Abstract
We evaluated the visual outcome of combined penetrating keratoplasty (PKP) and 25G pars plana vitrectomy (PPV) performed without a temporary keratoprosthesis or endoscopy in a patient with vitreoretinal disease complicated by severe corneal opacity. The patient was a 68-year-old woman who had severe corneal opacity and silicone oil in her left eye after several previous intraocular surgeries for rhegmatogenous retinal detachment and proliferative vitreoretinopathy. We successfully performed a combined surgery of conventional PKP followed by 25G PPV without the use of a keratoprosthesis. At 6 months after surgery, visual acuity had not improved, and the density of corneal endothelial cells of the donor cornea had declined from 3,205 to 1,969 cells/mm<sup>2</sup>. However, corneal transparency remained good, and additional surgery for vitreoretinal disease was not necessary. The combined surgical procedure designed to minimize the number of open-sky steps and to limit vitreoretinal complications thus proved to be safe and achieved stable corneal clarity in a patient with vitreoretinal disease and severe corneal opacity.
Keywords: 25G pars plana vitrectomy, Penetrating keratoplasty, Combined surgery, Keratoprosthesis, Corneal opacity
Introduction
Corneal opacity occurs as a primary or secondary condition and impedes observation of the ocular fundus. In individuals with vitreoretinal diseases, severe corneal opacity necessitates the use of a temporary keratoprosthesis or endoscopy for performance of vitreoretinal surgery [1, 2, 3]. Such procedures are not optimal and are often inconvenient; however, with endoscopy providing a narrow field of view at low resolution. Furthermore, the corneal opacity remaining after surgery with endoscopy hinders patient management and further observation of the ocular fundus.
Penetrating keratoplasty (PKP) is an open-sky corneal transplantation surgery in which the full-thickness cornea of the patient is resected and a donor cornea implanted [4]. Lamellar corneal surgery such as lamellar keratoplasty and endothelium transplantation (DSAEK) has recently been developed as an alternative to PKP [5, 6, 7, 8]. Such surgery replaces only the diseased portion of the host cornea, leaving the healthy portion intact, and it has been found to be associated with a better recovery of visual acuity (VA) and fewer intraoperative or postoperative complications including a lower incidence of rejection and greater resistance to trauma compared with PKP [9, 10]. In addition to graft rejection or failure, complications of PKP include the development of bacterial keratitis and secondary glaucoma [11, 12, 13, 14, 15]. It is also important to minimize the risk of expulsive hemorrhage during the open-sky period of PKP, and a technique to avoid the open-sky condition during PKP has been described [16].
A wide-angle viewing system has been developed to provide a panoramic image of the fundus for the safe and efficient performance of vitreoretinal surgery, even in eyes with a small pupil [17]. In addition, the combination of this system with chandelier lighting provides a good view of the peripheral region of the retina and allows implementation of the bimanual technique for vitrectomy [18, 19]. Chandelier illumination is also effective for the performance of cataract surgery in patients with severe corneal opacity [20]. These developments have contributed to the widespread application of microincisional vitrectomy surgery to the treatment of various vitreoretinal pathologies including severe vitreoretinal diseases such as proliferative diabetic retinopathy and proliferative vitreoretinopathy (PVR).
We here report the results of simultaneous PKP and 25G pars plana vitrectomy (PPV) without the use of a keratoprosthesis or endoscopy in a patient with severe corneal opacity and silicone oil in her eye as a result of several previous intraocular surgeries for rhegmatogenous retinal detachment and PVR.
Case Report
A 68-year-old woman was referred to our Department for the performance of PKP and PPV. Her left eye had severe corneal opacity due to bullous keratopathy, and silicone oil was present in the eye as the result of prior intraocular surgeries for rhegmatogenous retinal detachment and PVR. The VA of her left eye was 3/20, and we were not able to perform satisfactory funduscopy because of the corneal opacity, although retinal detachment was evident.
