Abstract
AIM
To investigate the prevalence and risk factors of age-related cataract (ARC), ARC surgery procedures, and postoperative vision results among adults over 50 years old in the Binhu District of Wuxi City, China.
METHODS
Thirty basic sampling units were analyzed via a cluster random sampling method. Detailed medical histories were collected and eye examinations were performed. Cataract prevalence and surgical procedures were quantified.
RESULTS
Among the 6150 participants, 1421 cataract cases were diagnosed and prevalence was 23.1%. The prevalence of cortical, nuclear, and posterior subcapsular cataracts increased with age (P<0.001). Cataract prevalence was significantly higher among elderly, female, or illiterate individuals and people with hypertension, diabetes, and a history of smoking and drinking (all P<0.05). As participant age increased and education level decreased, the frequency of cataract blindness surgeries gradually decreased, but without statistical significance within groups (P>0.05). The odds ratio of cataract patients who had or did not have cataract surgery was 3.15 (87/28) and the frequency of cataract blindness surgery was 75.7% (87/115). Poor visual outcomes was in 107 eyes (40.7%) after cataract surgery. Poor vision was mostly caused by uncorrected reflective errors (30.9%) and ocular comorbidities (41.1%). The prevalence of cataract surgery complications was 5.7% (15/263). Surgical complications and posterior capsular opacification were avoidable factors facilitating poor vision.
CONCLUSION
ARC, especially in females and illiterate individuals, presents a public health problem in this district. Poor visual outcomes after cataract surgery are frequent. High-quality cataract surgeries and treatment of ocular comorbidities are vital.
Keywords: age-related cataract, cataract surgery, prevalence, blindness
INTRODUCTION
Epidemiological investigations show that the main disease causing blindness in China was age-related cataract (ARC)[1]. In our previous report, cataracts were still the main cause of visual impairments in the Binhu District of Wuxi City, China[2]. With an aging population[3], the prevalence of cataract patients in China increases yearly and the social burden caused by cataracts is an inevitable problem[4]. Recently, surveys have been conducted around the country on the prevalence of cataracts; the results show that the prevalence varies significantly with different regions and ethnic groups[5]–[7]. Therefore, it is important to explore potential ARC risk factors in the area to determine possible approaches for cataract prevention.
The Jiangsu Province is an economically developed region in China; the Binhu District of Wuxi City in the southern region of Jiangsu and is part of the economic triangle of Suzhou, Wuxi, and Changzhou City[8]. Regardless of the rapid growth of China's population and economy, there have been no large-scale epidemiological investigations of eye diseases in this region, and relevant information on cataract diseases is lacking. In this study, cataract prevalence, the number of cataract surgeries, and potential risk factors in the Binhu District of Wuxi City were systematically studied, providing a scientific basis for further blindness prevention and treatment strategies.
SUBJECTS AND METHODS
Ethical Approval
The survey followed the Helsinki Declaration and the Medical Ethics Committee of the Wuxi 9th Affiliated Hospital of Soochow University (No. KT2019007). All participants signed an informed written consent.
Participants
The Binhu District consists of 10 streets and townships with a population of 46 000, accounting for 1/10 of Wuxi City[2]. The people we surveyed were aged 50y and older. According to the household registration, people who temporarily left the district, were sick at home, or hospitalized were still considered for the study. The total population of the 30 basic sampling units was 28 450 and the population of people over 50 years old was 6725 (23.6%). The survey was conducted from February 2017 to August 2018 and included entry and clinical eye exam information.
According to the 1985 Eye Disease Survey in Shunyi County, Beijing[9], the rate of bilateral blindness in people aged 50y and over was 2.65%. Based on the prevalence of bilateral blindness within a ±25% error range, the sample size was calculated by simple random sampling and with a 95% confidence interval (CI). It was estimated that the response rate in the investigation might reach at least 90%; thus, the final calculation required a minimum of 5018 samples. According to the 2006 China Nine Province Eye Disease Survey Project[10], we applied a random number table to the basic sampling units and used a simple random sampling method to extract 30 survey points. The 50-year-old and above population at these survey points met the needs of the calculated sample size.
Clinical Examinations
The inspection process is fully described in our previous report[2]. Briefly, the investigator gave the participant a general physical examination, a comprehensive eye exam, and a questionnaire. Clinical ophthalmologic examinations were performed by 7 ophthalmologists, including 2 senior ophthalmologists, as project leaders. All examination data were entered into the epidemiological questionnaire.
