Abstract
AIM
To analyze the systemic factors including stroke history related to the retinal artery occlusion (RAO).
METHODS
Patients with an exact diagnosis of RAO in the medical database of the Kailuan Corporation were identified as the case group. Five patients without RAO were added for each case from the Kailuan Study and matched for sex and age (age±2) as the control group. The Kailuan Study is a general population-based cohort study in northern China, in which a total of 101 510 individuals (81 110 men) aged 18-98y were recruited to participate in the study. And the participants were bi-annually re-examined. The database of both groups was from Kailuan study of 2010 cohort. All the information, including the demographic characteristics, lifestyle behaviors, medical comorbidities, medical history, family medical history, drug usage, anthropometric measurements, blood pressure measurement, blood sample laboratory assessment, urine tests, and other physical examinations were all collected. A retrospective nested case-control method was used for this study. Conditional multivariate logistic regression was used to analyze the risk factors with SPSS 13.0 software and SAS 9.3 software.
RESULTS
A total of 45 patients were included as the case group, and the control group included 225 patients. In the case group, 28 patients (62.2%) had a central retinal artery occlusion (CRAO), and 17 patients (37.8%) had a branch retinal artery occlusion (BRAO). A total of 18 patients (40.0%) had a stroke before the RAO (mean 4.04±3.88y before the RAO), and 31 patients (81.6%) had infarctions or malacia identified by the cranial computed tomography (CT) scans. The basal ganglia and centrum semiovale were the most frequently involved regions. Plaques in the common carotid artery were present in 32 patients (88.9%). Conditional multivariate logistic regression analysis showed that the RAO was found to be associated with the history of stroke (P=0.0023, OR=28.794; 95%CI: 3.322-249.586).
CONCLUSION
A history of stroke can significantly increase the incidence of RAO. Exists of plaque in the carotid artery is mean more than its severe stenosis for RAO.
Keywords: retinal artery occlusion, stroke, risk factor, embolic source, carotid plaque
INTRODUCTION
Retinal artery occlusion (RAO) is an emergency in ophthalmology and can cause severe damage to visual acuity (VA). The incidence of RAO is below 3.5/100 000[1], and the prognosis is grave. Furthermore, the lifetime of central retinal artery occlusion (CRAO) patients is reduced by 10y as compared with healthy controls[2]. Its diagnosis is relatively definite, according to the sudden visual deterioration history, stereoscopic colour fundus photography and fluorescence fundus angiography (FFA) examination. According to the pathogeny, researchers divided CRAO into 4 categories: non-arteritic CRAO, non-arteritic CRAO with cilioretinal artery sparing, arteritic CRAO with giant cell arteritis, branch retinal artery occlusion (BRAO) consists of BRAO and cilioretinal artery occlusion (CLRAO)[3]–[4].
The embolic source of RAO mainly from carotid arteries and aorta. And it can also be caused by running embolic material arising in the course of atrial fibrillation or dilated left ventricle, giant cell arteritis, and other autoimmune diseases or haematological disorders[5]–[6]. The reported systemic diseases associated with RAO include hypertension, hyperlipidemia, and peripheral vascular disease. Studies confirmed that RAO patients associated with an increased risk of stroke, and stroke risk in CRAO patients was 2.7-fold higher as compared with controls, especially the first week after the CRAO occurrence[7]–[9]. But whether the stroke history or asymptomatic infarction in the head can imply a risk for RAO need to be studied.
The nested case-control study method is usually used to those diseases with a low incidence or when the interest of exposure factors difficult to obtain. But this method requires the case group and the control group from the same cohort to get an efficient statistical result with low selection bias. This study aimed to investigate the systemic risk factors for RAO in a large population with the nested case-control study to identify potential subgroups at risk, especially those patients with a stroke history, and help to identify potential areas for future study.
SBUJECTS AND METHODS
Ethical Approval
The study was performed according to the guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of Kailuan General Hospital. All the participants signed a written informed consent form. And all personal information about the participants is fully protected.
Data Sources
The study was a retrospective study based on the Kailuan Medical Network, which was connected with the insurance system and the medical records of all the participants of Kailuan Study were added in real-time. The Kialuan study was a prospective cohort study conducted in the community of Kailuan in the industrial city of Tangshan, China. Between June 2006 and October 2007, a total of 101 510 individuals (81 110 men) aged 18-98y were recruited to participate in the study, and the participants were bi-annually re-examined. The Kailuan Corporation is a large coal mining company in Tangshan city, in the Hebei Province of China. The medical insurance centre has a separate division for this corporation; thus, almost all medical information of the employees and retirees can be searched for in this database. The medical insurance policy in Tangshan is set to provide reimbursements for local in-patients only. Most critical patients would be hospitalized. And we can search all the patients' diagnosis, names, sex, identity card numbers, and find the hospital for where and when the therapy be taken in this database.
