; 2000. [Google Scholar]
- 31.Desai J, Swash M. Fasciculations: what do we know of their significance? J Neurol Sci. 1997;152(Suppl 1):S43–S48. doi: 10.1016/S0022-510X(97)00243-8 [DOI] [PubMed] [Google Scholar]
- 32.Jacobson SA, Simpson RG, Lubahn C, et al. Characterization of fibromyalgia symptoms in patients 55–95 years old: a longitudinal study showing symptom persistence with suboptimal treatment. Aging Clin Exp Res. 2015;27(1):75–82. doi: 10.1007/s40520-014-0238-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moon HS, Kim YD, Song BH, Cha YD, Song JH, Lee MH. Position of dorsal root ganglia in the lumbosacral region in patients with radiculopathy. Korean J Anesthesiol. 2010;59(6):398–402. doi: 10.4097/kjae.2010.59.6.398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bortoluzzi M, Di Lauro L, Marini G. Benign intracranial hypertension with spinal and radicular pain. Case report. J Neurosurg. 1982;57(6):833–836. doi: 10.3171/jns.1982.57.6.0833 [DOI] [PubMed] [Google Scholar]
- 35.Groves MD, McCutcheon IE, Ginsberg LE, Kyritsis AP. Radicular pain can be a symptom of elevated intracranial pressure. Neurology. 1999;52(5):1093–1095. doi: 10.1212/WNL.52.5.1093 [DOI] [PubMed] [Google Scholar]
- 36.Moosa A, Joy MA, Kumar A. Extensive radiculopathy: another false localising sign in intracranial hypertension. J Neurol Neurosurg Psychiatry. 2004;75(7):1080–1081. [PMC free article] [PubMed] [Google Scholar]
- 37.Kincaid O, Rowin J. Intracranial hypertension causing polyradiculopathy and late or absent F-waves. J Neurol Neurosurg Psychiatry. 2006;77(12):1384–1386. doi: 10.1136/jnnp.2006.092387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Round R, Keane JR. The minor symptoms of increased intracranial pressure: 101 patients with benign intracranial hypertension. Neurology. 1988;38(9):1461–1464. doi: 10.1212/WNL.38.9.1461 [DOI] [PubMed] [Google Scholar]
- 39.Hulens M, Rasschaert R, Dankaerts W, Stalmans I, Vansant G, Bruyninckx F. Spinal fluid evacuation may provide temporary relief for patients with unexplained widespread pain and fibromyalgia. Med Hypotheses. 2018;118:55–58. doi: 10.1016/j.mehy.2018.06.017 [DOI] [PubMed] [Google Scholar]
- 40.Mesrati F, Vecchierini MF. F-waves: neurophysiology and clinical value. Neurophysiol Clin. 2004;34(5):217–243. doi: 10.1016/j.neucli.2004.09.005 [DOI] [PubMed] [Google Scholar]
- 41.Almansa C, Rey E, Sanchez RG, Sanchez AA, Diaz-Rubio M. Prevalence of functional gastrointestinal disorders in patients with fibromyalgia and the role of psychologic distress. Clin Gastroenterol Hepatol. 2009;7(4):438–445. doi: 10.1016/j.cgh.2008.12.005 [DOI] [PubMed] [Google Scholar]
- 42.Fusco HCSC, Filho MAGP, Haddad JM, Zanetti MRD, Marques AP, Ferreira EAG. Lower urinary tract symptoms and perineal function in women with and without fibromyalgia: a cross-sectional study. Clin Rheumtol. 2019;38(10):2885–2890. doi: 10.1007/s10067-019-04617-y [DOI] [PubMed] [Google Scholar]