The examination includes general information such as the person's name, sex, age, occupation, education level (illiteracy refers to the level of education below primary school); history of previous eye diseases and treatment, including a history of cataracts and other diseases; previous chronic diseases of the whole body (hypertension, diabetes); and a history of bad habits (smoking, drinking, etc.). The light box of the E-word standard early diabetic retinopathy treatment study (ETDRS) vision table (Precision Vision No. 2305) was used to assess the participant's presenting visual acuity (PVA), the same way as Zhao et al[11] used in an epidemiological investigation survey. If a person infrequently wore long-term corrective glasses, the naked-eye vision was examined. If the PVA was not more than 20/40, the refractive status was assessed with an automatic refractometer (RM-8000, Topcon, Japan) and best corrected visual acuity (BCVA) was checked. Next, ophthalmologists used a slit lamp microscope (YZF1, Suzhou Visual, China) to examine characteristics such as the conjunctiva, cornea, anterior chamber depth, iris, pupil for light reflection, and lens; they used a YZ6F direct ophthalmoscope (YZ6F, Suzhou visual, China) to perform a fundus examination of a natural pupil. If fundus examination was affected by media opacity, the examination was performed after the pupil was dilated with compound topiramine eye drops (Shengtian Pharmaceutical Co. Ltd., Japan). Participants with glaucoma or shallow anterior chambers were examined only under small pupil condition.
Grading of Cataract and Lens Opacities
The cataract diagnostic criteria are based on the Lens Opacities Classification System III (LOCS III)[12]. Cortical lens opacity was classified as grade 5 (C1-C5); nuclear lens opacity was classified as grade 6 (NO1NC1-NO6NC6). Posterior capsule opacity was classified as grade 5 (P1-P5). In our study, we defined cortical, nuclear, and posterior subcapsular cataract lens opacity as a LOCS III value ≥2 in at least 1 eye.
There were 3 types of combined cataracts in the absence of the lens after cataract extraction and intraocular lens implantation. We defined ‘any cataract’ to meet the above criteria. When 1 cataract is of different types (cortical, nuclear, or posterior subcapsular) in the same eye, that eye could be divided into different cataract types at the same time. If 1 or both eyes were diagnosed as having a cataract, the person counted as 1 cataract patient. We excluded patients with congenital or traumatic cataracts. Besides, cataract patients who had a combination of high myopia, a natural lens, and long-term use of steroid were also excluded. However, among the cases of low vision after cataract surgery, high myopia fundus degeneration was not excluded as a possible cause.
For this study, the criteria for cataract surgery statistics were defined as opacity of the lens, BCVA≤20/63. The criteria for blindness and low vision were based on the blind criteria established by the World Health Organization (WHO) in 1973. Those with a BCVA<20/400 were defined as blindness; those with a visual acuity ≥20/400 but <20/63 were defined as having low vision.
Prevalence of Cataract Blindness Surgery
The ratio of cataract blindness (CB) patients who had undergone cataract surgery to cataract patients who were eligible for cataract surgery in the whole population was calculated. The number of cataract patients who were eligible for cataract surgery included CB patients who had undergone cataract surgery and CB patients who had not undergone cataract surgery but would qualify. During the investigation, due to a lack of relevant information such as the preoperative vision of cataract patients who had undergone cataract surgery, the patients who had undergone cataract surgery are assumed to have CB based on previous experience[13].
Data Analysis
We performed the analysis using SPSS 17.0 version (IBM, NY, USA). The χ2 test was used to compare the impact of age, sex, education level, and medical history including hypertension, diabetes, smoking, and drinking as well as other categorical data on cataract prevalence in the population. P<0.05 was considered statistically significant.
RESULTS
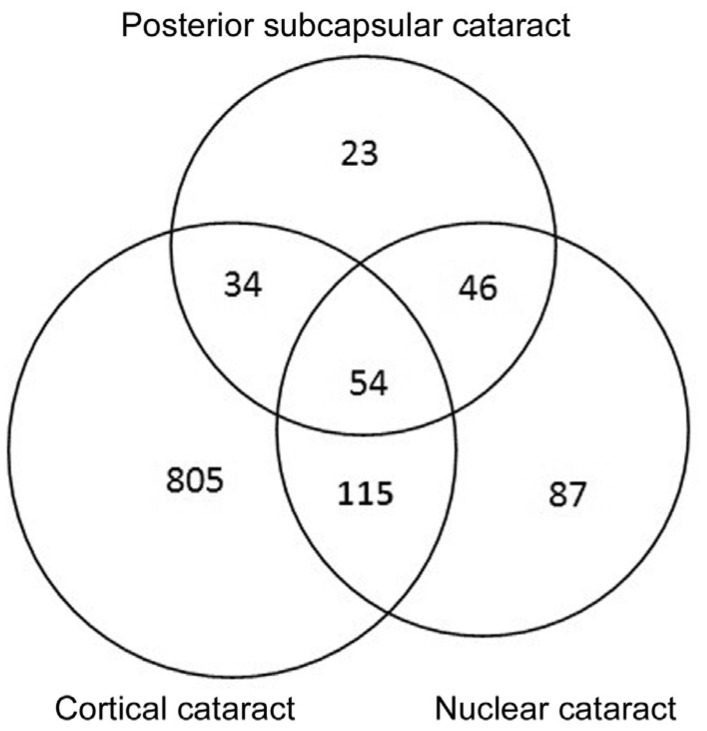
Among the 6725 eligible people, 6150 (response rate, 91.44%) completed a detailed ophthalmic examination, which was the same as our previous study[2]. The average age of participants and non-participants were 60.8±10.1 and 59.41±9.9y, respectively (P<0.001, unpaired t-test), with a higher number of women in our study than men (male-to-female ratio, 2826:3324 vs 304:271; P<0.001, χ2 test). The prevalence rate of ‘any cataract’ was 23.1% (95%CI 22.1%-24.2%) among elderly persons over 50 years old. The prevalence rates of cortical, nuclear, and posterior subcapsular cataracts were 16.4% (95%CI 15.5%-17.3%), 4.9% (95%CI 4.4%-5.5%) and 1.8% (95%CI 1.5%-2.2%), respectively (Table 1). Regarding the relationships among the 1421 cases of cortical, nuclear, and posterior subcapsular cataracts, cortical cataracts were the most common (1008/1421, 70.9%) and simple cortical cataract prevalence was 56.7% (805/1421); notably, cortical and nuclear cataracts were the most common (54+115)/1421, 11.9%) in combined cataract cases (Figure 1).