All participants underwent questionnaire assessments, and clinical and laboratory examinations were conducted in the 11 hospitals responsible for the healthcare of this community in Tangshan every two years since 2006. Questionnaires were administered in person by qualified doctors, in which information was obtained including demographic and socioeconomic data, education level, average income of each family member, medical history, family medical history, alcohol consumption, smoking status, dietary data, physical activity, and sleeping duration and quality. The questionnaires, anthropometric measurements, blood pressure measurement, blood sample laboratory assessment, urine tests, and other physical examination findings were all performed by rigorously trained doctors and nurses and have been described in detail previously[10]–[12].
The “retinal artery occlusion” was searched for in the Kailuan Medical Database for the Kailuan Corporation between 2006 and 2015. And then all these patients were needed to be checked with the detailed medical records in the hospital where the patients were diagnosed with the disease. All those patients were needed to meet the inclusion criteria. And those without detailed medical records or could not meet the inclusion criteria been excluded.
Thinking about most people took the carotid ultrasonography examination in the 2010 Kailuan Study, we randomly added 5 people without RAO disease matched by age (age±2) and sex for each patient in the 2010 Kailuan Study to be the control group. And all these people had been checked without RAO by normal eye examination in the Ophthalmology Department. And all the analyses about the demographic and clinical features in the two groups were based the results in the 2010. And all these cases in the two groups were followed to 2015.
The medical records were checked and recorded all the demographic data of case group, including age, sex, lifestyle, dietary habits, complicated systemic diseases, and drug usage, were recorded. Ophthalmic evaluations included the following: VA; intraocular pressure measurement; slit-lamp examination of the anterior segment, lens, and vitreous; stereoscopic colour fundus photography; FFA; and visual field testing with an automated perimeter. The results of carotid ultrasounds, echocardiograms, cranial computed tomography (CT) scans and blood tests were recorded. Body mass index (BMI) was calculated as follows: BMI (kg/m2)=body weight (kg)/height2 (m2). The estimated glomerular filtration rate (eGFR) was calculated with the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation[13]. Other systemic or neurologic evaluations were also performed to rule out related causes of visual loss.
Inclusion Criteria for the Study
In line with the RAO diagnostic criteria, the diagnosis of RAO was based on the presence of various classical clinical findings as follows[14]: 1) There was a history of a sudden onset of visual deterioration in the eye. 2) On the initial ophthalmic evaluation, there was evidence of acute retinal ischaemia in the distribution of the occluded retinal artery. 3) FFA showed evidence of the absence or marked stasis of circulation in the involved branch of the retinal artery, except in eyes with transient RAO. All criteria had to be fulfilled for inclusion in the study.
Patients with a detailed systemic disease history and physical examination record were included.
RAO associated with temporal arterits was excluded either clinically based on the presence of symptoms and the presence of an elevated erythrocyte sedimentation rate (ESR) or protein C or based on temporal artery biopsy, where possible.
Statistical Analysis
A retrospective nested case-control analysis was used for this study. SAS 9.3 software was used to record the information and perform a conditional multivariate logistic regression analysis. Statistical analyses were performed with SPSS 13.0 software and SAS software by one researcher who was blinded to the disease status of the patients, the medications, the examination findings, and the time sequence. All the variables collected in the Kailuan Study were selected to make statistical analysis. At first, the measurement data and numerical data were statistically analyzed with the t-test or the χ2 test, respectively, to evaluate the demographic and clinical features between the two groups. The conditional multivariate logistic regression analysis was used to analyse the risk factors for RAO. A P value <0.05 was considered statistically significant.
