Abstract
Background
Neurosurgical task shifting and task sharing (TS/S), delegating clinical care to non-neurosurgeons, is ongoing in many hospital systems in which neurosurgeons are scarce. Although TS/S can increase access to treatment, it remains highly controversial. This survey investigated perceptions of neurosurgical TS/S to elucidate whether it is a permissible temporary solution to the global workforce deficit.
Methods
The survey was distributed to a convenience sample of individuals providing neurosurgical care. A digital survey link was distributed through electronic mailing lists of continental neurosurgical societies and various collectives, conference announcements, and social media platforms (July 2018–January 2019). Data were analyzed by descriptive statistics and univariate regression of Likert Scale scores.
Results
Survey respondents represented 105 of 194 World Health Organization member countries (54.1%; 391 respondents, 162 from high-income countries and 229 from low- and middle-income countries [LMICs]). The most agreed on statement was that task sharing is preferred to task shifting. There was broad consensus that both task shifting and task sharing should require competency-based evaluation, standardized training endorsed by governing organizations, and maintenance of certification. When perspectives were stratified by income class, LMICs were significantly more likely to agree that task shifting is professionally disruptive to traditional training, task sharing should be a priority where human resources are scarce, and to call for additional TS/S regulation, such as certification and formal consultation with a neurosurgeon (in person or electronic/telemedicine).
Conclusions
Both LMIC and high-income countries agreed that task sharing should be prioritized over task shifting and that additional recommendations and regulations could enhance care. These data invite future discussions on policy and training programs.
Key words: Global health, Global neurosurgery, LMIC, Neurotrauma, Task sharing, Task shifting, Workforce
Abbreviations and Acronyms: HIC, High-income country; LMIC, Low- and middle-income country; NSOAP, National Surgical Anesthesia and Obstetric Plan; TS/S, Task shifting and task sharing; WHO, World Health Organization
Introduction
The United Nations Sustainable Development Goals for 2030 require concerted efforts for building surgical capacity to increase timely access to safe and affordable care.1, 2, 3, 4 A major focus in low- and middle-income countries (LMICs) is the ability to deliver trauma care, and because 69 million individuals have all-cause traumatic brain injury annually, neurosurgery is a critical component of this workforce expansion.5, 6, 7 However, in many LMICs, the neurosurgical capacity is only 1%–10% of the minimum expected neurosurgeon ratio per population, which is 0.01–0.1 neurosurgeons per 100,000 population; the expected ratio is at least 1/100,000 to address the complete range of neurosurgical conditions8, 9 and 0.5/100,000 people if addressing only neurotrauma.10
Despite multifaceted approaches to increase neurosurgical capacity (e.g., increasing the number of residency training programs, short-term missions, training camps, twinning, and encore careers) the workforce deficit remains substantial.11, 12, 13, 14 Consequently, there is an increasing interest in the use of neurosurgical task shifting and task sharing (TS/S): delegating certain neurosurgical tasks to nonneurosurgeon specialists, such as general surgeons, general practitioners, or nonphysician clinicians.14, 15 Although task shifting is redistribution of both duties and clinical autonomy from neurosurgeons to those with shorter training and fewer qualifications, task sharing involves a team-based approach with collective input and shared responsibility for patient care.16 TS/S is a workforce strategy that is more rapid and economical than traditional training; however, it is highly controversial because of safety, ethical, financial, legal, and professional implications.14 On one hand, having a necessary operation via TS/S may be superior to no care, and TS/S may offer acute stabilization of emergency patients to enable safer transfer to tertiary-care facilities.12, 13, 17, 18, 19 Conversely, TS/S theoretically raises concerns for lower-quality care and disrupting professional roles if less-skilled workers substitute for higher-skilled staff. As we come together as a global neurosurgical community to strategize for meeting the Sustainable Development Goals of 2030, it is vital to understand the current perspectives within the field before we decide how TS/S will play a role in workforce expansion.
The objectives of this survey were to gain a thorough understanding of practices and perceptions of TS/S. The results are intended to inform future discussions on policy and training programs and elucidate whether TS/S is a permissible temporary solution to the workforce deficit or if efforts should focus only on full training programs.
Methods
Survey Design
A modified Delphi method was used to construct, pilot, and refine the questionnaire.20 The consulting panel of experts involved neurosurgeons from 20 countries, most with experience of living or working in a country striving to expand the neurosurgical workforce. Questions were framed to elucidate perspectives on various components of TS/S, particularly as they related to a theoretic task-sharing model outlined by the Lancet Commission on Global Surgery.21 The surveys were available in English, French, and Spanish (Appendix 1) and were approved by the institutional review board at Harvard University (IRB18-0158). The target audience included neurosurgery providers, defined as any health worker providing operative neurosurgical care. Neurosurgery providers were characterized into 4 groups: specialist neurosurgeons (dedicated neurosurgery consultants/attendings); general surgeons (general surgery consultants/attendings who have not completed a formal residency/registrar/fellowship training in neurosurgery); general practitioners (those with a medical license but without dedicated surgical training); and nonphysician providers (those who are from a nursing background or from some other nonphysician background).
Survey Dispersal
The surveys were available through an anonymous online link to the Qualtrics platform (Provo, Utah, USA). Our methods strived to achieve representation from the maximum number of countries (at the expense of calculating individual response rates), which mirrors the methods of the WFSA Global Anesthesia Workforce Survey.22 The surveys were distributed via electronic mailing lists of continental societies and various other neurosurgical groups, e-mail to personal contacts, QR codes, and social media platforms through various methods: the Congress of Continental Association of African Neurosurgical Societies distributed through e-mail lists and advertised at Annual Meeting in Abuja, Nigeria (global neurosurgery session, 80–100 attendees)23; the European Association of Neurosurgical Societies distributed through e-mail lists and advertised at the Annual Conference in Belgium (approximately 1600 attendees annually)24; the Asian Australasian Society of Neurological Surgeons through their e-mail list; the Chair of the World Federation of Neurosurgical Societies sent to all subcommittees; and the National Institute for Health Research Global Health Research Group on Neurotrauma distributed through e-mail and social media. All 28 neurosurgeons who took part in survey creation assisted in additional dispersal, and the coauthors broadcasted on multiple social media outlets (e.g., Facebook groups, Twitter, and neurosurgical WhatsApp collectives). Participation in the survey was voluntary and without remuneration. Given the method of dissemination, a response rate calculation could not be obtained. The survey remained open from July 2018 to January 2019. At the end of the survey, individuals were invited to list their name in a separate form to receive collaborator status.
Data Analysis
All survey data were exported for analysis on January 18, 2019 from Qualtrics into an Excel file and analyzed using Stata 14.0 (StataCorp LLC, College Station, Texas, USA). Data were grouped according to World Health Organization (WHO) regions (African Region, Region of the Americas–US and Canada, Region of the Americas–Latin America, South-East Asia Region, European Region, Eastern Mediterranean Region, and Western Pacific Region) and then reported at the level of individual countries. Data were grouped and analyzed according to 2018 World Bank Income Data: high-income countries (HICs), versus LMICs.25 Perspectives on TS/S were elicited using Likert Scale scores: a score of 1 represents “strongly agree”; 2, “agree”; 3, “neutral”; 4, “disagree”; and 5, “strongly disagree.” Data were analyzed by descriptive statistics and univariate regression of Likert Scale scores and arranged from the most agreeable statements to least agreeable statements. Probability values <0.05 were considered significant. Respondent free text comments were used to represent general themes.