Table 1. Sex- and age-specific prevalence of each age-related cataract type.
| Age group (y) | Participants | Any cataract type |
Cortical |
Nuclear |
Posterior subcapsular |
||||
| n | % (95%CI) | n | % (95%CI) | n | % (95%CI) | n | % (95%CI) | ||
| Female | |||||||||
| 50-59 | 1098 | 134 | 12.2 (10.3-14.3) | 47 | 4.3 (3.2-5.7) | 28 | 2.6 (1.7-3.7) | 6 | 0.5 (0.2-1.2) |
| 60-69 | 1385 | 312 | 22.5 (20.4-24.8) | 225 | 16.2 (14.3-18.3) | 65 | 4.7 (3.6-5.9) | 13 | 0.9 (0.5-1.6) |
| 70-79 | 621 | 276 | 44.4 (40.5-48.5) | 226 | 36.4 (32.6-40.3) | 45 | 7.2 (5.3-9.6) | 18 | 2.9 (1.7-4.5) |
| ≥80 | 220 | 122 | 55.5 (48.6-62.1) | 111 | 50.5 (43.7-57.2) | 35 | 15.9 (11.3-21.4) | 25 | 11.4 (7.5-16.3) |
| Total | 3324 | 844 | 25.4 (23.9-26.9) | 609 | 18.3 (17.0-19.7) | 173 | 5.2 (4.5-6.0) | 62 | 1.9 (1.4-2.4) |
| Male | |||||||||
| 50-59 | 1089 | 142 | 13.0 (11.1-15.2) | 56 | 5.1 (3.9-6.6) | 18 | 1.7 (0.1-2.6) | 5 | 0.5 (0.1-1.1) |
| 60-69 | 1216 | 238 | 19.6 (17.4-21.9) | 159 | 13.1 (11.2-15.1) | 53 | 4.3 (3.3-5.7) | 9 | 0.7 (0.3-1.4) |
| 70-79 | 414 | 141 | 34.1 (29.5-38.8) | 131 | 31.6 (27.2-36.4) | 43 | 10.4 (7.6-13.7) | 15 | 3.7 (2.0-5.9) |
| ≥80 | 107 | 56 | 52.3 (42.5-62.1) | 53 | 49.5 (39.7-59.4) | 15 | 14.0 (8.1-22.1) | 20 | 18.7 (11.8-27.4) |
| Total | 2826 | 577 | 20.4 (18.9-21.9) | 399 | 14.1 (12.9-15.5) | 129 | 4.6 (3.8-5.4) | 49 | 1.7 (1.3-2.3) |
| All | |||||||||
| 50-59 | 2187 | 276 | 12.6 (11.3-14.1) | 103 | 4.7 (3.9-5.7) | 46 | 2.1 (1.5-2.8) | 15 | 0.6 (0.4-1.1) |
| 60-69 | 2601 | 550 | 21.1 (19.6-22.8 ) | 384 | 14.8 (13.4-16.2) | 118 | 4.5 (3.8-5.4) | 22 | 0.8 (0.5-1.3) |
| 70-79 | 1035 | 417 | 40.3 (37.3-43.4) | 357 | 34.5 (31.6-37.5) | 88 | 8.5 (6.9-10.4) | 40 | 3.9 (2.8-5.2) |
| ≥80 | 327 | 178 | 54.4 (48.9-59.9) | 164 | 50.2 (44.6-55.7) | 50 | 15.2 (11.6-19.7) | 34 | 10.4 (7.3-14.2) |
| Total | 6150 | 1421 | 23.1 (22.1-24.2) | 1008 | 16.4 (15.5-17.3) | 302 | 4.9 (4.4-5.5) | 111 | 1.8 (1.5-2.2) |
CI: Confidence interval.
Figure 1. A Venn diagram of 1421 patients with cortical, nuclear and posterior subcapsular cataracts.