RESULTS
Demographic and Clinical Characteristics
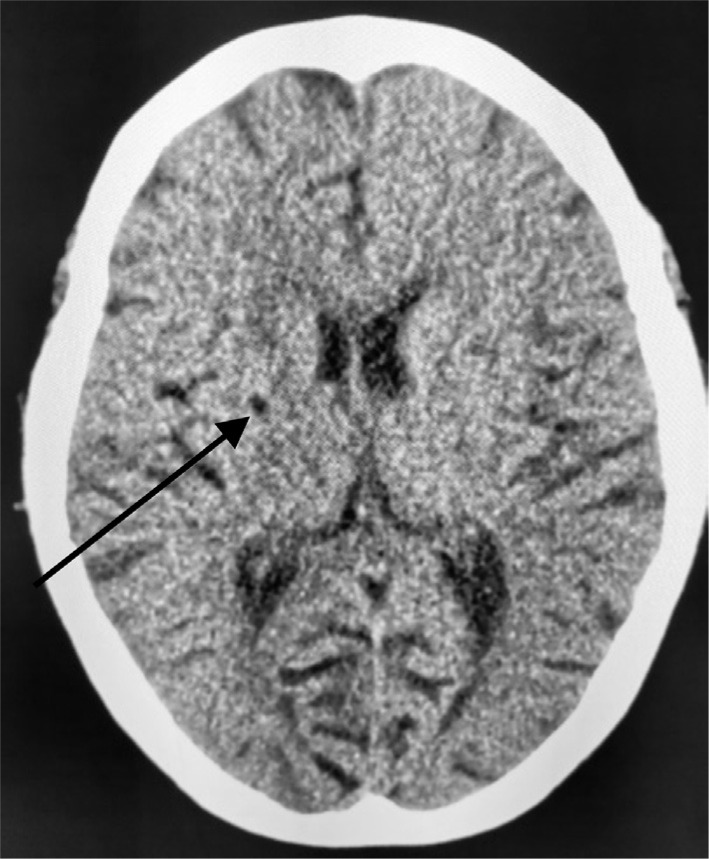
Based on the Kailuan Medical Database of the Kailuan Corporation between 2006 and 2015, 65 patients were diagnosed with RAO. According to the diagnostic inclusion criteria and after excluding patients without detailed medical records, 45 patients (45 eyes) were included in the analysis. The mean age was 59.98±10.26y. A total of 39 patients (86.7%) were male. Twenty patients were excluded because the papers recorded their medical records could not be found in the hospital. The control group had 225 patients, with a mean age of 60.01±10.14y. The follow-up time ranged from 2 to 114mo (mean 44.91±30.23mo) in the case group. And in control group, it was 60mo (from 2010 to 2015). Twenty-eight patients (62.2%) had CRAO, 17 patients (37.8%) had BRAO (Table 1), in which 2 patients had CLRAO (Figure 1). One patient with CLRAO case suffered from the onset of RAO in the morning. The length of time between the onset of the RAO attack and admission to the hospital ranged from 2h to 1mo (mean 82.51±126.77h).
Table 1. BRAO-the affected branch.
| Affected branch | Cases (%) |
| Nasalis superior | 2 (11.8) |
| Nasalis inferior | 0 |
| Temporalis superior | 3 (17.7) |
| Temporalis inferior | 10 (58.8) |
| Cilioretinal artery | 2 (11.8) |
BRAO: Branch retinal artery occlusion.
Figure 1. The fundus examination of the right eye.
CRAO with cilioretinal artery spring.
Visual Acuity
Of the 28 CRAO patients, the initial VA evaluation at admission revealed light perception VA in 9 patients (32.1%), hand motion VA in 6 patients (21.4%) and counting fingers VA in 6 patients (21.4%); 7 patients (25.0%) had a VA better than 0.01. Of the 17 BRAO patients, VA evaluation revealed counting fingers VA in 1 patient (5.9%); 6 patients (35.3%) had a VA<0.1 and 10 patients (58.9%) had a VA≥0.1. Three patients (6.7%) among all the RAO patients experienced an improvement of 2 lines in VA after undergoing eye massage, treatment to decrease the intraocular pressure, vasodilator medicine intravenous drip, or other therapies included intravenous fibrinolytic agents, oxygen inhalation, oral aspirin, and so on, to improve the microcirculation, in which one patient were treated with nitroglycerin before being seen by an ophthalmologist. The condition of two patients (4.4%) worsened.
Neovascular Glaucoma
One patient (2.2%) had complications of neovascular glaucoma 2mo after the onset CRAO because of the ocular ischaemia. The other 44 patients (97.8%) did not have complications of neovascular glaucoma during follow-up time span.
Associated Systemic Abnormalities
Comorbidity of systemic diseases
Totally 33 patients (73.3%) had a comorbidity of hyperlipidaemia. Thirty patients (66.7%) had a comorbidity of hypertension, 18 patients (40.0%) had a history of stroke, 11 patients (24.4%) had coronary disease, and 10 patients (22.2%) had diabetes mellitus. Furthermore, other than the 18 patients who had a stroke before the onset of RAO (mean 4.04±3.88y before the RAO), there were another 10 patients (22.2%) who were diagnosed with stroke based on imaging while hospitalized in the RAO ward, and 3 patients (6.7%) had a stroke at 1, 4, and 7y, respectively, after the onset of RAO. There were 3 patients (6.7%) who had cancer, 1 had lung cancer, 1 had lymphoma, and 1 had prostatic carcinoma.