Results
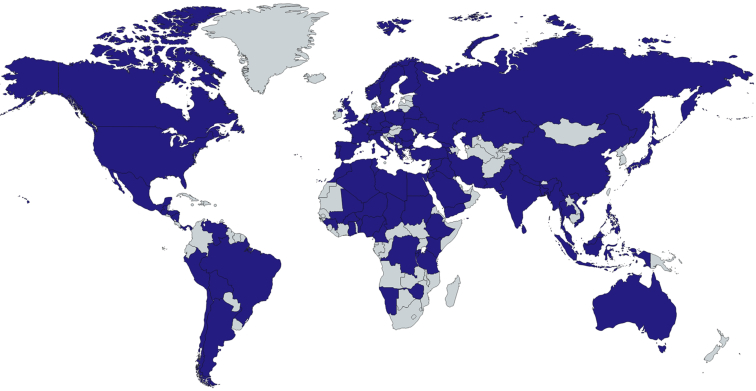
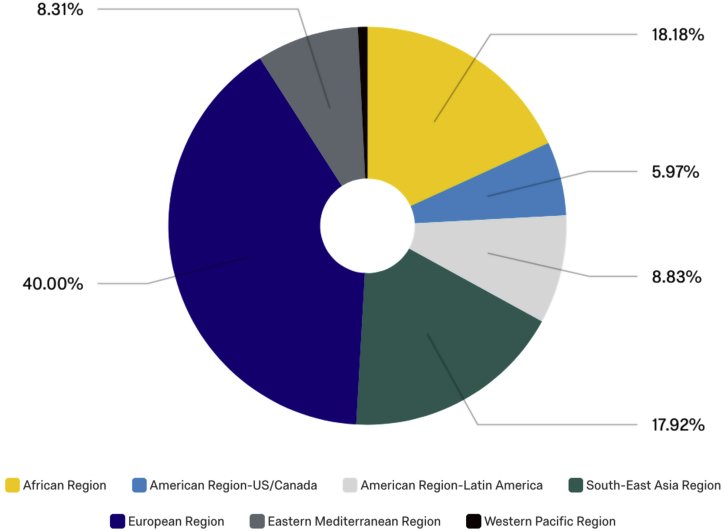
We obtained returns from 105 of 194 WHO member countries (54.1%). In addition, we obtained information for 1 nonmember country (Taiwan), with a total of 391 respondents (162 individuals from HICs and 229 from LMICs; Figure 1, Table 1). The African WHO Region had 70 respondents (17.9%), 5.9% of replies were from the America–US/Canada Region, 39.4% were from the European Region, 9.0% from the Eastern Mediterranean Region, 8.7% from the Latin American Region, and 0.8% from the Western Pacific Region (Figure 2). These countries included (participant count in parentheses): Afghanistan (1), Albania (1), Algeria (8), Argentina (7), Armenia (1), Australia (2), Austria (3), Bangladesh (4), Belgium (3), Benin (1), Bolivia (1), Bosnia and Herzegovina (1), Brazil (6), Bulgaria (2), Burkina Faso (1), Burundi (1), Cameroon (2), Canada (2), Chad (1), Chile (1), China (2), Colombia (6), Democratic Republic of the Congo (4), Cyprus (1), Czech Republic (3), Egypt (17), Ethiopia (7), Finland (5), France (3), Georgia (1), Germany (10), Greece (9), Guatemala (1), Guinea (1), Honduras (2), India (28), Indonesia (5), Iran (1), Iraq (4), Israel and the Occupied Territories (5), Italy (28), Jordan (3), Kazakhstan (1), Kenya (2), Libya (4), Northern Macedonia (1), Malawi (2), Malaysia (10), Maldives (1), Mali (1), Mexico (5), Moldova (1), Morocco (5), Myanmar (1), Namibia (1), Nepal (3), Netherlands (3), Nicaragua (2), Nigeria (14), Norway (1), Pakistan (11), Peru (4), Philippines (7), Poland (1), Portugal (8), Puerto Rico (1), Romania (5), Rwanda (2), Saudi Arabia (3), Serbia (5), Singapore (2), Somalia (1), South Africa (1), Spain (10), Sri Lanka (1), St. Vincent and the Grenadines (1), Sudan (2), Swaziland (2), Sweden (1), Switzerland (1), Syrian Arab Republic (3), Taiwan (1), Tanzania (1), Thailand (1), Tunisia (1), Turkey (16), Ukraine (2), United Kingdom (22), United States (14), Venezuela, RB (1), Vietnam (2), West Bank and Gaza (3), Republic of Yemen (1), and Zambia (1).
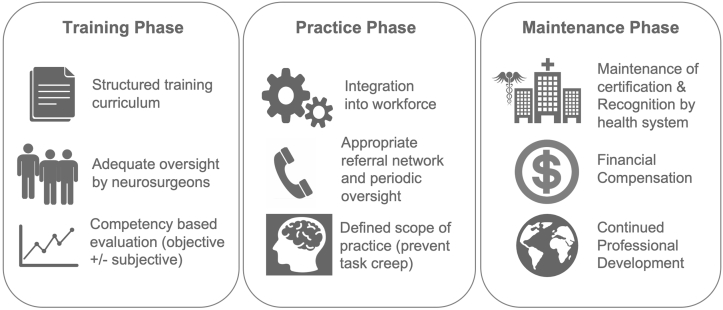
Figure 1.
An ideal task-sharing model divided into 3 phases of training, practice, and maintenance of providers.
(Figure from Robertson et al.18).
Table 1.
Demographics of Respondents
| Variable | Number of Responses (%) (N = 391) |
|---|---|
| Age (years) | |
| <29 | 66 (16.9) |
| 30–39 | 181(46.3) |
| 40–49 | 81 (20.7) |
| 50–59 | 38 (9.7) |
| 60–69 | 23 (5.9) |
| ≥70 | 2 (0.5) |
| Gender | |
| Male | 321 (82.1) |
| Female | 69 (17.7) |
| Other | 1 (0.3) |
| Region | |
| African Region | 70 (17.9) |
| American Region–US/Canada | 23 (5.9) |
| American Region–Latin America | 34 (8.7) |
| Eastern Mediterranean Region | 35 (9.0) |
| European Region | 154 (39.4) |
| South-East Asia Region | 72 (18.4) |
| Western Pacific Region | 3 (0.77) |
| Training level | |
| Consultant neurosurgeon | 235 (60.1) |
| Neurosurgery trainee | 120 (30.7) |
| Consultant general surgeon | 2 (0.5) |
| General surgery trainee | 4 (1.0) |
| General practitioner | 9 (2.3) |
| Other (clinical officer, nonphysician provider) | 21 (5.4) |
| Years of practice | |
| Still in training | 94 (24.0) |
| 0–5 | 107 (27.4) |
| 6–10 | 90 (23.2) |
| 11–20 | 52 (13.3) |
| 21–30 | 29 (7.4) |
| >30 | 19 (4.9) |
| Neurosurgical society member | |
| American Association of Neurological Surgeons | 99 (30.2) |
| Asian Australasian Society of Neurological Surgeons | 13 (4.0) |
| Continental Association of African Neurosurgical Societies | 31 (9.5) |
| European Association of Neurosurgical Societies | 170 (51.8) |
| Latin American Federation of Neurosurgical Societies | 15 (4.6) |
| Neurosurgical subspecialty (multiple selection) | |
| General | 285 (21.6) |
| Pediatric | 109 (8.3) |
| Tumor | 244 (18.5) |
| Vascular | 140 (10.6) |
| Functional | 70 (5.3) |
| Spine | 190 (14.4) |
| Trauma | 204 (15.5) |
| Intensive/neurocritical care | 75 (5.7) |
| Place of practice (multiple selection) | |
| Public/governmental sector | 218 (32.1) |
| Private | 122 (18.0) |
| University teaching hospital | 308 (45.4) |
| Charitable/not-for-profit | 18 (2.7) |
| Religious hospital | 13 (1.9) |
| Setting | |
| Urban | 370 (94.9) |
| Rural | 20 (5.1) |
| Hospital level | |
| 1: Small hospital or health center, a small number of beds and a sparsely equipped operating room for minor procedures | 17 (4.4) |
| 2: District or provincial hospital, 100–300 beds, and adequately equipped major and minor operating rooms | 58 (15.0) |
| 3: Referral hospital, 300–≥1000 beds with basic intensive care facilities | 311 (80.6) |
Figure 2.