The prevalence of ‘any cataract’ in females was 25.4% (95%CI 23.9%-26.9%), which was higher than that in males 20.4%, [95%CI 18.9%-21.9%, odds ratio (OR)=1.326, P<0.001]. The prevalence of cortical cataracts in females was 18.3% (95%CI 17.0%-19.7%), which is 14.1% in males (95%CI 12.9%-15.5%, OR=1.671, P<0.001). Also, the incidence of cortical, nuclear and post-posterior subcapsular ARC increased with age (Figure 2; P<0.001).
Figure 2. The prevalence of all cataract types as well as cortical, nuclear, and post-posterior subcapsular cataracts in different age groups gradually increased with age.
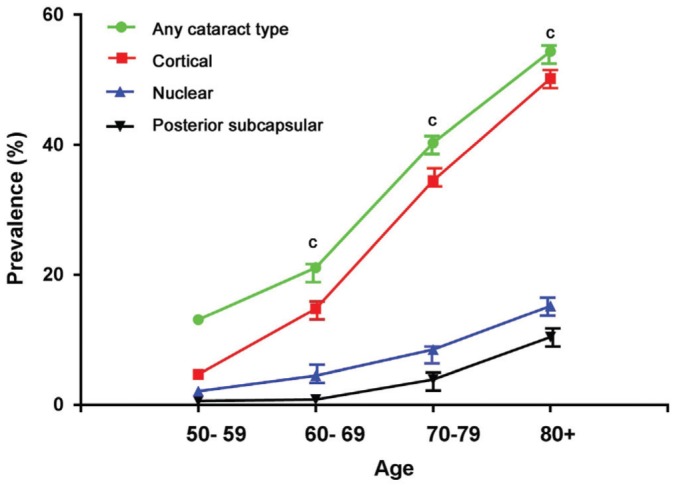
There was a significant difference between the 2 age groups of each type (cP<0.001).
The data in Table 2 shows that a person's age (χ2=493.6, P<0.001), sex (χ2=67.0, P<0.001), and education level (χ2=308.1, P<0.001), as well as a history of hypertension (χ2=140.1, P<0.001), diabetes (χ2=71.2, P<0.001), smoking (χ2=6.68, P<0.05) and drinking (χ2=7.84, P<0.05) were related to statistically significant differences in ‘any cataract’ prevalence. Additionally, for different subtypes of cataract, we found that increased age, education level, hypertension, and diabetes were potential risk factors for cortical, nuclear, and posterior subcapsular cataracts, whereas sex (female), smoking, and alcohol drinking increased only the risk of cortical cataracts.
Table 2. Baseline characteristics of each potential risk factor in the study.
| Baseline characteristics | Participants | Any cataract | Cortical | Nuclear | Posterior subcapsular |
| Age (y) | |||||
| 50-59 | 2187 | 276 (13.1) | 103 (4.7) | 46 (2.1) | 15 (0.6) |
| 60-69 | 2601 | 550 (21.1) | 384 (14.8) | 118 (4.5) | 22 (0.8) |
| 70-79 | 1035 | 417 (40.3) | 357 (34.5) | 88 (8.5) | 40 (3.9) |
| ≥80 | 327 | 178 (54.4)c | 164 (50.2)c | 50 (15.2)c | 34 (10.4)c |
| Gender | |||||
| Male | 2826 | 577 (20.4) | 399 (14.1) | 129 (4.6) | 49 (1.7) |
| Female | 3324 | 844 (25.4)c | 609 (18.3)c | 173 (5.2) | 62 (1.9) |
| Education | |||||
| Illiteracy | 552 | 282 (51.1) | 123 (22.3) | 50 (9.1) | 25 (4.5) |
| Elementary school | 1824 | 465 (25.5) | 469 (25.7) | 156 (8.6) | 55 (3.0) |
| Middle school | 2369 | 432 (18.2) | 333 (14.1) | 65 (2.7) | 20 (0.8) |
| ≥High school | 1405 | 242 (17.2)c | 83 (5.9)c | 31 (2.2)c | 11 (0.7)c |
| Hypertension | |||||
| Yes | 2435 | 754 (31.0) | 553 (22.7) | 156 (6.4) | 48 (2.0) |
| No | 3715 | 667 (18.0)c | 455 (12.2)c | 146 (3.9)c | 63 (1.7)a |
| Diabetes | |||||
| Yes | 568 | 212 (37.3) | 256 (25.4) | 43 (7.6) | 39 (6.9) |
| No | 5582 | 1209 (21.7)c | 752 (13.5)c | 259 (4.6)b | 72 (1.3)c |
| Smoking | |||||
| Never | 4355 | 1019 (23.4) | 682 (15.7) | 214 (4.9) | 75 (1.7) |
| Current | 885 | 220 (24.8) | 173 (19.5) | 42 (4.7) | 19 (2.1) |
| Former | 910 | 182 (20.0)a | 153 (16.8)a | 46 (5.1) | 17 (1.9) |
| Alcohol drinking | |||||
| Never | 5378 | 1212 (22.5) | 856 (15.9) | 258 (4.8) | 96 (1.8) |
| Current | 564 | 152 (26.9) | 115 (20.4) | 33 (5.8) | 11 (2.0) |
| Former | 208 | 57 (27.4)a | 37 (17.8)a | 11 (5.3) | 4 (1.9) |
aP<0.05, bP<0.01, cP<0.001.