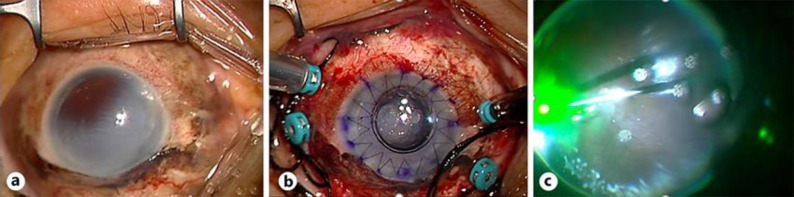
Surgery was performed with the patient under general anesthesia. We initially performed conventional PKP followed by 25G PPV without the use of a keratoprosthesis (Fig. 1). In brief, the scleral ring was sutured with 7–0 silk, the host cornea was excised at a diameter of 8.0 mm with the use of a Hessburg-Barron trephine (Katena, Denville, NJ, USA), and the donor cornea was punched out at a diameter of 8.25 mm with a Barron donor punch (Katena) and was sutured with 10–0 Ethilon. After PKP, with the donor cornea in place, we performed vitrectomy with a Constellation 25G system (Alcon, Hünenberg, Switzerland) and with a wide-angle viewing system (Resight noncontact wide-angle lenses; Carl Zeiss Meditec, Jena, Germany) to observe the fundus. The procedure was a standardized four-channel vitrectomy, with the four channels being made with 25G trocar needles at a distance of 4 mm from the limbus. Chandelier illumination was fixed to provide wide-angle diffuse lighting. The proliferative membrane was peeled away and removed with 25G forceps and 25G vertical or horizontal scissors (Alcon). Exchange of intraocular fluid was performed. Finally, the four cannulas were removed, the eye was tamponaded with SF6, and the sclerotomies were sutured with 8-0 Vicryl.
Fig. 1.
Surgery for the left eye of the study patient. a Corneal clouding as a result of bullous keratopathy. b After PKP, four 25G ports were made for PPV. c Laser irradiation for repositioning of the detached retina. The view through the transplanted donor cornea was good.
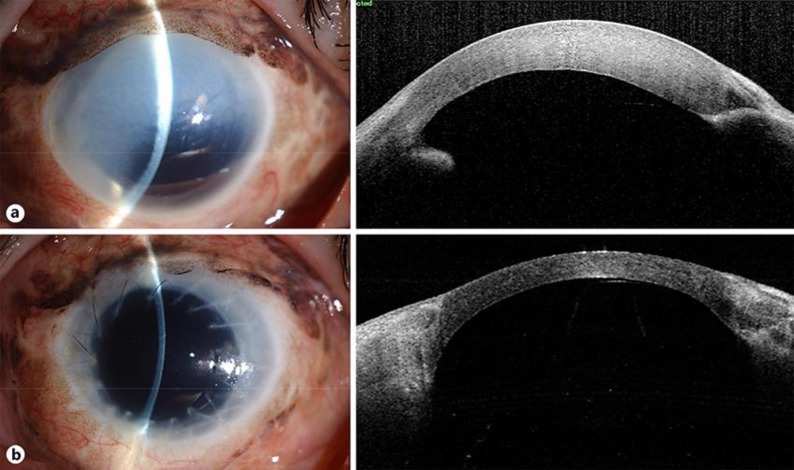
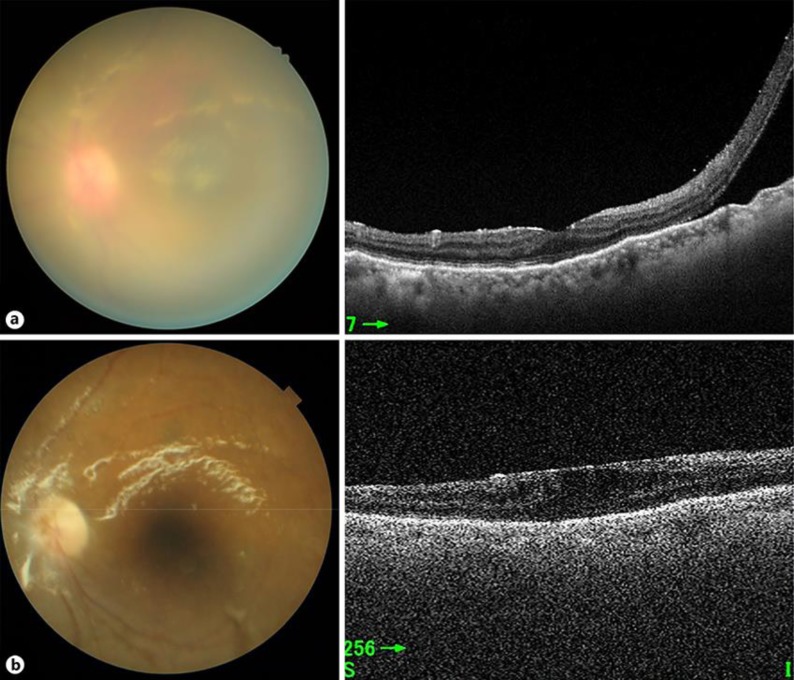
The donor graft remained clear during the operation and therefore did not hinder the procedure, and perforation of the cornea did not occur. Images obtained from the patient before and 6 months after the surgery are shown in Figure 2 and 3, and other findings are presented in Table 1. Although VA was decreased at 6 months post-surgery, there were no serious postoperative complications including vitreoretinal events. Intraocular pressure was not increased after surgery. The donor graft remained clear, so that we were able to perform postoperative funduscopy. The density of the donor corneal endothelial cells had declined from 3,205 to 1,969 cells/mm2 at 6 months after surgery. Retinal redetachment did not occur after surgery.
Fig. 2.
Anterior ocular segment images of the patient's left eye before (a) and 6 months after surgery (b). a Corneal clouding was apparent due to bullous keratopathy, and the cornea appeared thickened. Left and right images were obtained with a slitlamp microscope and by optical coherence tomography, respectively. b The transplanted cornea was clear and of normal thickness.
