Abstract
Background
Contraceptive education is generally a standard component of postpartum care, although the effectiveness is seldom examined. The assumptions that form the basis of such programs include postpartum women being motivated to use contraception and that they will not return to a health provider for family planning advice. Women may wish to discuss contraception both prenatally and after hospital discharge. Nonetheless, two‐thirds of postpartum women have unmet needs for contraception. In the USA, many adolescents have repeat pregnancies within a year of giving birth.
Objectives
Assess the effectiveness of educational interventions for postpartum women on contraceptive use
Search methods
We searched for trials through June 2015 in PubMed, CENTRAL, CINAHL, POPLINE, and Web of Science. For current trials, we searched ClinicalTrials.gov and ICTRP. Previous searches also included EMBASE and PsycInfo. We also examined reference lists of relevant articles. For earlier versions, we contacted investigators to locate additional reports.
Selection criteria
We considered randomized controlled trials (RCTs) that examined postpartum education about contraceptive use, whether delivered to individuals or to groups of women. Studies that randomized clusters rather than individuals were eligible if the investigators accounted for the clustering in the analysis. The intervention must have started within one month after delivery.
Data collection and analysis
We assessed titles and abstracts identified during the literature searches. The data were abstracted and entered into Review Manager. Studies were examined for methodological quality. For dichotomous outcomes, the Mantel‐Haenszel odds ratio (OR) with 95% confidence interval (CI) was calculated. Where data were sFor continuous variables, we computed the mean difference (MD) with 95% CI. Due to varied interventions and outcome measures, we did not conduct meta‐analysis.
Main results
Twelve trials met our eligibility criteria, included the three added in this update. The studies included a total of 4145 women. Eight trials were conducted in the USA; the others were from Australia, Nepal, Pakistan, and Syria. Four studies provided one session before hospital discharge; three had structured counseling of varying intensity and one involved informal counseling. Of eight interventions with than one contact, five focused on adolescents. Three of the five involved home visiting, one provided multiple clinic services, and one had in‐person contact and phone follow‐up. Of the remaining three for women of varying ages, two involved home visits and one provided phone follow‐up.
Our sensitivity analysis included six trials with evidence of moderate or high quality. In a study with adolescents, the group with home‐based mentoring had fewer second births within two years compared to the control group (OR 0.41, 95% CI 0.17 to 1.00). The other five interventions had no effect. Of trials with lower quality evidence, two showed some effectiveness. In Nepal, women with an educational session immediately postpartum were more likely to use contraception at six months than those with a later or no session (OR 1.62, 95% CI 1.06 to 2.50). In an Australian study, teenagers in a structured home‐visiting program were more likely to have effective contraception use at six months than those with standard home visits (OR 3.24; 95% CI 1.35 to 7.79).
Authors' conclusions
We focused our results summary on trials with moderate or high quality evidence. Overall, the overall quality of evidence in this review was moderate to low and the evidence of effectiveness was mostly low quality. The interventions could be improved by strengthening the program design and implementation. Some studies did not report program training for providers, adherence to the intervention protocol, or measurement of participants' knowledge and skills. Many trials did not have an objective outcome measure, i.e., pregnancy test or structured questionnaire for contraceptive use. Valid and reliable outcome measures are needed to obtain meaningful results. Still, given the associated costs and logistics, some programs would not be feasible in many settings.
Plain language summary
Education about family planning for women who have just given birth
Counseling about family planning is standard for most women who just gave birth. Few providers and researchers have looked at how well the counseling works. We do not know if postpartum women want to use family planning or whether they will return to a health provider for birth control advice. Women may wish to discuss family planning before they have the baby and after they leave the hospital. Women may also prefer to talk about birth control along with other health issues. In this review, we looked at the effects of educational programs about family planning for women who just had a baby.
Through June 2015, we searched for trials of education about family planning after having a baby. We also wrote to researchers to find other trials. The trials had to study how much the program affected family planning use. The program must have occurred within a month after the birth. We entered the data into RevMan and used the odds ratio to examine effect. We also looked at the quality of the research methods.
We found 12 trials with 4145 women. Eight studies were from the USA and the others were from Australia, Nepal, Pakistan, and Syria. Four trials provided one counseling session before hospital discharge. Of eight studies with more than one contact, five focused on teens. Three of the five had home visiting, one used clinic services, and one had personal and phone contacts. Of three studies with women and teens, two had home visits and one used phone contact.
Six trials had results of moderate quality. In a study with adolescents, the group with home‐based mentoring had fewer second births within two years compared to the control group. Of trials with lower quality evidence, two showed some effect. In Nepal, more of the women with some counseling right after delivery may use birth control at six months than those with a session later or none. In Australia, more teens in a special home‐visiting program used birth control correctly at six months than those with standard home visits.
We found moderate to low quality results overall. Most of those with some effect were low quality. Better program design and carrying out could make them stronger. Even still, some programs might cost too much for some settings.
Summary of findings
for the main comparison.
| Special education compared with routine or delayed education for contraceptive use | ||||
|
Patient or population: women with postpartum status Settings: clinic or community Intervention: special contraception education Comparison: see Comments | ||||
| Outcomes | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments |
| Second birth (by 24 months) | OR 0.41 (95% CI 0.17 to 1.00) | Participants = 149 (Black 2006) | ⊕⊕⊕⊝ moderate | Home mentoring vs usual care |
| Contraception use (at 6 months): immediate session vs no immediate session | OR 1.62 (95% CI 1.06 to 2.50) | Participants = 393 (Bolam 1998) | ⊕⊕⊝⊝ low | Education: immediate vs later |
| Effective contraception use (at 6 months) | OR 3.24 (95% CI 1.35 to 7.79) | Participants = 124 (Quinlivan 2003) | ⊕⊕⊝⊝ low | Home visiting: structured vs routine |
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
Background
Description of the condition
Nearly two‐thirds of women in their first postpartum year have an unmet need for family planning (Ross 2001; USAID 2014). Data from 17 countries show that return to sexual activity is associated with the return of menses, breastfeeding status, and postpartum duration but not generally associated with contraceptive use (Borda 2010). Millions of women, especially in lower‐resource areas, are at risk for unplanned pregnancy and its consequent morbidity and mortality. Even in higher‐resource areas such as the USA, nearly 60% of pregnancies are unintended, i.e., either unwanted (23%) or mistimed (37%) (Mosher 2012). First‐time adolescent mothers who do not start contraception before hospital discharge are more likely to have a repeat pregnancy within two years (Damle 2015). While adolescents may start using contraception during the postpartum period, they often discontinue due to lack of information or support (Wilson 2011).
Description of the intervention
Contraceptive education is generally considered a standard component of postpartum care. The counseling is frequently part of discharge planning but may also begin antepartum (Glasier 1996; Glazer 2011). Postpartum contraception counseling is often limited to one encounter, which is unlikely to affect behavior. Decisions about contraception made right after counseling may differ considerably from contraceptive use postpartum (Engin‐Üstün 2007; Glazer 2011). In some locations, postpartum care may be limited and undocumented, and may focus on the infant rather than the mother (Do 2013).
Postpartum women may wish to discuss contraception prenatally or after hospital discharge, preferably in the context of general education about maternal and child health (Glasier 1996; Ozvaris 1997). Many women are comfortable with advice and a prescription from their physician during well‐baby visits (Fagan 2009). In a rural area in Bangladesh, intensive provision of maternal and child health and family planning programs resulted in increased uptake of contraceptives (Koenig 1992). A recent trial examined the effect on contraceptive use from integrating family planning into infant immunization services (FHI 360 2013). However, the women were 6 to 12 months postpartum by that time.
Educational interventions provided to individuals or groups may increase contraceptive uptake as well as improve use and continuation of the chosen method. Counseling may involve a single contact or multiple sessions. Personal interaction can help women choose an appropriate method and obtain detailed information about method use. Social marketing can have greater reach and may increase awareness and promote use of contraceptives (Chapman 2012). Educational projects may also utilize technology, such as mobile phone reminders for appointments and medication use. Some programs engage peer educators or community workers to provide reminders and encourage method continuation.
Why it is important to do this review
In the past, midwifery and obstetric texts rarely questioned the effectiveness of postpartum contraceptive education, though it was considered a responsibility in postpartum care (Keith 1980; Semeraro 1996). Research evaluating such education is still sparse. More is known about the appropriateness of specific contraceptive methods for postpartum women than about how to help women use certain contraceptives (Shaw 2007). This review examines randomized controlled trials of postpartum interventions to educate women about contraceptive use. In this update we sought additional evidence on the effectiveness of such efforts.
Objectives
We assessed the effectiveness of educational interventions for postpartum women on contraceptive use.
Methods
Criteria for considering studies for this review
Types of studies
We considered randomized controlled trials (RCTs) that examined postpartum education about contraceptive use, whether delivered to individuals or to groups of women. Studies that randomized clusters rather than individuals were eligible if the investigators accounted for the clustering in the analysis.
Types of participants
Women gave birth at 20 weeks of gestation or more. We excluded trials focused on the needs of women with alcohol or drug problems and trials focused on women with chronic health conditions such as HIV or diabetes.
Types of interventions
Trials were included if they evaluated postpartum education provided to influence uptake of contraception including lactational amenorrhea. Educational interventions may have been based on written materials, video or audio recordings, or individual or group counseling. The intervention must have started postpartum and begun within one month of delivery.
Types of outcome measures
Primary outcomes
To be included, trials had to have data on unplanned pregnancies or contraceptive choice or use. The trials may have had other primary outcomes.
Secondary outcomes
Additional outcomes were knowledge and attitudes about contraception and satisfaction with postnatal care.
Search methods for identification of studies
Electronic searches
Through June 2015, we conducted searches of MEDLINE, Cochrane Central Register of Controlled Trials (CENTRAL), POPLINE, CINAHL, and Web of Science. We also searched for current trials via ClinicalTrials.gov and ICTRP. The search strategies are given in Appendix 1. Previous search strategies also included EMBASE and PsycINFO; they are shown in Appendix 2.
Searching other resources
Reference lists of relevant papers were examined for additional citations. For previous versions, we also contacted investigators in the field to seek unpublished trials or published trials we may have missed in our searches.
For the initial review in 1999, the authors contacted the following organizations for advice about relevant research: Guttmacher Institute, California Family Health Council, Contraceptive Research and Development, Couple to Couple League, Engender Health, European Commission, Health, Family Planning and AIDS Unit, Family Planning Association of Queensland, Family Planning Councils of America, Family Planning International Assistance, Family Planning Management Development, Healthy Women, Johns Hopkins University Center for Communication Programs, Marie Stopes International, National Family Planning and Reproductive Health Association, Planned Parenthood Global Partners, Population and Community Development Association, Population Reference Bureau, Prime II, Program of Appropriate Technology in Health. The authors also searched databases listing publications by the Population Council, Family Health International (now FHI 360), and the World Health Organization.
Data collection and analysis
Selection of studies
One author reviewed the search results and a second author examined the reports identified for appropriate categorization. We excluded studies that randomized clusters rather than individuals and did not account for the clustering in the analysis. For the initial review, the three authors independently assessed the studies to determine which were suitable for inclusion. The authors resolved any differences by discussion.
Data extraction and management
Two authors conducted the data extraction. One author entered the data into Review Manager (RevMan 2014), and a second author checked accuracy (Contributions of authors). These data included the study characteristics, risk of bias, and outcome data.
Assessment of risk of bias in included studies
Intervention fidelity
We used the framework in Borrelli 2011 to assess the quality of the intervention. Domains of treatment fidelity are study design, training of providers, delivery of treatment (intervention), receipt of treatment, and enactment of treatment skills. The framework was intended for assessing current trials. Criteria of interest for our review are shown below.
Study design: had a curriculum or treatment manual
Prior training of providers: specified providers' credentials
Project‐specific training: provided standardized training for the intervention
Delivery: assessed adherence to the protocol
Receipt: assessed participants' understanding and skills regarding the intervention.
In this update, we revised the terminology for the first four criteria, but the concepts are the same. We added the fifth criterion of 'Receipt' in this version of this review, based on newer information in Borrelli 2011. For the assessment of evidence quality, we downgraded the studies that met fewer than four of the five criteria.
Research design
Included trials were evaluated for methodological quality in accordance with recommended principles (Higgins 2011). Factors considered included randomization method, allocation concealment, blinding, and losses to follow‐up and early discontinuation. This information was entered into the Risk of bias tables (Characteristics of included studies).
Measures of treatment effect