n (%)
The OR in Table 3 was defined as the ratio of CB patients who had undergone surgery to CB patients who had not undergone surgery. The OR of CB surgery in the study was 3.1 (87/28), and the total surgery frequency among CB patients was 75.7% (87/115). The frequency of CB surgery in participants who were over 70 years old, male, and illiterate was relatively low. The OR comparing CB patients under 70 years of age to those over 70 was high but without a statistically significant difference (χ2=3.81, P>0.05). Compared with females, the OR of male CB patients having surgery and those without surgery was low, but again without a statistically significant difference (χ2=0.86, P>0.05). Compared with non-illiterate people, there was no significant difference in the OR of CB patients who received surgery to illiterate CB patients who did not receive surgery (χ2=0.49, P>0.05; Table 3).
Table 3. The prevalence of surgery for cataract blindness.
| Baseline characteristics | Participants | Cataract surgeries (n) |
CB in participants (n) | CB surgery |
||
| Cataract | CB | Frequency | OR | |||
| Age (y) | ||||||
| 50-59 | 2187 | 18 | 7 | 1 | 87.5 | 7.0 |
| 60-69 | 2601 | 49 | 23 | 3 | 88.5 | 7.7 |
| 70-79 | 1035 | 62 | 28 | 11 | 71.8 | 2.6 |
| ≥80 | 327 | 47 | 29 | 12 | 70.7 | 2.4 |
| Gender | ||||||
| Male | 2826 | 64 | 26 | 11 | 70.3 | 2.4 |
| Female | 3324 | 112 | 61 | 17 | 78.2 | 3.6 |
| Education | ||||||
| Illiteracy | 552 | 45 | 25 | 10 | 71.4 | 2.5 |
| Elementary school | 1824 | 46 | 21 | 11 | 63.6 | 1.9 |
| Middle school | 2369 | 42 | 22 | 5 | 81.5 | 3.7 |
| ≥High school | 1405 | 43 | 19 | 2 | 90.5 | 6.3 |
| All | 6150 | 176 | 87 | 28 | 75.7 | 3.1 |
CB: Cataract blindness; OR: Odds ratio.
Two hundred sixty-three people had undergone cataract surgery. Among the postoperative population, PVA≥20/40 accounted for 34.2% and PVA<20/63 accounted for 40.7% while BCVA≥20/40 accounted for 42.2% and BCVA<20/63 accounted for 37.7%. According to the WHO standard for low vision (<20/63), 107 eyes (40.7%) had low vision. The causes of low vision were uncorrected refractive error (30.9%), ocular comorbidities including macular degeneration (41.1%), posterior capsular opacification (PCO; 14.0%) and surgical complications (14.0%; Tables 4 and 5). High myopia fundus degeneration, optic nerve, and corneal astigmatism were the major causes of poor vision after cataract surgery. The prevalence of cataract surgery complications was 5.7% (15/263) in the study.
Table 4. Visual acuity after cataract surgery.
| VA | BCVA |
PVA |
||
| n | % (95%CI) | n | % (95%CI) | |
| ≥20/40 | 111 | 42.2 (36.2-48.4) | 90 | 34.2 (28.5-40.3) |
| 20/63-<20/40 | 79 | 30.0 (24.6-36.0) | 68 | 25.9 (20.7-31.6) |
| 20/200-<20/63 | 34 | 12.9 (9.1-17.6) | 57 | 21.7 (16.8-27.1) |
| <20/200 | 39 | 14.8 (10.8-19.7) | 50 | 19.0 (14.5-24.3) |
| Total eyes | 263 | 100 | 263 | 100 |
VA: Visual acuity; PVA: Presenting visual acuity; BCVA: Best corrected visual acuity; CI: Confidence interval.
Table 5. Causes of poor visual acuity after cataract surgery.
| Causes | Eyes | % (95% CI) |
| Ocular comorbidities | 44 | 41.1 (31.7-51.0) |
| Uncorrected refractive error | 33 | 30.9 (22.3-40.5) |
| Surgical complications | 15 | 14.0 (7.3-21.0) |
| PCO | 15 | 14.0 (7.3-21.0) |
| Total | 107 | 100 |
Poor visual acuity is defined as PVA<20/63. CI: Confidence interval; PCO: Posterior capsular opacification; PVA: Presenting visual acuity.
DISCUSSION
In this study, nuclear and cortical cataract was the most common combined ARC type. Compared with similar surveys in China, the prevalence rate was higher than that in the Shunyi District of Beijing (15.57%)[7], Qidong City of the Jiangsu Province (21.35%)[14], rural areas of the Jiangsu Province (18.3%)[15], and Doumen County of the Guangdong Province (20.93%)[16]; however, the prevalence in the Binhu District was lower than that in Shanghai City (29.86%)[17], high altitude areas of the Yunnan Province (23.84%)[18], Chifeng City of Inner Mongolia (31.39%)[19], and other areas. Compared with foreign countries, cataract prevalence in the Binhu District was higher than that in India as reported by Singh et al[20] regarding combined cataract in rural and urban areas (12.68% and 18.6%, respectively); the prevalence in the present study was also lower than the results reported by Tsai et al[21] (59.2%).