Fig. 3.
Posterior ocular segment images of the patient's left eye before (a) and 6 months after surgery (b). a Retinal detachment was apparent by optical coherence tomography (right), but it was difficult to perform funduscopy (left). b The transplanted cornea remained clear, so it was possible to perform funduscopy, and retinal redetachment had not occurred.
Table 1.
Study patient's outcome at 6 months after surgery
| Visual acuity |
Intraocular pressure, mm Hg |
Endothelial cell density of donor cornea, cells/mm2 |
|||
|---|---|---|---|---|---|
| pre | post | pre | post | pre | post |
| 3/20 | 1.8/20 | 2 | 2 | 3,205 | 1,969 |
Discussion
We have here presented clinical data for a patient treated simultaneously by PKP and 25G PPV without the use of a keratoprosthesis or endoscopy. The cornea remained transparent after surgery, and retinal detachment did not recur. Although there was a decline in VA and endothelial cell density apparent 6 months after compared with before surgery, our results thus suggest that simultaneous PKP and PPV without the use of a keratoprosthesis or endoscopy is a potential new surgical treatment option that is less traumatic and shorter in duration than existing options for patients with vitreoretinal conditions and severe corneal opacity.
Because the patient's IOP was 2 mm Hg before surgery, which is generally called hypotony, we performed the surgery very carefully. As a result, IOP was not changed between before and after surgery. Eyes that have undergone previous vitreoretinal surgeries have been reported to be susceptible to hypotony [21]. Hypotony may coexist with complications such as maculopathy and choroidal detachment, but there were no such complications in the present patient. However, careful monitoring of patients for hypotony after our surgical procedure is still warranted.
A keratoprosthesis is usually used for vitrectomy in patients with severe corneal opacity [22, 23, 24]. The number of open-sky steps during such surgery with a keratoprosthesis is twice that for our surgical procedure. Open-sky steps can lead to complications during corneal surgery, such as expulsive suprachoroidal hemorrhage during PKP. The frequency of suprachoroidal hemorrhage has been found to be 0.45–0.56% during or after PKP with or without a keratoprosthesis [25, 26, 27, 28]. Suprachoroidal hemorrhage did not occur during our surgical procedure, suggesting that the combination of PKP with vitrectomy in the absence of a keratoprosthesis may increase safety.