For the dichotomous outcomes, the Mantel‐Haenszel odds ratio (OR) with 95% confidence interval (CI) was calculated. An example is the proportion of women who initiated use of a particular contraceptive method. Fixed and random effects give the same result if no heterogeneity exists, as when a comparison includes only one study. Where data were sparse, we used the Peto OR. For continuous variables, the mean difference (MD) was computed with 95% CI. Review Manager uses the inverse variance approach.
Assessment of heterogeneity
Due to varied study designs, we were unable to conduct meta‐analysis. Therefore, we did not need to assess statistical heterogeneity. However, we address heterogeneity due to differences in interventions, study design, and populations in the Discussion.
Data synthesis
We applied principles from GRADE to assess the quality of evidence and address confidence in the effect estimates (Balshem 2011; Higgins 2011). Our assessment of the body of evidence is based on the quality of evidence from the studies. When a meta‐analysis is not viable because of varied interventions or outcome measures, a summary of findings table is not feasible. Therefore, we did not conduct a formal GRADE assessment, i.e., with an evidence profile and summary of findings table, for all outcomes (Guyatt 2011).
Our assessment of evidence quality included the design, implementation, and reporting of both the intervention and the trial. We incorporated the quality of intervention evidence into the overall assessment of evidence quality. We considered RCTs to be high quality then downgraded for the following:
intervention fidelity information for fewer than four criteria;
no information on randomization sequence generation or allocation concealment, or risk of bias was high for one;
outcome assessment lacked an objective measure, e.g., pregnancy test or structured questionnaire for contraceptive use;
follow‐up less than three months for contraceptive use or less than six months for pregnancy;
loss to follow‐up greater than 20%.
Sensitivity analysis
The sensitivity analysis included evidence of moderate or high quality.
Results
Description of studies
Results of the search
The 2012 search produced 217 new references. After reviewing the titles and abstracts, 212 were discarded due to not meeting the eligibility criteria. We examined the full text of five reports; two were later excluded. Three reports from two trials were added to the eight trials included in earlier versions of this review. In addition, we included two ongoing trials identified in clinical trials databases.
In 2015, searches of databases yielded 277 unduplicated citations. A total of 101 duplicates were removed electronically or by hand. With one identified from other sources, the total of unduplicated references was 278. We reviewed the full text of eight items. We included three primary reports; one was a conference abstract for which we had the ClinicalTrials.gov listing. We also included one secondary article and two abstracts related to full reports. We excluded two primary reports. From recent clinical trial listings, we obtained 40 unduplicated trials. We categorized one as ongoing and updated one listing from the earlier review.
Included studies
We included 12 trials that met our eligibility criteria after adding 3 in this update (Simmons 2013; Tang 2014; Torres 2014). The studies included a total of 4145 women; the mean was 319 and the median was 240. One trial had a preliminary report published as a conference abstract (Torres 2014).
Eight studies were conducted in the USA; the other four were from Australia (Quinlivan 2003), Nepal (Bolam 1998), Pakistan (Saeed 2008), and Syria (Bashour 2008). Six trials focused on adolescents (O'Sullivan 1992; Quinlivan 2003; Black 2006; Barnet 2009; Katz 2011) or young women (Gilliam 2004).
The studies varied in the content and format of the education provided (Table 15).
1. Intervention description.
| Study | N | Population | Country | Intervention location; medium | Intervention content |
| O'Sullivan 1992 | 243 | Adolescents | USA | Well‐baby clinic | Special well‐baby care |
| Bolam 1998 | 540 | Women | Nepal | Hospital and home | Health education, including infant care and family planning |
| Quinlivan 2003 | 139 | Adolescents | Australia | Home | Structured support and counseling |
| Gilliam 2004 | 33 | Young women (<= 25 years) | USA | Hospital | Oral contraceptive use |
| Black 2006 | 181 | Adolescents | USA | Home | Parenting (included contraception) |
| Bashour 2008 | 903 | Women | Syria | Home | Education and support, including breastfeeding and contraception |
| Saeed 2008 | 648 | Women | Pakistan | Hospital | Contraceptive use |
| Barnet 2009 | 237 | Adolescents | USA | Home; CAMI | Parenting (included contraception); case management |
| Katz 2011 | 249 | Adolescents | USA | Community; cell phone | Health risks and teen attitudes; included reproductive health planning |
| Simmons 2013 | 50 | Women | USA | Hospital; phone | LARC, logistics |
| Tang 2014 | 800 | Women | USA | Hospital; script | LARC |
| Torres 2014 | 121 | Women | USA | Hospital; script | Relative effectiveness of methods |
CAMI = computer‐assisted motivational intervention LARC = long‐acting reversible contraception
Four provided one educational session before hospital discharge, with the content focused on contraception. Three had routine or alternative care as the comparison (Gilliam 2004; Tang 2014; Torres 2014); in the fourth, the control group had no intervention (Saeed 2008).
Eight trials provided more than one contact. In addition to contraception, some addressed broader health education or parenting issues while others provided logistical support or case management. The interventions involved one or more home visits (Quinlivan 2003; Black 2006; Bashour 2008; Bolam 1998; Barnet 2009), clinic contacts (O'Sullivan 1992), or phone sessions (Katz 2011; Simmons 2013).
All reports had some information regarding intervention fidelity (Table 2). All reports had information on the intervention content or its development. In most trials, clinicians provided the education and had some intervention training although the intensity of training varied. In a few studies, the women who provided the intervention had demographics similar to those of the participants.
2. Intervention fidelity information.
| Study | Curriculum or manual | Provider credentials | Training for intervention | Assessed adherence to protocol | Assessed intervention receipta | Fidelity criteria met |
| O'Sullivan 1992 | 4 goals and specific services identified; which professionals provide each component | Directed by nurse practitioner; providers included social worker, pediatrician and nurse practitioner, volunteers | Volunteers were 'trained' | _ | _ | 3 |
| Bolam 1998 | Format and content identified for sessions including key messages | 3 health educators, 2 midwives, 1 community health worker | Providers were 'trained' to give the health education | Investigators monitored weekly and gave feedback | Knowledge of infant health issues (primary outcome) | 5 |
| Quinlivan 2003 | Structured home visits outlined in report | Certified midwives | _ | _ | Knowledge of contraception (primary outcome) | 3 |
| Gilliam 2004 | Developed counseling program, video, pamphlet; development described | Resident physicians, nurses for additional counseling | Training session for resident physicians and nurses | _ | Knowledge of OCs (secondary outcome) | 4 |
| Black 2006 | Curriculum with 19 lessons; order could vary after 2 sessions | 2 Black women, college‐educated, in their 20s, single mothers, living independently | 'Extensive' training provided | Weekly supervisory sessions | _ | 4 |
| Bashour 2008 | Objectives for each visit; breastfeeding in visits 2 and 3, family planning in visit 4 | Registered midwives | 5 days of special training | _ | _ | 3 |
| Saeed 2008 | Counseling leaflet used | Physicians | Providers had 40‐minute training on leaflet and interview methods. | _ | _ | 3 |
| Barnet 2009 | Structured software (computer‐assisted motivational intervention (CAMI)); 20‐min stage‐matched motivational interviewing (MI); parenting curriculum | African American paraprofessional women from participants' communities; had empathetic qualities, rapport with adolescents, community knowledge | 2.5 days on transtheoretical model, MI, and CAMI | First 4 months, counselors met biweekly with MI supervisor (discussed audiotapes and gave feedback) | _ | 4 |
| Katz 2011 | Curriculum with standardized format and session structure; teen workbooks with visual material on topics | Masters‐level young women of similar racial‐ethnic background as teens | _ | Process evaluation included delivery | _ | 3 |
| Simmons 2013 | _ | 2 personal assistants with contraceptive counseling experience (OBGYN resident, 4th‐year medical student) | _ | Contacts planned; additional counseling as needed | _ | 2 |
| Tang 2014 | 1‐minute script | Research assistants | _ | _ | _ | 2 |
| Torres 2014 | Written structured script on all contraceptive methods by effectiveness | _ | _ | _ | Knowledge assessed with 'widely accepted instrument' | 2 |
aAssessed participants' understanding and skills regarding the intervention.
Outcomes included contraceptive use, pregnancy, and contraceptive knowledge. All trials assessed contraceptive use; six reported on repeat pregnancy or second birth. In Characteristics of included studies, we focus on the primary and secondary outcomes for this review. Studies may have had additional outcomes.
Risk of bias in included studies
Details for each study can be found in Characteristics of included studies. The trial with only a conference abstract had limited design information (Torres 2014).
Intervention quality
All reports provided some documentation of intervention content and most had implementation information (Table 2). A few did not provide much or any information on training of providers for the specific intervention. Only five reported on how the investigators assessed delivery adherence, i.e., whether the intervention was provided as intended.
Outcome assessment was limited in many studies (Table 3). That is, three of six trials that assessed pregnancies or repeat births had some objective validation, such as pregnancy test or vital statistics. Some studies assessed or reported contraceptive use with one dichotomous item, while others had structured questionnaires. Three studies had limited follow‐up periods. The short‐term nature of several interventions may also have limited the usefulness of the effectiveness measures.
3. Evidence quality.
| Study | Intervention fidelity < 4 items | Randomization; allocation concealment | Outcome assessment | Follow‐up period | Loss > 20% | Evidence qualitya,b | Evidence of effectiveness |
| Barnet 2009 | _ | _ | _ | _ | _ | High | _ |
| Black 2006 | _ | _ | ‐1 | _ | _ | Moderate | Fewer repeat births (by 24 months) |
| Gilliam 2004 | _ | _ | _ | _ | ‐1 | Moderate | _ |
| Katz 2011 | ‐1 | _ | _ | _ | _ | Moderate | _ |
| Simmons 2013 | ‐1 | _ | _ | _ | _ | Moderate | _ |
| Bashour 2008 | ‐1 | _ | _ | ‐1 | _ | Moderate to lowc | _ |
| Bolam 1998 | _ | _ | ‐1 | _ | ‐1 | Low | Use of contraception (at 6 months) |
| Quinlivan 2003 | ‐1 | _ | ‐1 | _ | _ | Low | Effective use of contraception (at 6 months) |
| Tang 2014 | ‐1 | _ | _ | ‐1 | _ | Low | _ |
| O'Sullivan 1992 | ‐1 | ‐1 | ‐1 | _ | _ | Very low | Fewer repeat pregnancies (by 18 months) |
| Saeed 2008 | ‐1 | _ | ‐1 | ‐1 | _ | Very low | Use of contraception (at 8 to 12 weeks) |
| Torres 2014 | ‐1 | ‐1 | ‐1d | _ | ‐1d | Very low | Use of highly effective contraception (at 3 months) |
aRCTs considered high quality then downgraded: 1) intervention fidelity < 4 criteria; 2) no information on randomization sequence generation or allocation concealment, or risk of bias was high for one; 3) outcome assessment lacked an objective measure (e.g., pregnancy test or structured questionnaire for contraceptive use); 4) follow‐up < 3 months for contraceptive use or < 6 months for pregnancy; 5) loss to follow‐up > 20% bSensitivity analysis included evidence of moderate or high quality cModerate for contraceptive use; low for pregnancy dUnknown; preliminary report
Allocation
Five trials provided information on sequence generation and used sealed envelopes to conceal the allocation (Bolam 1998; Quinlivan 2003; Gilliam 2004; Bashour 2008; Tang 2014). Four had information on the randomization procedure but nothing on allocation concealment (Saeed 2008; Barnet 2009; Katz 2011; Simmons 2013). Three did not have information on sequence generation or concealment (O'Sullivan 1992; Black 2006; Torres 2014).
Blinding
Blinding of assignment was not possible in many trials, given the nature of the interventions. However, the outcome assessors were blind to group of allocation in three trials (Bolam 1998; Bashour 2008; Saeed 2008). Research team members were blinded in three studies (Gilliam 2004; Simmons 2013; Tang 2014). One trial was open (Torres 2014).
Incomplete outcome data
Losses to follow‐up were greater than 20% in two trials: Bolam 1998 (25% at three months and 27% at six months) and Gilliam 2004 (52% by one year). Losses were not as high overall as for some trials in contraceptive education (Lopez 2013).
Other potential sources of bias
Black 2006 excluded participants after randomization due to missing data. Barnet 2009 excluded one participant who had a stillborn infant and one whose two‐month‐old infant died.
Effects of interventions
See: Table 1
Counseling (one contact)
Four studies provided a single counseling session focused on contraception (Gilliam 2004; Saeed 2008; Tang 2014; Torres 2014). Torres 2014 also reportedly facilitated access to the woman's desired contraceptive method, but we had limited information from the conference abstract. Three trials were conducted in the USA and one in Pakistan (Saeed 2008). Gilliam 2004 focused on young women (<= 25 years old), two trials included participants from age 14 up to 45 years (Tang 2014) or up to 50 years (Torres 2014), and Saeed 2008 did not have any age specifications.
Gilliam 2004 (N = 33) provided a multi‐component intervention of counseling, videotape about oral contraceptives (OC), and written material. The comparison group had usual care. The experimental and comparison groups were not significantly different in the proportions that continued oral contraceptive use at one year (Analysis 1.1), those who switched the type of contraceptive used (Analysis 1.2), or known pregnancies (Analysis 1.3). The investigators noted that the sample size was not sufficient to detect a 20% difference between groups, due to resource limitations.
In Saeed 2008 (N = 648), the experimental group received informal counseling on contraception plus a pamphlet. The control group had no intervention. At 8 to 12 weeks postpartum in Saeed 2008, women in the counseling group were more likely to report using contraception (OR 19.56; 95% CI 11.65 to 32.83) (Analysis 2.1). For choice of contraceptive, all women in the counseling group planned to use a modern contraceptive method by six months postpartum compared to a third of the control group (Peto OR 18.53, 95% CI 13.15 to 26.12) (Analysis 2.2). The physician‐assessor was reportedly blinded to study arm.
Tang 2014 (N = 800) used a one‐minute script on long‐acting, reversible contraception (LARC). Long‐acting methods include intrauterine contraception and the subdermal implant. Women were followed up by phone after the six‐week visit. The comparison group received routine counseling at the hospital, which was not standardized. Despite the large sample size, the study arms did not differ significantly for LARC use (Analysis 3.1), interest in but not using LARC (Analysis 3.2), or use of any contraceptive method (Analysis 3.3).
For Torres 2014 (N = 121), we had preliminary information from the conference abstract. Results were from three months of follow‐up. The trial plans to follow 362 participants for 36 months (12 months for the primary outcome) with completion in 2016. Women with a preterm birth received structured counseling on the relative effectiveness of contraceptive methods, while the comparison group had usual care. The experimental group also reportedly had some assistance with access to the desired contraceptive method, but details were not available. The group with structured counseling was more likely than the routine care group to be using a highly effective contraceptive method at three months (OR 2.23, 95% CI 1.03 to 4.83) (Analysis 4.1). Mean increase in contraceptive knowledge was also higher for structured counseling compared to routine care (MD 2.30, 95% CI 2.00 to 2.60) (Analysis 4.2). No detail was available regarding the knowledge assessment.
1.1. Analysis.