The main reasons for prevalence rate differences among regions may include variations in economic levels, altitude, latitude, race, ultraviolet radiation, and climate. Age was also an important factor that affected cataract prevalence. Different age starting points of the individuals participating in studies in different countries and regions also affected cataract prevalence. Studies conducted in Shanghai[17], India[20] and other countries involved surveying the population aged 60 years and above, and Yunnan's high-altitude area study included the population aged 40y and above[18].
Cataract prevalence varied among people of different ages, sexes, and educational levels in the present survey. Cataract formation was generally considered as an age-related disease in the past; this study also supported this view. Also, cataract prevalence in females was higher than that in males in this study, which was consistent with previous studies[21]–[23]. The higher prevalence of cataracts in females may be related to the longer life span of females than that of males. Moreover, estrogen and progesterone levels may also have some influence on cataract formation, but the specific mechanism is still unclear[24]–[25]. The prevalence rate of cataracts in the illiterate population was higher than that in the educated population. Such people generally work outdoors for long periods and may be exposed to more ultraviolet radiation, potentially increasing cataract prevalence. Naturally, further survey was needed to perform.
In this survey, a history of hypertension and diabetes, smoking, and drinking were all important factors affecting cataract prevalence. Kisic et al[26] showed that ARC formation in hypertensive patients was associated with increased exposure to biomolecular oxidative damage. The oxidative changes of biomolecules in these patients were related to the increased activity of prooxidative enzymes xanthine oxidase, myeloperoxidase, and glutathione peroxidase, as well as the activity of a lower extracellular superoxide dismutase activity and the total reducing ability of plasma. Studies on diabetes in both animals and humans demonstrate increased aldose reductase activity, which is related to cataract progression[27]. Langford-Smith et al[28] found that compared with non-smokers, aluminum and vanadium ions in smokers increased; these changes in metal ions may lead to cataract formation by inducing an oxidative stress pathway that regulates extracellular matrix structure/function and cytotoxicity. Currently, more researchers support the link between alcohol consumption and cataracts, but the specific mechanism of the effect of alcohol on cataracts is still unclear[29]–[30].
The frequency of CB surgery not only objectively reflects the effectiveness of blindness prevention and treatment, but also provides data for future goals for CB surgery. Thus, the frequency of cataract surgery in this survey can provide a reliable and sufficient basis for the prevention and treatment of blindness in the future. According to the visual acuity classification criterion provided by the WHO, the coverage rate of cataract surgery for people ≥50 years old in the Binhu District is 75.7%, lower than that of Shanghai (84.6%) under the same standard[17], but higher than that of most other regions in China[7],[14],[19]. Although there was a lack of previous clinical data on the prevention and treatment of blindness in this region, the results of this survey showed that compared with other regions in China, the prevention and treatment of blindness in this region is relatively effective. With increasing age, the prevalence of patients who had undergone CB surgery decreased, which may be due to a decreased ability to pay or a decreased chance of seeing a doctor to accept cataract surgery. Further studies are needed in this regard. There was no significant difference in surgery frequency among CB patients regarding sex and educational level.
Regarding cataract surgery outcomes in this study, 19.0% of eyes had PVA<20/200, 34.2% of eyes had PVA≥20/40, and 40.7% of eyes had PVA<20/63, which were very similar to the Taizhou Eye study[22]. However, these vision results are not satisfactory. In our study, ocular comorbidities, including macular degeneration, were very high. Ocular comorbidities deserve more clinical attention because they may affect postoperative visual results. This suggests that we should need more communication with patients and their families to assess vision before cataract surgery. Also, we also found a higher proportion of PCO and surgical complications (28%) after cataract surgery. This finding means that the doctors should strengthen quality surgical treatment and postoperative follow-up.
A strength of our study was the high survey response rate (91.44%); also, the standardized examination process was adopted to grade lens opacity using the LOCS III system. Lens opacity and fundus diseases were measured based on the WHO visual standard. However, we only conducted fundus examinations and acquired fundus photos for individuals suffering from fundus diseases. Therefore, more detailed posterior segment examination tools, such as non-mydriatic fundus camera, optical coherence tomography, were not utilized; this presents a limitation in our study. Moreover, we may have underestimated the fundus diseases due to severe lens opacity, including vitreous diseases, age-related macular degeneration, and optic atrophy.