Endoscopy is sometimes adopted for vitrectomy in patients with severe corneal opacity that obscures the fundus [29, 30, 31]. Anatomic structure and visual function of the retina were found to be improved by 25G endoscopic vitrectomy in all studied patients with PVR and severe corneal opacity [32]. Vitrectomy with endoscopy as a surgical technique is difficult to perform; however, our combined surgical procedure is more straightforward and did not give rise to complications such as retinal redetachment or vitreous hemorrhage. Our procedure may thus be more convenient and safer than vitrectomy with endoscopy.
A wide-angle viewing system provides a panoramic view of the fundus and thereby increases the safety and efficiency of vitreoretinal surgery, even in eyes with a small pupil or corneal opacity [17]. In addition, such a system with chandelier lighting also provides a good view of the peripheral region of the retina and allows implementation of the bimanual technique for vitrectomy [18, 19]. The further development of instruments may improve the success of our combination surgery for patients with severe corneal opacity and vitreoretinal diseases.
The corneal endothelium plays a key role in the maintenance of corneal transparency. Corneal damage induced by inflammation, infection, or trauma including surgery can lead to endothelial cell loss. Loss of corneal endothelial cells (density of 1,500–2,000 cells/mm2) was found to be apparent 1 year after PKP [33, 34]. The decrease in the number of endothelial cells after PKP is associated with various risk factors including donor graft status, recipient factors and operation in these pathological processes [35, 36, 37]. In the present patient, corneal endothelial cell density at 6 months after surgery was 1,969 cells/mm2, corresponding to an endothelial cell loss of 1,236 cells/mm2. These results demonstrate that our combination surgery has no great influence on corneal endothelial cells after surgery. Further studies remain to be performed.
Unfortunately, the patient was transferred to another hospital before we were able to perform an assessment at 12 months post-surgery. Nevertheless, her endothelial cell density was sufficient to maintain transparency of the corneal graft for up to 6 months. Simultaneous PKP and PPV without a keratoprosthesis or endoscopy thus appears to support maintenance of an adequate corneal endothelial cell density for preservation of corneal transparency after surgery. Corneal transparency might be improved further by the use of a larger donor graft, given that larger grafts have been found to be associated with higher endothelial cell density in the first decade after surgery [38, 39]. Such larger grafts may also be associated with a higher risk of graft rejection and secondary glaucoma, however.
In conclusion, combined PKP and PPV with the implantation of a donor cornea appears to be a safe and effective option for the management of complicated retinal detachment in the presence of severe corneal opacity. It could lead to a clear cornea graft at least in the short term. This procedure may be considered as an alternative option when surgical time has to be shortened and when the donor graft has a good endothelial cell count. Longer studies would be valuable and welcome.
Statement of Ethics
Informed consent was obtained from the patient, and the study protocol was reviewed and approved by Yamaguchi University Hospital Institutional Review Board. The study was conducted in accordance with the Declaration of Helsinki.
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contributions
Takuya Yoshimoto designed the study and wrote the initial draft of the manuscript. Kazuhiro Kimura contributed to the analysis and interpretation of data and assisted in the preparation of the manuscript. All other authors have contributed to data collection and interpretation, and critically reviewed the manuscript. All authors approved the final version of the manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Acknowledgements
We wish to thank the timely help given by the medical staff of Yamaguchi University Hospital in medical practice.