Comparison 1 Oral contraceptive education program (1 session) versus routine counseling, Outcome 1 Continuation of oral contraceptives at one year.
1.2. Analysis.

Comparison 1 Oral contraceptive education program (1 session) versus routine counseling, Outcome 2 Switched contraceptives by one year.
1.3. Analysis.
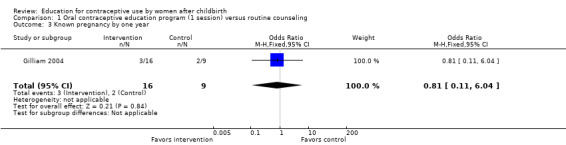
Comparison 1 Oral contraceptive education program (1 session) versus routine counseling, Outcome 3 Known pregnancy by one year.
2.1. Analysis.

Comparison 2 Contraceptive counseling (1 session) versus no counseling, Outcome 1 Use of any contraceptive at 8 to 12 weeks postpartum.
2.2. Analysis.

Comparison 2 Contraceptive counseling (1 session) versus no counseling, Outcome 2 Choice of modern contraceptive (using or plan to use) at 8 to 12 weeks postpartum.
3.1. Analysis.

Comparison 3 LARC script (1‐minute) + routine counseling versus routine counseling, Outcome 1 LARC use after 6 weeks.
3.2. Analysis.