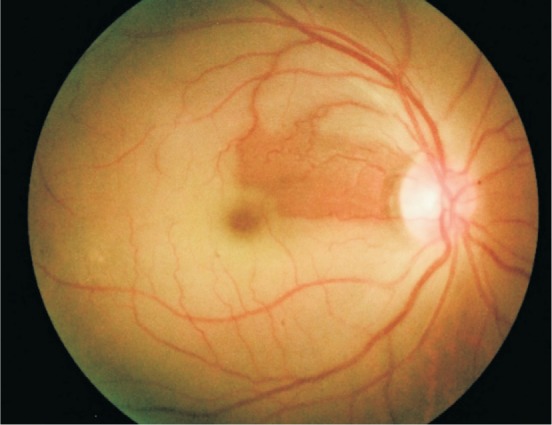
Carotid ultrasonography
There were 36 patients (80.0%) who underwent carotid artery ultrasonography examinations in the RAO group in the time when they took therapy for the RAO in the hospital, and 32 of these patients (88.9%) had plaques in the common carotid artery. Twenty-nine patients (90.6%) had bilateral involvement of the common carotid arteries. Thirty-one patients (96.9%) had plaques in the carotid artery ipsilateral to the affected eye. There were 2 patients (6.3%) who had stenosis of approximately 63% and 80%, respectively, and all the other patients (30 cases, 93.8%) had <50% stenosis. In the common carotid artery, 7 patients (21.9%) had hypoechoic plaques only, 9 patients (28.1%) had hyperechoic plaques only, and 16 patients (50.0%) had plaques with mixed echogenicity. Three patients (8.3%) had plaques in the internal carotid artery (Figure 2). The 3 internal carotid artery plaques were all hypoechoic plaques (Table 2). Forty-three cases in the RAO group took the examination in 2010 Kailuan study. Twenty-three cases (51.1%) had plaques in the carotid artery. All the people in the control group took the examination in 2010 Kailuan study. And 163 cases (72.4%) had plaques in the carotid artery.
Figure 2. Carotid artery ultrasonography.
The plaque in the left internal carotid artery (yellow arrow).
Table 2. The carotid artery ultrasonography.
| Variable | The common carotid | The internal carotid |
| Took examination | 36 (80.0) | 36 (80.0) |
| Normal | 4 (11.1) | 33 (91.7) |
| Abnormal | 32 (88.9) | 3 (8.3) |
| Bilateral | 29 (90.6) | 0 |
| Ipsilateral with the sick eye | 31 (96.9) | 2 (66.7) |
| Stenosis <50% | 30 (93.8) | 3 (100) |
| Stenosis ≥50% | 2 (6.3) | 0 |
n (%)
Echocardiography
Transthoracic echocardiography was performed in 28 patients (62.2%). Nine patients (32.1%) had abnormal findings that manifested as valvular insufficiency and valvular regurgitation. A single valve or multiple valves were involved. The mitral valve was involved in 8 patients (88.9%). The aortic valve was involved in 4 patients (44.4%). The tricuspid valve was involved in 3 patients (33.3%). Three patients had an arrhythmia, and all of them manifested as bradyarrhythmia.
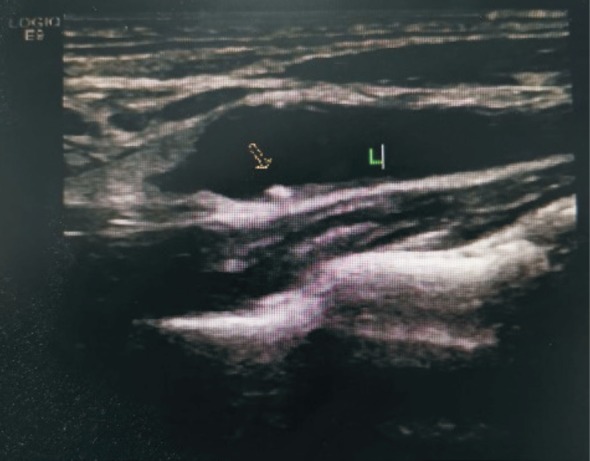
Cranial computed tomography scan
A cranial CT scan was performed in 38 patients (84.4%), in which 31 patients (81.6%) had infarctions or malacia, and the lesions were single or multiple. The basal ganglia and centrum semiovale were the most frequently involved regions (Figure 3). Twenty-two patients (71.0%) had a lesion ipsilateral to the affected eye (Table 3).
Figure 3. Cranial CT scan.
Malacia in the basal ganglia (black arrow).
Table 3. The cranial CT scan.
| Variable | Cases (%) |
| Took examination | 38 (84.4) |
| Normal | 7 (18.4) |
| Abnormal | 31 (81.6) |
| Ipsilateral with the sick eye | 22 (71.0) |
| The basal ganglia involved | 27 (87.1) |
| Semioval involved | 7 (22.6) |
| Ventriculus lateralis involved | 5 (16.1) |
Statistical Analysis of Risk Factors
The major demographic and clinical features of the two group was showed in Table 4, which included the demographic information, lifestyle, comorbidities and systemic diseases of the patients and other major basic data. In the univariable logistic regression analysis showed that smoking (P=0.007, OR=2.368, 95%CI: 1.270-4.415), stroke (P<0.001, OR=23.427, 95%CI: 12.754-43.035), and systolic pressure (P=0.001, OR=1.020, 95%CI: 1.008-1.032) had significant difference. With the conditional multivariate logistic regression analysis, RAO was found to be associated with the history of stroke (P=0.0023, OR=28.794; 95%CI: 3.322-249.586).