Survey respondents' country of reporting. A total of 391 individuals from 106 countries completed the survey.
(Created with mapchart.net.).
Most respondents were fully trained neurosurgery consultants/attendings (60.1%), followed by neurosurgery trainees (30.7%); other providers of neurosurgical care also completed the survey. Regarding years of clinical experience, survey participants were equally distributed between having ≥10 years of consultant-level experience, 5–10 years of experience, 0–5 years of experience, and currently being in a training program. Most (94.9%) were working in an urban setting, and >80% were working in a level 3 referral hospital (300–≥1000 beds with basic intensive care facilities). Hospital type was chiefly university teaching hospitals (45.4%), followed by public/governmental sector hospitals (32.1%) and private practice (18.0%). There was a broad distribution of neurosurgical subspecialties and membership of international neurosurgical societies, particularly the European Association of Neurosurgical Societies.
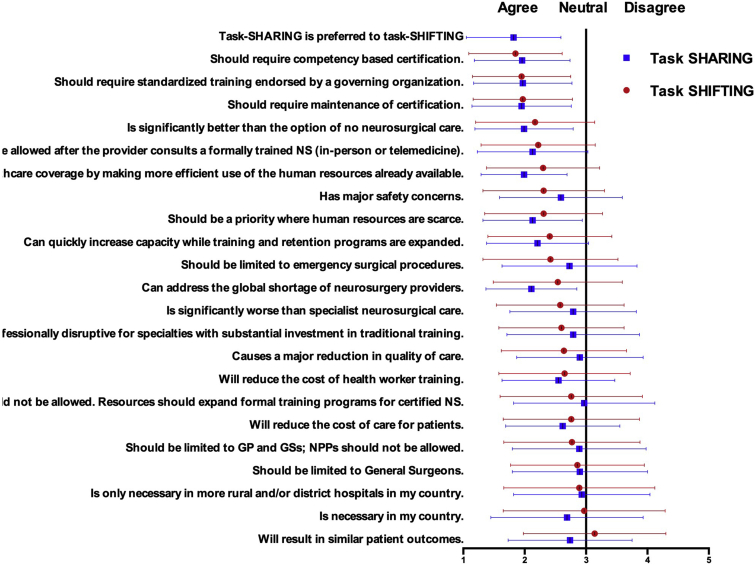
Overall Perspectives
The most agreed on statement was that task sharing is preferred to task shifting (Figure 3). Respondents also reported that task sharing would result in similar patient outcomes (compared with care delivered by a neurosurgeon), whereas task shifting would not result in comparable care. There was broad consensus that both task shifting and task sharing should require competency-based evaluation, standardized training endorsed by governing organizations, and maintenance of certification. The largest differences between perspectives on task shifting versus task sharing were that it results in similar patient outcomes; it can improve health care coverage by making more efficient use of the human resources already available; it has major safety concerns; and it is necessary in my country.
Figure 3.
World Health Organization Regions of survey respondents.
Perspectives by Country Income Status
Because TS/S is more often practiced in LMICs than in HICs, and subjective opinions may vary accordingly, the perspectives of these respective practices were analyzed by World Bank country income status. Univariate regression of Likert Scale scores comparing LMICs and HICs are shown for task shifting in Table 2 and task sharing in Table 3. Results are arranged from the most agreeable statements to least agreeable.
Table 2.
Perspectives on Task Shifting by World Bank Income Classification
| Task Shifting | Total | Low- and Middle-Income Country, Mean (SD) | High-Income Country, Mean (SD) | B-Coefficient | Standard Error | 95% Confidence Interval | P Value | |
|---|---|---|---|---|---|---|---|---|
| Should require competency-based certification | 1.85 (0.76) | 1.79 (0.70) | 1.93 (0.83) | –0.06 | 0.04 | –0.14 | 0.02 | 0.15 |
| Should require standardized training endorsed by a governing organization | 1.95 (0.81) | 1.86 (0.75) | 2.06 (0.87) | –0.08 | 0.04 | –0.15 | 0.00 | 0.04 |
| Should require maintenance of certification | 1.97 (082) | 1.87 (0.76) | 2.10 (0.87) | –0.08 | 0.04 | –0.16 | –0.01 | 0.03 |
| Is significantly better than the option of no neurosurgical care | 2.17 (0.97) | 2.13 (0.93) | 2.23 (1.04) | –0.03 | 0.03 | –0.09 | 0.04 | 0.40 |
| Should be allowed only after the provider consults a formally trained neurosurgeon (in person or via electronic/telemedicine consultation) | 2.22 (0.93) | 2.07 (0.88) | 2.43 (0.96) | –0.10 | 0.03 | –0.17 | –0.04 | 0.001 |
| Can improve health care coverage by making more efficient use of the human resources already available | 2.30 (0.93) | 2.29 (0.89) | 2.31 (0.95) | 0.01 | 0.03 | –0.06 | 0.73 | 0.86 |
| Should be a priority where human resources are scarce | 2.31 (0.96) | 2.30 (0.95) | 2.32 (0.97) | –0.01 | 0.03 | –0.07 | 0.06 | 0.86 |
| Has major safety concerns | 2.31 (0.99) | 2.27 (1.01) | 2.37 (0.95) | –0.02 | 0.03 | –0.09 | 0.04 | 0.43 |
| Can quickly increase capacity while training and retention programs are expanded | 2.41 (1.01) | 2.28 (1.00) | 2.58 (1.02) | –0.07 | 0.03 | –0.13 | –0.01 | 0.02 |
| Should be limited to emergency surgical procedures | 2.42 (1.10) | 2.22 (1.11) | 2.69 (1.03) | –0.10 | 0.03 | –0.15 | –0.04 | <0.001 |
| Can address the global shortage of neurosurgery providers | 2.54 (1.06) | 2.52 (0.99) | 2.55 (1.11) | 0.01 | 0.03 | –0.05 | 0.72 | 0.84 |
| Is significantly worse than specialist neurosurgical care | 2.58 (1.04) | 2.62 (1.04) | 2.52 (1.05) | 0.02 | 0.03 | –0.03 | 0.08 | 0.42 |
| Is professionally disruptive, because these new roles will encroach on specialties where professionals invest great time and resources into their training | 2.60 (1.03) | 2.47 (1.04) | 2.76 (0.99) | –0.07 | 0.03 | –0.13 | –0.01 | 0.02 |
| Causes a major reduction in quality of care | 2.64 (1.02) | 2.61 (1.04) | 2.69 (1.00) | –0.02 | 0.03 | –0.08 | 0.04 | 0.56 |
| Will reduce the cost of health worker training | 2.65 (1.08) | 2.64 (1.12) | 2.66 (1.02) | 0.00 | 0.03 | –0.06 | 0.05 | 0.91 |