Comparison 3 LARC script (1‐minute) + routine counseling versus routine counseling, Outcome 2 Interested in but not using LARC after 6 weeks.
3.3. Analysis.

Comparison 3 LARC script (1‐minute) + routine counseling versus routine counseling, Outcome 3 Using any contraceptive after 6 weeks.
4.1. Analysis.

Comparison 4 Focused contraceptive counseling (1 session) versus usual care, Outcome 1 Use of highly effective contraceptive method at 3 months.
4.2. Analysis.

Comparison 4 Focused contraceptive counseling (1 session) versus usual care, Outcome 2 Increase in contraceptive knowledge by 3 months.
Programs with two or more contacts (home, clinic, or phone)
Eight trials provided interventions that covered a range of health and lifestyle issues, including contraception. Five targeted adolescents; four were conducted in the eastern USA (O'Sullivan 1992; Black 2006; Barnet 2009; Katz 2011) and one in Australia (Quinlivan 2003). The three that included adult women were conducted in Syria (Bashour 2008), Nepal (Bolam 1998), and the northwestern USA (Simmons 2013).
Adolescents
Five trials focused on adolescents, three of which involved home visiting.
For Quinlivan 2003 (N = 139), young women in the experimental group had a structured home‐visiting program as opposed to standard home visits. Girls in the experimental group were more likely to have effective contraceptive use at six months than those in the comparison group (OR 3.24; 95% CI 1.35 to 7.79) (Analysis 5.1). We did not have sufficient data to analyze contraceptive knowledge in this review. Reportedly, the mean difference in contraceptive knowledge at six months favored the experimental group (reported MD 0.92; 95% CI 0.32 to 1.52).
Black 2006 (N = 181) evaluated second births during home visits. The experimental group had multiple home visits over two years, while the controls had usual care. The mean number of intervention visits was 6.63 (standard deviation 6.58). The adolescents in the treatment group were less likely to have had a second birth within two years than the usual care group (OR 0.41; 95% CI 0.17 to 1.00) (Analysis 6.1).
For Barnet 2009 (N = 237), the experimental groups received a computer‐assisted motivational intervention (CAMI) plus a parenting curriculum (CAMI+) and case management. The comparison groups had the CAMI or usual care. The study arms did not differ significantly for repeat births by 24 months from index birth (Analysis 7.1). Births were assessed through Vital Statistics; 100% of the index births were located. The repeat birth rates for both CAMI groups were lower than, but not significantly different from, the rate for the usual care group. The figures were 13.8% for CAMI plus parenting curriculum (CAMI+), 17.2% for CAMI‐only, and 25% for usual care. Abortion information was obtained at the follow‐up interview. The investigators provided the percentages for reported abortions: CAMI+ 22%, CAMI‐only 20%, and usual care 21%.
5.1. Analysis.

Comparison 5 Home visiting: structured versus routine, Outcome 1 Effective use of contraception at 6 months.
6.1. Analysis.

Comparison 6 Home‐based mentoring (multiple visits) versus usual care, Outcome 1 Second birth by 24 months.
7.1. Analysis.

Comparison 7 Computer‐assisted motivational interviewing (CAMI) with parenting curriculum versus CAMI‐only versus usual care, Outcome 1 Repeat birth by 24 months.
The other two trials for adolescents provided clinic‐based services plus reminders or cell‐phone counseling.
In O'Sullivan 1992 (N = 243), the experimental group had special services provided within the well‐baby clinic, including reminder contacts. The comparison group had the usual well‐baby care. The teenagers in the experimental group were less likely to have a repeat pregnancy (self‐reported) by 18 months compared to the control group (OR 0.35; 95% CI 0.17 to 0.70) (Analysis 8.1). The difference in pregnancies was largely within the subgroup of clinic dropouts. Of the control group, 29/91 had a repeat pregnancy versus 9/60 in the experimental group (data not shown).
Katz 2011 (N = 249) provided a cell‐phone counseling intervention, supplemented by quarterly group sessions. Subsequent pregnancy was assessed via cell phone calls at 3, 9, 15, and 21 months. Pregnancy status was confirmed by urine pregnancy tests at 6, 12, 18 and 24 months. Pregnancy rates did not differ significantly between the study groups during the two‐year follow‐up (Analysis 9.1). The rates were 31% for the group with the cell phone intervention and 36% for the usual care group.
8.1. Analysis.

Comparison 8 Special postpartum care (including contraception) versus routine services (multiple well‐baby contacts), Outcome 1 Repeat pregnancy (self‐report) by 18 months.
9.1. Analysis.

Comparison 9 Phone counseling + follow‐up versus usual services, Outcome 1 Repeat pregnancy by 24 months.
Adult and younger women
Of three interventions for women of various ages, one provided phone follow‐up and two involved home visits.
In Simmons 2013 (N = 50), the special intervention group received reminders and assistance with follow‐up visits as well as counseling by phone. The comparison group had usual care. The groups did not differ significantly for LARC placement by three months in this small trial (Analysis 9.2).
In Bashour 2008 (N = 903), the experimental group had up to four home visits, with the last one focusing on family planning. One study group had a single visit without family planning and the control group had usual care, which did not include a home visit. At four months, the study groups did not differ significantly in contraceptive use (Analysis 10.1; Analysis 10.2) or in self‐reported pregnancy (Analysis 10.3; Analysis 10.4).
For Bolam 1998 (N = 540), two of the four study groups had health education during their postpartum hospital stay. One of those had a second session at three months that included family planning. A third group had the educational session at three months, and the fourth received no health education (Types of interventions). We grouped those with a health education session during their postpartum hospital stay (with or without a later session) and those with a later session or no session. The two groups did not differ significantly for contraceptive use at three months (Analysis 11.1). However, at six months, the group with an immediate postpartum session was more likely to use contraception than the group with a later or no session (OR 1.62; 95% CI 1.06 to 2.50) (Analysis 11.2). We also compared the arms within those groups at six months (three‐month data were not available). Women with an immediate and later session did not differ significantly in contraceptive use from those with one immediate session (Analysis 11.3). Also, contraceptive use among women with only the later session was not significantly different from those with no educational session (Analysis 11.3). Exclusive breastfeeding was emphasized in the immediate postpartum session. The study arms did not differ significantly in exclusive breastfeeding at three months or for more than five months (Analysis 11.4 to Analysis 11.6).
9.2. Analysis.

Comparison 9 Phone counseling + follow‐up versus usual services, Outcome 2 LARC use at 3 months.
10.1. Analysis.

Comparison 10 Home visiting: 4 visits versus 1 visit versus usual care, Outcome 1 Contraception use at 4 months: 4 visits versus 1 visit.
10.2. Analysis.

Comparison 10 Home visiting: 4 visits versus 1 visit versus usual care, Outcome 2 Contraception use at 4 months: 1 visit versus usual care.
10.3. Analysis.

Comparison 10 Home visiting: 4 visits versus 1 visit versus usual care, Outcome 3 Pregnancy (self‐report) at 4 months postpartum: 4 visits versus 1 visit.
10.4. Analysis.

Comparison 10 Home visiting: 4 visits versus 1 visit versus usual care, Outcome 4 Pregnancy (self‐report) at 4 months postpartum: 1 visit versus usual care.
11.1. Analysis.

Comparison 11 Health education (including contraception): immediate, later, or no session, Outcome 1 Contraception use at 3 months: immediate session versus no immediate session.
11.2. Analysis.

Comparison 11 Health education (including contraception): immediate, later, or no session, Outcome 2 Contraception use at 6 months: immediate session versus no immediate session.
11.3. Analysis.

Comparison 11 Health education (including contraception): immediate, later, or no session, Outcome 3 Contraception use at 6 months.
11.4. Analysis.

Comparison 11 Health education (including contraception): immediate, later, or no session, Outcome 4 Exclusive breastfeeding at 3 months: immediate session versus no immediate session.
11.6. Analysis.
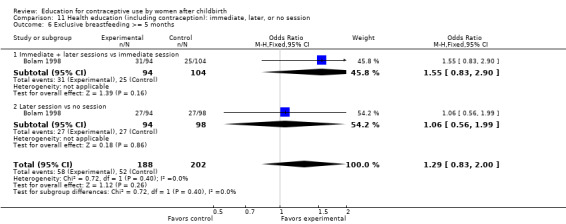
Comparison 11 Health education (including contraception): immediate, later, or no session, Outcome 6 Exclusive breastfeeding >= 5 months.
Discussion
Summary of main results
Sensitivity analysis
We focus here on the six trials with evidence of moderate or high quality (Table 3). One USA study had evidence of intervention effectiveness (Black 2006). In that trial, the experimental group had enhanced services through a home‐visiting program versus usual care for the controls. The experimental group had fewer repeat pregnancies or second births within two years compared to the control group. Second births were assessed during home visits.
The other five trials with evidence of moderate or high quality showed no effect of the intervention. All assessed contraceptive use and three examined pregnancies (a fourth had low quality evidence for pregnancy). The three trials with adolescents or young women provided the following: one multi‐component session (without sufficient power to detect differences) (Gilliam 2004), computer‐assisted motivational interviewing plus case management (Barnet 2009), and a cell‐phone counseling intervention with multiple contacts (Katz 2011). Of the two trials that included adult women, one had up to four home visits with one visit focused on family planning (Bashour 2008) and the other provided reminders and assistance with follow‐up visits as well as phone counseling (Simmons 2013).
Other results
Six trials provided evidence of low or very low quality in our assessment. Of three studies with low quality evidence, two showed evidence of effect on contraceptive use (Bolam 1998; Quinlivan 2003). An Australian trial was based on a home‐visiting program for adolescents, and compared structured versus standard home visits (Quinlivan 2003). The group with structured visits was more likely to use effective contraception at six months than the group with routine care. From Nepal, a four‐arm study provided health education for women of varying ages, including family planning for two groups at different times (Bolam 1998). Three trials with very low quality evidence also showed some effect on pregnancy or contraceptive use (Table 3). A recent study was downgraded largely because of limited information in the preliminary report (Torres 2014). This trial may be rated higher when more information is available on design and implementation.
Of nine studies with low, moderate, or high quality evidence, three showed any significant difference between comparison groups (Table 1). With so few studies overall, we could not detect any pattern based on number of contacts or population of focus. Half of the programs showed some evidence of effect, regardless of the number of contacts.
Of six trials that focused on adolescents or young women, three showed some effect of the intervention. Two had fewer repeat pregnancies or births within the experimental group; both involved home‐visiting programs. The third provided clinic services and reminders, and showed more effective use of contraception in the special‐intervention group.
Of six trials that included women of various ages, three had some effect on contraceptive use. They provided one counseling session versus none, structured counseling versus usual care, and health education including family planning.
Overall completeness and applicability of evidence
We did not combine any trials in meta‐analysis due to varying interventions and outcome measures. The included trials represented various types of postpartum education: one contact or multiple‐session programs in five countries. Several interventions were provided during the postpartum hospital stay, while others began two or three weeks later. In some trials, family planning education was integrated with other health education or health services. The six trials showing positive effects were conducted in Australia, Nepal, Pakistan, and the USA. However, five provided low quality evidence. We did not examine interventions for postpartum contraception that began during the prenatal period. For example, Adanikin 2013 assigned women to either three sessions in the last trimester or the usual single session at the six‐week postpartum visit. Women with the prenatal sessions were more likely to use modern contraceptives at six months compared with the group that only had one postnatal session.
Clinics are likely to vary in the type and amount of usual services. In an urban teaching hospital in the USA, a retrospective study examined factors associated with repeat pregnancy among first‐time adolescent mothers (Damle 2015). Lower risk of rapid repeat pregnancy was found among those with a postpartum visit by eight weeks and who initiated use of long‐acting reversible contraception (LARC) by eight weeks. Special populations may also benefit from targeted programs. In Shanghai, migrant women had an unintended pregnancy rate about four times that of permanent residents (Huang 2014). A contraceptive services program provided counseling and a choice of contraceptive methods for migrant women. The education was provided in the maternity ward prior to delivery, with a second session if time was too limited. Long‐acting methods available prior to discharge included tubal ligation, IUD insertion immediately after delivery, and injection of depot medroxyprogesterone acetate (DMPA). Condoms were provided to those who did not desire a long‐acting method. Contraceptive use at 12 months was 97%, with IUD and condom use at about 39% each followed by tubal ligation at 8% and DMPA at 7%.
Costs for home‐visiting or multiple‐contact programs could be a limiting factor for many settings. Two studies in this review addressed costs. In O'Sullivan 1992, both groups received well‐baby care in the clinic. The hospital estimated the cost per visit to be lower for special care than routine care. The savings were attributed to several factors, such as combining services and not using medical residents who would need training and faculty supervision. In a 2010 article from Barnet 2009, the weighted mean costs for any CAMI were US $2064 per teen. Costs per teen were US $1449 for CAMI‐only and US $2635 for CAMI + parenting curriculum.
Quality of the evidence
Six studies had evidence of moderate or high quality (Table 3), but the overall quality of evidence was moderate to low. Most evidence of effectiveness came from trials of low or very low quality. Our assessment considers the intervention design and implementation as well as the basic trial design. For the latter, Figure 1 summarizes the risk of bias for the review overall. Risk of bias for individual trials is shown in Figure 2. Most trials were published since the first CONSORT guidelines, which have been updated (Schulz 2010), so the trials would be expected to have adequate reporting.
1.

Risk of bias graph: authors' judgements about risk of bias as percentages across all included studies
2.