Table 4. The major demographic and clinical features of RAO group and control group.
| Variable | The RAO group (n=45) | The control group (n=225) | Total (n=270) | P |
| Male | 36 (80.0) | 195 (86.7) | 231 (85.6) | 0.809 |
| Age (y) | 59.98±10.26 | 60.01±10.14 | 60.01±10.14 | 0.985 |
| BMI (kg/m2) | 25.25±3.66 | 24.48±2.71 | 24.60±2.90 | 0.107 |
| HR (min) | 72.64±7.98 | 72.39±11.67 | 72.43±11.16 | 0.894 |
| SBP (mm Hg) | 141.37±19.96 | 134.18±20.89 | 135.37±20.87 | 0.035 |
| DBP (mm Hg) | 84.64±11.54 | 82.78±10.77 | 83.09±10.90 | 0.296 |
| FPG (mmol/L) | 5.85±2.92 | 5.35±1.34 | 5.44±1.71 | 0.078 |
| TG (mmol/L) | 1.48±0.93 | 1.61±1.26 | 1.59±1.21 | 0.540 |
| TC (mmol/L) | 5.13±0.90 | 4.77±0.89 | 4.83±0.90 | 0.105 |
| Carotid plaque | 23 (51.1)a | 163 (72.4) | 186 (68.9) | 0.008 |
| Smoking | 25 (55.6) | 84 (37.3) | 109 (40.4) | 0.030 |
| Drinking | 13 (28.9) | 78 (34.7) | 91 (33.7) | 0.494 |
| Stroke | 17 (37.8) | 1 (0.4) | 18 (6.7) | <0.001 |
| Myocardial infarction | 3 (6.7) | 3 (1.3) | 6 (2.2) | 0.060 |
| Cancer | 3 (6.7) | 3 (1.3) | 6 (2.2) | 0.060 |
RAO: Retinal artery occlusion; BMI: Body mass index; HR: Heart rate; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; FPG: Fasting plasma glucose; TG: Triglyceride; TC: Total cholesterol. aTwo cases were missed.
n (%)
DISCUSSION
Patients with RAO routinely describe a history of acute painless catastrophic visual loss, and the final VA of 80% of patients is less than counting fingers VA[3]. Because of the poor prognosis of RAO, many studies focus on the risk factors for RAO to provide some suggestions for prevention.
In this study, the VA prognosis was poor in the case group, and some patients even worsened. The length of time between when the patients recognized their VA loss and when they sought therapy ranged from 2h to 1mo (mean 82.51±126.77h), which suggests that the knowledge of this emergency in the general population is very poor.
Systemic Risk Factors
Systemic diseases, such as hypertension, diabetic mellitus, and hyperlipidemia, are widely believed to be associated with RAO[15]–[18]. In addition, atrial fibrillation, coronary heart disease, coronary artery bypass graft surgery, facial plastic surgery, Susac's syndrome, systemic lupus erythaematosus, patent foramen ovale and lymphocytic leukaemia have also been reported to cause CRAO[19]–[27]. And these conditions predispose to stroke. In this study, hyperlipidemia (33 cases, 73.3%) was the most common comorbidity, followed by hypertension (30 cases, 66.7%), which were similar to the Callizo et al[9]. The presence of these systemic diseases may cause multi-systemic dysfunction, microcirculation disorders, and changes in blood rheology, all of which may indirectly increase the risk to suffer RAO.
The two vascular systems that form the cerebral artery include the following: the internal carotid arterial system and the vertebral-basilar arterial system. The main branches of the internal carotid arterial system in the brain are the ophthalmic artery, the anterior cerebral artery, the middle cerebral artery, the anterior choroidal artery, and the posterior communicating artery. The ophthalmic artery is a branch of the cerebral artery that arises from the internal carotid artery. RAO may share similar risk factors with cerebrovascular diseases because of their shared vascular origins[28]. The risk factors including the hypertension, diabetes mellitus, body-mass index, smoking, alcoholism, and so on, were related with the ischemic stroke[29]–[30]. The relationship between cholesterol and ischemic stroke is controversial. But still, researchers consider the hypercholesterolemia should not be neglected in the prevention of ischemic stroke[31].
In this study, the incidence of the stroke in both the case group and the control group were higher than the average Chinese people[32]. For one thing, the Tangshan city is a costal city, which means the people lived there take much seafood. And another, the Kailuan general corporation is a coal mining company, in which most employees are male. Therefore, the diet habit and lifestyle may be a factor for its high incidence in this whole group. But there is no study focused on the stroke incidence of these people worked in the coal mining company.