References
- 1.Harissi-Dagher M, Durr GM, Biernacki K, Sebag M, Rhéaume MA. Pars plana vitrectomy through the Boston Keratoprosthesis type 1. Eye (Lond) 2013 Jun;27((6)):767–9. doi: 10.1038/eye.2013.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morishita S, Kita M, Yoshitake S, Hirose M, Oh H. 23-gauge vitrectomy assisted by combined endoscopy and a wide-angle viewing system for retinal detachment with severe penetrating corneal injury: a case report. Clin Ophthalmol. 2011;5:1767–70. doi: 10.2147/OPTH.S25373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roters S, Hamzei P, Szurman P, Hermes S, Thumann G, Bartz-Schmidt KU, et al. Combined penetrating keratoplasty and vitreoretinal surgery with silicone oil: a 1-year follow-up. Graefes Arch Clin Exp Ophthalmol. 2003 Jan;241((1)):24–33. doi: 10.1007/s00417-002-0587-3. [DOI] [PubMed] [Google Scholar]
- 4.Ing JJ, Ing HH, Nelson LR, Hodge DO, Bourne WM. Ten-year postoperative results of penetrating keratoplasty. Ophthalmology. 1998 Oct;105((10)):1855–65. doi: 10.1016/S0161-6420(98)91030-2. [DOI] [PubMed] [Google Scholar]
- 5.Maier P, Reinhard T, Cursiefen C. Descemet stripping endothelial keratoplasty—rapid recovery of visual acuity. Dtsch Arztebl Int. 2013 May;110((21)):365–71. doi: 10.3238/arztebl.2013.0365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Price MO, Gorovoy M, Price FW, Jr, Benetz BA, Menegay HJ, Lass JH. Descemet's stripping automated endothelial keratoplasty: three-year graft and endothelial cell survival compared with penetrating keratoplasty. Ophthalmology. 2013 Feb;120((2)):246–51. doi: 10.1016/j.ophtha.2012.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ang M, Mehta JS, Anshu A, Wong HK, Htoon HM, Tan D. Endothelial cell counts after Descemet's stripping automated endothelial keratoplasty versus penetrating keratoplasty in Asian eyes. Clin Ophthalmol. 2012;6:537–44. doi: 10.2147/OPTH.S26343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alqudah AA, Terry MA, Straiko MD, Greiner MA, Davis-Boozer D. Immediate endothelial cell loss after penetrating keratoplasty. Cornea. 2013 Dec;32((12)):1587–90. doi: 10.1097/ICO.0b013e3182a73822. [DOI] [PubMed] [Google Scholar]
- 9.Baydoun L, Tong CM, Tse WW, Chi H, Parker J, Ham L, et al. Endothelial cell density after descemet membrane endothelial keratoplasty: 1 to 5-year follow-up. Am J Ophthalmol. 2012 Oct;154((4)):762–3. doi: 10.1016/j.ajo.2012.06.025. [DOI] [PubMed] [Google Scholar]
- 10.Anshu A, Price MO, Price FW., Jr Risk of corneal transplant rejection significantly reduced with Descemet's membrane endothelial keratoplasty. Ophthalmology. 2012 Mar;119((3)):536–40. doi: 10.1016/j.ophtha.2011.09.019. [DOI] [PubMed] [Google Scholar]
- 11.Sugar J. The collaborative corneal transplantation studies. Arch Ophthalmol. 1992 Nov;110((11)):1517–8. doi: 10.1001/archopht.1992.01080230015004. [DOI] [PubMed] [Google Scholar]
- 12.Williams KA, Roder D, Esterman A, Muehlberg SM, Coster DJ. Factors predictive of corneal graft survival. Report from the Australian Corneal Graft Registry. Ophthalmology. 1992 Mar;99((3)):403–14. doi: 10.1016/s0161-6420(92)31960-8. [DOI] [PubMed] [Google Scholar]