Risk of bias summary: authors' judgements about risk of bias item for each included study
Authors' conclusions
Implications for practice.
The trials varied in the types of educational programs, settings, and populations served. With so few studies overall, we could not see any pattern based on number of contacts or population of focus. Half of the interventions led to more contraceptive use or fewer unplanned pregnancies. One with home visiting for adolescent mothers had moderate quality evidence. However, most of the trials that showed some effect provided low quality information. Those interventions could be improved by strengthening the program design and implementation. Still, given the associated costs and logistics, some programs would not be feasible in many settings.
Implications for research.
The overall quality of evidence was moderate to low. The evidence of intervention effectiveness was mostly low quality. Reasons included the design and implementation of the intervention and the trial, as well as reporting limitations. Some trials did not report program training for providers, assessment of adherence to the intervention protocol, or measurement of participants' knowledge and skills after the program. Some shortcomings may result from space limitations in journals. However, many trials did not have an objective outcome measure, i.e., pregnancy test or structured questionnaire for contraceptive use. Valid and reliable outcome measures are needed to obtain meaningful results.
What's new
| Date | Event | Description |
|---|---|---|
| 8 July 2015 | New search has been performed | Searches updated |
| 5 May 2015 | New citation required but conclusions have not changed | 3 new trials did not change conclusions |
| 28 January 2015 | New search has been performed | Included 3 new trials included (Simmons 2013; Tang 2014; Torres 2014); excluded 1 trial that was previously included but did not have data on our primary outcomes (Proctor 2006) |
| 7 January 2015 | Amended | Edited wording of Objectives and Types of outcome measures to reflect focus of current review |
History
Protocol first published: Issue 1, 1998 Review first published: Issue 4, 1999
| Date | Event | Description |
|---|---|---|
| 28 June 2012 | New citation required but conclusions have not changed | New trials did not show evidence of effectiveness. We assessed the quality of evidence (Data synthesis), which included quality of intervention evidence (Table 15) and then overall quality of evidence (Table 3). |
| 30 May 2012 | New search has been performed | Searches updated; two new trials included (Barnet 2009; Katz 2011). |
| 9 November 2009 | New citation required and conclusions have changed | We had 7 trials to add. We excluded studies that had issues regarding unit of analysis, i.e., 2 studies from the original review (Foreit 1993; Sayegh 1976).Consequently, the conclusions changed in this version. |
| 25 June 2009 | New search has been performed | New trials added (Bashour 2008; Black 2006; Gilliam 2004; Proctor 2006a; Quinlivan 2003; Saeed 2008). O'Sullivan 1992 was moved to 'included studies,' due to defining postpartum education as that which occurred within 1 month of delivery. Added searches of clinical trial databases. |
| 15 June 2009 | Amended | Expanded time frame for postpartum education to include programs initiated in less than a month after delivery. Included use of health care services as an outcome. |
| 21 May 2009 | Amended | Authors added to lead update (LM Lopez, DA Grimes) |
| 15 April 2008 | Amended | Converted to new review format. |
| 1 March 2002 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
In 2012, S Mullins of FHI 360 helped review search results and conducted the second data abstraction for the new trials.
For the 2006 revision, M Gulmezoglu of WHO extracted data from Nacar 2003, which was published in Turkish. From FHI 360, C Manion searched the electronic databases.
The 1999 Cochrane Review was an update of a pre‐Cochrane review (Hay‐Smith 1994). The original authors acknowledge the assistance provided by V Kallianes and B Winikoff of the Population Council in identifying research on this topic for the 1999 review and the assistance from A Lusher of the Oxford Cochrane Centre in developing the search strategy for the 2002 update.
Appendices
Appendix 1. Search 2015
Because we expanded some of the strategies, we ran certain searches from the initiation of the database. For others, date limitations are shown.
MEDLINE via PubMed (7 July 2015)
("Contraception"[Mesh] OR "Contraception Behavior"[Mesh] OR "Contraceptive Agents"[Mesh] OR "Contraceptive Devices"[Mesh] OR "family planning") AND (educat* OR counsel* OR communicat* OR "information dissemination" OR intervention* OR choice OR choose OR use) AND ("Postpartum Period"[Mesh] OR "Postnatal Care"[Mesh] OR postpartum OR post‐partum OR postnatal OR "repeat pregnancy"[tiab] OR mothers[ti]) AND (Clinical Trial[ptyp])
CENTRAL (2015, Issue 2 (on 3 March 2015))
Title, Abstract, Keywords: contracept* OR family planning AND Title, Abstract, Keywords: counsel* OR communicat* OR educat* OR information disseminat* OR intervention OR choice OR choose OR use AND Title, Abstract, Keywords: postpartum OR post‐partum OR postnatal OR repeat pregnancy OR mothers
POPLINE (3 March 2015)
All fields: counsel* OR educat* or communicat* OR information dissemination OR choice OR choose OR use Keyword: Contraception AND Keyword: Postpartum Filter by keyword: Research report
CINAHL (2 December 2014)
counseling or sex education or client education or health promotion or teaching or counsel* or debrief* or educat* or teach* AND postnatal period or postnatal* or post?natal* or postpartum or post?partum or post‐partum or postpartal* or maternity or maternal or mother* or puerperium AND birth control or contraceptive devices or family planning or sterilization?sex or (family n6 planning) or contracept* or (pregnan* n6 prevent*) or (birth n6 control) AND clinical trial* or clinical stud* or randomized n controlled n trial* or randomised n controlled n trial* or random*
Published Date: 20120101‐20141231
Web of Science (2 December 2014)
TOPIC:(contracept*) AND TOPIC: (educat* OR counsel* OR communicat* OR "information dissemination" OR intervention* OR choice OR choose OR use) AND TOPIC: (postpartum OR postnatal) Refined by: DOCUMENT TYPES: ( ARTICLE OR MEETING ABSTRACT OR PROCEEDINGS PAPER ) Timespan: 2012‐2014 Indexes: SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH
ClinicalTrials.gov (2 December 2014)
Search terms: (postpartum OR post‐partum OR postnatal OR repeat pregnancy) AND (contraceptive OR contraception OR births OR home visit* OR family planning) Study type: Interventional Conditions: NOT (preterm OR low birth weight OR HIV OR PCOS OR labor OR congenital OR influenza OR drug OR diabetes) Interventions: NOT (insertion OR supplement* OR caesarean) Title acronym/Titles: NOT (depression OR violence OR exercise OR IVF OR chlamydia OR immunization OR smokers OR smoking OR smoke OR preeclampsia OR pain OR obese OR obesity OR weight OR nutrition) Gender: Studies with female participants First received: 01/01/2012 to 12/02/2014
ICTRP (3 March 2015)
Title: postpartum OR post‐partum OR postnatal OR maternal OR maternity OR mothers OR repeat pregnancy Intervention: contraceptive OR contraception OR births OR home visits OR family planning Recruitment status: All Date of registration: 1 January 2012 to 3 March 2015
Appendix 2. Previous searches
2012
MEDLINE via PubMed (01 January 2009 to 29 May 2012)
("Contraception"[Mesh] OR "Contraception Behavior"[Mesh] OR "Contraceptive Agents"[Mesh] OR "Contraceptive Devices"[Mesh] OR "family planning") AND (educat* OR counsel* OR communicat* OR "information dissemination" OR intervention* OR choice OR choose OR use) AND ("Postpartum Period"[Mesh] OR "Postnatal Care"[Mesh] OR postpartum OR post‐partum OR postnatal) Limits Activated: Clinical Trial, Randomized Controlled Trial
CENTRAL (2009 to 29 May 2012)
contracept* OR family planning in Title, Abstract or Keywords AND counsel* OR communicat* OR educat* OR information disseminat* OR intervention OR choice OR choose OR use in Title, Abstract or Keywords AND postpartum OR post‐partum OR postnatal in Title, Abstract or Keywords
POPLINE (2009 to 29 May 2012)
title/keyword ‐(counseling/clinic activities/counselors/family planning education/health education/population education/family planning program*/sex education/family planning center*/teaching material*/counsel*/debrief*/educat*/teach*/birth control*/ family planning) & (postpartum program*/puerperium/postpartum women/maternal‐child health service*/maternal health service*/postnatal*/post‐partum/postpartum/postpartal*/puerperium/maternity/maternal/mother*) & (clinical trial/random*) OR abstract ‐(counseling/clinic activities/counselors/family planning education/health education/population education/family planning program*/sex education/family planning center*/teaching material*/counsel*/debrief*/educat*/teach*/birth control*/ family planning) & (postpartum program*/puerperium/postpartum women/maternal‐child health service*/maternal health service*/postnatal*/post‐partum/postpartum/postpartal*/puerperium/maternity/maternal/mother*) & (clinical trial/random*)
CINAHL (through Ebscohost) (2009 to 30 May 2012)
counseling or sex education or client education or health promotion or teaching or counsel* or debrief* or educat* or teach* AND postnatal period or postnatal* or post?natal* or postpartum or post?partum or post‐partum or postpartal* or maternity or maternal or mother* or puerperium AND birth control or contraceptive devices or family planning or sterilization?sex or (family n6 planning) or contracept* or (pregnan* n6 prevent*) or (birth n6 control) AND clinical trial* or clinical stud* or randomized n controlled n trial* or randomised n controlled n trial* or random*
PsycINFO (2009 to 30 May 2012)
(counseling or sex education or client education or health promotion or teaching or counsel* or debrief* or educat* or teach*) AND (postnatal period or postnatal* or post?natal* or postpartum or post?partum or post‐partum or postpartal* or maternity or maternal or mother* or puerperium) AND (birth control or contraceptive device* or contraceptive agent* or "family planning" or sterilization?sex or family N6 planning or contracept* or pregnan* N6 prevent* or birth N6 control) AND (clinical trial* or clinical stud* or randomized N1 controlled N1 trial* or randomised N1 controlled N1 trial* or random*)
ClinicalTrials.gov (29 May 2012)
Search terms: (postpartum OR post‐partum OR postnatal OR matern* OR mothers) AND (contraceptive OR contraception OR births OR home visit* OR family planning) Conditions: NOT (preterm OR low birth weight OR HIV OR pregnancy OR labor OR congenital OR influenza OR drug) Interventions: NOT (insertion OR supplement* OR caesarean)
ICTRP (29 May 2012)
Title: postpartum OR post‐partum OR postnatal OR maternal OR maternity OR mothers Condition: NOT (preterm OR low birth weight OR HIV OR pregnancy) Intervention: (contraceptive OR contraception OR births OR home visits OR family planning)
2009
MEDLINE via Pubmed (20 May 2009)
("Contraception"[Mesh] OR "Contraception Behavior"[Mesh] OR "Contraceptive Agents"[Mesh] OR "Contraceptive Devices"[Mesh] OR "family planning") AND (educat* OR counsel* OR communicat* OR "information dissemination" OR intervention* OR choice OR choose OR use) AND ("Postpartum Period"[Mesh] OR "Postnatal Care"[Mesh] OR postpartum OR post‐partum OR postnatal) AND (Clinical Trial[ptyp] OR Randomized Controlled Trial[ptyp] OR Clinical Trial, Phase I[ptyp] OR Clinical Trial, Phase II[ptyp] OR Clinical Trial, Phase III[ptyp] OR Clinical Trial, Phase IV[ptyp] OR Comparative Study[ptyp] OR Controlled Clinical Trial[ptyp] OR Evaluation Studies[ptyp])
CENTRAL (20 May 2009)
contracept* OR family planning in Title, Abstract or Keywords AND counsel* OR communicat* OR educat* OR information disseminat* OR intervention OR choice OR choose OR use in Title, Abstract or Keywords AND postpartum OR post‐partum OR postnatal in Title, Abstract or Keywords
EMBASE (19 February 2009)
1. exp COUNSELING/ 2. exp HEALTH EDUCATION/ 3. SEXUAL EDUCATION/ or TEACHING/ or PATIENT SATISFACTION/ 4. (counsel$ or debrief$ or educat$ or teach$).ti,ab. 5. 1 or 2 or 3 or 4 6. exp POSTNATAL CARE/ 7. exp MATERNAL CARE/ 8. MATERNAL BEHAVIOR/ 9. HOSPITAL DISCHARGE/ 10. (postnatal$ or postpartum or post‐partum or post partum or postpartal$).ti,ab. 11. (maternity or maternal or mother$).ti,ab. 12. puerperium.ti,ab. 13. 6 or 7 or 8 or 9 or 10 or 11 or 12 14. exp BIRTH CONTROL/ or exp CONTRACEPTION/ 15. exp CONTRACEPTIVE DEVICE or exp CONTRACEPTIVE AGENT/ 16. exp GESTAGEN/ 17. ((family adj6 planning) or contracept$ or (pregnan$ adj6 prevent$)).ti,ab. 18. (birth adj6 control).ti,ab. 19. 14 or 15 or 16 or 17 or 18 20. 5 and 13 and 19 21. CLINICAL STUDY/ or CLINICAL ARTICLE/ or CASE CONTROL STUDY/ or LONGITUDINAL STUDY/ or MAJOR CLINICAL STUDY/ or PROSPECTIVE STUDY/ or CLINICAL TRIAL/ or MULTICENTER STUDY/ or PHASE 3 CLINICAL TRIAL/ or PHASE 4 CLINICAL TRIAL/ or RANDOMIZED CONTROLLED TRIAL/ or CONTROLLED STUDY/ or CROSSOVER PROCEDURE/ or DOUBLE BLIND PROCEDURE/ or INTERMETHOD COMPARISON/ or SINGLE BLIND PROCEDURE/ or PLACEBO/ 22. (allocat$ or assign$ or compar$ or control$ or cross over$ or crossover$ or factorial$ or latin square or latin‐square or followup or follow up or placebo$ or prospective$ or random$ or trial$ or versus or vs).ti,ab. 23. (clinic$ adj25 study).ti,ab. 24. (clinic$ adj25 trial).ti,ab. 25. (singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).ti,ab. 26. 21 or 22 or 23 or 24 or 25 27. NONHUMAN/ OR ANIMAL/ OR ANIMAL EXPERIMENT/ 28. HUMAN/ AND (NONHUMAN/ OR ANIMAL OR ANIMAL EXPERIMENTATION/) 29. 27 not 28 30. 26 not 29 31. 20 and 30
POPLINE (19 February 2009)
title/keyword ‐(counseling/clinic activities/counselors/family planning education/health education/population education/family planning program*/sex education/family planning center*/teaching material*/counsel*/debrief*/educat*/teach*/birth control*/ family planning) & (postpartum program*/puerperium/postpartum women/maternal‐child health service*/maternal health service*/postnatal*/post‐partum/postpartum/postpartal*/puerperium/maternity/maternal/mother*) & (clinical trial/random*) OR abstract ‐(counseling/clinic activities/counselors/family planning education/health education/population education/family planning program*/sex education/family planning center*/teaching material*/counsel*/debrief*/educat*/teach*/birth control*/ family planning) & (postpartum program*/puerperium/postpartum women/maternal‐child health service*/maternal health service*/postnatal*/post‐partum/postpartum/postpartal*/puerperium/maternity/maternal/mother*) & (clinical trial/random*)
CINAHL (19 February 2009)