In conclusion, the public health problems caused by cataracts cannot be ignored. In this study, different type of cataract (cortical, nuclear, subcapsular) had a higher prevalence rate with age increase and female overall. Our data suggest that elderly, female, and illiterate people should be the focus of cataract and blindness prevention in the region in the future. As an economically developed region in southern Jiangsu, the Binhu district of Wuxi City has a high population density with aging individuals. This survey shows that the frequency of cataract surgery in this district is 75.7%, which is higher than that in most parts of China, indicating the level of CB prevention effort. Uncorrected refractive error and ocular comorbidities were the leading causes in poor visual results after ARC surgery. Overall, ophthalmologists and governments still have a long way to go to find and treat cataract early and reduce the difficulty, risk, and postoperative complications associated with CB to improve people's quality of life.
Acknowledgments
Foundation: Supported by the Institutional Project Funding (No.20184712).
Conflicts of Interest: Chen X, None; Zhou DY, None; Shen J, None; Wu YB, None; Sun QZ, None; Dong JM, None; Yu JC, None.
REFERENCES
- 1.Tang Y, Wang X, Wang J, Huang W, Gao Y, Luo Y, Lu Y. Prevalence and causes of visual impairment in a Chinese adult population: The Taizhou Eye Study. Ophthalmology. 2015;122(7):1480–1488. doi: 10.1016/j.ophtha.2015.03.022. [DOI] [PubMed] [Google Scholar]
- 2.Chen X, Zhou D, Shen J, Wu YB, Sun Q, Dong J, Yu J. Prevalence and causes of visual impairment in adults in Binhu district, Wuxi, China. Med Sci Monit. 2018;24:317–323. doi: 10.12659/MSM.908218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou Q, Friedman DS, Lu H, Duan X, Liang Y, Yang X, Wang F, Wang N. The epidemiology of age-related eye diseases in Mainland China. Ophthalmic Epidemiol. 2007;14(6):399–407. doi: 10.1080/09286580701331974. [DOI] [PubMed] [Google Scholar]
- 4.Rao GN, Khanna R, Payal A. The global burden of cataract. Curr Opin Ophthalmol. 2011;22(1):4–9. doi: 10.1097/ICU.0b013e3283414fc8. [DOI] [PubMed] [Google Scholar]
- 5.Bao YZ, Cao XG, Li XX, Chen J, Hu JX, Zhu T. Screening of cataract surgery in four rural populations aged 50 years old and above in western China. Zhonghua Yi Xue Za Zhi. 2009;89(35):2454–2457. [PubMed] [Google Scholar]
- 6.Shi XY, Ke YF, Jin N, Zhang HM, Wei RH, Li XR. The prevalence of vision impairment and refractive error in 3654 first year students at Tianjin Medical University. Int J Ophthalmol. 2018;11(10):1698–1703. doi: 10.18240/ijo.2018.10.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu H, Zhao JL, Lu H, Li FR, Mao J, Ellwein LB, Jiang LJ, Zhang Y, Yang YQ, Wang Y, Gao XC, Zhang WB. Prevalence of blindness and moderate and severe visual impairment among adults aged 50 years or above in the Shunyi District of Beijing: the China Nine-Province Survey. Zhonghua Yan Ke Za Zhi. 2012;48(3):199–204. [PubMed] [Google Scholar]
- 8.Binhu tourism (Chinese) [Accessed on November 10, 2019]. http://www.wxbh.gov.cn/.
- 9.Zhao J, Jia L, Sui R, Zhang C, Xiang L, Zhang H, Sun G, Song X, Mao J. Prevalence of blindness among adults aged 50 years or above in Shunyi County of Beijing. Zhonghua Yan Ke Za Zhi. 1999;35(5):341–347. [PubMed] [Google Scholar]
- 10.Zhao JL, Wang Y, Gao XC, Ellwein LB, Liu H. Sampling and measurement methods of the protocol design of the China Nine-Province Survey for blindness, visual impairment and cataract surgery. Zhonghua Yan Ke Za Zhi. 2011;47(9):779–784. [PubMed] [Google Scholar]
- 11.Zhao J, Ellwein LB, Cui H, Ge J, Guan H, Lv J, Ma X, Yin J, Yin ZQ, Yuan Y, Liu H. Prevalence of vision impairment in older adults in rural China: the China Nine-Province Survey. Ophthalmology. 2010;117(3):409–416. 416.e1. doi: 10.1016/j.ophtha.2009.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gali HE, Sella R, Afshari NA. Cataract grading systems: a review of past and present. Curr Opin Ophthalmol. 2019;30(1):13–18. doi: 10.1097/ICU.0000000000000542. [DOI] [PubMed] [Google Scholar]
- 13.Zhao J, Sui R, Jia L. Prevalence of cataract and surgical coverage among adults aged 50 or above in Shunyi District of Beijing, China. Zhonghua Yan Ke Za Zhi. 2001;37(1):3–8. [PubMed] [Google Scholar]