In this study, 18 patients (40.0%) had a stroke before RAO (mean 4.04±3.88y before the RAO). In addition, 10 patients (22.2%) diagnosed with stroke based on imaging while hospitalized in the RAO ward by the cranial CT scan, which suggests that many people have unnoticed cerebral lesions before the onset of RAO. Twenty-two patients (71.0%) had lesions ipsilateral to the affected eye. The conditional multivariate logistic regression showed that a history of stroke indicates a significantly higher risk of RAO (P=0.0023, OR=28.794; 95%CI: 3.322-249.586). Previous studies have shown that RAO patients were more susceptible to stroke in the first year after the onset of RAO, particularly after the first week[7],[33]–[34]. Unlike in a prior study[7], 3 patients (6.7%) had a stroke at 1, 4 and 7y, respectively, after the onset of RAO in this study. Therefore, stroke patients should pay close attention to their visual condition, and RAO patients should also be evaluated for cerebral lesions.
Embolic Source
The carotid arteries and the heart are the main embolic sources[14]. In this study, 9 patients (32.1%) had abnormal echocardiography, which manifested as valvular insufficiency and valvular regurgitation. There were 36 patients (80.0%) who underwent carotid artery ultrasonography examinations in the RAO group. Thirty-two patients (88.9%) had plaques in the common carotid artery, and 29 patients (90.6%) had bilateral involvement of the common carotid arteries. In addition, plaques with mixed echogenicity were the most frequent type of plaque, which may be indicative of the instability of these plaques and their tendency to move to other organs. Most patients had carotid artery stenosis of <50%, which was different from the findings of Rudkin et al[35], who reported that 27% of RAO patients had moderate or significant carotid artery stenosis (>50%). A total of 31 patients (96.9%) had plaques ipsilateral to the affected sick eye, suggesting that ipsilateral plaques in the common carotid artery were the main embolic source. The presence of a plaque in the common carotid artery may be more indicative than carotid artery stenosis of subsequent retinal embolism; this finding is in contrast to the findings of Babikian et al[36], who considered that severe extra-cranial stenosis of the internal carotid artery was the most common condition associated with retinal ischaemia and embolism. In this study, the incidence of the carotid plaque in the control group was higher than the case group. It was the statistical result. But the exact reason had not been found out.
We were able to collect relatively complete medical information because of the Tangshan local medical insurance policy. And this study was made in those people lived in a large environment, which may help find the natural condition for the RAO. A history of stroke can significantly increase the incidence of RAO. Exists of plaque in the carotid artery is mean more than its severe stenosis for the RAO. The Plaques in the common carotid artery, especially with the mixed echogenicity plaque, were the most common source of the emboli, suggesting that patients with carotid artery plaques should pay close attention to their visual condition after a stroke in order to achieve an earlier diagnosis and better prognosis of RAO. The main limitation in our study was the small sample size. The results need to be validated in larger cohorts.
Acknowledgments
Foundations: Supported by National Natural Science Foundation of China (No.81570891; No.81272981); the Beijing Municipal Administration of Hospitals' Ascent Plan (No.DFL20150201); Beijing Natural Science Foundation (No.7151003); Advanced Health Care Professionals Development Project of Beijing Municipal Health Bureau (No.2014-2-003); Study on Individual Diagnosis and Therapy Strategy for Malignant Uveal Melanoma (No.2016-1-2051); Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support (No.ZYLX201307); Science & Technology Project of Beijing Municipal Science & Technology Commission (No.Z151100001615052).
Conflicts of Interest: Xiao YY, None; Wei WB, None; Wang YX, None; Lu AD, None; Chen SH, None; Song L, None; Wu SL, None.
REFERENCES
- 1.Ivanisević M, Karelović D. The incidence of central retinal artery occlusion in the district of Split, Croatia. Ophthalmologica. 2001;215(3):245–246. doi: 10.1159/000050868. [DOI] [PubMed] [Google Scholar]