| Will reduce the cost of care for patients | 2.76 (1.11) | 2.70 (1.16) | 2.85 (1.03) | –0.03 | 0.03 | –0.08 | 0.03 | 0.29 |
| Should not be allowed. Resources should focus only on expanding the training programs for formal, certified neurosurgical positions | 2.76 (1.16) | 2.58 (1.15) | 2.76 (1.16) | –0.08 | 0.03 | –0.13 | –0.03 | 0.003 |
| Should be limited to general practitioners and general surgeons; nonphysician providers should not be allowed | 2.77 (1.12) | 2.68 (1.11) | 2.91 (1.11) | –0.05 | 0.03 | –0.10 | 0.01 | 0.09 |
| Should be limited to general surgeons | 2.86 (1.09) | 2.66 (1.09) | 3.13 (1.02) | –0.10 | 0.03 | –0.15 | –0.04 | 0.001 |
| Is necessary only in more rural and/or district hospitals in my country | 2.89 (1.23) | 2.61 (1.13) | 3.27 (1.26) | –0.11 | 0.02 | –0.15 | –0.06 | <0.001 |
| Is necessary in my country | 2.97 (1.33) | 2.68 (1.23) | 3.38 (1.36) | –0.10 | 0.02 | –0.14 | –0.06 | <0.001 |
| Will result in similar patient outcomes | 3.14 (1.17) | 3.11 (1.17) | 3.17 (1.17) | –0.01 | 0.03 | –0.06 | 0.04 | 0.69 |
SD, standard deviation.
Table 3.
Perspectives on Task Sharing by World Bank Income Classification
| Task sharing | Total | Low- and Middle-Income Country, Mean (SD) | High-Income Country, Mean (SD) | B-Coefficient | Standard Error | 95% Confidence Interval | P Value | |
|---|---|---|---|---|---|---|---|---|
| Is preferred to task shifting, where new groups/cohorts perform procedures with full autonomy | 1.81 (0.78) | 1.76 (0.77) | 1.90 (0.78) | –0.06 | 0.04 | –0.13 | 0.02 | 0.17 |
| Should require maintenance of certification | 1.95 (0.81) | 1.83 (0.78) | 2.10 (0.83) | –0.10 | 0.04 | –0.18 | –0.03 | 0.01 |
| Should require competency-based certification | 1.96 (0.79) | 1.88 (0.73) | 2.07 (0.84) | –0.08 | 0.04 | –0.15 | 0.00 | 0.06 |
| Should require standardized training endorsed by a governing organization | 1.97 (0.81) | 1.91 (0.79) | 2.06 (0.83) | –0.05 | 0.04 | –0.13 | 0.02 | 0.16 |
| Can improve health care coverage by making more efficient use of the human resources already available | 1.99 (0.70) | 1.92 (0.71) | 2.08 (0.67) | –0.08 | 0.04 | –0.17 | 0.00 | 0.06 |
| Is significantly better than the option of no neurosurgical care | 1.99 (0.80) | 1.92 (0.78) | 2.09 (0.83) | –0.06 | 0.04 | –0.14 | 0.02 | 0.12 |
| Can address the global shortage of neurosurgery providers | 2.11 (0.74) | 2.03 (0.73) | 2.22 (0.76) | –0.08 | 0.04 | –0.17 | 0.00 | 0.05 |
| Should be allowed only after the provider consults a formally trained neurosurgeon (in person or via electronic/telemedicine consultation) | 2.12 (0.90) | 2.00 (0.86) | 2.29 (0.94) | –0.09 | 0.03 | –0.15 | –0.02 | 0.01 |
| Should be a priority where human resources are scarce | 2.13 (0.81) | 2.03 (0.79) | 2.27 (0.82) | –0.09 | 0.04 | –0.17 | –0.02 | 0.02 |
| Can quickly increase capacity while training and retention programs are expanded | 2.21 (0.83) | 2.11 (0.82) | 2.34 (0.83) | –0.09 | 0.04 | –0.16 | –0.01 | 0.02 |
| Will reduce the cost of health worker training | 2.55 (0.92) | 2.46 (0.92) | 2.67 (0.92) | –0.06 | 0.03 | –0.13 | 0.01 | 0.07 |
| Has major safety concerns | 2.59 (1.01) | 2.45 (1.03) | 2.78 (0.95) | –0.08 | 0.03 | –0.14 | –0.02 | 0.01 |
| Will reduce the cost of care for patients | 2.62 (0.93) | 2.51 (0.94) | 2.77 (0.91) | –0.07 | 0.03 | –0.14 | –0.01 | 0.03 |
| Is necessary in my country | 2.69 (1.24) | 2.27 (1.05) | 3.26 (1.26) | –0.16 | 0.02 | –0.20 | –0.11 | <0.001 |
| Will result in similar patient outcomes | 2.73 (1.01) | 2.64 (1.08) | 2.88 (0.91) | –0.06 | 0.03 | –0.12 | 0.00 | 0.07 |
| Should be limited to emergency surgical procedures | 2.73 (1.10) | 2.57 (1.18) | 2.95 (0.95) | –0.08 | 0.03 | –0.13 | –0.02 | 0.01 |
| Is significantly worse than specialist neurosurgical care | 2.79 (1.04) | 2.71 (1.08) | 2.89 (0.96) | –0.04 | 0.03 | –0.10 | 0.02 | 0.21 |
| Is professionally disruptive, because these new roles will encroach on specialties where professionals invest great time and resources into their training | 2.79 (1.09) | 2.71 (1.14) | 2.90 (1.00) | –0.04 | 0.03 | –0.10 | 0.02 | 0.15 |
| Should be limited to general practitioners and general surgeons; nonphysician providers should not be allowed | 2.88 (1.09) | 2.74 (1.14) | 3.09 (0.99) | –0.07 | 0.03 | –0.13 | –0.02 | 0.01 |
| Causes a major reduction in quality of care | 2.90 (1.03) | 2.80 (1.08) | 3.02 (0.95) | –0.05 | 0.03 | –0.11 | 0.01 | 0.09 |
| Should be limited to general surgeons | 2.90 (1.10) | 2.65 (1.14) | 3.24 (0.94) | –0.12 | 0.03 | –0.17 | –0.06 | <0.001 |
| Is necessary only in more rural and/or district hospitals in my country | 2.93 (1.11) | 2.74 (1.06) | 3.18 (1.13) | –0.09 | 0.03 | –0.14 | –0.03 | 0.002 |
| Should not be allowed. Resources should focus only on expanding the training programs for formal, certified neurosurgical positions | 2.97 (1.15) | 2.83 (1.21) | 3.16 (1.03) | –0.06 | 0.03 | –0.11 | –0.01 | 0.03 |
SD, standard deviation.