counseling or sex education or client education or health promotion or teaching or counsel* or debrief* or educat* or teach* AND postnatal period or postnatal* or post?natal* or postpartum or post?partum or post‐partum or postpartal* or maternity or maternal or mother* or puerperium AND birth control or contraceptive devices or family planning or sterilization?sex or (family n6 planning) or contracept* or (pregnan* n6 prevent*) or (birth n6 control) AND clinical trial* or clinical stud* or randomized n controlled n trial* or randomised n controlled n trial* or random*
PsycINFO (19 February 2009)
(counseling or sex education or client education or health promotion or teaching or counsel* or debrief* or educat* or teach*) AND (postnatal period or postnatal* or post?natal* or postpartum or post?partum or post‐partum or postpartal* or maternity or maternal or mother* or puerperium) AND (birth control or contraceptive device* or contraceptive agent* or "family planning" or sterilization?sex or family N6 planning or contracept* or pregnan* N6 prevent* or birth N6 control) AND (clinical trial* or clinical stud* or randomized N1 controlled N1 trial* or randomised N1 controlled N1 trial* or random*)
ClinicalTrials.gov (16 June 2009)
Search terms: postpartum OR post‐partum OR postnatal OR matern* OR mothers Conditions: NOT (preterm OR low birth weight OR HIV OR pregnancy) Interventions: (contraceptive OR contraception OR births OR home visit* OR family planning) NOT (insertion OR supplement* OR caesarean)
ICTRP (16 June 2009)
Title: postpartum OR post‐partum OR postnatal OR maternal OR maternity OR mothers Condition: NOT (preterm OR low birth weight OR HIV OR pregnancy) Intervention: (contraceptive OR contraception OR births OR home visits OR family planning)
2001
MEDLINE OvidWeb (1966 to 2001 August) and The Cochrane Controlled Trials Register
1. COUNSELING/ 2. SEX COUNSELING/ 3. PATIENT EDUCATION/ 4. HEALTH EDUCATION/ 5. HEALTH PROMOTION/ 6. exp TEACHING/ 7. (counsel$ or debrief$ or educat$ or teach$).ti,ab. 8. 1 or 2 or 3 or 4 or 5 or 6 or 7 9. POSTNATAL CARE/ 10. exp PUERPERIUM/ 11. MATERNAL HEALTH SERVICES/ 12. MATERNAL‐CHILD HEALTH CENTERS/ 13. MATERNAL BEHAVIOR/ 14. PATIENT DISCHARGE/ 15. (postnatal$ or post‐partum or postpartum or post partum or postpartal$).ti,ab. 16. (maternity or maternal or mother$).ti,ab. 17. puerperium.ti,ab. 18. discharg$.ti,ab. 19. 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 20. CONTRACEPTION BEHAVIOR/ 21. exp CONTRACEPTION/ 22. exp CONTRACEPTIVE AGENTS/ 23. exp CONTRACEPTIVE DEVICES/ 24. exp FAMILY PLANNING/ 25. FAMILY PLANNING POLICY/ 26. POPULATION CONTROL/ 27. ((family adj6 planning) or contracept$ or (pregnan$ adj6 prevent$)).ti,ab. 28. (birth adj6 control).ti,ab. 29. 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 30. 8 and 19 and 29 31. 30 and human/ 32. RANDOMIZED CONTROLLED TRIAL.pt. 33. CONTROLLED CLINICAL TRIAL.pt. 34. RANDOMIZED CONTROLLED TRIALS/ 35. RANDOM ALLOCATION/ 36. DOUBLE‐BLIND METHOD/ 37. SINGLE‐BLIND METHOD/ 38. CLINICAL TRIAL.pt. 39. exp CLINICAL TRIALS 40. (clin$ adj25 trial$).ti,ab. 41. ((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).ti,ab. 42. PLACEBOS/ 43. (placebo$ or random$).ti,ab. 44. RESEARCH DESIGN/ 45. COMPARATIVE STUDY/ 46. exp EVALUATION STUDIES/ 47. exp CASE‐CONTROL STUDIES/ or exp COHORT STUDIES/ 48. (control$ or prospective$ or volunteer$).ti,ab. 49. (latin square or latin‐square).ti,ab. 50. (cross‐over$ or cross over$).ti,ab. 51. factorial$.ti,ab. 52. CROSS‐OVER STUDIES/ 53. 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 54. (animal not (human and animal)).sh. 55. 53 not 54 56. 55 and 31
N.B. for searching The Cochrane Controlled Trials Register please substitute "*" for "$" and "near" for "adj"
EMBASE, OvidWeb (1980 to 2001 August)
1. exp COUNSELING/ 2. exp HEALTH EDUCATION/ 3. SEXUAL EDUCATION/ or TEACHING/ or PATIENT SATISFACTION/ 4. (counsel$ or debrief$ or educat$ or teach$).ti,ab. 5. 1 or 2 or 3 or 4 6. exp POSTNATAL CARE/ 7. exp MATERNAL CARE/ 8. MATERNAL BEHAVIOR/ 9. HOSPITAL DISCHARGE/ 10. (postnatal$ or postpartum or post‐partum or post partum or postpartal$).ti,ab. 11. (maternity or maternal or mother$).ti,ab. 12. puerperium.ti,ab. 13. 6 or 7 or 8 or 9 or 10 or 11 or 12 14. exp BIRTH CONTROL/ or exp CONTRACEPTION/ 15. exp CONTRACEPTIVE DEVICE or exp CONTRACEPTIVE AGENT/ 16. exp GESTAGEN/ 17. ((family adj6 planning) or contracept$ or (pregnan$ adj6 prevent$)).ti,ab. 18. (birth adj6 control).ti,ab. 19. 14 or 15 or 16 or 17 or 18 20. 5 and 13 and 19 21. CLINICAL STUDY/ or CLINICAL ARTICLE/ or CASE CONTROL STUDY/ or LONGITUDINAL STUDY/ or MAJOR CLINICAL STUDY/ or PROSPECTIVE STUDY/ or CLINICAL TRIAL/ or MULTICENTER STUDY/ or PHASE 3 CLINICAL TRIAL/ or PHASE 4 CLINICAL TRIAL/ or RANDOMIZED CONTROLLED TRIAL/ or CONTROLLED STUDY/ or CROSSOVER PROCEDURE/ or DOUBLE BLIND PROCEDURE/ or INTERMETHOD COMPARISON/ or SINGLE BLIND PROCEDURE/ or PLACEBO/ 22. (allocat$ or assign$ or compar$ or control$ or cross over$ or crossover$ or factorial$ or latin square or latin‐square or followup or follow up or placebo$ or prospective$ or random$ or trial$ or versus or vs).ti,ab. 23. (clinic$ adj25 study).ti,ab. 24. (clinic$ adj25 trial).ti,ab. 25. (singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).ti,ab. 26. 21 or 22 or 23 or 24 or 25 27. NONHUMAN/ OR ANIMAL/ OR ANIMAL EXPERIMENT/ 28. HUMAN/ AND (NONHUMAN/ OR ANIMAL OR ANIMAL EXPERIMENTATION/) 29. 27 not 28 30. 26 not 29 31. 20 and 30
POPLINE (1970 to 2001 August)
1. COUNSELING/ 2. CLINIC ACTIVITIES/ 3. COUNSELORS/ 4. FAMILY PLANNING EDUCATION/ 5. HEALTH EDUCATION/ 6. POPULATION EDUCATION/ 7. FAMILY PLANNING PROGRAMS/ 8. SEX EDUCATION 9. FAMILY PLANNING CENTERS/ 10. TEACHING MATERIALS/ 11. counsel$ or debrief$ or educat$ or teach$ or birth control$ or family planning 12. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 13. POSTPARTUM PROGRAMS/ 14. PUERPERIUM/ 15. POSTPARTUM WOMEN/ 16. MATERNAL‐CHILD HEALTH SERVICES/ 17. MATERNAL HEALTH SERVICES/ 18. postnatal$ or post‐partum or postpartum or postpartal$ or puerperium 19. maternity or maternal or mother$ 20. 13 or 14 or 15 or 16 or 17 or 18 or 19 21. 12 and 20
CINAHL, SliverPlatter (1982 to 2001 October)
1. "Counseling"/ all topical subheadings / all age subheadings 2. "Sexual‐Counseling"/ all topical subheadings / all age subheadings 3. "Patient‐Education"/ all topical subheadings / all age subheadings 4. "Patient‐Discharge‐Education"/ all topical subheadings / all age subheadings 5. "Health‐Education"/ all topical subheadings / all age subheadings 6. "Sex‐Education"/ all topical subheadings / all age subheadings 7. "Health‐Promotion"/ all topical subheadings / all age subheadings 8. "Teaching"/ all topical subheadings / all age subheadings 9. (counsel* or debrief* or educat* or teach*) in ti,ab 10. "Postnatal‐Care"/ all topical subheadings / all age subheadings 11. "Postnatal‐Period"/ all topical subheadings / all age subheadings 12. "Puerperium"/ all topical subheadings / all age subheadings 13. "Maternal‐Health‐Services"/ all topical subheadings / all age subheadings 14. "Maternal‐Child‐Health"/ all topical subheadings / all age subheadings 15. "Maternal‐Behavior"/ all topical subheadings / all age subheadings 16. (postnatal* or post natal* or post‐natal* or post‐partum or post partum or postpartum or postpartal*) in ti,ab 17. (maternity or maternal or mother*) in ti,ab 18. puerperium in ti,ab 19. discharg* in ti,ab 20. #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 21. #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 22. explode "Contraception"/ all topical subheadings / all age subheadings 23. explode "Contraceptive‐Agents"/ all topical subheadings / all age subheadings 24. explode "Contraceptive‐Devices"/ all topical subheadings / all age subheadings 25. explode "Family‐Planning"/ all topical subheadings / all age subheadings 26. ((family near6 planning) or contracept* or (pregnan* near6 prevent*) or (birth near6 control*)) in ti,ab 27. #22 or #23 or #24 or #25 or #26 28. #20 and #21 and #27
PsycINFO SilverPlatter (1899 to 2001 October)
1. "Counseling‐" in DE 2. "Sex‐Education" in DE 3. "Client‐Education" in DE 4. "Health‐Education" in DE 5. "Health‐Promotion" in DE 6. "Teaching‐" in DE 7. (counsel* or debrief* or educat* or teach*) in ti,ab 8. #1 or #2 or #3 or #4 or #5 or #6 or #7 9. "Postnatal‐Period" in DE 10. (postnatal* or post natal* or post‐natal* or postpartum or post partum or post‐partum or postpartal*) in ti,ab 11. (maternity or maternal or mother*) in ti,ab 12. puerperium in ti,ab 13. #9 or #10 or #11 or #12 14. explode "Birth‐Control" 15. explode "Contraceptive‐Devices" 16. "Family‐Planning" in DE 17. explode "Sterilization‐Sex" 18. (family near6 planning) or contracept* or (pregnan* near6 prevent*) or (birth near6 control*) 19. #14 or #15 or #16 or #17 or #18 20. #8 and #13 and #19
SIGLE SilverPlatter (1980 to 2001 June)
1. (counsel* or debrief* or educat* or teach*) 2. postnatal* or post natal* or post‐natal* or postpartum or post partum or post‐partum or postpartal* 3. maternity or maternal or mother* 4. puerperium 5. #2 or #3 or #4 6. (family near6 planning) or contracept* or (pregnan* near6 prevent*) or (birth near6 control*) 7. #1 and #5 and #6
ASSIA Bowker Saur CD‐ROM (1987 to 2001 November)
1. ft=educat$ 2. ft=advice 3. ft=advise$ 4. ft=debrief$ 5. ft=teach$ 6. ft=counsel$ 7. cs=1 or cs=2 or cs=3 or cs=4 or cs=5 or cs=6 8. ft=postpartum 9. ft=postnatal$ 10. ft=puerperium 11. cs=8 or cs=9 or cs=10 12. ft=pregnan$ prevent$ 13. ft=contracept$ 14. ft=family planning 15. ft=abstinen$ 16. ft=birth control$ 17. ft=fertility regulat$ 18. ft=fertility control$ 19. cs=12 or cs=13 or cs=14 or cs=15 or cs=16 or cs=17 or cs=18 20. cs=7 and cs=11 and cs=19 21. cs=7 and cs=11 22. cs=11 and cs=19
Data and analyses
Comparison 1. Oral contraceptive education program (1 session) versus routine counseling.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Continuation of oral contraceptives at one year | 1 | 25 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.11, 3.99] |
| 2 Switched contraceptives by one year | 1 | 25 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.37, 10.92] |
| 3 Known pregnancy by one year | 1 | 25 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.11, 6.04] |
Comparison 2. Contraceptive counseling (1 session) versus no counseling.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Use of any contraceptive at 8 to 12 weeks postpartum | 1 | 600 | Odds Ratio (M‐H, Fixed, 95% CI) | 19.56 [11.65, 32.83] |
| 2 Choice of modern contraceptive (using or plan to use) at 8 to 12 weeks postpartum | 1 | 600 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 18.53 [13.15, 26.12] |
Comparison 3. LARC script (1‐minute) + routine counseling versus routine counseling.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 LARC use after 6 weeks | 1 | 738 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.93, 2.09] |
| 2 Interested in but not using LARC after 6 weeks | 1 | 738 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.31 [0.95, 1.80] |
| 3 Using any contraceptive after 6 weeks | 1 | 734 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.79, 2.08] |
Comparison 4. Focused contraceptive counseling (1 session) versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Use of highly effective contraceptive method at 3 months | 1 | 121 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.23 [1.03, 4.83] |
| 2 Increase in contraceptive knowledge by 3 months | 1 | 121 | Mean Difference (IV, Fixed, 95% CI) | 2.30 [2.00, 2.60] |
Comparison 5. Home visiting: structured versus routine.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Effective use of contraception at 6 months | 1 | 124 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.24 [1.35, 7.79] |
Comparison 6. Home‐based mentoring (multiple visits) versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Second birth by 24 months | 1 | 149 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.17, 1.00] |
Comparison 7. Computer‐assisted motivational interviewing (CAMI) with parenting curriculum versus CAMI‐only versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Repeat birth by 24 months | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 CAMI + parenting curriculum versus usual care | 1 | 148 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.21, 1.11] |
| 1.2 CAMI‐only versus usual care | 1 | 155 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.29, 1.37] |
Comparison 8. Special postpartum care (including contraception) versus routine services (multiple well‐baby contacts).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Repeat pregnancy (self‐report) by 18 months | 1 | 221 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.17, 0.70] |
Comparison 9. Phone counseling + follow‐up versus usual services.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Repeat pregnancy by 24 months | 1 | 249 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.47, 1.35] |
| 2 LARC use at 3 months | 1 | 49 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.38, 4.34] |
Comparison 10. Home visiting: 4 visits versus 1 visit versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Contraception use at 4 months: 4 visits versus 1 visit | 1 | 565 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.89, 1.75] |
| 2 Contraception use at 4 months: 1 visit versus usual care | 1 | 580 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.62, 1.20] |
| 3 Pregnancy (self‐report) at 4 months postpartum: 4 visits versus 1 visit | 1 | 554 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.49 [0.33, 6.74] |
| 4 Pregnancy (self‐report) at 4 months postpartum: 1 visit versus usual care | 1 | 585 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.20, 5.01] |
Comparison 11. Health education (including contraception): immediate, later, or no session.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Contraception use at 3 months: immediate session versus no immediate session | 1 | 402 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.50 [0.88, 2.54] |
| 2 Contraception use at 6 months: immediate session versus no immediate session | 1 | 393 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.62 [1.06, 2.50] |
| 3 Contraception use at 6 months | 1 | 393 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.58, 1.37] |
| 3.1 Immediate + later sessions vs immediate session | 1 | 199 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.48, 1.52] |
| 3.2 Later session vs no session | 1 | 194 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.50, 1.80] |
| 4 Exclusive breastfeeding at 3 months: immediate session versus no immediate session | 1 | 403 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.67, 1.49] |
| 5 Exclusive breastfeeding >= 5 months: immediate session versus no immediate session | 1 | 390 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.65, 1.57] |
| 6 Exclusive breastfeeding >= 5 months | 1 | 390 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.83, 2.00] |
| 6.1 Immediate + later sessions vs immediate session | 1 | 198 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.83, 2.90] |
| 6.2 Later session vs no session | 1 | 192 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.56, 1.99] |
11.5. Analysis.