- 13.Vail A, Gore SM, Bradley BA, Easty DL, Rogers CA, Armitage WJ. Conclusions of the corneal transplant follow up study. Collaborating Surgeons. Br J Ophthalmol. 1997 Aug;81((8)):631–6. doi: 10.1136/bjo.81.8.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sit M, Weisbrod DJ, Naor J, Slomovic AR. Corneal graft outcome study. Cornea. 2001 Mar;20((2)):129–33. doi: 10.1097/00003226-200103000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Tan DT, Janardhanan P, Zhou H, Chan YH, Htoon HM, Ang LP, et al. Penetrating keratoplasty in Asian eyes: the Singapore Corneal Transplant Study. Ophthalmology. 2008 Jun;115((6)):975–982.e1. doi: 10.1016/j.ophtha.2007.08.049. [DOI] [PubMed] [Google Scholar]
- 16.Arslan OS, Unal M, Arici C, Cicik E, Mangan S, Atalay E. Novel method to avoid the open-sky condition in penetrating keratoplasty: covered cornea technique. Cornea. 2014 Sep;33((9)):994–8. doi: 10.1097/ICO.0000000000000186. [DOI] [PubMed] [Google Scholar]
- 17.Inoue M. Wide-angle viewing system. Dev Ophthalmol. 2014;54:87–91. doi: 10.1159/000360453. [DOI] [PubMed] [Google Scholar]
- 18.Eckardt C. Twin lights: a new chandelier illumination for bimanual surgery. Retina. 2003 Dec;23((6)):893–4. doi: 10.1097/00006982-200312000-00039. [DOI] [PubMed] [Google Scholar]
- 19.Eckardt C, Eckert T, Eckardt U. 27-gauge Twinlight chandelier illumination system for bimanual transconjunctival vitrectomy. Retina. 2008 Mar;28((3)):518–9. doi: 10.1097/IAE.0b013e3181607a0f. [DOI] [PubMed] [Google Scholar]
- 20.Oshima Y, Shima C, Maeda N, Tano Y. Chandelier retroillumination-assisted torsional oscillation for cataract surgery in patients with severe corneal opacity. J Cataract Refract Surg. 2007 Dec;33((12)):2018–22. doi: 10.1016/j.jcrs.2007.07.055. [DOI] [PubMed] [Google Scholar]
- 21.Mimouni M, Abualhasan H, Derman L, Feldman A, Mazzawi F, Barak Y. INCIDENCE AND RISK FACTORS FOR HYPOTONY AFTER 25-GAUGE PARS PLANA VITRECTOMY WITH NONEXPANSILE ENDOTAMPONADE. Retina. 2018 Jan;40((1)):41–46. doi: 10.1097/IAE.0000000000002336. [DOI] [PubMed] [Google Scholar]
- 22.Lee DS, Heo JW, Choi HJ, Kim MK, Wee WR, Oh JY. Combined corneal allotransplantation and vitreoretinal surgery using an Eckardt temporary keratoprosthesis: analysis for factors determining corneal allograft survival. Clin Ophthalmol. 2014 Feb;8:449–54. doi: 10.2147/OPTH.S60008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yan H, Cui J, Zhang J, Chen S, Xu Y. Penetrating keratoplasty combined with vitreoretinal surgery for severe ocular injury with blood-stained cornea and no light perception. Ophthalmologica Journal international d'ophtalmologie International journal of ophthalmology. Z Augenheilkd. 2006;220:186–9. doi: 10.1159/000091763. [DOI] [PubMed] [Google Scholar]
- 24.Kiang L, Sippel KC, Starr CE, Ciralsky J, Rosenblatt MI, Radcliffe NM, et al. Vitreoretinal surgery in the setting of permanent keratoprosthesis. Arch Ophthalmol. 2012 Apr;130((4)):487–92. doi: 10.1001/archophthalmol.2011.1115. [DOI] [PubMed] [Google Scholar]
- 25.Ingraham HJ, Donnenfeld ED, Perry HD. Massive suprachoroidal hemorrhage in penetrating keratoplasty. Am J Ophthalmol. 1989 Dec;108((6)):670–5. doi: 10.1016/0002-9394(89)90859-3. [DOI] [PubMed] [Google Scholar]
- 26.Gloor B, Kalman A. [Choroidal effusion and expulsive hemorrhage in penetrating interventions—lesson from 26 patients] Klin Monatsbl Augenheilkd. 1993 Mar;202((3)):224–37. doi: 10.1055/s-2008-1045587. [DOI] [PubMed] [Google Scholar]
- 27.Price FW, Jr, Whitson WE, Ahad KA, Tavakkoli H. Suprachoroidal hemorrhage in penetrating keratoplasty. Ophthalmic Surg. 1994 Aug;25((8)):521–5. [PubMed] [Google Scholar]