On task shifting, there were statistically significant differences between LMICs and HICs on 10 of 22 statements. Respondents from LMICs were more in agreement with requiring standardized training endorsed by a governing organization, requiring maintenance of certification, and allowing task shifting only after the provider consults a formally trained neurosurgeon (in person or via electronic/telemedicine consultation) and limiting task shifting to emergency surgical procedures. Respondents from LMICs were also more in agreement that task shifting can quickly increase capacity while training and retention programs are expanded and were more likely to acknowledge that task shifting is professionally disruptive, because these new roles encroach on specialties in which professionals invest great time and resources into their training. In statements that bordered agreeable/neutral stances, more respondents from LMICs noted that task shifting should not be allowed, because resources should focus only on expanding the training programs for formal certified neurosurgical positions. There were 3 statements with which LMICs agreed whereas HICs disagreed: 1) task shifting should be limited to general surgeons; 2) task shifting is necessary in their country; and 3) task shifting is necessary only in more rural and/or district hospitals in their country.
On task sharing, there were statistically significant differences between LMICs and HICs on 12 of 23 statements. Respondents from LMICs were more in agreement with requiring maintenance of certification and allowing task sharing only after the provider consults a formally trained neurosurgeon (in person or via electronic/telemedicine consultation) and that task sharing can address the global shortage of neurosurgery providers. Respondents from LMICs were also more in agreement that task sharing should be a priority where human resources are scarce and can quickly increase capacity while training and retention programs are expanded. In statements that bordered agreeable/neutral stances, more individuals from LMICs expressed that task sharing has major safety concerns, reduces the cost of care for patients, and should be limited to emergency surgical procedures. There were 4 statements with which LMICs agreed whereas HICs disagreed: 1) task sharing should be limited to general practitioner and general surgeons (nonphysician providers should not be allowed), 2) task sharing should be limited to general surgeons; 3) task sharing is necessary only in more rural and/or district hospitals in their country; and 4) task sharing should not be allowed, because resources should focus only on expanding the training programs for formal certified neurosurgical positions.
Discussion
This survey is the first study to investigate the global perspectives on TS/S care provision in neurosurgery. As the recent survey on TS/S prevalence showed that TS/S is ongoing in many LMICs (Robertson et al.accepted to World Neurosurgery),26 a clear understanding of how HICs and LMICs view TS/S will facilitate consensus-based approaches for health system strengthening and enhance buy-in for policy adoption. As shown in previous global health initiatives, generation of political priority and success of an intervention is highly contingent on cohesion between the actors involved and consensus surrounding the definition of, cause of, and solutions to the problem.2, 27
Overall, the most agreed on statement was that task sharing is preferred to task shifting. Respondents also believed that task sharing could result in similar patient outcomes (compared with care delivered by a neurosurgeon), whereas task shifting would not result in comparable care and was believed to have major safety concerns. The premise behind this result is that a more extensively trained neurosurgeon would be regularly involved in overseeing or having iterative input on care delivery, echoing opinions held in the general surgery realm.28 The broad consensus that both task shifting and task sharing should require competency-based evaluation, standardized training endorsed by governing organizations, and maintenance of certification is encouraging because it affirms consensus regarding the severity of the problem and potential effective solutions.
When perspectives were stratified by income class, LMICs were more agreeable than HICs to additional TS/S regulation. For both task shifting and task sharing, LMICs were significantly more in favor of standardized training endorsed by a governing organization, requiring maintenance of certification, and allowing task shifting only after the provider consults a formally trained neurosurgeon (in person or via electronic/telemedicine consultation). LMICs were also more likely to acknowledge that task shifting is professionally disruptive and were more optimistic that task sharing can address the global shortage of neurosurgery providers, agreeing that task sharing should be a priority where human resources are scarce and that it can quickly increase capacity while training and retention programs are expanded.
Seeing the LMIC countries that expressed that TS/S is needed in their country simultaneously call for additional regulation is a powerful finding that supports why the time is ripe for the generation of political priority for initiatives to address TS/S in neurosurgery. Since the report of the Lancet Commission on Global Surgery in 2015, there has been a campaign for developing National Surgical Anesthesia and Obstetric Plans (NSOAPs) in LMICs. In NSOAP, the LMICs' Ministries of Health work with global consultants, such as the Program of Global Surgery and Social Change at Harvard Medical School, to strategize and create action steps to meet the Sustainable Development Goals of 2030.29 The first country to create a National Surgical Plan was Ethiopia in 2016 (entitled Saving Lives Through Safe Surgery [SaLTS]), and many other countries have initiated their own NSOAP since.30 The process of forming an NSOAP is a shared decision-making approach that emphasizes the needs and desires of the LMIC within the recommendations put forth by consultants based on available data and previous experience. In this process, it is key that policy makers from HICs (given that more HIC members have seats at the table of global policy-making organizations and meetings) do not impose unfounded ideas on the LMIC. However, when the group planning a health system–strengthening agenda has ownership over ideas and visions for change, then, policies, local advances, and implementation systems are more effective.2, 27 Thus, having LMICs (where TS/S is most relevant) be the nations most keen to implement structure in TS/S practice suggests that there is a greater likelihood that TS/S-associated policies will be accepted and put into practice. Because countries write their respective NSOAPs, information on TS/S should be included. Recommendations on how TS/S programs could be structured within an NSOAP are now accessible in the Comprehensive Policy Recommendations for Head and Spine Injury Care in LMICs,31 which emphasizes task sharing over task shifting. Nonetheless, the ethics, health system regulation details, and precautions of TS/S in neurosurgery warrant further discussion.
This perspectives survey allows us to gauge the opinions of the actors, the consensus regarding the ideas (potential solutions), and issue characteristics (severity of the problem and effective solutions). By comparing the HIC perspectives with those from LMICs, we can understand where differing opinions may lie and avoid miscommunication and the Global North telling the Global South what should and should not be done, in a pseudocolonialist fashion. For instance, given that some HICs have an overabundance of neurosurgical providers, a lesser burden of neurosurgical disease that requires emergent intervention, more medicolegal implications, and board certification that is tightly regulated to ensure quality of care, perspectives of neurosurgeons from these areas may differ greatly from those in areas facing a large neurotrauma burden without sufficient neurosurgical care. This is a real issue, as highlighted in a recent perspective piece in Lancet Neurology as a rebuttal to a previously published article on task shifting and sharing (“Training nonphysicians as neurosurgeons in sub-Saharan Africa”):14
Views on Africa by European and North American experts are commonly provided with little input from Africans who have the necessary insight… We invite readers of The Lancet Neurology to learn about initiatives in Africa, and perhaps consider our views on solutions to our challenges. They might be surprised.32
Hence, these results point to where there is agreement but also where further discussion may be needed before policy recommendation are made.