- 2.Lorentzen SE. Occlusion of the central retinal artery. A follow-up. Acta Ophthalmol (Copenh) 1969;47(3):690–703. doi: 10.1111/j.1755-3768.1969.tb08157.x. [DOI] [PubMed] [Google Scholar]
- 3.Hayreh SS, Zimmerman MB. Central retinal artery occlusion: visual outcome. Am J Ophthalmol. 2005;140(3):376–391. doi: 10.1016/j.ajo.2005.03.038. [DOI] [PubMed] [Google Scholar]
- 4.Hayreh SS, Zimmerman MB. Fundus changes in central retinal artery occlusion. Retina. 2007;27(3):276–289. doi: 10.1097/01.iae.0000238095.97104.9b. [DOI] [PubMed] [Google Scholar]
- 5.Hwang GJ, Woo SJ, Hwang JM, Jung C, Park KH, Kwon OK. Reversal of ischemic retinopathy following balloon angioplasty of a stenotic ophthalmic artery. J Neuroophthalmol. 2010;30(3):228–230. doi: 10.1097/WNO.0b013e3181dc2078. [DOI] [PubMed] [Google Scholar]
- 6.Leisser C. Risk factor analysis in patients with retinal artery occlusion with respect to transesophageal echocardiography. Spektrum Augenheilkd. 2014;28(3):118–120. [Google Scholar]
- 7.Chang YS, Jan RL, Weng SF, Wang JJ, Chio CC, Wei FT, Chu CC. Retinal artery occlusion and the 3-year risk of stroke in Taiwan: a nationwide population-based study. Am J Ophthalmol. 2012;154(4):645–652.e1. doi: 10.1016/j.ajo.2012.03.046. [DOI] [PubMed] [Google Scholar]
- 8.Rim TH, Han JN, Choi YS, Hwang SS, Lee CS, Lee SC, Kim SS. Retinal artery occlusion and the risk of stroke development: twelve-year nationwide cohort study. Stroke. 2016;47(2):376–382. doi: 10.1161/STROKEAHA.115.010828. [DOI] [PubMed] [Google Scholar]
- 9.Callizo J, Feltgen N, Pantenburg S, Wolf A, Neubauer AS, Jurklies B, Wachter R, Schmoor C, Schumacher M, Junker B, Pielen A, European Assessment Group for Lysis in the Eye Cardiovascular risk factors in central retinal artery occlusion: results of a prospective and standardized medical examination. Ophthalmology. 2015;122(9):1881–1888. doi: 10.1016/j.ophtha.2015.05.044. [DOI] [PubMed] [Google Scholar]
- 10.Wu SL, Huang ZR, Yang XC, Zhou Y, Wang AX, Chen L, Zhao HY, Ruan CY, Wu YT, Xin AJ, Li KB, Jin C, Cai J. Prevalence of ideal cardiovascular health and its relationship with the 4-year cardiovascular events in a northern Chinese industrial city. Circ Cardiovasc Qual Outcomes. 2012;5(4):487–493. doi: 10.1161/CIRCOUTCOMES.111.963694. [DOI] [PubMed] [Google Scholar]
- 11.Wang AX, Liu XX, Guo XH, Dong Y, Wu YT, Huang Z, Xing AJ, Luo YX, Jonas JB, Wu SL. Resting heart rate and risk of hypertension: results of the Kailuan cohort study. J Hypertens. 2014;32(8):1600–1605. discussion 1605. doi: 10.1097/HJH.0000000000000230. [DOI] [PubMed] [Google Scholar]
- 12.Wang A, Wu J, Zhou Y, Guo X, Luo Y, Wu S, Zhao X. Measures of adiposity and risk of stroke in china: a result from the Kailuan study. PLoS One. 2013;17;8(4):e61665. doi: 10.1371/journal.pone.0061665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Becker BN, Vassalotti JA. A software upgrade: CKD testing in 2010. Am J Kidney Dis. 2010;55(1):8–10. doi: 10.1053/j.ajkd.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 14.Hayreh SS, Podhajsky PA, Zimmerman MB. Retinal artery occlusion: associated systemic and ophthalmic abnormalities. Ophthalmology. 2009;116(10):1928–1936. doi: 10.1016/j.ophtha.2009.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Avery MB, Magal I, Kherani A, Mitha AP. Risk of stroke in patients with ocular arterial occlusive disorders: a retrospective Canadian study. J Am Heart Assoc. 2019;8(3):e010509. doi: 10.1161/JAHA.118.010509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cheung N, Lim L, Wang JJ, Islam FM, Mitchell P, Saw SM, Aung T, Wong TY. Prevalence and risk factors of retinal arteriolar emboli: the Singapore Malay Eye Study. Am J Ophthalmol. 2008;146(4):620–624. doi: 10.1016/j.ajo.2008.05.033. [DOI] [PubMed] [Google Scholar]
- 17.Chang YS, Ho CH, Chu CC, Wang JJ, Tseng SH, Jan RL. Risk of retinal artery occlusion in patients with diabetes mellitus: a retrospective large-scale cohort study. PLoS One. 2018;13(8):e0201627. doi: 10.1371/journal.pone.0201627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheng HC, Pan RH, Yeh HJ, Lai KR, Yen MY, Chan CL, Wang AG. Ambient air pollution and the risk of central retinal artery occlusion. Ophthalmology. 2016;123(12):2603–2609. doi: 10.1016/j.ophtha.2016.08.046. [DOI] [PubMed] [Google Scholar]