- 28.Patel SV, Hodge DO, Bourne WM. Corneal endothelium and postoperative outcomes 15 years after penetrating keratoplasty. Am J Ophthalmol. 2005 Feb;139((2)):311–9. doi: 10.1016/j.ajo.2004.09.045. [DOI] [PubMed] [Google Scholar]
- 29.Ayyildiz O, Hakan Durukan A. Comparison of endoscopic-assisted and temporary keratoprosthesis-assisted vitrectomy in combat ocular trauma: experience at a tertiary eye center in Turkey. J Int Med Res. 2018 Jul;46((7)):2708–16. doi: 10.1177/0300060518769798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huang YF, Chang CJ. Endoscope-assisted vitrectomy in the management of retinal detachment with corneal opacity. Taiwan J Ophthalmol. 2017 Jul-Sep;7((3)):164–7. doi: 10.4103/tjo.tjo_25_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Marra KV, Yonekawa Y, Papakostas TD, Arroyo JG. Indications and techniques of endoscope assisted vitrectomy. J Ophthalmic Vis Res. 2013 Jul;8((3)):282–90. [PMC free article] [PubMed] [Google Scholar]
- 32.Kita M, Fujii Y, Hama S. Twenty five-gauge endoscopic vitrectomy for proliferative vitreoretinopathy with severe corneal opacity. Jpn J Ophthalmol. 2018 May;62((3)):302–6. doi: 10.1007/s10384-018-0578-5. [DOI] [PubMed] [Google Scholar]
- 33.Bertelmann E, Pleyer U, Rieck P. Risk factors for endothelial cell loss post-keratoplasty. Acta Ophthalmol Scand. 2006 Dec;84((6)):766–70. doi: 10.1111/j.1600-0420.2006.00726.x. [DOI] [PubMed] [Google Scholar]
- 34.Price MO, Gorovoy M, Benetz BA, Price FW, Jr, Menegay HJ, Debanne SM, et al. Descemet's stripping automated endothelial keratoplasty outcomes compared with penetrating keratoplasty from the Cornea Donor Study. Ophthalmology. 2010 Mar;117((3)):438–44. doi: 10.1016/j.ophtha.2009.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chung SH, Kim HK, Kim MS. Corneal endothelial cell loss after penetrating keratoplasty in relation to preoperative recipient endothelial cell density. Ophthalmologica Journal international d'ophtalmologie International journal of ophthalmology. Z Augenheilkd. 2010;224:194–8. doi: 10.1159/000252983. [DOI] [PubMed] [Google Scholar]
- 36.Ku BI, Hsieh YT, Hu FR, Wan IJ, Chen WL, Hou YC. Endothelial cell loss in penetrating keratoplasty, endothelial keratoplasty, and deep anterior lamellar keratoplasty. Taiwan J Ophthalmol. 2017 Oct-Dec;7((4)):199–204. doi: 10.4103/tjo.tjo_55_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shimazaki J, Shimmura S, Ishioka M, Tsubota K. Randomized clinical trial of deep lamellar keratoplasty vs penetrating keratoplasty. Am J Ophthalmol. 2002 Aug;134((2)):159–65. doi: 10.1016/s0002-9394(02)01523-4. [DOI] [PubMed] [Google Scholar]
- 38.Lass JH, Benetz BA, Gal RL, Kollman C, Raghinaru D, Dontchev M, et al. Writing Committee for the Cornea Donor Study Research Group Donor age and factors related to endothelial cell loss 10 years after penetrating keratoplasty: Specular Microscopy Ancillary Study. Ophthalmology. 2013 Dec;120((12)):2428–35. doi: 10.1016/j.ophtha.2013.08.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Terry MA, Li J, Goshe J, Davis-Boozer D. Endothelial keratoplasty: the relationship between donor tissue size and donor endothelial survival. Ophthalmology. 2011 Oct;118((10)):1944–9. doi: 10.1016/j.ophtha.2011.02.023. [DOI] [PubMed] [Google Scholar]