- 14.Guan HJ, Lu H, Dai Z, Li M, Wang Y, Hu JY, Shi J, Zhao JL, Ellwein LB, Wang Y, Gao XC. Prevalence and surgery status of cataract among adults aged 50 years or above in Qidong City of Jiangsu Province: the China Nine-Province Survey. Zhonghua Yan Ke Za Zhi. 2012;48(3):219–225. [PubMed] [Google Scholar]
- 15.Guan HJ, Yao Y, Liang CK, Zhu RR, Liu BH, Qi YX, Fu DH, Zhang JF, Yin L, Shi J, Yang M. Prevalence and surgical status of cataract among adults aged 50 years or above in rural Jiangsu Province. Zhonghua Yi Xue Za Zhi. 2013;93(5):330–335. [PubMed] [Google Scholar]
- 16.Xu J, He M, Wu K, Li S. The prevalence of cataract in Doumen County, Guangdong Province. Zhonghua Yan Ke Za Zhi. 1999;35(6):465–467. [PubMed] [Google Scholar]
- 17.Hu JY, Yan L, Chen YD, Du XH, Li TT, Liu DA, Xu DH, Huang YM, Wu Q. Population-based survey of prevalence, causes, and risk factors for blindness and visual impairment in an aging Chinese metropolitan population. Int J Ophthalmol. 2017;10(1):140–147. doi: 10.18240/ijo.2017.01.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu JP, Zhao SZ, Li XY, Liu WJ, Wei RH, Hua N, Li Y, Wang TC, Zou YY, Zhao XY, Liang J, Ren XJ. Prevalence survey of cataract among adults aged 40 or above in a multiethnic rural district in the high altitude area of Yunnan province. Chinese Journal of Practical Ophthalmology. 2012;30(3):340–344. [Google Scholar]
- 19.Cui W, Liu ZY, Yu GB. Survey of cataract rate and surgical coverage in agricultural and pastoral area of Chifeng Keshenketeng in Inner Mongolia. Zhonghua Shiyan Yanke Zazhi. 2012;30(5):462–466. [Google Scholar]
- 20.Singh S, Pardhan S, Kulothungan V, Swaminathan G, Ravichandran JS, Ganesan S, Sharma T, Raman R. The prevalence and risk factors for cataract in rural and urban India. Indian J Ophthalmol. 2019;67(4):477–483. doi: 10.4103/ijo.IJO_1127_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tsai SY, Hsu WM, Cheng CY, Liu JH, Chou P. Epidemiologic study of age-related cataracts among an elderly Chinese population in Shih-Pai, Taiwan. Ophthalmology. 2003;110(6):1089–1095. doi: 10.1016/S0161-6420(03)00243-4. [DOI] [PubMed] [Google Scholar]
- 22.Tang Y, Wang X, Wang J, Huang W, Gao Y, Luo Y, Yang J, Lu Y. Prevalence of age-related cataract and cataract surgery in a Chinese adult population: The Taizhou Eye Study. Invest Ophthalmol Vis Sci. 2016;57(3):1193–1200. doi: 10.1167/iovs.15-18380. [DOI] [PubMed] [Google Scholar]
- 23.Xu Y, He J, Lin S, Zhang B, Zhu J, Resnikoff S, Lu LN, Zou H. General analysis of factors influencing cataract surgery practice in Shanghai residents. BMC Ophthalmol. 2018;18(1):102. doi: 10.1186/s12886-018-0767-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zetterberg M, Celojevic D. Gender and cataract——the role of estrogen. Curr Eye Res. 2015;40(2):176–190. doi: 10.3109/02713683.2014.898774. [DOI] [PubMed] [Google Scholar]
- 25.Zhang XH, Sun HM, Ji J, Zhang H, Ma WJ, Jin Z, Yuan JQ. Sex hormones and their receptors in patients with age-related cataract. J Cataract Refract Surg. 2003;29(1):71–77. doi: 10.1016/s0886-3350(02)01436-0. [DOI] [PubMed] [Google Scholar]
- 26.Kisic B, Miric D, Zoric L, Rasic JV, Grbic R, Popovic LM, Arsic AM. Xanthine oxidase activity in patients with age-related cataract associated with hypertension. Braz J Med Biol Res. 2018;51(5):e6129. doi: 10.1590/1414-431X20176129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Obrosova IG, Chung SS, Kador PF. Diabetic cataracts: mechanisms and management. Diabetes Metab Res Rev. 2010;26(3):172–180. doi: 10.1002/dmrr.1075. [DOI] [PubMed] [Google Scholar]
- 28.Langford-Smith A, Tilakaratna V, Lythgoe PR, Clark SJ, Bishop PN, Day AJ. Age and smoking related changes in metal ion levels in human lens: implications for cataract formation. PLoS One. 2016;11(1):e0147576. doi: 10.1371/journal.pone.0147576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hiratsuka Y, Ono K, Murakami A. Alcohol use and cataract. Curr Drug Abuse Rev. 2009;2(3):226–229. doi: 10.2174/1874473710902030226. [DOI] [PubMed] [Google Scholar]
- 30.Gong Y, Feng K, Yan N, Xu Y, Pan CW. Different amounts of alcohol consumption and cataract: a meta-analysis. Optom Vis Sci. 2015;92(4):471–479. doi: 10.1097/OPX.0000000000000558. [DOI] [PubMed] [Google Scholar]