Future Directions
Surgical workforce deficits compounded by high burdens of surgical disease have led many LMICs to depend on visiting surgeons and TS/S. Although traditional training of neurosurgeons is preferred, task sharing can be used to broaden workforce coverage, and task shifting is the least supported option for workforce expansion. To ensure patient safety and mitigate negative consequences of task sharing, having a robust training and sustaining model is paramount. As mentioned by the Lancet Commission, shown in Figure 4, and crystallized by the survey, task-sharing models should have systematic training and competency-based evaluation before allowing task-sharing providers to practice.21 Subsequently, local supervision should happen periodically to ensure maintenance of skills and competencies, and proper referral networks should be established for complex cases and complications. The ratio of specialists to task-sharers recommended by the Lancet Commission was 1:4,21 and the ratio recently reported in the Philippines task-sharing study (2:9) seems to expand access and preserve safety.18 Task-sharers should be officially recognized and supported by their institutions with a clear definition of their scope of practice, adequate financial remuneration, and clear opportunities for career progression to prevent attrition of practitioners and prevent task-creep. Task sharing should be performed in concert with residency strengthening and organized geographic distribution of neurosurgical providers. Ideally, robust residency training programs would provide appropriate specialty knowledge and technical skills to deliver high-quality care. Even if a full-time neurosurgical task-sharing model were permanently adopted, countries would still need to develop fully trained and competent neurosurgeon leaders who can champion future teams of task-sharing efforts. Given the upscaling of access to safe, timely, and affordable neurosurgery and the consequent reduction in disability-adjusted life years, we believe that this model would potentiate significant health and economic benefits to the institutions and system. Many of the coauthors of this project have come together to sculpt the Comprehensive Policy Recommendations for Head and Spine Injury Care in LMICs. This document spans neurotrauma surveillance, prevention, prehospital care, hospital care, and rehabilitation stages and discusses all in the context of infrastructure, workforce, service delivery, financing, information management, and governance. A small component of this policy involves facilitating safe training and recommendations for task-sharing models. Neurosurgeons from HICs can partner with LMICs as they formulate their National Surgical Plans and strive to address the burden of neurosurgical disease in their respective countries.
Figure 4.
Overall perspectives on task-shifting (red) and task-sharing (blue) practices. Data are arranged from most agreeable statements to most disagreeable according to task shifting. NS, specialist neurosurgeon; GP, general practitioner; GS, general surgeon; and NPP, nonphysician provider.
Economics of TS/S
It is paramount to consider the return on investment for neurosurgical workforce expansion and economic impact of TS/S. In a recent analysis by Rudolfson et al.,5 a value-of-output model predicted that failing to address the top 5 neurosurgical conditions in LMICs would amount to annual losses in gross domestic product of US$4.4 trillion during 2015–2030. However, workforce expansion requires substantial investment. In the Lancet Commission on Global Surgery report, it was estimated that the cost of scaling up the surgical, anesthetic, and obstetrician workforce to a minimum of 20 providers per 100,000 population would be between U.S. $71 billion and $146 billion and would take a median of 34,121 person years.33 However, if task sharing were used in a 4:1 associate clinician/specialist ratio, the cost and training time would be each reduced by 40%.1 The Técnicos de cirurgia in Mozambique is an example of cost-savings in a task-shifting model34; 30-year costs per major obstetric surgery were $38.9 for task-shifting proceduralists and $144.1 for specialist surgeons and obstetrician/gynecologists. Importantly, this was a task-shifting model, not a sharing model, so remuneration within task sharing may be different because specialists remain involved in consultation. Additional cost-effectiveness and cost-benefit studies should be performed for ongoing TS/S models to help frame discussions with ministries of health and ministries of finance to develop robust NSOAP plans and health budgets. Task sharing should not be seen as a quicker and cheaper option for care provision at the expense of investing in local residency training programs to develop fully trained and competent leaders who can champion future teams of task-sharing efforts.
Limitations
The limitations of this study warrant further discussion. Although efforts were made to represent a diverse sample of both HICs and LMICs across the 7 WHO regions, and we obtained returns from 105 of 194 WHO member countries (54.1%), with a total of 391 respondents (162 individuals from HICs and 229 from LMICs), this is a small sample of total neurosurgeons. In addition, a large percentage of respondents were from urban settings, and these individuals may have limited information about nonneurosurgeon providers and ongoing practices in rural or remote parts of the country. Consequently, the sample responses may not accurately represent perspectives held by the broader neurosurgeon community. Nonetheless, this study represents one of the first attempts to elucidate global perspectives on TS/S in neurosurgery and will facilitate further discussion on workforce solutions.
Conclusions
Given the global workforce deficit in neurosurgery, there is an increasing interest in the use of neurosurgical TS/S. However, TS/S remains highly controversial because of safety, ethical, financial, legal, and professional implications. This perspectives survey aimed to elucidate current perceptions of neurosurgical TS/S to guide the implementation of TS/S as a practical strategy for neurosurgical workforce expansion in LMICs. Both LMIC and HIC countries agreed that task sharing should be prioritized over task shifting and that additional recommendations and regulations could increase the level of care, such as additional governance by professional surgical societies, requiring standardized training, competency-based evaluation, clear role definition, maintenance of certification, adequate oversight, and proper referral networks for complex cases. Importantly, LMICs, in which TS/S occurs more often, were significantly more agreeable to additional structure and regulation for TS/S. These findings represent a call to action for future discussions on policy and training programs surrounding task sharing for neurosurgery in regions where there is an unmet burden of neurosurgical disease and a dearth of specialist neurosurgeons.
Declaration of Competing Interest
A.G.K. is supported by the National Institute for Health Research (NIHR) Global Health Research Group on Neurotrauma. The Group was commissioned by the NIHR using Official Development Assistance funding (project 16/137/105). The views expressed in this manuscript are those of the authors and are not necessarily those of the UK National Health Service, NIHR, or the UK Department of Health.
Acknowledgments
We would like to acknowledge those who served as expert consultants for survey creation (in addition to those who were coauthors in the writing of the article): Jeffrey Rosenfeld, Naci Balak, Ahmed Ammar, Magnus Tisel, Michael M. Haglund, Timothy R. Smith, Ivar Mendez, Jannick Brennum, Stephen Honeybul, Akira Matsumara, Severien Muneza, Andres Rubiano, Patrick Kamalo, Graham Fieggen, Basant Misra, Gene Bolles, David Adelson, Robert Dempsey, and Peter Hutchinson.
Footnotes
Kee B. Park and Marike L.D. Broekman are co-senior authors.
Contributor Information
Faith C. Robertson, Email: frobertson@partners.org.