Comparison 11 Health education (including contraception): immediate, later, or no session, Outcome 5 Exclusive breastfeeding >= 5 months: immediate session versus no immediate session.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Barnet 2009.
| Methods | Location: Baltimore, MD (USA) Recruitment time: February 2003 to October 2007 Sample size calculation and outcome of focus: not specified |
|
| Participants | General with N: 237 pregnant adolescents Source: 5 urban prenatal care clinics providing prenatal care to mainly low‐income African American women without insurance or under Medicaid Inclusion criteria: 12 to 18 years old, pregnancy >= 24 weeks gestation Exclusion criteria: pregnancy did not result in live birth and withdrawn if the infant died in neonatal period, since parenting was an intervention focus. |
|
| Interventions | Computer‐assisted motivational intervention (CAMI) on quarterly basis; motivational interviewing on contraception by CAMI counselors; parenting curriculum from Black 2006 included contraception
1) CAMI+: multi‐component home‐visiting intervention (parent training and case management) 2) CAMI‐only: single component, home‐based intervention 3) Usual care Timing: 6 weeks to 24 months postpartum with maximum of 9 quarterly sessions |
|
| Outcomes | Primary: repeat birth by 24 months postpartum (assessed via Vital Statistics) Secondary: abortion since index child's birth Additional data provided by investigator: losses by arm to help interpret abortion information obtained at 24‐month interview |
|
| Notes | If participant became pregnant, CAMI was stopped because questions on contraception were no longer relevant and program did not allow skipping. Secondary article (Barnet 2010) examined cost‐effectiveness. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly assigned, 'computer‐generated permuted blocks'. Investigator communicated that ratio was 3:3:2, with 6 used for intervention groups and 4 for control. Block size 16 would account for ratio rather than reported block size 6. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Outcome assessment: obtained from Vital Statistics |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up: none for primary outcome (obtained from Vital Statistics) Investigator provided loss by study arm at 24 month‐interview (counts and %): 17% CAMI+, 16% CAMI‐only, 24% Usual care Exclusions after randomization: 1 participant with stillborn infant and 1 whose 2‐month‐old infant died |
Bashour 2008.
| Methods | Location: Damascus, Syria Recruitment time: June to December 2004 Sample size calculation and outcome of focus: Power analysis based on postpartum morbidity, i.e., hemorrhoids: ability to detect decrease from 15% in control to 7% in treatment group. |
|
| Participants | General with N: 903 women who recently gave birth Source: Maternity Teaching Hospital Inclusion criteria: delivered healthy newborn, lived within 30 km of hospital, and available for 6 months Exclusion criteria: delivered prematurely; baby weighed < 2500 g or had congenital anomaly |
|
| Interventions | Home visits to educate and support women who had recently given birth Registered midwives had 5 days of special training for home visits. Breastfeeding was addressed in visits 2 and 3; family planning in visit 4. Three arms: Group A: 4 home visits on days 1, 3, 7, 30 following delivery Group B: visit on day 3, similar to visit to Group A (included breastfeeding but not family planning) Group C: standard of care in Syria (no visit after discharge) |
|
| Outcomes | Primary: contraceptive use and type (pills, IUD, condoms, others) via pre‐tested structured questionnaire; self‐reported pregnancy also reported Secondary: maternal and child morbidities; continuation of breastfeeding; uptake on first vaccines Assessed at 4 months postpartum |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Communication with investigator indicated block size was 21 with 7 assigned to each study arm. Report had indicated randomization in 'blocks of 7...caseload of 21 eligible deliveries per day was assumed.' |
| Allocation concealment (selection bias) | Low risk | Numbered opaque and sealed envelopes; process supervised by midwives not otherwise involved in study. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Midwives who did home visits not blinded. Outcome assessors blinded to assignment; they could tell assignment from interviews but not fully aware of study objectives. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up: 3% (27/903) due to refusals (N = 9) or bad addresses (N = 18); by group: A, 5% (16/301); B, 2% (7/301); C, 1% (4/301) |
Black 2006.
| Methods | Location: Baltimore, MD (USA) Recruitment time: September 1997 to December 1999 Sample size calculation and outcome of focus: not specified |
|
| Participants | General with N: 181 female adolescents were recruited shortly after delivery Source: 3 urban hospitals Inclusion criteria: low income (< 185% poverty level), < 18 years old, first‐time delivery, black race, no indication of cocaine or heroin use in chart, no chronic illness that would interfere with parenting or adolescent development; infant was term (>= 37 weeks) and > 2500 g; infant had no congenital problem, chronic illness, or disability Exclusion criteria: no information |
|
| Interventions | Study focus: delaying second births ‐ parenting, contraception 1) Home‐based curriculum for adolescent mothers, maximum of 19 lessons; participants were seen twice per month until infant's first birthday. Intervention included information about access to birth control, and condoms were provided at each visit. After first 2 visits, facilitators could vary order of sessions, as well as combine or repeat them. 2) Usual care Duration: maximum 19 visits for experimental group at 2 per month (40% had >= 8 visits); evaluation visits at 6, 13, and 24 months for both groups | |
| Outcomes | Primary: second birth by 24 months (assessed in home); contraceptive use presented by second birth rather than by randomized group Secondary: examine second births by greater intervention participation and by risk practice and family formation |
|
| Notes | Unable to obtain data on contraceptive use by study arm | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'Randomization procedure' stratified on maternal age and child's gender |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Loss to follow‐up: overall 18%; intervention 20% (17/87); control 16% (15/94) Exclusions after randomization: excluded from analysis 32 mothers without 24‐month evaluation (17 treatment and 15 control), because intent was to assess second births. Could have had 13‐month evaluations. |
Bolam 1998.
| Methods | Location: Kathmandu, Nepal Recruitment time: November 1994 to May 1996 Sample size calculation and outcome of focus: sample size estimated for range of outcomes; for family planning, sample size based on 20% uptake in control and 33% in experimental group |
|
| Participants | General with N: 540 women Source: public maternity hospital Inclusion criteria: all pregnant women admitted to hospital for delivery who resided in two communities Exclusion criteria: no information |
|
| Interventions | Experimental: individual 20‐minute health education session, interactive and supportive covering infant feeding, treatment of diarrhea, management of acute respiratory infection in infants, immunization, and contraception. Intervention provided before discharge from hospital (some emphasis on exclusive breastfeeding); second education session in home 3 months post‐delivery (some emphasis on family planning). Group A: Health education immediately after birth and at 3 months Group B: Health education immediately after birth Group C: Health education at 3 months Group D: No health education |
|
| Outcomes | Primary: duration of exclusive breast feeding (>= 5 months); contraceptive use at 3 and 6 months postpartum (reported as 1 dichotomous item) Secondary: infant's nutritional status |
|
| Notes | Intervention designed to cover range of important issues for maternal and infant health in Nepal. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Individual women randomly allocated either when in labor or shortly after delivery. Restricted randomization in blocks of 20. |
| Allocation concealment (selection bias) | Low risk | Details in sealed envelopes for consecutively recruited mothers |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Patients and health educators not blinded; outcome assessors blind to group of assignment. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up: 25% at 3 months and 27% at 6 months: main reason, mother moving back to parental home (cultural tradition) Exclusions (withdrawn from study): 10 infant deaths spread across all study arms and 2 stillbirths |
Gilliam 2004.
| Methods | Location: Chicago, IL (USA) Recruitment time: 1998 to 1999 Sample size calculation and outcome of focus: Resources did not permit sample size needed to detect 20% difference between groups. |
|
| Participants | General with N: 33 African American low‐income females Participants enrolled during prenatal care and randomized after delivery. Source: Prentice Ambulatory Care Clinic at Northwestern Memorial Hospital; resident‐run clinic for low‐income women receiving public assistance. Inclusion criteria: <= 25 years old, unplanned pregnancy, intending to use oral contraceptive (OCs) postpartum Exclusion criterion: history of consistent or successful oral contraceptive use prior to pregnancy |
|
| Interventions | Postpartum, one‐time intervention 1) Multi‐component intervention with counseling, videotape about OCs, and written material 2) Resident‐physician counseling (usual care) Follow‐up: 1 year |
|
| Outcomes | Primary: continuation rate; switch to other contraceptives; pregnancy rate (most by self‐report) Assessment of adherence through collection of pill packs and self‐reports; multiple questions for continuation Secondary: knowledge of OCs; data reported in secondary article for total sample, not by study arm (Gilliam 2003) Assessed at 1 year |
|
| Notes | 43 enrolled but only 33 randomized; reasons included participants changing mind about using OCs, delivering at outside hospital, and failure of study team to randomize participant prior to leaving hospital due to miscommunication with nursing staff, or leaving after 24‐hour rather than 48‐hour stay. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers table; randomized following delivery |
| Allocation concealment (selection bias) | Low risk | Study packets in envelopes that "concealed the contents" |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Research team members reportedly blind to group participation; details not provided |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss overall: 17/33 = 52% dropped out by 1 year Pregnancy data for 9 who dropped out via records or contacting participant, leaving data loss at 8/33 = 24% |
Katz 2011.
| Methods | Location: Washington, DC (USA) and adjoining metropolitan area Recruitment time: November 2005 to August 2009 Sample size calculation and outcome of focus: not specified |
|
| Participants | General with N: 249 pregnant or newly parenting teens Source: prenatal clinics and local high schools Inclusion criteria: African American or Latina primiparous pregnant teens, aged 15 to 18 years as well as 19‐year‐olds who had not graduated from high school Exclusion criteria: no information |
|
| Interventions | 1) Intervention group (N = 125): curriculum goal to improve reproductive health planning and motivate teens to delay further childbearing; focused on knowledge of health risks and positive teen attitudes Included sexual partner communication and negotiation, resisting peer pressure for risk behaviors, and connectedness with family, health care provider, school and work; minimal content on parenting. Process: Teens received cell phones for 18 months of counseling sessions and quarterly group sessions. Counselors met with each teen face‐to‐face, provided cell phones, and scheduled weekly counseling calls for first 6 months. Each teen assigned one counselor for study. Biweekly phone sessions scheduled during subsequent 12 months for maximum of 42 sessions over 18 months postpartum. Two‐hour dinner group sessions held quarterly over 2 years at hospitals serving pregnant and parenting teens. 2) Usual care (N = 124): health and education services generally provided through schools or healthcare facilities Duration: 24 months |
|
| Outcomes | Primary: time to subsequent conception Secondary: influence of treatment intensity on subsequent conception Pregnancy status assessed via telephone at 3, 9, 15 and 21 months; confirmed by urine pregnancy test at 6, 12, 18 and 24 months. |
|
| Notes | Analysis according to treatment assignment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table programmed within web‐based data management system; stratified by age group (15 to 17 or >= 18 years) and by hospital of delivery |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Losses: intervention 5 (4%) and control 7 (5.6%) (dropped out < 21 months postpartum or > 3 months before study close) |
O'Sullivan 1992.
| Methods | Location: Eastern USA Recruitment time: not specified Sample size calculation and outcome of focus: not specified; 'random assignment to experimental and control groups was used, resulting in sample size that would yield adequate statistical power' |
|
| Participants | General with N: 243 postpartum teenagers Source: large urban teaching hospital Inclusion criteria: <= 17 years old, delivered healthy baby at specified hospital, no previous children (previous pregnancy acceptable) Exclusion criterion: planned to place child for adoption. All participants were single, African American, and received Medicaid. |
|
| Interventions | Special care versus routine well‐baby care 1) Special care: clinic directed by nurse practitioner and staffed by pediatrician, another nurse practitioner, and social worker; goals of preventing repeat pregnancy, mother's return to school, up‐to‐date immunizations for infant, and less use of emergency care for infant; reminder phone calls and letters for appointments 2) Routine care: 8 appointments from 2 weeks postpartum to 18 months Assessment at 18 months |
|
| Outcomes | Primary: repeat pregnancy (self‐report) and return to school by interview; attendance at clinic, full immunization, and emergency room visit by chart review Secondary: no mention |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Programs had high dropout rates, but 91% overall were located for 18‐month interview. Program dropouts: by 6 months, 37% experimental and 63% routine care; by 18 months, 60% experimental and 82% routine care |
Quinlivan 2003.
| Methods | Location: Australia Recruitment time: July 1998 to December 2000 Sample size calculation and outcome of focus: sample size estimate based on ability to detect increase in knowledge score |
|
| Participants | General with N: 139 teenagers enrolled prenatally; randomized immediately after delivery Source: teenage pregnancy clinic for first‐time mothers Inclusion criteria: < 18 years old, speak English, intend to continue with pregnancy and to keep infant Exclusion criteria: living > 150 km from hospital or known fetal abnormality |
|
| Interventions | 1) Routine services plus structured home visits (1 to 4 hours each) from nurse midwives at week 1 and 2 and at months 1, 2, 4, and 6 2) Routine postnatal support, counseling, and information from hospital, including access to routine home‐visiting |
|
| Outcomes | Primary: knowledge regarding contraception and breastfeeding; insufficient data available for analysis here Secondary: effective use of contraception (following manufacturer's guidelines and without use of emergency contraception) Assessment at 6 months |
|
| Notes | Due to age of study (conducted 1998 to 2000), we did not request additional data from investigator. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Generated by computer' |
| Allocation concealment (selection bias) | Low risk | Numbered, sealed, opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up: none Overall loss: 9% (12/136 randomized); 11 withdrawals due to adverse neonatal outcomes (9 in group with no home visit) and 1 consent withdrawn (home visit group) |
Saeed 2008.
| Methods | Location: Islamabad, Pakistan Recruitment time: February 2006 to September 2007 Sample size calculation and outcome of focus: no information |
|
| Participants | General with N: 648 women Source: Shifa International Hospital Inclusion criteria: admitted to labor ward after delivery, regardless of pregnancy duration, delivery mode or fetal outcome Exclusion criteria: no information |
|
| Interventions | 1) 20‐minute informal counseling on contraception in presence of husband or other close relative; didactic approach with opportunity to ask questions; one‐page pamphlet on contraceptive methods; 40‐minute training for providers on counseling leaflet and interview methods 2) No counseling or pamphlet | |
| Outcomes | Primary: contraceptive use postpartum (any being used or planned; method chosen) For this review, we examined modern contraceptive use, excluding coitus interruptus. Secondary: no mention Follow‐up at 8 to 12 weeks postpartum; no indication of standard questions for follow‐up though initial assessment was standardized |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomized into 2 groups by "block of 4 randomization charts" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Physician recording follow‐up data was blinded to study arms. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Losses to follow‐up: 48/648 (7.4%); complete data for 299 intervention and 301 control women |
Simmons 2013.
| Methods | Location: Portland, Oregon (USA) Recruitment time: May 2011 to November 2011 Sample size calculation and outcome of focus: based on 75% LARC use by 3 months in intervention group as per published report; 25 in each group for 90% power to detect 50% difference at alpha .05 |
|
| Participants | General with N: 50 women with public insurance Source: postpartum unit at Oregon Health & Science University (OHSU) Inclusion: 18 to 38 years old, speak English or Spanish, received prenatal care through OHSU resident clinic, and stated intention to use LARC (etonogestrel implant, levonorgestrel IUS, or copper IUD) Exclusion: did not meet inclusion criteria or incarcerated at time of delivery and unable to return for follow‐up |
|
| Interventions | All women had routine contraceptive counseling during prenatal care and contraceptive plan prior to delivery. 1) Intervention: additional assistance from contraceptive 'personal assistants' who had contraceptive counseling experience; phone call 2 weeks after discharge to confirm LARC interest, answer questions, provide counseling as needed, schedule postpartum visit; 3 days prior to appointment, phone call reminder and logistical support; if appointment missed, 1 to 3 more calls and additional targeting counseling as needed 2) Control: routine postpartum follow‐up, including scheduling own 6‐week appointment |
|
| Outcomes | Primary: self‐reported placement of LARC; risk factors for non‐uptake of LARC in postpartum period LARC placed at 4‐ to 6‐week postpartum visit Secondary: identify risk factors for no uptake of LARC in postpartum period Assessment by phone questionnaire at 3 months postpartum |
|
| Notes | LARC not provided in study to ensure observed effect related to intervention and not to removal of financial barriers. IUC: LNG‐IUS; Copper T380; etonogestrel implant |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme in 1:1 ratio |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Placement of LARC occurred at routine postpartum clinic visit (4 to 6 weeks postpartum). Providers not aware of participants being in study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up: intervention 0/25; control 1/25 (4%) did not plan for LARC (excluded after randomization) |
Tang 2014.
| Methods | Location: Raleigh, North Carolina (USA) Recruitment time: May 2011 to January 2012 Sample size calculation and outcome of focus: Assumed 20% LARC use in control, based on state survey results. Analysis population of 626 (313 in each arm) required for 80% power using two‐side alpha .05 to detect 10% increase to 30% LARC use in intervention arm. Assuming 20% drop‐out rate, 800 planned. |
|
| Participants | General with N: 800 healthy postpartum women Source: WakeMed Hospital Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | 1) Intervention: routine postpartum counseling plus one‐minute script (LARC script), given to women during postpartum admission. Script informs about long‐acting reversible contraceptive (LARC) methods, i.e., contraceptive implant and IUD 2) Control: routine postpartum counseling (no LARC script and no standard counseling) |
|
| Outcomes | Primary: self‐reported LARC use Secondary: self‐reported interest in LARC use; use of any contraceptive method; reasons for not using contraceptive method of choice Assessment by 10‐min phone survey (25 items) after 6‐week postpartum visit |
|
| Notes | Due to error in preparing allocation envelopes, 394 allocated to LARC script (15 incorrectly) and 403 to no LARC script (19 incorrectly). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Simple 1:1 randomization scheme by computer generated blocks of 6, 8 and 10; developed and stored by statistician at North Carolina Translational and Clinical Sciences Institute |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, opaque, sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double blind (investigator and outcomes assessor); research assistants who opened allocation envelope were not same as those who completed participant follow‐up survey. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up: intervention 31/400 (8%); control 31/400 (8%) |
Torres 2014.
| Methods | Location: Salt Lake City, Utah (USA), university hospital Recruitment time: April 2013 to October 2014 Sample size calculation and outcome of focus: no mention |
|
| Participants | General with N: 121 women to date of 362 planned; age 14 to 50 years Inclusion criteria: deliver premature infant at study institution; gestational age between 24 weeks 0 days and 36 weeks 6 days Exclusion criteria: delivered via cesarean section and had sterilization procedure at time of cesarean section |
|
| Interventions | 1) Focused contraceptive counseling with written, structured script describing all contraceptive methods in rank order, from most effective to least effective in preventing pregnancy; abstract mentions facilitating access to desired contraceptive method 2) Standard postpartum contraceptive counseling for all patients at hospital |