- 19.Yen JC, Lin HL, Hsu CA, Li YC, Hsu MH. Atrial fibrillation and coronary artery disease as risk factors of retinal artery occlusion: a nationwide population-based study. Biomed Res Int. 2015;2015:374616. doi: 10.1155/2015/374616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bahceci Simsek I, Ozay B. Retinal precapillary arteriolar occlusion after coronary artery bypass grafting surgery. Heart Surg Forum. 2016;19(1):E8–E11. doi: 10.1532/hsf.1347. [DOI] [PubMed] [Google Scholar]
- 21.Lin YC, Chen WC, Liao WC, Hsia TC. Central retinal artery occlusion and brain infarctions after nasal filler injection. QJM. 2015;108(9):731–732. doi: 10.1093/qjmed/hcu235. [DOI] [PubMed] [Google Scholar]
- 22.Hong JH, Ahn SJ, Woo SJ, Jung C, Chang JY, Chung JH, Han MK. Central retinal artery occlusion with concomitant ipsilateral cerebral infarction after cosmetic facial injections. J Neurol Sci. 2014;346(1-2):310–314. doi: 10.1016/j.jns.2014.08.030. [DOI] [PubMed] [Google Scholar]
- 23.Ammar MJ, Kolomeyer AM, Bhatt N, Tamhankar MA, Mullen MT, Brucker AJ. Recurrent branch retinal artery occlusion from susac syndrome: case report and review of literature. Retin Cases Brief Rep. 2018 doi: 10.1097/ICB.0000000000000751. [DOI] [PubMed] [Google Scholar]
- 24.Hua L, Patel K, Corbett JJ. Bilateral central retinal artery occlusion in a patient with systemic lupus erythematosus. J Stroke Cerebrovasc Dis. 2015;24(6):e139–e141. doi: 10.1016/j.jstrokecerebrovasdis.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 25.Bawankar P, Samant P, Lahane S, Jain A, Pathak P. Combined central retinal artery and vein occlusion as the presenting manifestation of systemic lupus erythematosus. Indian J Ophthalmol. 2018;66(12):1864. doi: 10.4103/ijo.IJO_996_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chatziralli IP, Parikakis EA, Mitropoulos PG. Undiagnosed patent foramen ovale as a rare cause for branch retinal artery occlusion. Eur J Ophthalmol. 2015;25(5):e88–e90. doi: 10.5301/ejo.5000608. [DOI] [PubMed] [Google Scholar]
- 27.Berryman J, Moshiri A, Chang M. Chronic lymphocytic leukaemia presenting as branch retinal artery occlusion and optic disc infiltration. BMJ Case Rep. 2018;2018:bcr-2018-227691. doi: 10.1136/bcr-2018-227691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhou Y, Zhu WG, Wang CY. Relationship between retinal vascular occlusions and incident cerebrovascular diseases: a systematic review and meta-analysis. Medicine (Baltimore) 2016;95(26):e4075. doi: 10.1097/MD.0000000000004075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cannon CP. An overview of stroke and the impact of atrial fibrillation. Am J Manag Care. 2010;16(10 Suppl):S273–S277. [PubMed] [Google Scholar]
- 30.Ishigami K, Okuro M, Koizumi Y, Satoh K, Iritani O, Yano H, Higashikawa T, Iwai K, Morimoto S. Association of severe hypertension with pneumonia in elderly patients with acute ischemic stroke. Hypertens Res. 2012;35(6):648–653. doi: 10.1038/hr.2012.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heuschmann PU, Kircher J, Nowe T, Dittrich R, Reiner Z, Cifkova R, Malojcic B, Mayer O, Bruthans J, Wloch-Kopec D, Prugger C, Heidrich J, Keil U. Control of main risk factors after ischaemic stroke across Europe: data from the stroke-specific module of the EUROASPIRE III survey. Eur J Prev Cardiol. 2015;22(10):1354–1362. doi: 10.1177/2047487314546825. [DOI] [PubMed] [Google Scholar]
- 32.Liu LP, Wang D, Wong KS, Wang YJ. Stroke and stroke care in China: huge burden, significant workload, and a national priority. Stroke. 2011;42(12):3651–3654. doi: 10.1161/STROKEAHA.111.635755. [DOI] [PubMed] [Google Scholar]
- 33.Park SJ, Choi NK, Yang BR, Park KH, Lee J, Jung SY, Woo SJ. Risk and risk periods for stroke and acute myocardial infarction in patients with central retinal artery occlusion. Ophthalmology. 2015;122(11):2336–2343.e2. doi: 10.1016/j.ophtha.2015.07.018. [DOI] [PubMed] [Google Scholar]
- 34.Recchia FM, Brown GC. Systemic disorders associated with retinal vascular occlusion. Curr Opin Ophthalmol. 2000;11(6):462–467. doi: 10.1097/00055735-200012000-00013. [DOI] [PubMed] [Google Scholar]
- 35.Rudkin AK, Lee AW, Chen CS. Vascular risk factors for central retinal artery occlusion. Eye (Lond) 2010;24(4):678–681. doi: 10.1038/eye.2009.142. [DOI] [PubMed] [Google Scholar]
- 36.Babikian V, Wijman CA, Koleini B, Malik SN, Goyal N, Matjucha IC. Retinal ischemia and embolism. Etiologies and outcomes based on a prospective study. Cerebrovasc Dis. 2001;12(2):108–113. doi: 10.1159/000047689. [DOI] [PubMed] [Google Scholar]