Global Neurosurgery Survey Collaborators:
Jeffrey Rosenfeld, Naci Balak, Ahmed Ammar, Magnus Tisel, Michael Haglund, Timothy Smith, Ivar Mendez, Jannick Brennum, Stephen Honeybul, Akira Matsumara, Severien Muneza, Andres Rubiano, Patrick Kamalo, Graham Fieggen, Basant Misra, Gene Bolles, David Adelson, Robert Dempsey, Peter Hutchinson, Alexandrina Nikova, Osama Ghazala, Elubabor Buno, Shibashish Bhattacharjee, Takahiro Iizuka, Jafri Malin Abdullah, Bipin Chaurasia, Eghosa Morgan, Rodolfo E. Alcedo-Guardia, Lynne Lourdes N. Lucena, Kadir Oktay, Omar Ibrahim AbdAllah, Ahlem Saihi, Gacem Abdeldjalil, Mahi Asmaa, Claudio Yampolsky, Laura P. Saladino, Francisco Mannara, Sonal Sachdev, Benjamin Price, Vincent Joris, Nourou Dine Adeniran Bankole, Edgar M. Carrasco, Mirsad Hodzic, Marcos Wagner de Sousa Porto, Robson Amorim, Igor Lima Maldonado, Bizoza Yves, Gonzalo Suarez, Felipe Constanzo, Johanna Cecilia Valdeblanquez Atencio, Karen Alexa Ruiz Mora, Juan Manuel Rodriguez Gil, Kiriakos Paraskeva, Emrah Egemen, Trevcsor Ngamasata, Jeff Ntalaja, Antoine Beltchika, Glennie Ntsambi, Goertz Mirenge Dunia, Mahmoud M. Taha, Mohamed Arnaout, Ramez Kirollos, Mohamed Kassem, Omar Elwardany, Ahmed Negida, Birhanu Dolango, Mikael Aseged, Alemu Adise Mldie, Tsegazeab Laeke, Abenezer Aklilu, Esayas Adefris, Teemu Luoto, Rezai Jahromi Behnam, Emmanuel De Schlichting, Bougaci Nassim, Pierre Bourdillon, Martin N. Stienen, Stephan Lackermair, Franziska Anna Schmidt, Juergen Konczalla, Adrien Holzgreve, Andre Sagerer, Dieter M. Weinert, Paulette Kumi, Aaron Lawson McLean, James Loan, Julian Cahill, Simon Dockrell, Fardad T. Afshari, Paul May, Stephen Honeybul, Alkinoos Athanasiou, Steven Papadopoulos, Edroulfo-Georgios Espinoza, Athanasios Chatzisotiriou, Pavlos Vlachogiannis, Konstantina Karabatsou, Thanasis Paschalis, Christos Tsitsipanis, Gabriel Mauricio Longo Calderan, Ronny Leiva, Harsh Deora, Sreenivas Mukkamala, Dipesh Batra, Arvind Sukumaran, Kanishk Parmar, Anuj Bahl, Amit Agrawal, Nirankar Dev, Nikhil Thakur, Sanjay Behari, Chandrasekhar B.V.K. Yandrapati, Ritesh Bhoot, Pragnesh Bhatt, Uday Bhaumik, Manish Agrawal, Antony Thomas, Harish Chandrappa, Ankit Mathur, Petra Wahjoepramono, Selfy Oswari, Rafid Al-Mahfoudh, Abbas Alnaji, Nidal Abuhadrous, Bakr Abo Jarad, Ibrahim Nour, Or Cohen-Inbar, Roberto Colasanti, Alfredo Conti, Giovanni Raffa, Corrado Castrioto, Matteo M. Baccanelli, Santino Ottavio Tomasi, Matteo Zoli, Andrea Veroni, Andrea Di Cristofori, Luigi Giannachi, Laura Lippa, Donatella Sgubin, Morgan Broggi, Marcello Barbato, Francesco Restelli, Mario Ganau, Graziano Taddei, Hamzeh Albadawi, Mohammed Salameh, Madieyva Gulmira, Muffaq Lashhab, Walid El Gaddafi, Mohammad Altoumi, S.M. Manvinder, Davendran Kanesen, Mario Teo, Prabu Rau Sriram, Sarah Atiqah M. Zamri, Vayara Perumall Vinodh, Moussa Denou, Adyl Melhaoui, Oumaima Outani, Mahjouba Boutarbouch, Armin Gretschel, Pradhumna Yadav, Balgopal Karmacharya, Fatih Incekara, Hugo den Boogert, Buccket Argvoello Lopez, Hassane Ali Amadou, Danjuma Sale, Sanusi Bello, Poluyi Edward, Alvan-Emeka Ukachukwu, Evaristus Nwaribe, Ikechukwu Aniaku, Aliyu Baba Ndajiwo, Olabamidele Ayodele, Gyang Markus Bot, Sunday David Ndubuisu Achebe, Bakht Jamal, Muhammad Tariq, Ghulam Farooq, Tariq Khan, Danyal Zaman Khan, Ahtesham Khizar, Zahid Hussain, Anisa Nazir, Marco Gonzales-Portillo, Jhosep Silvestre Bautista, Roland A. Torres, Abigail Javier-Lizan, Isagani Jodl G. de los Santos, Jr., Nuno Morais, Lydia Dias, Carolina Noronha, Jovelo Monteiro Silva, Alexandra Seromenho-Santos, Kiril Lozanche, Ionut Negoi, Alexandru Tascu, Danil A. Kozyrev, Menelas Nkeshimana, Claire Karekezi, Marcel Didier Ndayishyigikiye, Faisal Alabbass, Faisal Farrash, Rawan Alhazmi, Jagos Golubovic, Milan Lepifá, Rosanda Ilifá, Aleksandar Stanimirovifá, Sergio Garcia-Garcia, Carlos A. Rodriguez Arias, Ruth Lau, Juan Delgado-Fernandez, Miguel A. Arraez, C. Fernandez Mateos, Ana M. Castano Leon, Saman Wadanamby, David Bervini, Hamisi K. Shabani, Kriengsak Limpastan, Khalil Ayadi, Altay Sencer, Ali Yalcinkaya, Elif Eren, Naci Balak, Recep Basaran, Abdulkerim Gokoglu, Vyval Mykola, Felicita Tayong, Gail Rosseau, Mario Zuccarello, Carolyn Quinsey, Michael C. Dewan, Paul H. Young, Edward Laws, Jack Rock, David B. Kurland, Carrie R. Muh, Eri Dario Delgado Aguilar, Kenneth Burns, Jacob Low, Conor Keogh, Chris Uff, Alfio Spina, and Fayez Alelyani
Supplementary Data
References
- 1.Dare A.J., Bleicher J., Lee K.C. Generation of national political priority for surgery: a qualitative case study of three low-income and middle-income countries. Lancet. 2015;385(suppl 2):S54. doi: 10.1016/S0140-6736(15)60849-2. [DOI] [PubMed] [Google Scholar]
- 2.Smith S.L., Shiffman J. Setting the global health agenda: the influence of advocates and ideas on political priority for maternal and newborn survival. Soc Sci Med. 2016;166:86–93. doi: 10.1016/j.socscimed.2016.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ahmed F., Michelen S., Massoud R., Kaafarani H. Are the SDGs leaving safer surgical systems behind? Int J Surg. 2016;36:74–75. doi: 10.1016/j.ijsu.2016.09.095. [DOI] [PubMed] [Google Scholar]
- 4.Barthelemy E.J., Park K.B., Johnson W. Neurosurgery and Sustainable Development Goals. World Neurosurg. 2018;120:143–152. doi: 10.1016/j.wneu.2018.08.070. [DOI] [PubMed] [Google Scholar]
- 5.Rudolfson N., Dewan M.C., Park K.B., Shrime M.G., Meara J.G., Alkire B.C. The economic consequences of neurosurgical disease in low- and middle-income countries [e-pub ahead of print] J Neurosurg. 2018 doi: 10.3171/2017.12.JNS17281. https://doi.org/10.3171/2017.12.JNS17281. [DOI] [PubMed] [Google Scholar]
- 6.Dewan M.C., Rattani A., Fieggen G. Global neurosurgery: the current capacity and deficit in the provision of essential neurosurgical care. Executive Summary of the Global Neurosurgery Initiative at the Program in Global Surgery and Social Change [e-pub ahead of print] J Neurosurg. 2018 doi: 10.3171/2017.11.JNS171500. https://doi.org/10.3171/2017.11.JNS171500. [DOI] [PubMed] [Google Scholar]