|
| Outcomes | Primary: use of highly effective contraceptive method at 3 months postpartum Secondary: pregnancy and use of highly effective method; assessed at 12, 24, and 36 months |
|
| Notes | Preliminary results from conference abstract and study information from ClinicalTrials.gov; primary outcomes assessed mid‐2014; study to be completed mid‐year 2016 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No mention |
| Allocation concealment (selection bias) | Unclear risk | No mention |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Loss to follow‐up: no mention; unknown number randomized; analyzed data from 121 women followed for 3 months |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adanikin 2013 | Not exclusively postpartum |
| Barnet 2007 | Intervention began in third trimester of pregnancy |
| Christie 2011 | No mention of contraception |
| El‐Kamary 2004 | Family planning only had to be provided within 12‐month period of program for 90% of clients. Therefore, contraception education was not an integral part of intervention. |
| FHI 360 2013 | Intervention did not begin within one month postpartum. Women were 6 to 12 months postpartum. |
| Foreit 1993 | Two maternity floors and associated outpatient clinics were randomly selected and randomly assigned to treatment and control groups. Women were assigned to a maternity floor based on availability. Analysis could not be adjusted for cluster assignment with only two units (floors). |
| Lee 2007 | Assignment adapted from Sayegh 1976. Coin flip determined which rooms were assigned to program first. Even‐numbered rooms were experimental group and odd‐numbered were control group. Cluster assignment (by room) not addressed in analysis. |
| Lee 2011 | Assignment adapted from Sayegh 1976 and similar to that used in Lee 2007. Odd‐numbered wards were experimental group and were divided in half (wards 1, 3, 5, 7, 11 and wards 13, 15, 17, 19, 21, 23). Even numbered wards were control group. Coin flip determined which half of experimental group received program first; midway through the study, other half received program. Rooms with double occupancy were assigned as unit. Cluster assignment (by room) not addressed in analysis. |
| Nacar 2003 | Allocation likely to have been alternate. Questionnaire about eligibility criteria was administered to intervention and control groups on alternate days. The intervention was given immediately following questionnaire. |
| Norr 2003 | No apparent education on contraception |
| Olds 2002 | Enrolled prenatally; no clear starting point for home visits after delivery; could have been a month or longer. |
| Omu 1989 | Intervention began during pregnancy. |
| Proctor 2006 | Report did not include data for our primary outcomes; focused on participant satisfaction with counseling method. Trial also assessed type of contraceptive used after counseling, but report only presented results in figure without actual numbers. |
| Ransjo‐Arvidson 1998 | No apparent education on contraception (no standard health education) |
| Sayegh 1976 | Alternate rooms allocated to educational program using a coin toss to determine starting point. Patients were allocated to 1 of 10 rooms (2 beds each) based on availability. Cluster assignment (by room) not addressed in analysis. |
| Smith 2002 | Experimental group did not receive education postpartum (only prenatally). Some controls (standard local counseling) had some postpartum education. |
Characteristics of ongoing studies [ordered by study ID]
Sadler 2014.
| Trial name or title | Minding the baby home visiting: program evaluation |
| Methods | Randomized trial, single blind (outcomes assessor) parallel assignment at two sites in New Haven, CT (USA) |
| Participants | 150 first‐time mothers, age 14 to 25 years Inclusion criteria: having a first child, speak English, and obtain primary care from community health center Exclusion criteria: no psychosis or terminal illness |
| Interventions | Experimental: weekly home visits for one year, followed by bi‐weekly home visits until child is 24 months of age, provided to young at‐risk families by team of nurse practitioner and social worker home visitors No Intervention: routine primary care at community health center |
| Outcomes | Primary: maternal life course outcomes (delay rapid subsequent childbearing within 24 months of older child's birth), as well as maternal reflective capacities, infant attachment, and child abuse or neglect Secondary: dose of intervention, cost analysis for program, and description of reflective functioning in pregnant adolescents |
| Starting date | Sep 2009; estimated completion Aug 2014 |
| Contact information | Patricia Miller: 1‐203‐785‐5589; patricia.miller@yale.edu Andrea Miller: 1‐203‐785‐5589; andrea.miller@yale.edu |
| Notes | ClinicalTrials.gov last updated 13 June 2014 |
Schreiber 2013.
| Trial name or title | Adolescent Postpartum Contraceptive Counseling Intervention (PPCI) |
| Methods | Randomized open label parallel assignment study |
| Participants | Women 14 to 19 years old Inclusion criteria: 14 to 19 years old, primiparous, immediately postpartum, delivery of a full term live singleton infant (> 37 weeks at Hospital of the University of Pennsylvania (HUP) Exclusion criteria: not planning to reside in or near Philadelphia for next year |
| Interventions | Experimental: brief in‐person standardized contraceptive counseling intervention that included empowerment messaging and instrument to clarify participants' preferences for contraception in terms of future childbearing goals Control: routine postpartum contraceptive counseling |
| Outcomes | Primary: repeat pregnancy at 1 year Secondary: contraceptive choice, use and continuation rates; contraceptive satisfaction |
| Starting date | March 2012; estimated completion December 2013 |
| Contact information | Courtney Schreiber: 1‐215‐615‐6531; corischreiber@yahoo.com |
| Notes | ClinicalTrials.gov last updated 3 June 2014 |
Contributions of authors
2015: L Lopez ran the searches, conducted the secondary data extraction, and incorporated the new trials into the manuscript. T Grey helped review search results, examined study reports for eligibility, and conducted the primary data extraction for new trials. M Chen reviewed and commented on trial implementation and statistical issues. J Hiller reviewed and commented on the manuscript.
2012: L Lopez reviewed the search results, conducted the primary data extraction, incorporated the trials into the report, and drafted the revised manuscript. M Chen reviewed the methods and interpretation of results. J Hiller reviewed the quality assessment information. DA Grimes, formerly of FHI 360, identified another ongoing trial. All authors reviewed and commented on the manuscript.
2009: L Lopez reviewed the search results, conducted the primary data abstraction, incorporated the trials into the report, and drafted the revised manuscript. J Hiller provided input on the inclusion and exclusion criteria for trials and edited the manuscript. D Grimes, formerly of FHI 360, conducted the second data abstraction, checked the data entry, and edited the manuscript. M Chen provided statistical consultation on cluster randomized trials.
1999: J Hiller and E Griffith contributed to the protocol preparation. J Hiller, E Griffith, and F Jenner examined trials found after the literature search and the finalization of the report. J Hiller and E Griffith abstracted data. J Hiller was responsible for the literature search, examination of literature used for background information, input of the data, and drafting the report through 2002.
Sources of support
Internal sources
Adelaide University (JEH, through 2002), Australia.
Health Services Research Unit, University of Aberdeen (JEH, 1997), UK.
External sources
-
National Institute of Child Health and Human Development, USA.
2009 to 2015: Support for conducting the review and updates at FHI 360
-
U.S. Agency for International Development, USA.
2009 to 2012: Support for conducting the review and updates at FHI 360
-
Cochrane Health Promotion and Public Health Field, Australia.
Through 2002: Support for conducting the review (JEH)
Declarations of interest
None known
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Barnet 2009 {published data only}
- Barnet B, Liu J, DeVoe M, Duggan AK, Gold MA, Pecukonis E. Motivational intervention to reduce rapid subsequent births to adolescent mothers: a community‐based randomized trial. Annals of Family Medicine 2009; Vol. 5, issue (3):436‐45. [DOI] [PMC free article] [PubMed]
- Barnet B, Rapp T, DeVoe M, Mullins CD. Cost‐effectiveness of a motivational intervention to reduce rapid repeated childbearing in high‐risk adolescent mothers: a rebirth of economic and policy considerations. Archives of Pediatrics & Adolescent Medicine 2010; Vol. 164, issue 4:370‐6. [DOI] [PubMed]
Bashour 2008 {published data only}
- Bashour HN, Kharouf MH, Abdulsalam AA, Asmar K, Tabbaa MA, Cheikha SA. Effect of postnatal home visits on maternal/infant outcomes in Syria: a randomized controlled trial. Public Health Nursing 2008;25(2):115‐25. [DOI] [PubMed] [Google Scholar]
Black 2006 {published data only (unpublished sought but not used)}
- Black MM, Bentley ME, Papas MA, Oberlander S, Teti LO, McNary S, et al. Delaying second births among adolescent mothers: a randomized, controlled trial of a home‐based mentoring program. Pediatrics 2006;118(4):e1087‐99. [DOI] [PubMed] [Google Scholar]
- Black MM, Siegel EH, Abel Y, Bentley ME. Home and videotape intervention delays early complementary feeding among adolescent mothers. Pediatrics 2001;107(5):e67. [DOI] [PubMed] [Google Scholar]
Bolam 1998 {published data only}
- Bolam A, Manandhar DS, Shreshtha P, Ellis M, Costello AM. The effects of postnatal health education for mothers on infant care and family planning practices in Nepal: a randomised controlled trial. British Medical Journal 1998;316(7134):805‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gilliam 2004 {published data only}
- Gilliam M, Knight S, McCarthy M. Success with oral contraceptives: a pilot study. Contraception 2004;69(5):413‐8. [DOI] [PubMed] [Google Scholar]
- Gilliam ML, Knight S, McCarthy M. Importance and knowledge of oral contraceptives in antepartum, low‐income, African American adolescents. Journal of pediatric and adolescent gynecology 2003;16(6):355‐60. [PUBMED: 14642956] [DOI] [PubMed] [Google Scholar]
Katz 2011 {published data only}
O'Sullivan 1992 {published data only}
- O'Sullivan AL, Jacobsen BS. A randomized trial of a health care program for first‐time adolescent mothers and their infants. Nursing Research 1992;41(4):210‐5. [PubMed] [Google Scholar]
Quinlivan 2003 {published data only}
- Quinlivan JA Box H, Evans SF. Postnatal home visits in teenage mothers: a randomised controlled trial. Lancet 2003;361(9361):893‐900. [DOI] [PubMed] [Google Scholar]
Saeed 2008 {published data only}
- Saeed GA, Fakhar S, Rahim F, Tabassum S. Change in trend of contraceptive uptake‐‐effect of educational leaflets and counseling. Contraception 2008;77(5):377‐81. [DOI] [PubMed] [Google Scholar]
Simmons 2013 {published data only}
- Simmons K, Edelman A, Yanit K, Li H, Jensen J. Effect of personalized contraceptive assistance on uptake of long‐acting reversible contraceptives (LARC) by postpartum women. Contraception 2012;86(3):320. [DOI] [PubMed] [Google Scholar]
- Simmons KB, Edelman AB, Li H, Yanit K E, Jensen JT. Personalized contraceptive assistance and uptake of long‐acting, reversible contraceptives by postpartum women: a randomized, controlled trial. Contraception 2013;88(1):45‐51. [DOI] [PubMed] [Google Scholar]
Tang 2014 {published data only}
- Tang J, Stuart G. Barriers to receiving long‐acting reversible contraception in the postpartum period. Contraception 2013;88(3):437. [DOI] [PubMed] [Google Scholar]
- Tang JH, Dominik R, Re S, Brody S, Stuart GS. Characteristics associated with interest in long‐acting reversible contraception in a postpartum population. Contraception 2013;88(1):52‐7. [DOI] [PubMed] [Google Scholar]
- Tang JH, Dominik RC, Zerden ML, Verbiest SB, Brody SC, Stuart GS. Effect of an educational script on postpartum contraceptive use: A randomized controlled trial. Contraception 2014;90(2):162‐7. [DOI] [PubMed] [Google Scholar]
Torres 2014 {published data only}
- Torres L, Turok DK, Sander J, Clark E, Godfrey E. Focused contraceptive counseling and case management versus usual care in women postpartum from a preterm birth: a randomized controlled trial. Contraception 2014;90(3):317. [Google Scholar]
- Turok DK. Optimizing Postpartum Contraception in Women with Preterm Births. https://clinicaltrials.gov/ct2/show/NCT01864629 (accessed 19 February 2015).
References to studies excluded from this review
Adanikin 2013 {published data only}
- Adanikin AI, Onwudiegwu U, Loto OM. Influence of multiple antenatal counselling sessions on modern contraceptive uptake in Nigeria. European Journal of Contraception and Reproductive Health Care 2013;18(5):381‐7. [DOI] [PubMed] [Google Scholar]
Barnet 2007 {published data only}
- Barnet B, Liu J, DeVoe M, Alperovitz‐Bichell K, Duggan AK. Home visiting for adolescent mothers: effects on parenting, maternal life course, and primary care linkage. Annals of Family Medicine 2007;5(3):224‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Christie 2011 {published data only}
El‐Kamary 2004 {published data only}
- El‐Kamary SS, Higman SM, Fuddy L, McFarlane E, Sia C, Duggan AK. Hawaii's healthy start home visiting program: determinants and impact of rapid repeat birth. Pediatrics 2004;114(3):e317‐26. [DOI] [PubMed] [Google Scholar]
FHI 360 2013 {published data only}
- Dulli L. Postpartum family planning service through enhanced family planning in immunization services (PPFP‐IZ). http://clinicaltrials.gov/ct2/show/NCT01115361 (accessed 6 March 2014). [NCT01115361]
- FHI 360. Research Findings: Integration of Postpartum Family Planning with Child Immunization Services in Rwanda. Research Triangle Park, NC: FHI 360/Headquarters; 2013 Aug.
Foreit 1993 {published data only (unpublished sought but not used)}
- Foreit KG, Foreit JR, Lagos G, Guzman A. Effectiveness and cost effectiveness of postpartum IUD insertion in Lima, Peru. International Family Planning Perspectives 1993;19:19‐24. [Google Scholar]
- Guzman A, Lagos G, Herrera J, Foreit JR. Immediate post‐partum and post‐abortion family planning program.. Final Report. Profamilia and Instituto Peruano del Seguro Social (IPSS). (Project supported by the Population Council and funded by the US Agency for International Development, Office of Population, under contract number AID/DPE‐3030‐000‐4074‐00, Operations Research to Improve Family Planning Maternal‐Child Health Services Delivery Systems in Latin America and the Caribbean (INOPAL) 1990.
Lee 2007 {published data only}
- Lee JT Yen HW. Randomized controlled evaluation of a theory‐based postpartum sexual health education programme. Journal of Advanced Nursing 2007;60(4):389‐401. [DOI] [PubMed] [Google Scholar]
Lee 2011 {published data only}
Nacar 2003 {published data only}
- Nacar M Ozturk A, Ozturk Y. [The effect of family planning education given during postpartum period on the use of contraceptive methods]. Erciyes Tip Dergisi 2003;25:122‐30. [Google Scholar]
Norr 2003 {published data only}
- Norr KF, Crittenden KS, Lehrer EL, Reyes O, Boyd CB, Nacion KW, et al. Maternal and infant outcomes at one year for a nurse‐health advocate home visiting program serving African Americans and Mexican Americans. Public Health Nursing 2003;20(3):190‐203. [DOI] [PubMed] [Google Scholar]
Olds 2002 {published data only}
- Olds DL, Robinson J, O'Brien R, Luckey DW, Pettitt LM, Henderson CR Jr, et al. Home visiting by paraprofessionals and by nurses: a randomized, controlled trial. Pediatrics 2002;110(3):486‐96. [DOI] [PubMed] [Google Scholar]
- Olds DL, Robinson J, Pettitt L, Luckey DW, Holmberg J, Ng RK, et al. Effects of home visits by paraprofessionals and by nurses: age 4 follow‐up results of a randomized trial. Pediatrics 2004;114(6):1560‐8. [DOI] [PubMed] [Google Scholar]
Omu 1989 {published data only}
- Omu AE, Weir SS, Janowitz B, Covington DL, Lamptey PR, Burton NN. The effect of counseling on sterilization acceptance by high‐parity women in Nigeria. International Family Planning Perspectives 1989;15:66‐71. [Google Scholar]
Proctor 2006 {published data only (unpublished sought but not used)}
- Proctor A, Jenkins TR, Loeb T, Elliot M, Ryan A. Patient satisfaction with 3 methods of postpartum contraceptive counselling. A randomized, prospective trial. Journal of Reproductive Medicine 2006;51(5):377‐82. [PubMed] [Google Scholar]
Ransjo‐Arvidson 1998 {published data only}
- Ransjö‐Arvidson AB, Chintu K, Ng'andu N, Eriksson B, Susu B, Christensson K, et al. Maternal and infant health problems after normal childbirth: a randomised controlled study in Zambia. Journal of Epidemiology and Community Health 1998;52(6):385‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sayegh 1976 {published data only}
- Sayegh J, Mosley WH. The effectiveness of family planning education on acceptance of contraception by postpartum mothers. Johns Hopkins Medical Journal 1976;139(Suppl):31‐7. [PubMed] [Google Scholar]
Smith 2002 {published data only}
- Smith KB, Spuy ZM, Cheng L, Elton R, Glasier AF. Is postpartum contraceptive advice given antenatally of value?. Contraception 2002;65(3):237‐43. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Sadler 2014 {published data only}
- Sadler L. Minding the baby home visiting: program evaluation. http://clinicaltrials.gov/ct2/show/NCT01458145 (accessed 3 December 2014).
- Sadler LS, Newlin KH, Johnson‐Spruill I, Jenkins C. Beyond the medical model: interdisciplinary programs of community‐engaged health research. Clinical and Translational Science 2011;4(4):285‐97. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schreiber 2013 {published data only}
- Schreiber C. Adolescent Postpartum Contraceptive Counseling Intervention (PPCI). http://clinicaltrials.gov/ct2/show/NCT01814930 (accessed 4 December 2014).
Additional references
Balshem 2011
- Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. Journal of Clinical Epidemiology 2011;64(4):401‐6. [DOI] [PubMed] [Google Scholar]
Borda 2010
- Borda MR, Winfrey W, McKaig C. Return to sexual activity and modern family planning use in the extended postpartum period: an analysis of findings from seventeen countries. African Journal of Reproductive Health. 2011/08/05 2010; Vol. 14, issue 4:72‐9. [PubMed]
Borrelli 2011
- Borrelli B. The assessment, monitoring, and enhancement of treatment fidelity in public health clinical trials. Journal of Public Health Dentistry 2011;71(s1):S52‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chapman 2012
- Chapman S, Jafa K, Longfield K, Vielot N, Buszin J, Ngamkitpaiboon L, et al. Condom social marketing in sub‐Saharan Africa and the Total Market Approach. Sexual Health 2012;9(1):44‐50. [DOI] [PubMed] [Google Scholar]
Damle 2015
- Damle LF, Gohari AC, McEvoy AK, Desale SY, Gomez‐Lobo V. Early initiation of postpartum contraception: does it decrease rapid repeat pregnancy in adolescents?. Journal of Pediatric and Adolescent Gynecology 2015;28(1):57‐62. [DOI] [PubMed] [Google Scholar]
Do 2013
- Do M, Hotchkiss D. Relationships between antenatal and postnatal care and post‐partum modern contraceptive use: evidence from population surveys in Kenya and Zambia. BMC Health Services Research 2013;13:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Engin‐Üstün 2007
- Engin‐Üstün Y, Üstün Y, Cetin F, Meydanh MM, Kafkash A, Sezgin B. Effect of postpartum counseling on postpartum contraceptive use. Archives of Gynecology and Obstetrics 2007;275(6):429‐32. [DOI] [PubMed] [Google Scholar]
Fagan 2009
Glasier 1996
- Glasier AF, Logan J, McGlew TJ. Who gives advice about postpartum contraception?. Contraception 1996;53(4):217‐20. [DOI] [PubMed] [Google Scholar]
Glazer 2011
Guyatt 2011
- Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction‐GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology 2011;64(4):383‐94. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. John Wiley & Sons, Ltd, (accessed 26 Mar 2012).
Huang 2014
- Huang Y, Merkatz R, Zhu H, Roberts K, Sitruk‐Ware R, Cheng L. The free perinatal/postpartum contraceptive services project for migrant women in Shanghai: effects on the incidence of unintended pregnancy. Contraception 2014;89(6):521‐7. [DOI] [PubMed] [Google Scholar]
Keith 1980
- Keith l, Berger GS. Control of reproduction in the puerperal state.. In: Aladjem S, editor. Obstetrical practice. St. Louis: CV Mosby Company, 1980:Chapter 16. [Google Scholar]
Koenig 1992
- Koenig MA, Rob U, Khan MA, Chakraborty J, Fauveau V. Contraceptive use in Matlab, Bangladesh in 1990: levels, trends, and explanations. Studies in Family Planning 1992;23(6 Pt 1):352‐64. [PubMed] [Google Scholar]
Lopez 2013
- Lopez LM, Tolley EE, Grimes DA, Chen M, Stockton LL. Theory‐based interventions for contraception. Cochrane Database of Systematic Reviews 2013, Issue 8. [DOI: 10.1002/14651858.CD007249.pub4] [DOI] [PubMed] [Google Scholar]
Mosher 2012
- Mosher WD, Jones J, Abma JC. Intended and unintended births in the United States: 1982‐2010. National Center for Health Statistics reports; no 55. Hyattsville, MD (USA): National Center for Health Statistics, 2012. [PubMed] [Google Scholar]
Ozvaris 1997
- Ozvaris SB, Akin A, Yildiran M. Acceptability of postpartum contraception in Turkey. Advances in Contraceptive Delivery Systems 1997;13:63‐71. [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Centre, The Cochrane Collaboration, 2014.
Ross 2001
- Ross JA Winfrey WL. Contraceptive use, intention to use and unmet need during the extended postpartum period. International Family Planning Perspectives 2001;27(1):20‐7. [Google Scholar]
Schulz 2010
- Schulz KF, Altman DG, Moher D, for the CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010; Vol. 340:c332. [DOI] [PMC free article] [PubMed]
Semeraro 1996
- Semeraro P. Postpartum family planning services: Challenges for the future.. In: Murray, SF editor(s). In: Midwives and safer motherhood. London: Mosby, 1996:Chapter 6. [Google Scholar]
Shaw 2007
- Shaw E, Kaczorowski J. Postpartum care ‐ what's new?. Current Opinion in Obstetrics and Gynecology 2007;19(6):561‐7. [DOI] [PubMed] [Google Scholar]
USAID 2014
- United States Agency for International Development. Postpartum Family Planning (PPFP) Toolkit. www.k4health.org/toolkits/ppfp (accessed 8 September 2014).
Wilson 2011
References to other published versions of this review
Hay‐Smith 1994
- Hay‐Smith J. Education on contraceptive use by postpartum mothers [revised 27 January 1994]. Cochrane Collaboration; Pregnancy and Childbirth Module. Oxford: Update software, 1994; Vol. 2.