- 7.Dewan M.C., Rattani A., Gupta S. Estimating the global incidence of traumatic brain injury [e-pub ahead of print] J Neurosurg. 2018 doi: 10.3171/2017.10.JNS17352. https://doi.org/10.3171/2017.10.JNS17352. [DOI] [PubMed] [Google Scholar]
- 8.El Khamlichi A. Neurosurgery in Africa. Clin Neurosurg. 2005;52:214–217. [PubMed] [Google Scholar]
- 9.Park K.B., Johnson W.D., Dempsey R.J. Global neurosurgery: the unmet need. World Neurosurg. 2016;88:32–35. doi: 10.1016/j.wneu.2015.12.048. [DOI] [PubMed] [Google Scholar]
- 10.Corley J., Lepard J., Barthelemy E., Ashby J.L., Park K.B. Essential neurosurgical workforce needed to address neurotrauma in low- and middle-income countries. World Neurosurg. 2019;123:295–299. doi: 10.1016/j.wneu.2018.12.042. [DOI] [PubMed] [Google Scholar]
- 11.Corley J.A., Rosseau G. Encore careers: a solution to the unmet need in global neurosurgical care [e-pub ahead of print] J Neurosurg. 2019 doi: 10.3171/2018.11.JNS183298. https://doi.org/10.3171/2018.11.JNS183298. [DOI] [PubMed] [Google Scholar]
- 12.Mullan F., Frehywot S. Non-physician clinicians in 47 sub-Saharan African countries. Lancet. 2007;370:2158–2163. doi: 10.1016/S0140-6736(07)60785-5. [DOI] [PubMed] [Google Scholar]
- 13.Chu K., Rosseel P., Gielis P., Ford N. Surgical task shifting in Sub-Saharan Africa. PLoS Med. 2009;6:e1000078. doi: 10.1371/journal.pmed.1000078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burton A. Training non-physicians as neurosurgeons in sub-Saharan Africa. Lancet Neurol. 2017;16:684–685. doi: 10.1016/S1474-4422(17)30246-6. [DOI] [PubMed] [Google Scholar]
- 15.Bartelme T. Beacon Press; Boston, MA: 2017. A Surgeon in the Village: An American Doctor Teaches Brain Surgery in Africa. [Google Scholar]
- 16.World Health Organization . World Health Organization; Geneva: 2008. Task Shifting: Global Recommendations and Guidelines. [Google Scholar]
- 17.Ashengo T., Skeels A., Hurwitz E.J.H., Thuo E., Sanghvi H. Bridging the human resource gap in surgical and anesthesia care in low-resource countries: a review of the task sharing literature. Hum Resour Health. 2017;15:77. doi: 10.1186/s12960-017-0248-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robertson F., Briones R., Baticulon R., Leather A., Gormley W., Lucena L. King’s College; London: 2018. Is Task-sharing a Safe Solution to the Neurosurgery Workforce Deficit? A Retrospective Cohort Study in the Philippines. MSc Thesis, Global Health with Global Surgery. [Google Scholar]
- 19.Luck T., Treacy P.J., Mathieson M., Sandilands J., Weidlich S., Read D. Emergency neurosurgery in Darwin: still the generalist surgeons' responsibility. ANZ J Surg. 2015;85:610–614. doi: 10.1111/ans.13138. [DOI] [PubMed] [Google Scholar]
- 20.McCampbell C., Helmer O. An experimental application of the Delphi method to the use of experts. Management Science. 1993;9:458–467. [Google Scholar]
- 21.Meara J.G., Leather A.J., Hagander L. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Surgery. 2015;158:3–6. doi: 10.1016/j.surg.2015.04.011. [DOI] [PubMed] [Google Scholar]
- 22.Kempthorne P., Morriss W.W., Mellin-Olsen J., Gore-Booth J. The WFSA Global Anesthesia Workforce Survey. Anesth Analg. 2017;125:981–990. doi: 10.1213/ANE.0000000000002258. [DOI] [PubMed] [Google Scholar]
- 23.Mahmud M.R., Mansur Idris M. A glance at neurosurgery in Nigeria Following the 3rd CAANS Congress. 2018. https://aansneurosurgeon.org/inside-neurosurgeon/a-glance-at-neurosurgery-in-nigeria-following-the-3rd-caans-congress/ Available at: Accessed Jan 5, 2019.
- 24.European Association of Neurosurgical Societies The European Association of Neurosurgical Societies Congress. 2019. https://www.eans.org/ Available at: Accessed April 10, 2019.
- 25.World Bank New country classifications by income level: 2018. https://blogs.worldbank.org/opendata/new-country-classifications-income-level-2018-2019 Available at: Accessed July 5, 2018.
- 26.Robertson F.C., Briones R.A., Mekary R.E. Task-sharing for emergency neurosurgery: A Retrospective Cohort Study in the Philippines. World Neurosurg. 2019:100058. doi: 10.1016/j.wnsx.2019.100058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hafner T., Shiffman J. The emergence of global attention to health systems strengthening. Health Policy Plan. 2013;28:41–50. doi: 10.1093/heapol/czs023. [DOI] [PubMed] [Google Scholar]
- 28.Smith M. Is task sharing preferred to task shifting in the provision of safe surgical care? Surgery. 2018;164:559–560. doi: 10.1016/j.surg.2018.05.005. [DOI] [PubMed] [Google Scholar]
- 29.Program in Global Surgery and Social Change National Surgical Planning. https://www.pgssc.org/national-surgical-planning Available at: Accessed May 15, 2019.
- 30.Burssa D., Teshome A., Iverson K. Safe surgery for all: early lessons from implementing a national government-driven surgical plan in Ethiopia. World J Surg. 2017;41:3038–3045. doi: 10.1007/s00268-017-4271-5. [DOI] [PubMed] [Google Scholar]
- 31.Park K., Khan T., Olufemi Adeleye A. Comprehensive Policy Recommendations for Head and Spine Injury Care in LMICs. 2019. https://docs.wixstatic.com/ugd/d9a674_1ba60c38a07341a7bbbe8b1e3f0ff507.pdf Available at: Accessed June 3, 2019. [DOI] [PubMed]
- 32.Figaji A., Taylor A., Mahmud M.R. On progress in Africa, by African experts. Lancet Neurol. 2018;17:114. doi: 10.1016/S1474-4422(17)30457-X. [DOI] [PubMed] [Google Scholar]
- 33.Daniels K.M., Riesel J.N., Meara J.G. The scale-up of the surgical workforce. Lancet. 2015;385(suppl 2):S41. doi: 10.1016/S0140-6736(15)60836-4. [DOI] [PubMed] [Google Scholar]
- 34.Kruk M.E., Pereira C., Vaz F., Bergstrom S., Galea S. Economic evaluation of surgically trained assistant medical officers in performing major obstetric surgery in Mozambique. BJOG. 2007;114:1253–1260. doi: 10.1111/j.1471-0528.2007.01443.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.